Abstract
Background:
Efforts to reduce socioeconomic inequities in cardiovascular disease include interventions to change the built environment. We aimed to explore whether socioeconomic inequities in coronary heart disease (CHD) incidence are ameliorated or exacerbated in environments supportive of physical activity (PA).
Methods:
We used data from the REGARDS study, which recruited US-residents aged 45 or older between 2003 and 2007. Our analyses included participants at risk for incident CHD (n=20,808), followed until December 31st 2014. We categorized household income and treated it as ordinal: (1) $75,000+, (2) $35,000-$74,000, (3) $20,000-$34,000, and (4) <$20,000. We operationalized PA-supportive environments using characteristics within a 1-km residential buffer: walkable destinations density, physical activity facility density, and proportion green land cover. We used Cox proportional hazards models to estimate the adjusted association of income with incident CHD, and tested effect modification by PA-supportive environment variables.
Results:
We found a 25% (95% CI: 1.17 to 1.34) increased hazard of CHD per 1-category decrease in household income category. Adjusting for PA-supportive environments slightly reduced this association (HR=1.23). The income-CHD association was strongest in areas without walking destinations (HR=1.57), an interaction which reached statistical significance in analyses among men. In contrast, the income-CHD association showed a trend toward being strongest in areas with the highest percentage of green land cover.
Conclusions:
Indicators of a physical activity supportive environment show divergent trends to modify socioeconomic inequities in CHD . Built environment interventions should measure the effect on socioeconomic inequities.
Keywords: Neighborhood/place, socio-economic, Cardiovascular Disease
INTRODUCTION
Cardiovascular diseases (CVD) are a leading cause of death among developing and developed nations [1]. In the US, CVD accounted for 840,678 deaths in 2016, approximately 1 of every 3 deaths [2], and 121.5 million American adults had some form of CVD between 2013 and 2016 [2]. Yet, the distribution of CVD burdens within the US population highlights persistent inequities.
Socioeconomic position has been associated with CVD incidence and mortality, whether operationalized based on education [3], income [4], or social class [5]. In the Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort study, participants with low income and low education have a 42% higher risk of incident coronary heart disease (CHD) (95% CI: 1.14–1.76) than those with high income and high education [3]. There are several pathways through which socioeconomic inequities in health could emerge and be maintained [6], including through barriers to residing in neighborhoods with health-supportive built environments [7]. Indeed, studies have assessed whether and how built environments can prevent CVD [8], including through support of physical activity [9]. However, exposure to built environment characteristics do not necessarily follow a pattern suggestive of deprivation amplification [10]. People from lower socioeconomic positions live in neighborhoods may disproportionately lack high quality green spaces to use as settings for physical activity [11], yet tend to live in neighborhoods with greater walkability (an “advantage in disadvantage” [12,13]).
Complementary to the possibility that built environments represent a pathway connecting socioeconomic disadvantage to cardiovascular risk is the less commonly explored possibility that socioeconomic inequities are themselves modified by neighborhood conditions [14–18]. Individual-level longitudinal studies in particular have potential to complement the existing evidence by allowing for measurement of socioeconomic characteristics and neighborhood conditions prior to cardiovascular disease onset.
This study uses data from the REGARDS study to investigate differences in the magnitude of socioeconomic inequities in incident coronary heart disease (CHD) across neighborhood built environments that differ in indicators of support for physical activity. We hypothetize that the association between socioeconomic position and CHD will be ameliorated in environments more supportive of physical activity.
METHODS
Study population
The REGARDS cohort is a US-national, population-based study of 30,239 community-dwelling participants aged 45 or older who self-identified as non-Hispanic Black or white. Recruitment between 2003 and 2007 was designed to oversample participants from the southeastern US-Stroke Belt (North Carolina, South Carolina, Georgia, Alabama, Mississippi, Tennessee, Arkansas, and Louisiana)[19] and non-Hispanic Blacks; the study design and objectives are described elsewhere [20]. At enrollment, participants completed detailed surveys and clinical measures, collected via phone and in-home visits performed by trained technicians [20]. Standardized follow-up telephone contacts were conducted every 6 months to detect change of home residence, hospitalizations, and deaths. The study team additionally queries the National Death Index annually to assess whether any participants have died.
This study was restricted to those free of CHD at baseline and those with complete data for socioeconomic and neighborhood characteristics. We excluded participants with self-report of myocardial infarction or coronary revascularization procedure at baseline or evidence of prior myocardial infarction on the baseline electrocardiogram (N=5314). We also excluded those with no information on baseline household income (N=3730) or neighborhood built environment (occurring because we were not able to geocode a home address within the 48 contiguous United States and characterize the surrounding enviornment (N=884).
