Abstract
Social isolation in community-dwelling older adults with dementia is a growing health issue that can negatively affect health and well-being. To date, little attention has been paid to the role of technology in improving their social participation. This systematic review aims to provide a systematic overview of the effects of technological interventions that target social participation in community-dwelling older adults with and without dementia. The scientific databases Medline (PubMed), PsycINFO, CINAHL, Web of Science, and the Cochrane Library were systematically searched and independently screened by two reviewers. Results were synthesized narratively. The methodological quality of included studies was independently assessed by two reviewers. In total, 36 studies of varying methodological quality were identified. Most studies evaluated social networking technology and ICT training programs. Three studies focused on people with dementia. Quantitative findings showed limited effects on loneliness, social isolation, and social support. Nevertheless, several benefits related to social participation were reported qualitatively. Social interaction, face-to-face contact, and intergenerational engagement were suggested to be successful elements of technological interventions in improving the social participation of community-dwelling older adults. Rigorous studies with larger sample sizes are highly needed to evaluate the long-term effects of technology on the multidimensional concept of social participation.
Keywords: social participation, technology, dementia, older adults, community
1. Introduction
The world’s population is aging due to demographic changes. In 2020, 727 million people were aged 65 and over. According to the Department of Economic and Social Affairs of the United Nations, 1.5 billion people worldwide will be above this age by 2050 [1]. At the same time, the prevalence of dementia and other age-related neurodegenerative conditions is steadily increasing. Currently, there are 50 million people living with dementia worldwide. This number is expected to increase to 152 million by 2050 [2].
Social isolation is a growing health issue in the aged population [3,4]. It has been reported that more than 75 million adults in Europe experience social isolation [5]. In the United States, 24% of community-dwelling older adults were estimated to be socially isolated [6]. Recently, these numbers have increased rapidly across the globe due to the COVID-19 pandemic, especially among people with cognitive impairment [7]. In a recent Dutch study, more than half of the community-dwelling participants with cognitive decline reported not having any face-to-face contact with friends (52%) or family (57%) during the pandemic [7]. This kind of social isolation can negatively affect their mental and physical health [8,9], mortality [10], well-being, and quality of life [11]. Furthermore, poor social engagement is positively associated with an increased dementia risk [12,13,14]. Correspondingly, social relationships and participation in social activities can have a protective effect against cognitive decline and dementia [14,15]. However, community-dwelling people with dementia tend to experience difficulties participating in social situations, which might be the result of limited emotion perception [16], irritability, and fluctuating mood [17]. Moreover, due to the progressive deterioration of cognitive skills and the stigma associated with dementia, they are more likely to avoid social situations out of embarrassment or to even lose their interest in socializing in the community [18,19]. In combination with difficulties in spatial orienting, this avoiding behavior can result in limited participation in social activities, which subsequently can lead to social isolation and feelings of loneliness [19,20]. While social isolation refers to the objective lack of social connections, loneliness refers to the subjective feeling of lacking social connections [21].
There is a growing body of literature that has endorsed the urgent need for interventions targeting social participation in older adults. The definition of social participation, however, varies in the literature. In the renewed definition of health by Huber et al., social participation is one of the domains of social health and is described as “the ability to participate in social activities including work” [22] (p. 2). Whereas this definition focuses on the ability to socially participate, the definition by Levasseur et al. focuses on the element of social interaction [23]. According to them, social participation is defined as the “person’s involvement in activities that provide interaction with others in society or the community” [23] (p. 2148). Various studies in the field of gerontology have been using different concepts with comparable definitions, such as social connectedness [24] or social engagement [14]. Despite the indistinct use of these closely-related concepts, researchers agree on the potential benefits of psychosocial interventions in terms of (1) reducing social isolation or feelings of loneliness [3,8,25], (2) increasing well-being by fulfilling social needs [26,27], or (3) reducing mild cognitive impairment (MCI) and dementia risk [13]. Furthermore, several systematic reviews have highlighted the potential of technological interventions in enhancing the social participation of older adults [24,28,29,30]. Especially during the COVID-19 pandemic, the role of technological interventions has become crucial in preventing social isolation and loneliness [31].
Despite the vulnerability of people with dementia for social isolation, and their essential need for social contacts, very little attention has been paid to the effects of technological interventions that target social participation in this population [32,33]. To date, only one systematic review that explored the effects of ICT-based applications on the social participation of people with dementia could be identified [34]. The review includes different types of technology, such as electronic tagging technology, smart homes, and regular computers. The results of this systematic review indicate that technological solutions could facilitate and enhance social participation. Nevertheless, only two of the included studies had used a quantitative control group design, and the overall methodological quality of the included studies was—according to Pinto-Bruno et al.—poor [34]. In addition, the review covered literature published up to May 2016. It is likely that new technological interventions have been developed in the past five years, given the rising digital literacy among older adults [35]. As such, it is important to keep abreast of the developments. Since this review had a specific focus on people with dementia who live in residential care facilities, it is still unclear how technological interventions influence the social participation among older adults with dementia living in the community.
The present systematic review aims to provide a comprehensive overview of the effects of technological interventions that address social participation in community-dwelling older adults with dementia. In this paper, the definition of social participation by Levasseur et al. [23] will be used. Due to limited studies that directly target people with dementia, this systematic review included studies targeting older adults with and without dementia in order to provide a broader scope. Therefore, the following research questions were formulated: (1) what technological interventions have been studied that address the social participation of community-dwelling older adults with and without dementia, and (2) what are their effects and elements of success? It is anticipated that this research will contribute to a better understanding of technological interventions that have been studied and their role in enhancing social participation in community-dwelling older adults with and without dementia.
2. Materials and Methods
This systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (registration number: CRD42020206654). It followed the procedures for systematic review reporting as stated by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [36].
2.1. Search Strategy
In June 2020, the five electronic databases Medline (PubMed), PsycINFO, CINAHL, Web of Science, and the Cochrane Library were systematically searched. During the development of the search strategy, it was discovered that there are only limited studies referring to people with cognitive impairment. Consequently, the search was extended to studies that evaluated a technological intervention related to the social participation of community-dwelling older adults with and without cognitive impairment. The last search was conducted on 22 June 2020. In a later stage, citation tracing was used to identify additional studies from the reference lists of included studies and relevant systematic reviews [24,28,29,30,37].
The search strategy was based on the PICO model. It included synonyms of the following three categories: “older adults” (population), “technology” (intervention), and “social participation” (outcome). The search strategy used a combination of free text words with Medical Subject Headings (MeSH), Thesaurus terms, or CINAHL Subject Headings. It covered studies published between January 2000 and June 2020. The strategies for each of the electronic databases were developed and conducted by the first reviewer, discussed with the research team, and peer reviewed by an expert scientific information specialist of the Maastricht University Library. The full electronic search strategy conducted in Medline (PubMed) is displayed in Table 1.
Table 1.
Full search strategy of electronic database Medline (PubMed).
| Categories | Search Terms |
|---|---|
| #1 Population synonyms | Middle Aged[MeSH] OR middle aged[title/abstract] OR Aged[MeSH] OR aged[title/abstract] OR elderly[title/abstract] OR older adults[title/abstract] |
| #2 Intervention synonyms | Technology[title/abstract] OR technological[title/abstract] OR technologies[title/abstract] |
| #3 Outcome synonyms | Community Participation[MeSH] OR community participation[title/abstract] OR Social Participation[MeSH] OR social participation[title/abstract] OR Interpersonal Relations[MeSH] OR interpersonal relations[title/abstract] OR Social Isolation[MeSH] OR social isolation[title/abstract] OR social health[title/abstract] OR social activity[title/abstract] OR social activities[title/abstract] OR social interaction[title/abstract] |
| Limiters | Results by year: from 2000–2020 |
| #4 Combination of categories | #1 AND #2 AND #3 |
2.2. Eligibility Criteria
Studies had to meet the following study characteristics to be included in the systematic review: (1) reported the effects of a technological intervention (no design restrictions imposed), (2) were aimed at community-dwelling older adults (defined as aged 55 and older) with or without cognitive impairment, (3) targeted social participation (defined as a “person’s involvement in activities that provide interaction with others in society or the community” [23] (p. 2148)) and/or social isolation, or reported effects related to social participation/social isolation, and (4) reported at least one outcome related to older adults with or without cognitive impairment. In order to ensure the accessibility of the systematic review findings within the international scientific community, only studies written in English were included. Furthermore, studies had to be published in 2000 or later to be included in the present review.
2.3. Study Selection
Two reviewers screened independently the titles and abstracts (P.H. and L.M.M.B.) and the full-texts (P.H. and W.Q.K.) of identified records, using a screening tool based on the eligibility criteria (see in Supplementary Materials). Discrepancies regarding the inclusion of full-text records were discussed with a third reviewer (M.E.d.V.) and resolved by consensus. If multiple reports of the same study were included in the systematic review, they were treated as a single study, after comparing for any discrepancies. The reference lists of included full-text records were screened by the first reviewer in order to possibly include additional studies. The records identified through citation tracing followed the same screening process as the records identified through the electronic search strategy.
2.4. Data Extraction
Data extraction of the included full-text records was performed by the first reviewer and checked by a second reviewer. Discrepancies regarding the extracted data were discussed between the two reviewers and resolved by consensus. The data extraction form (see in Supplementary Materials) was developed by the first reviewer and discussed with the research team. The form was pilot-tested on five randomly selected full-text records and subsequently adapted. When additional information or clarification regarding study data was required, the corresponding author of the study was contacted by mail.
Information relating to the general study characteristics was extracted, such as the country of data collection, the study aim, the study design, and the study population. To gain insight into the effects of technological interventions, information about the study outcomes (definition of outcomes, time points measured, outcome measures, and their validity) as well as the main findings/conclusions was extracted. Detailed information about the intervention was also extracted. This information included the aim, duration, timing, providers, setting, and theoretical basis of the intervention. In addition, text passages were extracted that possibly indicated factors explaining the success or failure of the technological intervention in influencing social participation.
2.5. Data Synthesis
Due to the heterogeneity of study designs, types of technologies, structure of interventions, and outcome measures of included studies, a quantitative synthesis of results was not appropriate. Therefore, a narrative synthesis was conducted to summarize the findings of included studies using descriptive tables and textual descriptions [38].
2.6. Quality Assessment
Two reviewers (P.H. and W.Q.K.) independently assessed the methodological quality of the included studies, discussed their individual ratings, and agreed on a final rating. Three different quality assessment tools were used, based on the study design of the included studies: quantitative, qualitative, or mixed methods. The kappa coefficients (κ) for the individual ratings of each assessment tool were calculated to determine the inter-rater agreement [39].
Given the variety in study design of included quantitative studies, the Effective Public Health Practice Project (EPHPP) tool was used to rate their methodological quality and to assess the risk of bias at the study level [40]. The tool consists of six component ratings, stimulating the reviewer to critically reflect whether: (1) study participants were representative of the study population, (2) randomization was used, (3) relevant confounders were described and controlled, (4) outcome assessor(s) and study participants were blinded, (5) data collection tools were shown to be valid and reliable, and (6) withdrawals and drop-outs were reported. The rating of each component (i.e., strong, moderate, or weak) was facilitated by a dictionary and led to an overall rating of the methodological quality (i.e., strong, moderate, or weak).
