Abstract
The COVID-19 pandemic has had a severe impact on mental health worldwide, with increased rates of anxiety and depression widely documented. The aim of this study was to examine unguided low intensity cognitive behaviour therapy for anxiety and depression during the pandemic. A sample of 225 individuals in Australia and the United Kingdom (M age 37.79, SD = 14.02, range 18–80 years; 85% female) were randomised into intervention or waitlist control. The intervention group demonstrated significant decreases in anxiety (d = 0.36 [0.18, 0.54]) and depression (d = 0.28 [0.11, 0.45]) compared to controls. The majority of participants (96%) rated the intervention as useful, and most (83%) reported they spent 30 min or less reading the guide, with 83% agreeing the intervention was easy to read. The results indicate that low intensity cognitive behaviour therapy has efficacy in reducing anxiety and depression during the COVID-19 pandemic. There is an urgent need to disseminate low intensity psychological therapies to improve mental health in this challenging time.
Keywords: Cognitive behaviour therapy, COVID-19, Pandemic, Low intensity, Anxiety, Depression, Randomised trial
Increases in anxiety and depression in response to the COVID-19 pandemic have been documented worldwide. Recent studies with over 17,000 people in the United Kingdom (UK) (Pierce et al., 2020) and over 300,000 people in the United States (US) (Twenge & Joiner, 2020) found significantly increased rates of anxiety and depression during the pandemic compared to pre COVID-19. Holmes et al. (2020) reported individuals in the UK rated the prospect of becoming physically unwell as a lower concern compared to the response to the pandemic (e.g., social distancing and resultant social isolation). In Australia, Dawel et al. (2020) conducted a survey of 1296 adults, and found elevated anxiety on the Generalised Anxiety Disorder questionnaire (GAD-7; Spitzer et al., 2006) (M = 4.4) and depression on the Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001) (M = 5.4) compared to population norms, similar to rates seen in the UK (GAD-7, M = 5.7; PHQ-9, M = 6.6; Fancourt et al., 2020). The COVID-19 pandemic in Australia worsened since this survey was completed. At the time of Dawel et al.’s (2020) survey there had been 19 deaths, whereas at the time of writing in April 2021 there have been 910 deaths. A second wave in the state of Victoria, Australia, resulted in a higher number of cases and deaths and a stringent lockdown (including travel no more than 5 km from one's residence and night time curfews), and the longest COVID lockdown worldwide to date, lasting for 112 days. COVID-19 is increasing exponentially in many regions, with documented negative mental health impacts in the United States (e.g., Fitzpatrick et al., 2020), India (e.g., Verma & Mishra, 2020) and Europe (e.g., Gonzalez-Sanguino et al., 2020). There is an urgent need to address the increased mental health problems as a result of the pandemic.
Low-intensity Cognitive Behaviour Therapy (CBT) is a scalable intervention which could be widely disseminated during the pandemic, and is defined as a CBT intervention which utilises self-help materials as either unguided or guided interventions, with no more than 6 h of guidance (Shafran et al., 2021). The successful wide-scale roll-out of low-intensity CBT in the UK through the Increasing Access to Psychological Therapies (IAPT) scheme has demonstrated effectiveness, as well as significant cost savings to the health system (Clark, 2018). It also meets an important gap in service provision, as there is an insufficient number of CBT specialists to meet demand worldwide (Fairburn & Patel, 2014). This is particularly pertinent in the current situation where a sharp and rapid increase in mental health symptoms is occurring globally due to the pandemic (Xiong et al., 2020).
The aim of the current research was to evaluate unguided low intensity CBT targeted at anxiety and depression during the COVID-19 pandemic. It was hypothesised that participants randomised to the intervention will show significantly lower symptoms of anxiety and depression, the primary outcome, after 1 week compared to control participants who were on a waitlist before receiving the intervention. We also sought feedback on the intervention from participants, in order to shape future iterations of the intervention.
1. Method
1.1. Participants
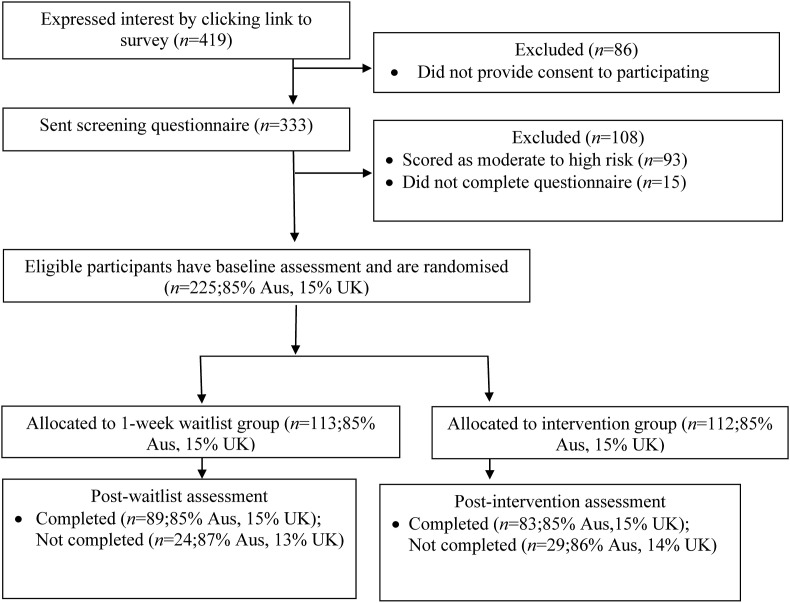
Inclusion criteria were above 18 years of age and residing in Australia or the United Kingdom. Exclusion criteria were moderate to high suicide risk. Fig. 1 illustrates a flow chart of participants. Participants were recruited on the internet via a social media advertisement run in Australia and the UK which stated “are you interested in improving your mental health during the COVID-19 pandemic?” and provided the study website link. Participants then engaged in a screening survey on the website. There were 419 individuals who initially expressed interest by commencing the survey on the study website. Some were excluded due to not completing the consent form or screening questionnaire. Of the 318 individuals who consented and were screened for suicide risk, 28% were not included in the trial due to moderate to high suicide risk. These participants with high suicide risk were immediately emailed information on crisis and mental health services, as well as the intervention.
