Abstract
Objectives
Spousal death is a common late-life event with health-related sequelae. Evidence linking poor mental health to disease suggests the hypothesis that poor mental health following death of a spouse could be a harbinger of physical health decline. Thus, identification of bereavement-related mental health symptoms could provide an opportunity for prevention.
Methods
We analyzed data from N = 39,162 individuals followed from 1994 to 2016 in the U.S. Health and Retirement Study; N = 5,061 were widowed during follow-up. We tested change in mental and physical health from prebereavement through the 5 years following spousal death.
Results
Bereaved spouses experienced an increase in depressive symptoms following their spouses’ deaths but the depressive shock attenuated within 1 year. Bereaved spouses experienced increases in disability, chronic-disease morbidity, and hospitalization, which grew in magnitude over time, especially among older respondents. Bereaved spouses were at increased risk of death compared to nonbereaved respondents. The magnitude of depressive symptoms in the immediate aftermath of spousal death predicted physical-health decline and mortality risk over 5 years of follow-up.
Discussion
Bereavement-related depressive symptoms indicate a risk for physical health decline and death in older adults. Screening for depressive symptoms in bereaved older adults may represent an opportunity for intervention to preserve healthy life span.
Keywords: Bereavement, CESD, Depression, Mortality, Physical health
Death of a spouse is a common life event for older adults and has significant health consequences. Bereavement is associated with acute increase in symptoms of depression, which manifest right around the time of death and subside within a year (Clayton, 1979; Kaufman, Lee, Vaughon, Unuigbe, & Gallo, 2018; Parkes, 1964; Taylor Jr, Kuchibhatla, Ostbye, Plassman, & Clipp, 2008; Zisook, Paulus, Shuchter, & Judd, 1997; Zisook & Shuchter, 1991, 1993). In contrast to the transience of depressive symptoms, physical-health sequelae of bereavement may be more persistent, as indicated by increased risk of death among the bereaved (Elwert & Christakis, 2008; Jones, Bartrop, Forcier, & Penny, 2010; Kaprio, Koskenvuo, & Rita, 1987; Prior et al., 2018; Shah et al., 2013; Shrira, Palgi, Bodner, & Shmotkin, 2016; Stahl, Arnold, Chen, Anderson, & Schulz, 2016). Despite empirical evidence for a link between mental- and physical-health sequelae of bereavement (Parkes, 1964) along with stress-biology theory positing several mechanisms for a causal relationship, including chronic inflammation and mitochondrial stress (Danese & McEwen, 2012; Han et al., 2019; Miller & Blackwell, 2006), mental- and physical-health sequelae of bereavement are most-often studied in isolation from one another. New data linking mental health symptoms with acceleration of aging-related physiologic deterioration (Brown et al., 2018; Lohman, Dumenci, & Mezuk, 2016; Moffitt & Caspi, 2019) provide evidence to support the stress-biology theory and suggest that mental-health sequelae of bereavement may represent a cause of subsequent physical health decline. If so, this connection would have implications for screening and management of mental-health sequelae of bereavement and potentially for preventive intervention to preserve health in aging.
However, there are significant methodological challenges associated with testing for connection between mental- and physical-health sequelae of bereavement. At a minimum, data are needed that track spouses’ mental and physical health over time, from before a spouse dies through the period of grief and recovery that follows. In addition, three further challenges must be overcome. First, bereavement-related health decline must be distinguished from the typical pattern of health decline that occurs with aging. Second, mental- and physical-health decline may accelerate during the period leading up to spousal death (Einiö, Moustgaard, Martikainen, & Leinonen, 2017; Vable, Subramanian, Rist, & Glymour, 2015). Sequelae of the specific shock of bereavement must be distinguished from the health declines during the prebereavement period. Third, mental- and physical-health sequelae of bereavement manifest over different time scales; transient mental-health sequelae arise and resolve over months while persistent physical-health sequelae emerge over years. To study links between mental- and physical-health sequelae of bereavement, observations of mental health symptoms during the months following bereavement must be linked with observations of physical health declines occurring over the following years. The aim of this study was to address these challenges in order to conduct a robust test of the linkage between mental- and physical-health sequelae of bereavement.
We analyzed longitudinal data tracking N = 39,162 adults aged 51 and older during the period 1994–2016 in the U.S. Health and Retirement Study, a nationally representative study of U.S. older adults (Juster & Suzman, 1995). During follow-up, we observed bereavement in 5,061 Health and Retirement Study (HRS) respondents. We first tested the short-term effect of spousal death on depressive symptoms. We next tested associations of spousal death with bereaved respondents’ disability, chronic disease morbidity, hospitalizations, and mortality over the 5 years following bereavement. Finally, we tested if those respondents who experienced more severe depression in the months following their spouses’ deaths went on to experience more severe declines in physical health over subsequent years. These analyses are designed to determine whether heightened depression following spousal death may act as a leading indicator of future physical-health decline.
Method
Data
The U.S.-based HRS is a nationally representative longitudinal study of health and aging ongoing since 1992 (Juster & Suzman, 1995). HRS includes a nationally representative sample of adults aged 51 and older and their spouses; its representativeness and design (in particular, long-term longitudinal collection of both mental and physical health measures) make it ideal for this study. We analyzed RAND Corporation’s 2016 HRS data release (v1); these data include N = 39,162 respondents meeting inclusion criteria: Respondents had to be over 50 and only married at most once during the course of HRS follow-up (see Supplementary Information A1 for more detail on respondents who remarried). Between the 1994 and 2016 observation waves, HRS observed these respondents over five waves on average (N total observations = 215,656). Summary statistics for HRS health measures are reported in Supplementary Table S1.
