Abstract
Purpose of Review
In recent years, the spectrum of neurological manifestations of antiphospholipid syndrome (APS) has been growing. We provide a critical review of the literature with special emphasis on presentation, proposed mechanisms of disease, and treatment of neurological involvement in APS.
Recent Findings
Although stroke is the most common cause of neurological manifestations in patients with APS, other neurological disorders have been increasingly associated with the disease, including cognitive dysfunction, headache, and epilepsy. Direct oral anticoagulants have failed to show non-inferiority compared to vitamin K antagonists for the prevention of major thrombotic events. Antiphospholipid antibodies are often found in patients with acute COVID-19 but clear evidence supporting an association between these antibodies and the risk of thrombotic events, including stroke and cerebral venous thrombosis, is still lacking.
Summary
APS patients may present with several distinct neurological manifestations. New criteria will facilitate the classification of patients presenting with increasingly recognized non-criteria neurological manifestations.
Keywords: Antiphospholipid, Thrombosis, Stroke, Headache, Anticoagulation
Introduction
Antiphospholipid syndrome (APS) is an immune-mediated disorder characterized by pregnancy morbidity and arterial or venous thrombotic events associated with persistent antiphospholipid antibodies (aPL) [1]. These include lupus anticoagulant (LA), anticardiolipin (aCL), and anti-β2-glycoprotein I antibodies (aB2GPI), among several others, all of which directed against phospholipid-binding proteins [2].
Overall, aPL are present in 1–5% of the general population, with a higher prevalence in older subjects [3]. However, only a subset of patients actually develops APS [3]. The estimated prevalence of APS is 40–50/100,000 subjects, with an incidence of 5 cases per 100,000 subjects per year [4]. APS is a major cause of thrombosis, with a classically cited “20% rule,” as it was said to account for up to 20% of unprovoked deep vein thrombosis (DVT), 20% of strokes in young adults (<50 years), and up to 20% of women with recurrent fetal loss. These figures have been more recently updated to 20% of DVT, 20–30% of strokes in young adults (<50 years), and 10–15% of women with recurrent fetal loss [5, 6].
APS is usually divided into two groups: primary APS, also named Hughes syndrome, and secondary APS, associated with another systemic inflammatory rheumatic disease. In fact, approximately 50% of patients with APS have a secondary form in association with an inflammatory disease, most commonly systemic lupus erythematosus (SLE) [7]. It has been shown that up to 10% of patients with primary APS are diagnosed with SLE within 10 years and redefined as secondary APS [8]. In turn, around a third of SLE patients have identifiable antiphospholipid antibodies, with roughly 10% developing APS [9]. Infections and drugs, such as phenothiazines, procainamide, quinine, and anti-TNF agents, are apparently able to induce aPL, usually transiently and without associated hypercoagulability [10–12]. Current classification criteria require the presence of both clinical and laboratory findings and are represented in Table 1 [1]. They may assist but are not intended for diagnosis, which should always be established clinically by the attending physician [13].
Table 1.
Revised classification criteria for APS [1]
| Clinical criteria (≥1 of the following) | |
|---|---|
| Vascular thrombosis | ≥1 clinical episodes of venous, arterial, or small vessel thrombosis in any tissue or organ |
| Pregnancy morbidity |
≥1 unexplained deaths of a morphologically normal fetus at or beyond the 10th week of gestation ≥1 premature births of a normal neonate before the 37th week of gestation caused by placental insufficiency (eclampsia or severe preeclampsia) ≥3 unexplained consecutive abortions before the 10th week of gestation |
| Laboratory criteria (≥1 of the following) | |
| Lupus anticoagulant in plasma, on ≥2 occasions at least 12 weeks apart (detected according to the International Society of Thrombosis and Haemostasis) | |
| Anticardiolipin antibody (IgG or IgM) in serum or plasma and in medium or high titer on ≥2 occasions at least 12 weeks apart (measured by standardized ELISA) | |
| Anti-β2-glycoprotein-I antibody (IgG or IgM) in serum or plasma and in high titer on ≥2 occasions at least 12 weeks apart (measured by standardized ELISA) | |
In rare cases, catastrophic APS, also named Asherson syndrome, occurs as a rapidly progressive thromboembolic disease characterized by the involvement of three or more organ systems, simultaneously or within 1 week, with histological evidence of predominant small vessel occlusion [14].
In addition to the clinical features considered in the classification criteria, APS can present with other common non-criteria manifestations, including thrombocytopenia, livedo reticularis, arthralgia, or heart valve disease (mitral valve more frequently involved) [15]. New criteria are being developed, including some of the aforementioned non-criteria manifestations [16].
Vascular thrombosis, the main clinical feature, can occur in any tissue or organ, with a wide range of events and symptoms that may include many neurological manifestations.
This article summarizes the central and peripheral nervous system involvement in APS.
Pathophysiology
Currently, over 30 different types of aPL are known [17, 18]. B2GPI is recognized as one of the most relevant antigens in the pathophysiology of APS [19]. Autoantibodies targeting this antigen are diverse, but the presence of anti-domain I antibodies has been strongly correlated to thrombosis, especially in the venous territory [20]. These are part of the so-called non-criteria aPL, some of which are displayed in Table 2. Non-criteria aPL are generally not assessed in clinical practice. However, they are currently an intense area of investigation, with special attention on their relevance for the diagnosis, pathogenesis, and phenotype of APS. Some have been described to a greater extent, such as the phosphatidylserine-dependent antiprothrombin antibody (aPS/PT). Studies have shown an association between aPS/PT and thrombosis besides higher diagnostic sensitivity and specificity for APS when compared to aCL [31]. It also seems to be relevant in thrombosis [32–35] and obstetric [36] risk stratification in APS [28, 37].
Table 2.
Non-criteria aPL and their association to APS manifestations
| Non-criteria aPL | Associated APS manifestation |
|---|---|
| Antibodies against prothrombin (aPT) | Arterial thrombosis [21, 22] and disease severity [23] |
| CNS manifestations (copresence of aPT, aPG, aAN, and aPI) [21] | |
| Considerably more prevalent in males [21] | |
| aB2GPI (including IgA) | Chorea in young female patients [24, 25] |
| Thrombosis [26] | |
| Phosphatidylserine/prothrombin complex | Strongly correlates with the presence of LA [27] |
| Arterial and venous thrombosis [28] | |
| Thrombotic microangiopathy (considered a milestone for catastrophic APS) [28] | |
| Anti-phosphatidylserine (aPS) | Pregnancy morbidity (copresence with aCL) [21] |
| Anti-phosphatidylglycerol (aPG) | CNS manifestations (copresence of aPT, aPG, aAN, and aPI) [21] |
| Anti-vimentin | Disease severity [23] |
| Anti-annexin 5 (aAN) | Pregnancy morbidity [21, 29] |
| CNS manifestations (copresence of aPT, aPG, aAN, and aPI) [21] | |
| Anti-phosphatidic acid | IgM inversely associated to venous thrombosis [21] |
| Fetal loss but not thrombosis [26] | |
| Anti-phosphatidylinositol (aPI) | CNS manifestations (copresence of aPT, aPG, aAN, and aPI) [21] |
| Significantly associated with thrombosis in patients with APS and SLE [30] | |
| Anti-phosphatidylethanolamine (aPE) | Disease severity [23] |
The most common location of arterial thrombosis is the cerebral circulation, with ischemic stroke or transient ischemic attack (TIA) being the initial presentation in almost 30% of adults with APS [38•]. However, more recent evidence supports the concept that APS-associated neurologic dysfunction extends beyond the classical thromboembolic events and is also related with immune-mediated vascular, inflammatory, and direct neuronal effects [39]. Increased permeability of the blood–brain barrier can be due both to small/microvessel thrombosis, with subsequent ischemia, but also to the direct effects of antiphospholipid antibodies [40]. These have been shown to trigger leukoadhesion and complement activation, further breaching this barrier and resulting in neurotoxicity from cytokines and antibodies [40].
Risk factors for each clinical phenotype of neurological involvement have been suggested but are not yet fully understood. In a recent study by Volkov et al. [21••], assessing the presence of 20 different aPLs and its correlation to different manifestations in APS, central nervous system (CNS) manifestations were shown to be correlated to a specific aPL profile, with simultaneous positivity for IgG antibodies against prothrombin, phosphatidylglycerol, phosphatidylinositol, and annexin-5. Previous studies have also suggested a correlation between cognitive deficit and higher titers of aPLs [41]. Female patients had a higher prevalence of migraine, while epilepsy was more common in men [42]. In turn, chorea was more frequent in young female patients with APS carrying aB2GPI [24, 25]. More studies, however, are needed to better understand which pathological pathways are involved in APS-associated neurological disease, as well as additional clinical and biological predictors, including the value of non-criteria aPLs [23].