To appraise the methodological quality of included qualitative studies, a checklist based on the quality criteria synthesized by Walsh and Downe was used [41]. These quality criteria were chosen for their detailed description and their coverage of the concept of trustworthiness in qualitative research as defined by Lincoln and Guba [42]. Within the checklist, each of the 12 criteria was rated (i.e., criterion met, criterion partly met, or criterion unmet), covering the following categories: scope and purpose, design, sampling strategy, analysis, interpretation, reflexivity, ethical dimensions, and relevance and transferability. In a next step, points were awarded for each rated criterion (i.e., criterion met = 1 point, criterion partly met = 0.5 points, criterion unmet = 0 points). By adding up the points, an overall rating of the methodological quality with a maximum of 12 points was determined.
Studies in this systematic review were considered as mixed methods studies as long as a combination of qualitative and quantitative data collection and analysis procedures was described. Based on the recommendations of Heyvaert et al. [43], the methodological quality of mixed methods studies was appraised using the EPHPP tool for the quantitative part of the study, the quality criteria by Walsh and Downe for the qualitative part of the study, and the mixed methods criteria by Creswell and Plano Clark to evaluate the integration of both parts [44]. The latter consists of four criteria that evaluate whether: (1) the collection and analysis of quantitative and qualitative data were rigorous, (2) the integration of both data types was included in the results section, (3) the mixed methods research design was chosen logically, and (4) the mixed methods design was surrounded by theory and philosophy. Each of the four criteria was rated (i.e., criterion met, criterion partly met, or criterion met). Points were assigned for each rating (i.e., criterion met = 1 point, criterion partly met = 0.5 points, criterion unmet = 0 points), leading to an overall rating of the methodological quality with a maximum of 4 points.
3. Results
3.1. Study Selection
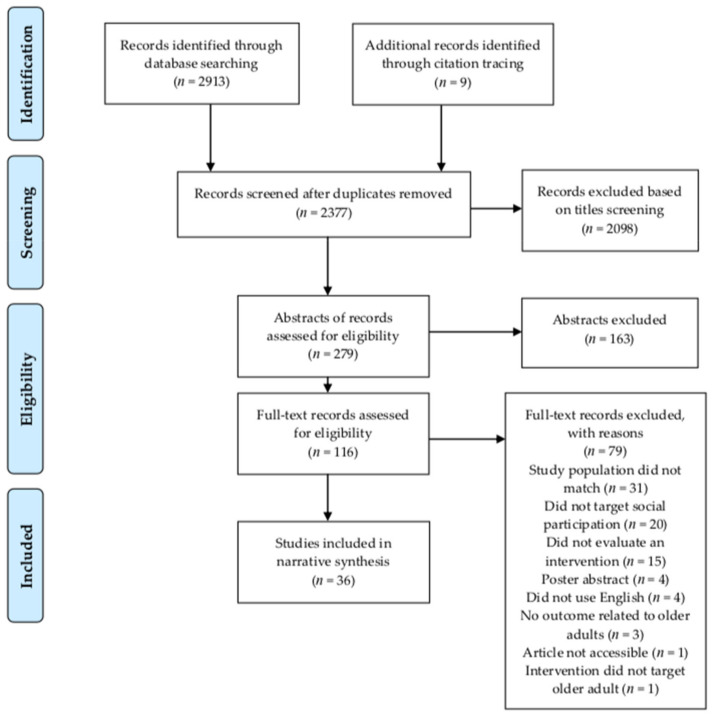
Figure 1 visualizes the study selection process based on the PRISMA guidelines [36]. The database search yielded 2913 records. After title and abstract screening, 79 of the 107 screened full-text records were excluded based on various reasons (see Figure 1). Next to the database search, 9 additional full-text records were identified through citation tracing. Two reports of the same study were identified and treated as one single study. As such, a total of 37 reports, covering 36 studies, met all of the inclusion criteria and were subsequently included in this systematic review.
Figure 1.
Study selection flowchart based on PRISMA guidelines.
3.2. Characteristics of Examined Studies
3.2.1. General Study Characteristics
Studies were published between 2005 and 2020. While 12 studies were published before or in the year 2015 [45,46,47,48,49,50,51,52,53,54,55,56], 24 studies were published after the year 2015 [57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80]. Studies were conducted in 11 different countries, with most of them being conducted in the USA . The majority of the included studies used a qualitative study design [45,47,48,49,57,59,60,61,62,66,68,69,75,76]. Of the remaining studies, 12 were of quantitative nature [46,52,55,56,63,65,67,71,73,74,78,80], and 10 studies were considered as mixed methods studies [50,51,53,54,58,64,70,72,77,79].
3.2.2. Study Population Characteristics
Sample sizes ranged from 5 [57] to 300 [63], with a majority of the participants being female. While most studies targeted older adults in general (with and without cognitive impairment), one third of the studies excluded older adults with cognitive impairment. Only three of the included studies evaluated the effect of technology on older adults with dementia: two qualitative studies [62,76] and one quantitative [78]. Next to that, one study focused on low-income older adults [69]. Several studies additionally evaluated the perceptions of other stakeholders: informal caregivers [48,76,78], family members [49,79], friends [79], volunteers [57,68] service coordinators [57], and young adult mentors [59].
3.2.3. Intervention Characteristics
Studies were heterogenous in terms of intervention characteristics. A third of the included studies focused on communication and social networking technology [45,46,47,49,51,54,57,61,66,68,73,79], and 10 evaluated ICT training programs [55,56,58,59,60,64,69,70,72,74]. Interestingly, the more recently published studies that evaluated these ICT training programs incorporated the concept of “reverse mentoring” [59,70,72]. Within this concept, young adults or students act as mentors and training instructors for older adult participants. Few studies addressed mobile applications [65,67,78,80] and gaming technology [52,62,75,76]. The remaining studies examined the effect of: activity-based musical engagement with iPads [50], a tablet-based language training program [77], the provision of Internet access [53], technology-assisted self-monitoring of physical activity [71], a Personal Reminder Information and Social Management (PRISM) system [63], and telecare [48].
In addition to the various types of technological interventions, the modality and aim of technological interventions varied as well. While 22 technologies included some kind of face-to-face contact, 14 technologies were fully virtual in nature [46,48,49,51,53,54,57,61,63,65,66,68,75,79]. Only 2 of the 36 included studies highlighted a explicit primary intervention aim to increase social participation [64,67]. Nonetheless, numerous studies mentioned addressing other social outcomes, such as social isolation and loneliness [47,51,54,56,57,65,70,71,72,74,75,79]. Although some of the remaining studies stated non-social intervention aims, such as improving cognitive function or increasing comfort with technology, more than half of them did not explicitly state an intervention aim at all [45,49,50,52,53,55,58,59,60,61,62,63,66,68,77].
3.3. Outcomes Related to Social Participation
Different variables were used to assess the effects of technological interventions on social participation outcomes. Loneliness was the most frequently measured psychosocial outcome identified in quantitative and mixed methods studies [46,51,52,54,55,56,63,65,67,70,72,73,74,77,80], followed by perceived social support [56,63,73,74,80] and social isolation [50,63,70,74]. Interestingly, the variables of loneliness, social isolation, and (perceived) social support were not measured coherently. While most of the studies measured loneliness as a distinct variable, Lee and Kim measured loneliness together with perceived social support as part of the concept of social isolation [70]. Slegers, van Boxtel, and Jolles assessed loneliness combined with the frequency and nature of the participants’ social network to evaluate the concept “social well-being” [55].
Less frequently measured outcomes included social network size [63], social integration [73], social connectedness [53,79], and social interaction [71,78]. Only one study explicitly stated social participation as quantitative outcome of interest [64]. Emas et al. used self-developed scales to assess social participation, defined in their study as the participants’ skill ability and confidence level in iPhone/iPad use. While the majority of included studies assessed the psychosocial outcomes at pretest and posttest, four studies assessed the outcomes one to three months after the intervention [51,56,72,74].
3.4. Quality Assessment
There was substantial agreement (κ = 0.699) between the two reviewers for the quality appraisal of quantitative studies before consensus was reached on the final rating [39]. Three quantitative studies were rated as strong [55,63,78]; three were rated as moderate [71,73,80]; and six were rated as weak [46,52,56,65,67,74]. From the data in Table 2, it is apparent that the quality of most study designs was strong. Eight of the quantitative studies were at first considered as Randomized Controlled Trials (RCTs) [46,52,55,56,63,71,78,80]. However, three studies did not describe the randomization procedure in their study methodology [46,52,56]. According to the EPHPP guidelines, these studies were classified as Clinical Controlled Trials (CCTs). One additional study was classified as a CCT because the randomized allocation of study participants conflicted with participants’ availability. The remaining quantitative studies were classified as single-group cohort studies [65,67,74].
Table 2.
Quality appraisal of quantitative studies (EPHPP) .
| Study | Selection Bias | Study Design | Confounders | Blinding | Data Collection Methods | Withdrawals and Drop-Outs | Global Rating |
|---|---|---|---|---|---|---|---|
| [78] | 2 | 1 | 1 | 2 | 1 | 1 | 1 |
| [55] | 2 | 1 | 1 | 3 | 1 | 1 | 1 |
| [63] | 2 | 1 | 1 | 2 | 1 | 2 | 1 |
| [71] | 3 | 1 | 1 | 2 | 1 | 1 | 2 |
| [73] | 3 | 1 | 1 | 2 | 1 | 1 | 2 |
| [80] | 3 | 1 | 1 | 2 | 1 | 1 | 2 |
| [46] | 2 | 1 | 3 | 3 | 1 | 1 | 3 |
| [56] | 3 | 1 | 1 | 3 | 3 | 2 | 3 |
| [52] | 3 | 1 | 3 | 3 | 3 | 1 | 3 |
| [67] | 3 | 2 | 3 | 3 | 3 | 1 | 3 |
| [74] | 3 | 2 | 3 | 3 | 1 | 3 | 3 |
| [65] | 3 | 3 | 3 | 3 | 3 | 1 | 3 |
Notes: 1 = strong, 2 = moderate, 3 = weak. Studies are named according to their reference number within this systematic review.
Several study aspects led to a lower methodological quality rating among quantitative studies. Overall, these studies were subjected to a high chance of selection bias. Only one study had a likely representative study sample [55]. Moreover, most included studies did not specify in most cases the percentage of selected individuals that agreed to participate in the study. In addition, several studies ( 6) did not mention about the blinding of outcome assessors.
For the methodological quality ratings of qualitative studies, a kappa coefficient (κ) of 0.415 was achieved, which indicated a moderate agreement between the two reviewers before consensus was reached on the final rating [39]. Table 3 shows a detailed overview of the individual criteria ratings and total ratings assigned for the methodological quality of included qualitative studies. The final ratings ranged from 5.5 [60] to 9 [66,76] out of 12. In general, included studies clearly stated their research aims or questions and were thoroughly contextualized by existing literature. However, a majority of the qualitative studies did not discuss the relationship between researcher and study participants nor the potential influence of researchers on the research process. Some studies did not provide a justification for the chosen sampling methods and the analytic approach used.
Table 3.