Fig. 1.
Diagram displaying the flow of participants through the study (note. Aus = Australia, UK = United Kingdom).
The final sample was 225 participants (193 from Australia, 32 from the UK), of which 112 participants were randomly allocated to the intervention group, and 113 to the waitlist group. Based on an a-priori power analysis for a MANCOVA using the method of Dattalo (2013) with an alpha level of 0.05, 80% power, a small effect size (f 2 = 0.02), two groups, three covariates, and two outcomes, 190 participants per treatment group would be required. This indicates the present study was underpowered. A small treatment effect size was based on a previous meta-analysis of unguided low intensity CBT (g = 0.27; Karyotaki et al., 2017).
1.2. Measures
Suicide Risk. The Mini International Neuropsychiatric Interview (MINI), version 5.0 (Sheehan et al., 1998) suicide risk questions were used to screen for suicide risk, where scores of 1–5 points indicate low risk, 6–8 moderate risk, and more than 10 high risk. The MINI has good validity, internal consistency and test-retest reliability (Sheehan et al., 1997).
Anxiety. The GAD-7 (Spitzer et al., 2006) was used to assess anxiety. The 7 items are scored on a four-point scale: Not at all (0) to Nearly every day (4), with total scores ranging from 0 to 28. Higher scores indicate higher anxiety, with scores of 0–4 representing minimal anxiety, 5–9 mild anxiety, 10–14 moderate anxiety, and 15 and above severe. The measure has good reliability (Dear et al., 2011), in the current study internal consistency was excellent (α = .90).
Depression. The PHQ-9 (Kroenke et al., 2001) was used to assess depressive symptoms. The 9 items are scored on a four-point scale; Not at all (0) to Nearly every day (4). Higher scores indicate higher depressive symptoms, with scores of 0–4 indicating minimal depression, 5–9 mild depression, 10–14 moderate depression, 15–19 moderately severe depression, and 20–27 severe depression. The scale has good reliability and validity (Lowe et al., 2004), in the current study internal consistency was excellent (α = .87).
Adherence to treatment. This was assessed using four items adapted from Thiels et al. (1998) and included items assessing the degree to which participants read the self-help intervention (0%, 25%, 75%, 100%), length of time spent reading the guide (0 min, 1–30 min, 30–60 min, 60–120 min, 120+ minutes), usefulness of the guide (1 = not useful at all to 5 = extremely useful), and whether the guide was easy to read (1 = strongly disagree to 5 = strongly agree).
Ease of Use. This was assessed using three items adapted from Rozental et al. (2020), which included items asking participants to rate how easy they found it to use aspects of the guide (1 = difficult to use to 3 = very easy to use). These aspects included the information provided, the accompanying strategies, and the additional resources that were included.
Intervention preferences. This was assessed using three items created for the purposes of this study. Specifically, participants were asked about format preference (i.e., hard paper copy, online on a website, or a mobile app), whether they preferred to have some guidance about the information presented (1 = strongly disagree to 5 = strongly agree), and whether they preferred to use the guide without assistance (1 = strongly disagree to 5 = strongly agree).
Engagement with the intervention and resources. Participants were asked whether they implemented any of the techniques outlined in the guide, and if they had, they were asked to specify which techniques (e.g., mindfulness, behavioural experiments) they had engaged in. Participants were also asked if they had followed up any of the online services and resources.
1.3. Intervention content
The intervention was a 10-page, 14-point Times New Roman PDF document, including text, graphics and worksheets (for example a behavioural experiment worksheet for challenging negative predictions). The intervention was adapted from a guide written by SE at the start of the pandemic for the World Confederation of CBT (WCCBT; www.wccbt.org), which included input from CBT experts around the world. The WCCBT intervention included information and translated versions in Chinese, Spanish and German and covered the US, UK, Australia/New Zealand, Europe, Asia, South America, and The Middle East. The parts of the guide relating to general strategies and resources in the UK and Australia were adapted from the WCCBT guide and new sections written. The strategies chosen were judged to be ones which may be easiest to explain in a very brief guide, and were viewed as a central component of effective strategies (e.g., behavioural experiments to challenge negative thinking). The intervention was made available online after the trial completion in October 2020 at: www.covidcbt.org. The Flesch-Kincaid grade point reading level was 11, understandable by a high school student, and contained CBT and mindfulness strategies applicable for adults, as well as sections on child and adolescent mental health, including specific strategies for children with special needs including autism and intellectual disability, for whom lockdown and mask-wearing can be particularly challenging. The intervention also contained links to CBT internet treatment sites, as well as evidence supported e-books on CBT for children, adolescents and adults, including those recommended on the UK's National Health Service (NHS) “reading well” online guide. The intervention contained a list of crisis and other services (e.g., suicide, domestic violence, Aboriginal and Torres Strait Islander mental health services for Australia, and UK crisis and other services, adapted depending on which country the participant was from).
