Abstract
Cavitary lung formation with spontaneous pneumothorax has been rarely reported as a complication of COVID-19 pneumonia. We report a rare case of a 38 years-old male patient affected by COVID-19 pneumonia, exceptionally complicated by a simultaneous giant cavity in the right upper lung and a small right pneumothorax in the right hemithorax. Whilst pneumothorax emphysema, giant bullae and pneumothorax with alveolar rupture are known to potentially develop in COVID-19 patients as a result of high-flow O2 support, the exact origin of the giant lung cavitation in our patient could be not confirmed. Cavitary lesions – featured by high mortality rate - are reportedly associated with lung infarctions and can be the aftermaths of pulmonary embolism, a rather common sequela of COVID-19 pneumonia. Radiological imaging is critical to support clinical decision making in the management of COVID-19 pneumonia, since not only it can visualize and stage the disease, but it can also detect and monitor the eventual onset of complications over time, even following patient discharge from hospital.
Keywords: COVID-19, Lung, Pneumothorax, Cavitary
Introduction
COVID-19 can present in various manifestations and computed tomographic (CT) imaging plays an critical role in diagnosing the stages of pneumonia caused by SARS-CoV-2 [1].
Idiopathic cavitary pulmonary lesions and pneumothorax are rare complications reportedly affecting a small proportion of COVID-19 patients [2], [3], [4], [5], [6],
Herein, we report a 38 years old male patient affected by COVID-19 pneumonia, developing simultaneous lung cavitation and pneumothorax.
Case presentation
On February 25, a 38-year-old-male patient presented to accident & emergency service (A&E) of Baqiyatallah hospital in Tehran (Iran) for fever (38˚C), complaining shortness of breath, chilling and malaise during the preceding 4 days. The patient had no relevant medical history.
Baseline O2 saturation at admission was 85%, increasing up to 92% following O2 supplementation. Laboratory tests showed a white blood cell count of 10,200/mm3 with 6.2% lymphocytes. The erythrocyte sedimentation rate (ESR = 84 mm/h) and the C reactive protein (CRP = 114.2 mg/L) were both importantly elevated. Liver function tests were also considerably abnormal [SGOT (AST) = 193 IU/L; SGPT (ALT) = 406 IU/L; alkaline phosphatase (ALP) = 609 IU/L]. Real time reversed polymerase chain reaction (RT-PCR) following nasopharyngeal swab samples resulted positive for SARS-CoV-2 infection.
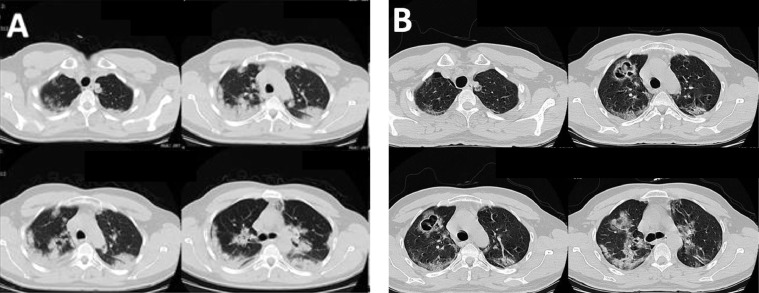
A Spiral multi-slice chest CT scan, performed on the same day of A&E admission, showed bilateral multilobar patchy ground glass opacities (GGOs) and consolidative lung opacities (CLO) with peripheral lung distribution (Fig. 1A), a radiological pattern compatible with COVID-19 pneumonia.
Fig. 1.
(A) Four IMAGES (on the first day, at hospital admission): multifocal subpleural patchy consolidative opacities compatible with COVID-19 pneumonia confirmed by RT-PCR test. (B) Four IMAGES (10 days later, at same chest level): significant clinical response to drug treatment, with a small right pneumothorax (black arrow) and an irregular wall cavitary lesion of about 40 mm in diameter (white arrow) at the right upper lung lobe.
