Abstract
Background: College students are among the heaviest users of smartphones and the Internet, and there is growing concern regarding problematic Internet (PIU) and smartphone use (PSU). A subset of adverse childhood experiences, household dysfunction [(HHD) e.g.; parental substance use, mental illness, incarceration, suicide, intimate partner violence, separation/divorce, homelessness], are robust predictors of behavioral disorders; however, few studies have investigated the link between HHD and PIU and PSU and potential protective factors, such as social support, among students. Methods: Data are from a diverse California student sample (N = 1027). The Smartphone Addiction Scale—Short Version and Internet Addiction Test assessed dimensions of addiction. Regression models tested associations between students’ level of HHD (No HHD, 1–3 HHD, ≥4 HHD) and PSU and PIU, and the role of extrafamilial social support in these relationships, adjusting for age, gender, ethnicity, SES, employment loss due to COVID-19, and depression. Results: Compared to students reporting no HHD, students with ≥4 HHD had twice the odds (AOR: 2.03, 95% CI: 1.21–3.40) of meeting criteria for PSU, while students with 1–3 HHD and ≥4 HHD had three and six times the odds of moderate to severe PIU (AORs: 2.03–2.46, CI:1.21–3.96) after adjusting for covariates. Extrafamilial social support was inversely associated with PIU and moderated the HHD–PSU association for students with 1–3 HHD. Conclusion: Students exposed to HHD may be especially vulnerable to developing behavioral addictions such as PSU and PIU. Extrafamilial social support offset the negative effects of HHD for PSU among the moderate risk group; implications for prevention efforts are discussed.
Keywords: adverse childhood experiences, Internet addiction, problematic smartphone use, social support, college students
1. Introduction
College students, and young adults generally, are the most likely population to go online and own digital devices such as smart phones and are among the heaviest users of the Internet [1,2,3]. Historically, students’ Internet activities have centered around research, communicating, browsing, and shopping [4]; however, with the proliferation of online applications and social media platforms, there has been a dramatic increase in the amount of time students spend online. While there are many advantages to accessing the Internet, there is a growing interest in the relationship between digital behaviors and young adults’ psychological wellbeing, the potential for excessive Internet use, and whether the features of compulsive use are consistent with attributes of other addictions [5,6,7]. Excessive or compulsive Internet use has been associated with loneliness and isolation [8,9,10], online gaming, gambling, and sex addictions [11,12], and prospectively with risk behaviors such as substance use [13]. Given the increasing concern over the potential for, and effects of, excessive use, investigating factors that exacerbate or inhibit vulnerability for problematic or compulsive Internet use has become an important area of Internet research, and one that has implications for the health and wellbeing of college students.
In a similar vein, devices such as smartphones that increase connectivity to the Internet have become essential tools for most Americans. Smartphones are mobile phones that perform many of the functions of a computer, have touch screen interface, and offer access to applications. Over 90% of American young adults now own a smart phone [3], and many of them acknowledge that they could not imagine their life without one [14]. Although smartphones offer easy access to the Internet and enhanced communication [15,16], there is mounting evidence of a potential for problematic/addictive smartphone use (PSU) [17,18,19]. As scientific understanding of behavioral addictions evolves, addictions such as Internet gambling have been added to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Although problematic Internet use (PIU) and PSU are not currently included in the DSM-5, research suggests a strong potential for compulsive use among younger populations, and there is mounting evidence suggesting that compulsive use is linked to psychological disorders [20,21,22], stress [23,24], sleep difficulties [25], and compromised academic performance [7,26,27,28]. Among students internationally [29,30,31,32,33], PIU and PSU prevalence are estimated to be between 10% and 44% and between 5% and 28%, respectively [34,35,36].
Problematic or compulsive Internet and smartphone use has been conceptualized as excessive, maladaptive use that a person is unable to regulate despite negative consequences, such as failing to meet responsibilities and obligations, a preoccupation with the Internet, and concealing and feeling guilty about use—features that are typical of substance dependence and addiction disorders [37,38,39,40]. According to Griffiths’ six-component model of addiction, addictions—whether substance or behavioral—share common characteristics; salience, mood modification, tolerance, withdrawal, conflict, and relapse that develop through similar biopsychosocial pathways [41,42]. Salience indicates a preoccupation with the Internet or digital device and “craving” the behavior; mood modification refers to engaging in the behavior to elevate mood or to avoid thinking about other aspects of life [43]; tolerance suggests that the amount of engagement in the behavior required to produce a desired experience increases over time [44]; withdrawal suggests the presence of physiological and psychological symptoms when decreasing or abstaining from the behavior; and conflict refers to compromised personal relationships, work or educational goals.
Among the most robust predictors of substance and behavioral addictions are adverse childhood experiences (ACE), a set of highly correlated traumatic and negative events experienced prior to age 18 that heighten risk for compromised health in adulthood [45,46]. A subset of ACE, and the focus of this study, is household dysfunction (HHD), defined as parent/caregiver stressors or behaviors (e.g., parental divorce, mental illness, suicide, substance use, intimate partner violence, homelessness, and incarceration). Family-based stressors (ACE) are a form of toxic stress that over time can damage a child’s stress response system, the processes that limit the intensity and duration of the stress response [47,48], and alter neurological structures and functioning [47,48]. In conjunction with these physiological changes, unpredictable and inconsistent parenting and home environments can impair the cognitive and emotional processes involved in self-regulation [49], self-esteem [50], and decision making that in turn increase vulnerability to maladaptive coping behaviors and addiction [51,52,53].
The effects of HHD on processes that promote or inhibit healthy behaviors may be especially relevant during the college years when students must learn to balance the demands of their academic goals, adapt to their increasing autonomy from family, assume greater responsibilities, and begin planning for their future. While the college experience can be a time of exploration and transformation, the enhanced susceptibility for engaging in risky behaviors during this transition period can threaten students’ ability to successfully obtain a degree, develop enduring social bonds, and participate in the work force [54,55,56,57,58].
There is substantial evidence linking family environments to socioeconomic disadvantage, academic challenges, and psychiatric morbidity over the life course [59,60], and studies have investigated the association between specific aspects of the family environment (e.g., sexual abuse or family violence and parent–child communication) and PIU, PSU, or individual Internet behaviors [61,62,63,64,65]. This work has found that young people who report a form of maltreatment or family discord are at greater risk for PIU and PSU or specific Internet behaviors (e.g., online gaming) than young adults without this history [36,66,67,68]. However, despite evidence that cumulative HHD is highly predictive of early adult developmental deficits, compromised mental health, and maladaptive behaviors, especially behaviors with an addictive potential [69,70,71,72], research assessing the association between household stressors (HHD) and health-compromising behaviors among US college students has lagged behind that conducted in other countries [29,30,31,32,33]. Within this limited body of work, there is evidence of a graded relationship (e.g., as the number of adversities/stressors increase, so does the risk for poorer outcomes) between HHD and depression, substance use, and alcohol-related consequences [73,74,75,76].
In contrast, and in the context of resilience, the buffering hypothesis suggests that if individuals facing chronic adversity have sufficient social or individual resources, they will be less vulnerable to maladaptive coping behaviors and experience fewer of the short and long-term pathogenic effects of stressful events [77]. In fact, developing social relationships is an important aspect of adolescent and early adult development [78,79] and perceived social support, a central feature of health and wellbeing across the lifespan [80,81,82], and it can promote wellbeing, reduce morbidity and mortality [83,84], and diminish the harmful effects of ACE [85].
Despite (a) young adults’ vulnerability for risky behavior, (b) the high prevalence of ACE documented in student populations, (c) and the pervasive use of the Internet and digital devices among this age group, the association between cumulative HHD and PIU and PSU has not been well studied in the US college population. Although research suggests that social support and relationships with important others can offset the negative effects of early adversity, whether social support buffers the association between HHD and PIU and PSU has yet to be determined. To address these gaps in the literature, the present study investigated the association between HHD and PIU and PSU with two widely used, validated instruments that have established thresholds of problematic Internet and smartphone use. The Smartphone Addiction Scale—Short Version (SAS-SV) developed by Kwon et al. [17] captures four of the six components of addiction [41]—conflict, withdrawal, tolerance, and salience—while the Internet Addiction Test (IAT) developed by Young [39] assesses salience, withdrawal, secrecy/concealment, lack of control, conflict, mood modification, and developing online relationships to replace relationships that may be missing or unfulfilling in offline settings. We hypothesized that students with a history of HHD, and especially multiple household stressors, would have higher odds of (H1) PIU and (H2) PSU. We also anticipated that perceived social support from friends would be protective such that (H3) students with a history of HHD who report high perceived social support from friends would have lower odds of PIU and PSU than their peers with the same history of HHD, but who have low perceived social support from friends.
