Abstract
Background
Although mindfulness-based interventions (MBIs) have demonstrated efficacy for alleviating psychological distress in cancer survivors, little is known about the extent to which participants adhere to assigned home practice. The purpose of this systematic review was to summarize and appraise the literature on rates and correlates of adherence to mindfulness home practice among cancer survivors.
Methods
Four databases (PubMed, Psychology and Behavioral Sciences, PsycInfo, and CINAHL) were searched for studies published before October 15, 2020. Articles were included if they evaluated the benefits of an MBI program for adults with cancer.
Results
Twenty-one studies (N=1811 participants) meeting the inclusion criteria were identified (randomized controlled trials (n=13), non-randomized controlled designs (n=2), single-group studies (n=6)). The pooled adherence rate for participants’ home practice was 60% of the assigned amount, which equated to 27 min per day during the intervention period. There was some evidence for a relationship between home practice of mindfulness techniques and improvements in mood, stress, anxiety, depression, and fear of cancer recurrence (correlation coefficients ranged from 0.33 to 0.67). Factors including marital status, mood disturbance at baseline, intervention modality, and personality traits were evaluated in relation to adherence to home practice, but the current literature was inadequate to evaluate whether a relationship exists.
Conclusion
Adherence to mindfulness home practice among cancer survivors is suboptimal, and most of the correlates of adherence studied to date are non-modifiable. More research is warranted to scrutinize the role of home practice in mindfulness-based interventions, including assessment of modifiable factors influencing adherence to improve benefits for this population.
Keywords: oncology, mindfulness, adherence, distress, complementary therapy
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
It is estimated that 28.4 million new cancer cases are projected to occur in 2040 worldwide, a 47% rise from the 19.3 million cases in 2020.1 Cancer-related distress, defined as
a multifactorial unpleasant emotional experience of a psychological, social, and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms and its treatment2
is experienced by approximately 30–50% of all cancer survivors.3,4 Distress can range from negative emotions, such as sadness, fear, and rumination, to potentially disabling mental health conditions, such as anxiety and depression.5 Given its negative impact on quality of life, there has been growing interest in developing and evaluating interventions to manage the distress faced by this population.5 Addressing patient distress issues across the cancer trajectory has also become standard practice in many oncology settings.
Mindfulness is the practice of directing focused attention towards experiences occurring in the present moment with a nonjudgmental and accepting attitude.6 Since the regular practice of mindfulness has been shown to help regulate negative emotions,6 the last two decades have seen a proliferation of evidence-based interventions grounded in mindfulness principles and techniques designed to target psychological distress.7 These are broadly referred to as mindfulness-based interventions (MBIs). Among cancer patients, multiple systematic reviews have provided evidence for the efficacy of MBIs in reducing symptoms of mood disturbance, anxiety, depression, and stress.7–9
Mindfulness-Based Stress Reduction (MBSR) is a standardized mindfulness protocol developed by Jon Kabat-Zinn and colleagues at the Massachusetts Medical Centre with well documented benefits for distressed cancer patients.10 This holistic mind-body program aims towards cultivation of mindfulness, being fully aware of present moment experience without resistance or judgment, through the implementation of three central formal practices: (1) the body scan, a guided attentional exercise which consists of systematically directing one’s attention throughout the body; (2) hatha yoga, a series of gentle mindful movements and postures to enhance body awareness; and (3) sitting meditation, to develop a capacity to systematically bring one’s attention to physical sensations, sensory stimuli, thoughts, and the breath.11 In addition to these formal practices, MBSR consists of informal practices of bringing mindful awareness to daily routines and activities (for example, mindful eating), which can help participants instill attitudes of non-judging and acceptance in everyday life.11 The standard MBSR curriculum consists of eight weekly, 2.5-hour group sessions that involve formal mindfulness practices, discussion and inquiry to facilitate sharing of experience and foster social support.11 MBSR also involves 45 minutes of daily formal and informal home practice and a 6-hour day-long retreat, usually between the 6th and 7th weeks of the program.11 The daily between-session practice for 45 min per day is specific to MBSR, and many non-standardized MBI programs require shorter formal home practice, often of about 20 minutes/day.9 Mindfulness Based Cancer Recovery (MBCR) is an adaptation of MBSR for people living with cancer.12 With the exception of shorter sessions (1.5 to 2 hours) to accommodate cancer patients, MBCR has similar structure to MBSR.12 The core components are also similar, but MBCR further emphasizes the use of supportive imagery, mindful yoga movement with cancer recovery in mind, loving‐kindness practice (ie, meditation exercise designed to enhance feelings of kindness and compassion for self and others), cognitive coping strategies, specific breathing and sleep exercises, and emphasis on group process and group support.12 One distinct feature of MBCR is focusing on coping with cancer and common oncology symptoms, such as sleep problems, pain, and fear of cancer recurrence.12
Mindfulness-Based Cognitive Therapy (MBCT) is another common evidence-based mindfulness program that differs from classic MBSR in its integration of core cognitive behavioral therapy features.13 MBCT was originally designed to help people in remission from recurrent bouts of depression by specifically targeting the cognitive processes that trigger relapse.13 MBCT is also a standard 8-week program with a day-long retreat and home practices.13 MBCT has also been adapted specifically for people with cancer,14 and other researchers have created shorter versions of MBSR also catering to cancer patients and survivors.15
All of these MBIs recognize the importance of between-session home practice as a method of mastering skills that are hypothesized as key mediators of intervention effects.16 The acquisition of knowledge and skills regarding mindfulness, and the understanding of how these practices can be individually implemented is often discovered through between-session practices.17 MBI programs presume that out-of-class practice will lead to improved skill and comfort with mindfulness, and thereby adherence to assigned practice exercises is considered to be a necessary condition for therapeutic effects and improved outcomes.18 As noted above, the quantity of daily home practice assigned in programs like MBSR is typically 45 minutes per day,11 often broken down into 30 minutes of meditation and 15 minutes of yoga, which represents a significant time commitment that may seem onerous or daunting for some participants. It is unclear to what extent participants with cancer adhere to home practice assigned as a part of MBI programs, and factors influencing adherence to home practice are not well understood. In addition, while studies in non-cancer populations suggest a dose-response relationship between home-practice and clinical outcomes,16,17 the necessity of home practice to achieve therapeutic benefit is not well established.18 It is also possible that the toxic effects of cancer and its treatments, side effects such as fatigue and insomnia, as well as deconditioning caused by reduced physical activity during treatment contribute to low adherence to mindfulness home practice, compared with non-cancer populations. Despite the presumed importance of home practice in MBIs, this has received relatively limited attention in the mindfulness literature. No cancer-specific systematic reviews have conducted a comprehensive assessment of adherence to home assignment in MBI programs. In fact, a recent meta-analysis investigating the effects of MBIs on anxiety outcomes in cancer patients noted that most studies do not include measures of time spent practicing mindfulness, and the authors cited this as a significant limitation to understanding the heterogeneous treatment effects found in their pooled analyses.9 It is crucial to critically evaluate the current state of knowledge regarding adherence to home practice in order to inform the development of more self-deliverable models of mindfulness for reducing psychological distress after cancer. Such knowledge may also guide efforts to enhance patient engagement in MBIs and inform future clinical research testing the efficacy and effectiveness of these programs among cancer patients experiencing psychological distress. Therefore, this systematic review aims to evaluate adherence to home practice in studies evaluating the effects of MBI programs on psychological distress outcomes in cancer patients. Specific objectives include:
To evaluate the extent to which cancer patients report completing formal (meditation, body scan, yoga) and/or informal (doing everyday activities mindfully) home practice exercises assigned within the context of MBIs.
To identify factors influencing adherence to mindfulness home practice among cancer patients.
To evaluate the relationship between the amount of home practice and intervention effects on psychological distress.
