Abstract
Emotional approach coping involves active attempts at emotional expression and processing in response to stressful circumstances. This study tested whether dispositional emotional approach coping processes predict changes in physical and mental health in community-dwelling older adults, particularly within the context of higher perceived stress. To test this, older adults (N = 150) completed assessments of emotional expression and emotional processing at study entry. They also completed measures of perceived stress, depressive symptoms, and ill-health (a composite of subjective and objective physical health indicators, which included blood draw for collection of biomarkers), every 6 months over 4.5 years. Emotional processing and emotional expression were not related significantly to ill-health at study entry. However, emotional processing (but not emotional expression) significantly predicted changes in ill-health. At higher levels of emotional processing, ill-health remained low and stable; at lower levels of emotional processing, ill-health increased over time. However, when perceived stress was high, higher emotional processing and emotional expression were related to lower depressive symptoms at study entry, but higher emotional processing was associated with increasing depressive symptoms over time. Emotional approach coping processes evidence prospective relations with health outcomes, which are partially conditioned by stress perceptions. Emotional processing appears to have a protective impact against declining physical health. Predictive relationships for depressive symptoms are more complex. Older adults with chronically high perceived stress might benefit from interventions that target emotion-regulating coping processes.
Keywords: emotional approach coping, emotional expression, emotional processing, depressive symptoms, older adults
Stressful experiences can disrupt emotional equilibrium and prompt the use of stable coping efforts aimed at regulating emotional responses (see Segerstrom & Smith, 2019). Such efforts can include a variety of strategies with the goal of up- or down-regulating positive or negative emotions (DeSteno, Gross, & Kubzansky, 2013), which in turn can affect physical and mental health. Researchers have increasingly turned attention toward understanding the relationships of approach-oriented, emotion-regulating coping with health (e.g., Smith, Lumley, & Longo, 2002). Evidence suggests older adults are more motivated to regulate negative affect than younger adults and are effective at doing so (Carstensen, 1992, 1995). This includes greater emotional control (Gross et al., 1997; Lawton, Kleban, Rajagopal, & Dean, 1992), less overall experiencing of negative affect (Carstensen, Pasupathi, Mayr, & Nesselroade, 2000; Carstensen et al., 2011; Kessler & Staudinger, 2009), and more success in blunting negative emotional responses to stressors (Birditt & Fingerman, 2003; Phillips, Henry, Hosie, & Milne, 2008; see also Charles & Carstensen, 2014). Older adults also tend to report less negative affect and more positive affect than younger cohorts (e.g., Charles, 2010).
How older adults effectively navigate stressful experiences requires additional investigation; the utility of emotional approach coping processes as predictors of physical and psychological health in community samples of older adults has received little study. Emotional approach coping involves the use of two distinct, yet overlapping, facets: emotional expression [EE] and emotional processing [EP]. EP reflects active attempts to acknowledge, explore, and understand emotions, whereas EE includes active verbal and/or nonverbal efforts to communicate or symbolize emotional experience (Stanton, Kirk, Cameron, & Danoff-Burg, 2000). Examination of independent, longitudinal relationships of EE and EP with health and depressive symptoms is the primary goal of the present study.
Emotional Approach Coping Processes
As a unitary construct, emotional approach coping involves “coping with adverse circumstances through intentionally processing and expressing emotions” (Stanton, 2011, p. 370). EE and EP, as facets of emotional approach coping, are specific strategies of coping and are elected in response to stressful experiences. These have included both dispositional (i.e., “indicate what you generally do, feel, and think when you experience stressful situations”) and situational (i.e., a specific stressor) measurement. Conceptual and empirical work on the development of emotional approach coping processes extends from the literature on stress and coping (Lazarus & Folkman, 1984) in response to the conclusion by Stanton and colleagues (1994) that across studies, emotion-focused coping was consistently associated with maladaptive outcomes. Noting the inconsistency of this observation with functionalist perspectives on emotion that suggest that expressing and processing emotions underlies successful self-regulation (Carver & Scheier, 1981; Frijda, 1986), they identified that widely used measures of emotion-focused coping were frequently confounded with distress and self-deprecation (see Stanton, 2011 for history of the construct).
Emotion-based coping is distinguishable from broader aspects of emotion regulation as it more narrowly focuses on reducing negative affect and managing specific stressful negative experiences (see Gross, 2014; Lazarus & Folkman, 1984); whereas emotion regulation includes processes related to the generation, timing, and expression of emotions (Ochsner & Gross, 2005) and can be measured on both expressive and avoidant dimensions (Gross & John, 2003). Well-established frameworks of emotion regulation can inform conceptualization of these emotion-regulating coping processes. For instance, Gross’s Process Model of Emotion Regulation outlines a normative emotional response trajectory with potential regulatory processes involved in response to a stressful external or internal event (Gross, 1998). The Process Model defines both cognitive (e.g., reappraisal) and behavioral (e.g., response modulation) dimensions that functionally overlap with coping by EP and EE, respectively. As such, expressing and processing emotion enables “emotional disturbances [to be] absorbed and decline to the extent that other experiences and behavior can proceed without disruption” (Rachman, 1980, p. 51) and might ultimately lead to greater mood repair (McFarland & Buehler, 1997) and physiological habituation (Foa & Kozak, 1986; Low, Stanton, & Danoff-Burg, 2006).
The growing body of research aimed at understanding the utility of coping through emotional approach suggests that EP and EE can carry a salutary impact on health (see Moreno, Wiley, & Stanton, 2017; Stanton, 2011). Stanton and Low (2012) identified support for a number of cognitive, affective, behavioral, and physiological mechanisms by which EE and EP might achieve effects on health. First, it appears that the processes of putting feelings to words can lessen emotional intensity and reduce amygdalar activation (e.g., Burklund, Creswell, Irwin, & Lieberman, 2014). Second, sharing common neural mechanisms with affect labeling (Burklund et al., 2014), processes of emotional approach coping reflect cognitive reappraisal and meaning-making from stressors to strengthen emotion regulation (e.g., Creswell et al., 2007; Pakenham, Smith, & Rattan, 2007; Pennebaker, Mayne, & Francis, 1997). Third, EP (and EE to a lesser extent) appears to enhance goal clarification and pursuit, thus directing attention toward goals that are of central importance and identifying barriers and pathways to goal achievement and problem-focused coping (Moreno et al., 2017; Pakenham et al., 2007; Stanton, Kirk, et al., 2000). As a fourth mechanism, coping through emotional approach processes might promote physiological habituation from sustained exposure to stressful events and improved autonomic recovery from stress arousal (e.g., Low, Stanton, & Bower, 2008; Low, Stanton, Thompson, Kwan, & Ganz, 2006; Stanton, Kirk, et al., 2000, Study 4), as well as higher heart rate variability (Seeley, Yanez, Stanton, & Hoyt, 2017). Finally, the use of EE serves to strengthen social relationships via willingness to express emotions with others and by way of helping individuals appropriately select and maximally draw upon their social environments (e.g., Carstensen, 1998; Manne et al., 2004).
Regarding physiological mechanisms, processes of emotional approach coping also might affect health by way of the immune system and particularly inflammation. Although acute, localized inflammation facilitates healing, chronic, systemic inflammation is associated with poorer health outcomes (see Couzin-Frankel, 2010). In a sample of young adults undergoing an acute laboratory stressor, higher dispositional use of EP was associated with a less pronounced increase in inflammatory markers in oral mucosal transudate (i.e., soluble tumor necrosis alpha receptor [sTNFα-RII] and interleukin-6 [IL-6]; note that the latter effect was not statistically significant after controlling for health behavior; Master et al., 2009). Among prostate cancer survivors, higher EP (controlling for EE) predicted lower plasma IL-6 and sTNF-RII four months later; in contrast, higher EE (controlling for EP) predicted higher sTNF-RII over time (Hoyt et al., 2013).
The Utility of Coping Through Emotional Expression and Processing
In the literature, emotional approach coping is often examined as a higher-order coping construct (see Stanton, 2011). Although studies measuring emotional approach coping as a unitary construct have shown associations with better adjustment to stressful circumstances (Cho, Park, & Blank, 2013; Juth, Dickerson, Zoccola, & Lam, 2015; Peters, 2006), EP and EE tend to share only moderate, positive correlations with each other (see Moreno et al., 2017). Thus, distinctions between EE and EP are common when these facets are examined separately (e.g., Hoyt et al., 2013; Stanton et al., 2000).
Understanding the differences (and similarities) in associations of EP and EE with health remains somewhat speculative. Notably, EE most often involves a shared process and so aspects of the social environment, including receptivity to emotional expression, may be critical to its adaptive utility (e.g., Hoyt, 2009). Such a process would manifest empirically as a significant interaction between EE and social variables on adaptive outcomes. EP, however, can be partially differentiated by its involvement of focused attention on stress-related emotions, and thus theoretically has been considered as a form of repetitive thought (see Watkins, 2008). In fact, in some studies EP (and not EE) has been shown to be positively correlated with rumination (Moreno et al., 2017), including depressive rumination and pervasive worry (Segerstrom, Stanton, Alden, & Shortridge, 2003, Study 1). It is also possible that EE and EP rely on different mechanisms to influence physical and mental health. EE and EP might be differentially related to different aspects of health or to different facets of psychological well-being (e.g., positive vs. negative affect).
Evidence suggests that EE and EP can have somewhat distinct effects. Among breast cancer patients, for example, higher cancer-related EE was associated longitudinally with less distress, while more EP predicted increased distress when EE was controlled (Stanton, Danoff-Burg, et al., 2000). Similarly, in a longitudinal study of women with metastatic breast cancer an increase in EE predicted improvements in depressive symptoms and life satisfaction, whereas EP at study entry predicted increased depressive symptoms and declining life satisfaction among highly expressive women (Stanton & Low, 2012). Conversely, among prostate cancer patients, declines in EP (but not in EE) predicted decrements in prostate-specific physical functioning (Hoyt, Stanton, Irwin, & Thomas, 2013). Such equivocal findings, particularly those related to EP warrant further investigation. Attempts at EP are not universally adaptive. When constructive, EP is intentional, goal-oriented, and facilitates dynamic problem-solving and values clarification (Hoyt, Austenfeld, & Stanton, 2016). However, when unconstructive, EP might involve repetitive or prolonged focus on negative emotional material that can maintain or even amplify negative emotional states (e.g., rumination, worry; Ehring & Watkins, 2008; Morrow & Nolen-Hoeksema, 1990). Tendencies toward perceiving daily circumstances as stressful, overwhelming, or uncontrollable might facilitate such unconstructive EP.