Bereavement
HRS records respondents’ death dates from the National Death Index and other sources (Bugliari et al., 2016). We analyzed death records for pairs of HRS spouses. We calculated time from spousal death as death date subtracted from HRS interview date (Supplementary Figures S1–S2). We analyzed data from n = 5,061 respondents widowed during follow-up and who were interviewed within 3 years of their spouse’s death. Bereaved respondents were more likely to be female (72% vs 56% in the HRS overall; see Supplementary Table S1) and to have been born earlier (mean birth year for HRS respondents = 1939 as compared to 1930 for our bereaved sample).
Mental Health Sequelae of Bereavement: Depressive Symptoms
We quantified mental-health sequelae of bereavement using a modified version of the Center for Epidemiologic Studies Depression (CES-D) scale (Radloff, 1977; Steffick, 2000). Modified CES-D scales have been shown to retain key measurement properties (Karim, Weisz, Bibi, & ur Rehman, 2015; Kohout, Berkman, Evans, & Cornoni-Huntley, 1993). Respondents gave yes/no responses to eight prompts (e.g., Is everything an effort? Did the respondent feel lonely? CES-D items are listed in Supplementary Information A2) based on their status the week prior to interview. We summed positive responses to compute respondents’ CES-D Scores. For some analyses, we standardize this CES-D score to have a mean of zero and standard deviation (SD) of 1.
Physical-Health Sequelae of Bereavement
We selected outcomes to represent burden of aging-related health decline that were measured in parallel across HRS assessment waves. Diagnosed chronic disease, disability, and mortality are three common metrics of physical health decline in aging. We also included hospitalization as an additional measure of health decline.
Chronic disease morbidity was measured as the count of chronic health conditions that respondents reported in response to prompts beginning “Has a doctor ever told you that you had….” The chronic conditions were high blood pressure, diabetes, cancer, lung disease, heart disease, stroke, and arthritis.
Disability was measured as counts of impairments to activities of daily living (ADLs) and instrumental activities of daily living (IADLs). We counted all activities for which the respondent reported some or more impairment. ADLs included bathing, dressing, eating, getting out of bed, and walking across a room. IADLs included using the phone, handling money, taking medication, shopping, and preparing meals.
Hospitalization was measured as the reported number of hospital stays during the previous 2 years. We coded all values of 10 or greater as 10. A limitation of the hospitalization measure is that, because reports capture information from the 2 years prior to the interview, the first observation following spousal death may include reports of hospitalizations occurring before spousal death. This limitation does not affect measures of hospitalization at two or more years following the death.
Mortality
Date of death was obtained HRS record linkage with the U.S. National Death Index and other sources (22).
To account for patterning of physical health outcomes with chronological age, measures were age-standardized for analysis. Details are reported below.
Analysis
We analyzed bereavement sequelae over the 5-year interval beginning with the first HRS interview following spousal death. We focused on the 5 years following spousal death because this interval captures at least two follow-up observations for each participant (HRS follows-up at 2-year intervals) while minimizing the sample restriction resulting from attrition. Our analysis aimed to address the three challenges to documenting connection among mental- and physical-health sequelae of bereavement outlined in the introduction. We describe our approach in detail (including a link to code that would allow for replication) in Supplementary Information A3. We outline this approach below.
To address the challenge of distinguishing sequelae of bereavement from typical aging-related health decline, we age-residualized measures of physical-health sequelae prior to analysis based on a model of normative aging. To develop a model for normative aging, we operationalized chronological age as a fifth-degree b-spline. We then conducted 100 bootstrap repetitions of the following analysis: We sampled one observation at random from each respondent in the HRS sample and regressed the health outcome on the age splines, sex, age–spline–sex interactions, and a series of dummy variables encoding the wave of the observation. We averaged coefficients across the bootstrap repetitions and use these averages to conduct our residualization. The residual values for the health measures carried forward into analysis thus represent deviations of a person’s health from the expectation given their chronological age. Supplementary Figure S5 shows that age-residualized health measures have no aging-related trends.
We conducted descriptive analysis comparing respondents mental and physical health before and after their spouse’s death. For physical health, which showed strong age-patterning in the HRS data, analysis focused on the age-residualized health values described above. We compared health before and after bereavement using person-level fixed-effects regression of health variables on an indicator of whether the observation was taken before or after spousal death (Equation 3, Supplementary Information A3).
To address the challenge of isolating effects of bereavement from health trends preceding spousal death, we used discontinuity models. We fitted person-level fixed-effects regression to repeated measures health data. The person-level fixed-effects regression focuses analysis on within-person change. This model holds constant all characteristics of the individual that do not change over time. To fit the discontinuity model, we conducted fixed-effects regression of health on a variable encoding time, an indicator variable coding whether the observation was taken before or after spousal death, and the interaction of those two variables (Supplementary Information A3, Equation 4). Time values were centered on date of spousal death. The coefficient for the indicator variable estimates immediate change in health at the time of spousal death. The time coefficient estimates the rate of change in health during the time leading up to spousal death. The interaction coefficient estimates the change in health decline occurring with bereavement.
To address the challenge of analyzing mental- and physical health sequelae of bereavement on different time scales, we modeled mental-health sequelae (CES-D depressive symptoms) using an exponential decay model (Lindstrom & Bates, 1990). We applied these models to data from the first observation of an individual after their spouses’ death (Supplementary Information A3, Equation 1). The exponential decay model uses CES-D data collected from respondents who were interviewed at varying amounts of time from their spouse’s death to estimate a function that describes how depressive symptoms decline with increasing time since spousal death. In the current analysis, we used the exponential decay model to calculate residual values for respondents that quantified how much more or less depressed they were than would be expected for the average bereaved HRS respondent observed at the same amount of time following their spouse’s death. To test connections between mental- and physical-health sequelae of bereavement, we inserted these residual values into the discontinuity model. Specifically, we modeled interactions between discontinuity-model terms and the CES-D residual values. The resulting model tests the hypothesis that transient depressive symptoms during bereavement predict health decline over the subsequent 5 years (Supplementary Information A3, Equation 5).
Missing Data
We conducted complete-case analysis, that is, respondents with missing data were excluded. Missing data are detailed in Supplementary Information A3.
