Abstract
Background
Black individuals with substance use disorders (SUD) are less likely to receive effective treatment and more likely to be incarcerated compared to White individuals. Despite this, research documenting racial disparities in healthcare use among people with SUD releasing from prison is limited.
Objectives
The goals of this study are to: 1) assess racial disparities in Medicaid enrollment among individuals released from prison with a history of substance use; and 2) characterize racial disparities in outpatient service use, emergency department (ED) use, and receipt of medication for opioid use disorder (MOUD) among those who do enroll in Medicaid.
Methods
This study included individuals with a history of substance use that were released from Wisconsin state correctional facilities from April 2015 through June 2017. Medicaid enrollment and claims data were analyzed to compare healthcare utilization 6 months post-release between individuals identifying as Black, White, or other races. The total sample included 15621 prison releases among 14400 unique persons with a history of substance abuse.
Results
Among the 15621 prison releases, 10836 (69.4%) were enrolled in Medicaid in the month of release. The proportion of prison releases among individuals of other races who enrolled in Medicaid (506/934, 54.2%) was significantly lower than the proportion among Black individuals (3679/5306, 69.3%) and White individuals (6651/9381, 70.9%). Among the subset of 7685 releases enrolled in Medicaid for 6 months post-release, 5040 (65.6%) had an outpatient visit within 6 months; 73.9% of White, 51.3% of Black, and 66.9% of other individuals. Relative to White individuals, Black individuals were 0.324 times less likely (P<0.001) and individuals of other races were 0.591 times less likely (P=0.004) to have an outpatient visit. Of the 7685 releases, 1016 (13.2%) had an ED visit within 6 months; 12.0% of White, 13.8% of Black and 25.1% of other individuals. Relative to White individuals, Black individuals were 1.23 times more likely (P=0.019) and individuals of other races were 2.64 times more likely (P<0.001) to have an ED visit. Black individuals were 0.100 times less likely (P<0.001) and individuals of other races were 0.435 times less likely (P=0.016) to receive MOUD post-release compared to White individuals.
Conclusions
Black adults with a history of substance use are significantly less likely than White adults to use non-emergency outpatient services after release from incarceration. Improving equitable access to outpatient services is needed to reduce health disparities across racial groups.
Keywords: racial disparities, post-release, substance abuse, medication for opioid use disorder, healthcare utilization
BACKGROUND
With 431 per 100,000 U.S. residents of all ages in state and federal prisons at year-end 2018 (Ann Carson 2020), the United States imprisons more of its population than any other country in the world (Prison Policy Initiative 2018). People of color are disproportionately affected at every stage of the judicial system. Relative to White persons, people of color are more likely to be stopped (Pierson et al. 2020), searched, arrested (Bureau of Justice Statistics 2016; Harris 2012), convicted, harshly sentenced and burdened with a lifelong criminal record (Council on Criminal Justice 2019; Mauer 2011; United States Sentencing Commission 2017). In the U.S., African Americans are 5.9 times more likely to be incarcerated than White Americans (Bureau of Justice Statistics 2018).
Mass incarceration and racial/ethnic disparities within the U.S. criminal justice system have been driven by the War on Drugs, which has been credited with creating policies that significantly contribute to racial/ethnic disparities in drug arrests (Tonry 2011). Racial and ethnic minorities continue to be more likely than White individuals to be incarcerated for nonviolent substance-related offenses and imprisoned for drug charges (Dumont et al. 2012; O’Hear 2009), despite similar rates of substance use (Rosenberg, Groves, and Blankenship 2017).
Racial disparities in healthcare utilization among the general population have also been well documented (Mayberry, Mili, and Ofili 2016; Nelson 2002). Studies have shown that relative to non-Hispanic White patients, Black patients are significantly less likely to receive influenza vaccinations (Egede and Zheng 2003), have a visit with a mental health professional (Fiscella et al. 2002), use primary care as their usual source of care (Gaskin et al. 2007), and receive major therapeutic procedures for a broad range of medical conditions (Harris, Andrews, and Elixhauser 1997; Wenneker and Epstein 1989). Additionally, Black patients are more likely than white patients to use the emergency department (ED) as their usual source of care (Brown et al. 2012). Studies also show that Black individuals are less likely to receive effective treatment for opioid use disorders (Hansen et al. 2016; Lagisetty et al. 2019). The sources of racial disparities include lack of access to health coverage and providers, communication difficulties between patient and provider (Nelson 2002), cultural barriers (Egede 2006), provider stigma (Budhwani and De 2019), and structural racism across various domains (Kunins 2020). These racial disparities in healthcare use disadvantage Black people by limiting their exposure to preventative health benefits, subsequently worsening their health conditions.
Although Medicaid expansion efforts have helped narrow racial disparities in health coverage and access to care (Baumgartner et al., 2020), individuals often lose Medicaid coverage during periods of incarceration and must overcome several barriers that make it difficult to re-enroll upon release (Grodensky et al., 2018). To facilitate Medicaid enrollment and improve health coverage upon release from incarceration, many states have implemented prerelease enrollment assistance programs. In the US, the availability of prerelease enrollment assistance is growing but remains variable across and within states (Bandara et al., 2015). In 2018, prerelease enrollment assistance was available in prisons within 38 states and within at least some jails in 32 states (Beck, 2020).
Despite the abundant literature describing how Black individuals with substance use disorders (SUD) are more likely to be incarcerated and less likely to receive effective treatment compared to White individuals, research documenting racial disparities in healthcare use among people with SUD releasing from prison is limited. The purpose of this paper is to determine whether racial disparities in Medicaid enrollment exist among those released from prison with a history of substance use, and among those who do enroll in Medicaid, whether racial disparities in health care use exist. Specifically, we examine use of outpatient services, use of emergency room services, and receipt of medication for opioid use disorder (MOUD) within 6 months of release from prison. Based on previous literature, we hypothesize that people of color will be less likely to enroll in Medicaid, less likely to receive outpatient care, more likely to utilize the emergency room, and less likely to receive MOUD than White individuals.
METHODS
Study Setting
Wisconsin is a state in the Great Lakes region of the U.S. with a population of approximately 5.8 million people (U.S. Census Bureau, 2019). The state of Wisconsin (WI) is among five states where the disparity in incarceration between Black and White individuals is more than 10 to 1 (The Sentencing Project 2016). As of 2017, Black individuals constituted 7% of Wisconsin state residents, but 29% of people in jail and 41% of people in prison (Vera Institute of Justice 2019).
On April 1, 2014, Wisconsin expanded Medicaid eligibility to all adults with income below 100% of the federal poverty level (FPL). Before April 2014, parents with income below 100% FPL were already eligible for Medicaid. Thus, this expansion notably included adults without dependent children. As a consequence of this expansion, most adults released from WI state correctional facilities are eligible for Medicaid. Subsequently, beginning in January 2015, the WI Department of Corrections (DOC) implemented pre-release Medicaid enrollment assistance, where discharge planning staff provide guidance on how to apply for Medicaid and individuals are given the opportunity to call an eligibility case worker from the correctional facility. This service is available to all adults incarcerated within WI state correctional facilities, which includes state prisons, correctional centers, and state-contracted beds within county jails. Under the enrollment assistance program, individuals may apply for Medicaid as early as the 20th day of the month prior to their month of release. Individuals generally obtain an eligibility decision on the day of application. Our research team found that Medicaid enrollment in the month of release from a Wisconsin state correctional facility increased 29 percentage points among the general incarcerated population and 30 percentage points among those with a history of substance use after implementation of the Medicaid eligibility expansion, and increased an additional 25 and 24 percentage points within the two groups, respectively, after implementation of the enrollment assistance program (Burns et al., 2021).