The question of whether EE and EP predict favorable adjustment has been addressed largely with regard to psychological outcomes. The potential benefit of EP or EE on markers of physical health and physiological function has not been examined as frequently, but salutary effects are suggested. Coping through EP was related to lower chronic pain in myofascial pain patients (Smith et al., 2002), longer survival in breast cancer patients (Reynolds et al., 2000), and efficacy of metabolic control in adolescents with Type 1 diabetes (Hughes, Berg, & Wiebe, 2012). EE was related to fewer medical appointments and better perceived physical health in breast cancer patients (Stanton, Danoff-Burg, et al., 2000).
Although findings generally suggest that emotional approach coping processes enhance physical and psychological adjustment, contextual and individual factors condition its influence. These factors include sex and gender-related processes (Hoyt, 2009; Hoyt et al., 2013; Stanton et al., 1994, Study 2), qualities of the stressor (Stanton et al., 1994, 2000), and close others’ receptivity to shared feelings (Hoyt, 2009; Stanton, Danoff-Burg, et al., 2000).
Emotional Approach Coping in Older Adulthood
Developmental processes may shape the use and utility of emotional approach coping processes. Socioemotional Selectivity Theory (SST; Carstensen, 2006; Carstensen, Isaacowitz, & Charles, 1999) is a motivational theory that posits that individuals select actions that maximize life satisfaction in a way that is consistent with their placement in the life span. It has been used to explain why and how emotional wellbeing changes across the life span. According to SST, when older adults appraise their circumstances as threatening or stressful, they often rely on accrued experience and knowledge to better navigate emotional problems and social conflicts compared to younger adults where circumstances are more likely to be novel (Carstensen et al., 2011). Additionally, older adults prioritize present-oriented emotional and interpersonal goals over future-oriented, knowledge-based goals (Carstensen, 2006). In general, older individuals develop better self-regulatory skills over time that include both cognitive and behavioral strategies for regulating stress-related emotional responses and maintaining a focus on pursuing valued actions (Heckhausen, Wrosch, & Schulz, 2010).
Despite such enhanced motivation and skill to regulate stress-related emotional responses, the Strength and Vulnerability Integration (SAVI) model acknowledges that specific age-related physiological and behavioral vulnerabilities might challenge the ability to regulate negative emotions (Charles, 2010). For instance, Charles (2010) suggests that decreasing flexibility in cardiovascular and HPA axis activity in older age impairs recovery from emotional stressors. Additionally, increased social isolation, neurological changes (e.g., decrease in working memory or attentional control), and increased health-related stressors are circumstances that could hinder the cognitive and behavioral attempts at coping through emotional approach processes. In fact, elevations in perceived stress may itself constitute vulnerability, particularly when stressors are chronic, unpredictable, and uncontrollable (e.g., a deteriorating health condition). At higher levels of perceived stress, failures in constructive attempts to process emotions could result in prolonged negative affect, and ultimately health-impairing physiological imbalance (Piazza, Almeida, Dmitrieva, & Klein, 2010).
Failures in effective regulation of emotion may come at a high physiological cost to older adults (Kunzmann et al., 2019). Decrements in emotion regulation can lead to greater physiological reactivity and poorer recovery from the stress response compared to younger adults (e.g., Piazza, Charles, Stawski, & Almeida, 2013). To date, only limited evidence suggests coping by emotional approach could yield impact on immune markers in older adults. In an experimental writing study, older adults were assigned either to induced EP and EE through writing about upsetting events or to a “time-management” control writing condition (Koschwanez et al., 2013). Written expressive disclosure significantly accelerated wound healing after punch biopsy compared to control writing (but had no effect on depressive symptoms).
The Current Study
This investigation is the only study to date to examine EE and EP in community-dwelling older adults, to our knowledge, and one of the few to examine the association of coping through EE and EP on an indicator of physical health composed of objective and subjective markers. The aim was to examine whether the dispositional tendency to cope through emotional processing and/or expression predicts change in physical health and depressive symptoms over time in this population. This study addresses specific gaps in the emotional approach coping literature by examining the potential of coping through EE and EP to benefit physical health over time and also to inform under what context these emotional approach coping processes might benefit or worsen depressive symptoms in older adults, with a focus on the chronic stress perceptions. Differences in the adaptive utility of EE and EP are likely to emerge with higher stress perceptions. Whereas EE may benefit health by promoting resolution of stress-related emotions or garnering involvement of a supportive other, during relatively high stress perceptions EP has potential to maintain negative emotion via negative repetitive thinking.
We hypothesized that more use of EP and EE would be associated with better physical and psychological health over time in older adults. Furthermore, we examined whether EP and EE moderate the impact of perceived stress on longitudinal trajectories of physical health and depressive symptoms. We expected that coping through EE would likely mitigate the negative impact of higher levels of perceived stress on health, whereas coping through EP in the presence of higher stress would be related to declining health and increasing depressive symptoms.
Method
Participants
Participants were 150 community-dwelling, older adults recruited from a community registry maintained by the Sanders-Brown Center on Aging at the University of Kentucky as part of a longitudinal study of health and aging (see Segerstrom, 2014; Segerstrom, Eisenlohr-Moul, Evans, & Ram, 2015; Segerstrom, Roach, Evans, Schipper, & Darville, 2010). The overall objective of the study was to examine stressful events and aging, including examining the health impact of stressful life events in married couples. Thus, only married individuals were eligible. In addition, all participants were 60 years of age or older (range 60–93) at study entry (see Table 1). In addition, participants reported existing health conditions at rates consistent with expected prevalence rates: Hypertension (71%), hyperlipidemia (50%), heart disease (39%), Parkinson’s disease (19%), and diabetes (10%).
Table 1.
Participant Characteristics (N = 150)
| Characteristic | % or M (SD) |
|---|---|
| M Age | 74.7 (SD = 6.2) |
| Gender (%) | |
| Female | 58 |
| Male | 42 |
| Ethnicity (%) | |
| White (non-Hispanic) | 96 |
| African American/Black | 4 |
| M Education (in years) | 15.9 (SD = 2.5) |
| Annual household income (%) | |
| $15,000 or less | 1.6 |
| $15,001–$45,000 | 26.9 |
| $45,001–$75,000 | 36.5 |
| $75,001–$100,000 | 12.2 |
| $100,001 or more | 22.8 |
To maximize integrity of assessments of immune parameters, exclusion criteria included diseases or disorders affecting the immune system, chemotherapy or radiation treatment within the past 5 years, unwillingness to undergo vaccination or venipuncture, immunomodulatory medications (e.g., opiates), and more than two of the following classes of medication: psychotropics, antihypertensives, hormone replacement, or thyroid supplements. To avoid dependency in the data, only one member of a married dyad was included in the current study. If the initially recruited member declined participation, then the partner was subsequently invited.
Procedure
After study procedures were approved by the University of Kentucky Institutional Review Board, potential participants were identified from a university-based volunteer subject pool and were contacted and screened by telephone. Following enrollment and informed consent, participants completed questionnaires verbally with a research assistant. Interviews took place at 6-month intervals. Participants received a $20 gift card at each completed wave. The current analysis uses data over 4.5 years: Wave 1 to Wave 10. Of the 150 participants who completed Wave 1, 135 completed Wave 2; 124, Wave 3; 117, Wave 4; 111, Wave 5; 109, Wave 6; 100, Wave 7; 92, Wave 8; 56, Wave 9; 34, Wave 10. Thus, a total of 1,028 complete person-waves were used in analyses.
Study completers did not differ from those not completing all 10 waves on age, education level, income, ethnicity, or on any EP, EE, or dependent variables. Missingness at later waves was due to participant dropout (N = 64) and mortality (N = 6). Finally, participants who had a later wave 1 enrollment date were unable to complete waves 8 through 10 before study end (N = 43). Because most of the attrition was due to later study start date, it is mainly ‘missingness completely at random’ and will not bias results. However, the primary predictor of attrition not due to start date was participant age at study entry. Thus, we adjust for age in statistical models to ameliorate this potential bias.
Measures
Emotional approach coping.
Emotional approach coping processes were measured at the first interview using the Emotional Approach Coping Scales (Stanton et al., 2000), which consist of the 4-item EP (e.g., “I take time to figure out what I’m really feeling”) and 4-item EE (e.g., “I feel free to express my emotions”) scales. Participants were instructed to complete items in reference to how they typically respond to problems and stressful experiences on a 4-point response scale (1 = I do not do this at all; 4 = I do this a lot). Both emotional approach coping subscales have been shown to demonstrate sound internal consistency and predictive validity (see Austenfeld & Stanton, 2004). In the current study, Cronbach’s alpha was .72 for EP and .82 for EE.
Perceived stress.
General stress perceptions were measured by the Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983) at each interview wave. The 10 questions assess the degree to which individuals appraise their lives as stressful (e.g., unpredictable, uncontrollable, overloaded) “in the last 30 days” (e.g., “How often have you felt that you were unable to control the important things in your life?”). Response options range from 0 (none of the time) to 4 (all of the time), and items are summed so that higher scores indicated greater perceived stress (possible range: 0–40). Calling upon variance decomposition methods (Cranford et al., 2006), we determined that PSS was reliable between individuals at each wave (R1F = .98) and within individuals across waves (RC = .76)1.
Ill-health.
Ill-health was assessed at each wave and computed as a composite score of three objective and one subjective components: Interleukin-6 (IL-6), beta2-microglobulin (β2 µ), an index of chronic disease (Clark, Von Korff, Saunders, Baluch, & Simon, 1995), and self-reported health. These components all reflect general health, and each individual component prospectively predicts morbidity and mortality (Clark et al., 1995; De-Salvo, Bloser, Reynolds, He, & Muntner, 2006; Volpato et al., 2001). The combination of measures more accurately captures a person’s overall health than any individual measure in isolation (Boggero, Eisenlohr-Moul, & Segerstrom, 2016). To create the composite ill-health variable, Z-scores were computed for each of the variables and averaged. Higher scores reflect worse overall health. The composite variable was reliable between individuals at each wave (R1F = .90) and within individuals across waves (RC = .81).