Methods
Search Strategy and Study Selection
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.19 Literature searches were performed including publications up to October 15, 2020 using four databases: PubMed, Psychology and Behavioral Sciences, PsycInfo, and Cumulative Index to Nursing and Allied Health (CINAHL). Search terms used in PubMed (see Appendix A) were adapted for use in the other databases. The search strategy was developed by a health sciences librarian. Articles were included if they (1) included a population of adults (≥18 years old) with cancer, or adults mixed with other age groups, such as young adults and adolescents with cancer, (2) evaluated the effects of a MBI program (MBSR, MBCR, or MBCT-or adapted program, or other studies where mindfulness was the core component of the intervention), (3) reported the average number of minutes of formal and/or informal home practice per day during the intervention period or reported data to allow its calculation, and (4) used a randomized or non-randomized controlled trial (RCT) design (with any type of control group) or single group design. The exclusion criteria were (1) non-peer reviewed studies (conference meetings and presentations, dissertations, gray literature), (2) studies published in non-English languages, and (3) studies of mixed interventions, such as mindfulness-based art therapy and mindfulness-based music therapy. Two reviewers (MB and AM or KP) independently reviewed titles and abstracts for eligibility (level 1 screening) followed by review of eligible full-text articles (level 2 screening).
Data Extraction and Data Synthesis
Data extraction was completed in parallel by two reviewers (MB and DO) using a pre-designed template that summarized details of (1) study design, (2) intervention, (3) patient characteristics, (4) home practice details including the recording method, (5) amount of mindfulness home practice in minutes both within the intervention period and during follow-up, (6) distress and stress-related outcome measures, including mood disturbance, depression, anxiety, fear of cancer recurrence, worry, ruminative thinking, and stress hormones, (7) intervention effects on distress and stress-related outcomes, and (8) data on the association between home practice and distress/stress-related outcomes. Discrepancies between reviewers were resolved by consensus.
After obtaining the average amount of home practice per day in minutes during the intervention period for all studies, a pooled average score was calculated by summing all averages divided by the total number of studies included. An adherence rate during the course of the intervention period was also calculated for each study using the following formula: average number of minutes of actual home practice per day/prescribed number of minutes per day x 100. In dose ranging studies (for example, participant asked to practice 15 to 45 minutes daily), the upper range limit was used to calculate adherence rate. A pooled adherence rate was also calculated by averaging the average scores for daily home practice in minutes across studies divided by the prescribed amount of daily home practice in minutes, multiplied by 100. The average amount of home practice per day in minutes during the follow-up period (between the end of the intervention and the follow-up assessment[s]) were also obtained where reported, but adherence rates during follow-up were not calculated as home practice was encouraged but not formally required after the end of the MBI programs. All the articles were read several times to become familiar with the methods used and main findings.
Assessment of Study Quality
The quality of evidence in the included studies was assessed using the National Institutes of Health (NIH) Quality Assessment Tools.20 These tools are tailored to different research designs to assess individual study quality, and therefore do not assess the overall level of evidence as a whole. Using the NIH Assessment Tool for Controlled Trials, controlled intervention studies were rated as “poor”, “fair”, or “good” based upon the following criteria: randomization, groups’ similarity at baseline, statistical power, blinding, concealment of treatment allocation, analysis plan, intent-to-treat analysis, psychometric properties of outcome measures, outcome reporting, avoiding other interventions, and attrition and adherence rates. Similarly, the NIH Quality Assessment Tool for Uncontrolled Before–After Studies, including 11 criteria (study objectives stated, eligibility criteria, sample representativeness, all eligible participants enrolled, sample size, intervention description and delivery, validity and reliability of outcome measures, assessor blinding, attrition, statistical methods, using interrupted time-series design), was used as appropriate. To reduce subjectivity in ratings, two reviewers (MB and DO) performed quality assessments of the articles included, and disagreements were resolved by consensus.
Results
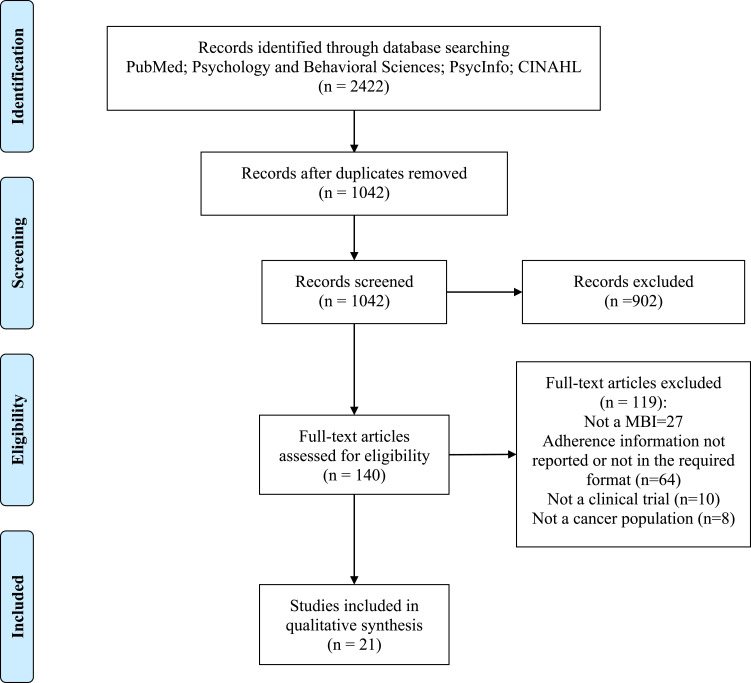
A total of 2422 citations were retrieved by the search. After removing duplicates, 1042 articles were screened for inclusion according to eligibility criteria. After full-text screening, 21 articles21–41 qualified for inclusion in the systematic review. A PRISMA flow diagram summarizing the literature search and screening process is presented in Figure 1. Study characteristics and findings of included studies are summarized in Table 1.
Figure 1.
PRISMA flow diagram of literature search process. Notes: PRISMA figure adapted from Liberati A, Altman D, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of clinical epidemiology. 2009;62(10). Creative Commons.
Table 1.
