Abstract
The role of worry and rumination in eating disorders (EDs) is controversial. This meta-analysis of the literature is aimed at clarifying the relationship between repetitive negative thinking (RNT) and EDs. In accordance with the PRISMA criteria, a comprehensive search of the literature was conducted on PubMed and PsycInfo from inception to March 2021. Search terms: “eating disorder/anorexia/bulimia/binge eating disorder” AND “worry/rumination/brooding/repetitive thinking”. A manual search of reference lists was also run. Forty-three studies were included. RNT was found to be associated with anorexia, bulimia, and binge eating disorder. A moderating effect was found for “presence/absence ED diagnosis” and “subtype of ED symptom”. ED patients showed higher RNT than the general population. No differences were observed for age or between worry and rumination in the magnitude of their association with EDs.
Keywords: repetitive negative thinking, rumination, worry, eating disorder, anorexia, bulimia, binge eating disorder
1. Introduction
Repetitive negative thinking (RNT) is a cognitive process characterised by a repetitive, frequent, and self-focused form of thinking [1]. Worry and rumination have been grouped under the construct of RNT [2,3]. Worry has been defined as a chain of thoughts and images laden with negative affects and relatively uncontrollable [4]. Worry is an attempt to engage in mental problem-solving on an issue whose outcome is unknown but contains the possibility of being negative. Rumination is defined as thoughts that repetitively focus attention on negative emotions and symptoms, their causes, meanings, and consequences [5]. Rumination can take verbal and imaginary forms [6], characterized by the tendency to repeatedly think on the self, upsetting events, and personal concerns [7]. Worry is usually focused on problem-solving and is more future-oriented, whereas rumination often consists of themes of loss and typically has a focus on past problems [8].
An extensive literature base has suggested that both worry and rumination are cognitive processes present across diverse disorders [2]. Worry is associated with anxiety disorders [9,10,11,12] and major depressive disorder [13,14,15]. Rumination is associated with both the development and persistence of mood and anxiety disorders [16,17,18,19,20,21,22,23,24], addictive behaviours [25,26], and schizophrenia [27].
It is extensively acknowledged that preoccupation with the control of eating, weight, and shape is conceptualized as core feature of eating disorder (ED) psychopathology [28,29]. Thus, it is conceivable that individuals presenting with EDs may report a stronger tendency to engage in RNT. A recent meta-analysis by Smith, Mason and Lavender [30] pointed out that rumination is concurrently and prospectively associated with ED psychopathology and that individuals with EDs showed higher levels of rumination than those without an ED. Although the association between rumination and EDs has been explored, no study has systematically examined the role of worry in EDs. Notwithstanding some evidence showing raised levels of worry in patients with EDs compared to controls from the general population [31,32,33], it is not possible to draw a conclusion about the association between worry and EDs due to the lack of a systematic review or meta-analysis.
Thus, an increasing number of studies have explored the association between RNT and EDs, and the relationship between rumination and EDs has been highlighted in the meta-analysis by Smith and colleagues [30]. However, to date, no qualitative or quantitative reviews have been performed that take into account both worry and rumination and possible moderators of the relationship between RNT and EDs. Clarifying this relationship could have implications for clinical practice, especially with respect to interventions aimed at interrupting RNT.
Through the use of meta-analytic techniques, the present study aimed to present a comprehensive evaluation of the literature on EDs, worry and rumination in order to: (1) extend the literature and estimate the magnitude of the association between EDs, worry and rumination; (2) explore the role of some moderators such (a) “subtypes of ED symptoms”, the (b) “presence vs. absence of a diagnosis of ED” and (c) “worry vs. rumination” and (3) “mean age of the sample” in shaping heterogeneity.
2. Materials and Methods
2.1. Study Selection
The methodology of the study selection will be reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [34].
2.1.1. Eligible Studies Included
The inclusion criteria applied to the literature search were: (a) English language articles published in peer-reviewed journals; (b) diagnosis of ED determined according to the standardized diagnostic criteria, including the Diagnostic and Statistical Manual of Mental Disorders (DSM) from the third to the fifth edition [35,36,37,38,39], the Research Diagnostic Criteria (RDC) [40] or the International Classification of Diseases (ICD) from the sixth to the tenth edition [41,42,43,44,45] and assessing worry and/or rumination; (c) studies using a case–control design/prospective cohort studies/large population-based cross-sectional studies/experimental studies and (d) information available to determine the effect size.
Studies including participants with a diagnosis of neurological and/or neurocognitive organic impairment, or co-occurrent psychiatric disorders or obese participants, were not included, as well as studies on cognitive processes not specifically referring to worry and rumination.
2.1.2. Information Sources and Search
PubMed and PsycInfo were systematically searched from inception to 31 March 2021. Furthermore, a manual search of reference lists from all the articles selected, full text-reviews and significant reviews was run. Search terms included: eating disorder/anorexia/bulimia/binge eating disorder combined using Boolean “AND” operator with worry/rumination/brooding/repetitive thinking.
2.1.3. Study Selection, Data Collection Process and Data Items
The studies’ eligibility was assessed through the following procedure: title screening, abstract screening and full paper screening. Titles and abstracts were screened by S.P. Articles appearing potentially relevant were retrieved by S.P. and independently assessed by S.P. and G.M. Consistent with the previous studies [46,47,48], disagreements on eligibility were resolved by consensus among authors (intercoder reliability: Cohen’s Kappa coefficient = 0.70). The following assumptions were made: if not specified, participants were considered without co-occurrent psychiatric disorders or neurological or neurocognitive organic impairment.
2.1.4. Assessment of Risk of Bias in Individual Studies
In order to ascertain the validity of the eligible studies, two investigators independently rated each study on the basis of the following markers: homogeneity of the sample regarding the diagnosis if present, appropriateness of random allocation if necessary and presence of a comparable group if appropriate. Disagreements were resolved by consensus [46,47,48] (intercoder reliability: Cohen’s Kappa coefficient = 0.80).
2.2. Quality Assessment
In accordance with previous studies [46,47,48,49], the quality of each eligible study was assessed independently by two investigators (S.P. and G.M.) using the Newcastle Ottawa scale for case–control studies and its adapted form for cross-sectional studies [49,50]. Disagreements were resolved by consensus (intercoder reliability: Cohen’s Kappa coefficient = 0.85).
2.3. Data Analyses
Analyses were conducted using Comprehensive Meta-analysis, CMA version 2.0 by Biostat. Using a random effects model, we calculated the effect size (ES), which was reported here as the standardized difference between the means of the two groups (Cohen’s d), together with their 95% CIs. According to Cohen’s criteria (Cohen, 1988), an ES of <0.20 is considered a small effect, an ES of about 0.50 is a moderate effect and ES of about 0.80 is a large effect. For the purposes of the current study, a positive ES indicated an association between RNT and eating problems. Each ES was calculated for each self-report symptoms scale included in the identified studies and averaged across measures to obtain an ES for each study [51,52].
In order to address the publication bias, i.e., the possibility that published studies have larger mean ES than unpublished studies, we checked the results using the “Trim and Fill” procedure [53] and the Classic Fail-safe Number method [54]. The “Trim and Fill” procedure is a nonparametric method that evaluates the effect of potential data censoring on the meta-analysis [53]. Using this method, a plot of each study’s ESs against the meta-sample’s ES and standard error was built. These plots should be shaped as a funnel when no data censoring is present. Since smaller or nonsignificant studies are less likely to be published, studies in the bottom left/right-hand corner of the plot are often omitted [55]. The most symmetrically right/left unmatching studies in the meta-analysis are thus trimmed and replaced with their missing counterparts imputed or “filled” in as mirror images of the trimmed outcomes [56]. This allows for the computation of an adjusted ES and relative CI. The Classic Fail-safe Number estimates the number of studies with nonsignificant findings, which are necessary to make the combined ES nonsignificant [56]. Meta-analyses with a fail-safe number higher than (5* studies number + 10) are usually considered free from publication bias [54].
The presence of heterogeneity across the studies was evaluated by the I2 index, which measures the proportion of total variation due to real differences in the variability of ESs among studies [56]. The Q statistic was used to test the heterogeneity of the specific set of ESs and the effects of the selected moderators [56]. We considered the following moderators: (a) subtypes of ED symptoms (anorexia nervosa (AN), bulimia nervosa (BN) and binge eating disorder (BED)); (b) presence vs. absence of any diagnosis of EDs (i.e., the comparison between patients and healthy controls from the population); (c) subtype of RNT: worry or rumination and (d) mean age of the sample.