The guide was specifically targeted towards the COVID-19 pandemic, for example discussion of resources and strategies for coping with unemployment and economic uncertainty, increasing exercise and social interactions within the constraints of local lockdown requirements (i.e., indoors and online), and problem-solving strategies regarding procrastination when working from home. For children and adolescents, suggested strategies were related to impacts on children's increased anxiety over COVID-19, and depressive symptoms resulting from social isolation, for example, home schooling and impact on disruption of social networks for school age youth. In older adults, reference was made to normalising increased anxiety over COVID-19, given the disproportionate impact on older adults frequently highlighted in the media. Suggestions were made to moderate media consumption on the pandemic for both children and adults, as recommended (Bendau et al., 2021) to improve mental health (see Table 1 ).
Table 1.
Intervention overview.
| Psychoeduction and normalising of anxiety |
| Self-care (healthy diet, exercise, moderating alcohol) and pleasant event scheduling |
| Reducing worry through decreasing consuming media about the pandemic, worry time |
| Addressing anxiety over finances through CBT and mindfulness strategies |
| Problem solving, progressive muscle relaxation and mindfulness |
| Challenging negative thinking with behavioural experiments and thought records |
| Resources for children and teenagers, and parents/carers of children with disabilities |
| Strategies for older adults (e.g., pleasant event scheduling, phone/internet social connections) |
| List of CBT websites in Australia and the UK and CBT self-help books for youth and adults |
1.4. Procedure
The study was approved by the Curtin University Human Research Ethics Committee (HRE2020-0424). The study was a randomised controlled trial and registered on the Australian New Zealand Clinical Trails Registry on 30 July 2020 (ACTRN12620000779976p). It was conducted from 7 August to 30 September 2020. Individuals who accessed the study website and expressed interest by following the participation survey link were shown an information and consent form. Individuals who provided informed consent completed the screening questions for suicide risk and, depending on their score calculated automatically by the online survey software Qualtrics®, eligible participants progressed to completing the baseline assessment (if low risk). Individuals with moderate to high suicide risk were exited from the survey, and immediately emailed a list of support services as well as a digital copy of the intervention. Individuals with high suicide risk were not included in the study so that they could receive the intervention immediately and did not need to wait a week for the intervention if they were randomised to the control group. After completing the baseline assessment (time 1), participants were randomly allocated to either the intervention or 1-week waitlist condition. Participants in the intervention group were then immediately emailed a digital copy of the intervention and advised to read over it for one week. Participants in the waitlist group were informed that they would receive the guide after completing the follow-up survey one week later (time 2). After one week, all participants were emailed a link to complete the follow-up survey. On completion of the follow-up survey, all participants were emailed an AUD$20 (or £10 for participants residing in the UK) voucher for their time, and waitlist group participants were emailed a digital copy of the intervention.
1.5. Randomisation and masking
Randomisation was conducted using an embedded randomiser within the survey software. Statistical analysis was performed by a statistician external to the trial (AJ), who analysed the data blind to treatment condition.
1.6. Statistical analysis
Analyses were conducted using the “lavaan” R package (Rosseel, 2012). Robust maximum-likelihood (MLR) estimation was used to account for any non-normality and missingness in the data. A multivariate analysis of covariance (MANCOVA)-style path model was used to test whether the groups differed in their post-treatment means, after controlling for pre-treatment differences and accounting for the correlated nature of the outcome measurements. The post-treatment scores were entered as correlated outcomes, with treatment group, respective pre-treatment score, and age entered as predictors. Additionally, two-way interactions were specified between treatment group and pre-treatment score, and age to test whether these constructs moderated the difference between treatment groups at post-treatment. By conducting this model in a path analysis framework, rather than a traditional MANCOVA, a different pre-treatment covariate can be specified for each outcome, a robust estimator can be used to account for any non-normality in the data. There was no missing data at baseline, and a 23.11% loss to follow-up (Intervention: 25.00%, Control: 21.24%). Missing data were accounted for using full-information maximum-likelihood.
Model fit for the path analysis was assessed using the χ2 statistic (p > .05 indicates good fit), the Comparative Fit Index (CFI; > 0.90 indicates good fit; Hu & Bentler, 1999), the Tucker & Lewis Index (TLI; > 0.90 indicates good fit; Hu & Bentler, 1999), and the Standardised Root Mean Squared Residual (SRMR; < 0.08 indicates good fit; Hu & Bentler, 1999). The Root Mean Square Error of Approximation (RMSEA) was not included, as it can falsely indicate poor fit in models with few degrees of freedom (Kenny et al., 2015).