Results
Death of a Spouse Is Associated with a Transient Increase in Symptoms of Depression
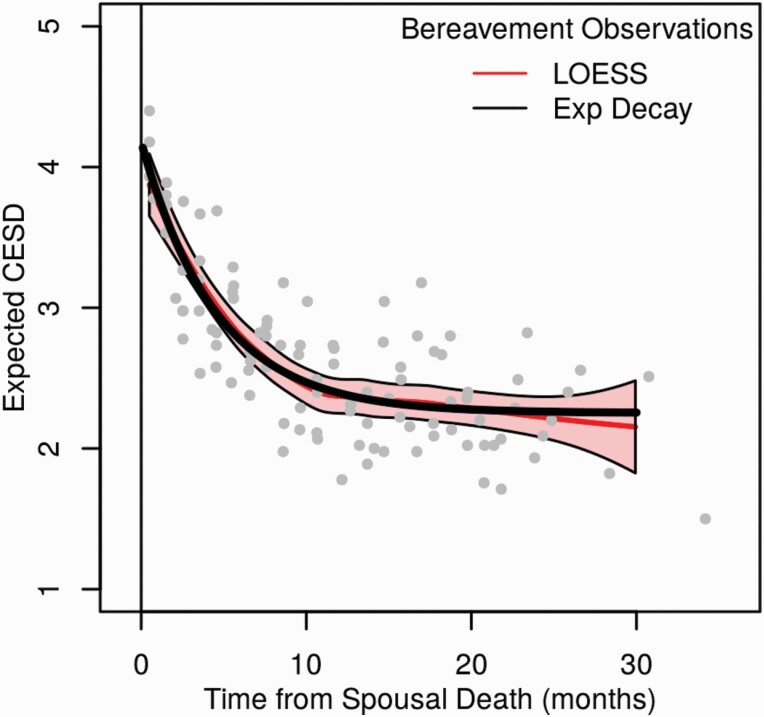
We visualized changes in depressive symptoms occurring following spousal death by plotting LOESS curves (Cleveland, 1979) of respondents’ CES-D scores in the years surrounding their spouses’ deaths (Figure 1). HRS respondents who lost their spouses experienced a sharp increase in depressive symptoms at the time of death and recovered toward the long-run level of depression within the following year, consistent with patterns observed in previous research (Zisook & Shuchter, 1991). In the first 2 years following their spouses’ deaths, respondents scored an average of 0.50 SD higher on the CES-D (95% confidence interval [CI] 0.45–0.56; Supplementary Table S3, Column 1) as compared to their CES-D scores from interviews prior to their spouses’ death. By the second interview following their spouse’s death, CES-D scores had returned toward baseline levels; scores were 0.08 SD higher on the CES-D (95% CI 0.02–0.13; Supplementary Table S3, Column 3).
Figure 1.
Depressive symptoms after spousal death. The figure shows a binned scatterplot and LOESS-fitted trend-lines illustrating Center for Epidemiologic Studies Depression scale (CES-D)-measured depressive symptoms during the 3 years before and after spousal death among widowed Health and Retirement Study (HRS) respondents (N = 5,061). LOESS-based trajectory of depression (with CI) for bereavement observations versus fits from exponenential decay models. LOESS and exponential decay estimates are based on original, not binned, data.
To model the sharp increase in depressive symptoms occurring at the time of spousal death and the subsequent exponential decline over time, we fitted an exponential decay model (Lindstrom & Bates, 1990) to CES-D scores from the first interview following spousal death (i.e., Equation 1, Supplementary Information A3). The average respondent experienced an increase of 1.93 (95% CI 1.62–2.24) depressive symptoms immediately following their spouse’s death and recovered to near their long-run mean over the next 8 months. Findings were similar for men and women (p-value for test of sex difference = .09) and for older and younger respondents (p-value for test of age difference = .99). Results from decay models are reported in Supplementary Table S2. Symptoms of loneliness and sadness accounted for most of the bereavement-related increase in CES-D scores (Supplementary Figures S7 and S8).
Death of a Spouse Is Associated with Persistent Increases in Burden of Disability, Morbidity, and Mortality
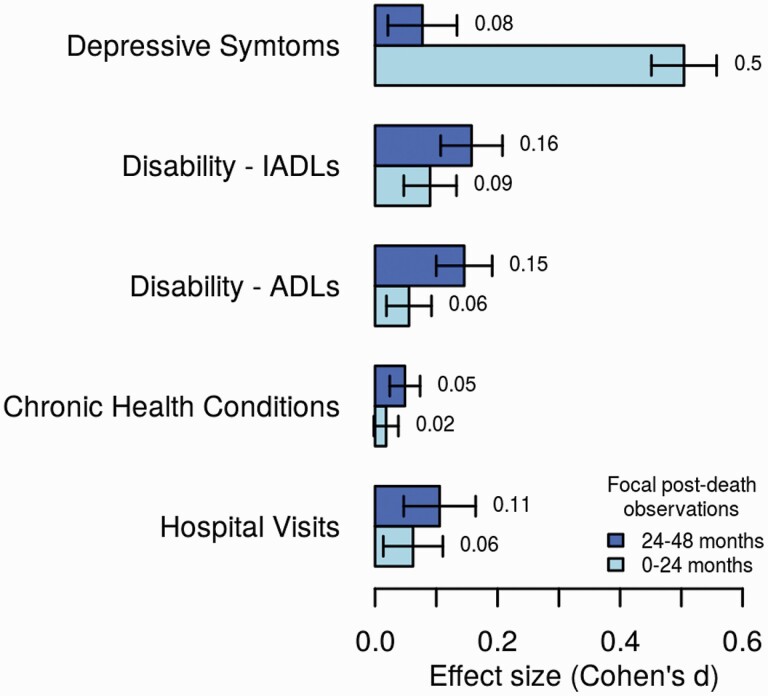
Parallel to our analysis of depressive symptoms, we found that respondents reported increased limitations to IADLs, ADLs, chronic disease morbidity, and hospitalizations within 2 years of spousal death as compared to levels reported at previous interviews (b = 0.02–0.09; Supplementary Table S3, Column 1). However, whereas bereaved respondents recovered from increased depressive symptoms within a year of their spouses’ deaths, physical health problems worsened over time. As of the second follow-up assessment after their spouses’ deaths, bereaved participants reported increased disability, morbidity, and hospitalizations as compared to their prebereavement baseline (b = 0.05–0.16 SD; Supplementary Table S3, Column 3). These increases were larger than increases measured at the first postbereavement assessment (as shown in Figure 2). Importantly, these estimates are adjusted for the expected increase in physical health problems that occurs with aging.