Neurological Manifestations of APS
The main neurological manifestations of APS are summarized in Fig. 1.
Fig. 1.
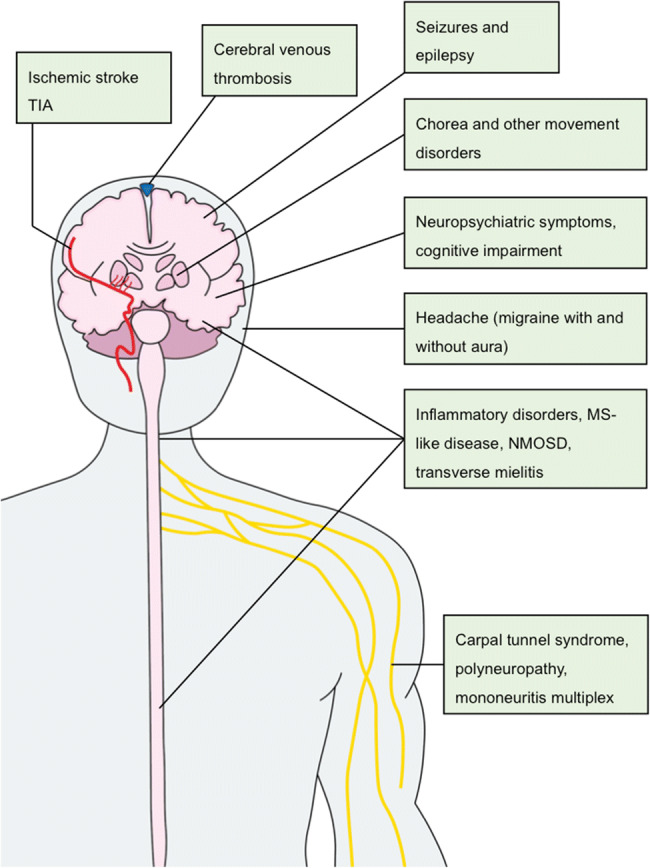
The main neurological manifestations of APS
Central Nervous System Manifestations
Cerebrovascular Disease
Cerebrovascular disease is the most common cause of neurological manifestations in patients with APS and, as a thromboembolic event, can be considered part of the clinical criteria for classifying APS. It includes acute ischemic stroke and TIA, for which APS is a known risk factor; cerebral venous thrombosis (CVT); and other less frequent disorders such as Sneddon’s syndrome and reversible cerebral vasoconstriction syndrome.
Ischemic Stroke and TIA
Stroke and TIA are the most common forms of clinical manifestation related with arterial circulation in APS [4, 38]. In the Euro-Phospholipid cohort, which included 1000 patients, stroke had a reported prevalence of 20%; and TIA occurred in 11% of all patients [38•]. On the other hand, the frequency of positive aPLs in stroke patients ranges between 7% and 15% [43], with an apparent age-dependent relationship between aPL positivity and stroke: the mean age of aPL-positive stroke patients is younger than the general population [44–46]; APS has been suggested to account for a significant proportion of acute ischemic stroke in young patients [47]; and the presence of aPL determines an over 5-fold increase in cerebrovascular thrombotic events (odds ratio [OR] of 5.48, 95% confidence interval [CI]: 4.42 to 6.79) in stroke patients under 50 years (median age of 37 years) [48]. In older patients, aPL positivity may be a less significant risk factor due to the competing cardiovascular risk factors, a differential effect between different aPLs, and bias derived from study design, as studies often exclude patients with cardioembolic stroke [49, 50]. The stroke mechanism in APS is thought to be mostly either thrombotic or cardioembolic. Still, intracranial occlusions and stenosis are present in 50% of patients with APS and stroke [45], and a vasculitis-like pattern has been observed, suggesting a concurrent vasculopathic process in some cases [51–53]. Cardioembolic mechanisms include left-sided cardiac valve abnormalities (irregular thickening due to immune complex deposition, vegetations, valve dysfunction) and, rarely, intracardiac thrombi [54–56]. Small vessel cerebrovascular disease is also often reported, leading to lacunar and subcortical strokes [57].
Cerebral Venous Thrombosis
CVT is a rare complication of APS, with a reported prevalence of 0.7% [38•]. On the other hand, APS contributes to a significant proportion of CVT cases (6–17% in cohort studies) [58], and aCL positivity may be found in 7–22% of patients [59, 60]. CVT may be the presenting symptom of APS [61]. Treatment should follow the general guidelines for CVT [62] and usually includes long-term anticoagulation [58].
Other Cerebrovascular Disorders
Sneddon’s syndrome is a slowly progressive noninflammatory thrombotic vasculopathy characterized by livedo racemosa and recurrent cerebrovascular (ischemic or hemorrhagic) events [63]. It is classically classified as aPL negative or aPL positive (41% of patients in one case series) [63, 64]. aPL-positive patients may have a clinical course similar to primary APS patients [63, 65]. Knowledge about the specific role of aPL in this syndrome, its clinical course, and ideal treatment is severely limited by the scarcity of reports. Less consistent associations of cerebrovascular disorders with APS include reversible cerebral vasoconstriction syndrome [66] and Moyamoya disease [67].
Seizures and Epilepsy
Epilepsy has a prevalence of around 6 to 9% in people with APS [38, 68, 69]. Seizure risk differs between primary and secondary APS, with a prevalence of epilepsy higher in the latter (6% and 14%, respectively) [68]. In a group of 240 primary APS patients, seizures were part of the neurological findings in 8% of the patients [70]. The exact pathogenesis of seizures related to APS is unknown, in part due to the combined inclusion of primary and secondary APS in most cohorts. Nevertheless, there are several proposed mechanisms including microthrombosis-induced ischemia leading to vascular epilepsy, aPL neuronal binding and injury, aPL-mediated inhibition of GABA receptors, and immune-mediated neuronal damage [69, 71, 72]. Although there have been several studies assessing the association of aPL with seizures or epilepsy in primary and secondary APS patients, results have been contradictory (see Noureldine et al. [72•] for a review). Clinical manifestations are protean, and all types of seizures may be reported, including electroencephalographic abnormalities without clinically evident seizures [46, 72]. Testing for aPL is only recommended in young patients with atypical seizures or in individuals with multiple MRI abnormalities for which no other plausible cause is found [72•]. There are no specific anti-epileptic drug regimens recommended for seizures in APS patients, and anticoagulation in the absence of ischemic lesions or a clear diagnosis of APS — that is, with isolated aPL and no other typical APS manifestations — is controversial.
Cognitive and Neuropsychiatric Manifestations
The frequent comorbidity of APS and aPL positivity with other autoimmune disorders, in particular with SLE, has hampered the establishment of a clear-cut cognitive profile and risk of neuropsychiatric abnormalities in patients with APS [73]. Proposed pathophysiologic mechanisms include a prothrombotic state, an inflammatory response, and a neuronal immune-/aPL-mediated response [73]. Cognitive impairment is present in 19–40% of aPL-positive patients and 42–80% of primary APS patients [39, 73–76]. A study enrolling 143 APS patients with moderate and high aPL titers found a linear relationship between aPL titers and cognitive dysfunction [76]. The prototypical manifestation in primary APS is a subcortical pattern of mild cognitive impairment [46, 74]. Dementia (classified as multi-infarct dementia) was shown to affect 2.5% of APS patients included in the Euro-APS cohort that includes both primary and secondary APS [38•]. APS should therefore be ruled out in young subjects with otherwise unexplained dementia [77]. Chronic ischemic cerebrovascular disease associated with aCL antibodies may be responsible for a vascular/multi-infarct dementia that may partially improve with the institution of APS therapy [47, 77, 78]. Reports on favorable cognitive outcomes with immunosuppression (rituximab) also exist [79], but lack of evidence precludes therapeutic guidelines for cognitive dysfunction in APS.
Other neuropsychiatric symptoms including psychotic, mood, and anxiety disorders have been reported in APS [73, 80, 81]. It has been postulated that the high prevalence of aPL in patients with psychosis may be due to aPL induction of some antipsychotic drugs [82–84]. Nevertheless, older age, cerebral lesions, and triple aPL positivity are considered risk factors for psychiatric manifestations in APS [46, 84]. Acute encephalopathy characterized by confusion, disorientation, and hyperreflexia was reported in 1.1% of APS patients [38, 85].