With regard to the individual components, IL-6 and β2 µ were used as biomarkers of inflammation. IL-6 is a proinflammatory cytokine secreted by T cells and macrophages (Clark, 2008). β2 µ is a protein expressed on the surface of immune cells as part of the histocompatibility complex and is a good indicator of cellular immune activation (Clark, 2008). β2 µ in the bloodstream is higher in individuals with viral infection, cancer, and other chronic inflammatory disorders and is elevated in those with chronic inflammatory disorders compared with healthy controls (Amighi et al., 2011; Bethea & Forman, 1990; Buchwald, Wener, Pearlman, & Kith, 1997; Cooper & Plesner, 1980; Yılmaz, Köklü, Yüksel, & Arslan, 2014).
Sera were frozen at –80 °C and analyzed in annual batches using high-sensitivity ELISA kits for IL-6 (R&D Systems, Minneapolis, MN). Mean intraassay coefficient of variance for all IL-6 assays was 1.9% and the mean interassay coefficient of variance was 4.5%. To improve normality, IL-6 and β2 µ results were log-10 transformed. β2 µ was assessed using ALPCO (Salem, NH) diagnostic β2 µ immunoassay kits. Mean intraassay coefficient of variance for all β2 µ assays was 2.9% and the mean interassay coefficient of variance was 3.9%. Inflammatory marker data for waves at which individuals currently had an acute infection (n = 8) or cancer (n = 2) or had undergone surgery requiring hospitalization in the past 6 months (n = 6) were removed.
The Chronic Disease Score (CDS), a measure of chronic disease severity calculated from weighted pharmacy data, age, and sex, predicts total medical costs and correlates strongly with mortality, hospitalizations, self-rated health, and self-reported disability (Clark et al., 1995; Putnam et al., 2002). At each wave, participants provided a list of current medications, which were coded into medication classes, and each medication class was multiplied by its empirically derived weight. To avoid having overlapping predictors and dependent variables, the CDS was computed without the gender and age adjustments.
Self-rated health was measured using a single item from the Medical Outcomes Study Health-Related Quality of Life scale (Stewart & Ware, 1992). Using a 5-point scale ranging from (1 = excellent; 5 = poor), participants are asked to rate their “general” health. Higher scores reflect worse self-rated health. Self-rated health is a good predictor of mortality, with those reporting “poor” health having a twofold increase in mortality risk relative to those reporting “excellent” health (DeSalvo et al., 2006).
Depressive symptoms.
The Geriatric Depression Scale (GDS; Yesavage et al., 1982) is designed to measure depressive symptoms in older adults without conflation with unrelated somatic complaints. Participants responded to 30 yes/no items (e.g., “Do you often feel downhearted?”) in reference to the past week. Responses are summed to yield a score ranging from 0 to 30. GDS scores ranging from 0 to 9 are considered to be within the normal range, scores between 10 and 19 are suggestive of “mild” depressive symptoms, and scores greater than 20 suggest more significant depressive symptoms (Yesavage et al., 1982). The GDS has demonstrated validity and reliability (Yesavage et al., 1982). Because GDS responses were dichotomous, reliability was calculated on 5 parcels of 6 items. To account for allocation variability, 150 data sets, each with random allocation of items to parcels, were created; reliability was calculated for each one, and the mean and range across the 150 data sets were obtained (Sterba & MacCallum, 2010; Sterba & Rights, 2016). The GDS was reliable between individuals at each wave (mean R1F = 0.82, range = 0.81–0.83) and within individuals across waves (mean RC = 0.75, range = 0.73–0.77).
Demographics.
Participants reported their age, level of education, income, ethnicity, height and weight, and other sociodemographic variables at the first interview.
Data Analysis
The aims of this study were to examine whether EP and EE at study entry predict patterns of change over 4.5 years in physical and mental health indictors (i.e., ill-health and GDS), and whether EP and EE moderate the relationship of stress and trajectories of the two outcomes over time. Multilevel models were conducted using the Hierarchical Linear Modeling program (HLM; Bryk & Raudenbush, 1992). Because we assumed that GDS and ill-health fluctuated over time, it was useful to assess the extent to which total variance in these variables was due to within-person change relative to individual differences using the intraclass correlation (ICC; Raudenbush & Bryk, 2002). An ICC that is close to 0 indicates that variability is attributable mostly to within-person changes, and a correlation that is close to 1 suggests that variability is attributable mostly to individual differences (Snijders & Bosker, 1993). We calculated ICC before conducting the HLM analyses.
The ICC for PSS was .65, suggesting both stable between-person differences and within-person changes. Therefore, the PSS was centered within person (Enders & Tofighi, 2007) such that each person had a between-person, Level 2 predictor that constituted that person’s PSS mean across all time points and a within-person, Level 1 predictor that constituted the change from that person’s PSS mean at each time point.
A two-level model was designated in which 10 waves of interviews were nested within each participant. Dependent variables were within-person (level-1) variables in which the outcome for each person at each time point was a function of the person’s own intercept, the effect of time, within-person changes in stress, and an error term. EP, EE, and PSS means were between-person (level-2) variables. Time was centered at Wave 1, and coded as wave number (i.e., 0 to 9).
Level 1–Within individual:
| (1) |
Then, level-2 predictors (EP and EE) of the intercepts and slopes, as well averaged person-level PSS, were added to the models. EP and EE were examined in separate HLM models.
Level 2–Between individual:
| (2) |
| (3) |
| (4) |
EP and EE were centered around the mean. Regression coefficients were estimated using restricted maximum-likelihood estimation (Bryk & Raudenbush, 1992). An unrestricted variance-covariance structure, that is, a full covariance matrix in which every variance and covariance is free to be estimated from the data, was specified. Results are reported as γ weights (analogous to an unstandardized beta weight) with their associated t tests.
Using –2 log likelihood to determine the incremental improvement in model fit, a significant improvement in fit was obtained when random effects were included for time (change in the model –2 log likelihood = 20.60 and 62.01, df = 2, p < .001, for the GDS and ill-health models, respectively) and PSSwithin (change in the model –2 log likelihood = 103.92 and 7.94, df = 3, p < .001 and .05, for the GDS and ill-health models, respectively). Thus, time and PSS were treated as random effects.
Interactions were plotted following recommended procedures (Preacher, Curran, & Bauer, 2006) for HLM two-way and three-way interactions, with conditional, centered values of PSS, EP, and EE set at 1 SD above and below the mean. Models predicting ill-health included body mass index (BMI) as a statistical covariate.
Given the number of outcomes examined, we also considered results when applying a false discovery rate correction following recommended procedures (Benjamini & Hochberg, 1995). We estimated the proportion of expected Type I errors (i.e., false discovery rate) as an alternative to the overly strict Bonferroni correction. The false discovery rate was set to be .05 in this study. We calculated the Benjamini and Hochberg threshold for p values for the eight tests of interaction effects (i.e., between and within) predicting mental and physical health.
Results
Descriptive Statistics
Table 2 contains descriptive statistics. Average scores of emotional approach coping (EP: M = 2.81, SD = 0.66; EE: M = 2.84, SD = 0.74) were slightly higher than observations in a healthy young adult sample (EP: M = 2.61, SD = 0.62; EE: M = 2.45, SD = 0.71; Stanton et al., 2000, Study 1). Neither EE nor EP scores in the current study differed by gender.
Table 2.
Means (Standard Deviations) for Study Variables Across Time
| Variable | Wave 1 (n = 150) |
Wave 2 (n = 135) |
Wave 3 (n = 124) | Wave 4 (n = 117) |
Wave 5 (n = 111) |
Wave 6 (n = 110) |
Wave 7 (n = 103) |
Wave 8 (n = 95) |
Wave 9 (n = 60) |
Wave 10 (n = 36) |
|---|---|---|---|---|---|---|---|---|---|---|
| EP | 2.81 (0.66) | — | — | — | — | — | — | — | — | — |
| EE | 2.84 (0.74) | — | — | — | — | — | — | — | — | — |
| PSS | 10.7 (6.50) | 11.7 (5.80) | 11.8 (6.50) | 12.0 (5.90) | 11.5 (6.20) | 12.0 (6.10) | 12.0 (6.00) | 11.2 (5.40) | 12.0 (6.00) | 11.5 (4.70) |
| GDS | 4.25 (4.24) | 3.99 (3.81) | 4.16 (3.76) | 3.79 (3.31) | 3.79 (3.30) | 3.85 (3.59) | 4.25 (3.74) | 3.84 (3.46) | 3.85 (3.27) | 3.48 (2.64) |
| Ill-Health | −.02 (.72) | .05 (.65) | −.09 (.56) | −.03 (.58) | −.10 (.61) | −.06 (.67) | .06 (.82) | .14 (.74) | .11 (.76) | .05 (.79) |
| SRH | 2.31 (0.85) | 2.40 (0.89) | 2.29 (0.85) | 2.34 (0.78) | 2.30 (0.91) | 2.32 (0.86) | 2.36 (0.89) | 2.41 (0.82) | 2.39 (0.81) | 2.41 (0.99) |
| IL-6 | 0.57 (0.54) | 0.56 (0.65) | 0.34 (0.27) | 0.36 (0.27) | 0.32 (0.28) | 0.31 (0.31) | 0.31 (0.33) | 0.37 (0.33) | 0.37 (0.29) | 0.35 (0.33) |
| β2µ | 0.29 (0.41) | 0.49 (0.31) | 0.48 (0.31) | 0.53 (0.27) | 0.51 (0.28) | 0.52 (0.26) | 0.52 (0.32) | 0.52 (0.28) | 0.43 (0.32) | 0.45 (0.31) |
| CDS | 1133.58 (503.61) | 1071.94 (453.97) | 984.86 (430.07) | 986.71 (400.61) | 994.30 (395.54) | 1005.67 (454.50) | 1202.20 (576.72) | 1176.08 (474.61) | 1244.11 (593.71) | 1221.80 (483.16) |
Note. EP = emotional processing; EE = emotional expression; PSS = Perceived Stress Scale; GDS = Geriatric Depression Scale; SRH = self-reported health; IL-6 = Interleukin-6; β2µ = beta2-microglobulin; CDS = chronic disease score.
Measured at Wave 1, EP and EE were moderately correlated, r = .49, p < .001. EP was unrelated to averaged (within person, across time) ill-health, r = –.14, p = .10 and averaged (within person, across time) PSS, r = –.10, p = .24, and negatively correlated with averaged depressive symptoms, r = –.22, p = .008. EE was unrelated to averaged ill-health, r = –.08, p = .33 and negatively correlated with averaged depressive symptoms, r = –.32, p < .001 and averaged PSS, r = –.20, p = .02.