Figure 2.
Bereavement-related depressive symptoms decline with time since spousal death, whereas disability and morbidity increase. Figure graphs effect sizes and 95% confidence intervals for within-person comparisons of Center for Epidemiologic Studies Depression scale (CES-D) and physical health measures before and after spousal death. Effect sizes are graphed for comparisons of average levels predeath to the level at the first observation following spousal death (0–24 months after the death, light bars) and at the second observation following spousal death (24–48 months after the death, dark bars). Health outcomes were adjusted for aging-related decline and period effects (outcome measures were residualized for age [five splines], sex, interactions between the age-based splines and sex, and Health and Retirement Study (HRS) observation wave). Effect-sizes are reported in HRS standard deviation units. Results are based on Equation 3, Supplementary Information A3; full model results are shown in Supplementary Table S3 (minimum N = 13,152 observations of N = 3,145 individuals observed at two HRS observations following spousal death). The figure shows that the increase in depressive symptoms relative to prebereavement levels is largest in the first 2 years following spousal death and then declines. In contrast, increases in disability and morbidity grow larger with increasing follow-up time.
We tested if increasing time since spousal death was associated with worsening physical health outcomes using the discontinuity model (Supplementary Information A3, Equation 4). Increasing time since spousal death was associated with worsening physical health, over and above aging-related and prebereavement trends (Supplementary Figure S11). For ADLs and IADLs, this was due primarily to changes for older respondents (Supplementary Table S4) and declines were more pronounced for men as compared to women (Supplementary Figure S10).
Consistent with increase in health problems, bereaved respondents were also at increased risk of mortality over the 5 years of follow-up. Of the bereaved respondents, 22% died during this follow-up interval (see also Supplementary Figure S3). We compared 5-year mortality risk for bereaved respondents to 5-year mortality across all HRS observations. On average, mortality risk was 2.7 percentage points higher for observations following spousal death when compared with other observations (p < .001, Supplementary Table S5). This risk of increased mortality was concentrated among the older adults and men (Supplementary Information C).
Bereavement-Related Physical Health Declines Were Most Pronounced in Older HRS Respondents
Disability and morbidity were concentrated in older HRS respondents (Supplementary Figure S4B). We therefore investigated whether mental- and physical-health sequelae of bereavement differed for older as compared to younger HRS respondents. For mental-health sequelae, we found no difference; increases in depressive symptoms following spousal death were similar for younger HRS respondents as compared to older HRS respondents (Supplementary Table S2). In contrast, physical-health sequelae of bereavement were more severe for older HRS respondents and less severe for younger ones (see Supplementary Information C; results for disability, chronic disease, and hospitalization in Supplementary Table S3, columns 2 and 4; results for mortality in Supplementary Table S5, column 2).
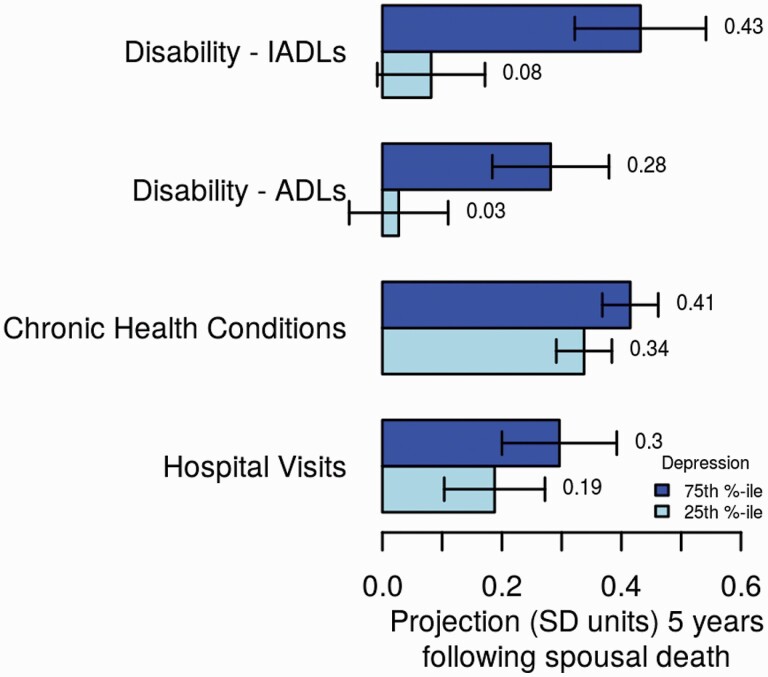
HRS respondents who experienced more depressive symptoms immediately following their spouse’s death suffered worse health decline over the following years when compared with respondents who experienced fewer depressive symptoms.To test if transient mental-health sequelae of bereavement were related to more persistent physical health sequelae, we incorporated results from our exponential decay analysis of depressive symptoms into our discontinuity models testing bereavement effects on physical health. We compared predicted health outcomes of respondents with relatively low levels of bereavement-related depressive symptoms (25th percentile, about two fewer symptoms than the norm) to health outcomes for respondents with relatively high levels of depressive symptoms (75th percentile, about two more symptoms than the norm). Because adverse health outcomes were concentrated among older HRS respondents, we conducted stratified analysis in older and younger respondents using age 74 at the time of spousal death as the cutoff.