Headache
Although migraineurs more frequently have aPL antibodies, migraine is most likely a comorbid condition with aPL positivity than a consequence of APS [86–88]. With an estimated prevalence of 20% in people with APS [38•], migraine may be a result of the high prevalence of headache in the general population and an age overlap between migraineurs and APS patients. On the other hand, data from some cohorts suggested migraine as a possible risk factor for stroke in aPL-positive patients [89], and both migraine with aura and aPL were found to be independent predictors of thrombotic event recurrence in young patients in an Italian multicenter cohort study [90].
To further the matter, Cavestro et al. [91•] recently conducted a study assessing the association among migraine, thrombophilic conditions, and vascular events. Among the 329 included migraine patients, 32% had at least one thrombophilic marker, and aPL positivity was more common than in controls (12.5% vs. 5.2%, OR 2.6, 95% CI 1.5–4.7). There was an association between thrombophilic changes and history of arterial — but not venous — vascular events in migraine patients but not in controls. The authors concluded that aPLs are associated with both migraine and thrombotic events and that migraine is probably secondary to the thrombophilic changes [88, 92]. As aPL is a common precursor to both conditions and an association was expected, causality cannot be assumed. Another recent retrospective study of 75 patients with refractory migraine and aPL described that most patients had an improvement in the frequency and/or severity of migraine after a 2–4-week trial of anti-thrombotic therapy (aspirin, clopidogrel, and/or anticoagulants) [93•]. Notably, treatment was associated with low bleeding risk, and the response was overall sustained during a mean follow-up period of 29.9 months (5 to 100 months) [93•]. Randomized controlled trials (RCTs) are needed to effectively assess this therapeutic option in this subset of migraine patients.
Demyelinating and Inflammatory Disorders
Neuroimmune and neuroinflammatory disorders related to APS are particularly remarkable as they are proof of the contribution of non-thrombotic mechanisms to APS pathophysiology. Inflammatory CNS involvement in APS may be due to a local immunologic dysregulation, blood–brain barrier dysfunction yielding access to the CNS immune compartment, direct neurotoxic effect of aPL antibodies, or molecular mimicry and cross-reactivity between myelin/myelin-related proteins and cerebral phospholipids [94••].
Multiple Sclerosis-Like Disease
The differential diagnosis between multiple sclerosis (MS), MS-like disease, and MS-SLE overlap syndrome, although supported by clinical and imaging features, remains challenging [46, 70, 95, 96]. MS predominantly affects women of childbearing age, similarly to APS, and the prevalence of aPL antibodies in MS patients has been reported in a wide range of 2 to 88% [94, 97, 98]. aPL positivity may be more frequent during MS relapses/exacerbations and in secondary progressive MS compared to relapsing–remitting MS [99–101]. Nevertheless, autoimmune disorders, such as MS, are more frequently associated with autoreactive antibodies, and the significance of aPL antibodies and MS is still to be determined [102–104]. MRI is useful to distinguish between MS and APS mimicking MS. Lesions in APS tend to maintain shape and size on repeat scanning, have lower total lesion volumes, are predominantly subcortical instead of periventricular, do not show the typical ovoid shape nor predilection for the corpus callosum, may affect the putamen, and are less associated to a reduction in brain parenchymal fraction [96, 97, 105, 106]. Cerebrospinal fluid (CSF) analysis with a normal cell count and absence of oligoclonal bands is in favor of APS [107]. As such, previous thrombotic events, acute onset of atypical symptoms, abnormal MRI lesion location, and response to anticoagulation can help affirm the diagnosis of APS [70, 97]. As a rule, screening of aPL in MS patients should be reserved for patients with atypical characteristics [108]. Early initiation of disease-modifying treatments in MS is associated with improved outcomes [109], so all laboratory, imaging, and clinical data must be carefully reviewed before diagnosing an MS-like APS syndrome, MS with aPL positivity, or the coexistence of both MS and APS.
Neuromyelitis Optica Spectrum Disorders
Neuromyelitis optica (NMO) and its spectrum disorders (NMOSD) are a group of autoimmune astrocytopathies/channelopathies with secondary demyelination [110] associated with a highly specific and pathogenic biomarker, the anti-aquaporin-4-IgG (AQP4-IgG) [110]. The hallmark of these disorders is a longitudinally extensive transverse myelitis (LETM) and a severe, often recurrent, optic neuritis [111]. NMOSD is frequently associated with other autoimmune rheumatic disorders such as Sjögren’s syndrome, rheumatoid arthritis, and SLE [112, 113]. In particular, aPL antibodies are found in 19–46% of NMOSD patients [114, 115]. Due to this overlap, APS patients with optic neuritis or LETM should be screened for AQP4, as instead (or in addition to) anticoagulation, long-term immunosuppression may be warranted [112, 116, 117].
Transverse Myelopathy and Myelitis
Transverse myelitis is infrequent in APS (0.4–4%) and may be a result of vascular or thrombotic mechanisms (i.e., vasculitis, ischemic cord necrosis) [38, 118]. The onset of motor or sensorial symptoms is most often sudden but may be subacute (up to 14 days); CSF analysis shows elevated protein and pleocytosis in a minority of patients, and early diagnosis and treatment are vital to prevent morbidity [119]. As TM may be the initial presentation of NMOSD or MS, adequate investigation, especially in the presence of an LETM or recurrent myelitis, should always be pursued.
Movement Disorders
Movement disorders, although rare, are classically considered non-thrombotic neurological manifestations of APS. The historical hypothesis is that lenticulo-striate artery occlusion produces ischemia of basal ganglia and explains the occurrence of these disorders [120]. Against this thrombotic hypothesis, there are several reports of patients with normal MRI and good response to immunomodulation and an increasingly studied direct effect of aPL on neuronal tissue, as explained previously [120]. Whether APS-related movement disorders are due to aPL-induced white matter and basal ganglia damage or to cerebrovascular disease is still to be ascertained [52, 78].
Chorea occurs in around 1% of patients with primary or secondary APS [38•]. It is more common in females, with a mean age of onset between 20 and 44 years. In a minority of patients (5.5 to 16.1%), there are ischemic signs on the basal ganglia [24, 25, 120, 121]. Clinically, aPL-related chorea can involve all body parts, is usually mild to moderate in severity, and is often associated with other neurologic and movement disorders such as ataxia and dystonia at the onset [24]. Moreover, chorea may appear in patients with high titers of aPLs without overt APS syndrome or other manifestations of immune-mediated conditions [120, 122]. Short follow-up times, fluctuating positive aPL titers, and heterogeneous investigation and treatment response cast doubt on the relationship between these entities. Interestingly, a fairly recent report described a 74-year old woman with a 6-month history of isolated oromandibular chorea, thrombocytopenia, and persistently positive LA and aCL antibodies who showed a complete resolution of symptoms after a trial of anticoagulant therapy with warfarin [123]. Treatment of APS-related chorea may include symptomatic relief with dopaminergic agents, anticoagulation, and immunossupression [83].
Other movement disorders have been reported in primary or secondary APS and in the presence of aPL antibodies, although less frequently, including ballismus (0.3% prevalence), dyskinesia, parkinsonism, and cerebellar ataxia [38, 124–127].
Peripheral Nervous System Manifestations of APS
Peripheral nerve involvement in primary APS may be a consequence of ischemic thrombosis of the vasa nervorum, vasculitis (with the prototypical mononeuritis multiplex presentation), or direct nerve damage by pathogenic antibodies [128]. Although reports on the relationship between aPLs and immune-mediated peripheral nerve syndromes exist (e.g., Guillain–Barré syndrome), they are scarce and confounded by concomitant intravenous immunoglobulin (IVIG) administration [129, 130]. An electrophysiological study in a sample of 26 primary APS patients (8 of whom with clinical signs of neuropathy) found abnormalities in nerve conduction studies (NCS) in 35% (n = 9) of the patients, independently of previous thrombotic events [131•]. The most frequent findings were carpal tunnel syndrome (23%), polyneuropathy (19%), and distal axonal sensorimotor neuropathy (15%). Most patients with abnormal NCS findings had no clinical signs of neuropathy (subclinical neuropathy) [131•].