2. Materials and Methods
A sample of 1027 students enrolled at a public university in Southern California agreed to participate in this study. An email containing a link to the survey was sent to randomly selected undergraduate and graduate classes in October 2020 and was open through December 2020 while the university maintained distance learning due to the COVID-19 pandemic. Approximately 60% of classrooms that were invited agreed to participate. Students who participated received information on study objectives and procedures and consented online. All aspects of the study were approved by the university IRB.
2.1. Measures
Sex was assessed with one question, “What sex were you assigned at birth, such as on an original birth certificate?” and coded male = 1 and female = 0. Ethnicity was measured with one question that asked, “How do you usually describe yourself?” and coded Non-Hispanic White = 0, Non-Hispanic Black = 1 Mexican = 2, Other Hispanic = 3, Asian = 4, and other and Bi/Multiracial = 5. Age was a continuous variable, and COVID-19 financial hardship was a continuous variable calculated by subtracting the hours worked after the COVID-19 shutdown from the hours worked prior to the shutdown. Due to the strong correlation between depression and PIU and PSU [6,7,86,87], we included an indicator of depression derived from the 10-item Center for Epidemiological Studies Depression Scale [88] to reduce confounding.
Perceived social support from friends was assessed with items from the Multidimensional Scale of Perceived Social Support developed by Zimet [89] that has been validated in diverse populations. For the purposes of the present study, only perceived social support from friends was used in the present study. Sample items include “My friends really try to help me,” and “I can count on my friends when things go wrong.” Response options were “Agree” coded = 1 or “Disagree” coded = 0. Responses were summed, with higher scores indicating greater perceived social support from friends.
Household dysfunction (HHD) items were adapted from the original ACE study [90]. Questions asked respondents if, prior to age 18, their caregivers misused alcohol, illegal drugs, or prescription drugs, engaged in intimate partner violence, suffered from mental illness, attempted suicide, were separated/divorced, incarcerated, homeless, or if they had stayed in a shelter. Household dysfunction was coded 0 = no HHD, 1 = 1–3 HHD, and 2 = ≥4 HHD.
Problematic smartphone use was measured using the Smartphone Addiction Scale Short Version (SAS-SV) developed by Kwon et al. [17]. SAS-SV assesses four of the six components of a widely used six-component model of addiction [41]: conflict, withdrawal, tolerance, and salience. Respondents selected options on a six-point Likert scale ranging from “Strongly Disagree” to “Strongly Agree” to statements such as “Missing planned work due to smartphone use” and “Constantly checking my smartphone so as not to miss conversations between other people on Facebook or Twitter”. As recommended by the developers, we adopted a score of 32 out of 60 as the threshold to distinguish high-risk (problematic/addictive) users. PSU was coded = 1 nonproblematic use = 0 (Cronbach alpha = 0.88).
Levels of Internet addiction were assessed using the 20-item Internet Addiction Test (IAT) [39]. The IAT assesses characteristics (e.g., salience, excessive use, neglect of work, anticipation, lack of control, neglect of social life) that are consistent with salience, mood alteration, withdrawal, secrecy, and conflict. Sample items include “How often do you neglect household chores to spend more time online?”, “How often do your grades or school work suffer because of the among of time you spend online?”, “How often do you try to cut down the among of time you spend online and fail?”, and “How often do you try to hide how long you’ve been online?” Response options are on a 5-point Likert scale 0 = Not applicable, 1 = Rarely, 2 = Occasionally, 3 = Frequently, 4 = Often, and 5 = Always (Cronbach’s alpha = 0.92). As recommended by developers, scores ranging from 0 to 30 reflect normal levels of Internet usage, scores ranging from 31 to 49 indicate the presence of mild levels of Internet addiction, scores between 50 and 79 indicate the presence of moderate levels of Internet addiction/compulsivity, and scores between 80 and 100 reflect severe levels of Internet addiction. Because only 13 students reported severe Internet addiction, we collapsed the moderate and severe categories, resulting in a three-level variable coded normal use = 0, mild = 1, and moderate to severe = 2 Internet addiction.
2.2. Analytic Plan
Missing data, a common problem in survey studies, ranged from 3.0% to 8.0% (Table 1). Multiple imputation by chained equations (MICE), an approach outlined by van Buuren, Boshuizen, and Knook [91], was conducted to account for missing items. MICE does not assume a joint multivariate normal distribution, and unlike single imputation, multiple imputation builds into the model the uncertainty/error associated with the missing data and instead uses a separate conditional distribution for each imputed variable [92,93,94]. We used M = 10 imputations as recommended for valid estimates with <10% missing data that reduce sampling error due to imputations [91,95,96]. The uncertainty parameter estimation in the missing data case is the average of the parameter estimate obtained over M = 10 imputed datasets. The variance of estimation is partitioned into the within-imputation variance, which captures typical sampling variability, and the between-imputation variance, which captures the estimation variability due to missing data. Missing data are described in Table 1.
Table 1.
Summary of missing data.
| N = 1273 | Completed | Imputed | Total |
|---|---|---|---|
| Sex | 1027 | 0 | 1027 |
| Age | 1027 | 0 | 1027 |
| Ethnicity | 973 | 54 | 1027 |
| COVID work loss | 1027 | 0 | 1027 |
| Depression | 1027 | 0 | 1027 |
| Peer Support | 991 | 36 | 1027 |
| ACE: Household Dysfunction | 1027 | 0 | 1027 |
| Problematic Internet Use (PIU/IA) | 981 | 46 | 1027 |
| Problematic Smartphone Use (PSU/SA) | 950 | 77 | 1027 |
Note: Complete + Imputed = Total; imputed is the minimum across m of the number of filled-in observations.
A multivariable logistic regression model assessed the associations between HHD and PSU adjusting for age, sex, race/ethnicity, financial hardship due to COVID-19, depression, and peer social support. A second model that included an interaction term (HHD∗peer social support) assessed whether perceptions of peer social support could offset the negative effects of HHD for PSU. Results are reported as odds ratios (OR) and 95% confidence intervals (95% CI).
An ordinal logistic regression model assessed the association between HHD and mild, and moderate to severe IA adjusting for age, sex, race/ethnicity, financial hardship due to COVID-19, depression, and social support from friends. A second model included an interaction term (HHD*peer social support) and tested whether peer support buffered the association between HHD and mild and moderate to severe levels of IA. To understand the association between HHD and each level of IA (normal use, mild addiction, and moderate to severe addiction), the delta method was used to calculate the probability of normal use, mild IA, and moderate to severe IA for HHD categories (none, 1-3 HHD, and ≥4 HHD). All analyses were conducted using STATA v. 15 [97].
3. Results
Over 88% of study participants were between 18 and 29 years old, and approximately 12% of students were 30 years old or older. The majority of respondents were female (78%), and approximately one third of students identified as Mexican (38%), followed by Bi- or Multiracial (17%), Non-Hispanic White (16%), Asian (12%), other Hispanic (12%), and Non-Hispanic Black (4%). Students from the seven colleges on the campus participated. The percentages of respondents enrolled in the College of Education; Science and Mathematics; Engineering and Computer Science; and the Social and Behavioral Sciences were consistent with the university’s published data while the College of Arts, Media, and Communication; Business Economics; Humanities; and Health and Human Development were over or under-represented by 9–15%. Slightly over half the sample acknowledged experiencing some form of household dysfunction, 47% reported one to three household stressors, and 9% reported over four. Regarding Internet and smartphone use, over half of the sample could be classified as having normal levels of Internet use, about 34% as mild IA, and 10% were in the moderate to severe PIU category. Approximately 25% of students were at high risk for PSU (Table 2).
Table 2.