The 1st and 2nd authors independently coded the qualitative moderators in each study, and they reached consensus in the case of disagreements. No disagreements were found among the authors.
For dichotomous moderators, we carried out a subgroup analysis based on a mixed-effect model, assuming a common among-study variance component across the subgroups and a random effect model to combine the subgroups. A Q-test was used to test for heterogeneity across the subgroups [56].
3. Results
3.1. Study Selection
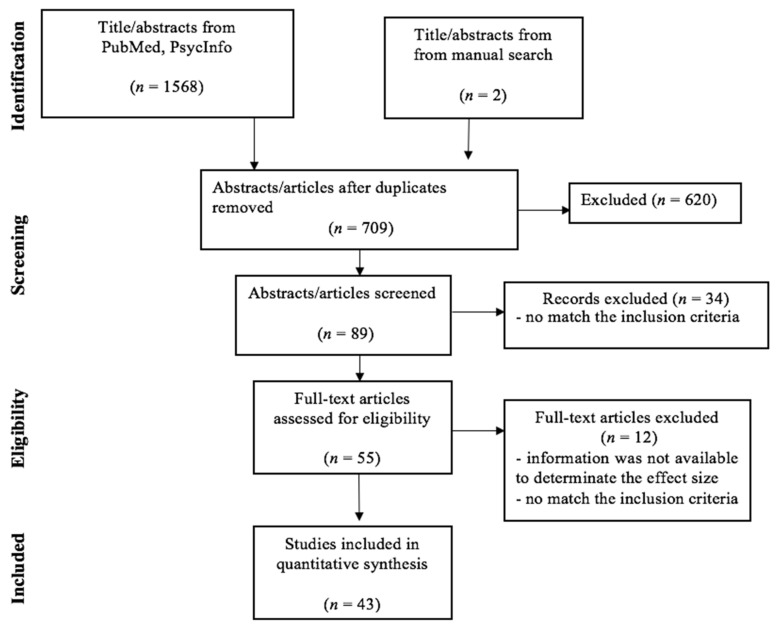
The search of the PubMed and PsycInfo databases and the manual search showed a total of 1570 citations. After removing the duplicates and reviewing the abstracts to exclude those that clearly did not meet the criteria (n = 620), 89 remained. Of these, 34 studies were excluded, because they did not meet the inclusion criteria. Of the 55 studies that remained, 12 studies were further discarded. Figure 1 illustrates the search and screening process. The 43 articles that met the inclusion criteria are listed in Table 1 and Table 2, along with their study characteristics. The total sample size of the selected studies comprised 10,391 participants; among them, 1345 were ED cases (AN = 521, BN = 278, BED = 325 and EDNOS = 221), and 9046 were healthy controls from the general population. The following is a summary of the literature concerning the association between ED, worry and rumination.
Figure 1.
Identification of independent studies for inclusion in the meta-analysis (flow chart). Forty-three studies of 57 cohorts, because some studies were considered more than once. Search Strategy: Limits: English; Search terms included: worry/rumination/brooding/repetitive thinking combined using Boolean “AND” operator with eating disorder/anorexia/bulimia/binge eating disorder.
Table 1.
Summary of the demographic characteristics of the studies assessed and the relationship between worry and eating behavior.
| Source | Study Design | Sample-Size | Age (Years) Mean ± SD | Sex % (n) | Diagnostic Tool Eating Measure |
Sub-Types of ED Symptoms | Worry Measure |
|---|---|---|---|---|---|---|---|
| Napolitano and Himes 2011 [31] | case–control | cases: 46 binge eating group without BED: 186 |
- | F: 100% (232) |
DSM-IV-TR EDDS |
BED | FOBES |
| Sassaroli et al. 2005 [32] | case–control | cases: 63 controls: 30 |
23.06 ± 4.54 vs. 26.32 ± 4.27 |
F: 100% (93) |
SCID-I | AN BN |
PSWQ |
| Sternheim et al. 2012 [33] | case–control | cases: 45 controls: 37 |
25.8 ± 8.5 vs. 27.8 ± 10.2 | not reported | DSM-IV EDE |
AN BN |
PSWQ Catastrophizing Interview |
| González et al. 2017 [57] | cross-sectional | general population: 176 | 31.2 ± 13.3 | F: 67% (118) | EAT | AN BN |
PSWQ |
| Kollei, et al. 2012 [58] | case–control | cases: 66 control: 33 |
AN: 26.94 ± 9.15 BN: 25.94 ± 8.25 CG: 26.91 ± 8.48 |
F: 95.45% (63) vs. 69.7% (23) |
DSM-IV | AN BN |
CITQ |
| Sapuppo et al. 2018 [60] | case–control | cases: 84 controls: 38 |
23.39 ± 4.75 vs. 25.31 ± 5.4 | F: 100% (122) |
SCID-I | AN BN |
PSWQ |
| Startup et al. 2013 [66] | cross-sectional | cases: 62 | 26.6 ± 7.8 | F: 93.5% (58) |
DSM-IV EDE |
AN | PSWQ |
| Zarychta et al. 2017 [67] | cross-sectional | general population: 1260 | 16.38 ± 0.80 | F: 41.7% (525) |
MBSRQ | - | MBSRQ |
| Crino et al. 2019 [68] | case–control | cases: 90 controls: 97 | 25.23 ± 8.33 vs. 20.63 ± 6.37 | F: 100% (187) |
DSM-5 | AN BN BED No-ED | TCQ |
| Hartmann et al. 2019 [69] | cross-sectional | cases: 95 | AN: 23.64 ± 0.62 BN: 26.09 ± 1.17 |
F: 98%(49) F: 97.78%(44) |
EDE-Q | AN BN |
Self-constructed worry item |
Note: AN: Anorexia Nervosa; BN: Bulimia Nervosa; BED: Binge Eating Disorder; CG: Control group; DSM-IV: Diagnostic and Statistical Manual of Mental Disorders; EAT: Eating Attitudes Test; EDE: Eating Disorder Examination; FOBES: Functional assessment of binge eating; PSWQ: Penn State Worry Questionnaire; CITQ: Control of Intrusive Thoughts Questionnaire; MBSRQ: The Multidimensional Body-Self Relations Questionnaire.
Table 2.
Summary of the demographic characteristics of the studies assessed the relationship between rumination and eating behavior.