Autonomic disorders (such as complex regional pain syndrome, labile hypertension, or postural tachycardia syndrome) have been described as presenting manifestations of APS and are postulated to be due to thrombotic or immune-mediated small-fiber dysfunction [132].
General Management of APS
The current standard of care for APS is based on anticoagulation and, in some cases, antiplatelet drugs. Besides clinical manifestations, the aPL type, number, persistence, and titers are important factors on the prognosis of APS as, for instance, a triple-positive profile is associated with a higher thrombotic risk. This so-called aPL profile should dictate the intensity of the treatment, particularly for primary prophylaxis in patients with aPL but non-criteria manifestations, such as neurological involvement [133]. Treatment of patients with APS and neurological manifestations is mostly based on indirect evidence from similar syndromes in non-APS patients. There are some case reports, small case series, and retrospective studies suggesting a possible benefit of anticoagulation and/or immunomodulation even in the absence of an overt thrombotic event (e.g., in patients with myelitis or headache), but the decision still relies mostly on a case-by-case analysis, without strong evidence to support it.
Primary thromboprophylaxis in aPL-positive individuals is usually low-dose aspirin, which was shown to reduce by half the risk of the first thrombosis [134]. For patients with venous thrombotic APS, the standard treatment is warfarin (or another vitamin K antagonist [VKA]) for a target international normalized ratio [INR] of 2–3 [133]. In patients with arterial thrombosis or recurrent venous thrombosis, an INR of 3.0–4.0 or the association of a VKA with low-dose aspirin is indicated [133]. The use of direct oral anticoagulants (DOACs) has been an area of great interest, as this would facilitate treatment adherence. However, there is no current definite use for DOACs in APS after several major trials failed to reach primary efficacy and safety endpoints [135–137]. The European League Against Rheumatism (EULAR) guidelines issued in 2019 warrant a single exception for rivaroxaban, which could be considered in patients with contraindications for VKA or unable to reach the target INR despite proper adherence [133]. Still, DOACs should not be used in patients with high titer aPL as evidenced in a recent RCT that was prematurely terminated because of an excess of arterial events in the rivaroxaban arm [138]. DOACs should also be avoided in patients with a history of arterial thrombosis due to a particularly high risk of recurrent thrombosis. This is a recommendation of major importance when focusing on neurological manifestations of APS, as stroke is one of the most common events. Efforts are being made towards assessing whether other DOACs are useful in APS, with no positive results so far [139–141].
For obstetric APS, the association of low-dose aspirin with prophylactic dose low molecular weight heparin (LMWH) is warranted [133]. The addition of hydroxychloroquine in obstetric APS refractory to anticoagulation and antiplatelet therapy may be considered [133, 142]. aPL-positive women without previous pregnancy complications or thrombotic manifestations should be started on low-dose aspirin alone [133, 142]. In turn, patients with thrombotic APS should switch VKA to full-dose LMWH, as the former is teratogenic [133, 142]. The recent 2020 American College of Rheumatology (ACR) guidelines strongly recommend against the addition of prednisone or IVIG in refractory obstetric APS, whereas EULAR guidelines suggest that this treatment may be considered in selected cases [133, 143]. Catastrophic APS may be treated with a combination of glucocorticoids, heparin, and plasma exchange or IVIG as the first-line treatments [133, 142]. Rituximab or eculizumab are selected for refractory catastrophic APS based on successful data from case reports [133, 144].
COVID-19 and Antiphospholipid Antibodies
Coronavirus disease 2019 (COVID-19) patients have a hypercoagulable state with a high prevalence of venous and arterial thrombosis [145], including ischemic stroke and CVT [146–148]. It is currently unclear, though, if these strokes have unique characteristics [146–148]. Some studies have proposed a connection between the increased thrombotic risk in COVID-19 patients and the presence of antiphospholipid antibodies. In fact, there is a high prevalence of LA in severe COVID-19 patients, up to 88% in several studies [145, 149, 150], which is significantly higher compared to other infections [151]. The association of this finding with thrombosis is however not fully established [145, 150]. Concomitant use of anticoagulation, hydroxychloroquine, and high levels of C-reactive protein may have influenced the LA test [152, 153].
aCL and aB2GPI have also been found in around 10 to 12% of critically ill COVID-19 patients [154]. In a multicenter study with 122 COVID-19 patients, prevalence and titers of aPL were neither consistently increased nor associated with thrombosis [155]. In a systematic review of patients with CVT associated to COVID-19, thrombophilia screening results were available for 12 out of 28 cases, of which three had positive lupus anticoagulant and two anticardiolipin antibodies [148]. As mentioned before, infection-induced, usually transient, aPLs are not associated with a higher thrombotic risk. Studies with larger cohorts, including less severe patients and evaluating the persistence of aPLs, are needed to assess this relationship.
Conclusions
Cerebrovascular disease is the most common cause of neurological manifestations in APS. However, these patients may present with other distinct neurological manifestations, most of which still have unclear pathophysiology. There is a growing interest in better assessing the role of inflammatory and direct neuronal effects in the pathogenesis of non-criteria manifestations and in establishing optimal therapy. There are a few recent reports suggesting a possible benefit of anticoagulation for selected non-criteria manifestations that are not classically considered to be thrombotic, although evidence is generally of poor quality. VKAs continue to be the mainstay of therapy for patients with thrombotic manifestations despite several trials evaluating the safety and efficacy of DOACs. The new classification criteria that are being developed are expected to facilitate the diagnosis in patients with non-criteria manifestations, such as neurological involvement, improve patient selection in clinical studies, and, ultimately, promote the identification of new therapeutic options.
Declarations
Conflict of Interest
Miguel Leal Rato and Matilde Bandeira each declare no potential conflicts of interest. Vasco C. Romão reports grants from MSD, personal fees from Janssen, and nonfinancial support from Novartis, Pfizer, and Medac. Diana Aguiar de Sousa reports nonfinancial support from Boehringer Ingelheim.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Neurology of Systemic Diseases
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Miguel Leal Rato and Matilde Bandeira contributed equally to this work.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Miyakis S, Lockshin MD, Atsumi T, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS) J Thromb Haemost. 2006;4(2):295–306. doi: 10.1111/j.1538-7836.2006.01753.x. [DOI] [PubMed] [Google Scholar]