Literature Summary
| Study | Participants | Design | Intervention | Measurement of Home-Practice | Distress-Related Outcome Measure | Results | Average Home Practice (% Adherence)a | |
|---|---|---|---|---|---|---|---|---|
| Speca et al 200021 Canada | 90 patients with various cancer types [average age=51 years; 78% females; 38% breast cancer; mean of 15 years of formal education] | Waitlist RCT | MBCR [7 weekly 90-min sessions, home practice 45min/day was encouraged using a booklet and audiotape] | Home practice log | POMS and SOSI, administered at baseline and postintervention | After the intervention, patients in the treatment group had significantly lower scores on POMS-TMD (−65% vs −12%) and subscales of depression and anxiety, and stress (−30.7% vs −11.1%) than control subjects. | 32 min/day (71%adherence) | |
| Carlson et al 200723 Canada | 59 patients with early stage 0-II breast (n=49) or localized prostate (n=10) cancer [average age=54 years; 85% females; 64% married; average time since cancer diagnosis= 1.1 years; average of 14.7 years of formal education] | Single-group | MBCR [8 weekly 90 mins sessions, 3-h retreat, home practice 45 min/day] | Daily log collected each week during class | POMS, SOSI, and salivary cortisol, assessed pre- and post-intervention, and at 6- and 12-month follow-up. | Changes in POMS scores over the course of the intervention and follow-up were not significant. Stress scores showed a significant reduction (−19.3%) over the course of the intervention, which were maintained over the follow-up period. The average daily mean of cortisol values and overall slope of the diurnal rate did not change from pre- to post-intervention, but cortisol levels decreased significantly over the course of the follow-up. | 37 min/day (82% adherence) | |
| Lengacher et al 200927 USA | 85 breast cancer survivors [average ag= 57 years; 72% White; 56% employed; 78% some college education or more; 70% stage 0–I cancer, 30% stage II–III; average time since treatment completion=5 months) | Waitlist RCT | MBSR [6 weekly 2-h sessions, home practice 15–45 min/day using a manual and CD] | Daily diary | CARS, STAI, PSS, and CESD, assessed at baseline and postintervention. | MBSR participants exhibited greater improvements in fear of recurrence, anxiety and depression scores, relative to controls. | 25.6 min/day (57% adherence) | |
| Foley et al 201032 Australia | 115 participants with various cancer types [average age= 55.1 years; 77% females; 42% breast cancer; 44% employed] | Waitlist RCT | MBCT [8 weekly 2-h sessions, 5-hr retreat day, home practice up to 1-h/day using mindfulness recordings] | Daily diary collected at intervention end | HAM-D, HAM-S, and DASS, assessed at baseline, postintervention, and 3 months postintervention. | There were significant improvements in depression (d= 0.83), anxiety (d= 0.59), and stress (d=0.53) scores for MBCT participants compared with controls. Benefits were maintained at 3-month postintervention. | 30 min/day (50% adherence) | |
| Lengacher et al 201228 USA | 26 patients with advanced stage cancer [average age= 53 years; 69% female; 73% White; 69% married; 30% breast cancer; 63% some college education or more] | Single-group | MBSR [6 weekly 2-h sessions, home practice 15–45 min/day using a manual and CD] | Daily diary | CARS, STAI, and CESD, assessed at baseline and postintervention. Salivary cortisol and interleukin-6 were assessed pre- and post-MBSR session at 1, 3, and 6 weeks. | Following the 6-week MBSR program, patients showed improvements in stress and anxiety. Patients also had significant decreases in cortisol at Weeks 1 and 3 but not at Week 6. Salivary cortisol and interleukin-6 levels at Week 6 were lower overall (before/after an MBSR session), compared with Week 1. | 14.3 min/day (31% adherence) | |
| Hoffman et al 201234 United Kingdom | 114 females with stage 0-III breast cancer [average age=49 years; average time since treatment completion=9.2 months; average time since diagnosis= 17.4 months] | Waitlist RCT | MBSR [8 weekly 2–2.5 classes, 6-h retreat, 45 min/day home practice using a CD and manual] | Weekly record sheets | POMS, assessed at baseline, 8 and 12 weeks | There were statistically significant lower POMS-TMD scores in the experimental group than in the control group at postintervention (d= −0.5) and follow-up (d=−0.4). Similarly, there were lower POMS-anxiety subscale scores in the experimental group at postintervention (d= −0.4) and follow-up (d= −0.5). | 21 min/day (46% adherence) | |
| Campbell et al 201225 Canada | 70 female cancer survivors [average age= 53 years; 74% breast cancer; 87% White; average time since diagnosis=24 months, average time since treatment completion=13 months; average years of education= 14.6 years; 75% married or living with a partner; 10% metastatic disease] | Non-randomized waitlist trial | MBCR [8 weekly 90 min classes, 6-h retreat, home practice 45 min/day] | Daily log collected each week during class | RRQ-Rumination subscale, assessed at weeks 1 and 8 | MBCR group participants had significantly lower rumination scores than controls pre-post intervention. | 33 min/day (73% adherence) | |
| Zernicke et al 201424 Canada | 62 underserved cancer survivors [73% females; 82% in a relationship; 92% White; 34% breast cancer; average age= 58 years; 34% retired or employed full time; 77% completed some type of postsecondary education] | Waitlist RCT | Online MBCR [8 weekly 2-hour synchronous group sessions, 6-h retreat, home practice 45 min/day using recordings and videos] | Daily log | POMS and C-SOSI, administered at baseline and postintervention. | MBCR participants exhibited significant improvements in POMS-TMD (d= 0.44) and stress (d=0.49) scores compared to waitlist controls. | 21.4 min/day (47% adherence) | |
| Labelle et al 201522 Canada | 211 patients with various cancer types [58% breast cancer; average age=52 years; 80% female; 92% White; 71% married; average years of education=15 years; 70% completed treatment; average time since diagnosis= 23 months] | Non-randomized waitlist trial | MBCR [8 weekly 90 min classes, 6-h retreat, home practice 45 min/day] | Daily log collected each week during class | POMS, RRQ, and PSWQ, assessed at baseline, weeks 4 and 8. | Relative to controls, MBCR participants demonstrated greater decreases in POMS (d= 0.52), rumination (d=0.68), and worry (d= 0.57) scores. | 27.3 min/day (60% adherence) | |
| Tamagawa et al 201526 Canada | 38 females with stage I (40%) or II [45%) breast cancer [average age=55 years; average time since diagnosis= 20 months; 61% employed; 63% married or cohabitating; average years of education= 15 years] | Single-group | MBCR [8 weekly 90 min classes, 6-h retreat, home practice 45 min/day using a program manual and two compact discs] | Daily log collected each week during class | POMS and PTGI, assessed at baseline and postintervention | Not reported (results published separately as part of a larger study) | 20.6 min/day (45% adherence) | |
| Johns et al 201530 USA | 35 patients with various cancer types [average age=58 years; 85% breast cancer; 94% females; 80% White; 71% college educated; 49% employed; 60% married, 60% had a comfortable income; average time since treatment completion= 51.3 months] |
Waitlist RCT | MBSR [7 weekly 2-h classes, no retreat, and home practice 20 min/day] | Weekly log | GAD-7 and PHQ-8, assessed at baseline, postintervention, and 1-month follow-up | Compared to controls, MBSR participants reported significant reductions in depression at postintervention (d= −1.30) and follow-up (d=−1.71). Anxiety scores were lower for MBSR participants than controls at follow-up (d = −0.98) but not at postintervention. | 35 min/day (>100% adherence) |
|
| Johannsen et al 201635 Denmark | 129 females with breast cancer [average age= 56.8 years; on average 40 months post- mastectomy or lumpectomy; 70% married; 43% employed; 69% more than 2 years of post-high school education] | Waitlist RCT | MBCT [8 weekly 90 min classes, no retreat, home practice 45 min/day using a CD] | Weekly homework records | HADS, assessed at baseline, 8 weeks, 3 and 6 months | Interactions between group and time were not significant, indicating no difference between groups. | 24 min/day (53% adherence) | |
| Johns et al 201631 USA | 71 patients with stage 0-III breast (n=60) or colorectal (n=11) cancer [average age= 56 years; 90% females; 70% White; 52.1% had a comfortable income; 54.9% married; average time since treatment completion= 2.4 years] | RCT with an active control group [psycho-educational support (PES)] | MBSR [8 weekly 2-h classes, no retreat, home practice 20 mins/day] vs a structurally equivalent PES program | Weekly log | GAD-7 and PHQ-8, assessed at baseline, postintervention, and 6 months later | Both groups exhibited significant improvements in anxiety (MBSR: postintervention d =−0.89, 6-month d =−0.74) and depression (MBSR: postintervention d=−1.05, 6-month d= −0.98) scores. Differences between groups were not significant. | MBSR: 16.8 min/day (84% adherence) PES: 13.2 min/day (66% adherence) |