Quality appraisal of qualitative studies (Walsh and Downe criteria) .
| Criteria | [66] | [76] | [61] | [45] | [47] | [48] | [59] | [68] | [69] | [75] | [62] | [57] | [49] | [60] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clear statement of, and rationale for, research question/aims/purposes | + | + | + | + | + | + | + | + | + | + | + | ± | ± | ± |
| Study thoroughly contextualized by existing literature | + | + | ± | + | + | ± | + | + | + | + | + | + | + | + |
| Method/design apparent and consistent with research intent | + | ± | ± | ± | + | ± | ± | – | ± | – | ± | ± | ± | ± |
| Data collection strategy apparent and appropriate | ± | + | + | ± | + | + | ± | ± | ± | ± | ± | ± | ± | ± |
| Sample and sampling method appropriate | ± | ± | ± | ± | ± | ± | ± | + | ± | ± | ± | – | ± | ± |
| Analytic approach appropriate | ± | ± | ± | ± | – | ± | ± | ± | ± | ± | ± | ± | – | ± |
| Context described and taken account of in interpretation | + | + | ± | ± | ± | ± | ± | + | + | + | ± | ± | ± | ± |
| Clear audit trail given | ± | + | + | ± | ± | ± | ± | ± | ± | ± | ± | ± | ± | – |
| Data used to support interpretation | + | ± | + | ± | ± | + | + | + | ± | + | + | + | ± | ± |
| Researcher reflexivity demonstrated | – | ± | – | ± | + | ± | – | – | – | – | – | – | ± | – |
| Demonstration of sensitivity to ethical concerns | + | ± | ± | ± | – | ± | ± | – | ± | ± | ± | ± | ± | ± |
| Relevance and transferability evident | + | + | + | + | ± | ± | + | + | + | + | ± | + | ± | ± |
| Total score | 9 | 9 | 8 | 7.5 | 7.5 | 7.5 | 7.5 | 7.5 | 7.5 | 7.5 | 7 | 6.5 | 6 | 5.5 |
Notes: +, criterion met (=1 point), ±, criterion partly met (=0.5 points), –, criterion unmet (=0 points). By adding up the points, a total score of the methodological quality with a maximum of 12 points was determined. Studies are named according to their reference number within this systematic review.
The kappa coefficient (κ) for the quality assessment of mixed methods studies equaled 0.617, which indicated a substantial agreement between the two reviewers before consensus was reached on the final rating [39]. The methodological quality ratings of mixed methods studies are displayed in Table 4. What stands out in the table is that both the quantitative and mixed methods final ratings indicate a weak methodological quality. None of the studies framed the mixed methods procedures within theory and philosophy. Moreover, most mixed methods studies did not integrate the qualitative and quantitative data strands. The qualitative final ratings ranged from 4 to 9 out of 12. Only a limited number of mixed methods studies discussed choices and procedures concerning qualitative sampling, data collection, and analysis in detail.
Table 4.
Quality appraisal of mixed methods studies (EPHPP, Walsh and Downe criteria, and Creswell and Plano Clark criteria) .
| Assessment Tools | Criteria | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EPHPP | Selection Bias | Study Design | Confounders | Blinding | Data Collection Methods | Withdrawals and Drop-Outs | Final Rating | |||||||
| [51] | 3 | 1 | 1 | 3 | 1 | 2 | 3 | |||||||
| [77] | 3 | 2 | 3 | 3 | 1 | 3 | 3 | |||||||
| [70] | 2 | 2 | 3 | 3 | 3 | 3 | 3 | |||||||
| [72] | 3 | 3 | 3 | 3 | 3 | 3 | 3 | |||||||
| [50] | 3 | 1 | 3 | 3 | 1 | 1 | 3 | |||||||
| [79] | 3 | 2 | 3 | 3 | 3 | 1 | 3 | |||||||
| [58] | 2 | 2 | 3 | 3 | 3 | 3 | 3 | |||||||
| [53] | 3 | 2 | 3 | 3 | 1 | 2 | 3 | |||||||
| [54] | 3 | 2 | 3 | 3 | 3 | 3 | 3 | |||||||
| [64] | 3 | 2 | 3 | 3 | 3 | 3 | 3 | |||||||
|
Qualitative
criteria |
Study purpose | Study scope | Study Design | Data collection | Sampling strategy | Analysis | Study context | Audit trail | Data to support interpretation | Reflexivity | Ethical dimensions | Transferability | Final rating | |
| [51] | + | ± | ± | + | ± | ± | + | + | ± | ± | + | + | 9 | |
| [77] | + | ± | ± | + | ± | ± | ± | ± | + | – | ± | ± | 7 | |
| [70] | ± | ± | – | ± | ± | ± | + | ± | + | – | ± | + | 6.5 | |
| [72] | + | + | ± | ± | ± | ± | ± | ± | – | – | ± | ± | 6 | |
| [50] | + | ± | – | ± | ± | ± | – | ± | ± | ± | ± | ± | 5.5 | |
| [79] | + | + | ± | ± | ± | – | ± | ± | ± | – | – | ± | 5.5 | |
| [58] | + | ± | – | ± | ± | ± | ± | – | ± | – | ± | ± | 5 | |
| [53] | + | + | ± | ± | – | – | – | – | ± | – | ± | ± | 4.5 | |
| [54] | + | + | – | ± | ± | – | ± | – | – | – | ± | ± | 4.5 | |
| [64] | + | ± | – | ± | ± | – | ± | – | ± | – | – | ± | 4 | |
| Mixed methods criteria | Frames the procedures within theory and philosophy | Organizes the procedures into specific research designs | Collects and analyses both qualitative and quantitative data rigorously | Intentionally integrates the two data strands | Final rating | |||||||||
| [51] | – | ± | ± | – | 1 | |||||||||
| [77] | – | ± | + | – | 1.5 | |||||||||
| [70] | – | ± | ± | – | 1 | |||||||||
| [72] | – | ± | ± | – | 1 | |||||||||
| [50] | – | ± | ± | ± | 1.5 | |||||||||
| [79] | – | – | ± | ± | 1 | |||||||||
| [58] | – | ± | ± | – | 1 | |||||||||
| [53] | – | ± | ± | ± | 1.5 | |||||||||
| [54] | – | ± | ± | – | 1 | |||||||||
| [64] | – | ± | ± | – | 1 | |||||||||
Notes: EPHPP: 1 = strong, 2 = moderate, 3 = weak; Qualitative criteria: +, criterion met (=1point); ±, criterion partly met (=0.5 points); –, criterion unmet (=0 points). By adding up the points, a total score of the methodological quality with a maximum of 12 points was determined; Mixed methods criteria: +, criterion met (=1point); ±, criterion partly met (=0.5 points); –, criterion unmet (=0 points). By adding up the points, a total score of the methodological quality with a maximum of 4 points was determined. Studies are named according to their reference number within this systematic review.
3.5. Effects of Interventions on Social Participation
3.5.1. Quantitative Findings
Table 5 synthesizes the findings of each included quantitative study, listed in descending order based on their methodological quality. Very few of the quantitative studies found statistically significant effects on social participation outcomes. Only one quantitative study could be identified that addressed exclusively community-dwelling older adults with dementia [78].
Table 5.
Design, methods, and findings related to social participation reported from included quantitative studies.
| Authors (Year), Country | Study Design 1 | Experimental Intervention | Control or Comparison Intervention | Setting | Participants ( = Sample Size) | Outcomes Related to Social Participation | Outcome Measures Related to Social Participation | Findings Related to Social Participation |
|---|---|---|---|---|---|---|---|---|
| Yu et al. (2019) [78], USA | RCT 2 | Mobile reminiscing therapy app “Memory Matters”: one-on-one 30 min sessions with an interventionist (2×/week) for 6 weeks followed by independent use for 6 weeks | Comparison: group 30 min sessions with an interventionist (2×/week) followed by group 30 min sessions with an activity director. Control: waitlist. | Older adults’ residence | Older adults with dementia and caregivers | Social Interaction (pretest, 6 weeks, posttest) | Pleasant Events Schedule-AD (PES-AD short version) | 6 weeks: significant higher social interaction of the individual MM group vs. the comparison and the control group . 12 weeks: not maintained. |
| Slegers, van Boxtel, and Jolles (2008) [55], the Netherlands | CCT 3 | Computer training program: 3 × 4 hr training sessions for 2 weeks, independent use of the computer combined with assignments (1×/2 weeks in the first 4 months, 1×/month for the last 8 months) | Comparison: 3 × 4 h training sessions for 2 weeks, followed by independent computer use. Control: No intervention. | Home-based (setting of training sessions not mentioned) | Older adults without cognitive impairments | Social well-being (pretest, 4 months, posttest) | De Jong Gierveld Loneliness Scale, self-reported nature, and frequency of social network | No significant positive (or negative) intervention effect on social well-being. |
| Czaja et al. (2018) [63], USA | CCT | Personal Reminder Information and Social Management (PRISM) system: use of the computer system for 12 months | Comparison: use of a notebook with printed content (similar to PRISM) for 12 months. | Home- based | Older adults without cognitive impairments | Social isolation, loneliness, perceived social support, and social network size (pretest, 6 months, posttest) | Friendship Scale, UCLA Loneliness Scale, Interpersonal Support Evaluation List, and Lubben Social Network Index | 6 months: significant decrease in loneliness and increase in perceived social support of the PRISM group vs. comparison group. 12 months: not maintained. |
| Matz-Costa et al. (2018) [71], USA | RCT | Engaged4Life program: (1) technology-assisted self-monitoring of physical activity for 8 weeks, (2) 3 hr psycho-education group session, (3) phone calls by peer mentors for 2.5 weeks (2×/week) | Comparison: technology-assisted self-monitoring of physical activity for 8 weeks. | Home- based | Older adults without cognitive impairments | Social interaction (pretest within first week, week 4) | Survey related to the quantity and quality of social interaction | No significant changes in social interaction of the intervention group vs. comparison group. |
| Myhre, Mehl, and Glisky (2017) [73], USA | CCT | Facebook: 2 hr training sessions for 1 week (3×/week), use of Facebook (1×/day) and writing posts (1×/week) for 7 weeks | Comparison: online diary website. 2 hr training sessions for 1 week (3×/week), use of diary website (1×/day) and writing data entries (1×/week) for 7 weeks. Control: waitlist. | Home-based combined with training sessions at computer lab classrooms | Older adults without cognitive impairments | Loneliness, social support, and social integration (pretest, posttest) | UCLA Loneliness Scale, Medical Outcomes Study Social Support Survey, Lubben Social Network Scale, and Social Provisions Scale | No significant differences in social support, loneliness, and social integration (pretest vs. posttest) in any of the groups. |
| Vanoh et al. (2019) [80], Malaysia | RCT | WESIHAT 2.0© (https://creativecommons.org/licenses/by-nc/3.0/, accessed on 14 April 2021) web-based wellness application: use of the application for 6 months, 30 min/day (4×/week) in combination with group counselling sessions in the first 3 months | Use of a health education pamphlet containing dietary recommendations for 6 months, in combination with dietary counselling. | Home-based combined with counselling sessions at a community hall | Older adults without cognitive impairment | Loneliness and social support (pretest, 3 months, posttest) | Three-item loneliness scale and Medical Outcome Social Support Survey (MOSS) | Significant interaction effect for informational support and tangible support . No statistically significant interaction effects for loneliness and other dimensions of social support. |
| Bickmore et al. (2005) [46], USA | CCT | Embodied Conversational Agent (ECA) “FitTrack”: daily interaction with the relational agent (who acted as an exercise advisor) for 2 months | Comparison: physical activity intervention for 2 months. | Home- based | Older adults without cognitive impairments | Loneliness (pretest, posttest) | R-UCLA Loneliness Scale | Loneliness decreased statistically significant in the control group , not in the intervention group. No significant group differences. |
| Woodward et al. (2011) [56], USA | CCT | Computer/Internet training program: 11 training sessions in a group delivered by the project coordinator for 6 months (1×/2weeks) | Control: no intervention. | Computer lab | Older adults | Social support and loneliness (pretest, 3 months, posttest, 3 months following the training) | Self-reported social network data, Multidimensional Scale of Perceived Social Support (MSPSS), De Jong Gierveld Loneliness Scale | No statistically significant differences in social support and loneliness between the groups. Trend of higher perceived social support in intervention group vs. control group. |
| Kahlbaugh et al. (2011) [52], USA | CCT | Playing Wii: 1 hr activity with an undergraduate student for 10 weeks (1×/week) | Comparison: 1 hr watching television with an undergraduate student for 10 weeks (1×/week). Control: no visit. | Home- based | Older adults | Loneliness (pretest, posttest) | UCLA Loneliness Scale | Significant decrease in loneliness from pretest to posttest in intervention group , increase in loneliness in comparison group. |
| Jansen- Kosterink et al. (2020) [67], the Netherlands | Cohort | Mobile application “GezelschApp” that stimulates users to engage in local activities together with other users: use of the application for 3 months combined with tailor-made coaching by a social worker | NA 4 | Home- based | Older adults | Loneliness (pretest, posttest) | De Jong Gierveld Loneliness Scale | Loneliness decreased among study participants (pretest vs. posttest). Not statistically significant. |
| Neil-Sztramko et al. (2020) [74], Canada | Cohort | iPad training program “AGE-ON”: 2 h education sessions (1×/week) for 6 weeks and use of the iPad/Internet at home | NA | Home-based (setting of training sessions not mentioned) | Older adults | Social isolation and loneliness (pretest, posttest), social support (pretest, posttest, 1 month following the program) | Duke Social Support Index (DSSI), De Jong Gierveld Loneliness Scale, Lubben Social Network Scale | No significant differences in any social outcome measures. |
| Goumopoulos, Papa, and Stavrianos (2017) [65], Greece | One group mid- and posttest | Tablet-based intervention “Senior App Suite”: use of the mobile application suite for 8 weeks | NA | Home- based | Older adults without cognitive impairments | Loneliness (pretest, posttest) | R-UCLA Loneliness Scale | “Senior App Suite” may reduce loneliness moderately . |
1 Study design as classified by the quality assessment (EPHPP). 2 RCT = randomized controlled trial. 3 CCT = clinical controlled trial. 4 NA = not applicable.