Sample characteristics (N = 1027).
| Biological Sex | Frequency (%) or M (SD) |
|---|---|
| Female | 804 (78.32) |
| Male | 223 (21.68) |
| Age | |
| 17–21 | 417 (40.57) |
| 22–29 | 475 (46.24) |
| 30+ | 135 (13.20) |
| Ethnicity | |
| Mexican | 392 (38.18) |
| Other and Bi-/Multiracial | 172 (16.74) |
| Non-Hispanic White | 169 (16.48) |
| Asian | 125 (12.20) |
| Other Hispanic | 124 (12.03) |
| Non-Hispanic Black | 45 (4.37) |
| Perceived Peer Social Support (MSPSS) | 9.59 (2.24) |
| COVID-19 Work Loss (Hours) | 5.09 (13.49) |
| Depressive Symptoms (CES_D) | |
| Low risk of depression | 631 (61.46) |
| Significant depressive symptoms | 396 (38.54) |
| Household dysfunction (ACE) | |
| No ACE | 450 (43.82) |
| 1–3 ACE | 484 (47.13) |
| 4+ ACE | 93 (9.06) |
| Problematic Internet Use (PIU) | |
| Normal use | 573 (55.80) |
| Mild dependence | 352 (34.32) |
| Moderate or severe dependence | 102 (9.88) |
| Problematic Smartphone Use (PSU) | |
| Low risk of PSU | 777 (75.68) |
| High risk of PSU | 250 (24.32) |
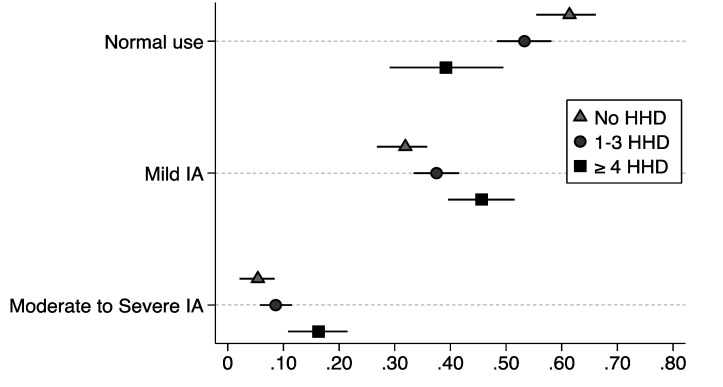
The results of the main-effects models are presented in Table 3. Students who reported 1–3 household stressors had higher proportional odds of mild Internet addiction vs. normal or moderate to severe than students who did not report any household dysfunction (AOR: 1.39, 95% CI: 1.05–1.83), whereas students who reported ≥4 household stressors had over twice the proportional odds of having moderate to severe Internet addiction vs. mild or normal Internet use (AOR: 2.46, 95% CI: 1.52–3.96), adjusting for covariates. In regard to peer social support, for every additional unit increase in the peer support score, there was a decrement in the proportional odds of mild or moderate to severe IA vs. normal Internet use (AOR: 0.91, 95% CI: 0.86–0.97). As seen in Figure 1, the probability of normal Internet use is far higher among students who report no HHD and relatively low among students with ≥4 household stressors, whereas the likelihood of mild and moderate to severe Internet use increases incrementally among students with 1–3 household stressors and ≥4 household stressors compared to students with no history of HHD.
Table 3.
Association between household dysfunction (HHD) and problematic Internet and smartphone use (N = 1027).
| Internet Addiction (IA) AOR (95% CI) |
Problematic Smartphone Use (PSU) AOR (95% CI) |
|
|---|---|---|
| Household Dysfunction (HHD) | ||
| 1–3 ACE | 1.39 (1.05–1.83) * | 1.40 (1.02–1.93) * |
| ≥4 ACE | 2.46 (1.52–3.96) ** | 2.03 (1.21–3.40) ** |
| Age | 0.93 (0.90–0.96) ** | 0.96 (0.93–0.99) * |
| Ethnicity | ||
| Non-Hispanic Black | 0.94 (0.47–1.89) | 1.11 (0.51–2.42) |
| Mexican | 0.51 (0.35–0.75) ** | 0.64 (0.40–1.00) |
| Other Hispanic | 0.73 (0.44–1.20) | 0.62 (0.34–1.12) |
| Asian | 1.54 (0.95–2.47) | 1.28 (0.72–2.28) |
| Other and Bi-/Multiracial | 0.89 (0.58–1.38) | 1.02 (0.63–1.66) |
| Biological Sex | ||
| Female | 1.09 (0.78–1.52) | 1.06 (0.73–1.55) |
| Perceived Social Support | 0.91 (0.86–0.97) ** | 0.93 (0.87–1.00) |
| COVID-19 Work Loss | 0.96 (0.99–1.01) | 0.99 (0.98–1.00) |
| Depression (CES_D) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) |
Note AOR: Adjusted Odds Ratio. Reference groups for ACE: No ACE; Ethnicity: Non-Hispanic White; Biological sex: Male. * = p < 0.05, ** p = < 0.01.
Figure 1.
Predicted probability with 95% confidence intervals of normal Internet use, mild Internet addiction, and moderate to severe Internet addiction for ACE groups, after adjusting for all covariates (i.e., age, gender, ethnicity, SES, COVID-19 employment loss, depression).
There was a similar pattern of results in models assessing the association between HHD and PSU. Students who reported 1–3 household stressors had higher odds of PSU (AOR: 1.40, 95% CI: 1.02–1.93) than their peers who did not report HHD, and students who had ≥4 household stressors had approximately twice the odds (AOR: 2.03, 95% CI: 1.21–3.40) of PSU than their peers. There was no association between peer support and PSU in the main-effects models.
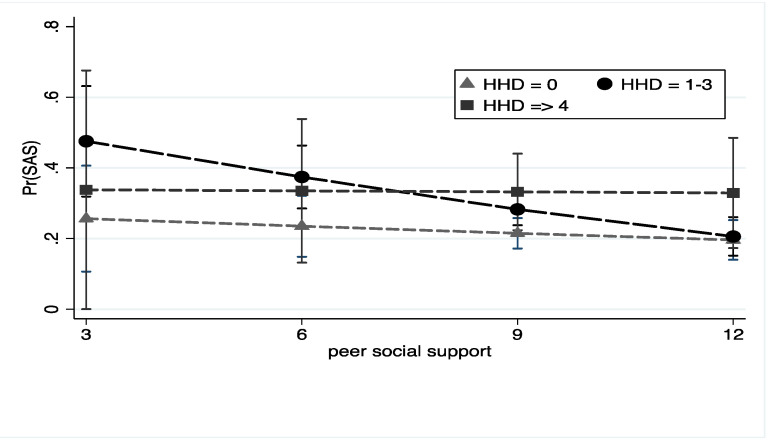
We also tested hypotheses that perceived that social support from friends would attenuate the negative effects of HHD for PIU and PSU. Social support from friends did not moderate the association between HHD and any level of PIU. However, as seen in Figure 2, higher levels of perceived peer social support offset the negative effect of HHD for PSU among students who reported 1–3 household stressors, but not among those reporting ≥4, adjusting for all covariates.
Figure 2.
HHD, peer social support, and problematic smartphone use. Note: Figure depicts the predicted probability with 95% confidence intervals of problematic smartphone use among students with a history of HHD at low and high levels of social support. All models adjusted for age, gender, ethnicity, SES, COVID-19 employment loss, and depression.
4. Discussion
This is one of the first studies to examine the association between cumulative HHD and problematic Internet and smartphone use in a diverse, American college sample. Over 50% of the sample reported at least one household stressor, and nearly 10% acknowledged four or more, estimates that are similar to those reported by national and community surveillance efforts [98,99]. Approximately 25% of students reported problematic smartphone use, 35% of students scored in the mild, and 10% scored in the moderate to severe PIU category, respectively. These estimates are also within range of those reported among young people and college students [100,101,102,103], although most studies have originated outside of the US.