The final sample size for complete case analyses was 20,808 participants. As sensitivity analysis, we used multiple imputations by chained equations with 10 datasets to assess robustness of our findings to missing at random data on income [21,22].
The REGARDS study protocol was reviewed and approved by the University of Alabama at Birmingham Institutional Review Board and all participating institutional review boards; all participants provided written informed consent.
Outcome variable: incident coronary heart disease
The outcome for this analysis was adjudicated incident CHD defined as myocardial infarction (MI) or acute CHD death. During the biannual follow-up contacts, any report of a heart-disease related event (including emergency department visit or hospitalization) or participant death prompted retrieval of medical records. For fatal events, medical history, hospital records, interviews with next of kin or proxies, and death certificate or National Death Index data were reviewed to adjudicate the cause of death, with definite or probable CHD death used in the analysis [23].
Cases were assigned to 2 adjudicators and disagreements were resolved by a committee, following published guidelines by the American Heart Association [23,24]. Briefly, MI was determined by: (1) considering clinical signs and symptoms suggestive of ischemia; (2) ECG findings consistent with ischemia or MI, guided by the Minnesota code and classified as evolving diagnostic, positive, nonspecific, or not consistent [25]; and (3) a rising and/or falling pattern in cardiac troponin level or creatine phosphokinase MB level over 6 or more hours, with a peak level greater than twice the upper limit of normal (diagnostic cardiac enzymes). Definite MI was defined based on diagnostic cardiac enzymes or ECG. Adjudication of an MI as probable relied on elevated but not diagnostic (i.e., equivocal) enzymes; a positive but not diagnostic electrocardiogram; or, if enzymes were missing, a positive ECG in the presence of ischemic signs or symptoms. Agreement between adjudicators for the outcomes included in this study (definite or probable MI or definite or probable acute CHD death) yielded a κ greater than 0.80.
Exposure variable: socioeconomic position
The primary measure of socioeconomic position was household income at baseline. We divided participants in 4 categories: (1) $75,000 and above, (2) $35,000-$74,000, (3) $20,000-$34,000, and (4) less than $20,000. For sensitivity analysis, we used a dichotomous socioecomic position variable combining household income and education previously used for analyses of CHD in REGARDS [3,26], with low socioeconomic position defined as either low annual household income (<$35,000) or low education (less than high school).
Physical activity supportive environments
We used three previously studied indicators of environmental support for physical activity: density of walking destinations [27], density of physical activity facilities [28], and proportion green land cover [29]. These characteristics were estimated for a 1-km buffer surrounging each participant’s geocoded home address at baseline and in each year of follow-up. Environment variables were constructed as time-varying to incorporate address updates during follow-up and changes captured in longitudinal geographic data.
Measures of walking destinations and physical activity facilities were created using the National Establishment Time-Series (NETS) [30,31] data. Commercially-licensed NETS provided annual establishment-level data for each January from 1990 to 2014 for US businesses and many nonprofit and government establishments. Walking destinations and physical activity facilities were classified informed by previous studies [32,33], with further details on data cleaning and categorization provided elsewhere [31]. Walking destinations were defined to include both potential destinations for daily living and those judged as amenities adding to pedestrian interest and overall walkability. Physical activity facilities included a variety of venues for physical activity or fitness, such as indoor gyms, that have been previously associated with both gym membership and objective physical activity [28]. Measures of green land cover are derived from the National Land Cover Dataset (NLCD). NLCD describes the visible features that cover the Earth’s surface, using land cover data derived from satellite imagery or aerial photography. We created measures of green land cover per km2 by summing across vegetation-related categories (41–95).
Covariates
We included demographics including age, sex and race (Black or white) as well as geographic variables including region of residence (Stroke Belt, Stroke Buckle, or other) and urbanicity (categorized as urban, large rural, small rural, or isolated small rural tract using Rural and Urban Commuting Areas categories).
Analysis
Descriptive analysis used baseline individual-level and neighborhood variables. We used Cox proportional hazards regression models to examine the association of income category with incident CHD. Observation started at REGARDS baseline, and events through December 31, 2014, were included in the analysis. Individuals were censored at the time of their event, death, or the end of the follow-up. An ordinal grouped linear income variable was used, coded such that HRs above one indicate that a lower income group is associated with an increased hazard of CHD.
Initial models (Model 1) were adjusted for sociodemographics and geographical covariates. After this, we adjusted for the three physical activity environment variables (Model 2). We calculated the proportional change in HR estimates with additional adjustment for physical activity environment using the following formula [34,35]:
To test effect modification, we introduced an interaction term between income (treated ordinally) and categorical versions of each physical activity environment exposures (walking destinations, physical activity facilities, green land cover). For each environment characteristic, we grouped participants into 5 categories. Because of a large number of zeros, the first category (lowest level) included those with no destinations (either walking destinations, physical activity facilities or green land cover) within their 1-km buffer, and among the participants with >0 categories were defined using quartiles.