|
| Lengacher et al 201829 USA | 15 stage 0‐III breast cancer survivors [average age= 57 years; 80% married; 93% White; average time since treatment completion= 10 months] | Single-group | Online asynchronous MBSR [6 weekly 2-h sessions, home practice 15–45 min/day using audio and video files] | Electronic practice diary | STAI, CESD, PSS, and CARS, assessed at baseline and postintervention | Following the program, participants reported significant improvements in anxiety (d=1.48), depression (d=1.62), stress (d=1.62), fear of recurrence overall (d=1.51), and fear of recurrence problems (d=1.31). | 36 min/day (80% adherence) | |
| Compen et al 201833 Netherlands | 245 patients with various cancer types [86% females; average age= 51.7 years; 62% breast cancer; 82% married; 68% high education] | Three-arm RCT (in-person MBCT vs online MBCT vs treatment as usual) | In-person MBCT [8 weekly 2.5-h group sessions, 6-h retreat, daily home practice using audio files] Online asynchronous MBCT [delivered individually and offered online material for 8 weeks, 6-h retreat, daily home practice] | Daily diary | HADS, FCRI, and RRQ-rumination subscale, assessed at baseline and postintervention | Compared with treatment as usual, both in-person and online MBCT groups exhibited significant improvements in HADS (d=0.45 and 0.71, respectively), fear of recurrence (d= 0.27 and 0.53, respectively), and ruminative thinking (d= 0.42 and 0.51, respectively) from baseline to postintervention. | All MBCT participants: 29.6 min/day bAdherence rate could not be calculated. In-person MBCT: 30.6 min/day Online MBCT: 28.7 min/day |
|
| Russell et al 201941 Australia | 69 patients with melanoma [54% females; average age= 54 years; 76% married; 39% university degree] | RCT (usual care control group) | 6-week web-based asynchronous MBI program. Participants were asked to practice daily. | Weekly online home practice questionnaire | FCRI, administered at baseline and postintervention | Compared with controls, MBI participants exhibited significant improvements in FCR severity (d=1.01) from baseline to postintervention. | 13.7 min/day bAdherence rate could not be calculated. | |
| Huberty et al 201939 USA | 128 patients with myeloproliferative neoplasm [average age=58 years; 81% females; 96% white; 61% well-educated with a bachelor’s education or higher; 74% married] | 4-group cross-over design RCT with a and an educational control group | 8-week app-based MBI program of two meditation apps (10% Happier and Calm). Participants were asked to practice 10 min/day. | Smartphone app developers reported weekly practice data to the research team. | PROMISSF-anxiety and PROMISSF-depression, assessed at baseline, week 5, and week 9. | 10% Happier app participants reported significant improvements in anxiety (d=−0.43) and depression (d=−0.38). No significant differences were found between baseline and postintervention scores for anxiety (d=−0.22) and depression (d=−0.29) among Calm app participants. | All study participants: 7.2 min/day (72% adherence) 10% Happier app: 4.4 min/day (44% adherence) Calm app: 10.1 min/day (100% adherence) |
|
| Donovan et al 201940 USA | 20 adolescents or young adults with sarcoma [57% females; average age=19 years; 65% white] | Single-group | 4-week app-based MBI program. Participants were encouraged to practice daily. | Not specified | PCQL-32- Psychological Functioning subscale, administered at baseline and postintervention | Changes in psychological functioning were not statistically significant. | 4 min/day bAdherence rate could not be calculated. | |
| Poletti et al 201936 Italy | 20 patients with metastatic cancer [average age= 54 years; 85% females; 60% undergoing treatment] | Single-group | MBSR [8 weekly 2.5-h classes, 4.5-h retreat, home practice 30 min/day using a CD] | Home practice diary collected at intervention end | POMS, assessed at baseline, postintervention, and 2 and 4 months postintervention | POMST-TMD and POMS-depression subscale scores significantly improved postintervention. Benefits were maintained at 2- and 4-month follow-up. | 19 min/day (63% adherence) | |
| Park et al 202037 Japan | 74 females with stage I–III breast cancer [average age=53.7 years; 60% married; 46% employed] | Waitlist RCT | MBCT [8 weekly 2-h classes, no retreat, home practice 20–45 min/day using a compact disc] | Not specified | HADS and CARS, assessed at baseline, 8 and 12 weeks | MBCT participants reported significant improvements in HADS (d=1.17) and fear of recurrence (d: 0.43), compared with controls. Benefits were maintained at follow-up (4 weeks postintervention). | 24 min/day (53% adherence) | |
| Zhao et al 202038 China | 135 breast cancer survivors [average age= 53 years; 50% diploma or university degree; 93% married; average time since treatment completion= 2.3 years] | Waitlist RCT | MBCT [6 weekly 90-min classes, home practice 20–40 min/day using an audio tape and handouts] | Daily log | No distress measure was included in this study. | No distress measure was included in this study. | 23.7 min/day (59% adherence) | |
Notes: aAdherence rate was calculated using the following formula: average number of minutes of actual home practice per day/prescribed number of minutes of home practice per day x 100. bStudies did not specify the length of assigned home practice, which precluded adherence rate calculation.
Abbreviations: POMS-TMD, Profile of Mood States – Total Mood Disturbance; HADS, Hospital Anxiety and Depression Scale; RRQ, Rumination–Reflection Questionnaire; GAD-7, Generalized Anxiety Disorder Scale; PHQ-8, Patient Health Questionnaire Depression Scale; CARS, Concerns About Recurrence Scale; FCRI, Fear of Cancer Recurrence Inventory; C-SOSI, Calgary Symptoms of Stress Inventory; SOSI, Symptoms of Stress Inventory; PSWQ, Penn State Worry Questionnaire; STAI, State-Trait Anxiety Inventory; CESD, Center for Epidemiological Studies Depression Scale; PSS, Perceived Stress Scale; HAM-D, Hamilton Depression Rating Scale; HAM-A, Hamilton Anxiety Rating Scale; DASS, Depression, Anxiety and Stress Scale; PTGI, Post-Traumatic Growth Inventory; PROMISSF, Patient Reported Outcomes Measurement Information System Short Form (8-item); PCQL-32, Pediatric Cancer Quality of Life Inventory.
Study Characteristics
Studies included were conducted in the USA (n =7),27–31,39,40 Canada (n = 6),21–26 Australia (n = 2),32,41 Netherlands (n = 1),33 United Kingdom (n = 1),34 Denmark (n = 1),35 Italy (n = 1),36 Japan (n = 1),37 and China (n = 1).38 The studies included 13 randomized controlled trials,21,24,27,30–35,37–39,41 six single-group studies with pre-post study design,23,26,28,29,36,40 and two non-randomized controlled trials.22,25
Participant Characteristics
Sample sizes ranged from 15 to 245 participants, for a total of 1811 participants (average age = 52.5 years) in all 21 studies. With the exception of one study of adolescents and young adults (13 to 25 years old),40 all studies included only adult participants (≥18 years old). Eight studies included only female participants,25,27,29,34–38 with the remaining 13 primarily consisting of females (54–94%). Ten studies reported ethnicity and predominantly included white participants (70–96%).22,24,25,27–31,39,40 Of the studies reporting level of education (n = 15),21–28,30,31,33,35,38,39,41 most consisted of generally well-educated participants (for example, average years of formal education >14 years (n=4); completed some type of postsecondary education (63–78%) (n=6)). Fourteen studies reported relationship status and primarily included married or partnered participants (54–93%).
Seven studies recruited only female participants with breast cancer,27,29,34–38 one breast (83%) or prostate cancer,23 one breast (84%) or colorectal cancer,31 one myeloproliferative neoplasm,39 one sarcoma,40 and one melanoma.41 The remaining nine studies included patients with multiple cancer types and primarily consisted of breast cancer (30–85%).21,22,24–26,28,30,32,33 Most studies (n=11) recruited patients who had completed all primary cancer treatments,23–25,27–31,34,35,41 and the remainder (n=10) did not restrict eligibility by treatment status. Average time since primary treatment completion, where reported (n=6),25,27,29–31,38 ranged from less than a year (5–10 months (n=2)),27,29 to just over 4 years (n=1).30 Nine studies only included stage 0–III cancer,23,26,27,29,31,34,37,38,41 and two only advanced or metastatic cancer.28,36 Across the remaining studies, early‐stage (0–III) were more represented than late‐stage (IV) or advanced cancer patients (66–94% vs 13–34%, respectively).21,22,24,25,28,30,32,33,35,36,39,40 Seventeen studies assessed distress as a primary outcome, and four of them screened for distress as part of inclusion criteria.24,26,33,37 The remaining four studies evaluated fatigue (n=2),30,31 pain (n=1),35 or sleep disturbance (n=1)38 as a primary outcome.