| Source | Study Design | Sample-Size | Age (Years) Mean ± SD |
Sex % (n) | Diagnostic Tool Eating Measure |
Sub-Types of ED Symptoms | Rumination Measure |
|---|---|---|---|---|---|---|---|
| González et al. 2017 [57] | cross-sectional | general population: 176 | 31.2 ± 13.3 | F: 67% (118) | EAT-26 | AN BN |
RRS |
| Naumann et al. 2015 [59] | experiment case-control | cases: 36 controls: 19 |
AN: 24.94 ± 8.92 BN: 23.28 ± 6.37 CG: 23.32 ± 8.02 |
F: 100% (111) |
DSM-IV-TR EDE |
AN BN |
Rumination experimentally induced by Nolen-Hoeksema and Morrow’s task (1993) RSQ |
| Troop and Treasure 1997 [61] | case–control | cases: 21 controls: 15 |
AN: 23.3 ± 5 BN: 25.4 ± 10.8 CG: 29.5 ± 9 |
F: 100% (36) | ICD-10 | AN BN |
Coping Strategies Interview |
| Cowdrey and Park 2012 [62] | cross-sectional | general population: 228 | 24.03 ± 7.62 | F:100% vs. 100% | EDE-Q | AN and Eating pathology | RRS-ED |
| AN: 42 | 24 ± 8.31 | ||||||
| Rawal et al. 2010 [63] | Study 1 cross-sectional |
students: 177 | 22.39 ± 5.13 | F: 68.92% (122) |
DSM-IV EDE-Q |
AN | Study 1 & 2: RRS |
| Study 2 case–control |
cases: 13 controls: 13 |
26.38 ± 8.77 vs. 25.77 ± 4.85 | F:100% vs. 100% | MINI EDE |
|||
| Wang and Borders 2018 [64] | Study 1 cross-sectional | undergraduate students: 126 | 19.7 ± 1.10 | F: 84% (106) | EDE-Q | Eating pathology | RRS |
| Study 2 cross-sectional | cases: 85 | 24.57 ± 9.95 | F: 87.1% (74) | ||||
| Mason and Lewis 2017 [65] | cross-sectional | general population Caucasian: 100 | 20.14 ± 1.82 | F = 100% | DSM-5 (binge eating episode) |
- | RSQ |
| African-America: 84 | 19.75 ± 1.86 | ||||||
| Startup et al. 2013 [66] | cross-sectional | cases: 62 | 26.6 ± 7.8 | F: 93.5% (58) |
DSM-IV EDE |
AN | CERTS |
| Connolly et al. 2007 [70] | cross-sectional | general population: 140 | 19.5 ± 2.57 | F 100% (140) | BES EDE-Q |
BED | BARQ |
| Nolen-Hoeksema et al. 2007 [71] | cross-sectional | general population: 496 | 13.5 ± 0.67 | F = 100% | DSM-IV EDE |
BN | RSQ |
| Harrell et al. 2008 [72] | cross-sectional | general population: 329 | 19.31 | F = 100% | Dieting and Bingeing Severity Scale | - | AFCI |
| Selby et al. 2008 [73] | cross-sectional | general population: 200 | 18.6 ± 2.36 | F: 68.5% (137) | EDI | BN | CERQ |
| Aldao and Nolen-Hoeksema 2010 [74] | cross-sectional | undergraduate students: 252 | 18.44 ± 0.66 | F: 55.6% (140) | EDE-Q | - | RRS |
| Holm-Denoma and Hankin 2010 [75] | cross-sectional | general population: 191 | 14.5 ± 1.4 | F = 100% | EDDS | BN | CRSQ |
| Verplanken and Tangelder 2011 [76] | cross-sectional | students: 303 | 24 ± 4 | F: 50.16% (152) |
EDS-5 | - | Negative Body Image Thinking |
| Gordon et al. 2012 [77] | cross-sectional | general population: 780 | 19.27 ± 2.12 | F: 65.7% (512) | BES | BED | RRS |
| Kelly et al. 2012 [78] | cross-sectional | general population: 419 | 18.95 ± 1.33 | F = 100% | EDE-Q | BED | CERQ |
| Hilt et al. 2013 [79] | cross-sectional | general population: 101 | 12.7 ± 1.14 | F = 100% | Children’s Eating Attitudes Test ChEAT | Eating pathology | CRSQ |
| Svaldi and Naumann 2014 [80] | cross-sectional | cases: 30 | 46.33 | F = 100% | DSM-IV-TR EDE |
BED | PTQ |
| Mason and Lewis 2015 [81] | cross-sectional | general population: 164 | - | F = 100% | BES | BED | CERQ |
| Breithaupt et al. 2016 [82] | cross-sectional | general population: 353 | 21.93 ± 5.78 | F = 85% (300) | EAT-26 | BN | RRS |
| Jungmann et al. 2016 [83] | cross-sectional | general population: 414 | 47.2 ± 16.7 | F: 54% (223) | EDI-2 | BN | RSQ |
| Maraldo et al. 2016 [84] | cross-sectional | community participants: 313 students: 296 |
34.74 ± 11.36 vs. 19.44 ± 1.75 | F = 100% | EDE-Q | Eating pathology | RRS |
| Naumann et al. 2016 [85] | case-control | cases: AN: 42 BN: 40 controls: 41 |
AN: 25.71 ± 10.65 BN: 25.78 ± 8.49 CG: 25.61 ± 10.30 |
F = 100% | DSM-IV EDE |
AN BN |
Self-constructed Visual Analog Scales |
| Seidel et al. 2016 [86] | case-control | cases: 37 controls: 33 |
AN: 16.40 ± 2.33 CG: 16.51 ± 3.79 |
F = 100% | DSM-IV EDI-2 |
AN | PTQ |
| Opwis et al. 2017 [87] | cross-sectional | general population: 295 | F: 30.23 ± 8.94 M: 30.76 ± 9.14 |
F: 69% (205) | EDE-Q | Eating pathology | RS-8 |
| Wang and Borders 2017 [88] | cross-sectional | general population: 116 | 24.8 ± 5.35 | M: 59.5% (69) | EAT-26 | Eating pathology | Items modified from the Rumination About Interpersonal Offences Scale |
| Wang et al. 2017 [89] | cross-sectional | cases: 237 | 47.9 ± 10 | F: 70% (167) | DSM-IV-TR EDE |
BED | RRS |
| Dondzillo et al. 2018 [90] | cross-sectional | general population: 73 | 18.59 ± 1.28 | F = 100% | DEBQ | AN | RRS-ED |
| Van Durme et al. 2018 [91] | cross-sectional | general population: 397 | 14.02 | F: 62.7% (249) | EDI-II | BN | FEEL-KJ |
| Birmachu et al. 2019 [92] | cross-sectional | general population: 300 | 22.99 ± 6.91 | F: 63.6% (190) | EDE-Q | Eating pathology | RRQ |
| Fresnics et al. 2019 [93] | cross-sectional | general population: 190 | 19.3 ± 1.10 | F: 84% (160) | EDE-Q | Eating pathology | RRS |
| Hernando et al. 2019 [94] | case-control | cases: 25 controls: 25 |
16.6 ± 2.24 vs. 19.08 ± 0.64 |
F = 100% | - | AN, BN, OSFED | RSQ |
| Smith et al. 2019 [95] | cross-sectional | undergraduate students: 263 | 20.3 ± 3.68 | F: 74.9% (197) | EDDS | Eating pathology | RRS |
| Branley-Bell and Talbot 2020 [96] | cross-sectional | general population: 129 | 9.27 ± 8.99 | F: 93.8% (121) | Self-reported ED | Eating pathology | RRS-ED |
Note: AN: Anorexia Nervosa; BN: Bulimia Nervosa; CG: control group; OSFED: Other Specified Feeding or Eating Disorders; ICD: International Classification of Diseases; DSM: Diagnostic and Statistical Manual of Mental Disorders; EAT-26: Eating Attitudes: Test EDE: Eating Disorder Examination; EDDS: Eating Disorder Diagnostic Scale; EDI-2: Eating Disorder Inventory; RSQ: Response Styles Questionnaire; BES: Binge Eating Scale; EDE-Q: Eating Disorders Examination Questionnaire; EDS-5: Eating Disturbance Scale; BARQ: Behavioural Anger Response Questionnaire; RRS: Ruminative Response Scale; RRS-ED: Ruminative Response Scale for Eating Disorders; MINI: Mini International Neuropsychiatric Interview; AFCI: Adult Emotion-Focused Coping Inventory; ChEAT: Children’s Eating Attitudes Test; CRSQ: Children’s Response Style Questionnaire; CERQ: Cognitive Emotion Regulation Questionnaire; EDE-Q: Eating Disorder Examination Questionnaire; RS-8: Rumination–Suppression-8 Scale; CERTS: Cambridge Exeter Repetitive Thought Scale; DEBQ: Dutch Eating Behaviour Questionnaire; FEEL-KJ: Fragebogen zur Erhebung der Emotionsregulation bei Kindern und Jugendlich; RRQ: Rumination–reflection Questionnaire.
A total of 43 studies, 10 on worry and 35 on rumination, were identified for inclusion in the meta-analysis. Thirteen reports were considered more than one time, since some studies included both AN and BN samples [32,33,57,58,59,60,61] or included clinical and general populations [62,63,64] or included different kinds of general populations [65] or included both worry and rumination [57,66], leaving a total of 57 entries for the meta-analysis.
3.2. Study Quality
None of the studies fulfilled all the Newcastle-Ottawa quality criteria. In twelve case–control studies, six studies scored 7/10, three studies scored equal to 6 and three studies scored 5/10. In thirty-three cross-sectional studies, three studies scored 8/10, 26 studies scored equal to 7, three study scored 6/10 and one scored 5/10. More details about the study quality for the case–control and cohort studies are reported in the Supplementary Materials in Tables S1 and S2, respectively.