Among older HRS respondents (n = 2,337), those with more severe depression following their spouse’s death experienced steeper increases in health problems in the subsequent years, primarily in counts of IADLs and ADLs. Differences are illustrated in Figure 3. At 5 years after spousal death, differences in health decline between these groups ranged from b = 0.35 for IADLs to b = 0.07 for chronic health conditions. Among older HRS respondents, physical-health differences between depressed and nondepressed respondents were larger for men as compared to women (Supplementary Figure S13). Among younger HRS respondents (aged 55–74, n = 2,178), effect sizes for associations between depressive symptoms and disabilities following bereavement were smaller (Supplementary Figure S12).
Figure 3.
Higher levels of bereavement-related depressive symptoms are associated with poor physical health 5 years following spousal death. Figure graphs predicted values and 95% confidence intervals for physical health outcomes of older respondents (aged 74 and older at the time of spousal death) with relatively high levels of bereavement-related depressive symptoms (75th percentile, dark bars) and relatively low levels of bereavement-related depressive symptoms (25th percentile, light bars). Analysis included all observations within 5 years of spousal death (minimum N = 16,766 observations of N = 2,337 individuals). Health outcomes were adjusted for aging-related decline and period effects (outcome measures were residualized for age [five splines], sex, interactions between the age-based splines and sex, and Health and Retirement Study [HRS] observation wave). Predicted health values are denominated in HRS standard deviation units. Confidence intervals were estimated via 1,000 bootstrap replications. Model results are reported in Supplementary Table S6.
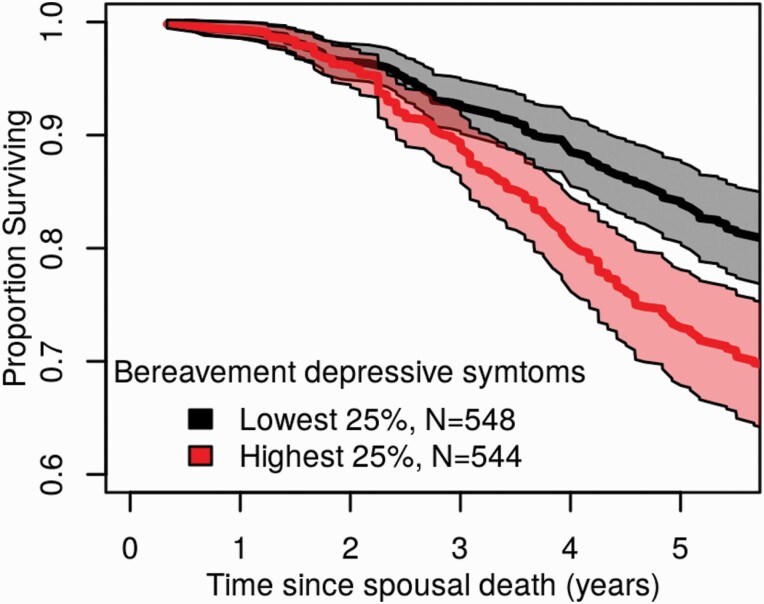
Parallel to analysis of morbidity and disability, older HRS respondents who experienced more severe depressive symptoms following their spouse’s deaths were more likely to die themselves over the subsequent 5 years (Figure 4). For respondents aged 74 and older at time of spousal death, those with relatively higher levels of bereavement-related depression had a 44% greater risk of death over the next 5 years as compared to respondents with relatively lower levels of bereavement-related depression (for the 75th percentile, risk of death was 21% (95% CI 17%–23%); for the 25th percentile, risk of death was 14% (95% CI 11%–17%); based on Supplementary Table S7). Sex differences were relatively small (Supplementary Table S7). Although absolute risks were much lower, respondents younger than 74 with relatively high levels of bereavement-related depression also experienced a 78% greater risk of death (again comparing predicted risk at 75th and 25th percentiles) over the next 5 years.
Figure 4.
Survival among bereaved respondents stratified by level of depression during bereavement. The figure plots survival curves for respondents with relatively low levels of bereavement-related depressive symptoms (25th percentile and below, dark slope) and relatively high levels of bereavement-related depressive symptoms (75th percentile and above, light slope). The figure shows poorer survival outcomes for those experiencing more severe depressive symptoms in bereavement.
Discussion
We analyzed connections between mental- and physical-health sequelae of bereavement in longitudinal data tracking 5,061 widowed older adults in the U.S. HRS. Bereavement was characterized by an acute increase in depressive symptoms, from which respondents recovered over roughly the next year. In contrast, bereaved respondents’ physical health worsened with time, especially their risk for disability and death, consistent with observations in previous studies (Hughes & Waite, 2009). Physical health declines were most pronounced in the oldest HRS respondents and among men. Intriguingly, our findings suggest that respondents’ acute and transient increases in depressive symptoms were connected with their subsequent longer-term declines in physical health. Thus, bereavement-related symptoms of depression appear to be a harbinger of subsequent physical health decline, with those older adults experiencing the most severe depressive symptoms following their spouses’ deaths going on to suffer the sharpest increases in risk for morbidity, disability, and mortality.
Our main innovation is the careful test of connections between transient symptoms of depression and longer-term physical health declines among bereaved older adults. We found that widows and widowers who experienced more severe increases in depressive symptoms in the first years following their spouse’s death went on to suffer steeper declines in physical health in the years afterward, even after accounting for health changes during the period leading up to spousal death. This pattern of decline in physical health was more pronounced among respondents who were in their 70s and 80s at the time of their spouse’s death as compared to respondents who were in their 50s and 60s. One explanation for the larger effect-sizes we observed for older as compared to younger HRS respondents is that aging-related declines in the physical health measures we studied are most pronounced after the age of 70 (e.g., see Supplementary Figure S4).