Three quantitative studies with a strong methodological quality rating did not find significant group differences at post-intervention follow-up. In the study by Slegers, van Boxtel, and Jolles [55], no significant intervention effect on social well-being or any other dimension of well-being could be identified. In contrast, in the study by Czaja et al. [63], significant changes between the two groups in the domains of loneliness and perceived social support were identified at mid-term follow-up. In addition, a decrease in social isolation could be found. Similarly, in the RCT by Yu et al. [78], outcomes related to social participation significantly improved at mid-term follow-up. While there were no significant differences between the three group in the primary outcome “mood”, there was a significant higher social interaction in the intervention group compared with the control and comparison group at 6 weeks. However, the significant group differences at mid-term follow-up reported in these two latter studies could not be maintained at post-intervention follow-up [63,78].
Six of the remaining nine quantitative studies failed to demonstrate statistically significant intervention effects on social participation outcomes in the intervention group [46,56,67,71,73,74]. It has to be noted that a majority of these studies were feasibility trials [46,67,71,74]. Two technological interventions did not focus on outcomes related to social participation as a primary aim [71,73]. Both studies found statistically significant effects on their primary outcomes of interest: physical activity [71] and cognitive function [73]. Of the three quantitative studies that reported statistically significant changes in social participation outcomes, two reported a significant decrease in loneliness among older adults [52,65]. Moreover, one study found a significant interaction effect for informational and tangible support [80].
3.5.2. Qualitative Findings
Synthesized information about the intervention, design, and main findings of included qualitative studies can be found in Table 6, sorted in descending order based on the studies’ quality assessment rating. Qualitative studies reported various benefits of technological interventions on the social participation of older adults. These benefits included: (1) maintenance or development of social relationships or connections [47,48,57,59,66,68,69], (2) improvements in social connectedness [49,60], (3) decrease in loneliness [45,57], (4) companionship and social interaction [61], and (5) improvements in communication [68]. In addition, study participants reported benefits of technological interventions in terms of life satisfaction [60], ICT skills [47], confidence in the use of technology [59], or physical activity [61]. Only two qualitative studies focused on community-dwelling older adults with dementia [62,76].
Table 6.
Methods and main findings reported from included qualitative studies.
| Authors (Year), Country | Technological Intervention | Setting | Participants ( Sample Size) | Data Collection Methods | Main Findings |
|---|---|---|---|---|---|
| Hemberg and Fischer (2018) [66], Finland | Real video communication “CaringTV” | Home-based | Older adults |
Interviews | Overarching theme: “Being in a movement toward becoming a unity as human being” [66] (p. 93). Technology facilitated making new experiences, dedicating new meaning to everyday life, and maintaining or developing social contacts/relationships. Welfare technology as: “a window toward the world” [66] (p. 93). |
| Unbehaun et al. (2018) [76], Germany | Exergames program: regular use of the system combined with visits of trained research assistants 2×/week for 8 months | 3 domestic environments and 4 day-care centers | Older adults with dementia and caregivers | Semi-structured interviews and ongoing evaluation of the prototype | Benefits for people with dementia: enhanced physical skills, increased motivation, showed learning effects, increased social interaction and sense of interpersonal relationships (in day-care home setting), improved daily life routine. Benefits for caregivers: relief for caregivers (e.g., freeing up time). |
| Chi et al. (2017) [61], USA | Digital pet avatar: daily interaction with a conversational agent (a cat or dog avatar) for 3 months | Home-based | Older adults without cognitive impairment | Secondary analysis of semi-structured interviews | Benefits: provided companionship, reminders, a journal, entertainment, increased social interaction and physical activity. System challenges: technical issues and the limited ability to make conversations. Major concerns: privacy, costs, and dependence. |
| Ballantyne et al. (2010) [45], Australia | Internet Social Networking Website (ISNW) “About My Age”: one-on-one education sessions delivered by project team members for 3 months (in the beginning, weekly support visits, then less frequently) | Home-based | Older adults |
Semi-structured interviews and reflective journals of the project team | Benefits: enabled exploration of other ways of communication, contributed to a positive and personalised learning experience (using the one-on-one approach), reduced temporal loneliness (extent varied per case), increased sense of connectivity to the outside world to some extent. |
| Biniok and Menke (2015) [47], Germany | Tablet with communication platform “SONIA”: training sessions in groups delivered by researchers and volunteers and use of the platform for 6 months | Home-based combined with training sessions at a university/community college | Older adults |
Group discussions and observations | ICT created, extended, and facilitated engagement in participation space: Participants with few social contacts: enhanced technological skills, increased self-esteem, and increased social participation. Socially active participants: growth and intensification of social contacts/interactions. Some participants (mostly with high technological skills): only slight changes in social participation. |
| Bowes and McColgan (2012) [48], UK |
Telecare | Home-based | Older adults and family caregivers | Semi-structured interviews | Independence: promoted participants’ confidence, feelings of safety, and freedom. Social Participation: enabled living in the community, enhanced relationships, but led to restriction in activities formerly enjoyed and narrowing of social networks. Identity: contributed to a positive sense of identity. |
| Breck, Dennis, and Leedahl (2018) [59], USA |
Cyber-Seniors Program: technology training lessons delivered by young adult mentors using reverse mentoring 1×/week | Senior center and other locations | Older adults and young adult mentors |
Session logs of young adult mentors and surveys | Benefits for older adults: gained confidence in the use of technology to make social connections digitally. Benefits for young adult mentors: enhanced leadership skills. Both: Age-related stereotypes were challenged. Intergenerational engagement and connections emerged. |
| Judges et al. (2017) [68], Canada |
Digital communication tool “InTouch”: social contact using the system with a paired volunteer 1×/week for 3 months | Home-based | Older adults and volunteer participants |
Semi-structured interviews, field notes of volunteer participants and the study coordinator, and data logs | Benefits: improved communication and positive changes in relationships. Use of technology led to mixed feelings in study participants. Adoption: 4 of the study participants were able to adopt “InTouch”. Internal motivation contributed to successful adoption. Key barriers to adoption: lack of volunteer support, social difficulties, and diverse health issues. |
| Kim and Gray (2016) [69], USA |
Computer training program: use of computer and 1 h training sessions of computer/Internet skills (1×/week) | Home-based combined with training sessions at senior housing facilities | Low-income older adults | Semi-structured interviews and interviewer’s field notes | Benefits: enhanced social connections, monetary benefits, and development of life skills. Barriers to program participation: fear of technology, low literacy, and distrust of governmental programs. Barriers to sustained Internet use: problems and costs of broadband services, concerns about cyber security, and limited proficiency. Success factors to sustained Internet use: ongoing technical support and individual ICT devices. |
| O’Brien, Smith, and Beck (2016) [75], USA | 3D virtual world “Second Life” (SL): training/onboarding for two weeks, SL events organized by trained staff for 8 weeks, independent use of SL for 2 weeks | Home-based | Older adults |
Semi-structured interviews | Older adults reported to be open to the possibility of creating online relationships within the virtual world. Most of the participants did not succeed in creating them. Obstacles to the formation of online relationships: personality, difficulties with other avatars, and lack of face-to-face interactions. |
| Cutler, Hicks, and Innes (2015) [62], UK | Digital gaming training program: 2 h training sessions (“Tech Clubs”) in groups delivered by facilitators for 6–8 weeks | Home-based combined with training sessions at 4 different venues | Older adults with dementia | Ethnographic field notes, self-complete questionnaires, and focus groups | Impact of digital gaming on healthy aging: promoted lifelong learning; increased physical activity, social interaction, and mental stimulation; and promoted independence. |
| Airola, Rasi, and Outila (2020) [57], Finland | Phone and video conferencing (VC) service: calls from a volunteer 1×/week | Home-based | VC service coordinator, volunteers, and older adult service users | Semi-structured interviews | Barriers to learning and using the service: technical problems, volunteer–user relationship, lack of technical skills, health status, and a negative attitude toward technology. Enablers to learning and using the service: technical support, social support networks, previous experience with technology, and a positive attitude toward new technologies. Benefits: facilitated to establish networks and reduce loneliness. |
| Cornejo, Tentori, and Favela (2013) [49], Mexico | Ambient Social Network System “Tlatoque”: use of an interactive display for 21 weeks | Home-based | Older adults and family members |
Semi-structured interviews and a focus group | Tlatoque supported social connectedness through: a higher frequency of social contacts (consensual meetings or opportunistic encounters around the system). the strengthening of social ties between the older adult and family members. |
| Burmeister et al. (2016) [60], USA |
iPad training program: 2 h training sessions in groups delivered by a peer trainer 1×/week for 4 months | Home-based combined with training sessions at a Seniors Citizen’s Club | Older adults |
Interviews, participants’ diaries, researchers’ observations, and peer trainer’s reports | Benefits: enhanced ICT skills, increased social connectedness, and improved life satisfaction. Important factors: individualized education approach and social connections between participants and peer trainer. |
3.5.3. Mixed Methods Findings
A summary of findings from mixed methods studies is detailed in Table 7. Less than half of the studies revealed significant intervention effects on social participation outcomes. One study found a significant increase in social participation among older adult participants [64]. In this study, social participation was measured as the participants’ skills ability and confidence level in several ICT-related tasks. Furthermore, three studies reported a statistically significant decrease in loneliness [54,70,72]. In addition to this, Lee and Kim [70] also found a decrease in total social isolation. The remaining six mixed methods studies did not find any statistically significant intervention effects on social participation outcomes [50,51,53,58,77,79]. All of them were carried out with small sample sizes and five of them were described as pilot studies [50,51,53,58,77,79].