Study Population
Individuals with a history of substance use that were released from WI DOC from April 1, 2015 through June 30, 2017 were included in this analysis. April 1, 2015 was chosen to allow a three-month phase-in period for the enrollment assistance program. Individuals were considered to have a history of substance use if they met any one of the following criteria: 1) self-reported opioid use of opioids; 2) a highly probable need for substance use disorder treatment; or 3) living with, or at risk of, hepatitis C virus (HCV) infection, which was included because the primary risk factor for new HCV infections is injection drug use (Zibbell et al. 2015).
We excluded individuals from our analyses who were incarcerated for less than 30 days, as these individuals may not have had adequate time to complete the discharge planning process. For healthcare utilization analyses, our outcomes capture healthcare use in the six-months post-release, so we excluded those who were not enrolled in Medicaid for six consecutive months post-release. Figure A presents the number and proportion of releases included after each eligibility criterion was applied, by racial groups.
Figure A:
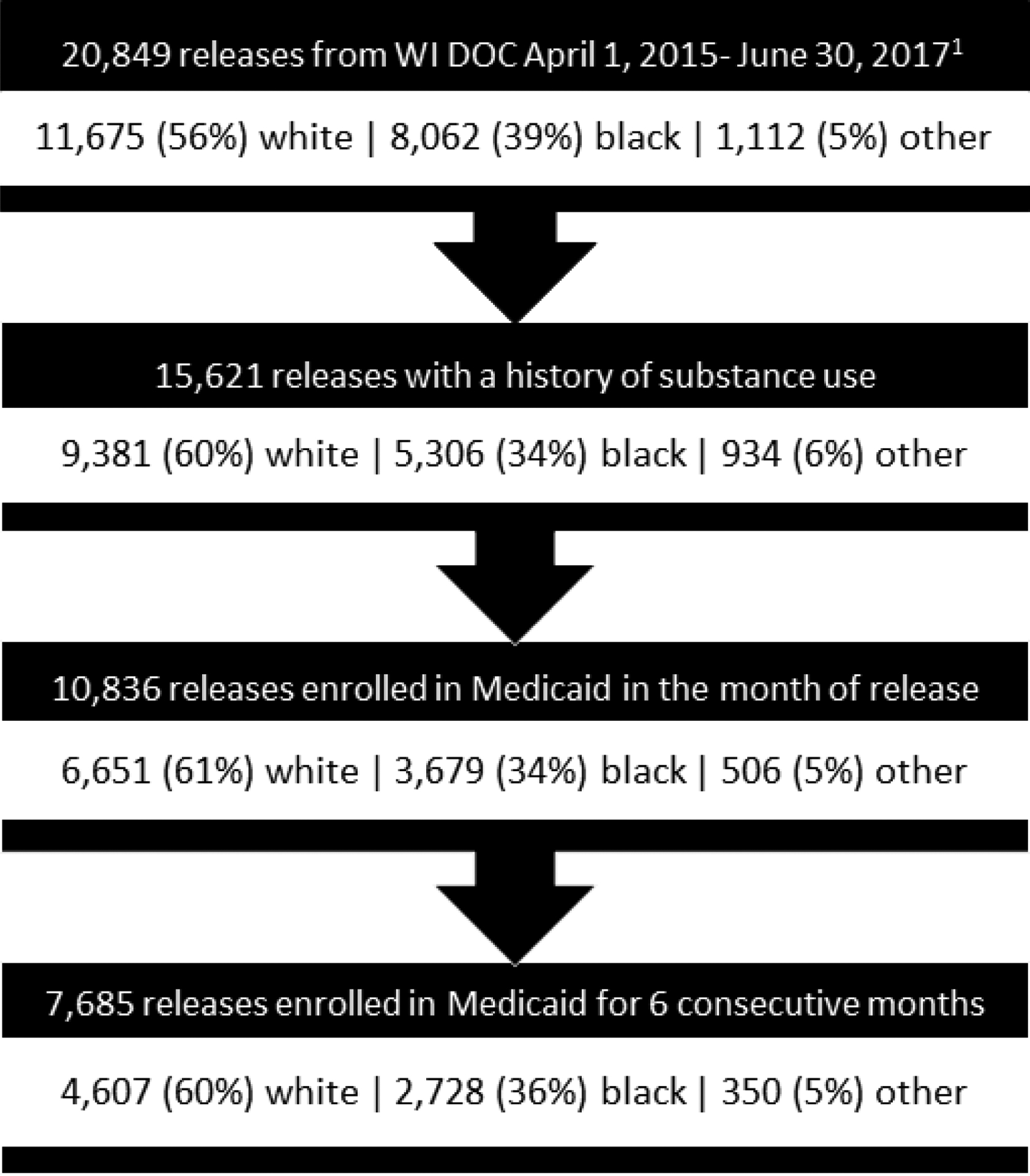
Sample construction demonstrating the number (%) of releases included after each study eligibility criterion was applied, by racial groups
1Releases from incarcerations of at least 30 days
Data Sources
We link Medicaid, Department of Corrections (DOC), Wisconsin State Lab of Hygiene (SLH), and the WI Electronic Disease Surveillance System (WEDSS) data at the person-level using the Institute for Research on Poverty’s Wisconsin Administrative Data Core at UW-Madison (Brown and Thornton 2020). Data are matched using the last four digits of Social Security Numbers, first and last names, dates of birth, and other characteristics if necessary, such as gender and race/ethnicity. Linkages are made using fuzzy matching methods to account for name variants, data entry errors, or other data quality issues.
We used data from the DOC, the SLH, and the WEDSS to identify individuals with a history of substance use. At least once during an individual’s incarceration, the DOC aims to collect self-reported information on the individual’s history of substance use and past treatment for substance use using a risk and needs assessment tool, the Correctional Offender Management Profiling for Alternative Sanctions (COMPAS). The COMPAS tool uses a proprietary algorithm to generate a score from these responses that reflects the need for substance use treatment: unlikely, probable, or highly probable (Northpointe Inc. 2012; Northpointe Institute for Public Management Inc. 2009). Additional information about the COMPAS instrument and the substance use questions used to generate a score is provided in Appendix A. The COMPAS tool also collects self-reported opioid use, including buprenorphine, codeine, fentanyl, heroin, methadone, morphine, opiates, vicodin. Three data sources were used to determine whether individuals had a history of or were at risk for HCV infection. First, the DOC provided a list of person-incarceration episodes for which the DOC provided an HCV prescription treatment to. Second, the SLH provided a list of person-incarceration episodes for which the DOC requested an HCV test upon prison admission, which is determined by a risk-based screening instrument that measures past injection drug use (Stockman et al. 2016). Finally, a list of study subjects who had ever had a positive antibody test for HCV before or during their incarceration was provided by the WEDSS.
The DOC data includes dates of admission and release, and serves as the source for study covariates including facility characteristics and individual demographics. Study outcomes were obtained from WI Medicaid enrollment and claims data.
Outcome Measures
Our first outcome was Medicaid coverage in the calendar month of release. This binary variable was set equal to one if the individual is enrolled in Medicaid in the month of release and zero otherwise. Although we do not observe if an individual was enrolled on the day of release, a previous analysis by our team demonstrates that Medicaid coverage in the month of release serves as an appropriate proxy for Medicaid coverage on the day of release (Burns et al., 2021).
Among those who enrolled in Medicaid, we also examine healthcare use during the six months post-release. Specifically, we examine whether individuals had any outpatient visit, an outpatient visit with a SUD diagnosis, any ED visit, and received medication for opioid use disorder (MOUD) within six months post-release. We also examine time (days) to any outpatient visit and any ED visit. Outpatient visits with a diagnosis code of SUD (excluding nicotine and tobacco use) in any position are defined as outpatient visits with SUD diagnosis. Receipt of MOUD is defined as having either (a) a prescription claim (i.e., NDC code) for buprenorphine, naltrexone (oral), injectable naltrexone, or buprenorphine/naloxone, or (b) a HCPCS code for buprenorphine/naloxone, methadone, or naltrexone within six months post-release. The Wisconsin Medicaid Program covered all types of MOUD during the study period (American Society of Addiction Medicine, n.d.). We also describe the number of ED visits for a general drug overdose and an opioid-specific overdose. A general drug overdose was defined as poisoning by any drug, medication, or biological substance, and an opioid-specific overdose was defined as poisoning by opium, methadone, other opioid, synthetic narcotics, unspecified/other narcotics, or heroin. However, because the occurrence of overdose-related ED visits was rare, we were unable to provide counts for all racial groups and conduct further analyses on these outcomes.