To formally test the global statistical significance of each income-environment interaction, we compared a model with and without the interaction terms using a likelihood ratio test. Results are presented overall, stratified by sex and race, and for sensitivity analyses with a combined measure of education and income as the exposure or including imputed data on household income. Analyses were conducted in R version 3.6.3.
RESULTS
Table 1 shows the main descriptive analyses. Participants with lower reported income were older, were disproportionately female and Black, and had a greater number of walking destinations in the 1-km buffer surrounding their baseline home address. Higher-income participants were more likely to live in urban areas, report higher education, have better self-reported health, and have a greater percentage of green land cover in their 1-km buffer.
Table 1.
Descriptive characteristics of included REGARDS participants by income category
| Total | Income less than $35,000 | Income $35,000 and above |
|---|---|---|
| (N=20,808) | (N=9,721) | (N=11,087) |
| 57.1% | 66.5% | 48.8% |
| 42.6% | 54.3% | 32.4% |
| 63 (13) | 66 (14) | 61 (12) |
| 10.8% | 20.2% | 2.6% |
| 25.1% | 34.4% | 16.8% |
| 27.3% | 27.6% | 26.9% |
| 36.9% | 17.8% | 53.7% |
| 34.6% | 37.4% | 32.1% |
| 20.6% | 20.2% | 20.9% |
| 44.8% | 42.4% | 46.9% |
| 2.2% | 2.3% | 2.2% |
| 5.7% | 6.1% | 5.3% |
| 11.0% | 11.9% | 10.3% |
| 81.0% | 79.7% | 82.2% |
| 17.9% | 12.1% | 23.1% |
| 32.5% | 26.0% | 38.2% |
| 34.1% | 38.6% | 30.2% |
| 12.9% | 19.2% | 7.4% |
| 2.5% | 4.0% | 1.1% |
| 44 (85) | 53 (90) | 35 (78) |
| 1 (2) | 1 (2) | 1 (2) |
| 0.59 (1.51) | 0.44 (1.40) | 0.72 (1.55) |
Values show median (IQR) or %
12 participants had missing data on education
1859 participatns had missing data on urbanicity
28 participants had missing data on self-reported health
Table 2 shows the results of the Cox regression models on the relationship between household income and CHD before (Model 1) and after adjustment by physical activity environment (Model 2). There was a strong association between household income and the risk of CHD, with residents of low income being more likely to experience incident CHD. Each 1-category decrease in household income was associated with a 25% increased hazard of CHD (HR: 1.25; 95% CI: 1.17 to 1.34%). In stratified analyses, the income-CHD association was strongest among women (HR=1.31) and among Blacks (HR=1.30), though confidence intervals for all stratified analyses overlapped.
Table 2.
Association between household income and incident coronary heart disease, overall and stratified by sex or race
| Model 1a | Model 2b | % attenuationc | |
|---|---|---|---|
| HR (95% CI) | HR (95% CI) | ||
| Overall (N=20,808) | |||
| Decrease in income category | 1.25 (1.17 – 1.34) | 1.24 (1.15 – 1.33) | 4.8% |
| Female (N=11,871) | |||
| Decrease in income category | 1.31 (1.18 – 1.47) | 1.30 (1.17 – 1.46) | 2.8% |
| Male (N=8,937) | |||
| Decrease in income category | 1.21 (1.11 – 1.33) | 1.20 (1.09 – 1.31) | 7.0% |
| Black (N=8,872) | |||
| Decrease in income category | 1.30 (1.17 – 1.45) | 1.29 (1.16 – 1.44) | 3.5% |
| White (N=11,936) | |||
| Decrease in income category | 1.21 (1.10 – 1.33) | 1.19 (1.09 – 1.31) | 8.5% |
Values shown are hazard ratios (HRs) and 95% confidence intervals (95% CI) for adjusted Cox models with income entered as a grouped linear variable (1=$75,000+, 2=$35,000-$74,000, 3=$20,000-$34,000, and 4=<$20,000), such that HRs above 1 indicate higher risk in lower income groups
Model 1: Adjusted for sociodemographic (age, sex and race) and geographic covariates (region of residence and urbanicity)
Model 2: Adjusted for sociodemographic and geographic ovariates in Model 1 plus adjust for indicators of a physical activity supportive environment: walking destinations, physical activity facilities, and green land cover
proportional attenuation in the hazard ratio following adjustment for indicators of a physical activity supportive environment (HRModel 1-HR Model 2)⁄(HR Model 1-1)*100 %
After adjustment for physical activity environment variables (Model 2), the association between income and CHD was shifted toward the null, but in all cases remained statistically significant. Overall, there was a 4.8% reduction in the HR after adjusting by physical activity environment variables, and none of the sex or race strate showed attenuation with adjustment by more than 8.5%.