Intervention Characteristics
Most studies (n=18) evaluated standardized MBI programs ((MBSR (n=7),27–31,34,36 MBCR (n=6),21–26 MBCT (n=5)32,33,35,37,38). The remaining three studies consisted of the following MBI interventions: (1) two smartphone-based mindfulness apps (10% Happier and Calm) including a range of daily meditations with a different focus (for example, 10% Happier: grief, gratitude, choice, and letting go; Calm: practicing patience, loving kindness, and gratitude);39 (2) a mobile-based app (customized version of an existing mindfulness app (Whil Concepts, Inc)) of different meditation techniques and breathing exercises, to help participants deal with negative thoughts and emotions and practice self-kindness through challenging times;40 and (3) an MBI program consisting of psychoeducation, formal and informal mindfulness practices.41
The most common mode of intervention delivery was in-person, group-based format (n=15), with the remainder using online (synchronous (n=1),24 asynchronous (n = 5)29,33,39–41) platforms. Group sizes were reported in eight studies and ranged from 4 to 25 participants per group.22,23,25,29,32,34,35,37 Three studies used an active comparison group: one compared in-person- vs online-MBCT;33 one MBSR to a structurally equivalent control condition (psychoeducational support);31 and one compared two mindfulness apps with an educational control group.39 Fifteen studies indicated groups were led by experienced or certified professional personnel, and eleven of them described the teacher’s credentials [clinical psychologist (n=8), nurse (n=2), medical doctor (n=1)]. Among standardized MBI programs (MBSR, MBCR, MBCT), six studies21,27–30,38 consisted of programs shorter [six (n=4) or seven (n=2) weekly classes] than the standard 8-week curriculum, and seven27–31,35,38 omitted the day-long retreat near the end of the program. To assist with home practice, most studies provided CDs, audio files, and/or a manual/booklet, and two used video recordings.24,29
Adherence to Home Practice
Most studies used self-report methods including daily or weekly logs, diaries, or forms to record home practice, with one using electronic diary recording [29]. In one smartphone app-based MBI, home practice was tracked by the app developers and reported weekly to the research team.39 In general, studies consisted of the following formal mindfulness home practices: a sitting meditation, gentle lying and yoga-based stretches, and/or body scan. Only six studies27–31,41 required informal practice by incorporating mindfulness into everyday situations in addition to formal mindfulness, yet none divided the reported amounts of total daily practice into formal and informal practice.
Across the 21 included studies, the pooled average of daily total home practice time during the treatment phase of the study was 23.5 min (range= 4–37 min). In line with standard home practice requirements, participants in eight studies were asked to practice 45 min daily,21–26,34,35 and the pooled average of actual practice time within these eight studies was 27 min/day (range=20.6–37 min), indicating suboptimal adherence (adherence rate=27/45 minx100=60%). One MBSR study consisted of home practice 30 min/day with an average actual daily practice time of 19 min/day, equating a 63% adherence rate (19/30 min x 100=63%).36 Similarly, two MBSR studies consisted of home practice 20 min/day to accommodate fatigued participants; one of them reported participants practiced on average 35 min/day (>100% adherence)30 and one 16.8 min/day (84% adherence).31 One MBCT study asked participants to practice up to 1-hour daily with participants completing on average 30 min/day (50% adherence).32 One app-based MBI consisted of home practice 10 min/day with participants completing on average 7.2 min/day (72% adherence).39 Five dose ranging studies asked participants to practice 15–20 to 40–45 min daily with adherence rates using the upper range limit (40–45 min) of 53%,37 57%,29 59%,38 80% (online asynchronous MBSR program),29 and 31% (study of advanced cancer patients).28 Overall, adherence rate was within the range of 40 to 60% in nine studies,22,24,26,27,32,34,35,37,38 more than 60% in eight studies,21,23,25,29–31,36,39 and less than 40% in one study.28 Three studies did not specify the length of assigned home practice, which precluded adherence rate calculation; one of them reported actual practice time of 29.6 min/day (MBCT),33 one 4 min/day (app-based MBI),40 and one 13.7 min/day (web-based MBI).41
Three studies23,30,35 tracked home practice of mindfulness during the follow-up period. In one waitlist RCT (7-week MBSR) of 35 cancer survivors, participants completed, on average, 35 min/day during the intervention period, and the majority (n=26) reported continued mindfulness practice during the 6-month follow-up for 20 min/day on average.30 In a second waitlist RCT (8-week MBCT) including 71 breast cancer survivors, the time spent on home practice among the treatment group (n=67) was, on average, 24 min/day, decreasing to 9 min/day (n=42) and 10 min/day (n=39) at 3- and 6-month follow-up, respectively.35 Similarly, participants in a single-group study of 59 patients with breast or prostate cancer practiced, on average, 37 min/day during the 8-week MBCT period, 19.6 min/day during the 6-month follow-up period (n=31), and 18 min/day during the time period between 6- and 12-month assessments (n=30).23 Overall, while participants continued to practice after the end of the MBI programs, they tended to practice less as time passed.
Factors Influencing Adherence
Only two studies26,33 evaluated factors influencing adherence to home practice. In one 8-week MBCR single-arm study including 38 breast cancer survivors, investigators did not find an association between the number of classes attended and amount of at-home mindfulness practice.26 Among the individual types of mindfulness practice, married or cohabitating females reported significantly more home practice of yoga than single, divorced, or widowed females (481 vs 260 min).26 Other factors associated with more yoga practice included lower baseline scores for depression (r=−0.44), as well as higher self-esteem (r=0.45), social support (r=0.41), and extraversion (r=0.35).26 Higher baseline anxiety scores were also associated with increased meditation practice time (r=0.36).26 In another RCT of 245 cancer survivors comparing in-person- vs online-MBCT, the average total daily home practice time did not differ significantly between groups (30.6 vs 28.7 min),33 indicating that the intervention modality was unrelated to home practice compliance.
Distress and Mindfulness Home Practice
Four studies21,27,28,34 found a relationship between home practice time and changes in psychological distress. In one waitlist RCT (8-week MBSR) of 114 breast cancer survivors, greater amounts of home practice were associated with improved scores on the Profile of Mood States-Total Mood Disturbance (POMS-TMD) and POMS-anxiety subscale.34 Another waitlist RCT (7-week MBCR) of 109 cancer patients found that participants who practiced more had larger reductions in POMS-TMD scores (r = −0.39), accounting for 15.5% of the variance in mood improvement.21 In a third RCT (6-week MBSR) of 85 breast cancer survivors, greater total home practice time was associated with decreases in perceived stress (r=−0.33).27 Among individual practices, minutes of body scan were related to positive changes in depression (r=−0.35), trait anxiety (r=−0.37), and perceived stress (r=−0.34), in which more practice time was associated with lower distress severity.27 Minutes of meditation were also associated with a decrease in fear of recurrence (r=−0.37), trait anxiety (r=−0.34) and perceived stress (r=−0.34).27 Similarly, in one single-arm study (6-week MBSR) of 26 patients with advanced stage cancer, home yoga was associated with a decrease in perceived stress (r = −0.47) and state anxiety (r =- 0.67), and home meditation with a decrease in state anxiety (r = −0.53).28
Two studies22,23 with positive effects on distress failed to show a dose-response relationship. In one nonrandomized waitlist trial (8-week MBCR) of 211 cancer survivors, no statistically significant associations were found between number of minutes of home meditation, yoga, and total practice and pre- to post-MBCR change in POMS-TMD, ruminative thinking, or worry scores.22 Similarly, a single-arm study (8-week MBCR) of 59 cancer survivors did not find a relationship between stress or cortisol changes and home practice minutes.23 Two studies27,38 did not evaluate distress changes, either published results separately or did not include a distress measure. All but two35,40 of the remaining studies yielded significant effects on distress, yet none addressed whether findings were related to home practice.
Study Quality Assessment
The results of the study quality assessments are provided in Supplementary File 1: Table S1A and B. A summary of the assessments is presented below.
Controlled Intervention Studies: Most studies (n=11)21,24,27,31–35,37–39 were randomized, adequately powered, and methodologically sound (for example, intent-to-treat analysis used) and, despite shortcomings in some of them such as not reporting blinding techniques, received a rating of “good”. Two RCTs30,41 were small and underpowered and received a rating of “fair”. The study by Labelle et al22 was adequately powered but non-randomized and suffered from high attrition (34%), and consequently was also rated as “fair”. Similarly, a non-randomized trial by Campbell et al25 had several unmet criteria, such as not performing power analysis, and received a rating of “fair”.
Single-Group Studies: All of the six single-group studies23,26,28,29,36,40 included employed appropriate methods for this research design, meeting most of the criteria on the NIH Assessment Tool. However, none was powered to detect a treatment effect, with sample sizes ranged from 15 to 59. They therefore received a rating of “fair”.