Statistical Analysis
We compared demographic and incarceration characteristics in the month of release across three racial groups using the chi-square test for categorical variables and analysis of variance (ANOVA) for continuous variables.
The primary predictor in all models was race. Individuals were determined to be White, Black, or other race. The “other” race category included individuals who were American Indian/Alaskan Native, Asian or Pacific Islander, or unknown. To assess racial disparities in study outcomes, we used mixed effects logistic regression. The unit of analysis was prison-release. Thus, individuals with multiple releases had repeated measures in the data. Cluster robust standard errors were used to adjust for the non-independence of observations within persons over time. We controlled for person and prison-release level covariates that may be related to study outcomes and may change over time. Demographic variables included age, gender, education, marital status, and whether their county of release was part of a metropolitan statistical area. We also included the duration of incarceration (months). Additionally, for the analysis of Medicaid enrollment specifically, we controlled for variables that may influence the discharge planning process, including the security level of the correctional facility, whether the facility had a paralegal benefit specialist available to assist with Medicaid enrollment, and type of release (e.g. under community supervision, etc.). Five facilities share three paralegal benefit specialists who assist inmates with the enrollment process. The DOC selected these five facilities based on the composition of their populations (e.g., relatively high prevalence of limited English proficiency, intellectual disabilities, mental illness, etc.).
To compare time (number of days) to any outpatient visit and time to any ED visit across racial groups, we conducted mixed effects Poisson regression using cluster robust standard errors and calculated incident rate ratios (IRR). Kaplan Meier survival curves were created for visualization. Covariates included in each model were age, gender, education, marital status, whether their county of release was part of a metropolitan statistical area, and duration of incarceration.
All analyses were conducted with Stata version 15 (College Station, TX). Statistical significance was defined as ɑ ≤ 0.05. The University of Wisconsin Institutional Review Board determined that this study qualified for exemption (protocol #2019-0058).
RESULTS
Descriptive Characteristics
Between April 1, 2015 and June 30, 2017, there were 15621 releases from 48 WI state correctional facilities among 14400 unique persons with a history of substance use. Across all racial groups, less than 1% were released from state-contracted beds in local jails. On average, subjects were incarcerated for 22.0 months and 35.7 years of age at release. Among the 15621 prison releases, 9381 (60.1%) were White, 5306 (34.0%) were Black, and 934 (6.0%) were other races. Among the 934 individuals of other races, 801 (85.8%) were American Indian or Alaskan Native, 128 (13.7%) were Asian or Pacific Islander, and 5 (0.5%) were unknown. The characteristics of prison releases by race are provided in Table A. Black releases were significantly less likely to be female, have a high school diploma or GED, and be released under community supervision. They were also incarcerated for longer durations and more likely to have a paralegal benefits specialist available at their release facility and be released to a metropolitan statistical area.
Table A:
Characteristics of prison releases among adults released from Wisconsin correctional facilities with a history of substance use, April 2015 -- June 2017
| Characteristic | White (N=9381) | Black (N=5306) | Other (N=934) |
|---|---|---|---|
| Number of unique persons | 8751 | 4774 | 875 |
| Female, n (%)* | 1303 (13.9) | 265 (5.0) | 137 (14.7) |
| Age at release, mean (SD)* | 36.1 (10.6) | 35.2 (11.0) | 34.6 (10.1) |
| Education, n (%)* | |||
| < High school diploma/GED | 1871 (19.9) | 1952 (36.8) | 214 (22.9) |
| ≥ High school diploma/GED | 7265 (77.4) | 2984 (56.2) | 702 (75.2) |
| Missing | 245 (2.6) | 370 (7.0) | 18 (1.9) |
| Marital Status, n (%)* | |||
| Single | 8239 (87.8) | 4531 (85.4) | 847 (90.7) |
| Married/Partnered | 987 (10.5) | 464 (8.7) | 78 (8.4) |
| Other | 155 (1.7) | 311 (5.9) | 9 (1.0) |
| Rurality of County of Release, n (%)* | |||
| Part of MSA | 6453 (68.8) | 4939 (93.1) | 479 (51.3) |
| Not part of MSA | 2646 (28.2) | 200 (3.8) | 432 (46.3) |
| Missing | 282 (3.0) | 167 (3.2) | 23 (2.5) |
| Months Incarcerated, mean (SD)* | 20.9 (28.1) | 24.3 (33.9) | 19.8 (24.2) |
| Type of Release, n (%)* | |||
| Supervision | 8773 (93.9) | 4523 (85.4) | 883 (95.2) |
| No Supervision | 258 (2.8) | 236 (4.5) | 23 (2.5) |
| Other | 317 (3.4) | 536 (10.1) | 22 (2.4) |
| Paralegal benefits specialists available at release facility, n (%)* | 3494 (37.3) | 2160 (40.7) | 323 (34.6) |
| Security level of release facility, n (%)* | |||
| Minimum | 1947 (26.7) | 861 (18.7) | 148 (19.4) |
| Medium | 4176 (57.2) | 3088 (67.1) | 451 (59.0) |
| Medium/Maximum | 450 (6.2) | 109 (2.4) | 69 (9.0) |
| Maximum | 661 (9.1) | 522 (11.3) | 89 (11.7) |
| Jail | 64 (0.9) | 24 (0.5) | 7 (0.9) |
p<0.05
Medicaid Enrollment
Among the 15621 releases, 10836 (69.4%) were enrolled in Medicaid in the month of release. The proportion of releases among individuals of other races who enrolled in Medicaid (506/934, 54.2%) was significantly lower than the proportion among Black individuals (3679/5306, 69.3%) and White individuals (6651/9381, 70.9%). After adjusting for confounding variables, Black individuals were 1.15 times more likely (95% CI 1.02–1.30; P=0.021) and individuals of other races were 0.388 times less likely (95% CI 0.307–0.489; P<0.001) to enroll in Medicaid relative to White individuals.
Among the 10836 releases enrolled in Medicaid in the month of release, there were 7685 (70.9%) releases among 7321 unique persons that were enrolled for at least six months and included in the healthcare utilization analyses. With 4607 (60.0%) White releases, 2728 (35.5%) Black releases, and 350 (4.6%) releases of other races, the proportion of releases in each racial group were comparable to the racial composition before applying the 6-month continuous enrollment criterion.
Outpatient Visits
Of the 7685 releases enrolled in Medicaid for at least 6 months post-release, 5040 (65.6%) had an outpatient visit. Among the 4607 White releases, 3406 (73.9%) had an outpatient visit within 6 months, compared with 51.3% (1400/2728) of Black releases and 66.9% (234/350) of releases of other races (Table B). Relative to White individuals, Black individuals were 0.324 times less likely (95% CI 0.257–0.409; P<0.001) and individuals of other races were 0.591 times less likely (95% CI 0.413–0.847; P=0.004) to have an outpatient visit. Furthermore, only 6.1% (167/2728) of Black individuals had an outpatient visit with a SUD diagnosis compared to 27.7% (1277/4607) of White individuals (OR 0.120; 95% CI 0.079–0.183; P<0.001).