- 2.Shoenfeld Y, Twig G, Katz U, Sherer Y. Autoantibody explosion in antiphospholipid syndrome. J Autoimmun. 2008;30(1-2):74–83. doi: 10.1016/j.jaut.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 3.Cervera R. Antiphospholipid syndrome. Thromb Res. 2017;151(Suppl):S43–S47. doi: 10.1016/S0049-3848(17)30066-X. [DOI] [PubMed] [Google Scholar]
- 4.Schreiber K, Sciascia S, de Groot PG, Devreese K, Jacobsen S, Ruiz-Irastorza G, Salmon JE, Shoenfeld Y, Shovman O, Hunt BJ. Antiphospholipid syndrome. Nat Rev Dis Prim. 2018;4:17103. doi: 10.1038/nrdp.2017.103. [DOI] [PubMed] [Google Scholar]
- 5.Ginsburg KS, Liang MH, Newcomer L, Goldhaber SZ, Schur PH, Hennekens CH, Stampfer MJ. Anticardiolipin antibodies and the risk for ischemic stroke and venous thrombosis. Ann Intern Med. 1992;117(12):997–1002. doi: 10.7326/0003-4819-117-12-997. [DOI] [PubMed] [Google Scholar]
- 6.Cervera R, Khamashta MA, Shoenfeld Y, Camps MT, Jacobsen S, Kiss E, Zeher MM, Tincani A, Kontopoulou-Griva I, Galeazzi M, Bellisai F, Meroni PL, Derksen RH, de Groot PG, Gromnica-Ihle E, Baleva M, Mosca M, Bombardieri S, Houssiau F, Gris JC, Quéré I, Hachulla E, Vasconcelos C, Roch B, Fernández-Nebro A, Piette JC, Espinosa G, Bucciarelli S, Pisoni CN, Bertolaccini ML, Boffa MC, Hughes GR, Euro-Phospholipid Project Group (European Forum on Antiphospholipid Antibodies) Morbidity and mortality in the antiphospholipid syndrome during a 5-year period: a multicentre prospective study of 1000 patients. Ann Rheum Dis. 2009;68(9):1428–1432. doi: 10.1136/ard.2008.093179. [DOI] [PubMed] [Google Scholar]
- 7.Cervera R, Serrano R, Pons-Estel GJ, Ceberio-Hualde L, Shoenfeld Y, de Ramón E, Buonaiuto V, Jacobsen S, Zeher MM, Tarr T, Tincani A, Taglietti M, Theodossiades G, Nomikou E, Galeazzi M, Bellisai F, Meroni PL, Derksen RHWM, de Groot PGD, Baleva M, Mosca M, Bombardieri S, Houssiau F, Gris JC, Quéré I, Hachulla E, Vasconcelos C, Fernández-Nebro A, Haro M, Amoura Z, Miyara M, Tektonidou M, Espinosa G, Bertolaccini ML, Khamashta MA. Morbidity and mortality in the antiphospholipid syndrome during a 10-year period: a multicentre prospective study of 1000 patients. Ann Rheum Dis. 2015;74(6):1011–1018. doi: 10.1136/annrheumdis-2013-204838. [DOI] [PubMed] [Google Scholar]
- 8.Levine JS, Branch DW, Rauch J. The antiphospholipid syndrome. N Engl J Med. 2002;346(10):752–763. doi: 10.1056/NEJMra002974. [DOI] [PubMed] [Google Scholar]
- 9.Ünlü O, Zuily S, Erkan D. The clinical significance of antiphospholipid antibodies in systemic lupus erythematosus. Eur J Rheumatol. 2016;3(2):75–84. doi: 10.5152/eurjrheum.2015.0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sène D, Piette J-C, Cacoub P. Antiphospholipid antibodies, antiphospholipid syndrome and infections. Autoimmun Rev. 2008;7(4):272–277. doi: 10.1016/j.autrev.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 11.Gharavi AE, Sammaritano LR, Wen J, Miyawaki N, Morse JH, Zarrabi MH, Lockshin MD. Characteristics of human immunodeficiency virus and chlorpromazine induced antiphospholipid antibodies: effect of beta 2 glycoprotein I on binding to phospholipid. J Rheumatol. 1994;21(1):94–99. [PubMed] [Google Scholar]
- 12.Dlott JS, Roubey RAS. Drug-induced lupus anticoagulants and antiphospholipid antibodies. Curr Rheumatol Rep. 2012;14(1):71–78. doi: 10.1007/s11926-011-0227-1. [DOI] [PubMed] [Google Scholar]
- 13.Aggarwal R, Ringold S, Khanna D, Neogi T, Johnson SR, Miller A, Brunner HI, Ogawa R, Felson D, Ogdie A, Aletaha D, Feldman BM. Distinctions between diagnostic and classification criteria? Arthritis Care Res. 2015;67(7):891–897. doi: 10.1002/acr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cervera R, Rodríguez-Pintó I, Colafrancesco S, Conti F, Valesini G, Rosário C, Agmon-Levin N, Shoenfeld Y, Ferrão C, Faria R, Vasconcelos C, Signorelli F, Espinosa G. 14th International Congress on Antiphospholipid Antibodies Task Force report on catastrophic antiphospholipid syndrome. Autoimmun Rev. 2014;13(7):699–707. doi: 10.1016/j.autrev.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 15.Ruiz-Irastorza G, Crowther M, Branch W, Khamashta MA. Antiphospholipid syndrome. Lancet (London, England) 2010;376(9751):1498–1509. doi: 10.1016/S0140-6736(10)60709-X. [DOI] [PubMed] [Google Scholar]
- 16.Barbhaiya M, Zuily S, Ahmadzadeh Y, et al. Development of new international antiphospholipid syndrome classification criteria phase I/II report: generation and reduction of candidate criteria.; 2020. doi:10.1002/acr.24520 [DOI] [PMC free article] [PubMed]
- 17.Mekinian A, Bourrienne M-C, Carbillon L, Benbara A, Noémie A, Chollet-Martin S, Tigaizin A, Montestruc F, Fain O, Nicaise-Roland P. Non-conventional antiphospholipid antibodies in patients with clinical obstetrical APS: prevalence and treatment efficacy in pregnancies. Semin Arthritis Rheum. 2016;46(2):232–237. doi: 10.1016/j.semarthrit.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 18.Shi H, Zheng H, Yin Y-F, Hu QY, Teng JL, Sun Y, Liu HL, Cheng XB, Ye JN, Su YT, Wu XY, Zhou JF, Norman GL, Gong HY, Shi XM, Peng YB, Wang XF, Yang CD. Antiphosphatidylserine/prothrombin antibodies (aPS/PT) as potential diagnostic markers and risk predictors of venous thrombosis and obstetric complications in antiphospholipid syndrome. Clin Chem Lab Med. 2018;56(4):614–624. doi: 10.1515/cclm-2017-0502. [DOI] [PubMed] [Google Scholar]
- 19.de Laat B, Mertens K, de Groot PG. Mechanisms of disease: antiphospholipid antibodies-from clinical association to pathologic mechanism. Nat Clin Pract Rheumatol. 2008;4(4):192–199. doi: 10.1038/ncprheum0740. [DOI] [PubMed] [Google Scholar]
- 20.de Laat B, Pengo V, Pabinger I, et al. The association between circulating antibodies against domain I of beta2-glycoprotein I and thrombosis: an international multicenter study. J Thromb Haemost. 2009;7(11):1767–1773. doi: 10.1111/j.1538-7836.2009.03588.x. [DOI] [PubMed] [Google Scholar]
- 21.Volkov I, Seguro L, Leon EP, et al. Profiles of criteria and non-criteria anti-phospholipid autoantibodies are associated with clinical phenotypes of the antiphospholipid syndrome. Auto- Immun highlights. 2020;11(1):8. doi: 10.1186/s13317-020-00131-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang S, Wu Z, Li J, Li P, Chen S, Wen X, Li L, Zhang W, Zhao J, Zhang F, Li Y. Clinical performance of antibodies to prothrombin and thrombin in Chinese patients with antiphospholipid syndrome: potential interest in discriminating patients with thrombotic events and non-thrombotic events. Rheumatol Int. 2017;37(4):579–584. doi: 10.1007/s00296-016-3594-0. [DOI] [PubMed] [Google Scholar]
- 23.Cervera R, Conti F, Doria A, Iaccarino L, Valesini G. Does seronegative antiphospholipid syndrome really exist? Autoimmun Rev. 2012;11(8):581–584. doi: 10.1016/j.autrev.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 24.Orzechowski NM, Wolanskyj AP, Ahlskog JE, Kumar N, Moder KG. Antiphospholipid antibody-associated chorea. J Rheumatol. 2008;35(11):2165–2170. doi: 10.3899/jrheum.080268. [DOI] [PubMed] [Google Scholar]
- 25.Reine P, Galanaud D, Leroux G, et al. Long-term outcome of 32 patients with chorea and systemic lupus erythematosus or antiphospholipid antibodies. Mov Disord. 2011;26(13):2422–2427. doi: 10.1002/mds.23851. [DOI] [PubMed] [Google Scholar]