Figure 1 shows patterns in how the strength of the relationship between income and CHD varies across categories of each indicator of a physical activity supportive environment. The left panel shows the interaction by walking destinations; the association between income and CHD was highest in areas with no walking destinations (HR=1.57) but did not show a clear trend across increasing quartiles of walking destination density (Q1=1.18, Q2=1.16, Q3=1.39, Q4=1.20). This statistical interaction reached significance only among males (interaction p value: 0.02). We did not find a statistically significant variation of the association between income and CHD within physical activity facilities groups (middle panel), though among males there was a trend suggestive of a stronger income-CHD association in contexts without physical activity facilities (interaction p value: 0.15). For green land cover (right panel), the association between income and CHD was stronger in areas in the highest quartile of green land cover, although the trend was not significant (interaction p value: 0.189). Among Blacks, there was a gradient suggestive of dose-response, such that areas with incrementally higher green land cover had stronger associations between income and CHD. On the other hand, both areas with the lowest and highest green land cover a relatively strong income-CHD association (interaction p value: 0.07).
Figure 1.
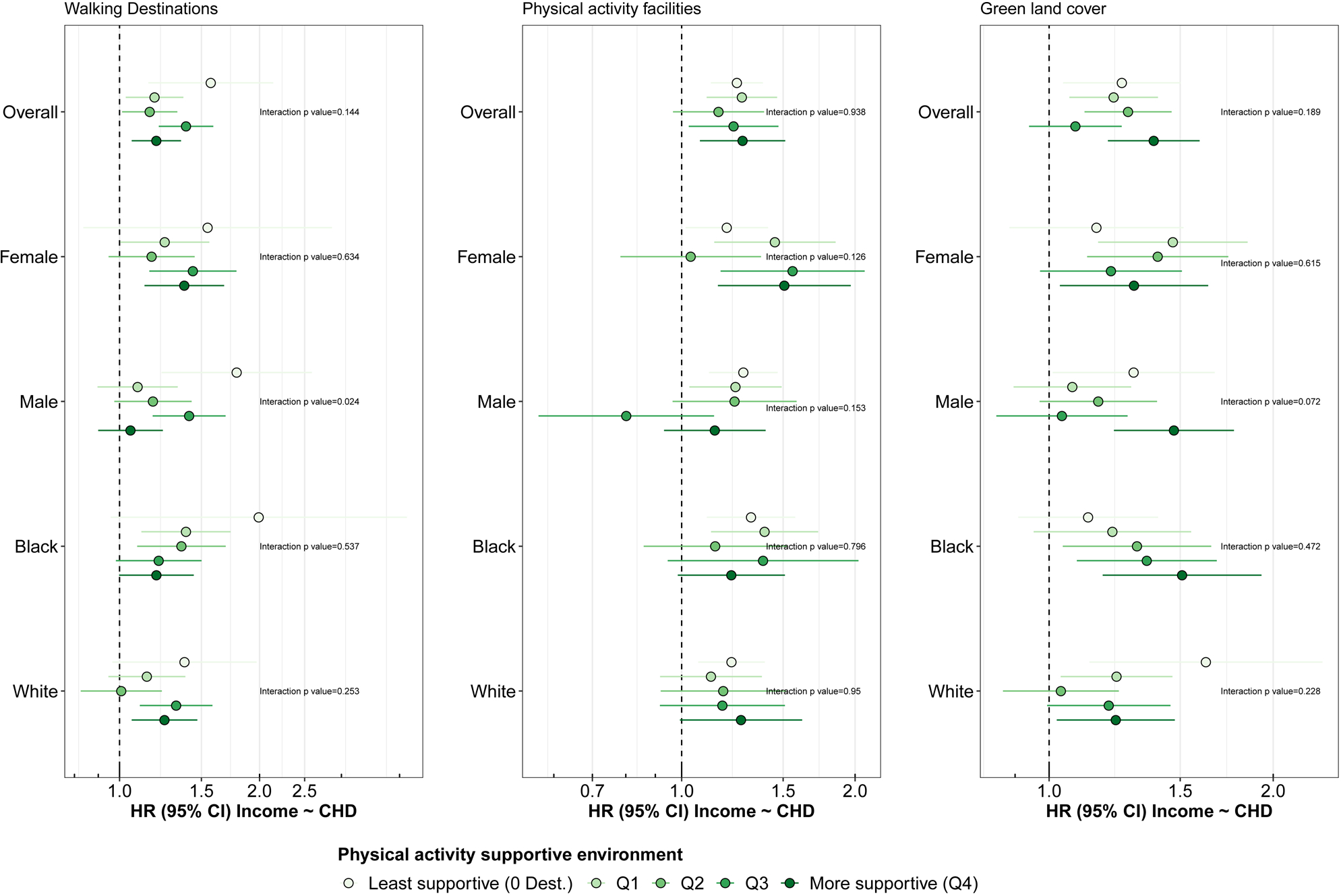
Effect modification by physical activity supportive environment for the association between income and coronary heart disease, considering and stratification by sex and race
Sensitivity analyses using a combination of education and income gave similar results in both adjusted (Supplementary file 1) and interaction models (Supplementary file 2). Sensitivity analyses using multiple imputations show no changes to our main inferences (Supplementary files 3 and 4).