Table B:
Prison releases in which healthcare services were utilized within 6 months of release among adults with a history of substance use who released from a Wisconsin state correctional facility and were enrolled in Medicaid for at least 6 months, April 2015 -- June 2017
| White (N=4607) REFERENCE n (%) | Black (N=2728) n (%) | Adjusted** OR (95% CI) | Other (N=350) n (%) | Adjusted** OR (95% CI) | |
|---|---|---|---|---|---|
| Any outpatient visit | 3406 (73.9) | 1400 (51.3) | 0.324 (0.257–0.409)* | 234 (66.9) | 0.591 (0.413–0.847)* |
| An outpatient visit with SUD diagnosis | 1277 (27.7) | 167 (6.1) | 0.120 (0.079–0.183)* | 104 (29.7) | 1.07 (0.751–1.524) |
| Any ED visit | 553 (12.0) | 375 (13.8) | 1.23 (1.035–1.466)* | 88 (25.1) | 2.64 (1.91–3.64)* |
| Receipt of MOUD | 368 (7.99) | 30 (1.10) | 0.100 (0.054–0.184)* | 15 (4.29) | 0.435 (0.220–0.859)* |
P<0.05
Adjusted for gender, age at release, education, marital status, rurality of county of release, and months incarcerated
Among the 5040 releases that had an outpatient visit within 6 months, the average time to a visit was 45.8 days (standard deviation: 44.5). Kaplan-Meier curves comparing the rate at which individuals in each racial group had an outpatient visit post-release are presented in Figure B.1. White individuals had outpatient visits sooner after release than Black or other race individuals. Compared to White individuals, Black individuals had a rate 1.27 times higher for the number of days to an outpatient visit (IRR: 1.266; 95% CI 1.181–1.356; P<0.001). Among those who had an outpatient visit, there was no significant difference between the rate at which White individuals and individuals of other races had a visit (IRR: 1.055; 95% CI 0.926–1.202; P=0.423).
Figure B.1:
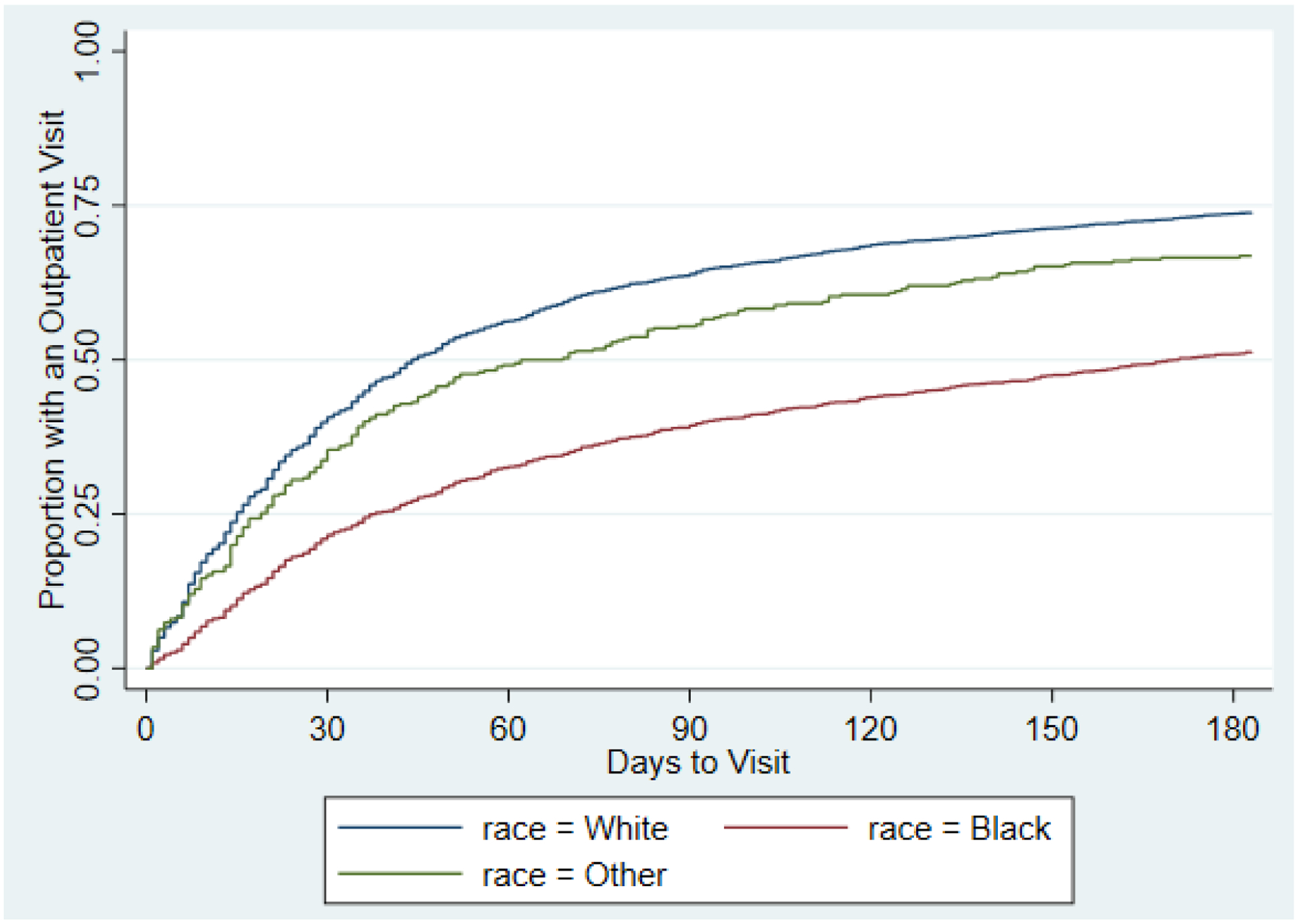
Time to any outpatient visit, by race, among adults released from Wisconsin correctional facilities with a history of substance use, April 2015 - June 2017
Emergency Department Visits
Of the 7685 releases enrolled in Medicaid for at least six months post-release, 1016 (13.2%) had an ED visit. Among the 4607 White releases, 553 (12.0%) had an ED visit within six months, compared to 13.8% (375/2728) of Black releases and 25.1% (88/350) of releases of other races. Relative to White individuals, Black individuals were 1.23 times more likely (95% CI 1.04–1.47; P=0.019) and individuals of other races were 2.64 times more likely (95% CI 1.91–3.64; P<0.001) to have an ED visit. There were 46 visits to the ED for a general drug overdose and 28 visits for an opioid-specific overdose among White individuals. Among Black individuals, there were 10 visits to the ED for a general drug overdose. Additional data on general drug overdoses and opioid-specific overdoses among Black individuals and individuals of other races were suppressed due to small cell sizes.
Among the 1016 releases with an ED visit within six months post-release, the average time to a visit was 44.1 days (standard deviation: 48.4). Kaplan-Meier curves comparing the rate at which individuals in each racial group had an ED visit post-release are presented in Figure B.2. Compared to White individuals, the rate at which individuals of other races had an ED visit was 1.44 times higher (95% CI 1.15–1.80; P=0.002). Among those who had an ED visit, there was no significant difference between the rate at which Black individuals and White individuals had a visit (OR: 1.00; 95% CI 0.821–1.22; P=0.997).