Discussion
This systematic review aimed to evaluate adherence to mindfulness home practice in cancer patients participating in MBI programs, to identify factors influencing adherence to home practice, and to estimate the relationship between home practice and psychological distress outcomes. Across the 21 studies included, the average time spent on home practice during MBI programs was 23.5 minutes per day; the range of assigned practice was wide, with a low of 10 min/day in a mindfulness app study to a full hour in one MBCT program. Rates of adherence across studies were variable, ranging from 31% to over 100%, according to the quantity of mindfulness home practice assigned. The amount of home practice reported is considerable, albeit less than assigned amounts. Among studies using the standard assignment of 45 minutes of practice per day, the pooled adherence rate for participants’ home practice was 60% of the assigned amount, which equated to 27 minutes per day. Average time per day spent practicing in studies that had lower quantities of assigned practice, such as 15–30 minutes, did not differ substantially from studies assigning standard amounts of home practice but, naturally, studies assigning less practice time tended to have better adherence rates. Additionally, all three studies23,30,35 that examined post-intervention home practice reported a decrease in average home practice time, dropping from 24–37 minutes per day during the intervention period to 10–20 minutes per day at 6-month follow-up.
Overall, the variable rates of practice within and across studies in the current review mirror findings by previous reviews. A systematic review of 43 studies, which included clinical and non-clinical populations, estimated 64% adherence to home practice and 30 min/day on average.42 Another recent review of 14 controlled studies did not report a pooled result across studies but found a range of 14 to 84% adherence to home practice and similarly noted decreases in the average time spent practicing over follow-up periods of 4 to 5 months.43
Although home practice is thought to be a key component of MBIs, only two studies identified in this review investigated predictors of adherence. Factors including marital status, mood disturbance at baseline, social support, and personality traits were found to be related to the amount of home practice (correlations were small to moderate, ranging between r=|0.35| to |0.45|).26,33 Future research should focus on further identifying factors affecting adherence. Specifically, studies should explore the relationship between home practice and demographic and/or medical characteristics, such as sex, gender, and disease severity, which are generally non-modifiable, to identify profiles of individuals at increased risk of nonadherence. Studies should also incorporate measures of modifiable predictors of treatment adherence. Treatment expectations, for example, were correlated with home practice adherence in a MBI for adolescents.44
Pending future quantitative investigations, qualitative studies of cancer patients participating in MBIs may provide insight into patient-oriented factors related to adherence that merit further investigation. For instance, a qualitative study among a sample of older adults identified time commitment and managing interruptions at home as major barriers to mindfulness home practice.45 Identifying modifiable factors is only the first step in improving compliance with the prescribed home practice regimen. This work will further inform ongoing efforts to determine optimal modes of intervention delivery and the necessary home practice resources and guidance provided to participants that will promote uptake and maintenance of home practice.
Results of methodologically sound investigations included in this review provide preliminary evidence of a relationship between home practice time and psychological distress outcomes among cancer patients. However, it is important to recognize that the methodological quality of the studies was primarily evaluated in relation to testing intervention effects, and not in relation to testing the association between home practice and psychological distress. Four studies reported statistically significant moderate-to-large negative correlations (ranging between r= −0.33 and −.67) between home practice time and measures of mood and anxiety,21,27,28,34 perceived stress and fear of cancer recurrence.27 Two studies reported non-significant correlations.22,23
These mixed results are consistent with those reported by previous systematic reviews of studies examining the effect of MBI programs on psychological distress in broader clinical and non-clinical samples.42,43 Lloyd et al43 found that home practice predicted clinical outcomes in four of seven studies examined, while Parsons et al42 found a small but statistically significant relationship between home practice and intervention outcomes, pooled across 28 studies (r=0.26). It is important to note that this evidence is correlational, and future research should utilize study designs that allow for causal conclusions to further investigate the influence of home practice on post-intervention psychological distress. These designs would also provide the statistical power necessary to examine whether the standard assignment of 45-minute per day is essential to positive clinical outcomes, or whether there may be a dose-response effect where shorter practice times also confer some benefit. This is an important question since optimal adherence may not be possible or desirable for all participants. The broader theoretical question of whether home practice, and if so how much home practice, is really essential to achieve benefit from MBIs remains, thus, unresolved, although more studies find a dose-response relationship than do not.
Studies included in this review used inconsistent methods to measure home practice. Many provided participants with diaries or logs to record daily or weekly practice and did not report details of the format. All investigations of MBI efficacy and/or effectiveness should include a standardized measure of home practice to allow for between-study comparison. The Mindfulness Adherence Questionnaire (MAQ), a scale designed to assess both the quantity and quality of mindfulness-meditation practice in the past week, is a promising candidate for widespread use. The MAQ distinguishes between formal and informal practice and is a reliable measure of quantity and quality of mindfulness practice that is responsive to change and is not driven by trait mindfulness.45 Since measures like the MAQ rely on retrospective self-report, which may introduce response biases, it is recommended to also provide participants with standardized practice diaries/logs measuring length, frequency and quality of daily home practice. One study in this review used a mindfulness app to objectively assess adherence.39 Although smartphone apps have shown the potential to more accurately track mindfulness home practice,46 further research is warranted to examine how they may affect intervention adherence and clinical outcomes in MBIs with cancer patients. While useful, paper and electronic diaries require participants to rely on memory and take time to log practice data, which may reduce participants’ compliance with diary protocols, in particular, when they fail to make timely entries, or exaggerate practice times, potentially invalidating the diary data.47 Smartphone apps’ tracking of mindfulness practice through the app not only could be a more reliable way to measure adherence and understand when and how often participants complete their assigned home practice, but also can reduce demands on research participants by eliminating the need to fill in diaries.
The present review has implications for MBI studies in cancer patients and mindfulness research more broadly. The evidence herein regarding less than optimal adherence to daily between-session home practice indicates a need to develop, test and implement strategies to facilitate adherence. For example, enhanced self-efficacy and self-motivation are factors suggested to improve the adoption and maintenance of health-related behaviors and self-care adherence.48 Understanding the role of these and other behaviour change techniques within the context of MBIs may provide greater scope for researchers to improve adherence to mindfulness home practice. One may argue that given the suboptimal adherence to mindfulness home practice identified in this review, increasing the length of assigned of home practice could be a way to increase actual practice time and improve benefits for participants. However, as noted above, the amount of home practice needed to achieve optimal benefit from MBI programs is currently unknown, and requires further investigation. Once evidence-based optimal home practice recommendations are established, these guidelines could be presented to participants, perhaps leading to better adherence as participants could feel confident about the minimum home practice required to achieve optimal benefit.
Limitations
The conclusions of this review should be interpreted in light of its limitations. This review focused on studies that were published in peer-reviewed journals in English; therefore, studies of MBIs with cancer populations published in the grey literature or in non-English languages that otherwise would meet criteria for inclusion are absent. Additionally, since meta-analysis was not performed, an assessment of statistical heterogeneity is not presented for this set of studies. Though a precise estimate is unavailable, it is likely that there is considerable variability of rates of home practice between studies. Previous meta-analyses of MBIs have generally found high statistical and clinical heterogeneity within MBI studies.9,49 This is reflected in the current review, since the study design, outcome measurement and intervention characteristics are quite different across the studies included. It is possible that the range of home practice estimates reported in this review may be a factor of this heterogeneity.
It is likely that this review does not precisely describe the amount of home practice by cancer patients participating in MBI programs. First, the upper range limit was used to calculate adherence rate in dose ranging studies, resulting in conservative adherence rates. Second, studies were only included if they reported quantifiable data on adherence to home practice (number of minutes). It is possible that articles that used other methods to describe adherence or did not report data on home practice had lower or higher adherence rates. Because these articles were excluded, this review cannot provide a comprehensive overview of the extent to which cancer patients complete home practice exercises assigned within the context of MBIs. This is an important methodological question, as participant enactment of skills taught by the intervention is a crucial component to estimate overall treatment fidelity and by extension, the internal validity of studies.50 Further, the very act of asking participants to self-monitor their home practice may act as an intervention to improve adherence when compared to naturalistic settings, which was not accounted for in this review.