Scores on the GDS are similar to those reported in a comparable sample of older adults (Knight, McMahon, Green, & Skeaff, 2004). At study entry, the majority (88.7%) of participants reported depressive symptoms within the normal range; however, 10% reported symptoms considered mild or moderate with the remaining (n = 2) reporting symptoms suggesting more significant depression. PSS scores ranged from 10.7 to 12.0 (SD = 5.4 –6.4) across time points and are similar to those of a Dutch sample of community-dwelling older adults (M age = 74.3, SD = 7.5; M PSS = 11.6, SD = 5.7; Korten, Comijs, Penninx, & Deeg, 2017).
Multilevel Modeling Predicting Changes in Health and Depressive Symptoms
Examination of ICCs suggested sufficient variance at each level for ill-health and depressive symptoms. The ICC was .72 for ill-health, indicating that 72% of the variance was attributable to individual differences, with the remainder (28%) representing fluctuations within persons over time. The ICC was .73 for GDS, indicating that 73% of the variance was attributable to individual differences, with 27% representing fluctuations within persons over time.
Preliminary analyses were conducted to inspect how ill-health and GDS changed over time by testing models with time as the only predictor. The slope coefficient for ill-health was positive and statistically significant (γ= 0.03, SE = 0.01, t(149) = 3.84, p < .001), indicating that, on average, ill-health scores increased 0.03 units at each wave (i.e., a 0.03 change on a z-score scale over the course of the study). There also was substantial individual variability in slopes (likelihood ratio test for the presence of a random slope: χ2(134) = 315.14, p < .001), indicating that some individuals might have had stable levels of ill-health while others changed over time. The slope coefficient for GDS was not significantly different from zero (γ= 0.04; SE = 0.04; t(149) = 1.11, p = .27). However, substantial variability was evident in individuals’ slopes over time (likelihood ratio test for the presence of a random slope: χ2(134) = 221.68, p < .001). Thus, significant individual differences existed in the shape of the trajectories of ill-health and GDS that could be predicted from EE and EP.
We then assessed whether EP or EE, PSS (between and within person), and their interactions were associated with health outcome intercepts and slopes. Tables 3 and 4 present a summary of results.
Table 3.
Hierarchical Linear Model: Emotional Processing
| GDS |
Ill-Healtha |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | γ | SE | t | df | p < | γ | SE | t | df | p < |
| Fixed effects | ||||||||||
| Intercept | 4.15 | 0.21 | 19.50 | 145 | .001 | −0.04 | 0.05 | −0.81 | 144 | .42 |
| Within–person level | ||||||||||
| Time (γ10) | 0.02 | 0.03 | 0.72 | 146 | .47 | 0.03 | 0.01 | 3.90 | 146 | .001 |
| PSSwithin (γ20) | 1.73 | 0.26 | 6.52 | 148 | .001 | 0.04 | 0.04 | 1.13 | 148 | .26 |
| Between–person level | ||||||||||
| Intercept effects (Wave 1) | ||||||||||
| EP (γ01) | −1.20 | 0.43 | −2.81 | 145 | .006 | −0.04 | 0.07 | −0.62 | 144 | .54 |
| PSSbetween (γ02) | 4.91 | 0.51 | 9.54 | 145 | .001 | 0.18 | 0.10 | 1.78 | 144 | .08 |
| EP × PSSbetween (γ03) | −2.86 | 0.96 | −2.97 | 145 | .004 | 0.09 | 0.12 | 0.69 | 144 | .49 |
| Slope effects (cross–level interaction) | ||||||||||
| EP × PSSwithin (γ21) | 0.05 | 0.46 | 0.10 | 148 | .92 | 0.07 | 0.05 | 1.33 | 148 | .19 |
| EP × Time (γ11) | 0.09 | 0.06 | 1.56 | 146 | .12 | −0.03 | 0.01 | −2.06 | 146 | .04 |
| PSSbetween × Time (γ12) | −0.00 | 0.06 | −0.04 | 146 | .97 | 0.02 | 0.01 | 1.06 | 146 | .29 |
| EP × PSSbetween × Time (γ13) | 0.37 | 0.13 | 2.90 | 146 | .004b | 0.02 | 0.03 | 0.88 | 146 | .38 |
| Random effects | Variance | χ2 | df | p < | Variance | χ2 | df | p < | ||
| Intercept | 5.62 | 480.09 | 118 | .001 | 0.29 | 512.14 | 117 | .001 | ||
| Time | 0.03 | 161.45 | 119 | .006 | 0.00 | 275.69 | 119 | .001 | ||
| PSSwithin | 4.61 | 286.56 | 121 | .001 | 0.02 | 133.66 | 121 | .20 | ||
| Residual | 2.81 | 0.12 | ||||||||
| Δχ2(7) = 4446.68 | Δχ2(7) = 1279.04 | |||||||||
Note. PSS = Perceived Stress Scale; GDS = Geriatric Depression Scale; EP = emotional processing. Bold values indicate p < .05.
Results controlled for body mass index (BMI).
Critical p-value with false discovery rate correction = .038.
Table 4.
Hierarchical Linear Model: Emotional Expression
| GDS |
Ill-Healtha |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | γ | SE | t | df | p < | γ | SE | t | df | p < |
| Fixed effects | ||||||||||
| Intercept | 4.07 | 0.23 | 18.08 | 145 | .001 | −0.06 | 0.05 | −1.27 | 144 | .21 |
| Within–person level | ||||||||||
| Time (γ10) | 0.02 | 0.03 | 0.84 | 146 | .40 | 0.03 | 0.01 | 3.63 | 146 | .001 |
| PSSwithin (γ20) | 1.70 | 0.26 | 6.43 | 148 | .001 | 0.04 | 0.04 | 1.18 | 148 | .24 |
| Between–person level | ||||||||||
| Intercept effects (predicting Wave 1 level) | ||||||||||
| EE (γ01) | −0.78 | 0.37 | −2.10 | 145 | .04 | 0.06 | 0.07 | 0.87 | 144 | .39 |
| PSSbetween (γ02) | 4.77 | 0.53 | 8.97 | 145 | .001 | 0.21 | 0.09 | 2.30 | 144 | .02 |
| EE × PSSbetween (γ03) | −2.32 | 0.83 | −2.81 | 145 | .006 | −0.24 | 0.11 | −2.14 | 144 | .03 |
| Slope effects (cross–level interaction) | ||||||||||
| EE × PSSwithin (γ21) | −0.62 | 0.36 | −1.76 | 148 | .08 | 0.05 | 0.04 | 1.19 | 148 | .24 |
| EE × Time (γ11) | 0.02 | 0.05 | 0.39 | 146 | .70 | −0.01 | 0.01 | −0.51 | 146 | .61 |
| PSSbetween × Time (γ12) | −0.02 | 0.06 | −0.29 | 146 | .78 | 0.02 | 0.02 | 1.10 | 146 | .29 |
| EE × PSSbetween × Time (γ13) | 0.22 | 0.09 | 2.37 | 146 | .02b | −0.00 | 0.02 | −0.14 | 146 | .89 |
| Random effects | Variance | χ2 | df | p < | Variance | χ2 | df | p < | ||
| Intercept | 5.80 | 480.97 | 118 | .001 | 0.28 | 500.62 | 117 | .001 | ||
| Time | 0.04 | 170.26 | 119 | .002 | 0.00 | 283.54 | 119 | .001 | ||
| PSSwithin | 4.47 | 298.15 | 121 | .001 | 0.02 | 135.09 | 121 | .18 | ||
| Residual | 2.81 | 0.12 | ||||||||
| Δχ2(7) = 4453.51 | Δχ2(7) = 1283.76 | |||||||||
Note. PSS = Perceived Stress Scale; GDS = Geriatric Depression Scale; EE = emotional expression. Bold values indicate p < .05.
Results controlled for body mass index (BMI).
Critical p-value with false discovery rate correction = .025.
Emotional processing.
Neither EP nor PSSbetween predicted levels of ill-health at Wave 1, nor did PSSwithin predict ill-health across time. However, in a significant EP by time interaction, EP predicted changes in ill-health over 4.5 years. Simple slopes of EP over time are depicted in Figure 1 at relatively high (+1 SD) and low (–1 SD) levels of EP. At higher levels of EP, ill-health remained low and stable over time (γ= 0.01, SE = 0.01, t = 1.03, p = .30). However, at lower levels of EP, ill-health significantly increased over time (γ= 0.05, SE = 0.01, t = 3.80, p < .001).
Figure 1.
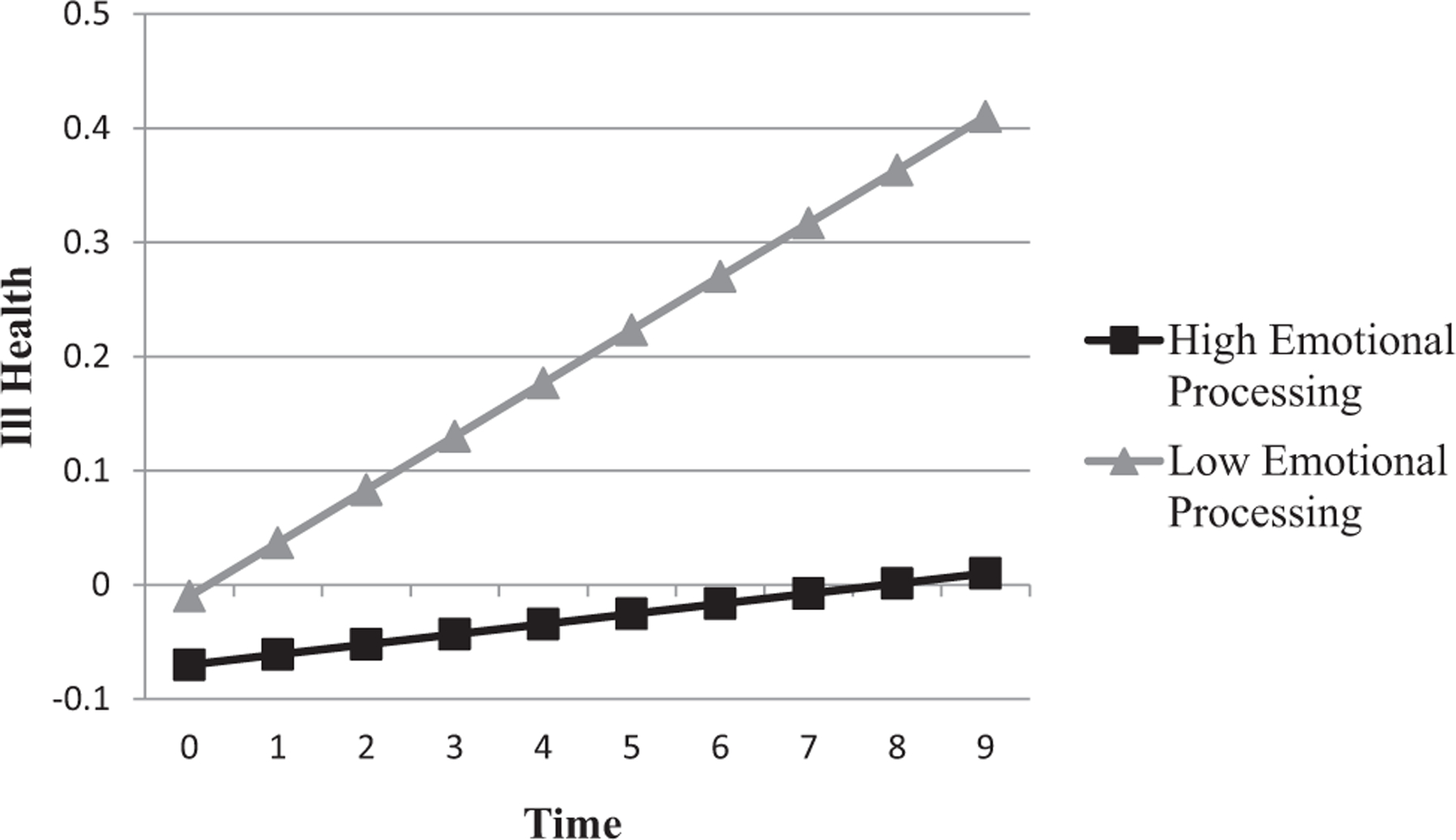
Emotional processing and change in ill health over time.