Figure B.2:
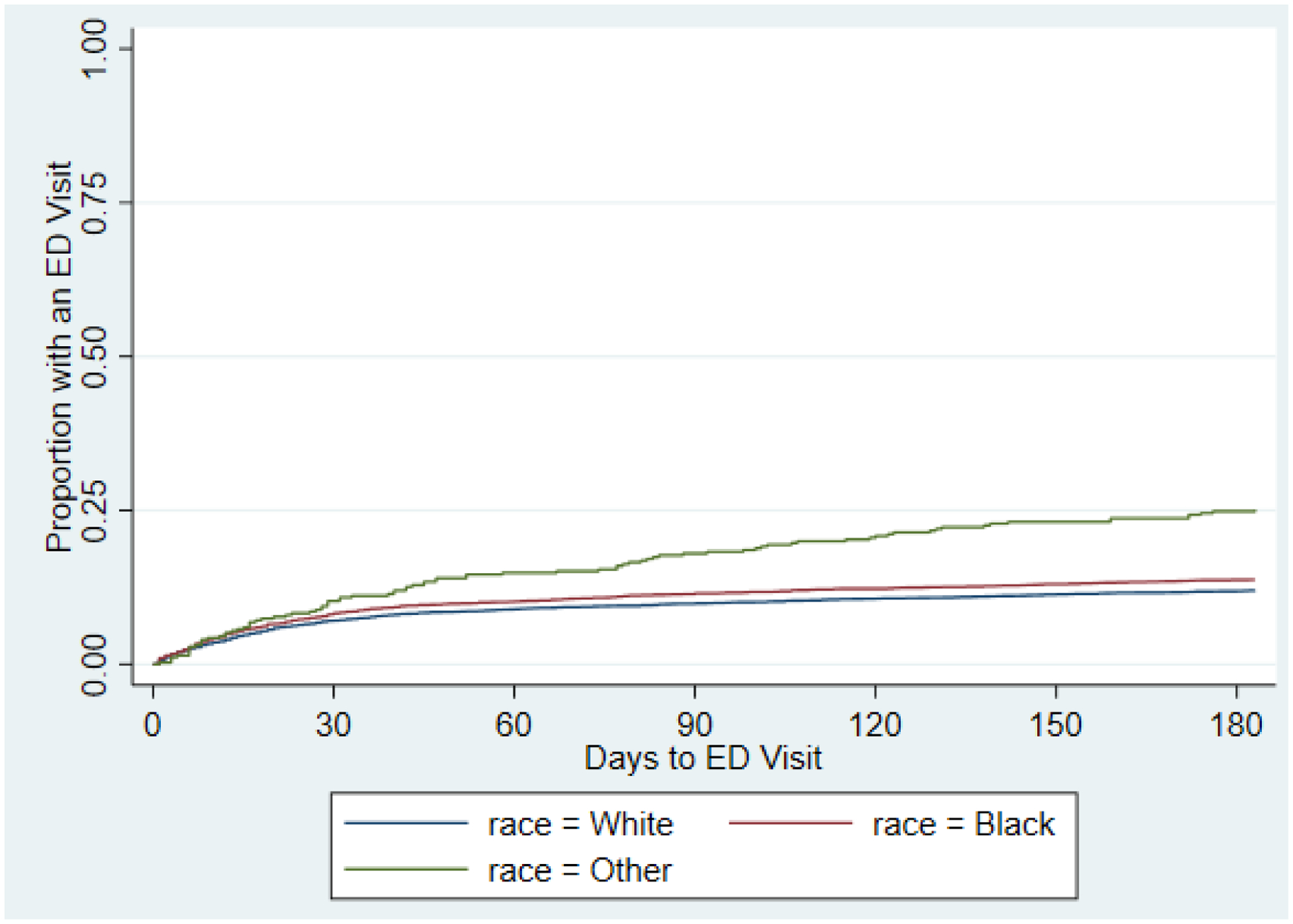
Time to any ED visit, by race, among adults released from Wisconsin correctional facilities with a history of substance use, April 2015 - June 2017
Receipt of MOUD
Among the 4607 White releases enrolled in Medicaid for at least six months post-release, 368 (8.0%) had a claim for MOUD within six months, compared to 1.1% (30/2728) of Black releases and 4.3% (15/350) of releases of other races. Relative to White individuals, Black individuals were 0.100 times less likely (95% CI 0.054–0.184; P<0.001) and individuals of other races were 0.435 times less likely (95% CI 0.220–0.859; P=0.016) to receive MOUD within six months of release.
DISCUSSION
Principal Findings
The goal of this study was to determine whether racial disparities in Medicaid enrollment exist among those released from prison with a history of substance use, and among those who do enroll in Medicaid, whether racial disparities in healthcare utilization exist. Despite the fact that Black individuals were slightly more likely than White individuals to enroll in Medicaid in the month of release, Black individuals were significantly less likely to utilize non-emergency outpatient services, and more likely to use the ED. This study also found that individuals of other races were significantly less likely than White individuals to enroll in Medicaid in the month of release. This finding must be interpreted with caution because approximately 86% of individuals of other races were American Indian or Alaskan Native, and many of these individuals may have healthcare access through the Indian Health Service (IHS), which provides direct medical and public health services to members of federally-recognized Native American Tribes and Alaska Native people (U.S. Department of Health and Human Services n.d.). However, similar to Black individuals, individuals of other races who did enroll in Medicaid were significantly less likely to utilize outpatient, non-emergency services after release from prison, and significantly more likely to utilize the ED. Non-White individuals were also significantly less likely than White individuals to receive MOUD within 6 months of release. Our findings demonstrate that racial disparities in healthcare service utilization continue to harm non-White, criminal justice-involved individuals, despite Medicaid expansion policies. This highlights the need for novel post-incarceration linkage to care models that address cultural needs for non-white individuals.
These results are consistent with previous studies conducted among the general population, which demonstrate increased use of the ED as the usual source of care and poorer access to MOUD among people of color (Brown et al. 2012; Hansen et al. 2016; Lagisetty et al. 2019). Because outpatient services encompass a variety of visit types, from an annual exam with a primary care physician to a consultation with a specialist, the literature on racial and ethnic disparities in outpatient care is mixed. In the current study, we use a very inclusive definition of outpatient visit which includes all non-emergency department outpatient visits billed to Medicaid. Prior studies demonstrate that African Americans and Hispanics are less likely to report their usual source of care is a doctor’s office, and they are more likely to depend on community health centers and EDs (Gaskin et al. 2007; Lillie-Blanton, Martinez, and Salganicoff 2013; The Commonwealth Fund 2002). The influence of race/ethnicity on where people receive health care warrants further investigation.
Strengths and Limitations
A strength of the current study is that we include all individuals with a history of substance use, despite whether they had a SUD diagnosis. This is important because prior studies demonstrate that White individuals have higher prevalence rates of diagnosed substance abuse disorders than do other racial and ethnic groups (Breslau et al. 2005; Kessler et al. 2005). Lower receipt of a SUD diagnosis coupled with lower receipt of outpatient care, as found in the current study, among Black individuals exacerbates racial disparities in health outcomes and must be addressed. Future studies are needed that examine racial disparities in the full continuum of care for substance abuse treatment and develop effective interventions and policies.
This study is not without limitations. A subset of our sample was identified using the COMPAS tool’s substance use treatment need score. This score has not been validated relative to a clinical or diagnostic tool. However, the prevalence of history of substance use that we observe in our sample is consistent with published estimates within state prison populations suggesting reasonable face validity (Bronson et al., 2017). Additionally, the COMPAS tool collects self-reported data and we were unable to determine whether self-reported substance use differed by race. Furthermore, the COMPAS tool does not collect diagnostic criteria for opioid use disorder and we were unable to determine type of SUD. Thus, there may be differential need for MOUD in the sample and the finding that non-White individuals were significantly less likely than White individuals to receive MOUD within 6 months of release must be interpreted with caution. Living with, or at risk of, HCV is also an imperfect proxy for having a history of injection drug use. It is possible that individuals living with HCV were infected through other means of transmission (e.g., blood transfusion). Additionally, the DOC’s risk-based screening instrument that determines HCV testing upon intake may capture people born between 1945–1965 (“baby boomers”), who have no other behavioral risks (Stockman et al. 2016). However, because individuals who are incarcerated likely have a different risk profile for HCV than the general baby boomer population, we expect most individuals living with, or at risk of, HCV in this study to have a history of injection drug use. Furthermore, the results from this study remained consistent when excluding persons who only met the inclusion criterion of living with, or at risk of, HCV (see Appendix B).