2. Results
Demographics. The demographics can be seen in Table 2 . At pre-treatment, 34.8% of the intervention group and 36.3% of the control group had a GAD-7 score ≥10, indicating moderate to severe anxiety. Similarly, 35.7% of the intervention group and 41.6% of the control group presented with a PHQ-9 score ≥10, indicating moderate to severe depressive symptoms. These proportions are markedly larger than those seen by Fancourt et al. (2020) in a UK population assessed during COVID-19, who reported 22.6% and 25% of their sample presenting with moderate to severe anxiety or depressive symptoms, respectively. Similarly, and perhaps unsurprisingly, these proportions are also markedly larger than pre-COVID community norms on the PHQ-9 (5.6%; Kroenke et al., 2001) and GAD-7 (5.1%; Löwe et al., 2008). Further, the pre-treatment means for anxiety (M(SD) = 8.37 (5.56) and depression M (SD) = 8.25(5.64) in our sample were significantly higher than means during the pandemic in Australia (anxiety, M(SD) = 4.4 (5.2), p < .001; depression, M(SD) = 5.4 (5.9), p < .001; Dawel et al., 2020) and the UK (anxiety, M(SD) = 5.7 (5.6), p < .001; depression, M(SD) = 6.6 (6.0), p = .002; Fancourt et al., 2020). Correlations between the baseline variables included in the analysis are provided in Table 3 . As would be expected, there was a strong positive correlation between the GAD-7 and PHQ-9, emphasising the necessity of treating them as correlated outcomes in the analysis.
Table 2.
Demographics of the sample.
| All participants |
Intention to treat |
||
|---|---|---|---|
| Intervention |
Control |
||
| (n = 225) | (n = 112) | (n = 113) | |
| Age | 37.79 (14.02) | 36.88(13.33) | 38.69(14.68) |
| Age range | 18–80 | 18–70 | 18–80 |
| Gender | |||
| Male | 31 | 14 | 17 |
| Female | 191 | 96 | 95 |
| Non-Binary | 2 | 1 | 1 |
| Prefer not to Say | 1 | 1 | 0 |
| Employment | |||
| Student | 22 | 9 | 13 |
| None/retired | 24 | 11 | 13 |
| Unemployed | 16 | 7 | 9 |
| Casual/Part-time | 58 | 34 | 24 |
| Full-time | 105 | 51 | 54 |
| Location | |||
| WA Perth | 89 | 45 | 44 |
| WA Regional | 10 | 4 | 6 |
| Rest of Australia | 93 | 47 | 46 |
| NSW Sydney | 24 | 12 | 12 |
| NSW Regional | 7 | 4 | 3 |
| VIC Melbourne | 39 | 19 | 20 |
| VIC Regional | 9 | 3 | 6 |
| QLD Brisbane | 6 | 3 | 3 |
| SA Adelaide | 4 | 2 | 2 |
| ACT Canberra | 2 | 2 | 0 |
| TAS Hobart | 2 | 1 | 1 |
| United Kingdom | 32 | 16 | 16 |
| Not reported | 1 | 0 | 1 |
Note. WA = Western Australia, NSW = New South Wales, VIC = Victoria, QLD = Queensland, SA = South Australia, ACT = Australian Capital Territory, TAS = Tasmania, Regional = rural/country area.
Table 3.
Correlations between baseline variables.
| PHQ-9 | GAD | Age | Gender | |
|---|---|---|---|---|
| PHQ-9 | ||||
| GAD | .72 | |||
| Age | -.22 | -.28 | ||
| Gender | .26 | .16 | .09 |
Note. Gender was treated as nominal (to retain all responses) and the ANOVA method for deriving a correlation coefficient was used. As gender is treated as unordered categorical, the directionality of the correlation is not available.
2.1. Changes over time
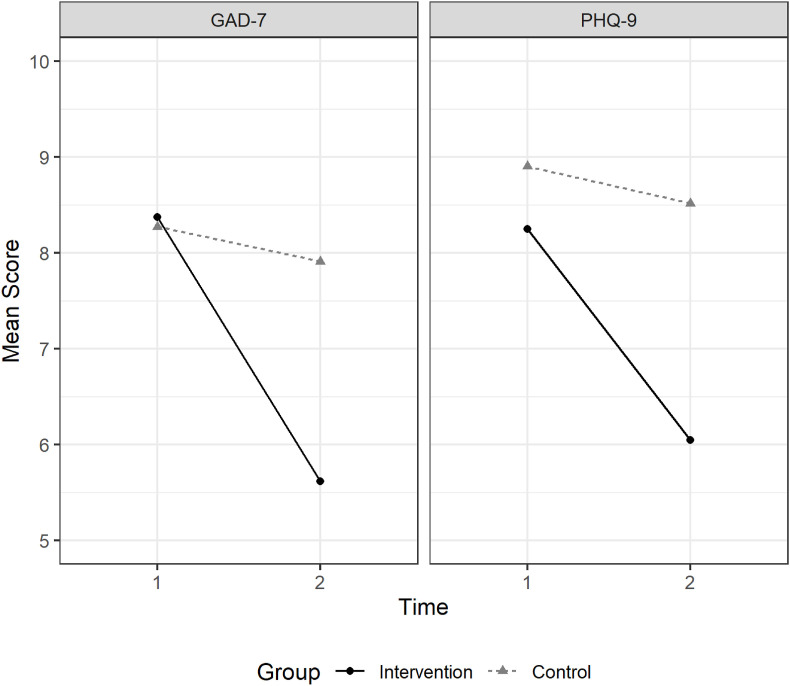
Pre- and post-intervention statistics are presented in Table 4 . Plots of the scale means for each group at each time are presented in Fig. 2 , where time 1 represents pre-treatment and time 2 post-treatment for the intervention group, and time 1 represents pre-waitlist, and time 2 post-waitlist, for the control group.