Table 7.
Design, methods, and findings related to social participation reported from included mixed methods studies.
| Authors (Year), Country |
Experimental Intervention | Setting | Participants ( Sample Size) | Outcomes Related to Social Participation | Quantitative Outcome Measures Related to Social Participation |
Qualitative Data Collection Methods | Findings Related to Social Participation |
|---|---|---|---|---|---|---|---|
| Hind et al. (2014) [51], UK | One-on-one telephone friendship (TF) vs. usual care control: (1) 10 to 20 min calls delivered by volunteer facilitators for six weeks (1×/week), followed by (2) 1 h TF groups for 12 weeks (1×/week) | Home-based | Older adults without cognitive impairments |
Loneliness (pretest, 6 months follow-up post randomization) |
De Jong Gierveld Loneliness Scale | Semi-structured interviews | Loneliness: no statistically significant improvement. Interviews: participant reported a lack of face-to-face contact and a dissatisfaction with group cohesion. |
| Ware et al. (2017) [77], France | Language training program: 2 h sessions of an English language training delivered by a native English-speaking psychologist using a tablet-based multimedia approach for 4 months (1×/week) | Laboratory of a hospital | Older adults without cognitive impairments | Loneliness (pretest, posttest) |
UCLA Loneliness Scale, and semi-structured interviews | Semi-structured interviews | Loneliness: no statistically significant improvement. Interviews: participants reported that they did not build strong social ties with other group participants. |
| Lee and Kim (2018) [70], USA | Intergenerational Mentor-Up (IMU) class: six 1 h one-on-one technology tutorial sessions delivered by college students (partly in groups) | Senior centers and housing facilities | Older adults without cognitive impairments | Social isolation (pretest, posttest) |
Perceived social isolation measure (loneliness and social support) and self-reported life stressors checklist | Interviews and researchers’ field notes | Total social isolation significantly decreased , with no significant change in lack of social support and a statistically significant decrease in loneliness . |
| Mullins et al. (2020) [72], USA | Internet Information Station program: three different computer classes delivered by students | Four apartment buildings of a Housing and Urban Development community | Older adults participating in program Older adults filling in the R-UCLA Loneliness Scale |
Loneliness (pretest, posttest at 4–6 weeks after the program) |
R-UCLA Loneliness Scale | Ethnographic interviews and observations | Participants reported enhanced social connectedness. Observed increase in participation in the common areas of the Housing and Urban Development community. Decrease in loneliness of the technology class group (vs. baseline group): significant change on the item “There is no one I can turn to”. |
| Engelbrecht a nd Shoemark (2015) [50], Australia | Activity-based musical engagement using iPads vs. Traditional Music Instruments (TMI): 1 h sessions of activity-based musical engagement in groups delivered by a therapist for 5 weeks (1×/week) | Not mentioned | Older adults without cognitive impairments | Social isolation (pretest, posttest) |
Friendship scale | Journal entries, researcher’s field notes, and session reflections | No significant differences in social isolation (1) between the iPad and the TMI group and (2) within the groups (pre- vs. posttest). Reported benefits for both groups: enhanced positive self-concepts and developed social cohesion and group identity. |
| Zaine et al. (2019) [79], UK and Brazil | Human-facilitated social networking system “Media Parcels”: use of the tablet-based system facilitated by a clinical psychologist for two weeks with family members (trial 1) or friends (trial 2) | Home-based | Older adults , family members , and older adult friends | Feelings of social connection (pretest, week 1, posttest) |
Self-developed Relationship Semantic Differential Scale (RSDS) | Interviews | Participants reported contacting each other more often and feeling closer to each other. |
| Arthanat, Vroman, and Lysack (2016) [58], USA | iPad training program: individualized one-on-one training sessions delivered by a coach (occupational therapy student) for 3 months (1×/month), then iPad use without assistance for 3 months | Home-based | Older adults without cognitive impairments |
Breadth and frequency of technology use related to social connections (pretest, 1 month, 2 months, 3 months, 4 months, posttest) | Self-developed questionnaire 1 | Field observations, self-developed end-of-study questionnaire, and focus groups | Modest (not significant) increase in activities involving social connections. Participants identified benefits and challenges of the program related to technology experiences, interactions with the coach, the training approach, and specific activities. |
| Mellor, Firth, and Moore (2008) [53], Australia | Providing internet access: use of computer/Internet for 12 months (with support on a daily basis for the first two weeks) | Retirement villages | Older adults | Social connectedness (pretest, 3 months, 6 months, 9 months, posttest) | Social Connectedness Scale | Semi-structured interviews | At 12 months: no significant differences in social connectedness. Benefits reported in interviews: positive impact on social connectedness. |
| Ring et al. (2015) [54], USA | ECA 2 motion sensor vs. non-sensor condition: interact with the ECA on a touchscreen computer (1×/day) for 1 week | Home-based | Older adults | Loneliness (pretest, posttest) |
UCLA Loneliness Scale | Diary entries and semi-structured interviews | Significant lower loneliness in intervention group vs. comparison group when interacting with the ECA . This indicates that the ECA is more effective in reducing loneliness when using a motion sensor to actively initiate social interactions with older adults. |
| Emas et al. (2018) [64], USA | iPad/iPhone training program: 1 h multimodal training sessions in groups 1×/week for 7 weeks | Home-based combined with training sessions at a gated retirement community | Older adults | Participants’ skill ability (PSA); participants’ confidence level (PCL) (pretest, posttest) |
Self-developed scales measuring PSA and PCL | Journaling prompts | Statistically significant increase in PSA of defining several Internet acronyms and statistically significant increase in PCL using FaceTime , and taking photos . Facilitation of social participation: participants reported to have gained skills and knowledge in communicating with loved ones using concepts such as FaceTime, texts, e-mails, and phone calls. |
1 Only two of the four categories of ICT activities were relevant: family connections and social connections. 2 ECA = embodied conversational agent.
Based on qualitative findings, study participants reported overall positive effects on social participation, such as enhanced social connectedness [53,72] and enhanced ICT skills that facilitated the communication with loved ones [64]. While one study found that participants in a group intervention developed social cohesion and group identity [50], two other studies found that participants in group intervention programs had a lack of group cohesion and social ties [51,77].
4. Discussion
This systematic review is, to our knowledge, the first to assess the potential of technological interventions in enhancing the social participation of community-dwelling older adults, including people with dementia. The primary aim of this review was to provide a comprehensive overview of technology that has been studied and used to address social participation in this study population. In total, 36 studies were included. A variety of technological interventions were identified, most of them being communication and social networking technology and ICT training programs. These findings correspond with findings from other systematic reviews that looked at the use of technology to address social isolation among older adults in general [28,29,30]. Baker et al. [30], however, identified pet robots as another technology-based intervention. As pet robot evaluations are mostly conducted in institutional care settings, it is not surprising that none of the included studies evaluated pet robots in community settings [81].
Based on the recency of the studies, we note an apparent shift away from computer-based interventions to more tablet- and smartphone-based interventions. This may be due to a greater ease of access to tablets and smartphones as compared to computer-based solutions since the former options are usually incorporated into one’s everyday life. Despite the fact that tablet- and smartphone-based technologies are portable and non-location bound, most studies that used these technologies conducted the interventions in participants’ homes. However, prior studies have shown that the engagement in community-based out-of-home activities can contribute to the social participation of older adults [82,83]. Considering this, it is surprising that only one study used technology to facilitate social participation in the community, by encouraging older adults via the mobile application “GezelschApp” to physically engage in community-based activities with others [67]. This finding may be explained by the fact that most studies did not have an explicit focus on improving social participation. Instead, their focus was on reducing the negative consequences of social isolation. This highlights the empirical consequences of having a poorly defined concept of social participation.
4.1. Effects of Interventions on Social Participation
Overall, quantitative and mixed methods studies showed that the use of technological interventions had limited effects on loneliness, social isolation, and social support. This may be attributed to the fact that many studies were pilot studies with small sample sizes. Nevertheless, qualitative findings were able to identify various benefits, such as the development of social connections and the improvement of social connectedness. As expected, only limited studies addressing people with dementia could be identified [62,76,78]. Due to the heterogeneity of study and intervention characteristics and the limited number of studies that targeted older adults with dementia, no subgroup analyses could be carried out to evaluate whether the effects may differ between people with and without dementia. Based on the body of evidence that has been synthesized narratively, no conclusion can be drawn regarding the effectiveness of technological interventions for people with dementia. Consequently, the present findings suggest that technological interventions may have the potential to alleviate loneliness and enhance social support in cognitively healthy older adults. As the effects on loneliness and social support were inconsistent, findings have to be interpreted with caution.
Such inconsistent findings were also reported in other systematic reviews in similar fields. Although the effects of ICT on loneliness were inconclusive in the review by Chen and Schulz [29], ICT was found to positively affect social connectedness, social isolation, and social support. A majority of the studies included in the review by Khosravi et al. [30] found positive effects in reducing loneliness or social isolation. These inconsistent study findings may be due to the use of different inclusion criteria. Khosravi et al. [30] for example included exclusively quantitative study findings related to a younger age group (older adults aged 50+) living in institutional care or community settings. In contrast, the present systematic review focused on various research designs including older adults aged 55 years or older living in a community setting. Regarding the effectiveness of technology on the social participation of people with dementia, other systematic reviews also failed to identify a high number of studies with rigorous study designs [34,37].