Because ethnicity data was missing for the majority of the study sample (66%), we were unable to examine ethnic disparities in Medicaid enrollment and post-release healthcare utilization. Future studies that examine these disparities among Hispanic or Latino, American Indian or Alaska Native, Asian, Native Hawaiian or other Pacific Islander populations are warranted. Lastly, generalizability is limited to individuals enrolled in Medicaid for 6 consecutive months post-release. Although we were unable to determine why an individual disenrolled within 6 months, we compared the duration of Medicaid enrollment across racial groups and found that the proportion of individuals who disenroll is comparable across racial groups (Appendix C).
Conclusions
In conclusion, racial disparities in Medicaid enrollment and healthcare use after release from incarceration are prevalent among people with a history of substance use. These disparities persist after expanding Medicaid eligibility criteria and implementing a prison-based enrollment assistant program. Continued lack of access to quality healthcare providers and effective substance use disorder treatment services among people of color will worsen existing disparities and prevent curbing of the mass incarceration and substance abuse epidemics plaguing the U.S. Equal access to essential healthcare services across all racial and ethnic groups is imperative. Further understanding how racial differences exist in order to enact policies and practices are warranted.
Highlights.
Black individuals released from prison are less likely to use outpatient services
Black persons are less likely to receive opioid use disorder treatment post-release
Higher use of emergency department among recently incarcerated Black persons
Similar rates of Medicaid enrollment between Black and White individuals
Acknowledgements:
The authors would like to thank the Wisconsin Department of Corrections and Department of Health services, for the use of data for this analysis, but these agencies do not certify the accuracy of the analyses presented.
Funding:
This work was supported by the Wisconsin Partnership Program and the National Institutes of Health [grant numbers R01DA047889-01 and 3UG3DA044826-02S1. Dr. Karli Hochstatter is supported by the National Institutes of Health [grant number T32DA037801].
Appendix A:
COMPAS Data Collection
The underlying function of the COMPAS instrument is to assess risk of recidivism including potentially modifiable correlates of recidivism including substance use.1,2 Available assessments of the validity of the COMPAS substance use score concern the degree to which this score is associated with recidivism rather than a clinical diagnosis of substance use disorder.1
The COMPAS tool is composed of various assessments. We obtained the most recently completed COMPAS assessments relative to the individual’s release date, and no more than 120 days after their release. An assessment may have a date after the release if it was conducted through the community supervision program.
Identifying individuals with a highly probable need for substance use treatment
For each individual, the Wisconsin Department of Corrections (WI DOC) aims to collect information at least once using the COMPAS Core assessment at intake or the COMPAS Reentry assessment close to the time of release.
There are some differences in the Core and Reentry assessments with respect to the substance use history questions although the WI DOC generates the same 3-category score indicating a need for treatment from each assessment: highly probable, probable, and unlikely. The specific questions on which this score is based for each assessment are noted below. We do not have access to the proprietary algorithm used to generate the score. However, in our internal analysis the vast majority of individuals identified as “highly probable” using the Core assessment had three or more positive responses to the substance use history questions. Using the Reentry assessment, the vast majority of individuals identified as highly probable had five or more positive response to the substance use history questions.
CORE Instrument Substance Use History Questions
Do you think your current/past legal problems are partly because of alcohol or drugs?
Were you using alcohol when arrested for your current offense?
Were you using drugs when arrested for your current offense?
Are you currently in formal treatment for alcohol or drugs such as counseling, outpatient, inpatient, residential?
Have you ever been in formal treatment for alcohol such as counseling, outpatient, inpatient, residential?
Have you ever been in formal treatment for drugs such as counseling, outpatient, inpatient, residential?
Do you think you would benefit from getting treatment for alcohol?
Do you think you would benefit from getting treatment for drugs?
Did you use heroin, cocaine, crack or methamphetamines as a juvenile?
COMPAS Reentry Instrument Substance Use History Questions
Committed Offenses while high/drunk?
Prior drug charges/convictions?
History of drug problems?
History of alcohol problems?
Prior treatments for drug/alcohol abuse?
Any history of failed drug/urine analysis test?
Is the inmate at risk for substance abuse problems?
Identifying individuals with self-reported opioid use
Another COMPAS assessment, the COMPAS Substance Abuse Module, which is not used in the above algorithm, asks individuals what substances they have a history of using. From the list of self-reported substances, the following are identified as opiates: buprenorphine, codeine, fentanyl, heroin, methadone, morphine, opiates, and Vicodin. Staff at the WI DOC, which include staff from WI DOC community corrections programs, are required to enter data into this assessment at intake. When an individual is reincarcerated or placed under community supervision, information may be added to this assessment. Thus, data on substances ever used likely became more complete over time (i.e. data is cumulative).
WI DOC staff members collecting the COMPAS data record all substances the individual self-reports having used. Although the purpose of this data point is to understand problematic drug use (e.g., misuse of prescription drugs and illicit drug use), it is possible that respondents interpret the question differently and report opioids used for pain management. We believe this scenario is uncommon because DOC staff collecting the data are aware of what information the question aims to collect. However, we cannot guarantee that people who used opioids strictly for pain management have been entirely excluded.
Appendix B:
We conducted a sensitivity analysis to determine whether the results found in this study remained consistent when excluding persons who only met the inclusion criterion of living with, or at risk of, HCV (inclusion criterion #3).
Table:
Prison releases in which healthcare services were utilized within 6 months of release among adults with a history of substance use who released from a Wisconsin state correctional facility and were enrolled in Medicaid for at least 6 months, April 2015 -- June 2017
| White (N=3187) REFERENCE n (%) | Black (N=1639) n (%) | Adjusted** OR (95% CI) | Other (N=235) n (%) | Adjusted** OR (95% CI) | |
|---|---|---|---|---|---|
| Any outpatient visit | 2390 (75.0) | 835 (51.0) | 0.314 (0.239–0.412)* | 158 (67.2) | 0.611 (0.405–0.920)* |
| An outpatient visit with SUD diagnosis | 947 (29.7) | 94 (5.7) | 0.110 (0.067–0.177)* | 71 (30.2) | 1.02 (0.689–1.515) |
| Any ED visit | 413 (13.0) | 230 (14.0) | 1.09 (0.869–1.364) | 62 (26.4) | 2.78 (1.84–4.19)* |
| Receipt of MOUD | 321 (10.1) | 21 (1.28) | 0.084 (0.039–0.179)* | 13 (5.53) | 0.448 (0.209–0.959)* |
P<0.05
Adjusted for gender, age at release, education, marital status, rurality of county of release, and months incarcerated
Appendix C:
To evaluate whether there were any differences in the length of time individuals of different racial groups were enrolled in Medicaid, we created survival plots using Kaplan-Meier estimation to compare the time enrolled between Black, White, and other racial groups. Individuals enrollment ended at the time in which they disenrolled from Medicaid or at the end of the study period (June 2017), whichever came first.