At Wave 1, higher EP and lower PSSbetween were related to lower GDS scores. In addition, decreases in PSSwithin were correlated with decreases in GDS scores. However, the between-person effect was qualified by a statistically significant EP* PSSbetween interaction for Wave 1 GDS (see Table 3). At study entry, higher EP was related to lower depressive symptoms only for those with high levels of perceived stress (at high PSSbetween: γ = –3.09, SD = 0.91, t = –3.38, p < .001; at low PSSbetween: γ = 0.69, SD = 0.58, t = 1.18, p = .24).
Increases in PSSwithin were associated with increases in depressive symptoms. However, the EP*PSSwithin interaction was not significantly related to depressive symptoms.
In the context of change in GDS over time, neither EP nor PSSbetween had a significant main effect. However, the interaction of EP and PSSbetween was significantly associated with the slope of GDS (see Figure 2a), and this effect withstood the false discovery rate correction.
Figure 2.
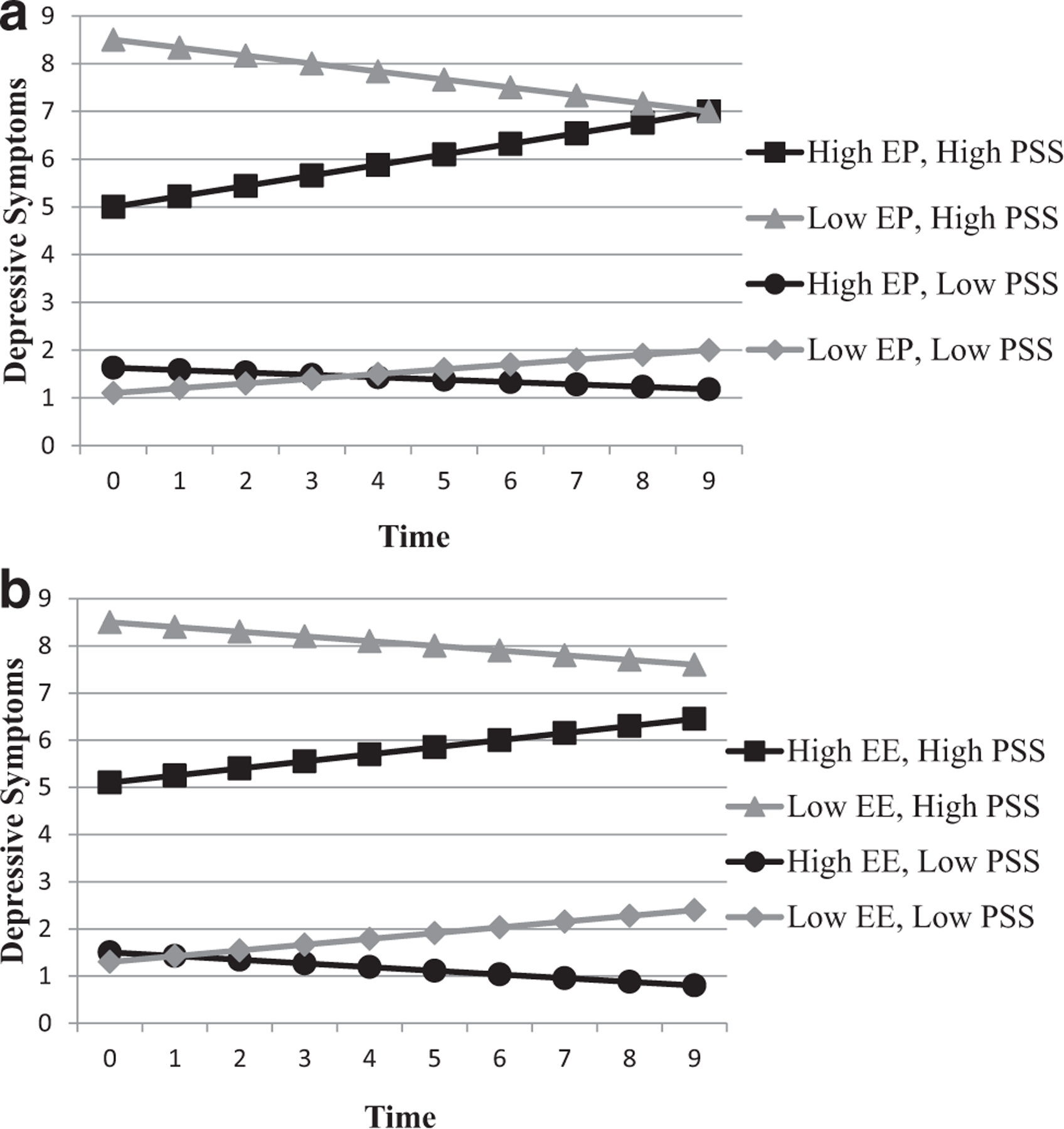
Interaction of EE and EP with PSSbetween on change in depressive symptoms over time. EE = emotional expression; EP = emotional processing; PSS = Perceived Stress Scale.
At relatively high perceived stress, higher EP predicted increasing GDS (γ = 0.22, SD = 0.05, t = 3.97, p < .001), whereas the simple slope for low EP showed a nonsignificant trend of decreasing depressive symptoms over time; (γ = –0.18, SD = 0.10, t = –1.79, p = .07). At low perceived stress, the simple slope for high EP was not statistically significant (γ = –0.05, SD = 0.07, t = –0.60, p = .55). The simple slope for low EP was statistically significant (γ = 0.09, SD = 0.04, t = 2.17, p = .03).
Emotional expression.
EE was not significantly associated with either the intercept or slope of ill-health. Increases in PSSwithin predicted increases in depressive symptoms. The EE* PSSwithin interaction significantly predicted ill-health at wave 1(see Table 4). At study entry, higher EE was related to higher ill-health only for those with low levels of perceived stress (at high PSSbetween: γ = –0.11, SD = 0.09, t = –1.10, p = .27; at low PSSbetween: γ = 0.22, SD = 0.10, t = 2.12, p = .04).
The EE* PSSbetween interaction significantly predicted depressive symptoms. At study entry, higher EE was related to lower depressive symptoms only for those with high levels of perceived stress (at high PSSbetween: γ = –2.40, SD = 0.82, t = –2.93, p = 0.004; at low PSSbetween: γ = 0.84, SD = 0.52, t = 1.63, p = .11).
In the context of change in GDS over time, neither EE nor PSSbetween had a significant main effect. However, the interaction between EE and PSSbetween significantly predicted the slope of GDS (see Figure 2b), and this effect withstood the false discovery rate correction. EE was not associated with changes in depressive symptoms in the context of high perceived stress (γ = 0.11 and –0.08, SD = 0.06 and 0.08, t = 1.35 and –1.210, p = .18 and .27 for high and low EE, respectively). At low perceived stress, there was an association of low EE with increasing GDS that approached statistical significance (γ = 0.11, SD = 0.06, t = 1.82, p = .07), but no significant association was observed for high EE (γ = –0.04, SD = 0.04, t = –1.06, p = .29).
Additional Analyses
Post hoc tests.
Post hoc models evaluated whether results differed as a function of participant gender or the presence of quadratic effects. No significant gender differences or quadratic effects were observed. Further, all models predicting GDS were repeated using GDS with a log-10 transformation. Results did not change significantly in magnitude, direction, or significance.
Sensitivity analyses.
As EP and EE were moderately correlated, r = .49, p < .001, analyses were repeated using a combined EP and EE model. The overall pattern of results did not change. However, the EP by time interaction fell just below statistical significance (p = .07); however, the strength and direction of the relationship did not change substantially and so the hypothesized separate models were retained. Likewise, the EE x EP interaction was tested to examine the possibility that coping by processing and expressing emotions have synergistic impact on health. However, the interaction terms were nonsignificant.
Discussion
Emotional approach coping processes have been associated with better adjustment to a variety of stressful circumstances, with the preponderance of evidence coming from studies of individuals with chronic illness. In the current study, lower dispositional coping through EP had a linear relationship with increasing ill-health over 4.5 years in this sample of older adults. Perhaps individuals who seldom cope through EP have little willingness or ability to engage with difficult emotions intentionally and actively. This denies opportunity for dynamic problem-solving, meaning-making, and resolution of emotions, which ultimately might contribute to prolonged physiological arousal and ill-health (Monin, Schulz, Lemay, & Cook, 2012).
Findings were more complex with regard to depressive symptoms. Cross-sectional data (at Wave 1) suggested a salutary relation of EE and EP with depressive symptoms. This association was observed at higher levels of perceived stress. However, relationships across time showed a somewhat different pattern. Relative to lower levels of EP, higher EP predicted lower but increasing levels of depressive symptoms across time in the context of high averaged perceived stress across time (the simple slopes for EE were nonsignificant). It is also possible that effects of initial EP decay over time in the presence of persistently high perceived stress. The observed pattern might suggest that the effects of EE and EP do not persist under high stress or that individuals abandon coping through emotional approach processes when stress is unrelenting.