- 26.Pignatelli P, Ettorre E, Menichelli D, Pani A, Violi F, Pastori D. Seronegative antiphospholipid syndrome: refining the value of “non-criteria” antibodies for diagnosis and clinical management. Haematologica. 2020;105(3):562–572. doi: 10.3324/haematol.2019.221945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tebo AE. Laboratory Evaluation of antiphospholipid syndrome: an update on autoantibody testing. Clin Lab Med. 2019;39(4):553–565. doi: 10.1016/j.cll.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 28.Hoxha A, Mattia E, Tonello M, Grava C, Pengo V, Ruffatti A. Antiphosphatidylserine/prothrombin antibodies as biomarkers to identify severe primary antiphospholipid syndrome. Clin Chem Lab Med. 2017;55(6):890–898. doi: 10.1515/cclm-2016-0638. [DOI] [PubMed] [Google Scholar]
- 29.Rand JH, Wu X-X, Quinn AS, Taatjes DJ. The annexin A5-mediated pathogenic mechanism in the antiphospholipid syndrome: role in pregnancy losses and thrombosis. Lupus. 2010;19(4):460–469. doi: 10.1177/0961203310361485. [DOI] [PubMed] [Google Scholar]
- 30.Amoroso A, Mitterhofer AP, Del Porto F, et al. Antibodies to anionic phospholipids and anti-beta2-GPI: association with thrombosis and thrombocytopenia in systemic lupus erythematosus. Hum Immunol. 2003;64(2):265–273. doi: 10.1016/s0198-8859(02)00789-9. [DOI] [PubMed] [Google Scholar]
- 31.Atsumi T, Ieko M, Bertolaccini ML, Ichikawa K, Tsutsumi A, Matsuura E, Koike T. Association of autoantibodies against the phosphatidylserine-prothrombin complex with manifestations of the antiphospholipid syndrome and with the presence of lupus anticoagulant. Arthritis Rheum. 2000;43(9):1982–1993. doi: 10.1002/1529-0131(200009)43:9<1982::AID-ANR9>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 32.Tonello M, Mattia E, Favaro M, del Ross T, Calligaro A, Salvan E, Hoxha A, Fedrigo M, Ruffatti A. IgG phosphatidylserine/prothrombin antibodies as a risk factor of thrombosis in antiphospholipid antibody carriers. Thromb Res. 2019;177:157–160. doi: 10.1016/j.thromres.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 33.Nakamura H, Oku K, Amengual O, Ohmura K, Fujieda Y, Kato M, Bohgaki T, Yasuda S, Atsumi T. First-line, non-criterial antiphospholipid antibody testing for the diagnosis of antiphospholipid syndrome in clinical practice: a combination of anti-β(2) -glycoprotein I domain I and anti-phosphatidylserine/prothrombin complex antibodies tests. Arthritis Care Res. 2018;70(4):627–634. doi: 10.1002/acr.23310. [DOI] [PubMed] [Google Scholar]
- 34.Žigon P, Podovšovnik A, Ambrožič A, Tomšič M, Hočevar A, Gašperšič N, Rotar Ž, Praprotnik S, Šemrl SS, Čučnik S. Added value of non-criteria antiphospholipid antibodies for antiphospholipid syndrome: lessons learned from year-long routine measurements. Clin Rheumatol. 2019;38(2):371–378. doi: 10.1007/s10067-018-4251-7. [DOI] [PubMed] [Google Scholar]
- 35.Núñez-Álvarez CA, Hernández-Molina G, Bermúdez-Bermejo P, Zamora-Legoff V, Hernández-Ramírez DF, Olivares-Martínez E, Cabral AR. Prevalence and associations of anti-phosphatidylserine/prothrombin antibodies with clinical phenotypes in patients with primary antiphospholipid syndrome: aPS/PT antibodies in primary antiphospholipid syndrome. Thromb Res. 2019;174:141–147. doi: 10.1016/j.thromres.2018.12.023. [DOI] [PubMed] [Google Scholar]
- 36.Canti V, Del Rosso S, Tonello M, et al. Antiphosphatidylserine/prothrombin antibodies in antiphospholipid syndrome with intrauterine growth restriction and preeclampsia. J Rheumatol. 2018;45(9):1263–1272. doi: 10.3899/jrheum.170751. [DOI] [PubMed] [Google Scholar]
- 37.Sciascia S, Sanna G, Murru V, Roccatello D, Khamashta MA, Bertolaccini ML. GAPSS: the Global Anti-Phospholipid Syndrome Score. Rheumatology (Oxford) 2013;52(8):1397–1403. doi: 10.1093/rheumatology/kes388. [DOI] [PubMed] [Google Scholar]
- 38.Cervera R, Boffa MC, Khamashta MA, Hughes GRV. The Euro-Phospholipid project: epidemiology of the antiphospholipid syndrome in Europe. Lupus. 2009;18(10):889–893. doi: 10.1177/0961203309106832. [DOI] [PubMed] [Google Scholar]
- 39.Tektonidou MG, Varsou N, Kotoulas G, Antoniou A, Moutsopoulos HM. Cognitive deficits in patients with antiphospholipid syndrome: association with clinical, laboratory, and brain magnetic resonance imaging findings. Arch Intern Med. 2006;166(20):2278–2284. doi: 10.1001/archinte.166.20.2278. [DOI] [PubMed] [Google Scholar]
- 40.Trysberg E, Nylen K, Rosengren LE, Tarkowski A. Neuronal and astrocytic damage in systemic lupus erythematosus patients with central nervous system involvement. Arthritis Rheum. 2003;48(10):2881–2887. doi: 10.1002/art.11279. [DOI] [PubMed] [Google Scholar]
- 41.Erkan D, Barbhaiya M, George D, Sammaritano L, Lockshin M. Moderate versus high-titer persistently anticardiolipin antibody positive patients: are they clinically different and does high-titer anti-beta 2-glycoprotein-I antibody positivity offer additional predictive information? Lupus. 2010;19(5):613–619. doi: 10.1177/0961203309355300. [DOI] [PubMed] [Google Scholar]
- 42.Cervera R, Piette JC, Font J, Khamashta MA, Shoenfeld Y, Camps MT, Jacobsen S, Lakos G, Tincani A, Kontopoulou-Griva I, Galeazzi M, Meroni PL, Derksen RH, de Groot PG, Gromnica-Ihle E, Baleva M, Mosca M, Bombardieri S, Houssiau F, Gris JC, Quéré I, Hachulla E, Vasconcelos C, Roch B, Fernández-Nebro A, Boffa MC, Hughes GR, Ingelmo M, Euro-Phospholipid Project Group Antiphospholipid syndrome: clinical and immunologic manifestations and patterns of disease expression in a cohort of 1,000 patients. Arthritis Rheum. 2002;46(4):1019–1027. doi: 10.1002/art.10187. [DOI] [PubMed] [Google Scholar]
- 43.Andreoli L, Chighizola CB, Banzato A, Pons-Estel GJ, De Jesus GR, Erkan D. Estimated frequency of antiphospholipid antibodies in patients with pregnancy morbidity, stroke, myocardial infarction, and deep vein thrombosis: a critical review of the literature. Arthritis Care Res. 2013;65(11):1869–1873. doi: 10.1002/acr.22066. [DOI] [PubMed] [Google Scholar]
- 44.Gašperšič N, Zaletel M, Kobal J, Žigon P, Čučnik S, Šemrl SS, Tomšič M, Ambrožič A. Stroke and antiphospholipid syndrome—antiphospholipid antibodies are a risk factor for an ischemic cerebrovascular event. Clin Rheumatol. 2019;38(2):379–384. doi: 10.1007/s10067-018-4247-3. [DOI] [PubMed] [Google Scholar]
- 45.Babikian VL, Brey RL, Coull BM, et al. Clinical and laboratory findings in patients with antiphospholipid antibodies and cerebral ischemia. Stroke. 1990;21(9):1268–1273. doi: 10.1161/01.STR.21.9.1268. [DOI] [PubMed] [Google Scholar]
- 46.Fleetwood T, Cantello R, Comi C. Antiphospholipid syndrome and the neurologist: from pathogenesis to therapy. Front Neurol. 2018;9(NOV). doi:10.3389/fneur.2018.01001 [DOI] [PMC free article] [PubMed]
- 47.Hughes GRV. Migraine, memory loss, and “multiple sclerosis”. Neurological features of the antiphospholipid (Hughes’) syndrome. Postgrad Med J. 2003;79(928):81–83. doi: 10.1136/pmj.79.928.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sciascia S, Sanna G, Khamashta MA, Cuadrado MJ, Erkan D, Andreoli L, Bertolaccini ML, APS Action The estimated frequency of Antiphospholipid antibodies in young adults with cerebrovascular events: a systematic review. Ann Rheum Dis. 2015;74(11):2028–2033. doi: 10.1136/annrheumdis-2014-205663. [DOI] [PubMed] [Google Scholar]