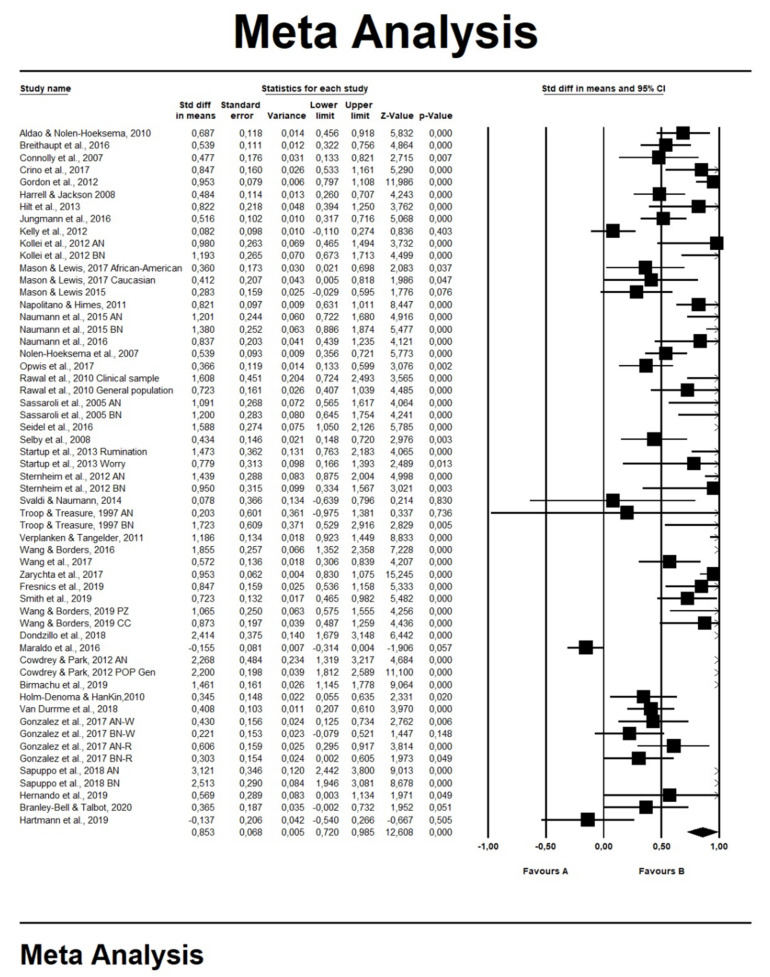
3.3. RT and Eating Problems
The 57 entries selected showed an average ES of 0.85 (SE: 0.07, 95% CI: 0.72–0.98; Test of Null (2-Tail): z-value = 12.61, p < 0.001, k = 57), which indicated a large positive association between eating problems and RNT (Figure 2). The ES is a global measure and has been calculated in all the studies included in the quantitative analysis. Duval and Tweedie’s trim-and-fill procedure indicated only five missing studies (adjusted ES g = 0.90, 95% CI: 0.75–1.06), with a classic fail-safe number estimated at 6897. Since we found heterogeneity among the studies (Q = 559.79, p < 0.001, I2 = 90.000), we conducted further analyses by testing the roles of the possible moderators.
Figure 2.
Forest plots for repetitive thinking and eating behavior. Box indicates effect sizes (ESs), while error bars represent 95% confidence intervals (CIs). The rumble represents the average ES. Note: Favors A = negative association between repetitive thinking and eating disorders. Favors B = positive association between repetitive thinking and eating disorders. The rumble represents the average ES.
Moderator Analyses: Subtypes of ED Symptoms, Presence vs. Absence of Diagnosis of EDs, Worry–Rumination and Age
For each moderator, a separate model was tested. For more details, see Table 3. The subgroup analysis revealed differences in ES for the types of ED symptoms (Q = 11.65, df = 2, p = 0.003): AN d = 1.35 (SE:0.20, 95% CI: 0.96–1.74; Test of Null (2-Tail): z-value = 7.76, p < 0.001, k = 14), BN d = 0.75 (SE:0.11, 95% CI: 0.54–0.97; Test of Null (2-Tail): z-value = 6.80, p < 0.001, k = 14); BED, d = 0.50 (SE:0.15, 95% CI: 0.20–0.80; Test of Null (2-Tail): z-value = 3.29, p = 0.001, k = 7).
Table 3.
Moderator analyses: subtypes of ED symptoms, presence vs. absence of diagnosis of EDs, worry–rumination and age.
| ES | β Point Estimate | SE | CI | p | |
|---|---|---|---|---|---|
| Subtypes of ED symptoms | 0.003 | ||||
| AN | 1.35 | 0.20 | 0.96–1.74 | <0.001 | |
| BN | 0.75 | 0.11 | 0.54–0.97 | <0.001 | |
| BED | 0.50 | 0.15 | 0.20–0.80 | 0.001 | |
| Presence vs. absence of diagnosis of EDs | 0.004 | ||||
| Clinical samples | 1.14 | 0.13 | 0.87–1.40 | <0.001 | |
| Healthy controls from the general population | 0.69 | 0.08 | 0.54–0.85 | <0.001 | |
| Repetitive Negative Thinking | 0.118 | ||||
| Worry | 1.04 | 0.14 | 0.76–1.32 | <0.001 | |
| Rumination | 0.79 | 0.08 | 0.64–0.94 | <0.001 | |
| Age | −0.0108 | 0.009 | −0.03–0.01 | 0.26 |
Note: ES = Effect Size; SE = Standard Error; CI = Confidence Interval; AN = Anorexia Nervosa; BN = Bulimia Nervosa; BED: Binge Eating Disorder.
We also found differences in the ES between studies based on clinical samples vs. studies based on the healthy controls from the general population (Q = 8.15, df = 1, p = 0.004): clinical samples ES: d = 1.14 (SE: 0.13, 95% CI: 0.87–1.40; Test of Null (2-Tail): z-value = 8.44, p < 0.001, k = 24); general population ES: d = 0.69 (SE:0.08, 95% CI: 0.54–0.85; Test of Null (2-Tail): z-value = 8.97, p < 0.001, k = 33).
No differences emerged from the comparison between the studies on worry vs. studies on rumination (Q = 2.45, df = 1, p = 0.118): worry ES: d = 1.04 (SE: 0.14, 95% CI: 0.76–1.32, Test of Null 2-Tail: z-value = 7.28, p < 0.001, k = 15); rumination ES: d = 0.79 (SE: 0.08, 95% CI: 0.64–0.94, Test of Null 2-Tail: z-value = 10.36, p < 0.001, k = 42).
Finally, there was not a significant effect of the variable “age” in shaping heterogeneity (age: β point estimate = −0.0108, SE = 0.009, 95% CI: −0.03–0.01, z-value = −1.12, p = 0.26, k = 55).
4. Discussion
To our knowledge, this is the first study on the relationship between EDs, worry and rumination based on a meta-analytic methodology. The main findings of the present meta-analysis indicate a significant association between RNT and EDs, given that: (a) RNT is highly associated with eating problems in both clinical and nonclinical samples (ESs range from 0.50 to 1.35) and (b) ED patients show higher levels of RNT than the general population. These findings are consistent with Smith and colleagues’ findings [30] but differ from these given that both worry and rumination have been found to be associated with ED symptoms. Moreover, our findings suggest that the strength of the association is not influenced by the age of the participants.
These findings raise an important question: How does RNT play a role in ED symptoms, such as dieting or binge eating? It has been shown that negative beliefs and negative emotions might act as a trigger for RNT that, in turn, further maintains the experience of emotional distress [2,3,66,97,98,99]. Moreover, it is well-known that dieting and binge eating could be a coping strategy to tackle negative emotions [29,99,100]. Should the latter perspective be taken, dieting could be construed as a strategy to cope with negative thoughts and/or emotions that act as a trigger of RNT. Binge eating could be a behavior aimed to reduce chronic stress due to RNT focused on dieting or independently from it. Even though clinical models, such as the Self-Regulatory Executive Function (S-REF) model [101], the Emotional Cascade Model (ECM) [73] or Fairburn’s model [29], might partially support these assumptions, further studies are required to directly test these hypotheses.
The Self-Regulatory Executive Function model (S-REF model) [101] postulates that several maladaptive forms of coping, including repetitive negative thinking (desire thinking, rumination and worry), maintain psychological distress. These maladaptive forms of coping are termed the “Cognitive Attentional Syndrome” (CAS) [102], which is activated and maintained by metacognitive beliefs (i.e., information individuals hold about their own cognition and coping) [102]. CAS is problematic, because it causes negative cognitive–affective states to remain in the consciousness rather than spontaneously decay, leading to failures to modify self-beliefs about control over the mind [103]. Given the association observed between RNT and ED symptoms, and the association between metacognitive beliefs and both EDs and behaviors [48], the S-REF model could explain the role of RNT in ED symptoms.
As postulated by the emotional cascade model [73], an event that triggers a negative emotion may lead to rumination about the event, increasing the intensity of the negative emotions. Furthermore, stress and negative emotional states may increase the level of rumination, which, in turn, may lead to an escalation (cascade) of negative feelings [104]. As a result, an individual may engage in eating behaviors as a coping strategy to tackle negative mood states. It may be assumed that worry and negative emotion are related to each other in the same way. There is mounting evidence that worry may maintain the experience of emotional distress [98].