These findings highlight the importance of perceived stress to the utility of emotional approach coping processes, at least with regard to depressive symptoms. It is important to consider the multifaceted nature of stress when interpreting these results. This study discriminated between long-term, self-reported stress perceptions (each individual’s mean across time) and short-term changes in stress perceptions (deviations from that mean at each time point). Long-term stress perceptions reflect a general tendency to appraise daily circumstances as uncontrollable or unpredictable. Such enduring stress perceptions are inconsistent with older adults’ motivations to avoid negative emotions and were associated with a pattern of increasing depressive symptoms when EP was relatively high. It is also possible that chronic stress perceptions themselves reflect an age-related vulnerability factor that alters regulating emotions through EP. Increasing chronicity or intensity of stress perceptions could indicate deficits in cognitive or behavioral attempts to adapt to stressful occurrences, particularly in the absence of new or worsening circumstances.
Inspection of Figures 2a and 2b, however, suggests that higher depressive symptoms over the course of the study were most likely when perceived stress was high and EP or EE was relatively low. High levels of chronically experienced perceived stress might reflect tendencies toward emotional lability, negative affectivity, or neuroticism. Thus, as anticipated, attempts to process emotions might be more likely to involve rumination or cycles of negative repetitive thought (see Hoyt et al., 2016; Segerstrom et al., 2010). Our findings follow observations in the literature (e.g., Low, Stanton, & Danoff-Burg, 2006) that find a benefit of emotional approach coping on adjustment only in the context of fewer stressful life events.
Research measuring stress as negative life events, physiological arousal, or chronic burden (e.g., daily caregiving, financial strain) might further elucidate the consequences of emotional approach coping processes under high levels of stress. EE and EP do not uniformly associate with better adjustment, and salutary findings are more likely when stressors were more recent (Moreno et al., 2017). Situational use of emotional approach coping processes in response to specific stressful life events (vs. general stress perceptions) might better signal coping flexibility in older adults than dispositional emotional approach coping as considered in this study. Use of EP in response to a named stressor may be less likely to involve perseverative thought that might occur when processing chronic universal stress perceptions. Moreover, prior work on coping with emotion in older adults suggests that the nature of the stressor determines coping. For instance, when compared to younger adults, older adults are more likely to use passive emotion-focused coping strategies such as avoidance, suppression, and escape and less likely to report approach-oriented strategies when faced with an emotion-laden stressor (Blanchard-Fields, Stein, & Watson, 2004).
Notably, EE and EP were measured in this study with regard to how participants generally respond (i.e., “indicate what you generally do, feel, and think when you experience stressful situations”). The Emotional Approach Coping Scales are designed to use either a dispositional or situational instruction set (Stanton et al., 2000), and much of the empirical support for EE and EP’s benefits in clinical populations accrues from situational, stressor-specific assessments. Because older adults are generally more skilled at emotion regulation than younger adults (see Davis, Zautra, Johnson, Murray, & Okvat, 2007), it might be that they are particularly adept at coping flexibility and therefore better able to use emotional approach coping processes in optimal moments and not universally. If so, situational assessment of emotional approach coping processes could provide a clearer understanding of its influence over time. Future studies might also use daily momentary assessments to link stressors and use of emotional approach coping processes or anchor observations to a situational context. Furthermore, for the present analyses, EE and EP as measured at study entry was the primary predictor; changes over time cannot account for the possibility of changes in use as the study progressed. Additionally, a goal of this study was to examine differential effects of EP and EE. Of course, EE and EP could work together. For instance, it might be that EE is optimally beneficial after individuals are able to label and understand their feelings.
What can be gleaned about the comparative use of emotional approach coping processes in older adults? Overall mean scores on EE and EP appeared to be only slightly higher than published means in younger adult samples (Stanton et al., 2000, Study 1). This contrasts with observations that coping through emotion-focused strategies tends to be preferred by older adults during stressful situations compared to younger adults (Blanchard-Fields et al., 2004; Folkman & Lazarus, 1988). However, simply comparing mean values is likely insufficient for understanding age differences. More information will be needed to identify how and when various coping strategies are called upon and the proportion of their use relative to alternate coping behaviors (e.g., cognitive vs. behavioral strategies). Future studies should compare shifts toward the use of EE and EP during periods of psychological and physiological stress in younger and older adults to better understand the motivational components of using emotional approach coping processes in stressful circumstances.
The pattern of results suggest some differences between EE and EP. In particular, EP predicted changes in ill-health over time and EE did not. The cognitive nature of EP might render more stability in effects over time. Compared to the often social nature of EE, which is impacted by the surrounding interpersonal environment, EP might be well-rehearsed with age. No similar longitudinal studies of healthy young cohorts exist to compare the impact of EP on changes in physical health indicators; however, it might be that the variability in the salutary nature of EP on health lessens with age. Likewise, the interpersonal influences that condition the utility of EE might also be subject to changes over the life span. Younger adults are more likely to encounter novel social situations and or more likely to have newer social relationships.
As one of the few longitudinal studies, this study has broader implications for future research on emotional approach coping. Results suggest that analyzing emotional approach coping as a unitary construct, particularly in samples of older adults, will likely fail to reveal the differential impact of EE and EP on health and depression. These separable facets of emotion-regulating coping might also be differently influenced by contextual factors.
Interpretation of results should be made in light of study limitations. The current sample had relatively high education and socioeconomic status, and all participants were married. Such factors likely serve as resources for coping. Additional research is needed with samples with greater economic, racial, and social diversity. The study tested a conceptual framework in which coping processes are proposed to influence health and depressive symptoms; reverse and reciprocal relationships are plausible. In that very little research is available on emotional approach coping processes in healthy older adults, this study should be considered as exploratory, though theoretically grounded. Also, this study used a composite measure to indicate physical health. Although the composite incorporates both subjective and objective components, other indicators of health might have different relationships with EE or EP. A strength of this study is its longitudinal design. By design, the study period was not anchored to a particular life event. Future work might examine emotional approach coping processes in regard to a specific context (e.g., adjustment to retirement). Despite documented gender influences across the emotional approach coping literature (Stanton, 2011), none were observed in this study. It might be that the impact of gender is more salient at younger ages when gender differences in emotion regulation skills are more pronounced (see Stanton et al., 2000) or when the stressor itself threatens aspects of gender-related self-image (see Hoyt, 2009; Hoyt et al., 2013).
The present study draws upon coping, emotion regulation, and life span theories to identify relationships of emotional approach coping processes to physical and emotional health over time and adds to our limited observations of emotion-regulating coping in older adults. More longitudinal studies are needed to document changes in dispositional changes in emotion-based coping across the life span. Cognitive and physiological changes in older aging could presuppose preferred coping strategies (Charles, 2010). Results point to the importance of stress perceptions in conditioning the potential utility of EE and EP with regard to psychological outcomes. Although more research will help define the appropriateness of intervention, findings suggest that older adults who tend to perceive events as uncontrollable and overwhelming could benefit from interventions designed to enhance emotion-regulating coping. Tailoring coping interventions to positively impact health should involve capitalizing on the strengths and developmental hallmarks of older adulthood. This might include a focus on coping strategies aimed at identifying and clarifying present-focused, emotionally meaningful goals that detract from ruminative, future-oriented thought (Sullivan-Singh, Stanton, & Low, 2015).
Acknowledgments
These findings have not been publicly presented elsewhere. However, mean values of the ill-health composite variable have been reported else-where (Boggero, Eisenlohr-Moul, & Segerstrom, 2016).
Preparation of this article was supported by Grants R01-AG026307, K02–033629, UL1-TR001998, P30-AG028383, R00MH109667, and SC1-CA187494 from the National Institutes of Health.
Footnotes
To facilitate estimation, within-person reliabilities for questionnaire measures administered across waves were estimated using variance components estimation in the general linear model function in SPSS (v22.0) on data from waves 2 through 6, which were relatively balanced in terms of the amount of missing data.
Contributor Information
Michael A. Hoyt, Department of Population Health and Disease Prevention and the Chao Comprehensive Cancer Center, University of California, Irvine.
Ian A. Boggero, College of Dentistry, University of Kentucky
Annette L. Stanton, Department of Psychology, University of California, Los Angeles.
Ashley Wei-Ting Wang, Department of Psychology, Soochow University.
Tory A. Eisenlohr-Moul, Department of Psychiatry, University of Illinois at Chicago
Suzanne C. Segerstrom, Department of Psychology, University of Kentucky.