DISCUSSION
In this study, residents reporting lower household income had a greater incidence of CHD compared to those with higher household income. We explored the contribution of the physical activity environment to these socioeconomic inequities. Adjustment for indicators of a physical activity supportive environment (walking destinations, physical activity facilities, and green land cover) led to a small reduction in the effect of socioeconomic position. Analyses investigating potential effect modification of the income-CHD association by physical activity supportive environment (and for combined socioeconomic status-CHD association in a sensitivity analysis) noted persistence of the association across strata. Trends in the magnitude of the association suggested that socioeconomic inequities in CHD were most pronounced in areas with no walking destinations or with the greatest green land cover, providing mixed support for our hypotheses.
Both socioeconomic position and physical activity environment features (such as walking destinations, physical activity facilities, and green land cover) have been associated previously with risk of CHD [3,9,36]. From an environmental justice perspective, previous studies have shown an unequal distribution of physical activity environment features within cities [11]. Thus, targeted investments to increase support for physical activity in the built environment might mitigate the CHD inequities. However, adjusting for selected indicators of a built environment supportive of physical activity did not appreciably reduced the relationship between socioeconomic position and CHD in our analyses. Previous research has studied how physical activity environment can mitigate inequities in physical activity [37,38], while other have looked at whether other neighborhood factors (such as violence and or neighborhood disorder) mediate the association between SES and CHD risk factors [14,16–18]. For instance, Turrel et al [37] found that, in Brisbane (Australia), there was a partial mediation by walkability features (residential density, street connectivity and land use mix) for the association between neighbourhood disadvantage and walking for transport. Pascual and collegues [38] studied physical activity facilities as potentially mediating the association between income and physical inactivity in Madrid (Spain).
In this present study, we were able to juxtapose patterns of effect modification across three indicators of an environment supportive of physical activity. Overall, socioeconomic inequities in CHD were noted across all strata, though a pattern of effect modification provided mixed support for our hypothesis; we found that socioeconomic inequities in CHD were greater in areas with no walking destinations and in areas with greater green land cover. One explanation is that walking destinations might act as an “advantage in the disadvantage” [12], where low-SES areas have greater availability of walking destinations [13]. Another possibility is that destination density and green land cover diverge in their implications for perceived safety, and CHD inequities are themselves exacerbated by safety concerns. In particular, areas with greater walking destinations might attract more pedestrian activity and be perceived as safer (following Jane Jacobs concept of “eyes on the street” [39]) while areas with greater green land cover might be perceived as less safe for physical activity [40].
Our work should be interpreted keeping in mind that that SES inequities in leisure-time physical activity in PA facilities and green spaces tend to be higher than those in transport-related physical activity (related with walkability) [41]. Previous studies have shown an interaction between SES and aspects of the built environment, such as walkability, and the risk of different health conditions and behaviors, especially physical activity [42]. Following this, Adkins et al suggest that unprivileged populations respond differently to built environment features due to safety, time to do physical activity, or working conditions, among others [43].
This study has several strengths. First, we were able to do a longitudinal study of 20,808 individuals from a national US sample, taking into account time-varying exposures to the physical activity environment. Second, we were able to use objective measures for both physical activity environment variables and CHD outcomes, avoiding the possibility of same source bias [44]. Third, we used multiple types of physical activity resources which map onto different types of physical activity that impact CHD. Lastly, we were able to use both adjusted and effect modification analyses to get a better sense of the role of the physical activity environment in CHD’s socioeconomic inequities.