Our primary hypotheses that students with a history of household dysfunction, and especially students with multiple co-occurring household stressors, would be at greater risk for problematic Internet and smartphone use were supported. This is concerning given that the SAS-SV and IAT assess the presence of life disturbance, difficulty concentrating, and an inability to meet obligations [14,104]—symptoms characteristic of addiction disorders [41,43]. The digital era and widespread use of the Internet and smartphones pose a risk of misuse for all young people, but especially individuals who are vulnerable to maladaptive coping and addictive behaviors. Scholars have argued that Internet and digital devices offer distractions and online activities that may be particularly attractive for young people seeking temporary relief from negative affect or feelings of distress [105,106]. This may be especially true for young adults who contend with the psychological and emotional impact of household dysfunction (i.e., parental mental illness or substance use) while they assume greater responsibility, manage academic obligations, and plan for the future. The joint effects of these developmental challenges and traumatic stressors can strain a young person’s available resources [107,108] and increase the likelihood of using digital devices and engaging in online activities to reduce stress and negative emotions [104,109,110]. However, compulsive digital device and Internet use as a means to relieve symptoms of psychological distress can actually exacerbate negative affect [109,111] and ensnare a young person in a cycle of increasing Internet and smartphone use to manage mood without ever addressing, or resolving, the underlying causes. Moreover, the wide availability and need for Internet and digital devices in daily life present challenges for the treatment and prevention of PIU and PSU [6].
The graded relationship between levels of HHD and PSU and PIU among this population is consistent with research demonstrating that early life adversity increases vulnerability for maladaptive coping behaviors, theorized to be a result of the ACE-related dysregulation of reward pathways and deficits in emotional and cognitive processing [112,113] that become more pronounced as the number of adversities increase [46]. In the context of PIU and PSU, there is burgeoning evidence that in comparison to individuals who do not report PSU or PIU, individuals who score as compulsive users on diagnostic instruments have significant structural and neural functioning differences that are similar to those of persons with substance use disorders [114,115]. Our results are preliminary, yet they align with and expand evidence that ACE are a shared risk factor for many of the behavioral addictions that compromise health, educational attainment, and life course wellbeing [98]. Although the mechanism through which any individual ACE affects health may be unique, the impact of a constellation of household stressors on physiological and psychological processes likely represents a common pathway to a range of long-term behavioral health issues [46]. If left unaddressed, a history of cumulative HHD can jeopardize academic performance and the degree to which students can leverage new academic and professional opportunities [45,59,116,117,118]—critical components of protecting the next generation from the harmful health effects of ACE.
In partial support of our hypothesis that perceived social support from peers would offset the negative effects of HHD, our results suggest that perceived peer social support can have promotive and protective effects for PIU and PSU, respectively. Perceived peer support was associated with lower odds of PIU, and although we did not assess online vs. offline support, this mirrors work that suggests strong interpersonal ties and perceived support from friends reduce risk for PIU [9,119,120]. High levels of perceived peer support, although not statistically associated with PSU in the main-effects model, offset the negative effects of HHD for PSU among students experiencing between one and three household stressors. This finding aligns with research demonstrating that social support can limit the physiological arousal and stress reactivity associated with traumatic circumstances and promote resilient functioning [121,122]. Despite the protective effects of strong bonds with teachers, peers, and members of important community groups for ACE-exposed populations [85,123,124], support from peers may be insufficient or need to be paired with direct services or additional individual or social assets to mitigate the negative effects of high levels (≥4 HHD) of adversity for PSU and PIU.
Given the importance of the college years for later-life advantage and the substantial evidence that ACE can jeopardize young adult mental and behavioral health, addressing the pervasive, long-term, negative consequence of these traumatic stressors for positive adjustment is imperative. College communities serve a diverse cross-section of young adults and are an opportune setting to provide support services for vulnerable students as they transition from adolescence to adulthood. The benefits of trauma-informed care for other segments of the population [125,126,127] make a persuasive argument for prioritizing prevention and intervention initiatives in settings that foster young peoples’ development [128,129] and promote positive health outcomes. An important area of future research is to identify individual, peer, community, and cultural assets that can offset the negative effects of HHD specifically, or ACE generally, for PSU, PIU, and other behavioral addictions and how these can be leveraged in prevention programs tailored to young adults.
Limitations
The present study had several limitations. First, these data are cross-sectional, do not support causal conclusions, and are generalizable only to college students attending universities in diverse, urban settings similar to that of Southern California. Second, although demographic profiles resembled college profiles, it is likely that the highest-risk students did not participate in the survey, and therefore, we underestimated the prevalence of PIU, PSU, HHD, and the association between HHD and PIU and PSU. Third, due to the limited number of students reporting ≥4 HHD, we may have underestimated the potential protective effects of peer social support for PSU. Fourth, we assessed household dysfunction retrospectively; however, since survey items explicitly referred to events prior to age 18, whereas PIU and PSU assessed recent behaviors, reverse temporality is unlikely. Fifth, the SAS-SV does not include items assessing mood or relapse, and although the threshold for PSU recommended by SAS-SV developers is widely used, it does not represent an established diagnostic criterion. Sixth, we did not ask whether students’ peer support sources were online or offline and thus were not able to determine whether online activities enhance students’ perceptions of having meaningful and supportive social ties. Lastly, our sample was predominantly female and may have led to over or underestimating the strength of associations.
Despite these limitations, this study is among the first to examine the relationship between HHD and PIU and PSU among a diverse sample of American college students. Further research among college populations using longitudinal designs to replicate these findings is suggested.
5. Conclusions
Given the high prevalence of ACE, PIU, and PSU in college populations, and based on the extraordinary net benefits of a college education, which may actually mitigate the effects of early life adversity [130], funding prevention and support services in higher education could substantially reduce the trauma-related mental and behavioral public health burden. Campus communities could play a pivotal role in promoting resilience during the transition from adolescence to adulthood by raising awareness of the risks and consequences of PIU and PSU, by encouraging students to access support services that can help them to cope with familial adversity, and by promoting the development of meaningful social bonds.