As regards the Fairburn’s “transdiagnostic” model of ED [29], it was proposed that binge eating could be triggered, among other factors, by adverse events and negative mood states. In turn, binge eating will tend to improve, albeit temporarily, a negative mood and serve as a distraction from negative thinking patterns. It can therefore be argued that an ED mindset characterized by cognitive processes such as worry and rumination exist, and this is activated in the presence of adverse events, leading to a negative mood and the maintenance of ED behaviors. These behaviors may serve to decrease negative emotions, interrupt worry and rumination and help manage (in the short-term) the adverse event. However, the manner in which worry, rumination and negative affectivity may interact in EDs remains unclear, with further studies required to disentangle this complex relationship.
The findings of the current meta-analysis suggest that RNT is associated with all subtypes of ED symptoms supporting a vision of RNT as a transdiagnostic process [2]; nevertheless, some differences may be identified in the strength of the association between RNT and the subtypes of ED symptoms: based on the ES values, the association between RNT and the subtypes of ED symptoms might be stronger in AN than in BN and BED. Taking as a framework the S-REF model [101], it could be hypothesized that there are differences among the ED symptom subtypes in maladaptive metacognitive beliefs that activate and maintain maladaptive forms of coping such as RNT; as highlighted in a recent systematic review [48], maladaptive metacognitive beliefs appear to be stronger in AN than in other ED subtypes. Furthermore, the moderate ES for BED could suggest that BED symptoms could be more closely related with a different form of RNT process such as desire thinking [78,105] rather than worry and rumination, albeit the scarce number of published studies on BED suggests caution in this interpretation.
Furthermore, our data, differently from a previous meta-analysis that exclusively focused on rumination [30], suggests that there is no difference between worry and rumination in the relationship with eating problems. This suggests, in line with the construct of RNT [2,3], that both processes are implicated in eating problems. Notwithstanding this observation, the additional data on worry may be in line with some evidence suggesting that, beyond having a common characteristic in repetitive thought, rumination and worry may have differential effects on the severity of mental illness [106,107]. Compared to rumination, worry appears to be a more influential cognitive vulnerability factor in predicting the increasing symptoms over time [106]. Focusing on the ED symptoms, negative thoughts about the weight and shape could activate worrying about eating and weight gain as a control strategy and associated negative beliefs and emotions; moreover, the worry about food may be a distraction from the preoccupations regarding self-esteem and interpersonal relations [32]. However, people with ED symptoms might also be worried about factors not strictly connected to the core features of EDs.
Finally, our data showed that age does not moderate the relationship between RNT and eating problems, leading to the hypothesis that the vicious circle among RNT, negative beliefs and emotions and eating behaviors could be independent from the passing of time. However, our data does not allow for further speculations on this issue.
A number of clinical and research implications rose from the findings of the current meta-analysis. Firstly, the assessment of RNT, in terms of worry and rumination, should not be overlooked during the anamnesis of a patient presenting with eating problems. Secondly, it could be important to inform patients presenting with eating problems that RNT is a disadvantageous mechanism that leads to worse clinical outcomes [108]. Thirdly, a treatment aimed to decrease the propensity to engage in RNT [108], such as Metacognitive Therapy [12] and Rumination-Based Therapy [109], should be considered as treatment options for EDs. Moreover, and based on the observed relationship between RNT and eating problems in the general population (ES = 0.69), early intervention in tackling RNT may help prevent more severe forms of problematic eating behaviour. Future research on EDs and eating problems could explore in depth the role of worry and rumination.
The value of this meta-analysis should be interpreted considering the strengths and limitations of the included studies. A significant strength is that the investigation of the relationship between worry, rumination and EDs was conducted across different subtypes of EDs, rather than in a specific ED, emphasizing the role of RNT in EDs. Some limitations should be also considered. The instruments used in the reviewed studies to evaluate the worry and rumination are not homogeneous: some studies used an instrument specific for ED (Ruminative Response Scale for Eating Disorders, RRS-ED); others used generic instruments (Ruminative Response Scale, RRS; Penn State Worry Questionnaire, PSWQ) or carried out an experiment. The majority of the studies were retrospective; hence, they are subject to a possible recall bias. Furthermore, the sample sizes were often small and composed only of female participants. Moderator analyses could be affected by this specific limitation. Thus, the analyses on moderators should be considered to be exploratory in nature. Moreover, focusing exclusively on published studies entails that the information about negative results is likely to be lost [110].
5. Conclusions
In conclusion, RNT represents a transdiagnostic phenomenon also involved in EDs. Future directions for research should include studies that: (1) explore in depth the worry and rumination in BED, since most studies have focused on AN and BN; (2) evaluate the relationship between RNT and EDs considering the possible confounder variables such as anxiety and depression [63,111]; (3) explore the relationship between RNT and negative emotion in EDs and (4) include longitudinal designs.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm10112448/s1, Table S1: Quality Assessment for Case-Control Studies using the Newcastle-Ottawa Scale, Table S2: Quality Assessment for Cross Sectional Studies using the Newcastle-Ottawa Scale.
Author Contributions
Conceptualization, acquisition, interpretation of data S.P. and G.M.; formal analysis S.S. (Simona Scaini) and S.P.; writing—original draft preparation S.P., G.M., S.S. (Simona Scaini); writing—review and editing S.P., G.M, S.S. (Simona Scaini), W.S., M.M.S.; supervision G.C., S.S. (Sandra Sassaroli), G.M.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Segerstrom S.C., Stanton A.L., Alden L.E., Shortridge B.E. A Multidimensional Structure for Repetitive Thought: What’s on Your Mind, and How, and How Much? J. Pers. Soc. Psychol. 2003;85:909. doi: 10.1037/0022-3514.85.5.909. [DOI] [PubMed] [Google Scholar]
- 2.Ehring T., Watkins E.R. Repetitive Negative Thinking as a Transdiagnostic Process. Int. J. Cogn. Ther. 2008;1:192–205. doi: 10.1521/ijct.2008.1.3.192. [DOI] [Google Scholar]
- 3.Watkins E.R. Constructive and unconstructive repetitive thought. Psychol. Bull. 2008;134:163–206. doi: 10.1037/0033-2909.134.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borkovec T., Robinson E., Pruzinsky T., DePree J.A. Preliminary exploration of worry: Some characteristics and processes. Behav. Res. Ther. 1983;21:9–16. doi: 10.1016/0005-7967(83)90121-3. [DOI] [PubMed] [Google Scholar]
- 5.Nolen-Hoeksema S., Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The Lorma Prieta earthquake. J. Pers. Soc. Psychol. 1991;65:115–121. doi: 10.1037/0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- 6.Papageorgiou C. Worry and rumination: Styles of persistent negative thinking in anxiety and depression. In: Davey G.C.L., Wells A., editors. Worry and Its Psychological Disorder. John Wiley; Chichester, UK: 2006. pp. 21–40. [Google Scholar]
- 7.Watkins E. Appraisals and strategies associated with rumination and worry. Pers. Individ. Differ. 2004;37:679–694. doi: 10.1016/j.paid.2003.10.002. [DOI] [Google Scholar]