Table 4.
Means and standard deviations of anxiety and depression pre and post intervention.
| Pre | Post | Baseline Difference from Community Norm | |
|---|---|---|---|
| GAD-7 | |||
| - Intervention | 8.37 (5.56) | 5.62 (4.36) | t(112.87) = 10.27, p < .001 |
| - Control | 8.27 (5.00) | 7.91 (4.65) | t(114.35) = 11.25, p < .001 |
| PHQ-9 | |||
| - Intervention | 8.25 (5.64) | 6.05 (4.87) | t(112.94) = 9.98, p < .001 |
| - Control | 8.90 (5.63) | 8.52 (5.85) | t(113.98) = 11.26, p < .001 |
Note. GAD-7 = Generalised Anxiety Disorder Questionnaire (Spitzer et al., 2006); PHQ-9 = Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001). GAD-7 community norm (M = 2.95, SD = 3.41) taken from Löwe et al. (2008). PHQ-9 community norm (M = 2.91, SD = 3.52) taken from Kocalevent et al. (2013). Comparisons conducted using two-sample Welch t-tests on summary statistics.
Fig. 2.
GAD-7 and PHQ-9 Means for each Treatment Group at each Assessment Time.
The MANCOVA-style path model with GAD-7 and PHQ-9 as correlated outcomes showed good fit to the data: χ2(df) = 8.50(4), p = .075; CFI = .986, TLI = .947, SRMR = .035. After accounting for pre-treatment levels, the control group had significantly higher anxiety on the GAD-7 following treatment compared to the intervention group, which was a small effect (d = 0.36 [0.18, 0.54]; see Table 5 for coefficients). While pre-treatment levels of anxiety were significantly positively associated with post-treatment severity, there was no moderation on the treatment effect. There was also no direct or moderating relationship from age. Similarly, after controlling for pre-treatment levels, the control group also had a significantly higher level of depressive symptoms following treatment compared to the intervention group, and this was a small effect (d = 0.28 [0.11, 0.45]; see Table 5 for coefficients). As with the GAD-7, there was a significant relationship with pre-treatment depressive symptoms. In contrast, however, there was an additional significant interaction between treatment group and pre-treatment depressive symptoms. This indicates that pre-treatment depressive symptoms were more strongly related to post-treatment depressive symptoms in the control group, compared to the intervention group.
Table 5.
Path analysis results – unstandardised regression coefficients and confidence intervals.
| Outcome | Predictor | B [95%CI] | p |
|---|---|---|---|
| GAD-7 | |||
| Group | 1.90 [0.93, 2.87] | < .001 | |
| Pre-Treatment GAD | 0.46 [0.34, 0.59] | < .001 | |
| Age | −0.01 [-0.06, 0.03] | .573 | |
| Group * Pre-Treatment | 0.12 [-0.06, 0.31] | .184 | |
| Group * Age | −0.02 [-0.08, 0.04] | .478 | |
| PHQ-9 | |||
| Group | 1.58 [0.61, 2.55] | .001 | |
| Pre-Treatment PHQ | 0.56 [0.45, 0.67] | < .001 | |
| Age | −0.02 [-0.07, 0.02] | .268 | |
| Group * Pre-Treatment | 0.21 [0.05, 0.36] | .009 | |
| Group * Age | −0.02 [-0.08, 0.04] | .416 | |
Note. GAD-7 = Generalised Anxiety Disorder Questionnaire (Spitzer et al., 2006); PHQ-9 = Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001). A model with gender as a moderator (excluding 2 non-binary individuals and 1 who did not wish to report their gender) showed a similar pattern of results and no direct or moderating effects of gender.
Post-hoc analysis - Victoria. During the trial, individuals in Melbourne, Australia were in the midst of a stringent lockdown compared to participants in other areas, none of whom at the time were in lockdown, consequently this was explored in Australian individuals only, to determine if lockdown versus no lockdown had an effect (see Table 6 for descriptive statistics). When replacing age with Victorian residence as a moderator although mean GAD-7 and PHQ-9 scores were higher for Victorian compared to non-Victorian participants, there were no significant main or moderating effects of Victorian residence (see Supplementary Table 1 for all coefficients).
Table 6.
Baseline Means and Standard Deviations by Victorian (VIC) vs. non-VIC Residence (Australian Individuals only).
|
Intervention |
Control |
|||
|---|---|---|---|---|
| Non-VIC | VIC | Non-VIC | VIC | |
| GAD-7 | 7.43 (5.47) | 9.36 (4.97) | 7.18 (4.84) | 10.42 (5.27) |
| PHQ-9 | 7.04 (5.36) | 9.05 (4.69) | 7.48 (5.13) | 11.08 (5.46) |
Note. GAD-7 = Generalised Anxiety Disorder Questionnaire (Spitzer et al., 2006); PHQ-9 = Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001).