Figure:
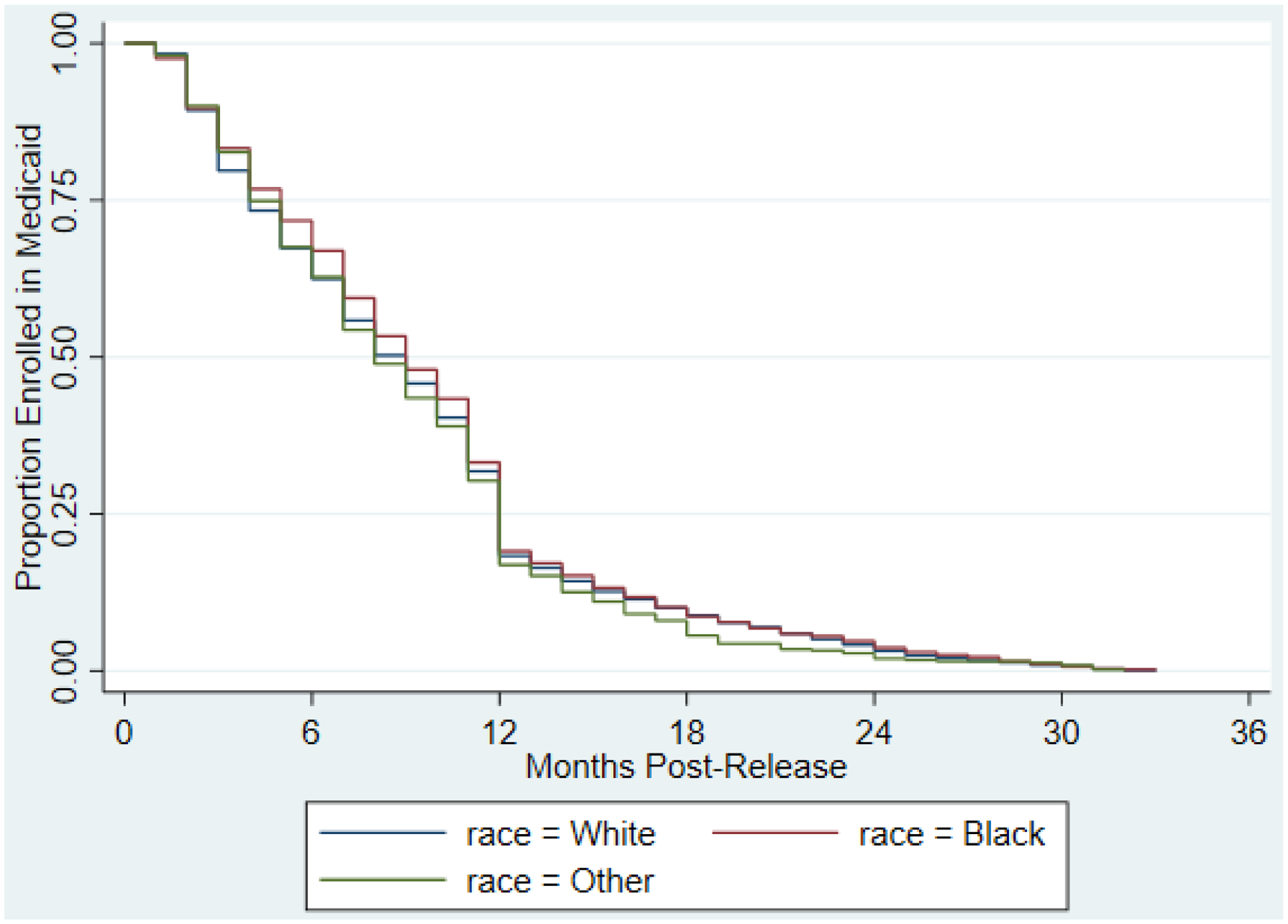
Length of time (months) enrolled in Medicaid during the study period (April 2015 - June 2017) after release from a Wisconsin correctional facility, by racial group.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none
Bibliography
- AcademyHealth. n.d. “The Medicaid Outcomes Distributed Research Network (MODRN) |AcademyHealth.” Retrieved December 9, 2020 (https://www.academyhealth.org/about/programs/medicaid-outcomes-distributedresearch-network-modrn).
- American Society of Addiction Medicine. (n.d.). Medicaid Coverage of Medications for the Treatment of Opioid Use Disorder. Retrieved March 10, 2021, from https://www.asam.org/docs/default-source/advocacy/State-medicaid-reports/State-medicaid-reports_wi.pdf
- Ann Carson E 2020. “Prisoners in 2018.” U.S. Department of Justice. Office of Justice Programs. Bureau of Justice Statistics. Retrieved September 11, 2020 (https://www.bjs.gov/content/pub/pdf/p18.pdf).
- Bandara SN, Huskamp HA, Riedel LE, McGinty EE, Webster D, Toone RE, & Barry CL (2015). Leveraging The Affordable Care Act To Enroll Justice-Involved Populations In Medicaid: State And Local Efforts. Health Affairs, 34(12), 2044–2051. 10.1377/hlthaff.2015.0668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgartner JC, Collins SR, Radley DC, & Hayes SL (2020, January). How ACA Narrowed Racial Ethnic Disparities Access to Health Care. Commonwealth Fund. 10.26099/kx4k-y932 [DOI] [Google Scholar]
- Beck A (2020, February 20). Medicaid Enrollment Programs Offer Hope To Formerly Incarcerated Individuals And Savings For States | Health Affairs Blog. Health Affairs Blog. https://www.healthaffairs.org/do/10.1377/hblog20200218.910350/full/ [Google Scholar]
- Breslau Joshua, Kendler Kenneth S., Su Maxwell, Gaxiola-Aguilar Sergio, and Kessler Ronald C.. 2005. “Lifetime Risk and Persistence of Psychiatric Disorders across Ethnic Groups in the United States.” Psychological Medicine 35(3):317–27. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronson J, Stroop J, Zimmer S, & Berzofsky M (2017). Drug Use, Dependence, and Abuse Among State Prisoners and Jail Inmates, 2007–2009 (NCJ 250546; p. 27). https://www.bjs.gov/content/pub/pdf/dudaspji0709.pdf
- Brown Lindsay E., Burton Ryan, Hixon Brian, Kakade Manasi, Bhagalia Parul, Vick Catherine, Edwards Andrew, and Hawn Mary T.. 2012. “Factors Influencing Emergency Department Preference for Access to Healthcare.” Western Journal of Emergency Medicine 13(5):410–15. doi: 10.5811/westjem.2011.11.6820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown Patricia, and Thornton Katie. 2020. Technical Report on Lessons Learned in the Development of the Institute for Research on Poverty’s Wisconsin Administrative Data Core.
- Budhwani Henna, and De Prabal. 2019. “Perceived Stigma in Health Care Settings and the Physical and Mental Health of People of Color in the United States.” Health Equity 3(1):73–80. doi: 10.1089/heq.2018.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Justice Statistics. 2016. Police Behavior during Traffic and Street Stops, 2011.
- Bureau of Justice Statistics. 2018. “Prisoners in 2016.”
- Burns M, Cook S, Brown L, Tyska S, & Westergaard R (2021). Increasing Medicaid enrollment among formerly incarcerated adults. Health Services Research. 10.1111/1475-6773.13634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Council on Criminal Justice. 2019. “Trends in Correctional Control by Race and Sex.” Retrieved September 27, 2020 (https://cdn.ymaws.com/counciloncj.org/resource/collection/4683B90A-08CF-493F-89ED-A0D7C4BF7551/Trends_in_Correctional_Control_-_FINAL.pdf).