We acknowledge that this study has several limitations. Household income was measured by self-report and entered as ordinal categories which may be subject to measurement error or bias; there were also missing income data, though results were similar in sensitivity analyses imputing instead of excluding all missing income values. Our indicators of physical activity supportive environment included heterogeneous walkable destinations (which represent only one component of walkability [45]), physical activity facilities which might require fees to enter, and green land cover that differs in accessibility and vegetation type. Despite the point-level annual resolution of the National Establishment Time-Series (NETS) source for walking destinations and physical activity facilities [30], misclassification is possible and validity checks to refine our categorization were limited to the most recent year (2014). Additionally, the focus on built environment measures within 1-km buffers around home addresses might not reflect where people participate in physical activity (including activity spaces around work, around children’s schools, or in areas accessed by vehicle). The REGARDS study ascertainment of CHD events requires notification by participants or via linkage to the NDI, so despite careful adjudication, there might be under-reporting of the CHD outcome or CHD events that have been erroneously included a probable. Finally, the impact of the built environment on CHD and CHD inequities may be small, creating challenges as we attempt to disentangle true causal effects from bias, including bias emerging from uncontrolled confounding. In the US context, race-based segregation and historic patterns of income inequities likely contribute to residual confounding by experiences of structural discrimination that connect place and race.
Conclusions
We found that REGARDS participants with lower socioeconomic position had a higher incidence of CHD. These inequities were relatively wide in areas with no walking destinations. In contrast, the income-CHD association showed a trend toward being strongest in areas with the highest percentage of green land cover. Indicators of a physical activity supportive environment show divergent trends to modify an income-CHD association, and future evaluation efforts should monitor the implications of built environment change for the magnitude of health inequities.
Supplementary Material
What is already known on this subject?
Previous studies have demonstrated that individuals of low socioeconomic position have more risk of developing cardiovascular disease. However, there is scarce information about how the built environment can ameliorate or exacerbate socioeconomic inequities in cardiovascular disease.
What this study adds?
Low-socioeconomic position individuals have greater risk of developing coronary heart disease and the built environment may modify this association. Socioeconomic inequities in coronary heart disease were noted to be larger in areas with no walking destinations.
Funding
The REGARDS research project is supported by cooperative agreement U01 NS041588 co-funded by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA), National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS or the NIA. Representatives of the NINDS were involved in the review of the manuscript but were not directly involved in the collection, management, analysis or interpretation of the data. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at: https://www.uab.edu/soph/regardsstudy/.
Additionally, the integration and analyses of geographic data were supported by the National Institute of Aging (grants 1R01AG049970, 3R01AG049970-04S1), Commonwealth Universal Research Enhancement (C.U.R.E) program funded by the Pennsylvania Department of Health - 2015 Formula award - SAP #4100072543, the Urban Health Collaborative at Drexel University, and the Built Environment and Health Research Group at Columbia University. PG was supported by Fundación Alfosno Martín Escudero 2018 Post-doctoral fellowship program. UB was supported by the Office of the Director of the National Institutes of Health under award number DP5OD26429.
Footnotes
Competing Interest
None declared.
REFERENCES
- 1.Beaglehole R, Bonita R. Global public health: a scorecard. Lancet 2008;372:1988–96. doi: 10.1016/S0140-6736(08)61558-5 [DOI] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation 2019;139:e209. doi: 10.1161/CIR.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 3.Lewis MW, Khodneva Y, Redmond N, et al. The impact of the combination of income and education on the incidence of coronary heart disease in the prospective Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort study Chronic Disease Epidemiology. BMC Public Health 2015;15:1–10. doi: 10.1186/s12889-015-2630-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mosquera PA, San Sebastian M, Waenerlund AK, et al. Income-related inequalities in cardiovascular disease from mid-life to old age in a Northern Swedish cohort: A decomposition analysis. Soc Sci Med 2016;149:135–44. doi: 10.1016/j.socscimed.2015.12.017 [DOI] [PubMed] [Google Scholar]