Post-hoc analysis - UK. As the UK experienced higher rates of COVID-19 than Australia, to explore if UK residence impacted intervention outcomes, the model was estimated using UK residence as a moderator (see Table 7 for means). Although UK residents had higher mean GAD-7 and PHQ-9 scores, there were no significant main or moderating effects of UK residence (see Supplementary Table 2 for all coefficients).
Table 7.
Baseline Means and Standard Deviations by United Kingdom (UK) vs. Australian Residence.
|
Intervention |
Control |
|||
|---|---|---|---|---|
| Australian | UK | Australian | UK | |
| GAD-7 | 7.88 (5.39) | 11.38 (5.78) | 8.05 (5.13) | 9.62 (3.98) |
| PHQ-9 | 7.50 (5.26) | 12.75 (5.92) | 8.44 (5.43) | 11.69 (6.15) |
Note. GAD-7 = Generalised Anxiety Disorder Questionnaire (Spitzer et al., 2006); PHQ-9 = Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001).
Post-hoc analysis – Completers vs Non-Completers. The baseline scale and demographic scores were compared between the individuals that dropped out of treatment and those that completed (see Supplementary Table 3 for all descriptives and test statistics). There were no significant differences in PHQ-9 (p = .232), GAD-7 (p = .090), or age (p = .896). There was a significant difference in gender (p = .037), with all participants who dropped out identifying as female. This is, however, consistent with the over-representation of female participants in the current sample.
2.2. Adherence to treatment and guide feedback
Of the participants who completed the intervention and provided feedback (n = 81), 71 (88%) indicated they had read 50% or more of the guide, with 46 (57%) reporting that they had read the full guide. Over three quarters of the participants (83%) reported that on average they spent 30 min or less reading the guide, with only 5 participants (6%) spending on average more than an hour reading the guide. The majority of participants (96%) agreed or strongly agreed that the intervention was useful. Most of the sample (86%) either agreed or strongly agreed that the guide was easy to read, with 10% neither agreeing nor disagreeing and 4% disagreeing.
2.3. Engagement with intervention
Of the individuals who answered follow up questions about the intervention, 70 (86%) indicated they had put in place at least one of the techniques outlined. The most endorsed techniques were exercise (56%) and self-care (53%), followed by mindfulness (48%), progressive muscle relaxation (46%), and pleasant event scheduling (31%). Fewer individuals endorsed problem solving techniques (20%) or using “worry time” to deal with worry and rumination (17%). Individuals were more likely to challenge unhelpful thoughts using a thought record (20%) compared to a behavioural experiment (10%). Just over half the individuals (52%) indicated that they had accessed one or more of the online treatment websites or resources listed for adults in the guide. The resources most commonly followed up were Beyond Blue (16%), The Black Dog Institute (16%), and The Association for Behavioural and Cognitive Therapies information sheets (15%). Twenty-one individuals (26%) indicated they had accessed one or more of the child and adolescent resources with Youth Beyond Blue (33%), ReachOut (24%), and Brave Online (14%) being the top three most followed up resources.
2.4. Intervention preference
When asked about their preferred format(s) for the intervention, 37 (46%) of participants would prefer to receive it as a mobile app, 31 (38%) as a paper copy, and 45 (56%) through a website online. When asked about if they would have benefited from receiving personal guidance, most participants (62%) said they preferred no guidance, with 20% reporting they would have liked guidance.
3. Discussion
The aim of the study was to examine the efficacy of brief unguided low intensity CBT in adults during the COVID-19 pandemic. The findings indicated small but significant reductions in anxiety (d = 0.36) and depression (d = 0.28) compared to a waitlist control. These findings are comparable to reviews of unguided internet interventions for anxiety and depression (Andersson, 2016), and a meta-analysis of unguided internet and low intensity interventions (d = 0.27; Karyotaki et al., 2017). The majority of participants reported the intervention was useful and easy to read, and attrition at post-treatment of 25% was reasonable and similar to other trials of internet delivered psychological therapies (Andersson, 2016).
Our sample were on average in a clinical range of anxiety and depression, demonstrating the need for interventions to be available during the pandemic. Further, the current sample's pre-intervention scores on anxiety and depression were significantly elevated compared to samples during the pandemic in Australia (Dawel et al., 2020) and the UK (Fancourt et al., 2020). In line with Dawel et al.’s (2020) findings, our results indicated elevated anxiety and depression in our community sample compared to population norms.
The results support the call for low intensity psychological interventions to be made rapidly available during the pandemic (Holmes et al., 2020; Wind et al., 2020). The intervention may be seen as a complement to more extensive CBT and psychological intervention services available online, and participants reported accessing several online resources outlined in the intervention. The advantage of the current intervention was its brevity, with most participants reading the intervention in less than 30 min. Importantly, despite the brevity and being completed over only a 1-week period there were significant treatment effects. Another advantage of the intervention is that we tailored the information to specifically address stress, anxiety and low mood with respect to the pandemic. Despite its brevity, the tailored nature of the intervention to worries about the pandemic may have had an impact because advertisements targeted individuals who were interested in improving their mental health during the pandemic. A strength was that the intervention was easily implemented, requiring no input from health professionals.