One important element, adherence to informal home practice, could not be assessed by this review because of inconsistencies or absence of reporting in included studies. Generally, informal practice rates are rarely included in studies of MBIs as they are difficult to quantify,42 and there are few empirical investigations of the relative effects of informal mindfulness practice when compared to formal practice.42,43 The results of this review also focus only on the quantity of home practice among cancer patients participating in MBIs, and do not provide information about the quality. Quality of practice reflects skill acquisition and application, for instance remaining present-focused and offering non-judgmental attention, suggesting that this may be an important factor moderating the relationship between adherence to home practice and clinical outcomes. However, it is notoriously difficult to measure; we would recommend using the MAQ in this situation.
Last, the generalizability of the results in this review is limited. Participant samples of included studies were predominantly well-educated white women with breast cancer who have completed active treatment. This is a commonly cited limitation of mindfulness-based research51 and psychosocial research with cancer patients more broadly.52 The majority of participant samples were also married or living with a partner, indicating unpartnered cancer patients are underrepresented in MBI studies. Future research must strive to evaluate the efficacy of MBIs and patterns of home practice in more diverse samples.
Conclusion
Adherence to mindfulness home practice among cancer patients is not optimal, and studies report a wide range of adherence rates and minutes of home practice. The literature is scarce to identify factors influencing adherence to home practice or to definitively conclude that there exists a relationship between home practice and post-intervention improvements in psychological distress. Further, the literature is limited by homogeneous samples, inconsistent measurement practices focusing mostly on the quantity of practice, and gaps in the assessment of informal practices. Addressing these limitations is critical to advance the research agenda on MBIs for treating psychological distress in cancer patients, and to further clarify the relative contribution of home practice on clinical outcomes.
Acknowledgments
We would like to thank Marcus Vaska for his suggestions and contributions towards the search strategy and article extraction that was used within this systematic review.
Funding Statement
LEC holds the Enbridge Research Chair in Psychosocial Oncology, cofounded by the Canadian Cancer Society Alberta/NWT Division and the Alberta Cancer Foundation, as well as a Canadian Institutes of Health Research Mentorship Chair in Innovative Clinical Trials. MB, DO, and CM are supported by the Training in Research and Clinical Trials in Integrative Oncology (TRACTION) fellowship from the University of Calgary. MB is funded by a University of Calgary “Eyes High” Postdoctoral Fellowship. DO is supported by a joint Cumming School of Medicine-Charbonneau Cancer Institute Postdoctoral Fellowship. CM is supported by the Alberta Innovates Support for Patient-Oriented Research (SPOR) Graduate Studentships and an award from the Fonds de la recherche en santé du Québec (FRQS).
Disclosure
Dr Linda E Carlson reports book royalties from New Harbinger and from American Psychological Association Press; also Program royalties from EMindful.com, outside the submitted work. The authors declare no conflict of interest.
References
- 1.Bray F, Weiderpass E GLOBOCAN 2020 database provides latest global data on cancer burden, cancer deaths; 2020. Available from: https://ascopost.com/news/december-2020/globocan-2020-database-provides-latest-global-data-on-cancer-burden-cancer-deaths/. Accessed January16, 2021.
- 2.National Comprehensive Cancer Network; 2017. Available from: https://www.nccn.org/patients/guidelines/content/PDF/distress-patient.pdf https://www.nccn.org/about/news/ebulletin/ebulletindetail.aspx?ebulletinid=1120. Accessed January4, 2021.
- 3.Carlson LE, Zelinski EL, Toivonen KI, et al. Prevalence of psychosocial distress in cancer patients across 55 North American cancer centers. J Psychosoc Oncol. 2019;37(1):5–21. doi: 10.1080/07347332.2018.1521490 [DOI] [PubMed] [Google Scholar]
- 4.Mehnert A, Hartung TJ, Friedrich M, et al. One in two cancer patients is significantly distressed: prevalence and indicators of distress. Psychooncology. 2018;27(1):75–82. doi: 10.1002/pon.4464 [DOI] [PubMed] [Google Scholar]
- 5.Carlson LE. Distress management through mind-body therapies in oncology. J Natl Cancer Inst Monogr. 2017;2017(52). doi: 10.1093/jncimonographs/lgx009 [DOI] [PubMed] [Google Scholar]
- 6.Creswell JD. Mindfulness interventions. Annu Rev Psychol. 2017;68(1):491–516. doi: 10.1146/annurev-psych-042716-051139 [DOI] [PubMed] [Google Scholar]
- 7.Shennan C, Payne S, Fenlon D. What is the evidence for the use of mindfulness-based interventions in cancer care? A review. Psychooncology. 2011;20(7):681–697. doi: 10.1002/pon.1819 [DOI] [PubMed] [Google Scholar]
- 8.Rush SE, Sharma M. Mindfulness-based stress reduction as a stress management intervention for cancer care: a systematic review. J Evid Based Complementary Altern Med. 2017;22(2):348–360. doi: 10.1177/2156587216661467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oberoi S, Yang J, Woodgate RL, et al. Association of mindfulness-based interventions with anxiety severity in adults with cancer: a systematic review and meta-analysis. JAMA Netw Open. 2020;3(8):e2012598. doi: 10.1001/jamanetworkopen.2020.12598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149(7):936–943. doi: 10.1176/ajp.149.7.936 [DOI] [PubMed] [Google Scholar]
- 11.Santorelli SF, Kabat-Zinn J, Blacker M, Meleo-Meyer F, Koerbel L Mindfulness-based stress reduction (MBSR) authorized curriculum guide; 2017. Available from: http://www.umassmed.edu/cfm/training/mbsrcurriculum. Accessed May17, 2021.
- 12.Carlson LE. Mindfulness-based interventions for coping with cancer. Ann N Y Acad Sci. 2016;1373(1):5–12. doi: 10.1111/nyas.13029 [DOI] [PubMed] [Google Scholar]
- 13.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. 2nd ed. New York: Guilford Publications; 2013. [Google Scholar]
- 14.Bartley T. Mindfulness-Based Cognitive Therapy for Cancer: Gently Turning Towards. Oxford: Wiley Blackwell; 2011. [Google Scholar]
- 15.Lengacher CA, Reich RR, Kip KE, et al. Influence of mindfulness-based stress reduction (MBSR) on telomerase activity in women with breast cancer (BC). Biol Res Nurs. 2014;16(4):438–447. doi: 10.1177/1099800413519495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bowen S, Kurz AS. Between-session practice and therapeutic alliance as predictors of mindfulness after mindfulness-based relapse prevention. J Clin Psychol. 2012;68(3):236–245. doi: 10.1002/jclp.20855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Birtwell K, Williams K, van Marwijk H, Armitage CJ, Sheffield D. An exploration of formal and informal mindfulness practice and associations with wellbeing. Mindfulness (N Y). 2019;10(1):89–99. doi: 10.1007/s12671-018-0951-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crane C, Crane RS, Eames C, et al. The effects of amount of home meditation practice in mindfulness based cognitive therapy on hazard of relapse to depression in the staying well after depression trial. Behav Res Ther. 2014;63:17–24. doi: 10.1016/j.brat.2014.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):1. doi: 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 20.National Institutes of Health. NIH Study Quality Assessment Tools; 2014. Available from: https://www.nhlbi.nih.gov/. Accessed December3, 2020.