The patient was treated with oral hydroxychloroquine sulfate 200mg twice a day, oral oseltamivir 75 mg twice a day, palliative therapy and O2 supplements. After 10 days of the latter treatment regimen, the WBC count decreased to 4.90/mm3 and the lymphocyte rate increased up to 24%. The ESR (95 mm/h) and CRP (115 mg/L) were still both elevated. The O2 saturation increased up to 89% without respiratory support and the patient's symptoms improved. As the patient's health conditions were progressively improving, a follow-up spiral chest computerized tomography (CT) scan, performed after 10 days since hospital admission, showed a significant reduction of the CLO and GGOs. However, the CT scan also revealed a giant cavity of about 40mm diameter, with a thick irregular wall in the right upper lung and a small pneumothorax in the right hemithorax (Fig. 1B).
Discussion
Classic COVID-19 pneumonia presents with GGO and CLO, predominantly in the lower lung lobes, without cavitary lesions, pneumothorax, lymphadenopathy and pleural effusion [3,4,7,8]. Complications of COVID-19 pneumonia can still arise over time and cavitary lung lesions (also of gigantic size) as well as pneumothorax have also been reported [2,4,[9], [10], [11], [12], [13]. Nevertheless, a simultaneous pneumothorax as well as cavitary lung formation is an exceptional and idiopathic feature.
Spontaneous pneumotorax can be a late evolution of COVID-19 pneumonia [14], although a bilateral sudden onset was also described in a 50 year old male smoker with history of mandibular carcinoma [15]. Emphysema, giant bullae and pneumothorax with alveolar rupture can develop in COVID-19 patients as a result of high-flow O2 support [12].
By contrast, pulmonary cavitary lesions are usually associated with mycobacterial diseases, fungal or parasitic infections, malignancies or autoimmune disorders [16,17]. Although the exact origin of the giant lung cavitation in our patient was not confirmed, diffuse alveolar damage, intra-alveolar haemorrhage and parenchymal necrosis associated with COVID-19 pneumonia can be explanatory factors [18,19]. Furthermore, cavitary lesions are reported in 4%-7% lung infarctions and can be the aftermaths of pulmonary embolism, a rather common complication of COVID-19 pneumonia [20, 21].
High mortality rates are reported with cavitations with due to pulmonary infarctions, whether infected or not [22]. Radiological imaging is therefore critical to support clinical decision making in the management of COVID-19 pneumonia, since not only it can visualize and stage the disease, but it can also detect and monitor the eventual onset of complications over time, even following patient discharge from hospital [4].
Authors’ contributions
All authors contributed equally to the drafting, designing and writing of the manuscript and provided critical revision. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This case report has been described in accordance with the ethical standards laid down in the “Declaration of Helsinki 1964.′′
Patient consent
Informed written consent was taken from the patient
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Acknowledgments: Not applicable.
Thanks to guidance and advice from ``Clinical Research Development Unit of Baqiyatallah Hospital’’
References
- 1.Campagnano S, Angelini F, Fonsi GB, Novelli S, Drudi FM. Diagnostic imaging in COVID-19 pneumonia: a literature review. J Ultrasound. 2021:1–13. doi: 10.1007/s40477-021-00559-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zoumot Z, Bonilla MF, Wahla AS, Shafiq I, Uzbeck M, El-Lababidi RM. Pulmonary cavitation: an under-recognized late complication of severe COVID-19 lung disease. BMC Pulm Med. 2021;21(1):24. doi: 10.1186/s12890-020-01379-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen Y, Chen W, Zhou J, Sun C, Lei Y. Large pulmonary cavity in COVID-19 cured patient case report. Ann Palliat Med. 2021;10(5):5786–5791. doi: 10.21037/apm-20-452. Jun 9:apm-20-452. [DOI] [PubMed] [Google Scholar]