Author Contributions
Conceptualization, M.F., S.Y. and S.M.B.; methodology, M.F., S.M.B.; software, M.F., J.W.; validation, M.F.,J.W. and C.J.R.; formal analysis, M.F.; investigation, M.F., S.M.B.; resources, M.F., S.M.B.; data curation, J.W., M.F.; writing—original draft preparation, M.F.; writing—review and editing, C.J.R., S.S., S.Y., T.R., J.W.; visualization, M.F., T.R.; supervision, M.F, S.M.B.; project administration, J.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of California State University Northridge (FY20-288; 4/20/2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Moreno M.A., Jelenchick L.A., Egan K.G., Cox E., Young H., Gannon K.E., Becker T. Feeling bad on Facebook: Depression disclosures by college students on a social networking site. Depress. Anxiety. 2011;28:447–455. doi: 10.1002/da.20805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verhoeven J.C., Heerwegh D., De Wit K. Information and communication technologies in the life of university freshmen: An analysis of change. Comput. Educ. 2010;55:53–66. doi: 10.1016/j.compedu.2009.12.002. [DOI] [Google Scholar]
- 3.Vogels E.A. Millennials Stand Out for Their Technology Use, But Older Generations also Embrace Digital Life. [(accessed on 25 February 2021)]; Available online: https://www.pewresearch.org/fact-tank/2019/09/09/us-generations-technology-use/
- 4.Rodgers S., Sheldon K.M. An Improved Way to Characterize Internet Users. J. Advert. Res. 2002;42:85–94. doi: 10.2501/JAR-42-5-85-94. [DOI] [Google Scholar]
- 5.Blackhart G.C., Fitzpatrick J., Williamson J. Dispositional factors predicting use of online dating sites and behaviors related to online dating. Comput. Hum. Behav. 2014;33:113–118. doi: 10.1016/j.chb.2014.01.022. [DOI] [Google Scholar]
- 6.Griffiths M., Pontes H., Kuss D. Clinical psychology of Internet addiction: A review of its conceptualization, prevalence, neuronal processes, and implications for treatment. Neurosci. Neuroecon. 2015;4:11–23. doi: 10.2147/NAN.S60982. [DOI] [Google Scholar]
- 7.Stevens C., Zhang E., Cherkerzian S., Chen J.A., Liu C.H. Problematic internet use/computer gaming among US college students: Prevalence and correlates with mental health symptoms. Depress. Anxiety. 2020;37:1127–1136. doi: 10.1002/da.23094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chou C., Condron L., Belland J.C. A Review of the Research on Internet Addiction. Educ. Psychol. Rev. 2005;17:363–388. doi: 10.1007/s10648-005-8138-1. [DOI] [Google Scholar]
- 9.Tsai H.F., Cheng S.H., Yeh T.L., Shih C.-C., Chen K.C., Yang Y.C., Yang Y.K. The risk factors of Internet addiction—A survey of university freshmen. Psychiatry Res. 2009;167:294–299. doi: 10.1016/j.psychres.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 10.Whang L.S.-M., Lee S., Chang G. Internet Over-Users’ Psychological Profiles: A Behavior Sampling Analysis on Internet Addiction. Cyberpsychol. Behav. 2003;6:143–150. doi: 10.1089/109493103321640338. [DOI] [PubMed] [Google Scholar]
- 11.Correa T., Hinsley A.W., Gil de Zúñiga H. Who interacts on the Web? The intersection of users’ personality and social media use. Comput. Hum. Behav. 2010;26:247–253. doi: 10.1016/j.chb.2009.09.003. [DOI] [Google Scholar]
- 12.Cole S.H., Hooley J.M. Clinical and personality correlates of MMO gaming: Anxiety and absorption in problematic internet use. Soc. Sci. Comput. Rev. 2013;31:424–436. doi: 10.1177/0894439312475280. [DOI] [Google Scholar]
- 13.Riehm K.E., Thrul J., Barrington-Trimis J.L., Kelleghan A., Mojtabai R., Leventhal A.M. Prospective Association of Digital Media Use with Alcohol Use Initiation and Progression Among Adolescents. Alcohol. Clin. Exp. Res. 2021;45:877–885. doi: 10.1111/acer.14578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith A.U.S. Smartphone Use in 2015. [(accessed on 25 February 2021)]; Available online: https://www.pewresearch.org/internet/2015/04/01/us-smartphone-use-in-2015/
- 15.Carbonell X., Chamarro A., Oberst U., Rodrigo B., Prades M. Problematic Use of the Internet and Smartphones in University Students: 2006–2017. Int. J. Environ. Res. Public Health. 2018;15:475. doi: 10.3390/ijerph15030475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dahlstrom E., Bichsel J. ECAR Study of Undergraduate Students and Information Technology. EDUCAUSE Center for Analysis and Research; Louisville, KY, USA: 2014. [Google Scholar]
- 17.Kwon M., Kim D.-J., Cho H., Yang S. The Smartphone Addiction Scale: Development and Validation of a Short Version for Adolescents. PLoS ONE. 2013;8:e83558. doi: 10.1371/journal.pone.0083558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee J., Cho B., Kim Y., Noh J. Emerging Issues in Smart Learning. Springer; Berlin/Heidelberg, Germany: 2014. Smartphone Addiction in University Students and Its Implication for Learning; pp. 297–305. [Google Scholar]
- 19.Lin Y.-H., Chiang C.-L., Lin P.-H., Chang L.-R., Ko C.-H., Lee Y.-H., Lin S.-H. Proposed Diagnostic Criteria for Smartphone Addiction. PLoS ONE. 2016;11:e0163010. doi: 10.1371/journal.pone.0163010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han L., Geng J., Jou M., Gao F., Yang H. Relationship between shyness and mobile phone addiction in Chinese young adults: Mediating roles of self-control and attachment anxiety. Comput. Hum. Behav. 2017;76:363–371. doi: 10.1016/j.chb.2017.07.036. [DOI] [Google Scholar]
- 21.Ho R.C., Zhang M.W., Tsang T.Y., Toh A.H., Pan F., Lu Y., Cheng C., Yip P.S., Lam L.T., Lai C.-M., et al. The association between internet addiction and psychiatric co-morbidity: A meta-analysis. BMC Psychiatry. 2014;14:183. doi: 10.1186/1471-244X-14-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee Y.-K., Chang C.-T., Lin Y., Cheng Z.-H. The dark side of smartphone usage: Psychological traits, compulsive behavior and technostress. Comput. Hum. Behav. 2014;31:373–383. doi: 10.1016/j.chb.2013.10.047. [DOI] [Google Scholar]
- 23.Augner C., Hacker G.W. Associations between problematic mobile phone use and psychological parameters in young adults. Int. J. Public Health. 2012;57:437–441. doi: 10.1007/s00038-011-0234-z. [DOI] [PubMed] [Google Scholar]
- 24.Mondal A., Kumar M. A study on Internet addiction and its relation to psychopathology and self-esteem among college students. Ind. Psychiatry J. 2018;27:61–66. doi: 10.4103/ipj.ipj_61_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sohn S.Y., Krasnoff L., Rees P., Kalk N.J., Carter B. The Association Between Smartphone Addiction and Sleep: A UK Cross-Sectional Study of Young Adults. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.629407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hawi N.S., Samaha M. To excel or not to excel: Strong evidence on the adverse effect of smartphone addiction on ac-ademic performance. Comput. Educ. 2016;98:81–89. doi: 10.1016/j.compedu.2016.03.007. [DOI] [Google Scholar]
- 27.Judd T. Making sense of multitasking: The role of Facebook. Comput. Educ. 2014;70:194–202. doi: 10.1016/j.compedu.2013.08.013. [DOI] [Google Scholar]
- 28.Rosen L.D., Carrier L.M., Cheever N.A. Facebook and texting made me do it: Media-induced task-switching while studying. Comput. Hum. Behav. 2013;29:948–958. doi: 10.1016/j.chb.2012.12.001. [DOI] [Google Scholar]
- 29.Alosaimi F.D., Alyahya H., Alshahwan H., Al Mahyijari N., Shaik S.A. Smartphone addiction among university students in Riyadh, Saudi Arabia. Saudi Med. J. 2016;37:675–683. doi: 10.15537/smj.2016.6.14430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen B., Liu F., Ding S., Ying X., Wang L., Wen Y. Gender differences in factors associated with smartphone addiction: A cross-sectional study among medical college students. BMC Psychiatry. 2017;17:1–9. doi: 10.1186/s12888-017-1503-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paek K.S. A convergence study the association between addictive smart phone use, dry eye syndrome, upper extremity pain and depression among college students. J. Korea Converg. Soc. 2017;8:61–69. doi: 10.15207/JKCS.2017.8.1.061. [DOI] [Google Scholar]