- 21.Speca M, Carlson LE, Goodey E, Angen M. A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med. 2000;62(5):613–622. doi: 10.1097/00006842-200009000-00004 [DOI] [PubMed] [Google Scholar]
- 22.Labelle LE, Campbell TS, Faris P, Carlson LE. Mediators of Mindfulness-Based Stress Reduction (MBSR): assessing the timing and sequence of change in cancer patients. J Clin Psychol. 2015;71(1):21–40. doi: 10.1002/jclp.22117 [DOI] [PubMed] [Google Scholar]
- 23.Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. 2007;21(8):1038–1049. doi: 10.1016/j.bbi.2007.04.002 [DOI] [PubMed] [Google Scholar]
- 24.Zernicke KA, Campbell TS, Speca M, McCabe-Ruff K, Flowers S, Carlson LE. A randomized wait-list controlled trial of feasibility and efficacy of an online mindfulness-based cancer recovery program: the eTherapy for cancer applying mindfulness trial. Psychosom Med. 2014;76(4):257–267. doi: 10.1097/PSY.0000000000000053 [DOI] [PubMed] [Google Scholar]
- 25.Campbell TS, Labelle LE, Bacon SL, Faris P, Carlson LE. Impact of Mindfulness-Based Stress Reduction (MBSR) on attention, rumination and resting blood pressure in women with cancer: a waitlist-controlled study. J Behav Med. 2012;35(3):262–271. doi: 10.1007/s10865-011-9357-1 [DOI] [PubMed] [Google Scholar]
- 26.Tamagawa R, Speca M, Stephen J, Pickering B, Lawlor‐Savage L, Carlson LE. Predictors and effects of class attendance and home practice of yoga and meditation among breast cancer survivors in a mindfulness‐based cancer recovery (MBCR) program. Mindfulness. 2015;6(5):1201‐ 1210. doi: 10.1007/s12671-014-0381-4 [DOI] [Google Scholar]
- 27.Lengacher CA, Johnson-Mallard V, Post-White J, et al. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psychooncology. 2009;18(12):1261–1272. doi: 10.1002/pon.1529 [DOI] [PubMed] [Google Scholar]
- 28.Lengacher CA, Kip KE, Barta M, et al. A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. J Holist Nurs. 2012;30(3):170–185. doi: 10.1177/0898010111435949 [DOI] [PubMed] [Google Scholar]
- 29.Lengacher CA, Reich RR, Ramesar S, et al. Feasibility of the mobile mindfulness-based stress reduction for breast cancer (mMBSR(BC)) program for symptom improvement among breast cancer survivors. Psychooncology. 2018;27(2):524–531. doi: 10.1002/pon.4491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johns SA, Brown LF, Beck-Coon K, Monahan PO, Tong Y, Kroenke K. Randomized controlled pilot study of mindfulness-based stress reduction for persistently fatigued cancer survivors. Psychooncology. 2015;24(8):885–893. doi: 10.1002/pon.3648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johns SA, Brown LF, Beck-Coon K, et al. Randomized controlled pilot trial of mindfulness-based stress reduction compared to psychoeducational support for persistently fatigued breast and colorectal cancer survivors. Support Care Cancer. 2016;24(10):4085–4096. doi: 10.1007/s00520-016-3220-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Foley E, Baillie A, Huxter M, Price M, Sinclair E. Mindfulness-based cognitive therapy for individuals whose lives have been affected by cancer: a randomized controlled trial. J Consult Clin Psychol. 2010;78(1):72–79. doi: 10.1037/a0017566 [DOI] [PubMed] [Google Scholar]
- 33.Compen F, Bisseling E, Schellekens M, et al. Face-to-face and internet-based mindfulness-based cognitive therapy compared with treatment as usual in reducing psychological distress in patients with cancer: a multicenter randomized controlled trial. J Clin Oncol. 2018;36(23):2413–2421. doi: 10.1200/JCO.2017.76.5669 [DOI] [PubMed] [Google Scholar]
- 34.Hoffman CJ, Ersser SJ, Hopkinson JB, Nicholls PG, Harrington JE, Thomas PW. Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: a randomized, controlled trial. J Clin Oncol. 2012;30(12):1335–1342. doi: 10.1200/JCO.2010.34.0331 [DOI] [PubMed] [Google Scholar]
- 35.Johannsen M, O’Connor M, O’Toole MS, Jensen AB, Højris I, Zachariae R. Efficacy of mindfulness-based cognitive therapy on late post-treatment pain in women treated for primary breast cancer: a randomized controlled trial. J Clin Oncol. 2016;34(28):3390–3399. doi: 10.1200/JCO.2015.65.0770 [DOI] [PubMed] [Google Scholar]
- 36.Poletti S, Razzini G, Ferrari R, et al. Mindfulness-based stress reduction in early palliative care for people with metastatic cancer: a mixed-method study. Complement Ther Med. 2019;47:102218. doi: 10.1016/j.ctim.2019.102218 [DOI] [PubMed] [Google Scholar]
- 37.Park S, Sato Y, Takita Y, et al. Mindfulness-based cognitive therapy for psychological distress, fear of cancer recurrence, fatigue, spiritual well-being, and quality of life in patients with breast cancer – a randomized controlled trial. J Pain Symptom Manage. 2020;60(2):381–389. doi: 10.1016/j.jpainsymman.2020.02.017 [DOI] [PubMed] [Google Scholar]
- 38.Zhao Y, Liu JE, Lewis FM, et al. Effects of mindfulness-based cognitive therapy on breast cancer survivors with insomnia: a randomised controlled trial. Eur J Cancer Care (Engl). 2020;29(5):e13259. doi: 10.1111/ecc.13259 [DOI] [PubMed] [Google Scholar]
- 39.Huberty J, Eckert R, Larkey L, et al. Smartphone-based meditation for myeloproliferative neoplasm patients: feasibility study to inform future trials. JMIR Form Res. 2019;3(2):e12662. doi: 10.2196/12662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Donovan E, Martin SR, Seidman LC, et al. A mobile-based mindfulness and social support program for adolescents and young adults with sarcoma: development and pilot testing. JMIR Mhealth Uhealth. 2019;7(3):e10921. doi: 10.2196/10921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Russell L, Ugalde A, Orellana L, et al. A pilot randomised controlled trial of an online mindfulness-based program for people diagnosed with melanoma. Support Care Cancer. 2019;27(7):2735–2746. doi: 10.1007/s00520-018-4574-6 [DOI] [PubMed] [Google Scholar]
- 42.Parsons CE, Crane C, Parsons LJ, Fjorback LO, Kuyken W. Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: a systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behav Res Ther. 2017;95:29–41. doi: 10.1016/j.brat.2017.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lloyd A, White R, Eames C, Crane R. The utility of home-practice in mindfulness-based group interventions: a systematic review. Mindfulness (N Y). 2018;9(3):673–692. [PMID: 29875880; PMCID: PMC5968057]. doi: 10.1007/s12671-017-0813-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Quach D, Gibler RC, Jastrowski Mano KE. Does home practice compliance make a difference in the effectiveness of mindfulness interventions for adolescents? Mindfulness. 2016;8(2):495–504. doi: 10.1007/s12671-016-0624-7 [DOI] [Google Scholar]
- 45.Parra DC, Wetherell JL, Van Zandt A, Brownson RC, Abhishek J, Lenze EJ. A qualitative study of older adults’ perspectives on initiating exercise and mindfulness practice. BMC Geriatr. 2019;19(1):354. doi: 10.1186/s12877-019-1375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mikolasek M, Witt CM, Barth J. Adherence to a mindfulness and relaxation self-care app for cancer patients: mixed-methods feasibility study. JMIR Mhealth Uhealth. 2018;6(12):e11271. doi: 10.2196/11271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stone AA, Shiffman S, Schwartz JE, Broderick JE, Hufford MR. Patient compliance with paper and electronic diaries. Control Clin Trials. 2003;24(2):182–199. doi: 10.1016/s0197-2456(02)00320-3 [DOI] [PubMed] [Google Scholar]
- 48.Slovinec D’Angelo ME, Pelletier LG, Reid RD, Huta V. The roles of self-efficacy and motivation in the prediction of short- and long-term adherence to exercise among patients with coronary heart disease. Health Psychol. 2014;33(11):1344–1353. doi: 10.1037/hea0000094 [DOI] [PubMed] [Google Scholar]
- 49.Sevilla-Llewellyn-Jones J, Santesteban-Echarri O, Pryor I, McGorry P, Alvarez-Jimenez M. Web-based mindfulness interventions for mental health treatment: systematic review and meta-analysis. JMIR Ment Health. 2018;5(3):e10278. doi: 10.2196/10278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. J Public Health Dent. 2011;71(s1):S52–S63. doi: 10.1111/j.1752-7325.2011.00233.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carlson LE. Uptake of mindfulness‐based interventions: a phenomenon of wealthy white western women? Clin Psychol. 2018;25:e12258. [Google Scholar]
- 52.Moyer A, Sohl SJ, Knapp-Oliver SK, Schneider S. Characteristics and methodological quality of 25 years of research investigating psychosocial interventions for cancer patients. Cancer Treat Rev. 2009;35(5):475–484. doi: 10.1016/j.ctrv.2009.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]