- 49.Roldan JF, Brey RL. Neurologic Manifestations of the antiphospholipid syndrome. Curr Rheumatol Rep. 2007;9:109–115. doi: 10.1007/s11926-007-0004-3. [DOI] [PubMed] [Google Scholar]
- 50.Brey RL. Management of the neurological manifestations of APS - what do the trials tell us? Thromb Res. 2004;114(5-6 SPEC. ISS.):489-499. doi:10.1016/j.thromres.2004.06.018 [DOI] [PubMed]
- 51.Provenzale JM, Barboriak DP, Allen NB, Ortel TL. Antiphospholipid antibodies: findings at arteriography. Am J Neuroradiol. 1998;19(4):611–616. [PMC free article] [PubMed] [Google Scholar]
- 52.Ricarte IF, Dutra LA, Abrantes FF, Toso FF, Barsottini OGP, Silva GS, de Souza AWS, Andrade D. Neurologic manifestations of antiphospholipid syndrome. Lupus. 2018;27(9):1404–1414. doi: 10.1177/0961203318776110. [DOI] [PubMed] [Google Scholar]
- 53.De Amorim LCD, Maia FM, Rodrigues CEM. Stroke in systemic lupus erythematosus and antiphospholipid syndrome: risk factors, clinical manifestations, neuroimaging, and treatment. Lupus. 2017;26(5):529–536. doi: 10.1177/0961203316688784. [DOI] [PubMed] [Google Scholar]
- 54.Erdogan D, Goren MT, Diz-Kucukkaya R, Inanc M. Assessment of cardiac structure and left atrial appendage functions in primary antiphospholipid syndrome: a transesophageal echocardiographic study. Stroke. 2005;36(3):592–596. doi: 10.1161/01.STR.0000154858.27353.df. [DOI] [PubMed] [Google Scholar]
- 55.Koniari I, Siminelakis SN, Baikoussis NG, Papadopoulos G, Goudevenos J, Apostolakis E. Antiphospholipid syndrome; its implication in cardiovascular diseases: a review. J Cardiothorac Surg. 2010;5(1):101. doi: 10.1186/1749-8090-5-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Panichpisal K, Rozner E, Levine SR. The management of stroke in antiphospholipid syndrome. Curr Rheumatol Rep. 2012;14(1):99–106. doi: 10.1007/s11926-011-0223-5. [DOI] [PubMed] [Google Scholar]
- 57.Provenzale JM, Barboriak DP, Alen NB, Ortel TL. Patients with antiphospholipid antibodies: CT and MR findings of the brain. AJR. 1996;167:1573–1578. doi: 10.2214/ajr.167.6.8956600. [DOI] [PubMed] [Google Scholar]
- 58.Silvis SM, De Sousa DA, Ferro JM, Coutinho JM. Cerebral venous thrombosis. Nat Rev Neurol. 2017;13(9):555–565. doi: 10.1038/nrneurol.2017.104. [DOI] [PubMed] [Google Scholar]
- 59.Martinelli I, Battaglioli T, Pedotti P, Cattaneo M, Mannucci PM. Hyperhomocysteinemia in cerebral vein thrombosis. Blood. 2003;102(4):1363–1366. doi: 10.1182/blood-2003-02-0443. [DOI] [PubMed] [Google Scholar]
- 60.Christopher R, Nagaraja D, Dixit NS, Narayanan CP. Anticardiolipin antibodies: a study in cerebral venous thrombosis. Acta Neurol Scand. 1999;99(2):121–124. doi: 10.1111/j.1600-0404.1999.tb00669.x. [DOI] [PubMed] [Google Scholar]
- 61.Tsai CL, Hueng DY, Tsao WL, Lin JC. Cerebral venous sinus thrombosis as an initial manifestation of primary antiphospholipid syndrome. Am J Emerg Med. 2013;31(5):888.e1–888.e3. doi: 10.1016/j.ajem.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 62.Ferro JM, Bousser MG, Canhão P, Coutinho JM, Crassard I, Dentali F, di Minno M, Maino A, Martinelli I, Masuhr F, Aguiar de Sousa D, Stam J, the European Stroke Organization European Stroke Organization guideline for the diagnosis and treatment of cerebral venous thrombosis – endorsed by the European Academy of Neurology. Eur J Neurol. 2017;24(10):1203–1213. doi: 10.1111/ene.13381. [DOI] [PubMed] [Google Scholar]
- 63.Samanta D, Cobb S, Arya K. Sneddon syndrome: a comprehensive overview. J Stroke Cerebrovasc Dis. 2019;28(8):2098–2108. doi: 10.1016/j.jstrokecerebrovasdis.2019.05.013. [DOI] [PubMed] [Google Scholar]
- 64.Francès C, Papo T, Wechsler B, Laporte J-L, Biousse V, Piette J-C. Sneddon syndrome with or without antiphospholipid antibodies: a comparative study in 46 patients. Medicine (Baltimore) 1999;78(4):209–219. doi: 10.1097/00005792-199907000-00001. [DOI] [PubMed] [Google Scholar]
- 65.Wu S, Xu Z, Liang H. Sneddon’s syndrome: a comprehensive review of the literature. Orphanet J Rare Dis. 2014;9:215. doi: 10.1186/s13023-014-0215-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gupta S, Zivadinov R, Ramasamy D, Ambrus JL. Reversible cerebral vasoconstriction syndrome (RCVS) in antiphospholipid antibody syndrome (APLA): the role of centrally acting vasodilators. Case series and review of literature. Clin Rheumatol. 2014;33(12):1829–1833. doi: 10.1007/s10067-013-2434-9. [DOI] [PubMed] [Google Scholar]
- 67.Wang Z, Fu Z, Wang J, Cui H, Zhang Z, Zhang B. Moyamoya syndrome with antiphospholipid antibodies: a case report and literature review. Lupus. 2014;23(11):1204–1206. doi: 10.1177/0961203314540761. [DOI] [PubMed] [Google Scholar]
- 68.Krause I, Leibovici L, Blank M, Shoenfeld Y. Clusters of disease manifestations in patients with antiphospholipid syndrome demonstrated by factor analysis. Lupus. 2007;16(3):176–180. doi: 10.1177/0961203306075977. [DOI] [PubMed] [Google Scholar]
- 69.Shoenfeld Y, Lev S, Blatt I, Blank M, Font J, von Landenberg P, Lev N, Zaech J, Cervera R, Piette JC, Khamashta MA, Bertolaccini ML, Hughes GR, Youinou P, Meroni PL, Pengo V, Alves JD, Tincani A, Szegedi G, Lakos G, Sturfelt G, Jönsen A, Koike T, Sanmarco M, Ruffatti A, Ulcova-Gallova Z, Praprotnik S, Rozman B, Lorber M, Chapman J, van-Breda-Vriezman P, Damoiseaux J. Features associated with epilepsy in the antiphospholipid syndrome. J Rheumatol. 2004;31(7):1344–1348. [PubMed] [Google Scholar]
- 70.Arnson Y, Shoenfeld Y, Alon E, Amital H. The antiphospholipid syndrome as a neurological disease. Semin Arthritis Rheum. 2010;40(2):97–108. doi: 10.1016/j.semarthrit.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 71.De Carvalho JF, Pasoto SG, Appenzeller S. Seizures in primary antiphospholipid syndrome: the relevance of smoking to stroke. Clin Dev Immunol. 2012;2012:1–7. doi: 10.1155/2012/981519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Noureldine MHA, Harifi G, Berjawi A, et al. Hughes syndrome and epilepsy: when to test for antiphospholipid antibodies? Lupus. 2016;25(13):1397–1411. doi: 10.1177/0961203316651747. [DOI] [PubMed] [Google Scholar]
- 73.Yelnik CM, Kozora E, Appenzeller S. Non-stroke central neurologic manifestations in antiphospholipid syndrome. Curr Rheumatol Rep. 2016;18(2):1–9. doi: 10.1007/s11926-016-0568-x. [DOI] [PubMed] [Google Scholar]
- 74.Jacobson MW, Rapport LJ, Keenan PA, Coleman RD, Tietjen GE. Neuropsychological deficits associated with antiphospholipid antibodies. J Clin Exp Neuropsychol. 1999;21(2):251–264. doi: 10.1076/jcen.21.2.251.931. [DOI] [PubMed] [Google Scholar]
- 75.Coín MA, Vilar-López R, Peralta-Ramírez I, Hidalgo-Ruzzante N, Callejas-Rubio JL, Ortego-Centeno N, Pérez-García M. The role of antiphospholipid autoantibodies in the cognitive deficits of patients with systemic lupus erythematosus. Lupus. 2015;24(8):875–879. doi: 10.1177/0961203315572717. [DOI] [PubMed] [Google Scholar]
- 76.Erkan D, Barbhaiya M, George D, Sammaritano L, Lockshin M. Moderate versus high-titer persistently anticardiolipin antibody positive patients: are they clinically different and does high-titer anti- β2-glycoprotein-I antibody positivity offer additional predictive information? Lupus. 2010;19(5):613–619. doi: 10.1177/0961203309355300. [DOI] [PubMed] [Google Scholar]