- 32.Tateno M., Kim D.-J., Teo A.R., Skokauskas N., Guerrero A.P.S., Kato T.A. Smartphone Addiction in Japanese College Students: Usefulness of the Japanese Version of the Smartphone Addiction Scale as a Screening Tool for a New Form of Internet Addiction. Psychiatry Investig. 2019;16:115–120. doi: 10.30773/pi.2018.12.25.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang Z., Asbury K., Griffiths M.D. An Exploration of Problematic Smartphone Use among Chinese University Students: Associations with Academic Anxiety, Academic Procrastination, Self-Regulation and Subjective Wellbeing. Int. J. Ment. Health Addict. 2018;17:596–614. doi: 10.1007/s11469-018-9961-1. [DOI] [Google Scholar]
- 34.Kuss D., Griffiths M., Karila L., Billieux J. Internet Addiction: A Systematic Review of Epidemiological Research for the Last Decade. Curr. Pharm. Des. 2014;20:4026–4052. doi: 10.2174/13816128113199990617. [DOI] [PubMed] [Google Scholar]
- 35.Wallace P. Internet addiction disorder and youth: There are growing concerns about compulsive online activity and that this could impede students’ performance and social lives. EMBO Rep. 2014;15:12–16. doi: 10.1002/embr.201338222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yates T.M., Gregor M.A., Haviland M.G. Child Maltreatment, Alexithymia, and Problematic Internet Use in Young Adulthood. Cyberpsychol. Behav. Soc. Netw. 2012;15:219–225. doi: 10.1089/cyber.2011.0427. [DOI] [PubMed] [Google Scholar]
- 37.Beard K.W. Internet Addiction: A Review of Current Assessment Techniques and Potential Assessment Questions. Cyberpsychol. Behav. 2005;8:7–14. doi: 10.1089/cpb.2005.8.7. [DOI] [PubMed] [Google Scholar]
- 38.Kim H.-J., Min J.-Y., Min K.-B., Lee T.-J., Yoo S. Relationship among family environment, self-control, friendship quality, and adolescents’ smartphone addiction in South Korea: Findings from nationwide data. PLoS ONE. 2018;13:e0190896. doi: 10.1371/journal.pone.0190896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Young K.S. Internet Addiction: The Emergence of a New Clinical Disorder. Cyberpsychol. Behav. 1998;1:237–244. doi: 10.1089/cpb.1998.1.237. [DOI] [Google Scholar]
- 40.Yuchang J., Cuicui S., Junxiu A., Junyi L. Attachment styles and smartphone addiction in Chinese college students: The mediating roles of dysfunctional attitudes and self-esteem. Int. J. Ment. Health Addict. 2017;15:1122–1134. doi: 10.1007/s11469-017-9772-9. [DOI] [Google Scholar]
- 41.Griffiths M. A ‘components’ model of addiction within a biopsychosocial framework. J. Subst. Use. 2005;10:191–197. doi: 10.1080/14659890500114359. [DOI] [Google Scholar]
- 42.Kuss D.J., Lopez-Fernandez O. Internet addiction and problematic Internet use: A systematic review of clinical research. World J. Psychiatry. 2016;6:143–176. doi: 10.5498/wjp.v6.i1.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Young K.S. Internet Addiction: A New Clinical Phenomenon and Its Consequences. Am. Behav. Sci. 2004;48:402–415. doi: 10.1177/0002764204270278. [DOI] [Google Scholar]
- 44.Tsai C.-C., Lin S.S. Internet Addiction of Adolescents in Taiwan: An Interview Study. Cyberpsychol. Behav. 2003;6:649–652. doi: 10.1089/109493103322725432. [DOI] [PubMed] [Google Scholar]
- 45.Anda R.F., Croft J.B., Felitti V.J., Nordenberg D., Giles W.H., Williamson D.F., Giovino G.A. Adverse Childhood Experiences and Smoking During Adolescence and Adulthood. JAMA. 1999;282:1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 46.Anda R.F., Felitti V.J., Bremner J.D., Walker J.D., Whitfield C.L., Perry B.D., Dube S.R., Giles W.H. The enduring effects of abuse and related adverse experiences in childhood. Eur. Arch. Psychiatry Clin. Neurosci. 2006;256:174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Danese A., McEwen B.S. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol. Behav. 2012;106:29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 48.Hankin B.L., Abela J.R.Z. Development of Psychopathology: A Vulnerability-Stress Perspective. SAGE Publications; Thousand Oaks, CA, USA: 2005. [Google Scholar]
- 49.Lackner C.L., Santesso D.L., Dywan J., O’Leary D.D., Wade T.J., Segalowitz S.J. Adverse childhood experiences are associated with self-regulation and the magnitude of the error-related negativity difference. Biol. Psychol. 2018;132:244–251. doi: 10.1016/j.biopsycho.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 50.Orth U. The family environment in early childhood has a long-term effect on self-esteem: A longitudinal study from birth to age 27 years. J. Pers. Soc. Psychol. 2018;114:637–655. doi: 10.1037/pspp0000143. [DOI] [PubMed] [Google Scholar]
- 51.Cavanaugh C.E., Petras H., Martins S.S. Gender-specific profiles of adverse childhood experiences, past year mental and substance use disorders, and their associations among a national sample of adults in the United States. Soc. Psychiatry Psychiatr. Epidemiol. 2015;50:1257–1266. doi: 10.1007/s00127-015-1024-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Perera B., Reece M., Monahan P., Billingham R., Finn P. Childhood Characteristics and Personal Dispositions to Sexually Compulsive Behavior Among Young Adults. Sex. Addict. Compulsivity. 2009;16:131–145. doi: 10.1080/10720160902905421. [DOI] [Google Scholar]
- 53.Felsher J.R., Derevensky J.L., Gupta R. Young Adults with Gambling Problems: The Impact of Childhood Maltreat-ment. Int. J. Ment. Health Addict. 2010;8:545–556. doi: 10.1007/s11469-009-9230-4. [DOI] [Google Scholar]
- 54.Arnett J.J. Emerging adulthood. A theory of development from the late teens through the twenties. Am. Psychol. 2000;55:469–480. doi: 10.1037/0003-066X.55.5.469. [DOI] [PubMed] [Google Scholar]
- 55.Hingson R., White A. New Research Findings Since the 2007 Surgeon General’s Call to Action to Prevent and Reduce Underage Drinking: A Review. J. Stud. Alcohol Drugs. 2014;75:158–169. doi: 10.15288/jsad.2014.75.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hudson J.I., Hiripi E., Pope H.G., Kessler R.C. The Prevalence and Correlates of Eating Disorders in the National Comorbidity Survey Replication. Biol. Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pascarella E.T. How College Affects Students: Ten Directions for Future Research. J. Coll. Stud. Dev. 2006;47:508–520. doi: 10.1353/csd.2006.0060. [DOI] [Google Scholar]
- 58.Schwartz S.J., Côté J.E., Arnett J.J. Identity and Agency in Emerging Adulthood: Two Developmental Routes in the Individualization Process. Youth Soc. 2005;37:201–229. doi: 10.1177/0044118X05275965. [DOI] [Google Scholar]
- 59.Anda R.F. The Health and Social Impact of Growing up with Adverse Childhood Experiences: The Human and Economic Costs of the Status Quo. [(accessed on 26 February 2021)]; Available online: http://www.theannainstitute.org/ACE%20folder%20for%20website/50%20Review_of_ACE_Study_with_references_summary_table_2_.pdf.
- 60.Green J.G., McLaughlin K.A., Berglund P.A., Gruber M.J., Sampson N.A., Zaslavsky A.M., Kessler R.C. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: Associations with first onset of DSM-IV disorders. Arch. Gen. Psychiatry. 2010;67:113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dalbudak E., Evren C., Aldemir S., Evren B. The severity of Internet addiction risk and its relationship with the severity of borderline personality features, childhood traumas, dissociative experiences, depression and anxiety symptoms among Turkish University Students. Psychiatry Res. 2014;219:577–582. doi: 10.1016/j.psychres.2014.02.032. [DOI] [PubMed] [Google Scholar]
- 62.Li W., Zhang X., Chu M., Li G. The Impact of Adverse Childhood Experiences on Mobile Phone Addiction in Chinese College Students: A Serial Multiple Mediator Model. Front. Psychol. 2020;11:834. doi: 10.3389/fpsyg.2020.00834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kircaburun K., Griffiths M.D., Billieux J. Psychosocial factors mediating the relationship between childhood emotional trauma and internet gaming disorder: A pilot study. Eur. J. Psychotraumatol. 2019;10:1565031. doi: 10.1080/20008198.2018.1565031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Park S.K., Kim J.Y., Cho C.B. Prevalence of Internet addiction and correlations with family factors among South Korean adolescents. Adolescence. 2008;43:895–909. [PubMed] [Google Scholar]
- 65.Schimmenti A., Passanisi A., Gervasi A.M., Manzella S., Famà F.I. Insecure Attachment Attitudes in the Onset of Problematic Internet Use Among Late Adolescents. Child Psychiatry Hum. Dev. 2014;45:588–595. doi: 10.1007/s10578-013-0428-0. [DOI] [PubMed] [Google Scholar]