There are several limitations of the study. First, there was no follow-up period, therefore it is not possible to determine if the reductions in anxiety and depression were durable. While reviews of low intensity internet delivered CBT have reported that effects are sustained over follow-up periods (Andersson, 2016), including up to five years after treatment (Hedman et al., 2011), future research should examine if the current intervention is durable by assessing follow-up. Second, the participants were from a wide range of areas with differing levels of COVID-19. For example, participants in Melbourne were in the midst of a stringent lockdown and there were higher rates of COVID-19 in the UK than Australia. While place of residence was not found to be a moderator of treatment response, it is possible that with larger sample sizes there may have been a difference. Third, we limited the symptom outcomes to anxiety and depression to minimise participant burden and dropout. Future research into the impacts on a wider range of measures of psychopathology and wellbeing, along with investigations into moderators of change, would be informative. Fourth, the intervention was suitable to higher income countries such as the UK and Australia, work is needed in lower-and-middle income countries to evaluate scalable interventions to mitigate the mental health impacts of the pandemic throughout the world. Fifth, the study was underpowered to detect a small effect size.
A final limitation of the study was that standard CBT and pandemic-specific materials were combined together, hence the design did not allow evaluation of the extent to which standard CBT materials or pandemic-specific materials contributed to the observed effects. The efficacy of the standard CBT component of the intervention has not been evaluated previously. Future research should seek to compare an unmodified and un-tailored standard low intensity CBT intervention with the pandemic specific version, in order to understand whether and how existing CBT interventions need to be expanded or altered to cover pandemic-related concerns. Despite this limitation, qualitative interviews with a subset of 22 participants in the intervention group which is described elsewhere (Egan et al., 2021) indicated that 91% of participants reported the intervention was useful. Qualitative themes included the usefulness of the specific pandemic related material, for example information regarding budgeting and job-related concerns and how to exercise while under lockdown (Egan et al., 2021). However, while qualitative feedback was sought at the end of treatment, a limitation was that pandemic specific concerns (e.g., isolation, homeschooling, unemployment) were selected based on the literature which had raised these areas as concerns in surveys during the pandemic (e.g., Dawel et al., 2020) and the researchers’ clinical judgement regarding what areas may be impacted during the pandemic. Individuals with lived experience of anxiety and depression were not consulted during the design of the intervention as to which areas they believe should have been included, although the intervention was updated at the end of treatment based on their feedback before widespread dissemination. Future research should seek to co-construct pandemic specific interventions with the people who will use the intervention being co-researchers and co-designing the intervention.
In summary, the findings indicated that very brief, low intensity CBT reduced anxiety and depression in adults during the COVID-19 pandemic. Further work is urgently needed on evaluating the dissemination of low intensity interventions during the pandemic, particularly the translation and dissemination of interventions in both high resource and lower-and middle-income countries to improve mental health worldwide.
Data sharing
Deidentified data is available upon request from the authors with a signed data access agreement and subject to Institutional approvals.
Author contribution statement
SE, PM, TW and RS designed the study. SE wrote the manuscript, PM, TW, DG, RA, TM and RS edited the manuscript. AJ conducted the statistical analysis. SU, CG and LW recruited participants and SU, CG, LW and SB disseminated the intervention. SE wrote the intervention with input from PM, TW, CG, RA, TM, RS and a range of CBT practitioners contributed to the content (see acknowledgements).
Role of funding source
This work was funded by a grant from the Department for Jobs, Tourism, Science and Innovation, Government of Western Australia, awarded to Sarah Egan at Curtin University. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Declaration of competing interest
We declare no conflict of interest.
Acknowledgments
We acknowledge the help of Rod Holland in formatting the intervention and graphic design. The following individuals provided input into the content of the guide: PM, TW, CG, RA, TM, RS, Professor Martin Antony, Professor Keith Dobson, Professor Leanne Hides, Dr Joel Howell, Professor Jennie Hudson, Dr Robert Leahy, Professor Lata McGinn, Dr Robert Schutze and Professor Susan Spence.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.brat.2021.103902.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- Andersson G. Internet-delivered psychological treatments. Annual Review of Clinical Psychology. 2016;12:157–179. doi: 10.1146/annurev-clinpsy-021815-093006. [DOI] [PubMed] [Google Scholar]
- Bendau A., Petzold M.B., Pyrkosch L., Maricic L.M., Betzler F., Rogoll J.…Plag J. Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. European Archives of Psychiatry and Clinical Neuroscience. 2021;271:283–291. doi: 10.1007/S00406-020-01171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark D.M. Realizing the mass public benefit of evidence-based psychological therapies: The IAPT program. Annual Review of Clinical Psychology. 2018;14:159–183. doi: 10.1146/annurev-clinpsy-050817-084833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dattalo P. Oxford University Press; 2013. Analysis of multiple dependent variables. [Google Scholar]