The relationship between depressive symptoms and aging-related physical-health decline is likely to be bidirectional (Kelley-Moore & Ferraro, 2005; Penninx, Deeg, van Eijk, Beekman, & Guralnik, 2000). Our analysis disentangles the pattern of reciprocal causation to isolate associations of depressive symptoms with subsequent physical health decline through three features of the research design. First, to guard against reverse causation, we tested short-term depressive symptoms as predictors of medium-to-long-term changes in morbidity, disability, and mortality. Second, to rule out confounding by stable individual differences, we analyzed within-person change over time. Third, to rule out confounding by prebereavement trends, we used discontinuity analysis to isolate health changes occurring after spousal death. Together, these design features identify a prospective association between depressive symptoms in the immediate aftermath of spousal death and increases in morbidity, disability, and mortality risk over the 5 years following the death. In summary, our analysis provides new evidence linking mental-health problems with subsequent physical-health decline in later life.
Our findings have implications for research into connections between mental and physical health in aging and for clinical and public health approaches to bereavement in older adults. Studies are needed to investigate mechanisms of the prospective association between bereavement-related depression and subsequent physical-health decline. One possibility is that transient symptoms of depression following spousal death induce lasting shifts in behavior that contribute to health decline, such as increased sedentary lifestyle. Such a process could also occur at the molecular level, with depression-related changes in immune-system dysregulation and chronic inflammation (Dantzer, O’Connor, Freund, Johnson, & Kelley, 2008; Miller & Raison, 2016) persisting after depressive symptoms resolve. Studies are also needed to test if specific risk factors predispose to bereavement-related health declines. Exposures accumulating from early-life including perinatal insults, childhood adversity, and socioeconomic disadvantage across the life course are associated with increased vulnerability to depression and greater burden of physical-health problems (Danese & McEwen, 2012; Lumey, Stein, & Susser, 2011; Matthews & Gallo, 2011; Miller, Chen, & Parker, 2011). And, genetic differences between individuals may explain variation in risk for depression in bereavement (Domingue, Liu, Okbay, & Belsky, 2017). Future research could test if individuals with a genetic liability for depression also experience more pronounced physical health declines following adverse life events.
For clinical and public-health approaches to managing bereavement in older adults, our analysis does not establish that treatment of mental health sequelae of bereavement could prevent subsequent physical health decline. However, the association identified in our study can inform prognosis for older adults who have suffered the loss of a spouse. Short-term, transient depressive symptoms related to bereavement are a harbinger of long-term physical health decline in older adults. At minimum, the results reported here amplify calls for increased efforts to integrate mental health screening into geriatrics practice (Siu et al., 2016; Smith & Meeks, 2019). They also suggest that follow-up to positive screens should extend beyond efforts to address symptoms of depression and include efforts to monitor and prevent physical health decline. To date evidence for efficacy of depression screening in primary care is limited (Mojtabai, 2017). Findings from this study suggest that evaluating effectiveness of depression screening in geriatric patients should include monitoring medium-term physical health outcomes as well as depressive symptoms.
We acknowledge limitations. The CES-D is an incomplete measurement of mental-health sequelae of bereavement. Replication of findings in studies with comprehensive assessment of depressive symptomatology and evaluation of other symptom dimensions is needed. However, an advantage of the brief symptom inventory used here is that it approximates a tool that could be deployed in clinical practice. All mental- and physical-health sequelae were reported by the respondents. Common reporter bias could inflate associations. However, physical-health sequelae continued to worsen years after respondents’ mental health had returned to prebereavement levels. Thus, associations were not driven by elevated depressive symptoms at the time respondents reported physical health problems. Nevertheless, replication of findings in data linking respondents with health care claims or clinical exam data will clarify effect sizes.
Our analysis treated bereavement as a homogeneous shock. There is, however, heterogeneity in the ways the bereaved experienced spousal loss (King, Carr, & Taylor, 2020). To the extent this heterogeneity is reflected in measured depressive symptoms, it will not bias our analysis. However, it is possible that specific social roles or caregiving obligations may affect mental- and physical-health sequelae of bereavement in different ways. Consistent with other research (Sasson & Umberson, 2014), we observed no sex differences in symptoms of depression following spousal death. But men experienced more pronounced health declines as compared to women. In parallel, the relationship of bereavement-related depression with future health declines was stronger for men as compared to women, although this difference was not observed for mortality. Further research is needed to clarify potential heterogeneity in the psychological impacts of bereavement and how this heterogeneity may affect physical health decline.
There are also limitations associated with the structure of HRS data collection and associated study design. Observations of HRS respondents immediately following their spouse’s death may selectively exclude respondents experiencing the most severe mental-health sequelae of bereavement. However, we did not observe a difference in the time intervals for observations bracketing spousal death as compared to other pairs of adjacent observations (Supplementary Figure S2B). A related limitation is that mortality selection may conceal the full extent of links between acute depressive symptoms of bereavement and physical health decline. We do not observe respondents who die during the interval between their spouse’s death and the next HRS interview. These respondents might choose to postpone their HRS interviews. However, we expect such missing data would bias towards estimates toward the null, making our estimates conservative. Finally, our focus on those respondents who did not remarry limits the generalizability of our findings to bereaved respondents who do not remarry.
Within the scope of these limitations, our findings highlight a potential opportunity for public health prevention. With an aging population, the number of older adults at risk for death of their spouse is growing. Our findings suggest that monitoring of depressive symptoms in bereaved older adults may help identify persons at risk for future health decline. Targeted interventions with individuals exhibiting particularly high levels of depression following the death of their spouse represent an opportunity to increase precision of geriatric medicine. In parallel, social interventions to address the isolation and loneliness that can result from the loss of a life partner may also help to blunt bereavement’s adverse physical health sequelae. Findings also suggest new directions for research to investigate mechanisms linking mental and physical health in aging. The advent of molecular datasets for social surveys, such as the U.S. Health and Retirement Study’s 2016 Venous Blood Study, opens new opportunities to explore biological mechanisms underpinning associations among spousal death, depressive symptoms, and increased risk for disability, morbidity, and mortality.