- 66.Forster M., Rogers C., Sussman S.Y., Yu S., Rahman T., Zeledon H., Benjamin S.M. Adverse childhood experiences and problematic smartphone use among college students: Findings from a pilot study. Addict. Behav. 2021;117:106869. doi: 10.1016/j.addbeh.2021.106869. [DOI] [PubMed] [Google Scholar]
- 67.Yang L., Sun L., Zhang Z., Sun Y., Wu H., Ye D. Internet addiction, adolescent depression, and the mediating role of life events: Finding from a sample of Chinese adolescents. Int. J. Psychol. 2014;49:342–347. doi: 10.1002/ijop.12063. [DOI] [PubMed] [Google Scholar]
- 68.Shi L., Wang Y., Yu H., Wilson A., Cook S., Duan Z., Peng K., Hu Z., Ou J., Duan S., et al. The relationship between childhood trauma and Internet gaming disorder among college students: A structural equation model. J. Behav. Addict. 2020;9:175–180. doi: 10.1556/2006.2020.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Björkenstam E., Dalman C., Vinnerljung B., Weitoft G.R., Walder D.J., Burström B. Childhood household dysfunction, school performance and psychiatric care utilisation in young adults: A register study of 96 399 individuals in Stockholm County. J. Epidemiol. Commun. Health. 2015;70:473–480. doi: 10.1136/jech-2015-206329. [DOI] [PubMed] [Google Scholar]
- 70.Forster M., Davis L., Shlafer R., Unger J.B. Household Incarceration and Salient Emerging Adult Role Transitions: Findings From an Urban Sample of Hispanic Youth. Emerg. Adulthood. 2018;7:3–11. doi: 10.1177/2167696817751749. [DOI] [Google Scholar]
- 71.Gauffin K., Hjern A., Vinnerljung B., Björkenstam E. Childhood Household Dysfunction, Social Inequality and Alcohol Related Illness in Young Adulthood. A Swedish National Cohort Study. PLoS ONE. 2016;11:e0151755. doi: 10.1371/journal.pone.0151755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Grigsby T.J., Forster M., Davis L., Unger J.B. Substance Use Outcomes for Hispanic Emerging Adults Exposed to In-carceration of a Household Member during Childhood. J. Ethn. Subst. Abuse. 2018;19:358–370. doi: 10.1080/15332640.2018.1511494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Berman I.S., Petretric P., Bridges A.J. Beyond child maltreatment: The incremental value of household dysfunction in the prediction of negative beliefs and internalizing symptoms in women. J. Am. Coll. Health. 2019:1–9. doi: 10.1080/07448481.2019.1687483. [DOI] [PubMed] [Google Scholar]
- 74.Forster M., Grigsby T.J., Rogers C.J., Benjamin S.M. The relationship between family-based adverse childhood ex-periences and substance use behaviors among a diverse sample of college students. Addict. Behav. 2018;76:298–304. doi: 10.1016/j.addbeh.2017.08.037. [DOI] [PubMed] [Google Scholar]
- 75.Merians A.N., Baker M.R., Frazier P., Lust K. Outcomes related to adverse childhood experiences in college students: Comparing latent class analysis and cumulative risk. Child Abus. Negl. 2019;87:51–64. doi: 10.1016/j.chiabu.2018.07.020. [DOI] [PubMed] [Google Scholar]
- 76.Shin S.H., McDonald S.E., Conley D. Patterns of adverse childhood experiences and substance use among young adults: A latent class analysis. Addict. Behav. 2018;78:187–192. doi: 10.1016/j.addbeh.2017.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Barrera M. Social Support Research in Community Psychology. Springer; Berlin/Heidelberg, Germany: 2000. pp. 215–245. [Google Scholar]
- 78.Carbery J., Buhrmester D. Friendship and Need Fulfillment During Three Phases of Young Adulthood. J. Soc. Pers. Relatsh. 1998;15:393–409. doi: 10.1177/0265407598153005. [DOI] [Google Scholar]
- 79.Graber R., Turner R., Madill A. Best friends and better coping: Facilitating psychological resilience through boys’ and girls’ closest friendships. Br. J. Psychol. 2015;107:338–358. doi: 10.1111/bjop.12135. [DOI] [PubMed] [Google Scholar]
- 80.Chu P.S., Saucier D.A., Hafner E. Meta-Analysis of the Relationships Between Social Support and Well-Being in Children and Adolescents. J. Soc. Clin. Psychol. 2010;29:624–645. doi: 10.1521/jscp.2010.29.6.624. [DOI] [Google Scholar]
- 81.Ertel K.A., Glymour M.M., Berkman L.F. Social networks and health: A life course perspective integrating observa-tional and experimental evidence. J. Soc. Pers. Relat. 2009;26:73–92. doi: 10.1177/0265407509105523. [DOI] [Google Scholar]
- 82.Uchino B.N. Current Perspectives in Psychology. Social Support and Physical Health: Understanding the Health Conse-Quences of Relationships. Yale University Press; London, UK: 2004. [Google Scholar]
- 83.Cohen S., Gottlieb B.H., Underwood L.G. Social Relationships and Health. Soc. Support Meas. Interv. 2000;59:3–26. doi: 10.1093/med:psych/9780195126709.003.0001. [DOI] [Google Scholar]
- 84.Uchino B.N. Social Support and Health: A Review of Physiological Processes Potentially Underlying Links to Disease Outcomes. J. Behav. Med. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 85.Forster M., Grigsby T.J., Gower A.L., Mehus C.J., McMorris B.J. The Role of Social Support in the Association between Childhood Adversity and Adolescent Self-injury and Suicide: Findings from a Statewide Sample of High School Students. J. Youth Adolesc. 2020;49:1195–1208. doi: 10.1007/s10964-020-01235-9. [DOI] [PubMed] [Google Scholar]
- 86.Banjanin N., Banjanin N., Dimitrijevic I., Pantic I. Relationship between internet use and depression: Focus on physi-ological mood oscillations, social networking and online addictive behavior. Comput. Hum. Behav. 2015;43:308–312. doi: 10.1016/j.chb.2014.11.013. [DOI] [Google Scholar]
- 87.Christakis D.A., Moreno M.M., Jelenchick L., Myaing M.T., Zhou C. Problematic internet usage in US college students: A pilot study. BMC Med. 2011;9:77. doi: 10.1186/1741-7015-9-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhang W., O’Brien N., Forrest J.I., Salters K.A., Patterson T.L., Montaner J.S.G., Hogg R.S., Lima V.D. Validating a Shortened Depression Scale (10 Item CES-D) among HIV-Positive People in British Columbia, Canada. PLoS ONE. 2012;7:e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1988;52:30–41. doi: 10.1207/s15327752jpa5201_2. [DOI] [Google Scholar]
- 90.Felitti V.J., Anda R.F., Nordenberg D., Williamson D.F., Spitz A.M., Edwards V., Koss M.P., Marks J.S. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. Am. J. Prev. Med. 1998;14:245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 91.van Buuren S., Boshuizen H.C., Knook D.L. Multiple imputation of missing blood pressure covariates in survival analysis. Stat. Med. 1999;18:681–694. doi: 10.1002/(SICI)1097-0258(19990330)18:6<681::AID-SIM71>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 92.Raghunathan T.E., Lepkowski J., Van Hoewyk J., Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv. Methodol. 2001;27:85–96. [Google Scholar]
- 93.van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat. Methods Med. Res. 2007;16:219–242. doi: 10.1177/0962280206074463. [DOI] [PubMed] [Google Scholar]
- 94.van Buuren S., Groothuis-Oudshoorn K. Multivariate Imputation by Chained Equations: MICE V1.0 User manual. J. Stat. Softw. 2000;45:5–39. [Google Scholar]
- 95.Graham J.W., Olchowski A.E., Gilreath T.D. How Many Imputations are Really Needed? Some Practical Clarifications of Multiple Imputation Theory. Prev. Sci. 2007;8:206–213. doi: 10.1007/s11121-007-0070-9. [DOI] [PubMed] [Google Scholar]
- 96.Rubin D.B. Multiple Imputation for Nonresponse in Surveys. Wiley; Hoboken, NJ, USA: 2004. [Google Scholar]
- 97.StataCorp LLC, College Station, TX, 2017. [(accessed on 15 February 2021)]; Available online: https://www.stata.com/company.
- 98.Merrick M.T., Ford D.C., Ports K.A., Guinn A.S., Chen J., Klevens J., Metzler M., Jones C.M., Simon T.R., Daniel V.M., et al. Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention—25 States, 2015–2017. Centers for Disease Control and Prevention; Atlanta, GA, USA: 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sacks V., Murphey D. The Prevalence of Adverse Childhood Experiences, Nationally, by State, and by Race or Ethnicity. [(accessed on 26 February 2021)]; Available online: https://ncvc.dspacedirect.org/handle/20.500.11990/1142.