- 5.McFadden E, Luben R, Wareham N, et al. Occupational social class, risk factors and cardiovascular disease incidence in men and women: A prospective study in the European Prospective Investigation of Cancer and Nutrition in Norfolk (EPIC-Norfolk) cohort. Eur J Epidemiol 2008;23:449–58. doi: 10.1007/s10654-008-9262-2 [DOI] [PubMed] [Google Scholar]
- 6.Krieger N A glossary for social epidemiology. J Epidemiol Community Heal 2001;55:693–700. doi: 10.1136/jech.55.10.693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diez Roux AV Residential environments and cardiovascular risk. J Urban Health 2003;80:569–89. doi: 10.1093/jurban/jtg065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sallis JF, Floyd MF, Rodríguez DA, et al. Role of Built Environments in Physical Activity, Obesity, and Cardiovascular Disease. Circulation 2012;125:729–37. doi: 10.1161/circulationaha.110.969022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malambo P, Kengne AP, De Villiers A, et al. Built environment, selected risk factors and major cardiovascular disease outcomes: A systematic review. PLoS One 2016;11:1–13. doi: 10.1371/journal.pone.0166846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Macintyre S Deprivation amplification revisited; or, is it always true that poorer places have poorer access to resources for healthy diets and physical activity? Int J Behav Nutr Phys Act 2007;4:32. doi: 10.1186/1479-5868-4-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jacobs J, Alston L, Needham C, et al. Variation in the physical activity environment according to area-level socio-economic position-A systematic review. Obes Rev 2019;:1–15. doi: 10.1111/obr.12818 [DOI] [PubMed] [Google Scholar]
- 12.King KE, Clarke PJ. A disadvantaged advantage in walkability: Findings from socioeconomic and geographical analysis of national built environment data in the United States. Am J Epidemiol 2015;181:17–25. doi: 10.1093/aje/kwu310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gullón P, Bilal U, Cebrecos A, et al. Intersection of neighborhood dynamics and socioeconomic status in small-area walkability: the Heart Healthy Hoods project. Int J Health Geogr 2017;16:21. doi: 10.1186/s12942-017-0095-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morenoff JD, House JS, Hansen BB, et al. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: The role of neighborhood context. Soc Sci Med 2007;65:1853–66. doi: 10.1016/j.socscimed.2007.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hussein M, Diez Roux AV, Mujahid MS, et al. Unequal Exposure or Unequal Vulnerability? Contributions of Neighborhood Conditions and Cardiovascular Risk Factors to Socioeconomic Inequality in Incident Cardiovascular Disease in the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol 2018;187:1424–37. doi: 10.1093/aje/kwx363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mujahid MS, Roux AVD, Cooper RC, et al. Neighborhood Stressors and Race/Ethnic Differences in Hypertension Prevalence (The Multi-Ethnic Study of Atherosclerosis). Am J Hypertens 2011;24:187–93. doi: 10.1038/ajh.2010.200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.King KE, Morenoff JD, House JS. Neighborhood Context and Social Disparities in Cumulative Biological Risk Factors. Psychosom Med 2011;73:572–9. doi: 10.1097/PSY.0b013e318227b062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schulz AJ, Mentz G, Lachance L, et al. Do observed or perceived characteristics of the neighborhood environment mediate associations between neighborhood poverty and cumulative biological risk? Heal Place 2013;24:147–56. doi: 10.1016/j.healthplace.2013.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lanska DJ, Kuller LH. The Geography of Stroke Mortality in the United States and the Concept of a Stroke Belt. Stroke 1995;26:1145–9. doi: 10.1161/01.STR.26.7.1145 [DOI] [PubMed] [Google Scholar]
- 20.Howard VJ, Gomez CR, Go RC, et al. The Reasons for Geographic and Racial Differences in Stroke Study: Objectives and Design. Neuroepidemiology 2005;25:135–43. doi: 10.1159/000086678 [DOI] [PubMed] [Google Scholar]
- 21.Rubin DB, Schenker N. Multiple imputation in health-care databases: an overview and some applications. Stat Med 1991;10:585–98. doi: 10.1002/sim.4780100410 [DOI] [PubMed] [Google Scholar]
- 22.Burns RA, Butterworth P, Kiely KM, et al. Multiple imputation was an efficient method for harmonizing the Mini-Mental State Examination with missing item-level data. J Clin Epidemiol 2011;64:787–93. doi: 10.1016/j.jclinepi.2010.10.011 [DOI] [PubMed] [Google Scholar]
- 23.Luepker RV, Apple FS, Christenson RH, et al. Case Definitions for Acute Coronary Heart Disease in Epidemiology and Clinical Research Studies: A Statement from the AHA Council on Epidemiology and Prevention. Circulation 2003;108:2543–9. doi: 10.1161/01.CIR.0000100560.46946.EA [DOI] [PubMed] [Google Scholar]
- 24.Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation 2018;138:1–34. doi: 10.1161/CIR.0000000000000617 [DOI] [PubMed] [Google Scholar]
- 25.Prineas RJ, Crow RS, Zhang Z-M. The Minnesota Code Manual of Electrocardiographic Findings. London: : Springer London; 2010. doi: 10.1007/978-1-84882-778-3 [DOI] [Google Scholar]