- 8.Olatunji B.O., Naragon-Gainey K., Wolitzky-Taylor K.B. Specificity of Rumination in Anxiety and Depression: A Multimodal Meta-Analysis. Clin. Psychol. 2013;20:225–257. doi: 10.1111/cpsp.12037. [DOI] [Google Scholar]
- 9.Chorpita B.F., Tracey S.A., Brown T.A., Collica T.J., Barlow D.H. Assessment of worry in children and adolescents: An adaptation of the Penn State Worry Questionnaire. Behav. Res. Ther. 1997;35:569–581. doi: 10.1016/S0005-7967(96)00116-7. [DOI] [PubMed] [Google Scholar]
- 10.Muris P., Meesters C., Merckelbach H., Sermon A., Zwakhalen S. Worry in Normal Children. J. Am. Acad. Child Psychiatry. 1998;37:703–710. doi: 10.1097/00004583-199807000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Perrin S., Last C.G. Worrisome thoughts in children referred for anxiety disorder. J. Clin. Child Adolesc. Psychol. 1997;26:181–189. doi: 10.1207/s15374424jccp2602_6. [DOI] [PubMed] [Google Scholar]
- 12.Wells A. Metacognitive Therapy for Anxiety and Depression. The Guilford Press; New York, NY, USA: 2009. [Google Scholar]
- 13.Andrews V.H., Borkovec T. The differential effects of inductions of worry, somatic anxiety, and depression on emotional experience. J. Behav. Ther. Exp. Psychiatry. 1988;19:21–26. doi: 10.1016/0005-7916(88)90006-7. [DOI] [PubMed] [Google Scholar]
- 14.Chelminski I., Zimmerman M. Pathological worry in depressed and anxious patients. J. Anxiety Disord. 2003;17:533–546. doi: 10.1016/S0887-6185(02)00246-3. [DOI] [PubMed] [Google Scholar]
- 15.Starcevic V. Pathological worry in major depression: A preliminary report. Behav. Res. Ther. 1995;33:55–56. doi: 10.1016/0005-7967(93)E0028-4. [DOI] [PubMed] [Google Scholar]
- 16.Calmes C.A., Roberts J.E. Repetitive Thought and Emotional Distress: Rumination and Worry as Prospective Predictors of Depressive and Anxious Symptomatology. Cogn. Ther. Res. 2007;31:343–356. doi: 10.1007/s10608-006-9026-9. [DOI] [Google Scholar]
- 17.Clark D.M., Wells A. A cognitive model of social phobia. In: Heimberg R., Liebowitz M., Hope D.A., Schneier F.R., editors. Social Phobia: Diagnosis, Assessment and Treatment. Guilford Press; New York, NY, USA: 1995. [Google Scholar]
- 18.Fresco D.M., Frankel A.N., Mennin D.S., Turk C.L., Heimberg R.G. Distinct and Overlapping Features of Rumination and Worry: The Relationship of Cognitive Production to Negative Affective States. Cogn. Ther. Res. 2002;26:179–188. doi: 10.1023/A:1014517718949. [DOI] [Google Scholar]
- 19.Harrington J.A., Blankenship V. Ruminative Thoughts and Their Relation to Depression and Anxiety. J. Appl. Soc. Psychol. 2002;32:465–485. doi: 10.1111/j.1559-1816.2002.tb00225.x. [DOI] [Google Scholar]
- 20.Kashdan T.B., Roberts J.E. Social anxiety, depressive symptoms, and post-event rumination: Affective consequences and social contextual influences. J. Anxiety Disord. 2007;21:284–301. doi: 10.1016/j.janxdis.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 21.McLaughlin K.A., Nolen-Hoeksema S. Rumination as a transdiagnostic factor in depression and anxiety. Behav. Res. Ther. 2011;49:186–193. doi: 10.1016/j.brat.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mellings T.M., Alden L.E. Cognitive processes in social anxiety: The effects of self-focus, rumination and anticipatory processing. Behav. Res. Ther. 2000;38:243–257. doi: 10.1016/S0005-7967(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 23.de Silveira M.É., Jr., Kauer-Sant’Anna M. Rumination in bipolar disorder: A systematic review. Rev. Bras. Psiquiatr. 2015;37:256–263. doi: 10.1590/1516-4446-2014-1556. [DOI] [PubMed] [Google Scholar]
- 24.Vassilopoulos S.P. Social anxiety and ruminative self-focus. J. Anxiety Disord. 2008;22:860–867. doi: 10.1016/j.janxdis.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 25.Caselli G., Ferretti C., Leoni M., Rebecchi D., Rovetto F., Spada M.M. Rumination as a predictor of drinking behaviour in alcohol abusers: A prospective study. Addiction. 2010;105:1041–1048. doi: 10.1111/j.1360-0443.2010.02912.x. [DOI] [PubMed] [Google Scholar]
- 26.Devynck F., Kornacka M., Sgard F., Douilliez C. Repetitive Thinking in Alcohol-Dependent Patients. Subst. Use Misuse. 2017;52:108–118. doi: 10.1080/10826084.2016.1222621. [DOI] [PubMed] [Google Scholar]
- 27.Halari R., Premkumar P., Farquharson L., Fannon D., Kuipers E., Kumari V. Rumination and Negative Symptoms in Schizophrenia. J. Nerv. Ment. Dis. 2009;197:703–706. doi: 10.1097/NMD.0b013e3181b3af20. [DOI] [PubMed] [Google Scholar]
- 28.Cooper Z., Fairburn C. The eating disorder examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. Int. J. Eat. Disord. 1987;6:1–8. doi: 10.1002/1098-108X(198701)6:1<1::AID-EAT2260060102>3.0.CO;2-9. [DOI] [Google Scholar]
- 29.Fairburn C.G., Cooper Z., Shafran R. Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behav. Res. Ther. 2003;41:509–528. doi: 10.1016/S0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- 30.Smith K.E., Mason T.B., Lavender J.M. Rumination and eating disorder psychopathology: A meta-analysis. Clin. Psychol. Rev. 2018;61:9–23. doi: 10.1016/j.cpr.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Napolitano M.A., Himes S. Race, weight, and correlates of binge eating in female college students. Eat. Behav. 2011;12:29–36. doi: 10.1016/j.eatbeh.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 32.Sassaroli S., Bertelli S., DeCoppi M., Crosina M., Milos G., Ruggiero G. Worry and eating disorders: A psychopathological association. Eat. Behav. 2005;6:301–307. doi: 10.1016/j.eatbeh.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 33.Sternheim L., Startup H., Saeidi S., Morgan J., Hugo P., Russell A., Schmidt U. Understanding catastrophic worry in eating disorders: Process and content characteristics. J. Behav. Ther. Exp. Psychiatry. 2012;43:1095–1103. doi: 10.1016/j.jbtep.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 34.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 35.American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. American Psychiatric Association; Washington, DC, USA: 1980. [Google Scholar]
- 36.American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. American Psychiatric Association; Washington, DC, USA: 1987. [Google Scholar]
- 37.American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; Washington, DC, USA: 1994. [Google Scholar]
- 38.American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; Washington, DC, USA: 2000. [Google Scholar]
- 39.American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; Washington, DC, USA: 2013. [Google Scholar]
- 40.Spitzer R.L., Endicott J., Robins E. Research Diagnostic Criteria: Rationale and reliability. Arch. Gen. Psychiatry. 1978;35:773. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization . Manual of the 28. International Statistical Classification of Diseases, Injuries, and Causes of Death. World Health Organization; Geneva, Switzerland: 1948. Sixth Revision of the International Lists of Diseases and Causes of Death, Adopted 1948. [Google Scholar]
- 42.World Health Organization . Manual of the 30. International Statistical Classification of Diseases, Injuries, and Causes of Death. World Health Organization; Geneva, Switzerland: 1957. Based on the Recommendations of the Seventh Revision Conference, 1955, and Adopted by the Ninth World Health Assembly under the WHO Nomenclature Regulations. [Google Scholar]
- 43.World Health Organization . Manual of the 32. International Statistical Classification of Diseases, Injuries, and Causes of Death. World Health Organization; Geneva, Switzerland: 1967. Based on Recommendations of the Eighth Revision Conference, 1965, and Adopted by the Nineteenth World Health Assembly. [Google Scholar]
- 44.World Health Organization . Manual of the 34. International Classification of Diseases, Injuries, and Causes of Death. World Health Organization; Geneva, Switzerland: 1977. Based on the Recommendations of the Ninth Revision Conference, 1975, and Adopted by the Twenty-Ninth World Health Assembly. [Google Scholar]
- 45.World Health Organization . The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. World Health Organization; Geneva, Switzerland: 1992. [Google Scholar]
- 46.Mansueto G., Caselli G., Ruggiero G.M., Sassaroli S. Metacognitive beliefs and childhood adversities: An overview of the literature. Psychol. Health Med. 2018;24:542–550. doi: 10.1080/13548506.2018.1550258. [DOI] [PubMed] [Google Scholar]