Findings of the present systematic review suggest that social interaction, face-to-face contact, and intergenerational engagement may be successful elements of technological interventions in enhancing the social participation in community-dwelling older adults. All seven studies that found a statistically significant intervention effect included a social interaction element [52,54,64,65,70,72,80]. This finding is not surprising, as social participation in the present review was defined as a “person’s involvement in activities that provide interaction with others in society or the community” [23] (p. 2148). Moreover, it is noteworthy that five of the seven studies had the element of a face-to-face contact [52,64,70,72,80]. Interestingly, three studies that demonstrated significant changes contained the element of intergenerational engagement between older adult study participants and younger adult students [52,70,72]. Gardiner, Geldenhuys, and Gott [84] looked at elements that should be included in interventions to successfully address social isolation and/or loneliness in the aged population. Three categories were identified: adaptability, productive engagement, and the use of a community development approach. Engagement within a group to socialize and build social connections was part of the productive engagement category. Furthermore, ten Bruggencate, Luijkx, and Sturm [26] argued that an intervention is successful in enhancing the social well-being of older adults when targeting their social needs. Interestingly, all of the three facilitators of social participation identified in the present systematic review could be seen as a way to fulfill the social need of social connections and connectedness [26,33]. As a consequence, a question arises around whether the technology is an intermediary to fulfill this social need rather than the technology producing the effect.
A major finding from our study was the inconsistent use of terms and concepts related to social participation. Social participation is a multidimensional concept that comprises the dimensions of social connections, volunteering, and engaging with others in activities for personal enjoyment [23,85]. However, most of the included studies in the present systematic review measured only one specific dimension of social participation: the dimension of social connections. Likewise, other systematic reviews that looked into interventions for social isolation found that a majority of studies mainly assessed outcomes related to this dimension, such as loneliness and social support [29,86]. While social isolation and loneliness are distinct concepts, they are sometimes used interchangeably by researchers. As social isolation refers to an actual lack of social connections [21], the facilitation of social participation can be considered equal to the decrease of social isolation [28]. More importantly, an actual improvement and enrichment of social connections does not necessarily mean a decrease in loneliness, defined as the subjective feeling of lacking social connections [21]. Given these points, the comparability of study findings is limited.
4.2. Methodological Quality of Included Studies
Overall, the methodological quality of studies was inconsistent across study designs. It has to be noted that the EPHPP component ratings “blinding” and “confounders” of several studies were difficult to rate due to the lack of a control group. As the EPHPP dictionary did not provide recommendations on how this issue should be addressed, the first author standardized the process by rating these component ratings as weak. In addition, a high selection bias could be observed across quantitative and mixed methods studies because study participants were mainly self-referred. This selection bias might have implications for the findings of the present systematic review. As mentioned before, limited quantitative evidence was found regarding the effectiveness of technological interventions on social participation. An explanation might be that older adults who are contacted and willing to participate in a study are not socially isolated. This explanation can be supported by the included studies that reported a lack of study participants with a high degree of social isolation at baseline [50,73,74,75]. In addition, the study participants’ digital literacy, attitudes toward technology, and investment in learning how to use a certain technology may have led to biased study findings. This issue was not covered by the used quality assessment tools. However, some studies addressed this issue by evaluating attitudes toward technology, use of technology, or digital literacy prior to the intervention. Other studies addressed this issue by providing training sessions on how to use the technology or by including study participants based on their digital literacy.
4.3. Strengths and Limitations
The strength of this study lies in the systematicity of our approach. The systematic search strategy that combined free text words with Medical Subject Headings (MeSH), Thesaurus terms, and CINAHL Subject Headings ensured the inclusion of relevant studies from various scientific databases. Moreover, the continuous involvement of two independent researchers throughout the entire review process enhanced the rigor of the screening and quality appraisal process. Using three different quality assessment tools furthermore enabled a thorough quality appraisal of the included studies, regardless of their design.
A number of potential limitations need to be considered. Firstly, a publication bias might have occurred, as this review was restricted to published results. Furthermore, the search was limited to studies written in English and published in peer-reviewed journals. Hence, research findings published in other sources, such as trade journals, were excluded. As such, potentially relevant publications may have been missed. Nevertheless, measures were taken to ensure the comprehensiveness of our search: the use of citation tracing, the use of different search terms related to the concept of social participation, and the inclusion of database-specific subject headings. Despite this, the search terms used in this systematic review may not cover all relevant studies since researchers use different terms to refer to the multidimensional concept of social participation. Secondly, included studies might be falsely considered as mixed methods studies, even when the respective study authors did not intentionally use a mixed methods design. Consequently, the methodological quality of those studies may have been rated inappropriately. Lastly, this systematic review included studies with diverse research designs and inconsistent methodological quality. The generalizability of the review findings may as a result be limited. However, the diversity of study designs broadened the scope of this review, identifying various technological interventions that target the social participation of community-dwelling older adults.
4.4. Implications for Practice and Future Research Directions
The present findings have implications for targeting the growing health issue of social isolation in the aged population. Due to the COVID-19 pandemic, social interaction occurred mainly digitally during the past year. As a consequence, older adults living in the community were not only socially excluded from society but were also digitally excluded from society [87,88]. Based on the present review findings, technology could play a crucial role in addressing these consequences of COVID-19 in community-dwelling older adults by providing opportunities to maintain social connections and to socially participate in the community. Policy makers should therefore prioritize the need of older adults to socially participate in the community and provide technological services to address this need. To ensure that these services can successfully address social participation, they should incorporate a social interaction element and provide possibilities to engage in out-of-home activities. Moreover, designers of technological interventions that target social participation might incorporate social interaction elements into the intervention.
As new technological solutions emerge every year and the number of older adults experiencing social isolation grows rapidly, future studies need to be carried out to evaluate the impact of emerging technologies on social participation outcomes. To capture the complex nature of social participation, it would be of value for studies to collect both qualitative and quantitative data. Furthermore, there is a need for a consistent terminology. Researchers should consider identifying and clearly defining the concept of interest in their studies. Due to a lack of an outcome measure that covers diverse social participation dimensions, studies should combine several validated outcome measures to assess social participation. Future studies should consider developing and validating an outcome assessment that covers all dimensions of social participation. Different health care professionals, such as occupational therapists, could use the tool to tailor their intervention to the individual needs of older adults living in the community. As the purpose of social participation is to facilitate the involvement in activities in the community [23], more studies should look into using technology to facilitate the participation in out-of-home social activities. In order to evaluate the long-term effects of technological interventions on social participation, studies with larger sample sizes that focus on older adults with a high degree of social isolation are needed. In addition, researchers not only should look into the effects of technological interventions, but also should explore whether these effects are mediated rather than produced by the technology.
In this systematic review, a lack of studies that address community-dwelling older adults with dementia was identified. Therefore, an important aspect to explore in future studies is the potential of technological interventions to reduce the social isolation of this study population. Moreover, it is likely that factors other than the ones identified in this review play a role in facilitating the social participation of people with dementia. According to Dröes et al. [89], personal and disease-related factors, social environment factors, and physical environment factors can impede or enhance their social participation. Similarly, the findings of Gaber et al. [90] suggest that contextual factors, such as characteristics of the physical and social environment, need to be considered when enhancing the social participation of people living with dementia. Further research should focus on identifying factors of technological interventions that facilitate social participation in older adults and, particularly, in older adults with dementia.
5. Conclusions
Technological interventions have shown the potential to alleviate loneliness and social isolation and to enhance social support. In particular, technological interventions that contain the elements of social interaction, face-to-face contact, or social engagement seemed to be most effective. This review is a starting point for future research regarding the use of technology to facilitate social participation among older adults and to thereby reduce their (risk of) social isolation, especially in the context of dementia.
Acknowledgments
We thank Nicolette Siep of the Maastricht University Library for the assistance given during the development of the search strategy. We also thank Roos Roberts at the Alzheimer Centrum Limburg (Maastricht University) for the support given during the screening process.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm10112308/s1, Tables S1–S6: Specific survey see in supplementary materials.
Author Contributions
Conceptualization, P.H.; methodology, P.H., L.M.M.B., A.N. and F.R.J.V., and M.E.d.V.; validation, F.R.J.V. and M.E.d.V.; formal analysis, P.H.; investigation, P.H., L.M.M.B., and W.Q.K.; data curation, P.H., L.M.M.B., W.Q.K., A.N., F.R.J.V. and M.E.d.V.; writing—P.H.; writing—review and editing, L.M.M.B., W.Q.K., A.N., F.R.J.V. and M.E.d.V.; visualization, P.H.; supervision, F.R.J.V. and M.E.d.V. All authors have read and agreed to the published version of the manuscript.
Funding
The research presented in this paper was carried out as part of the Marie Curie Innovative Training Network (ITN) action, H2020-MSCA-ITN-2018, under grant agreement number 813196.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analysis, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.United Nations Department of Economic and Social Affairs World Population Ageing 2020 Highlights: Living Arrangements of Older Persons. [(accessed on 3 March 2021)]; Available online: https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/undesa_pd-2020_world_population_ageing_highlights.pdf.
- 2.WHO Dementia. Key Facts. [(accessed on 8 December 2020)]; Available online: https://www.who.int/news-room/fact-sheets/detail/dementia.
- 3.Freedman A., Nicolle J. Social isolation and loneliness: The new geriatric giants. Approach for primary care. Can. Fam. Physician. 2020;66:176–182. [PMC free article] [PubMed] [Google Scholar]
- 4.Nicholson N.R. A review of social isolation: An important but underassessed condition in older adults. J. Prim. Prev. 2012;33:137–152. doi: 10.1007/s10935-012-0271-2. [DOI] [PubMed] [Google Scholar]
- 5.European Union Loneliness—An Unequally Shared Burden in Europe*. [(accessed on 23 January 2021)]; Available online: https://ec.europa.eu/jrc/sites/jrcsh/files/fairness_pb2018_loneliness_jrc_i1.pdf.