- Dawel A., Shou Y., Smithson M., Cherbuin N., Banfield M., Calear A.L., Farrer L.M., Gray D., Gulliver A., Housen T., McCallum S.M., Morse A.R., Murray, Newman E., Rodney Harris R.M., Batterham P.J. The effect of COVID-19 on mental health and wellbeing in a representative sample of Australian adults. Frontiers in Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.579985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dear B.F., Titov N., Sunderland M., McMillan D., Anderson T., Lorian C., Robinson E. Psychometric comparison of the Generalised Anxiety Disorder scale 7 and the Penn State Worry questionnaire for measuring response during treatment of generalised anxiety disorder. Cognitive Behaviour Therapy. 2011;40(3):216–227. doi: 10.1080/16506073.2011.582138. [DOI] [PubMed] [Google Scholar]
- Egan S.J., Shafran R., Wade T.D., Ure S., Gill C., Wilker L., Anderson R., Mazzucchelli T., McEvoy P. 2021. A qualitative examination of unguided low intensity cognitive behaviour therapy to reduce anxiety and depression during the COVID-19 pandemic. (Manuscript under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn C.G., Patel V. The global dissemination of psychological treatments: A road map for research and practice. American Journal of Psychiatry. 2014;171:495–498. doi: 10.1176/appi.ajp.2013.13111546. [DOI] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of depression and anxiety during enforced isolation due to COVID-19: Longitudinal analyses of 36,520 adults in England. MedRxiv. 2020 doi: 10.1101/2020.06.03.20120923. [DOI] [Google Scholar]
- Fitzpatrick K.M., Drawve G., Harris C. Facing new fears during the COVID-19 pandemic: The State of America's mental health. Journal of Anxiety Disorders. 2020;75 doi: 10.1016/j.janxdis.2020.102291. Article e10229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Sanguion C., Ausin B., Castellanos M.A., Saiz J., Lopez-Gomez A., Ugidos C., Munos M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedman E., Furmark T., Carlbring P., Ljotsson B., Ruck C., Lindefors N.…Andersson G. Five-year follow-up of internet-based cognitive behaviour therapy for social anxiety disorder. Journal of Medical Internet Research. 2011;13(2) doi: 10.2196/jmir.1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L.…Sweeney A., et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L.T., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Karyotaki E., Riper H., Twisk J., Hoogendoorn A., Kleiboer A., Mira A.…Huibers M.J.H., et al. Efficacy of self-guided internet-based cognitive behavioural therapy in the treatment of depressive symptoms: A meta-analysis of individual participant data. JAMA Psychiatry. 2017;74:351–359. doi: 10.1001/jamapsychiatry.2017.0044. [DOI] [PubMed] [Google Scholar]
- Kenny D.A., Kaniskan B., McCoach D.B. The performance of RMSEA in models with small degrees of freedom. Sociological Methods & Research. 2015;44(3):486–507. doi: 10.1177/0049124114543236. [DOI] [Google Scholar]
- Kocalevent R., Hinz A., Brähler E. Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. General Hospital Psychiatry. 2013;35:551–555. doi: 10.1016/j.genhosppsych.2013.04.006. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Decker O., Müller S., Brähler E., Schellberg D., Herzog W., Herzberg P.Y. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Medical Care. 2008;46:266–274. doi: 10.1097/mlr.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Lowe B., Kroenke K., Herzog W., Grafe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9) Journal of Affective Disorders. 2004;81:61–66. doi: 10.1016/S0165-0327(03)00198-8. [DOI] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S., Abel K.M. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y. lavaan. An R Package for Structural Equation Modeling. 2012;48(2):36. doi: 10.18637/jss.v048.i02. [DOI] [Google Scholar]
- Rozental A., Kothari R., Wade T., Egan S.J., Andersson G., Carlbring P., Shafran R. Reconsidering perfect: A qualitative study of the experiences of internet-based cognitive behaviour therapy for perfectionism. Behavioural and Cognitive Psychotherapy. 2020;48:432–441. doi: 10.1017/S1352465820000090. [DOI] [PubMed] [Google Scholar]
- Shafran R., Myles-Hooton P., Bennett S., Ost L.G. The concept and definition of ‘low intensity’ cognitive behaviour therapy. Behaviour Research and Therapy. 2021;138:103803. doi: 10.1016/j.brat.2021.103803. [DOI] [PubMed] [Google Scholar]
- Sheehan D.V., Lecrubier Y., Sheehan K.H., Amorim P., Janavs J., Weiller E., Hergueta T., Baker R., Dunbar G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–57. [PubMed] [Google Scholar]
- Sheehan D.V., Lecrubier Y., Sheehan K.H., Janavs J., Weiller E., Keskiner A.…Dunbar G.C. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. European Psychiatry. 1997;12:232–241. doi: 10.1016/S0924-9338(97)83297-X. [DOI] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Lowe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Thiels C., Schmidt U., Treasure J., Garthe R., Troop N. Guided self-change for bulimia nervosa incorporating use of a self-care manual. American Journal of Psychiatry. 1998;155:947–953. doi: 10.1176/ajp.155.7.947. [DOI] [PubMed] [Google Scholar]
- Twenge J.M., Joiner T.E. US Census Bureau‐assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID‐19 pandemic. Depression and Anxiety. 2020;37:954–956. doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma S., Mishra A. Depression, anxiety, and stress and socio-demographic correlates among general Indian public during COVID-10. International Journal of Social Psychiatry. 2020;66:756–762. doi: 10.1177/0020764020934508. [DOI] [PubMed] [Google Scholar]
- Wind T.R., Rijkeboer G., Andersson G., Riper H. The COVID-19 pandemic: The 'black' swan for mental health care and a turning point for e-health. Internet Interventions. 2020;20 doi: 10.1016/j.invent.2020.1003. Article e100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L.…McIntyre R.S. Impact of COVID-19 pandemicon mental health in the general population: A systematic review. Journal of Affective Disorders. 2020;277:55–64. doi: 10.1016/j.ad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.