- 47.Zhu C., Sun X., So S.H.-W. Associations between belief inflexibility and dimensions of delusions: A meta-analytic review of two approaches to assessing belief flexibility. Br. J. Clin. Psychol. 2018;57:59–81. doi: 10.1111/bjc.12154. [DOI] [PubMed] [Google Scholar]
- 48.Palmieri S., Mansueto G., Ruggiero G.M., Caselli G., Sassaroli S., Spada M.M. Metacognitive beliefs across eating disorders and eating behaviours: A systematic review. Clin. Psychol. Psychother. 2021 doi: 10.1002/cpp.2573. [DOI] [PubMed] [Google Scholar]
- 49.Herzog R., Álvarez-Pasquin M.J., Díaz C., Del Barrio J.L., Estrada J.M., Gil Á. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:154. doi: 10.1186/1471-2458-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wells G., Shea B., O’Connell D., Peterson J.E., Welch V., Losos M., Tugwell P. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis. Ottawa Hospital Research Institute; Ottawa, ON, Canada: 2010. [(accessed on 16 March 2021)]. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [DOI] [Google Scholar]
- 51.Hakamata Y., Lissek S., Bar-Haim Y., Britton J.C., Fox N.A., Leibenluft E., Ernst M., Pine D.S. Attention Bias Modification Treatment: A Meta-Analysis Toward the Establishment of Novel Treatment for Anxiety. Biol. Psychiatry. 2010;68:982–990. doi: 10.1016/j.biopsych.2010.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Scaini S., Belotti R., Ogliari A., Battaglia M. A comprehensive meta-analysis of cognitive-behavioral interventions for social anxiety disorder in children and adolescents. J. Anxiety Disord. 2016;42:105–112. doi: 10.1016/j.janxdis.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 53.Duval S., Tweedie R. Trim and Fill: A Simple Funnel-Plot-Based Method of Testing and Adjusting for Publication Bias in Meta-Analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 54.Rosenthal R. The file drawer problem and tolerance for null results. Psychol. Bull. 1979;86:638. doi: 10.1037/0033-2909.86.3.638. [DOI] [Google Scholar]
- 55.Juffer F., Van Ijzendoorn M.H. Adoptees do not lack self-esteem: A meta-analysis of studies on self-esteem of transracial, international, and domestic adoptees. Psychol. Bull. 2007;133:1067. doi: 10.1037/0033-2909.133.6.1067. [DOI] [PubMed] [Google Scholar]
- 56.Borenstein M., Hedges L.V., Higgins J., Rothstein H.R. References. John Wiley & Sons, Ltd.; Hoboken, NJ, USA: 2009. pp. 409–414. [Google Scholar]
- 57.González M., Ibáñez I., Barrera A. Rumination, worry and negative problem orientation: Transdiagnostic processes of anxiety, eating behavior and mood disorders. Acta Colomb. Psicol. 2017;20:42–52. [Google Scholar]
- 58.Kollei I., Brunhoeber S., Rauh E., De Zwaan M., Martin A. Body image, emotions and thought control strategies in body dysmorphic disorder compared to eating disorders and healthy controls. J. Psychosom. Res. 2012;72:321–327. doi: 10.1016/j.jpsychores.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 59.Naumann E., Tuschen-Caffier B., Voderholzer U., Caffier D., Svaldi J. Rumination but not distraction increases eating-related symptoms in anorexia and bulimia nervosa. J. Abnorm. Psychol. 2015;124:412. doi: 10.1037/abn0000046. [DOI] [PubMed] [Google Scholar]
- 60.Sapuppo W., Ruggiero G.M., Caselli G., Sassaroli S. The Body of Cognitive and Metacognitive Variables in Eating Disorders: Need of Control, Negative Beliefs about Worry Uncontrollability and Danger, Perfectionism, Self-esteem and Worry. Isr. J. Psychiatry Relat. Sci. 2018;55:55–63. [PubMed] [Google Scholar]
- 61.Troop N.A., Treasure J.L. Psychosocial factors in the onset of eating disorders: Responses to life-events and difficulties. Br. J. Med. Psychol. 1997;70:373–385. doi: 10.1111/j.2044-8341.1997.tb01913.x. [DOI] [PubMed] [Google Scholar]
- 62.Cowdrey F.A., Park R.J. The role of experiential avoidance, rumination and mindfulness in eating disorders. Eat. Behav. 2012;13:100–105. doi: 10.1016/j.eatbeh.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 63.Rawal A., Park R.J., Williams J.M.G. Rumination, experiential avoidance, and dysfunctional thinking in eating disorders. Behav. Res. Ther. 2010;48:851–859. doi: 10.1016/j.brat.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang S.B., Borders A. The unique effects of angry and depressive rumination on eating-disorder psychopathology and the mediating role of impulsivity. Eat. Behav. 2018;29:41–47. doi: 10.1016/j.eatbeh.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 65.Mason T.B., Lewis R.J. Examining social support, rumination, and optimism in relation to binge eating among Caucasian and African–American college women. Eat. Weight. Disord. 2017;22:693–698. doi: 10.1007/s40519-016-0300-x. [DOI] [PubMed] [Google Scholar]
- 66.Startup H., Lavender A., Oldershaw A., Stott R., Tchanturia K., Treasure J., Schmidt U. Worry and Rumination in Anorexia Nervosa. Behav. Cogn. Psychother. 2013;41:301–316. doi: 10.1017/S1352465812000847. [DOI] [PubMed] [Google Scholar]
- 67.Zarychta K., Mullan B., Kruk M., Luszczynska A. A vicious cycle among cognitions and behaviors enhancing risk for eating disorders. BMC Psychiatry. 2017;17:154. doi: 10.1186/s12888-017-1328-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Crino N., Touyz S., Rieger E. How eating disordered and non-eating disordered women differ in their use (and effectiveness) of cognitive self-regulation strategies for managing negative experiences. Eat. Weight. Disord. 2019;24:897–904. doi: 10.1007/s40519-017-0448-z. [DOI] [PubMed] [Google Scholar]
- 69.Hartmann A.S., Cordes M., Hirschfeld G., Vocks S. Affect and worry during a checking episode: A comparison of individuals with symptoms of obsessive-compulsive disorder, anorexia nervosa, bulimia nervosa, body dysmorphic disorder, illness anxiety disorder, and panic disorder. Psychiatry Res. 2019;272:349–358. doi: 10.1016/j.psychres.2018.12.132. [DOI] [PubMed] [Google Scholar]
- 70.Connolly A.M., Rieger E., Caterson I. Binge eating tendencies and anger coping: Investigating the confound of trait neuroticism in a non-clinical sample. Eur. Eat. Disord. Rev. 2007;15:479–486. doi: 10.1002/erv.765. [DOI] [PubMed] [Google Scholar]
- 71.Nolen-Hoeksema S., Stice E., Wade E., Bohon C. Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in female adolescents. J. Abnorm. Psychol. 2007;116:198–207. doi: 10.1037/0021-843X.116.1.198. [DOI] [PubMed] [Google Scholar]
- 72.Harrell Z.A.T., Jackson B. Thinking Fat and Feeling Blue: Eating Behaviors, Ruminative Coping, and Depressive Symptoms in College Women. Sex Roles. 2008;58:658–665. doi: 10.1007/s11199-007-9388-9. [DOI] [Google Scholar]
- 73.Selby E.A., Anestis M.D., Joiner T.E. Understanding the relationship between emotional and behavioral dysregulation: Emotional cascades. Behav. Res. Ther. 2008;46:593–611. doi: 10.1016/j.brat.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 74.Aldao A., Nolen-Hoeksema S. Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behav. Res. Ther. 2010;48:974–983. doi: 10.1016/j.brat.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 75.Holm-Denoma J.M., Hankin B.L. Perceived Physical Appearance Mediates the Rumination and Bulimic Symptom Link in Adolescent Girls. J. Clin. Child Adolesc. Psychol. 2010;39:537–544. doi: 10.1080/15374416.2010.486324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Verplanken B., Tangelder Y. No body is perfect: The significance of habitual negative thinking about appearance for body dissatisfaction, eating disorder propensity, self-esteem and snacking. Psychol. Health. 2011;26:685–701. doi: 10.1080/08870441003763246. [DOI] [PubMed] [Google Scholar]
- 77.Gordon K.H., Holm-Denoma J.M., Troop-Gordon W., Sand E. Rumination and body dissatisfaction interact to predict concurrent binge eating. Body Image. 2012;9:352–357. doi: 10.1016/j.bodyim.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 78.Kelly N.R., Lydecker J., Mazzeo S.E. Positive cognitive coping strategies and binge eating in college women. Eat. Behav. 2012;13:289–292. doi: 10.1016/j.eatbeh.2012.03.012. [DOI] [PubMed] [Google Scholar]
- 79.Hilt L.M., Roberto C.A., Nolen-Hoeksema S. Rumination mediates the relationship between peer alienation and eating pathology in young adolescent girls. Eat. Weight. Disord. 2013;18:263–267. doi: 10.1007/s40519-013-0042-y. [DOI] [PubMed] [Google Scholar]