- 26.Redmond N, Richman J, Gamboa CM, et al. Perceived stress is associated with incident coronary heart disease and all-cause mortality in low- but not high-income participants in the Reasons for Geographic And Racial Differences in Stroke study. J Am Heart Assoc 2013;2:e000447. doi: 10.1161/JAHA.113.000447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hirsch JA, Moore KA, Clarke PJ, et al. Changes in the built environment and changes in the amount of walking over time: Longitudinal results from the Multi-Ethnic study of Atherosclerosis. Am J Epidemiol 2014;180:799–809. doi: 10.1093/aje/kwu218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaufman TK, Rundle A, Neckerman KM, et al. Neighborhood Recreation Facilities and Facility Membership Are Jointly Associated with Objectively Measured Physical Activity. J Urban Heal 2019;96:570–82. doi: 10.1007/s11524-019-00357-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Villeneuve PJ, Jerrett M, Su JG, et al. Association of residential greenness with obesity and physical activity in a US cohort of women. Environ Res 2018;160:372–84. doi: 10.1016/j.envres.2017.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaufman TK, Sheehan DM, Rundle A, et al. Measuring health-relevant businesses over 21 years: Refining the National Establishment Time-Series (NETS), a dynamic longitudinal data set. BMC Res Notes 2015;8:1–13. doi: 10.1186/s13104-015-1482-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hirsch JA, Moore KA, Cahill J, et al. Business Data Categorization and Refinement for Application in Longitudinal Neighborhood Health Research: a Methodology. J Urban Heal Published Online First: 1 October 2020. doi: 10.1007/s11524-020-00482-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hirsch JA, Grengs J, Schulz A, et al. How much are built environments changing, and where?: Patterns of change by neighborhood sociodemographic characteristics across seven U.S. metropolitan areas. Soc Sci Med 2016;169:97–105. doi: 10.1016/j.socscimed.2016.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rundle AG, Chen Y, Quinn JW, et al. Development of a Neighborhood Walkability Index for Studying Neighborhood Physical Activity Contexts in Communities across the U.S. over the Past Three Decades. J Urban Heal 2019;96:583–90. doi: 10.1007/s11524-019-00370-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173–82. doi: 10.1037/0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- 35.Droomers M, Schrijvers CT, Stronks K, et al. Educational differences in excessive alcohol consumption: the role of psychosocial and material stressors. Prev Med (Baltim) 1999;29:1–10. doi: 10.1006/pmed.1999.0496 [DOI] [PubMed] [Google Scholar]
- 36.Manrique-Garcia E, Sidorchuk A, Hallqvist J, et al. Socioeconomic position and incidence of acute myocardial infarction: A meta-analysis. J Epidemiol Community Health 2011;65:301–9. doi: 10.1136/jech.2009.104075 [DOI] [PubMed] [Google Scholar]
- 37.Turrell G, Haynes M, Wilson LA, et al. Can the built environment reduce health inequalities? A study of neighbourhood socioeconomic disadvantage and walking for transport. Heal Place 2013;19:89–98. doi: 10.1016/j.healthplace.2012.10.008 [DOI] [PubMed] [Google Scholar]
- 38.Pascual C, Regidor E, Alvarez-Del Arco D, et al. Sports facilities in Madrid explain the relationship between neighbourhood economic context and physical inactivity in older people, but not in younger adults: a case study. J Epidemiol Community Health 2013;67:788–94. doi: 10.1136/jech-2013-202583 [DOI] [PubMed] [Google Scholar]
- 39.Brown SC, Mason CA, Lombard JL, et al. The Relationship of Built Environment to Perceived Social Support and Psychological Distress in Hispanic Elders: The Role of ‘Eyes on the Street’. Journals Gerontol Ser B Psychol Sci Soc Sci 2009;64B:234–46. doi: 10.1093/geronb/gbn011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ali O, Di Nardo F, Harrison A, et al. The link between perceived characteristics of neighbourhood green spaces and adults’ physical activity in UK cities: analysis of the EURO-URHIS 2 Study. Eur J Public Health 2017;27:761–5. doi: 10.1093/eurpub/ckx033 [DOI] [PubMed] [Google Scholar]
- 41.Scholes S, Bann D. Education-related disparities in reported physical activity during leisure-time, active transportation, and work among US adults: repeated cross-sectional analysis from the National Health and Nutrition Examination Surveys, 2007 to 2016. BMC Public Health 2018;18:926. doi: 10.1186/s12889-018-5857-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schüle SA, Bolte G. Interactive and Independent Associations between the Socioeconomic and Objective Built Environment on the Neighbourhood Level and Individual Health: A Systematic Review of Multilevel Studies. PLoS One 2015;10:e0123456. doi: 10.1371/journal.pone.0123456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Adkins A, Makarewicz C, Scanze M, et al. Contextualizing Walkability: Do Relationships Between Built Environments and Walking Vary by Socioeconomic Context? J Am Plan Assoc 2017;83:296–314. doi: 10.1080/01944363.2017.1322527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gullón P, Bilal U, Franco M. Physical activity environment measurement and same source bias. Gac Sanit 2014;28. doi: 10.1016/j.gaceta.2013.12.011 [DOI] [PubMed] [Google Scholar]
- 45.Sugiyama T, Neuhaus M, Cole R, et al. Destination and route attributes associated with adults’ walking: a review. Med Sci Sports Exerc 2012;44:1275–86. doi: 10.1249/MSS.0b013e318247d286 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