- Dumont Dora M., Brockmann Brad, Dickman Samuel, Alexander Nicole, and Rich Josiah D.. 2012. “Public Health and the Epidemic of Incarceration.” Annual Review of Public Health 33(1):325–39. doi: 10.1146/annurev-publhealth-031811-124614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egede Leonard E. 2006. “Race, Ethnicity, Culture, and Disparities in Health Care.” Journal of General Internal Medicine 21(6):667–69. doi: 10.1111/j.1525-1497.2006.0512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egede Leonard E., and Zheng Deyi. 2003. “Racial/Ethnic Differences in Influenza Vaccination Coverage in High-Risk Adults.” American Journal of Public Health 93(12):2074–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella Kevin, Franks Peter, Doescher Mark P., and Saver Barry G.. 2002. “Disparities in Health Care by Race, Ethnicity, and Language among the Insured: Findings from a National Sample.” Medical Care 40(1):52–59. [DOI] [PubMed] [Google Scholar]
- Gaskin Darrell J., Arbelaez Jose J., Brown Jorielle R., Petras Hanno, Wagner Fernando A., and Cooper Lisa A.. 2007. “Examining Racial and Ethnic Disparities in Site of Usual Source of Care.” Journal of the National Medical Association 99(1):22–30. [PMC free article] [PubMed] [Google Scholar]
- Grodensky CA, Rosen DL, Blue CM, Miller AR, Bradley-Bull S, Powell WA, Domino ME, Golin CE, & Wohl DA (2018). Medicaid Enrollment among Prison Inmates in a Non-expansion State: Exploring Predisposing, Enabling, and Need Factors Related to Enrollment Pre-incarceration and Post-Release. Journal of Urban Health : Bulletin of the New York Academy of Medicine, 95(4), 454–466. 10.1007/s11524-018-0275-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen Helena, Siegel Carole, Wanderling Joseph, and Danae DiRocco. 2016. “Buprenorphine and Methadone Treatment for Opioid Dependence by Income, Ethnicity and Race of Neighborhoods in New York City.” Drug and Alcohol Dependence 164:14–21. doi: 10.1016/j.drugalcdep.2016.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris DR, Andrews R, and Elixhauser A. 1997. “Racial and Gender Differences in Use of Procedures for Black and White Hospitalized Adults.” Ethnicity & Disease 7(2):91–105. [PubMed] [Google Scholar]
- Harris David A. 2012. HEARING ON “ENDING RACIAL PROFILING IN AMERICA”.
- Kessler Ronald C., Berglund Patricia, Demler Olga, Jin Robert, Merikangas Kathleen R., and Walters Ellen E.. 2005. “Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication.” Archives of General Psychiatry 62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kunins Hillary V. 2020. “Structural Racism and the Opioid Overdose Epidemic: The Need for Antiracist Public Health Practice.” Journal of Public Health Management and Practice 26(3):201–205. doi: 10.1097/PHH.0000000000001168. [DOI] [PubMed] [Google Scholar]
- Lagisetty Pooja A., Ross Ryan, Bohnert Amy, Clay Michael, and Maust Donovan T.. 2019. “Buprenorphine Treatment Divide by Race/Ethnicity and Payment.” JAMA Psychiatry 76(9):979–81. doi: 10.1001/jamapsychiatry.2019.0876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillie-Blanton Marsha, Rose Marie Martinez, and Alina Salganicoff. 2013. “Site of Medical Care: Do Racial and Ethnic Differences Persist?” Yale Journal of Health Policy, Law, and Ethics 1(1). [PubMed] [Google Scholar]
- Mauer Marc. 2011. “Addressing Racial Disparities in Incarceration.” 91(3). doi: 10.1177/0032885511415227. [DOI] [Google Scholar]
- Mayberry Robert M., Mili Fatima, and Ofili Elizabeth. 2016. “Racial and Ethnic Differences in Access to Medical Care:” Medical Care Research and Review. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- Nelson Alan. 2002. “Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care.” Journal of the National Medical Association 94(8):666–68. [PMC free article] [PubMed] [Google Scholar]
- Northpointe Inc. 2012. “Practitioners Guide to COMPAS.” Retrieved September 10, 2020 (http://www.northpointeinc.com/files/technical_documents/FieldGuide2_081412.pdf).
- Northpointe Institute for Public Management Inc. 2009. “Measurement & Treatment Implications of COMPAS Core Scales.” Retrieved September 10, 2020 (https://www.michigan.gov/documents/corrections/Timothy_Brenne_Ph.D.__Meaning_and_Treatment_Implications_of_COMPA_Core_Scales_297495_7.pdf).
- O’Hear Michael M. 2009. “Rethinking Drug Courts: Restorative Justice as a Response to Racial Injustice.” Stanford Law & Policy Review 20:463. [Google Scholar]
- Pierson Emma, Simoiu Camelia, Overgoor Jan, Sam Corbett-Davies Daniel Jenson, Shoemaker Amy, Ramachandran Vignesh, Barghouty Phoebe, Phillips Cheryl, Shroff Ravi, and Goel Sharad. 2020. “A Large-Scale Analysis of Racial Disparities in Police Stops across the United States.” Nature Human Behaviour 4(7):736–45. doi: 10.1038/s41562-020-0858-1. [DOI] [PubMed] [Google Scholar]
- Prison Policy Initiative. 2018. “States of Incarceration: The Global Context 2018.” Retrieved September 11, 2020 (https://www.prisonpolicy.org/global/2018.html).
- Rosenberg Alana, Groves Allison K., and Blankenship Kim M.. 2017. “Comparing Black and White Drug Offenders: Implications for Racial Disparities in Criminal Justice and Reentry Policy and Programming.” Journal of Drug Issues 47(1):132–42. doi: 10.1177/0022042616678614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockman Lauren J., Greer James, Holzmacher Ryan, Dittmann Beth, Hoftiezer Scott A., Alsum Lori E., Prieve Audrey, Westergaard Ryan P., Guilfoyle Sheila M., and Vergeront James M.. 2016. “Performance of Risk-Based and Birth-Cohort Strategies for Identifying Hepatitis C Virus Infection Among People Entering Prison, Wisconsin, 2014.” Public Health Reports 131(4):544–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Commonwealth Fund. 2002. “Diverse Communities, Common Concerns: Assessing Health Care Quality for Minority Americans – Findings from the Commonwealth Fund 2001 Health Care Quality Survey.” 80. [Google Scholar]
- The Sentencing Project. 2016. “The Color of Justice: Racial and Ethnic Disparity in State Prisons.” Retrieved September 11, 2020 (https://www.sentencingproject.org/publications/color-of-justice-racial-and-ethnic-disparity-in-state-prisons/).
- Tonry Michael H. 2011. Punishing Race: A Continuing American Dilemma. Oxford University Press. [Google Scholar]
- United States Sentencing Commission. 2017. Demographic Differences in Sentencing: An Update to the 2012 Booker Report. Washington, D.C. [Google Scholar]
- U.S. Census Bureau. (2019). QuickFacts: Wisconsin. https://www.census.gov/quickfacts/WI
- U.S. Department of Health and Human Services. n.d. “Indian Health Service | Indian Health Service (IHS).” Indian Health Service Retrieved December 7, 2020 (https://www.ihs.gov/default/).
- Vera Institute of Justice. 2019. “State Incarceration Trends in Wisconsin.” Retrieved September 11, 2020 (https://www.vera.org/downloads/pdfdownloads/state-incarceration-trends-wisconsin.pdf).
- Wenneker MB, and Epstein AM. 1989. “Racial Inequalities in the Use of Procedures for Patients with Ischemic Heart Disease in Massachusetts.” JAMA 261(2):253–57. [PubMed] [Google Scholar]
- Zibbell Jon E., Iqbal Kashif, Patel Rajiv C., Suryaprasad Anil, Sanders Kathy J., Moore-Moravian Loretta, Serrecchia Jamie, Blankenship Steven, Ward John W., Holtzman Deborah, Control Centers for Disease, and Prevention. 2015. “Increases in Hepatitis C Virus Infection Related to Injection Drug Use among Persons Aged ≤30 Years - Kentucky, Tennessee, Virginia, and West Virginia, 2006–2012.” MMWR. Morbidity and Mortality Weekly Report 64(17):453–58. [PMC free article] [PubMed] [Google Scholar]
References
- 1.Northpointe, Inc. Practitioner’s Guide to COMPAS Core. 2019. Accessed 1/27/20 at http://www.northpointeinc.com/files/technical_documents/FieldGuide2_081412.pdf
- 2.Northpointe Institute for Public Management, Inc. Measurement & Treatment Implications of COMPAS Core Scales. March 30, 2009. Accessed 1/27/20 at https://www.michigan.gov/documents/corrections/Timothy_Brenne_Ph.D.__Meaning_and_Treatment_Implications_of_COMPA_Core_Scales_297495_7.pdf