- 100.Haug S., Castro R.P., Kwon M., Filler A., Kowatsch T., Schaub M.P. Smartphone use and smartphone addiction among young people in Switzerland. J. Behav. Addict. 2015;4:299–307. doi: 10.1556/2006.4.2015.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hsieh K.-Y., Hsiao R.C., Yang Y.-H., Lee K.-H., Yen C.-F. Relationship between Self-Identity Confusion and Internet Addiction among College Students: The Mediating Effects of Psychological Inflexibility and Experiential Avoidance. Int. J. Environ. Res. Public Health. 2019;16:3225. doi: 10.3390/ijerph16173225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Krishnamurthy S., Chetlapalli S. Internet addiction: Prevalence and risk factors: A cross-sectional study among college students in Bengaluru, the Silicon Valley of India. Ind. J. Public Health. 2015;59:115–121. doi: 10.4103/0019-557X.157531. [DOI] [PubMed] [Google Scholar]
- 103.Shao Y.-J., Zheng T., Wang Y.-Q., Liu L., Chen Y., Yao Y.-S. Internet addiction detection rate among college students in the People’s Republic of China: A meta-analysis. Child Adolesc. Psychiatry Ment. Health. 2018;12:1–10. doi: 10.1186/s13034-018-0231-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Billieux J., Maurage P., Lopez-Fernandez O., Kuss D.J., Griffiths M.D. Can Disordered Mobile Phone Use Be Considered a Behavioral Addiction? An Update on Current Evidence and a Comprehensive Model for Future Research. Curr. Addict. Rep. 2015;2:156–162. doi: 10.1007/s40429-015-0054-y. [DOI] [Google Scholar]
- 105.Cheng C., Sun P., Mak K.K. Internet Addiction and Psychosocial Maladjustment: Avoidant Coping and Coping In-flexibility as Psychological Mechanisms. Cyberpsychol. Behav. Soc. Netw. 2015;18:539–546. doi: 10.1089/cyber.2015.0121. [DOI] [PubMed] [Google Scholar]
- 106.Yan W., Li Y., Sui N. The relationship between recent stressful life events, personality traits, perceived family func-tioning and internet addiction among college students. Stress Health. 2014;30:3–11. doi: 10.1002/smi.2490. [DOI] [PubMed] [Google Scholar]
- 107.Lazarus R.S., Folkman S. Stress, Appraisal, and Coping. Springer; Berlin/Heidelberg, Germany: 1984. [Google Scholar]
- 108.Moos R.H., Moos B.S. Life Stressors and Social Resources Inventory: A measure of Adults’ and Youths’ Life Contexts. Scarecrow Education; Lanham, MA, USA: 1997. [Google Scholar]
- 109.Kim J.-H., Seo M., David P. Alleviating depression only to become problematic mobile phone users: Can face-to-face communication be the antidote? Comput. Hum. Behav. 2015;51:440–447. doi: 10.1016/j.chb.2015.05.030. [DOI] [Google Scholar]
- 110.Snodgrass J.G., Lacy M.G., Dengah II H.J.F., Eisenhauser S., Batchelder G., Cookson R.J. A vacation from your mind: Problematic online gaming is a stress response. Comput. Hum. Behav. 2014;38:248–260. doi: 10.1016/j.chb.2014.06.004. [DOI] [Google Scholar]
- 111.Morahan-Martin J. Internet Use and Abuse and Psychological Problems. [(accessed on 26 February 2021)];2012 Available online: https://www.oxfordhandbooks.com/view/10.1093/oxfordhb/9780199561803.001.0001/oxfordhb-9780199561803-e-021.
- 112.Gilbert R., Widom C.S., Browne K., Fergusson D., Webb E., Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 113.Pollak S.D., Cicchetti D., Hornung K., Reed A. Recognizing emotion in faces: Developmental effects of child abuse and neglect. Dev. Psychol. 2000;36:679–688. doi: 10.1037/0012-1649.36.5.679. [DOI] [PubMed] [Google Scholar]
- 114.Hong S.-B., Zalesky A., Cocchi L., Fornito A., Choi E.-J., Kim H.-H., Suh J.-E., Kim C.-D., Kim J.-W., Yi S.-H. Decreased Functional Brain Connectivity in Adolescents with Internet Addiction. PLoS ONE. 2013;8:e57831. doi: 10.1371/journal.pone.0057831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Horvath J., Mundinger C., Schmitgen M.M., Wolf N.D., Sambataro F., Hirjak D., Kubera K.M., Koenig J., Wolf R.C. Structural and functional correlates of smartphone addiction. Addict. Behav. 2020;105:106334. doi: 10.1016/j.addbeh.2020.106334. [DOI] [PubMed] [Google Scholar]
- 116.Ford E.S., Anda R.F., Edwards V.J., Perry G.S., Zhao G., Li C., Croft J.B. Adverse childhood experiences and smoking status in five states. Prev. Med. 2011;53:188–193. doi: 10.1016/j.ypmed.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 117.Goodman E., McEwen B.S., Dolan L.M., Schafer-Kalkhoff T., Adler N.E. Social disadvantage and adolescent stress. J. Adolesc. Health. 2005;37:484–492. doi: 10.1016/j.jadohealth.2004.11.126. [DOI] [PubMed] [Google Scholar]
- 118.Shonkoff J.P., Garner A.S., Siegel B.S., Dobbins M.I., Earls M.F., McGuinn L., Garner A.S., Pascoe J., Wood D.L., Committee on Early Childhood, Adoption, and Dependent Care et al. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 119.Liu C.-Y., Kuo F.-Y. A Study of Internet Addiction through the Lens of the Interpersonal Theory. Cyberpsychol. Behav. 2007;10:799–804. doi: 10.1089/cpb.2007.9951. [DOI] [PubMed] [Google Scholar]
- 120.Wang E.S.-T., Wang M.C.-H. Social Support and Social Interaction Ties on Internet Addiction: Integrating Online and Offline Contexts. Cyberpsychol. Behav. Soc. Netw. 2013;16:843–849. doi: 10.1089/cyber.2012.0557. [DOI] [PubMed] [Google Scholar]
- 121.Rosal M.C., King J., Ma Y., Reed G.W. Stress, Social Support, and Cortisol: Inverse Associations? Behav. Med. 2004;30:11–21. doi: 10.3200/BMED.30.1.11-22. [DOI] [PubMed] [Google Scholar]
- 122.Reblin M., Uchino B.N. Social and emotional support and its implication for health. Curr. Opin. Psychiatry. 2008;21:201–205. doi: 10.1097/YCO.0b013e3282f3ad89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Forster M., Davis L., Grigsby T.J., Rogers C.J., Vetrone S.F., Unger J.B. The Role of Familial Incarceration and Ethnic Identity in Suicidal Ideation and Suicide Attempt: Findings from a Longitudinal Study of Latinx Young Adults in California. Am. J. Community Psychol. 2019;64:191–202. doi: 10.1002/ajcp.12332. [DOI] [PubMed] [Google Scholar]
- 124.Von Cheong E., Sinnott C., Dahly D., Kearney P.M. Adverse childhood experiences (ACEs) and later-life depression: Perceived social support as a potential protective factor. BMJ Open. 2017;7:e013228. doi: 10.1136/bmjopen-2016-013228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ko S.J., Ford J.D., Kassam-Adams N., Berkowitz S.J., Wilson C., Wong M., Brymer M.J., Layne C.M. Creating trauma-informed systems: Child welfare, education, first responders, health care, juvenile justice. Prof. Psychol. Res. Pract. 2008;39:396–404. doi: 10.1037/0735-7028.39.4.396. [DOI] [Google Scholar]
- 126.Listenbee R.L., Torre J., Boyle G., Cooper S.W., Deer S., Durfee D.T., James T., Lieberman A., Macy R., Marans S., et al. Report of the Attorney General’s National Task Force on Children Exposed to Violence; 2012; pp. 3–189. [(accessed on 26 February 2021)]; Available online: https://www.justice.gov/defendingchildhood/cev-rpt-full.pdf.
- 127.Taylor N., Siegfried C.B. Helping Children in the Child Welfare System Heal from Trauma: A Systems Integration Approach. PsycEXTRA Dataset. [(accessed on 26 February 2021)];2005 Available online: https://calio.dspacedirect.org/handle/11212/3143.
- 128.Hillygus D.S. The MISSING LINK: Exploring the Relationship Between Higher Education and Political Engagement. Politi. Behav. 2005;27:25–47. doi: 10.1007/s11109-005-3075-8. [DOI] [Google Scholar]
- 129.Krogstad J.M., Fry R. More Hispanics, Blacks Enrolling in College, but Lag in Bachelor’s Degrees. [(accessed on 26 February 2021)]; Available online: https://www.pewresearch.org/fact-tank/2014/04/24/more-hispanics-blacks-enrolling-in-college-but-lag-in-bachelors-degrees/
- 130.Hayward M.D., Gorman B.K. The long arm of childhood: The influence of early-life social conditions on men’s mortality. Demography. 2004;41:87–107. doi: 10.1353/dem.2004.0005. [DOI] [PubMed] [Google Scholar]