- 4.Selvaraj V, Dapaah-Afriyie K. Lung cavitation due to COVID-19 pneumonia. BMJ Case Rep. 2020;13(7) doi: 10.1136/bcr-2020-237245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martinelli AW, Ingle T, Newman J, Nadeem I, Jackson K, Lane ND. COVID-19 and pneumothorax: a multicentre retrospective case series. Eur Respir J. 2020;56(5) doi: 10.1183/13993003.02697-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alhakeem A, Khan MM, Al Soub H, Yousaf Z. Case report: COVID-19-associated bilateral spontaneous pneumothorax-a literature review. Am J Trop Med Hyg. 2020;103(3):1162–1165. doi: 10.4269/ajtmh.20-0680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haseli S, Khalili N, Bakhshayeshkaram M, Taheri MS, Moharramzad Y. Lobar distribution of COVID-19 pneumonia based on chest computed tomography findings; a retrospective study. Arch Acad Emerg Med. 2020;8:e55. [PMC free article] [PubMed] [Google Scholar]
- 9.Afrazi A, Garcia-Rodriguez S, Maloney JD, Morgan CT. Cavitary lung lesions and pneumothorax in a healthy patient with active coronavirus-19 (COVID-19) viral pneumonia. Interact Cardiovasc Thorac Surg. 2021;32(1):150–152. doi: 10.1093/icvts/ivaa238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ammar A, Drap ´e J, Revel M. Lung cavitation in COVID-19 pneumonia. Diagn Interv Imaging. 2021;102(2):117–118. doi: 10.1016/j.diii.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marchiori E, Nobre LF, Hochhegger B, Zanetti G. Pulmonary infarctions as the cause of bilateral cavitations in a patient with COVID-19. Diagn Interv Radiol. 2020 doi: 10.5152/dir.2020.20865. (16 December)https://doi.org/10.5152/dir.2020.20865 [Epub Ahead of Print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vural A, Kahraman AN. Pulmonary embolism and giant cavitary lesion developing after COVID-19 pneumonia. HCA Healthcare J Med. 2020 doi: 10.36518/2689-0216.1109. 1: Iss. 0, Article 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ufuk F, Yavas HG, Kis A. An unusual cause of spontaneous pneumothorax: post-COVID-19 pulmonary fibrosis. Am J Emerg Med. 2021 doi: 10.1016/j.ajem.2021.04.084. S0735-6757(21)00371-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shirai T, Mitsumura T, Aoyagi K, Okamoto T, Kimura M, Gemma T. COVID-19 pneumonia complicated by bilateral pneumothorax: a case report. Respir Med Case Rep. 2020;31 doi: 10.1016/j.rmcr.2020.101230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teng E, Bennett L, Morelli T, Banerjee A. An unusual presentation of pulmonary embolism leading to infarction, cavitation, abscess formation and bronchopleural fistulation. BMJ Case Rep. 2018 doi: 10.1136/bcr-2017-222859. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koroscil MT, Hauser TR. Acute pulmonary embolism leading to cavitation and large pulmonary abscess: a rare complication of pulmonary infarction. Respir Med Case Rep. 2017;20:72–74. doi: 10.1016/j.rmcr.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Menter T, Haslbauer JD, Nienhold R, Savic S, Hopfer H, Deigendesch N. Post-Mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction. Histopathology. 2020:198–209. doi: 10.1111/his.14134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yao XH, Li TY, He ZC, Ping YF, Liu HW, Yu SC. A pathological report of three COVID-19 cases by minimal invasive autopsies. Zhonghua Bing Li Xue Za Zhi. 2020;49:411–417. doi: 10.3760/cma.j.cn112151-20200312-00193. [DOI] [PubMed] [Google Scholar]
- 19.Libby LS, King TE, LaForce FM, Schwarz MI. Pul- monary cavitation following pulmonary infarc- tion. Medicine (Baltimore) 1985;64(5):342–348. doi: 10.1097/00005792-198509000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Griffin DO, Jensen A, Khan M, Chin J, Chin K, Saad J. Pulmonary embolism and increased levels of d-Dimer in patients with coronavirus disease. Emerg Infect Dis. 2020;26(8):1941–1943. doi: 10.3201/eid2608.201477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Butler MD, Biscardi FH, Schain DC, Humphries JE, Blow O, Spotnitz WD. Pulmonary resection for treatment of cavitary pulmonary infarction. Ann Thorac Surg. 1997;63(3):849–850. doi: 10.1016/s0003-4975(96)01253-2. [DOI] [PubMed] [Google Scholar]