References
- Amighi J, Hoke M, Mlekusch W, Schlager O, Exner M, Haumer M, . . . Wagner O (2011). Beta 2 microglobulin and the risk for cardiovascular events in patients with asymptomatic carotid atherosclerosis. Stroke, 42, 1826–1833. 10.1161/STROKEAHA.110.600312 [DOI] [PubMed] [Google Scholar]
- Austenfeld JL, & Stanton AL (2004). Coping through emotional approach: A new look at emotion, coping, and health-related outcomes. Journal of Personality, 72, 1335–1364. 10.1111/j.1467-6494.2004.00299.x [DOI] [PubMed] [Google Scholar]
- Benjamini Y, & Hochberg Y (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B, Statistical Methodology, 57, 289–300. [Google Scholar]
- Bethea M, & Forman DT (1990). Beta 2-microglobulin: Its significance and clinical usefulness. Annals of Clinical and Laboratory Science, 20, 163–168. [PubMed] [Google Scholar]
- Birditt KS, & Fingerman KL (2003). Age and gender differences in adults’ descriptions of emotional reactions to interpersonal problems. The Journals of Gerontology:Series B: Psychological Sciences and Social Sciences, 58, 237–245. 10.1093/geronb/58.4.P237 [DOI] [PubMed] [Google Scholar]
- Blanchard-Fields F, Stein R, & Watson TL (2004). Age differences in emotion-regulation strategies in handling everyday problems. Journal of Gerontology: Series B: Psychological and Social Sciences, 59, P261–P269. 10.1093/geronb/59.6.P261 [DOI] [PubMed] [Google Scholar]
- Boggero IA, Eisenlohr-Moul T, & Segerstrom SC (2016). Task-switching ability protects against the adverse effects of pain on health: A longitudinal study of older adults. British Journal of Health Psychology, 21, 434–450. 10.1111/bjhp.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryk AS, & Raudenbush SW (1992). Hierarchical linear models: Applications and data analysis methods Newbury Park, CA: Sage. [Google Scholar]
- Buchwald D, Wener MH, Pearlman T, & Kith P (1997). Markers of inflammation and immune activation in chronic fatigue and chronic fatigue syndrome. The Journal of Rheumatology, 24, 372–376. [PubMed] [Google Scholar]
- Burklund LJ, Creswell JD, Irwin MR, & Lieberman MD (2014). The common and distinct neural bases of affect labeling and reappraisal in healthy adults. Frontiers in Psychology, 5, 221. 10.3389/fpsyg.2014.00221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen LL (1992). Social and emotional patterns in adulthood: Support for socioemotional selectivity theory. Psychology and Aging, 7, 331–338. 10.1037/0882-7974.7.3.331 [DOI] [PubMed] [Google Scholar]
- Carstensen LL (1995). Evidence for a life-span theory of socioemotional selectivity. Current Directions in Psychological Science, 4, 151–156. 10.1111/1467-8721.ep11512261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen LL (1998). A life-span approach to social motivation. In Heckhausen J & Dweck CS (Eds.), Motivation and self-regulation across the life span (pp. 341–364). Cambridge, England: Cambridge University Press. 10.1017/CBO9780511527869.015 [DOI] [Google Scholar]
- Carstensen LL (2006). The influence of a sense of time on human development. Science, 312, 1913–1915. 10.1126/science.1127488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen LL, Isaacowitz DM, & Charles ST (1999). Taking time seriously. A theory of socioemotional selectivity. American Psychologist, 54, 165–181. 10.1037/0003-066X.54.3.165 [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Pasupathi M, Mayr U, & Nesselroade JR (2000). Emotional experience in everyday life across the adult life span. Journal of Personality and Social Psychology, 79, 644–655. 10.1037/0022-3514.79.4.644 [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Turan B, Scheibe S, Ram N, Ersner-Hershfield H, Samanez-Larkin GR, . . . Nesselroade JR (2011). Emotional experience improves with age: Evidence based on over 10 years of experience sampling. Psychology and Aging, 26, 21–33. 10.1037/a0021285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, & Scheier MF (1981). On the self-regulation of behavior New York, NY: Cambridge University Press. [Google Scholar]
- Charles ST (2010). Strength and vulnerability integration: A model of emotional well-being across adulthood. Psychological Bulletin, 136, 1068–1091. 10.1037/a0021232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles ST, & Carstensen LL (2014). Emotion regulation and aging. In Gross JJ (Ed.), Handbook of emotion regulation (2nd ed., pp. 203–218). New York, NY: Guilford Press. [Google Scholar]
- Cho D, Park CL, & Blank TO (2013). Emotional approach coping: Gender differences on psychological adjustment in young to middle-aged cancer survivors. Psychology & Health, 28, 874–894. 10.1080/08870446.2012.762979 [DOI] [PubMed] [Google Scholar]
- Clark DO, Von Korff M, Saunders K, Baluch WM, & Simon GE (1995). A chronic disease score with empirically derived weights. Medical Care, 33, 783–795. 10.1097/00005650-199508000-00004 [DOI] [PubMed] [Google Scholar]
- Clark WR (2008). In defense of self: How the immune system really works New York, NY: Oxford University Press. 10.1093/acprof:oso/9780195336634.001.0001 [DOI] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Cooper EH, & Plesner T (1980). Beta-2-microglobulin review: Its relevance in clinical oncology. Medical and Pediatric Oncology, 8, 323–334. 10.1002/mpo.2950080403 [DOI] [PubMed] [Google Scholar]
- Couzin-Frankel J (2010). Inflammation bares a dark side. Science, 330, 1621. 10.1126/science.330.6011.1621 [DOI] [PubMed] [Google Scholar]
- Cranford JA, Shrout PE, Iida M, Rafaeli E, Yip T, & Bolger N (2006). A procedure for evaluating sensitivity to within-person change: Can mood measures in diary studies detect change reliably? Personality and Social Psychology Bulletin, 32, 917–929. 10.1177/0146167206287721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JD, Lam S, Stanton AL, Taylor SE, Bower JE, & Sherman DK (2007). Does self-affirmation, cognitive processing, or discovery of meaning explain cancer-related health benefits of expressive writing? Personality and Social Psychology Bulletin, 33, 238–250. 10.1177/0146167206294412 [DOI] [PubMed] [Google Scholar]
- Davis MC, Zautra AJ, Johnson LM, Murray KE, & Okvat HA (2007). Psychosocial stress, emotion regulation, and resilience among older adults. In Aldwn CM, Park CL, & Spiro A (Eds.), Handbook of health psychology and aging (pp. 250–266). New York, NY: Guilford Press. [Google Scholar]
- DeSalvo KB, Bloser N, Reynolds K, He J, & Muntner P (2006). Mortality prediction with a single general self-rated health question. A meta-analysis. Journal of General Internal Medicine, 21, 267–275. 10.1111/j.1525-1497.2005.00291.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSteno D, Gross JJ, & Kubzansky L (2013). Affective science and health: The importance of emotion and emotion regulation. Health Psychology, 32, 474–486. 10.1037/a0030259 [DOI] [PubMed] [Google Scholar]
- Ehring T, & Watkins ER (2008). Repetitive negative thinking as a transdiagnostic process. International Journal of Cognitive Therapy, 1, 192–205. 10.1521/ijct.2008.1.3.192 [DOI] [Google Scholar]
- Enders CK, & Tofighi D (2007). Centering predictor variables in cross-sectional multilevel models: A new look at an old issue. Psychological Methods, 12, 121–138. 10.1037/1082-989X.12.2.121 [DOI] [PubMed] [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99, 20–35. 10.1037/0033-2909.99.1.20 [DOI] [PubMed] [Google Scholar]
- Folkman S, & Lazarus RS (1988). Coping as a mediator of emotion. Journal of Personality and Social Psychology, 54, 466–475. 10.1037/0022-3514.54.3.466 [DOI] [PubMed] [Google Scholar]
- Frijda NH (1986). The emotions New York, NY: Cambridge University Press. [Google Scholar]
- Gross JJ (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2, 271–299. 10.1037/1089-2680.2.3.271 [DOI] [Google Scholar]
- Gross JJ (Ed.). (2014). Emotion regulation: Conceptual and empirical foundations. Handbook of emotion regulation (2nd ed., pp. 3–20). New York, NY: Guilford Press. [Google Scholar]
- Gross JJ, Carstensen LL, Pasupathi M, Tsai J, Skorpen CG, & Hsu AYC (1997). Emotion and aging: Experience, expression, and control. Psychology and Aging, 12, 590–599. 10.1037/0882-7974.12.4.590 [DOI] [PubMed] [Google Scholar]
- Gross JJ, & John OP (2003). Individual differences in two emotion regulation processes: Implications for affect, relationships, and wellbeing. Journal of Personality and Social Psychology, 85, 348–362. 10.1037/0022-3514.85.2.348 [DOI] [PubMed] [Google Scholar]
- Heckhausen J, Wrosch C, & Schulz R (2010). A motivational theory of life-span development. Psychological Review, 117, 32–60. 10.1037/a0017668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyt MA (2009). Gender role conflict and emotional approach coping in men with cancer. Psychology & Health, 24, 981–996. 10.1080/08870440802311330 [DOI] [PubMed] [Google Scholar]
- Hoyt MA, Austenfeld J, & Stanton AL (2016). Processing coping methods in expressive essays about stressful experiences: Predictors of health benefit. Journal of Health Psychology, 21, 1183–1193. 10.1177/1359105314550347 [DOI] [PubMed] [Google Scholar]
- Hoyt MA, Stanton AL, Bower JE, Thomas KS, Litwin MS, Breen EC, & Irwin MR (2013). Inflammatory biomarkers and emotional approach coping in men with prostate cancer. Brain, Behavior, and Immunity, 32, 173–179. 10.1016/j.bbi.2013.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyt MA, Stanton AL, Irwin MR, & Thomas KS (2013). Cancer-related masculine threat, emotional approach coping, and physical functioning following treatment for prostate cancer. Health Psychology, 32, 66–74. 10.1037/a0030020 [DOI] [PubMed] [Google Scholar]
- Hughes AE, Berg CA, & Wiebe DJ (2012). Emotional processing and self-control in adolescents with type 1 diabetes. Journal of Pediatric Psychology, 37, 925–934. 10.1093/jpepsy/jss062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juth V, Dickerson SS, Zoccola PM, & Lam S (2015). Understanding the utility of emotional approach coping: Evidence from a laboratory stressor and daily life. Anxiety, Stress & Coping, 28, 50–70. 10.1080/10615806.2014.921912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler EM, & Staudinger UM (2009). Affective experience in adulthood and old age: The role of affective arousal and perceived affect regulation. Psychology and Aging, 24, 349–362. 10.1037/a0015352 [DOI] [PubMed] [Google Scholar]
- Knight RG, McMahon J, Green TJ, & Skeaff CM (2004). Some Normative and psychometric data for the Geriatric Depression Scale and the Cognitive Failures Questionnaire from a sample of healthy older persons. New Zealand Journal of Psychology, 33, 163–170. [Google Scholar]
- Korten NC, Comijs HC, Penninx BW, & Deeg DJ (2017). Perceived stress and cognitive function in older adults: Which aspect of perceived stress is important? International Journal of Geriatric Psychiatry, 32, 439–445. 10.1002/gps.4486 [DOI] [PubMed] [Google Scholar]