- 6.Cudjoe T.K.M., Roth D.L., Szanton S.L., Wolff J.L., Boyd C.M., Thorpe R.J., Jr. The Epidemiology of Social Isolation: National Health and Aging Trends Study. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020;75:107–113. doi: 10.1093/geronb/gby037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Maurik I.S., Bakker E.D., van den Buuse S., Gillissen F., van de Beek M., Lemstra E., Mank A., van den Bosch K.A., van Leeuwenstijn M., Bouwman F.H., et al. Psychosocial Effects of Corona Measures on Patients With Dementia, Mild Cognitive Impairment and Subjective Cognitive Decline. Front. Psychiatry. 2020;11:1088. doi: 10.3389/fpsyt.2020.585686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cornwell E.Y., Waite L.J. Social Disconnectedness, Perceived Isolation, and Health among Older Adults. J. Health Soc. Behav. 2009;50:31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heikkinen R.-L., Kauppinen M. Depressive symptoms in late life: A 10-year follow-up. Arch. Gerontol. Geriatr. 2004;38:239–250. doi: 10.1016/j.archger.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 10.Holt-Lunstad J., Smith T.B., Baker M., Harris T., Stephenson D. Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Perspect. Psychol. Sci. 2015;10:227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- 11.O’Rourke H.M., Duggleby W., Fraser K.D., Jerke L. Factors that Affect Quality of Life from the Perspective of People with Dementia: A Metasynthesis. J. Am. Geriatr. Soc. 2015;63:24–38. doi: 10.1111/jgs.13178. [DOI] [PubMed] [Google Scholar]
- 12.Kuiper J.S., Zuidersma M., Oude Voshaar R.C., Zuidema S.U., van den Heuvel E.R., Stolk R.P., Smidt N. Social relationships and risk of dementia: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res. Rev. 2015;22:39–57. doi: 10.1016/j.arr.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 13.Lara E., Martín-María N., de la Torre-Luque A., Koyanagi A., Vancampfort D., Izquierdo A., Miret M. Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Res. Rev. 2019;52:7–16. doi: 10.1016/j.arr.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Penninkilampi R., Casey A.-N., Singh M.F., Brodaty H. The Association between Social Engagement, Loneliness, and Risk of Dementia: A Systematic Review and Meta-Analysis. J. Alzheimers Dis. 2018;66:1619–1633. doi: 10.3233/JAD-180439. [DOI] [PubMed] [Google Scholar]
- 15.Poey J.L., Burr J.A., Roberts S.J. Social Connectedness, Perceived Isolation, and Dementia: Does the Social Environment Moderate the Relationship Between Genetic Risk and Cognitive Well-Being? Gerontologist. 2017;57:1031–1040. doi: 10.1093/geront/gnw154. [DOI] [PubMed] [Google Scholar]
- 16.Phillips L.H., Scott C., Henry J.D., Mowat D., Bell J.S. Emotion perception in Alzheimer’s disease and mood disorder in old age. Psychol. Aging. 2010;25:38–47. doi: 10.1037/a0017369. [DOI] [PubMed] [Google Scholar]
- 17.Saz P., López-Antón R., Dewey M.E., Ventura T., Martín A., Marcos G., De La Cámara C., Quintanilla M.A., Quetglas B., Bel M., et al. Prevalence and implications of psychopathological non-cognitive symptoms in dementia. Acta Psychiatr. Scand. 2009;119:107–116. doi: 10.1111/j.1600-0447.2008.01280.x. [DOI] [PubMed] [Google Scholar]
- 18.Singleton D., Mukadam N., Livingston G., Sommerlad A. How people with dementia and carers understand and react to social functioning changes in mild dementia: A UK-based qualitative study. BMJ Open. 2017;7:e016740. doi: 10.1136/bmjopen-2017-016740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burgener S.C., Buckwalter K., Perkhounkova Y., Liu M.F. The effects of perceived stigma on quality of life outcomes in persons with early-stage dementia: Longitudinal findings: Part 2. Dementia. 2013;14:609–632. doi: 10.1177/1471301213504202. [DOI] [PubMed] [Google Scholar]
- 20.Wettstein M., Wahl H.-W., Shoval N., Oswald F., Voss E., Seidl U., Frölich L., Auslander G., Heinik J., Landau R. Out-of-Home Behavior and Cognitive Impairment in Older Adults: Findings of the SenTra Project. J. Appl. Gerontol. 2012;34:3–25. doi: 10.1177/0733464812459373. [DOI] [PubMed] [Google Scholar]
- 21.de Jong Gierveld J., van Tilburg T., Dykstra P.A. Loneliness and Social Isolation. In: Vangelisti A.L., Perlman D., editors. The Cambridge Handbook of Personal Relationships. Cambridge University Press; Cambridge, UK: 2006. pp. 485–500. [DOI] [Google Scholar]
- 22.Huber M., Knottnerus J.A., Green L., van der Horst H., Jadad A.R., Kromhout D., Leonard B., Lorig K., Loureiro M.I., van der Meer J.W., et al. How should we define health? BMJ. 2011;343:d4163. doi: 10.1136/bmj.d4163. [DOI] [PubMed] [Google Scholar]
- 23.Levasseur M., Richard L., Gauvin L., Raymond É. Inventory and analysis of definitions of social participation found in the aging literature: Proposed taxonomy of social activities. Soc. Sci. Med. 2010;71:2141–2149. doi: 10.1016/j.socscimed.2010.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morris M.E., Adair B., Ozanne E., Kurowski W., Miller K.J., Pearce A.J., Santamaria N., Long M., Ventura C., Said C.M. Smart technologies to enhance social connectedness in older people who live at home. Australas. J. Ageing. 2014;33:142–152. doi: 10.1111/ajag.12154. [DOI] [PubMed] [Google Scholar]
- 25.Poscia A., Stojanovic J., La Milia D.I., Duplaga M., Grysztar M., Moscato U., Onder G., Collamati A., Ricciardi W., Magnavita N. Interventions targeting loneliness and social isolation among the older people: An update systematic review. Exp. Gerontol. 2018;102:133–144. doi: 10.1016/j.exger.2017.11.017. [DOI] [PubMed] [Google Scholar]
- 26.Ten Bruggencate T., Luijkx K.G., Sturm J. Social needs of older people: A systematic literature review. Ageing Soc. 2018;38:1745–1770. doi: 10.1017/S0144686X17000150. [DOI] [Google Scholar]
- 27.Ten Bruggencate T., Luijkx K.G., Sturm J. Friends or Frenemies? The Role of Social Technology in the Lives of Older People. Int. J. Environ. Res. Public Health. 2019;16:4969. doi: 10.3390/ijerph16244969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baker S., Warburton J., Waycott J., Batchelor F., Hoang T., Dow B., Ozanne E., Vetere F. Combatting social isolation and increasing social participation of older adults through the use of technology: A systematic review of existing evidence. Australas. J. Ageing. 2018;37:184–193. doi: 10.1111/ajag.12572. [DOI] [PubMed] [Google Scholar]
- 29.Chen Y.-R.R., Schulz P.J. The Effect of Information Communication Technology Interventions on Reducing Social Isolation in the Elderly: A Systematic Review. J. Med. Internet Res. 2016;18:e18. doi: 10.2196/jmir.4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khosravi P., Rezvani A., Wiewiora A. The impact of technology on older adults’ social isolation. Comput. Hum. Behav. 2016;63:594–603. doi: 10.1016/j.chb.2016.05.092. [DOI] [Google Scholar]
- 31.Shah S.G.S., Nogueras D., van Woerden H.C., Kiparoglou V. The COVID-19 Pandemic: A Pandemic of Lockdown Loneliness and the Role of Digital Technology. J. Med. Internet Res. 2020;22:e22287. doi: 10.2196/22287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Øksnebjerg L., Diaz-Ponce A., Gove D., Moniz-Cook E., Mountain G., Chattat R., Woods B. Towards capturing meaningful outcomes for people with dementia in psychosocial intervention research: A pan-European consultation. Health Expect. 2018;21:1056–1065. doi: 10.1111/hex.12799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van der Roest H.t.G., Meiland F.J.M., Maroccini R., Comijs H.C., Jonker C., Dröes R.M. Subjective needs of people with dementia: A review of the literature. Int. Psychogeriatr. 2007;19:559–592. doi: 10.1017/S1041610206004716. [DOI] [PubMed] [Google Scholar]
- 34.Pinto-Bruno Á.C., García-Casal J.A., Csipke E., Jenaro-Río C., Franco-Martín M. ICT-based applications to improve social health and social participation in older adults with dementia. A systematic literature review. Aging Ment. Health. 2017;21:58–65. doi: 10.1080/13607863.2016.1262818. [DOI] [PubMed] [Google Scholar]
- 35.Eurostat Internet Activities of People, by Age Class, EU-27, 2009 and 2019. [(accessed on 24 March 2021)]; Available online: https://ec.europa.eu/eurostat/statistics-explained/images/b/b7/Internet_activities_of_people%2C_by_age_class%2C_EU-27%2C_2009_and_2019_%28%25%29_AE2020.png.
- 36.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Neal D., van den Berg F., Planting C., Ettema T., Dijkstra K., Finnema E., Dröes R.-M. Can Use of Digital Technologies by People with Dementia Improve Self-Management and Social Participation? A Systemtic Review of Effect Studies. J. Clin. Med. 2021;10:604. doi: 10.3390/jcm10040604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Popay J., Roberts H., Sowden A., Petticrew M., Arai L., Rodgers M., Britten N., Roen K., Duffy S. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. A Product from the ESRC Methods Programme. Version 1. [(accessed on 9 November 2020)]; Available online: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.178.3100&rep=rep1&type=pdf.
- 39.Landis J.R., Koch G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 40.McMaster University Effective Public Health Practice Project (EPHPP): Quality assessment Tool for Quantitative Studies. [(accessed on 8 November 2020)]; Available online: https://merst.ca/ephpp/
- 41.Walsh D., Downe S. Appraising the quality of qualitative research. Midwifery. 2006;22:108–119. doi: 10.1016/j.midw.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 42.Lincoln Y.S., Guba E.G. Naturalistic Inquiry. SAGE Publications; Newbury Park, CA, USA: 1985. [Google Scholar]
- 43.Heyvaert M., Hannes K., Maes B., Onghena P. Critical Appraisal of Mixed Methods Studies. J. Mix. Methods Res. 2013;7:302–327. doi: 10.1177/1558689813479449. [DOI] [Google Scholar]
- 44.Creswell J.W., Plano Clark V.L. Designing and Conducting Mixed Methods Research. 3rd ed. SAGE Publications; Thousand Oaks, CA, USA: 2018. [Google Scholar]
- 45.Ballantyne A., Trenwith L., Zubrinich S., Corlis M. ‘I feel less lonely’: What older people say about participating in a social networking website. Qual. Ageing Older Adults. 2010;11:25–35. doi: 10.5042/qiaoa.2010.0526. [DOI] [Google Scholar]
- 46.Bickmore T.W., Caruso L., Clough-Gorr K., Heeren T. ‘It’s just like you talk to a friend’ relational agents for older adults. Interact. Comput. 2005;17:711–735. doi: 10.1016/j.intcom.2005.09.002. [DOI] [Google Scholar]
- 47.Biniok P., Menke I. Societal Participation of the Elderly: Information and Communication Technologies as a “Social Junction”. Anthropol. Aging. 2015;36:164–181. doi: 10.5195/aa.2015.102. [DOI] [Google Scholar]
- 48.Bowes A., McColgan G. Telecare for Older People: Promoting Independence, Participation, and Identity. Res. Aging. 2012;35:32–49. doi: 10.1177/0164027511427546. [DOI] [Google Scholar]
- 49.Cornejo R., Tentori M., Favela J. Enriching in-person encounters through social media: A study on family connectedness for the elderly. Int. J. Hum. Comput. Stud. 2013;71:889–899. doi: 10.1016/j.ijhcs.2013.04.001. [DOI] [Google Scholar]