Supplementary Material
Acknowledgments
Author Contributions: The study was designed by B. W. Domingue and D. W. Belsky. B. W. Domingue conducted all analyses. Drafting of manuscript was done primarily by B. W. Domingue and D. W. Belsky. All authors contributed critical feedback related to study design and execution and to manuscript preparation and revision.
Funding
A. Harrati is supported by the National Institute on Aging grant R01-AG026291. D. W. Belsky is supported by an Early Career Fellowship from Jacobs Foundation. This work was partially supported by National Institute on Aging grant R21AG054846 and Russell Sage Foundation grant 1810–08987. The Health and Retirement Study is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan.
Conflict of Interest
None reported.
References
- Brown, P. J., Wall, M. M., Chen, C., Levine, M. E., Yaffe, K., Roose, S. P., & Rutherford, B. R. (2018). Biological age, not chronological age, is associated with late-life depression. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 73(10), 1370–1376. doi: 10.1093/gerona/glx162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bugliari, D., Campbell, N., Chan, C., Hayden, O., Hayes, J., Hurd, M., ... St.Clair, P. (2016). Rand HRS data documentation, version P. Santa Monica, CA: RAND Center for the Study of Aging. [Google Scholar]
- Clayton, P. J. (1979). The sequelae and nonsequelae of conjugal bereavement. The American Journal of Psychiatry, 136(12), 1530–1534. doi: 10.1176/ajp.136.12.1530 [DOI] [PubMed] [Google Scholar]
- Cleveland, W. S. (1979). Robust locally weighted regression and smoothing scatterplots. Journal of the American Statistical Association, 74(368), 829–836. doi: 10.1080/01621459.1979.10481038 [DOI] [Google Scholar]
- Danese, A., & McEwen, B. S. (2012). Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiology & Behavior, 106(1), 29–39. doi: 10.1016/j.physbeh.2011.08.019 [DOI] [PubMed] [Google Scholar]
- Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W., & Kelley, K. W. (2008). From inflammation to sickness and depression: When the immune system subjugates the brain. Nature Reviews. Neuroscience, 9(1), 46–56. doi: 10.1038/nrn2297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domingue, B., Liu, H., Okbay, A., & Belsky, D. W. (2017). Genetic heterogeneity in depressive symptoms following the death of a spouse: Polygenic score analysis of the US Health and Retirement Study. American Journal of Psychiatry, 174(10), 963–970. doi: 10.1176/appi.ajp.2017.16111209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Einiö, E., Moustgaard, H., Martikainen, P., & Leinonen, T. (2017). Does the risk of hospitalisation for ischaemic heart disease rise already before widowhood? Journal of Epidemiology and Community Health, 71(6), 599–605. doi: 10.1136/jech-2016-207987 [DOI] [PubMed] [Google Scholar]
- Elwert, F., & Christakis, N. A. (2008). The effect of widowhood on mortality by the causes of death of both spouses. American Journal of Public Health, 98(11), 2092–2098. doi: 10.2105/AJPH.2007.114348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han, L. K. M., Verhoeven, J. E., Tyrka, A. R., Penninx, B. W. J. H., Wolkowitz, O. M., Månsson, K. N. T., Picard, M. (2019). Accelerating research on biological aging and mental health: Current challenges and future directions. Psychoneuroendocrinology, 106, 293–311. doi: 10.1016/j.psyneuen.2019.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes, M. E., & Waite, L. J. (2009). Marital biography and health at mid-life. Journal of Health and Social Behavior, 50(3), 344–358. doi: 10.1177/002214650905000307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, M. P., Bartrop, R. W., Forcier, L., & Penny, R. (2010). The long-term impact of bereavement upon spouse health: A 10-year follow-up. Acta Neuropsychiatrica, 22(5), 212–217. doi: 10.1111/j.1601-5215.2010.00482.x [DOI] [PubMed] [Google Scholar]
- Juster, F. T., & Suzman, R. (1995). An overview of the health and retirement study. Journal of Human Resources, 30, S7–S56. doi: 10.2307/146277 [DOI] [Google Scholar]
- Kaprio, J., Koskenvuo, M., & Rita, H. (1987). Mortality after bereavement: A prospective study of 95,647 widowed persons. American Journal of Public Health, 77(3), 283–287. doi: 10.2105/ajph.77.3.283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karim, J., Weisz, R., Bibi, Z., & ur Rehman, S. (2015). Validation of the eight-item center for epidemiologic studies depression scale (CES-D) among older adults. Current Psychology, 34(4), 681–692. [Google Scholar]
- Kaufman, J. E., Lee, Y., Vaughon, W., Unuigbe, A., & Gallo, W. T. (2018). Depression associated with transitions into and out of spousal caregiving. The International Journal of Aging and Human Development, 88(2), 127–149. doi: 10.1177/0091415018754310 [DOI] [PubMed] [Google Scholar]
- Kelley-Moore, J. A., & Ferraro, K. F. (2005). A 3-D model of health decline: Disease, disability, and depression among Black and White older adults. Journal of Health and Social Behavior, 46(4), 376–391. doi: 10.1177/002214650504600405 [DOI] [PubMed] [Google Scholar]
- King, B. M., Carr, D. C., & Taylor, M. G. (2020). Loneliness following widowhood: The role of the military and social support. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PubMed] [Google Scholar]
- Kohout, F. J., Berkman, L. F., Evans, D. A., & Cornoni-Huntley, J. (1993). Two shorter forms of the CES-D (center for epidemiological studies depression) depression symptoms index. Journal of Aging and Health, 5(2), 179–193. doi: 10.1177/089826439300500202 [DOI] [PubMed] [Google Scholar]
- Lindstrom, M. L., & Bates, D. M. (1990). Nonlinear mixed effects models for repeated measures data. Biometrics, 46(3), 673–687. doi: 10.2307/2532087 [DOI] [PubMed] [Google Scholar]