- Koschwanez HE, Kerse N, Darragh M, Jarrett P, Booth RJ, & Broadbent E (2013). Expressive writing and wound healing in older adults: A randomized controlled trial. Psychosomatic Medicine, 75, 581–590. 10.1097/PSY.0b013e31829b7b2e [DOI] [PubMed] [Google Scholar]
- Kunzmann U, Schilling O, Wrosch C, Siebert JS, Katzorreck M, Wahl HW, & Gerstorf D (2019). Negative emotions and chronic physical illness: A lifespan developmental perspective. Health Psychology, 38, 949–959. 10.1037/hea0000767 [DOI] [PubMed] [Google Scholar]
- Lawton MP, Kleban MH, Rajagopal D, & Dean J (1992). Dimensions of affective experience in three age groups. Psychology and Aging, 7, 171–184. 10.1037/0882-7974.7.2.171 [DOI] [PubMed] [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, appraisal, and coping New York, NY: Springer. [Google Scholar]
- Low CA, Stanton AL, & Bower JE (2008). Effects of acceptance-oriented versus evaluative emotional processing on heart rate recovery and habituation. Emotion, 8, 419–424. 10.1037/1528-3542.8.3.419 [DOI] [PubMed] [Google Scholar]
- Low CA, Stanton AL, & Danoff-Burg S (2006). Expressive disclosure and benefit finding among breast cancer patients: Mechanisms for positive health effects. Health Psychology, 25, 181–189. 10.1037/0278-6133.25.2.181 [DOI] [PubMed] [Google Scholar]
- Low CA, Stanton AL, Thompson N, Kwan L, & Ganz PA (2006). Contextual life stress and coping strategies as predictors of adjustment to breast cancer survivorship. Annals of Behavioral Medicine, 32, 235–244. 10.1207/s15324796abm3203_10 [DOI] [PubMed] [Google Scholar]
- Manne S, Ostroff J, Winkel G, Goldstein L, Fox K, & Grana G (2004). Posttraumatic growth after breast cancer: Patient, partner, and couple perspectives. Psychosomatic Medicine, 66, 442–454. [DOI] [PubMed] [Google Scholar]
- Master SL, Amodio DM, Stanton AL, Yee CM, Hilmert CJ, & Taylor SE (2009). Neurobiological correlates of coping through emotional approach. Brain, Behavior, and Immunity, 23, 27–35. 10.1016/j.bbi.2008.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarland C, & Buehler R (1997). Negative affective states and the motivated retrieval of positive life events: The role of affect acknowledgment. Journal of Personality and Social Psychology, 73, 200–214. 10.1037/0022-3514.73.1.200 [DOI] [Google Scholar]
- Monin JK, Schulz R, Lemay EP Jr., & Cook TB (2012). Linguistic markers of emotion regulation and cardiovascular reactivity among older caregiving spouses. Psychology and Aging, 27, 903–911. 10.1037/a0027418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno PI, Wiley JF, & Stanton AS (2017). Coping through emotional approach: The utility of processing and expressing emotions in response to stress. In Lopez SJ, Edwards L, & Marques S (Eds.), Oxford handbook of positive psychology (3rd ed., pp. 1–38). New York, NY: Oxford University Press. [Google Scholar]
- Morrow J, & Nolen-Hoeksema S (1990). Effects of responses to depression on the remediation of depressive affect. Journal of Personality and Social Psychology, 58, 519–527. 10.1037/0022-3514.58.3.519 [DOI] [PubMed] [Google Scholar]
- Ochsner KN, & Gross JJ (2005). The cognitive control of emotion. Trends in Cognitive Sciences, 9, 242–249. 10.1016/j.tics.2005.03.010 [DOI] [PubMed] [Google Scholar]
- Pakenham KI, Smith A, & Rattan SL (2007). Application of a stress and coping model to antenatal depressive symptomatology. Psychology, Health & Medicine, 12, 266–277. 10.1080/13548500600871702 [DOI] [PubMed] [Google Scholar]
- Pennebaker JW, Mayne TJ, & Francis ME (1997). Linguistic predictors of adaptive bereavement. Journal of Personality and Social Psychology, 72, 863–871. 10.1037/0022-3514.72.4.863 [DOI] [PubMed] [Google Scholar]
- Peters RM (2006). The relationship of racism, chronic stress emotions, and blood pressure. Journal of Nursing Scholarship, 38, 234–240. 10.1111/j.1547-5069.2006.00108.x [DOI] [PubMed] [Google Scholar]
- Phillips LH, Henry JD, Hosie JA, & Milne AB (2008). Effective regulation of the experience and expression of negative affect in old age. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences, 63, P138–P145. 10.1093/geronb/63.3.P138 [DOI] [PubMed] [Google Scholar]
- Piazza JR, Almeida DM, Dmitrieva NO, & Klein LC (2010). Frontiers in the use of biomarkers of health in research on stress and aging. The Journals of Gerontology: Series B: Psychological Sciences and Social Sciences, 65, 513–525. 10.1093/geronb/gbq049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza JR, Charles ST, Stawski RS, & Almeida DM (2013). Age and the association between negative affective states and diurnal cortisol. Psychology and Aging, 28, 47–56. 10.1037/a0029983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31, 437–448. 10.3102/10769986031004437 [DOI] [Google Scholar]
- Putnam KG, Buist DS, Fishman P, Andrade SE, Boles M, Chase GA, . . . Arnold Chan K (2002). Chronic disease score as a predictor of hospitalization. Epidemiology, 13, 340–346. 10.1097/00001648-200205000-00016 [DOI] [PubMed] [Google Scholar]
- Rachman S (1980). Emotional processing. Behaviour Research and Therapy, 18, 51–60. 10.1016/0005-7967(80)90069-8 [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models: Applications and data analysis methods (2nd ed.). Newbury Park, CA: Sage. [Google Scholar]
- Reynolds P, Hurley S, Torres M, Jackson J, Boyd P, & Chen VW (2000). Use of coping strategies and breast cancer survival: Results from the Black/White Cancer Survival Study. American Journal of Epidemiology, 152, 940–949. 10.1093/aje/152.10.940 [DOI] [PubMed] [Google Scholar]
- Seeley SH, Yanez B, Stanton AL, & Hoyt MA (2017). An emotional processing writing intervention and heart rate variability: The role of emotional approach. Cognition and Emotion, 31, 988–994. 10.1080/02699931.2016.1170667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segerstrom SC (2014). Affect and self-rated health: A dynamic approach with older adults. Health Psychology, 33, 720–728. 10.1037/a0033506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segerstrom SC, Eisenlohr-Moul TA, Evans DR, & Ram N (2015). Repetitive thought dimensions, psychological well-being, and perceived growth in older adults: A multilevel, prospective study. Anxiety, Stress & Coping, 28, 287–302. 10.1080/10615806.2014.947285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segerstrom SC, Roach AR, Evans DR, Schipper LJ, & Darville AK (2010). The structure and health correlates of trait repetitive thought in older adults. Psychology and Aging, 25, 505–515. 10.1037/a0019456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segerstrom SC, & Smith GT (2019). Personality and coping: Individual differences in response to emotion. Annual Review of Psychology, 70, 651–671. 10.1146/annurev-psych-010418-102917 [DOI] [PubMed] [Google Scholar]
- Segerstrom SC, Stanton AL, Alden LE, & Shortridge BE (2003). A multidimensional structure for repetitive thought: What’s on your mind, and how, and how much? Journal of Personality and Social Psychology, 85, 909–921. 10.1037/0022-3514.85.5.909 [DOI] [PubMed] [Google Scholar]
- Smith JA, Lumley MA, & Longo DJ (2002). Contrasting emotional approach coping with passive coping for chronic myofascial pain. Annals of Behavioral Medicine, 24, 326–335. 10.1207/S15324796ABM2404_09 [DOI] [PubMed] [Google Scholar]
- Snijders TA, & Bosker RJ (1993). Standard errors and sample sizes for two-level research. Journal of Educational Statistics, 18, 237–259. 10.3102/10769986018003237 [DOI] [Google Scholar]
- Stanton AL (2011). Regulating emotions during stressful experiences: The adaptive utility of coping through emotional approach. In Folk-man S (Ed.), The Oxford handbook of stress, health, and coping (pp. 369–386). New York, NY: Oxford University Press. [Google Scholar]
- Stanton AL, Danoff-Burg S, Cameron CL, Bishop M, Collins CA, Kirk SB, . . . Twillman R (2000). Emotionally expressive coping predicts psychological and physical adjustment to breast cancer. Journal of Consulting and Clinical Psychology, 68, 875–882. 10.1037/0022-006X.68.5.875 [DOI] [PubMed] [Google Scholar]
- Stanton AL, Danoff-Burg S, Cameron CL, & Ellis AP (1994). Coping through emotional approach: Problems of conceptualization and confounding. Journal of Personality and Social Psychology, 66, 350–362. 10.1037/0022-3514.66.2.350 [DOI] [PubMed] [Google Scholar]
- Stanton AL, Kirk SB, Cameron CL, & Danoff-Burg S (2000). Coping through emotional approach: Scale construction and validation. Journal of Personality and Social Psychology, 78, 1150–1169. 10.1037/0022-3514.78.6.1150 [DOI] [PubMed] [Google Scholar]
- Stanton AL, & Low CA (2012). Dispositional and stressor-related emotion regulation in the context of a chronic, life-limiting stressor. Journal of Personality, 80, 287–311. 10.1111/j.1467-6494.2011.00732.x [DOI] [PubMed] [Google Scholar]
- Sterba SK, & MacCallum RC (2010). Variability in parameter estimates and model fit across repeated allocations of items to parcels. Multivariate Behavioral Research, 45, 322–358. 10.1080/00273171003680302 [DOI] [PubMed] [Google Scholar]
- Sterba SK, & Rights JD (2016). Accounting for parcel-allocation variability in practice: Combining sources of uncertainty and choosing the number of allocations. Multivariate Behavioral Research, 51, 296–313. 10.1080/00273171.2016.1144502 [DOI] [PubMed] [Google Scholar]
- Stewart AL, & Ware JE (1992). Measuring functioning and wellbeing: The Medical Outcomes Study approach Durham, NC: Duke University Press. [Google Scholar]
- Sullivan-Singh SJ, Stanton AL, & Low CA (2015). Living with limited time: Socioemotional selectivity theory in the context of health adversity. Journal of Personality and Social Psychology, 108, 900–916. 10.1037/a0039047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volpato S, Guralnik JM, Ferrucci L, Balfour J, Chaves P, Fried LP, & Harris TB (2001). Cardiovascular disease, interleukin-6, and risk of mortality in older women: The women’s health and aging study. Circulation, 103, 947–953. 10.1161/01.CIR.103.7.947 [DOI] [PubMed] [Google Scholar]
- Watkins ER (2008). Constructive and unconstructive repetitive thought. Psychological Bulletin, 134, 163–206. 10.1037/0033-2909.134.2.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, & Leirer VO (1982). Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research, 17, 37–49. 10.1016/0022-3956(82)90033-4 [DOI] [PubMed] [Google Scholar]
- Yılmaz B, Köklü S, Yüksel O, & Arslan S (2014). Serum beta 2-microglobulin as a biomarker in inflammatory bowel disease. World Journal of Gastroenterology, 20, 10916–10920. 10.3748/wjg.v20.i31.10916 [DOI] [PMC free article] [PubMed] [Google Scholar]