- 50.Engelbrecht R., Shoemark H. The acceptability and efficacy of using iPads in music therapy to support wellbeing with older adults: A pilot study. AJMT. 2015;26:52. [Google Scholar]
- 51.Hind D., Mountain G., Gossage-Worrall R., Walters S.J., Duncan R., Newbould L., Rex S., Jones C., Bowling A., Cattan M. Putting Life in Years (PLINY): A randomised controlled trial and mixed-methods process evaluation of a telephone friendship intervention to improve mental well-being in independently living older people. Public Health Res. 2014;2 doi: 10.3310/phr02070. [DOI] [PubMed] [Google Scholar]
- 52.Kahlbaugh P.E., Sperandio A.J., Carlson A.L., Hauselt J. Effects of Playing Wii on Well-Being in the Elderly: Physical Activity, Loneliness, and Mood. Act. Adapt. Aging. 2011;35:331–344. doi: 10.1080/01924788.2011.625218. [DOI] [Google Scholar]
- 53.Mellor D., Firth L., Moore K. Can the Internet Improve the Well-being of the Elderly? Ageing Int. 2008;32:25–42. doi: 10.1007/s12126-008-9006-3. [DOI] [Google Scholar]
- 54.Ring L., Shi L., Totzke K., Bickmore T. Social support agents for older adults: Longitudinal affective computing in the home. J. Multimodal User Interfaces. 2015;9:79–88. doi: 10.1007/s12193-014-0157-0. [DOI] [Google Scholar]
- 55.Slegers K., van Boxtel M.P.J., Jolles J. Effects of Computer Training and Internet Usage on the Well-Being and Quality of Life of Older Adults: A Randomized, Controlled Study. J. Gerontol. B Psychol. Sci. Soc. Sci. 2008;63:176–184. doi: 10.1093/geronb/63.3.P176. [DOI] [PubMed] [Google Scholar]
- 56.Woodward A.T., Freddolino P.P., Blaschke-Thompson C.M., Wishart D.J., Bakk L., Kobayashi R., Tupper C. Technology and Aging Project: Training Outcomes and Efficacy from a Randomized Field Trial. Ageing Int. 2011;36:46–65. doi: 10.1007/s12126-010-9074-z. [DOI] [Google Scholar]
- 57.Airola E., Rasi P., Outila M. Older people as users and non-users of a video conferencing service for promoting social connectedness and well-being—A case study from Finnish Lapland. Educ. Gerontol. 2020;46:258–269. doi: 10.1080/03601277.2020.1743008. [DOI] [Google Scholar]
- 58.Arthanat S., Vroman K.G., Lysack C. A home-based individualized information communication technology training program for older adults: A demonstration of effectiveness and value. Disabil. Rehabil. Assist. Technol. 2016;11:316–324. doi: 10.3109/17483107.2014.974219. [DOI] [PubMed] [Google Scholar]
- 59.Breck B.M., Dennis C.B., Leedahl S.N. Implementing reverse mentoring to address social isolation among older adults. J. Gerontol. Soc. Work. 2018;61:513–525. doi: 10.1080/01634372.2018.1448030. [DOI] [PubMed] [Google Scholar]
- 60.Burmeister O.K., Bernoth M., Dietsch E., Cleary M. Enhancing Connectedness Through Peer Training for Community-Dwelling Older People: A Person Centred Approach. Issues Ment. Health. Nurs. 2016;37:406–411. doi: 10.3109/01612840.2016.1142623. [DOI] [PubMed] [Google Scholar]
- 61.Chi N.-C., Sparks O., Lin S.-Y., Lazar A., Thompson H.J., Demiris G. Pilot testing a digital pet avatar for older adults. Geriatr. Nurs. 2017;38:542–547. doi: 10.1016/j.gerinurse.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cutler C., Hicks B., Innes A. Does Digital Gaming Enable Healthy Aging for Community-Dwelling People with Dementia? Games Cult. 2015;11:104–129. doi: 10.1177/1555412015600580. [DOI] [Google Scholar]
- 63.Czaja S.J., Boot W.R., Charness N., Rogers W.A., Sharit J. Improving Social Support for Older Adults Through Technology: Findings from the PRISM Randomized Controlled Trial. Gerontologist. 2018;58:467–477. doi: 10.1093/geront/gnw249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Emas S., Montoya L., Chen A., Tran C., Tran P., Dharni A. Empowering Older Adults: Incorporating Technology for Retirement Adjustment. Phys. Occup. Ther. Geriatr. 2018;36:245–257. doi: 10.1080/02703181.2018.1497747. [DOI] [Google Scholar]
- 65.Goumopoulos C., Papa I., Stavrianos A. Development and Evaluation of a Mobile Application Suite for Enhancing the Social Inclusion and Well-Being of Seniors. Informatics. 2017;4:15. doi: 10.3390/informatics4030015. [DOI] [Google Scholar]
- 66.Hemberg J., Fischer R.S. A Window Toward the World. Older Adults’ Experiences of Becoming in Health and Developing as Human Beings Through Interacting With Others Using Real Video Communication. Holist. Nurs. Pract. 2018;32:90–97. doi: 10.1097/HNP.0000000000000254. [DOI] [PubMed] [Google Scholar]
- 67.Jansen-Kosterink S.M., Bergsma J., Francissen A., Naafs A. The first evaluation of a Mobile application to encourage social participation for community-dwelling older adults. Health Technol. 2020;10:1107–1113. doi: 10.1007/s12553-020-00430-9. [DOI] [Google Scholar]
- 68.Judges R.A., Laanemets C., Stern A., Baecker R.M. “InTouch” with seniors: Exploring adoption of a simplified interface for social communication and related socioemotional outcomes. Comput. Hum. Behav. 2017;75:912–921. doi: 10.1016/j.chb.2017.07.004. [DOI] [Google Scholar]
- 69.Kim J., Gray J. Qualitative Evaluation of an Intervention Program for Sustained Internet Use Among Low-Income Older Adults. Ageing Int. 2016;41:240–253. doi: 10.1007/s12126-015-9235-1. [DOI] [Google Scholar]
- 70.Lee O.E.-K., Kim D.-H. Bridging the Digital Divide for Older Adults via Intergenerational Mentor-Up. Res. Soc. Work Pract. 2018;29:786–795. doi: 10.1177/1049731518810798. [DOI] [Google Scholar]
- 71.Matz-Costa C., Lubben J., Lachman M.E., Lee H., Choi Y.J. A Pilot Randomized Trial of an Intervention to Enhance the Health-Promoting Effects of Older Adults’ Activity Portfolios: The Engaged4Life Program. J. Gerontol. Soc. Work. 2018;61:792–816. doi: 10.1080/01634372.2018.1542371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mullins L.B., Skemp L., Reed D., Emerson M. Internet Programming to Reduce Loneliness and Social Isolation in Aging. Res. Gerontol. Nurs. 2020;13:233–242. doi: 10.3928/19404921-20200320-01. [DOI] [PubMed] [Google Scholar]
- 73.Myhre J.W., Mehl M.R., Glisky E.L. Cognitive Benefits of Online Social Networking for Healthy Older Adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 2017;72:752–760. doi: 10.1093/geronb/gbw025. [DOI] [PubMed] [Google Scholar]
- 74.Neil-Sztramko S.E., Coletta G., Dobbins M., Marr S. Impact of the AGE-ON Tablet Training Program on Social Isolation, Loneliness, and Attitudes Toward Technology in Older Adults: Single-Group Pre-Post Study. JMIR Aging. 2020;3:e18398. doi: 10.2196/18398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.O’Brien C.J., Smith J.L., Beck D.E. Real relationships in a virtual world: Social engagement among older adults in Second Life. Gerontechnology. 2016;15:171–179. doi: 10.4017/gt.2016.15.3.006.00. [DOI] [Google Scholar]
- 76.Unbehaun D., Vaziri D.D., Aal K., Wieching R., Tolmie P., Wulf V. Exploring the Potential of Exergames to affect the Social and Daily Life of People with Dementia and their Caregivers; Proceedings of the CHI 2018; Montreal, QC, Canada. 21–26 April 2018; p. 62. [Google Scholar]
- 77.Ware C., Damnee S., Djabelkhir L., Cristancho V., Wu Y.-H., Benovici J., Pino M., Rigaud A.-S. Maintaining Cognitive Functioning in Healthy Seniors with a Technology-Based Foreign Language Program: A Pilot Feasibility Study. Front. Aging Neurosci. 2017;9:42. doi: 10.3389/fnagi.2017.00042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yu F., Mathiason M.A., Johnson K., Gaugler J.E., Klassen D. Memory matters in dementia: Efficacy of a mobile reminiscing therapy app. Alzheimers Dement. (N. Y.) 2019;5:644–651. doi: 10.1016/j.trci.2019.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zaine I., Frohlich D.M., Rodrigues K.R.D.H., Cunha B.C.R., Orlando A.F., Scalco L.F., Pimentel M.D.G.C. Promoting Social Connection and Deepening Relations Among Older Adults: Design and Qualitative Evaluation of Media Parcels. J. Med. Internet Res. 2019;21:e14112. doi: 10.2196/14112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vanoh D., Shahar S., Razali R., Ali N.M., Manaf Z.A., Noah S.A.M., Nur A.M. The Effectiveness of a Web-Based Health Education Tool, WESIHAT 2.0, among Older Adults: A Randomized Controlled Trial. J. Alzheimers Dis. 2019;70:S255–S270. doi: 10.3233/JAD-180464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pu L., Moyle W., Jones C., Todorovic M. The Effectiveness of Social Robots for Older Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Studies. Gerontologist. 2019;59:e37–e51. doi: 10.1093/geront/gny046. [DOI] [PubMed] [Google Scholar]
- 82.Mulry C.M., Piersol C.V. The Let’s Go Program for Community Participation: A Feasibility Study. Phys. Occup. Ther. Geriatr. 2014;32:241–254. doi: 10.3109/02703181.2014.932316. [DOI] [Google Scholar]
- 83.Johnson J.K., Stewart A.L., Acree M., Nápoles A.M., Flatt J.D., Max W.B., Gregorich S.E. A Community Choir Intervention to Promote Well-Being Among Diverse Older Adults: Results From the Community of Voices Trial. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020;75:549–559. doi: 10.1093/geronb/gby132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gardiner C., Geldenhuys G., Gott M. Interventions to reduce social isolation and loneliness among older people: An integrative review. Health Soc. Care Community. 2016;26:147–157. doi: 10.1111/hsc.12367. [DOI] [PubMed] [Google Scholar]
- 85.Douglas H., Georgiou A., Westbrook J. Social participation as an indicator of successful aging: An overview of concepts and their associations with health. Aust. Health Rev. 2017;41:455–462. doi: 10.1071/AH16038. [DOI] [PubMed] [Google Scholar]
- 86.Dickens A.P., Richards S.H., Greaves C.J., Campbell J.L. Interventions targeting social isolation in older people: A systematic review. BMC Public Health. 2011;11:647. doi: 10.1186/1471-2458-11-647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Morrow-Howell N., Galucia N., Swinford E. Recovering from the COVID-19 Pandemic: A Focus on Older Adults. J. Aging Soc. Policy. 2020;32:526–535. doi: 10.1080/08959420.2020.1759758. [DOI] [PubMed] [Google Scholar]
- 88.Chen A.T., Ge S., Cho S., Teng A.K., Chu F., Demiris G., Zaslavsky O. Reactions to COVID-19, information and technology use, and social connectedness among older adults with pre-frailty and frailty. Geriatr. Nurs. 2021;42:188–195. doi: 10.1016/j.gerinurse.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dröes R.M., Chattat R., Diaz A., Gove D., Graff M., Murphy K., Verbeek H., Vernooij-Dassen M., Clare L., Johannessen A., et al. Social health and dementia: A European consensus on the operationalization of the concept and directions for research and practice. Aging Ment. Health. 2017;21:4–17. doi: 10.1080/13607863.2016.1254596. [DOI] [PubMed] [Google Scholar]
- 90.Gaber S.N., Nygård L., Brorsson A., Kottorp A., Charlesworth G., Wallcook S., Malinowsky C. Social Participation in Relation to Technology Use and Social Deprivation: A Mixed Methods Study Among Older People with and without Dementia. Int. J. Environ. Res. Public Health. 2020;17:4022. doi: 10.3390/ijerph17114022. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.