- 80.Svaldi J., Naumann E. Effects of Rumination and Acceptance on Body Dissatisfaction in Binge Eating Disorder. Eur. Eat. Disord. Rev. 2014;22:338–345. doi: 10.1002/erv.2312. [DOI] [PubMed] [Google Scholar]
- 81.Mason T.B., Lewis R.J. Minority Stress and Binge Eating Among Lesbian and Bisexual Women. J. Homosex. 2015;62:971–992. doi: 10.1080/00918369.2015.1008285. [DOI] [PubMed] [Google Scholar]
- 82.Breithaupt L., Rallis B., Mehlenbeck R., Kleiman E. Rumination and self-control interact to predict bulimic symptomatology in college students. Eat. Behav. 2016;22:1–4. doi: 10.1016/j.eatbeh.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 83.Jungmann S.M., Vollmer N., Selby E.A., Witthöft M. Understanding Dysregulated Behaviors and Compulsions: An Extension of the Emotional Cascade Model and the Mediating Role of Intrusive Thoughts. Front. Psychol. 2016;7:994. doi: 10.3389/fpsyg.2016.00994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Maraldo T.M., Zhou W., Dowling J., Wal J.S.V. Replication and extension of the dual pathway model of disordered eating: The role of fear of negative evaluation, suggestibility, rumination, and self-compassion. Eat. Behav. 2016;23:187–194. doi: 10.1016/j.eatbeh.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 85.Naumann E., Tuschen-Caffier B., Voderholzer U., Svaldi J. Spontaneous Emotion Regulation in Anorexia and Bulimia Nervosa. Cogn. Ther. Res. 2016;40:304–313. doi: 10.1007/s10608-015-9723-3. [DOI] [Google Scholar]
- 86.Seidel M., Petermann J., Diestel S., Ritschel F., Boehm I., King J.A., Geisler D., Bernardoni F., Roessner V., Goschke T., et al. A naturalistic examination of negative affect and disorder-related rumination in anorexia nervosa. Eur. Child Adolesc. Psychiatry. 2016;25:1207–1216. doi: 10.1007/s00787-016-0844-3. [DOI] [PubMed] [Google Scholar]
- 87.Opwis M., Salewski C., Schmidt J., Martin A. Gender differences in eating behavior and eating pathology: The mediating role of rumination. Appetite. 2017;110:103–107. doi: 10.1016/j.appet.2016.12.020. [DOI] [PubMed] [Google Scholar]
- 88.Wang S.B., Borders A. Rumination mediates the associations between sexual minority stressors and disordered eating, particularly for men. Eat. Weight. Disord. 2017;22:699–706. doi: 10.1007/s40519-016-0350-0. [DOI] [PubMed] [Google Scholar]
- 89.Wang S.B., Lydecker J.A., Grilo C.M. Rumination in Patients with Binge-Eating Disorder and Obesity: Associations with Eating-Disorder Psychopathology and Weight-bias Internalization. Eur. Eat. Disord. Rev. 2017;25:98–103. doi: 10.1002/erv.2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dondzilo L., Rieger E., Palermo R., Byrne S., Bell J. Correction: The mediating role of rumination in the relation between attentional bias towards thin female bodies and eating disorder symptomatology. PLoS ONE. 2018;13:e0196143. doi: 10.1371/journal.pone.0196143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Van Durme K., Goossens L., Bosmans G., Braet C. The Role of Attachment and Maladaptive Emotion Regulation Strategies in the Development of Bulimic Symptoms in Adolescents. J. Abnorm. Child Psychol. 2017;46:881–893. doi: 10.1007/s10802-017-0334-1. [DOI] [PubMed] [Google Scholar]
- 92.Birmachu A.M., Heidelberger L., Klem J. Rumination and perceived social support from significant others interact to predict eating disorder attitudes and behaviors in university students. J. Am. Coll. Health. 2019 doi: 10.1080/07448481.2019.1682001. [DOI] [PubMed] [Google Scholar]
- 93.Fresnics A.A., Wang S.B., Borders A. The unique associations between self-compassion and eating disorder psychopathology and the mediating role of rumination. Psychiatry Res. 2019;274:91–97. doi: 10.1016/j.psychres.2019.02.019. [DOI] [PubMed] [Google Scholar]
- 94.Hernando A., Pallás R., Cebolla A., García-Campayo J., Hoogendoorn C.J., Roy J.F. Mindfulness, rumination, and coping skills in young women with Eating Disorders: A comparative study with healthy controls. PLoS ONE. 2019;14:e0213985. doi: 10.1371/journal.pone.0213985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Smith K.E., Mason T.B., Anderson N.L., Lavender J.M. Unpacking cognitive emotion regulation in eating disorder psychopathology: The differential relationships between rumination, thought suppression, and eating disorder symptoms among men and women. Eat. Behav. 2019;32:95–100. doi: 10.1016/j.eatbeh.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 96.Branley-Bell D., Talbot C.V. Exploring the impact of the COVID-19 pandemic and UK lockdown on individuals with expe-rience of eating disorders. J. Eat. Disord. 2020;8:1–12. doi: 10.1186/s40337-020-00319-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Martino F., Caselli G., Berardi D., Fiore F., Marino E., Menchetti M., Prunetti E., Ruggiero G.M., Sasdelli A., Selby E., et al. Anger rumination and aggressive behaviour in borderline personality disorder. Pers. Ment. Health. 2015;9:277–287. doi: 10.1002/pmh.1310. [DOI] [PubMed] [Google Scholar]
- 98.Salters-Pedneault K., Roemer L., Tull M., Rucker L., Mennin D.S. Evidence of Broad Deficits in Emotion Regulation Associated with Chronic Worry and Generalized Anxiety Disorder. Cogn. Ther. Res. 2006;30:469–480. doi: 10.1007/s10608-006-9055-4. [DOI] [Google Scholar]
- 99.Vann A., Strodl E., Anderson E. Thinking about internal states, a qualitative investigation into metacognitions in women with eating disorders. J. Eat. Disord. 2013;1:22. doi: 10.1186/2050-2974-1-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Vinai P., Da Ros A., Cardetti S., Casey H., Studt S., Gentile N., Tagliabue A., Vinai L., Vinai P., Bruno C., et al. The DSM-5 effect: Psychological characteristics of new patients affected by Binge Eating Disorder following the criteria of the DSM-5 in a sample of severe obese patients. Eat. Weight Disord. 2016;21:107–113. doi: 10.1007/s40519-015-0218-8. [DOI] [PubMed] [Google Scholar]
- 101.Wells A., Matthews G. Modelling cognition in emotional disorder: The S-REF model. Behav. Res. Ther. 1996;34:881–888. doi: 10.1016/S0005-7967(96)00050-2. [DOI] [PubMed] [Google Scholar]
- 102.Wells A. Emotional Disorders and Metacognition: Innovative Cognitive Therapy. Wiley; Chichester, UK: 2000. [Google Scholar]
- 103.Spada M.M., Caselli G., Nikčević A.V., Wells A. Metacognition in addictive behaviors. Addict. Behav. 2015;44:9–15. doi: 10.1016/j.addbeh.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 104.Spada M.M., Caselli G., Fernie B.A., Manfredi C., Boccaletti F., Dallari G., Gandini F., Pinna E., Ruggiero G.M., Sassaroli S. Desire thinking: A risk factor for binge eating? Eat. Behav. 2015;18:48–53. doi: 10.1016/j.eatbeh.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 105.Mansueto G., Martino F., Palmieri S., Scaini S., Ruggiero G.M., Sassaroli S., Caselli G. Desire Thinking across addictive behaviours: A systematic review and meta-analysis. Addict. Behav. 2019;98:106018. doi: 10.1016/j.addbeh.2019.06.007. [DOI] [PubMed] [Google Scholar]
- 106.Hong R.Y. Worry and rumination: Differential associations with anxious and depressive symptoms and coping behavior. Behav. Res. Ther. 2007;45:277–290. doi: 10.1016/j.brat.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 107.Hoyer J., Gloster A.T., Herzberg P.Y. Is worry different from rumination? Yes, it is more predictive of psychopathology! GMS Psycho Soc. Med. 2009;6 doi: 10.3205/psm000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kaplan D.M., Palitsky R., Carey A.L., Crane T.E., Havens C.M., Medrano M.R., Reznik S.J., Sbarra D.A., O’Connor M.-F. Maladaptive repetitive thought as a transdiagnostic phenomenon and treatment target: An integrative review. J. Clin. Psychol. 2018;74:1126–1136. doi: 10.1002/jclp.22585. [DOI] [PubMed] [Google Scholar]
- 109.Watkins E.R. Rumination-Focused Cognitive-Behavioral Therapy for Depression. Guilford Publications; New York, NY, USA: 2018. [Google Scholar]
- 110.Fava G.A. Meta-Analyses and Conflict of Interest. CNS Drugs. 2012;26:93–96. doi: 10.2165/11587940-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 111.Cowdrey F.A., Park R.J. Assessing rumination in eating disorders: Principal component analysis of a minimally modified ruminative response scale. Eat. Behav. 2011;12:321–324. doi: 10.1016/j.eatbeh.2011.08.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.