- Lohman, M., Dumenci, L., & Mezuk, B. (2016). Depression and frailty in late life: Evidence for a common vulnerability. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 71(4), 630–640. doi: 10.1093/geronb/gbu180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumey, L. H., Stein, A. D., & Susser, E. (2011). Prenatal famine and adult health. Annual Review of Public Health, 32, 237–262. doi: 10.1146/annurev-publhealth-031210-101230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews, K. A., & Gallo, L. C. (2011). Psychological perspectives on pathways linking socioeconomic status and physical health. Annual Review of Psychology, 62, 501–530. doi: 10.1146/annurev.psych.031809.130711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, A. H., & Raison, C. L. (2016). The role of inflammation in depression: From evolutionary imperative to modern treatment target. Nature Reviews. Immunology, 16(1), 22–34. doi: 10.1038/nri.2015.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, G. E., & Blackwell, E. (2006). Turning up the heat: Inflammation as a mechanism linking chronic stress, depression, and heart disease. Current Directions in Psychological Science, 15(6), 269–272. doi: 10.1111/j.1467-8721.2006.00450.x [DOI] [Google Scholar]
- Miller, G. E., Chen, E., & Parker, K. J. (2011). Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin, 137(6), 959–997. doi: 10.1037/a0024768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt, T. E., & Caspi, A. (2019). Psychiatry’s opportunity to prevent the rising burden of age-related disease. JAMA Psychiatry, 76(5), 461–462. doi: 10.1001/jamapsychiatry.2019.0037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai, R. (2017). Universal depression screening to improve depression outcomes in primary care: Sounds good, but where is the evidence? Psychiatric Services (Washington, D.C.), 68(7), 724–726. doi: 10.1176/appi.ps.201600320 [DOI] [PubMed] [Google Scholar]
- Parkes, C. M. (1964). Recent bereavement as a cause of mental illness. The British Journal of Psychiatry, 110, 198–204. doi: 10.1192/bjp.110.465.198 [DOI] [PubMed] [Google Scholar]
- Penninx, B. W. J. H., Deeg, D. J. H., van Eijk, J. T. H. M., Beekman, A. T. F., & Guralnik, J. M. (2000). Changes in depression and physical decline in older adults: A longitudinal perspective. Journal of Affective Disorders, 61(1–2), 1–12. doi: 10.1016/S0165-0327(00)00152-X [DOI] [PubMed] [Google Scholar]
- Prior, A., Fenger-Grøn, M., Davydow, D. S., Olsen, J., Li, J., Guldin, M. B., & Vestergaard, M. (2018). Bereavement, multimorbidity and mortality: A population-based study using bereavement as an indicator of mental stress. Psychological Medicine, 48(9), 1437–1443. doi: 10.1017/S0033291717002380 [DOI] [PubMed] [Google Scholar]
- Radloff, L. S. (1977). The CES-D scale. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Sasson, I., & Umberson, D. J. (2014). Widowhood and depression: New light on gender differences, selection, and psychological adjustment. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69(1), 135–145. doi: 10.1093/geronb/gbt058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah, S. M., Carey, I. M., Harris, T., Dewilde, S., Victor, C. R., & Cook, D. G. (2013). The effect of unexpected bereavement on mortality in older couples. American Journal of Public Health, 103(6), 1140–1145. doi: 10.2105/AJPH.2012.301050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrira, A., Palgi, Y., Bodner, E., & Shmotkin, D. (2016). Which category of lifetime adversity accelerates physical impairment among Israeli older adults? European Journal of Ageing, 13(4), 323–334. doi: 10.1007/s10433-016-0366-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siu, A. L., Bibbins-Domingo, K., Grossman, D. C., Baumann, L. C., Davidson, K. W., Ebell, M., . . . the US Preventive Services Task Force (USPSTF). (2016). Screening for depression in adults: US preventive services task force recommendation statement. JAMA, 315(4), 380. doi: 10.1001/jama.2015.18392 [DOI] [PubMed] [Google Scholar]
- Smith, R., & Meeks, S. (2019). Screening older adults for depression: Barriers across clinical discipline training. Innovation in Aging, 3(2), igz011. doi: 10.1093/geroni/igz011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahl, S. T., Arnold, A. M., Chen, J. Y., Anderson, S., & Schulz, R. (2016). Mortality after bereavement: The role of cardiovascular disease and depression. Psychosomatic Medicine, 78(6), 697–703. doi: 10.1097/PSY.0000000000000317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffick, D. (2000). Documentation of affective functioning measures in the health and retirement study. Retrieved from https://hrs.isr.umich.edu/publications/biblio/5411
- Taylor, D. H.Jr, Kuchibhatla, M., Ostbye, T., Plassman, B. L., & Clipp, E. C. (2008). The effect of spousal caregiving and bereavement on depressive symptoms. Aging & Mental Health, 12(1), 100–107. doi: 10.1080/13607860801936631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vable, A. M., Subramanian, S. V., Rist, P. M., & Glymour, M. M. (2015). Does the “widowhood effect” precede spousal bereavement? Results from a nationally representative sample of older adults. The American Journal of Geriatric Psychiatry, 23(3), 283–292. doi: 10.1016/j.jagp.2014.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zisook, S., Paulus, M., Shuchter, S. R., & Judd, L. L. (1997). The many faces of depression following spousal bereavement. Journal of Affective Disorders, 45(1–2), 85–95. doi: 10.1016/S0165-0327(97)00062-1 [DOI] [PubMed] [Google Scholar]
- Zisook, S., & Shuchter, S. R. (1991). Depression through the first year after the death of a spouse. The American Journal of Psychiatry, 148(10), 1346–1352. doi: 10.1176/ajp.148.10.1346 [DOI] [PubMed] [Google Scholar]
- Zisook, S., & Shuchter, S. R. (1993). Major depression associated with widowhood. The American Journal of Geriatric Psychiatry, 1(4), 316–326. doi: 10.1097/00019442-199300140-00006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.