- 77.Gómez-Puerta JA, Cervera R, Calvo LM, Gómez-Ansón B, Espinosa G, Claver G, Bucciarelli S, Bové A, Ramos-Casals M, Ingelmo M, Font J. Dementia associated with the antiphospholipid syndrome: clinical and radiological characteristics of 30 patients. Rheumatology. 2005;44(1):95–99. doi: 10.1093/rheumatology/keh408. [DOI] [PubMed] [Google Scholar]
- 78.Sanna G, Bertolaccini ML, Cuadrado MJ, Khamashta MA, Hughes GRV. Central nervous system involvement in the antiphospholipid (Hughes) syndrome. Rheumatology. 2003;42(2):200–213. doi: 10.1093/rheumatology/keg080. [DOI] [PubMed] [Google Scholar]
- 79.Erkan D, Vega J, Ramón G, Kozora E, Lockshin MD. A pilot open-label phase II trial of rituximab for non-criteria manifestations of antiphospholipid syndrome. Arthritis Rheum. 2013;65(2):464–471. doi: 10.1002/art.37759. [DOI] [PubMed] [Google Scholar]
- 80.Maes M, Meltzer H, Jacobs J, Suy E, Calabrese J, Minner B, Raus J. Autoimmunity in depression: increased antiphospholipid autoantibodies. Acta Psychiatr Scand. 1993;87(3):160–166. doi: 10.1111/j.1600-0447.1993.tb03349.x. [DOI] [PubMed] [Google Scholar]
- 81.Raza H, Epstein SA, Pao M, Rosenstein DL. Mania: psychiatric manifestations of the antiphospholipid syndrome. Psychosomatics. 2008;49(5):438–441. doi: 10.1176/appi.psy.49.5.438.Mania. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sokol DK, O’Brien RS, Wagenknecht DR, Rao T, McIntyre JA. Antiphospholipid antibodies in blood and cerebrospinal fluids of patients with psychosis. J Neuroimmunol. 2007;190(1-2):151–156. doi: 10.1016/j.jneuroim.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 83.Graf J. Central nervous system manifestations of antiphospholipid syndrome. Rheum Dis Clin N Am. 2017;43(4):547–560. doi: 10.1016/j.rdc.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 84.Gris JC, Cyprien F, Bouvier S, Cochery-Nouvellon E, Lavigne-Lissalde G, Mercier E, Balducchi JP. Antiphospholipid antibodies are associated with positive screening for common mental disorders in women with previous pregnancy loss. The NOHA-PSY observational study. World J Biol Psychiatry. 2019;20(1):51–63. doi: 10.1080/15622975.2017.1333146. [DOI] [PubMed] [Google Scholar]
- 85.Briley DP, Coull BM, Goodnight SH. Neurological disease associated with antiphospholipid antibodies. Ann Neurol. 1989;25(3):221–227. doi: 10.1002/ana.410250303. [DOI] [PubMed] [Google Scholar]
- 86.Cavestro C, Micca G, Molinari F, et al. Migraineurs show a high prevalence of antiphospholipid antibodies. J Thromb Haemost. 2011;9(7):1350–1354. doi: 10.1111/j.1538-7836.2011.04348.x. [DOI] [PubMed] [Google Scholar]
- 87.Schürks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T. Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ. 2009;339(7728):1015. doi: 10.1136/bmj.b3914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Islam MA, Alam F, Wong KK. Comorbid association of antiphospholipid antibodies and migraine: a systematic review and meta-analysis. Autoimmun Rev. 2017;16(5):512–522. doi: 10.1016/j.autrev.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 89.Silvestrini M, Cupini LM, Matteis M, De Simone R, Bernardi G. Migraine in patients with stroke and antiphospholipid antibodies. Headache J Head Face Pain. 1993;33(8):421–426. doi: 10.1111/j.1526-4610.1993.hed3308421.x. [DOI] [PubMed] [Google Scholar]
- 90.Pezzini A, Grassi M, Lodigiani C, Patella R, Gandolfo C, Zini A, Delodovici ML, Paciaroni M, del Sette M, Toriello A, Musolino R, Calabrò RS, Bovi P, Adami A, Silvestrelli G, Sessa M, Cavallini A, Marcheselli S, Bonifati DM, Checcarelli N, Tancredi L, Chiti A, del Zotto E, Spalloni A, Giossi A, Volonghi I, Costa P, Giacalone G, Ferrazzi P, Poli L, Morotti A, Rasura M, Simone AM, Gamba M, Cerrato P, Micieli G, Melis M, Massucco D, de Giuli V, Iacoviello L, Padovani A, Italian Project on Stroke in Young Adults (IPSYS) Investigators Predictors of long-term recurrent vascular events after ischemic stroke at young age: the Italian project on stroke in young adults. Circulation. 2014;129(16):1668–1676. doi: 10.1161/CIRCULATIONAHA.113.005663. [DOI] [PubMed] [Google Scholar]
- 91.• Cavestro C, Degan D, Micca G, et al. Thrombophilic alterations, migraine, and vascular disease: results from a case-control study. Neurol Sci. 2021. 10.1007/s10072-020-05006-zA recent case-control study on the association between migraine, thrombophilic conditions, and vascular events. [DOI] [PubMed]
- 92.Mawet J, Kurth T, Ayata C. Migraine and stroke: in search of shared mechanisms. Cephalalgia. 2015;35(2):165–181. doi: 10.1177/0333102414550106. [DOI] [PubMed] [Google Scholar]
- 93.• Schofield JR, Hughes HN, Birlea M, Hassell KL. A trial of antithrombotic therapy in patients with refractory migraine and antiphospholipid antibodies: a retrospective study of 75 patients. Lupus. 2021. 10.1177/0961203320983913A retrospective study of 75 patients with refractory migraine and aPL who were given a 2–4-week trial of antiplatelets or anticoagulation showed a high rate of symptomatic response to antithrombotic therapy and a low bleeding risk on long-term follow-up. [DOI] [PubMed]
- 94.•• D’Angelo C, Franch O, Fernández-Paredes L, et al. Antiphospholipid antibodies overlapping in isolated neurological syndrome and multiple sclerosis: neurobiological insights and diagnostic challenges. Front Cell Neurosci. 2019;13. 10.3389/fncel.2019.00107An insightfully written review on the pathophysiological mechanisms of neuroimmune disorders associated with APS, with a particular focus on multiple sclerosis. [DOI] [PMC free article] [PubMed]
- 95.Ijdo JW, Conti-Kelly AM, Greco P, et al. Anti-phospholipid antibodies in patients with multiple sclerosis and MS-like illnesses: MS or APS? Lupus. 1999;8:109–115. doi: 10.1191/096120399678847461. [DOI] [PubMed] [Google Scholar]
- 96.Cuadrado MJ, Khamashta MA, Ballesteros A, Godfrey T, Simon MJ, Hughes G. Can Neurologic manifestations of Hughes (antiphospholipid) syndrome be distinguished from multiple sclerosis. Medicine (Baltimore) 2000;79:57–68. doi: 10.1097/00005792-200001000-00006. [DOI] [PubMed] [Google Scholar]
- 97.Uthman I, Noureldine MHA, Berjawi A, Skaf M, Haydar AA, Merashli M, Hughes GRV. Hughes syndrome and multiple sclerosis. Lupus. 2015;24(2):115–121. doi: 10.1177/0961203314555539. [DOI] [PubMed] [Google Scholar]
- 98.Renaud M, Aupy J, Uring-Lambert B, Chanson JB, Collongues N, Blanc F, de Sèze J. Isolated anti-β2-glycoprotein I antibodies in neurology: a frontier syndrome between multiple sclerosis and antiphospholipid syndrome? Eur J Neurol. 2014;21(6):901–906. doi: 10.1111/ene.12408. [DOI] [PubMed] [Google Scholar]
- 99.Bidot CJ, Horstman LL, Jy W, Jimenez JJ, Bidot C Jr, Ahn YS, et al. Clinical and neuroimaging correlates of antiphospholipid antibodies in multiple sclerosis: a preliminary study. BMC Neurol. 2007;7. 10.1186/1471-2377-7-36. [DOI] [PMC free article] [PubMed]
- 100.Garg N, Zivadinov R, Ramanathan M, Vasiliu I, Locke J, Watts K, Lema J, Rajeswary J, Munschauer FE, Ambrus J, Jr, Weinstock-Guttman B. Clinical and MRI correlates of autoreactive antibodies in multiple sclerosis patients. J Neuroimmunol. 2007;187(1-2):159–165. doi: 10.1016/j.jneuroim.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 101.Filippidou N, Krashias G, Pericleous C, Rahman A, Ioannou Y, Giles I, Demetriou C, Anatolitou A, Christodoulou C, Pantzaris M, Lambrianides A. The association between IgG and IgM antibodies against cardiolipin, β2-glycoprotein I and domain I of β2-glycoprotein I with disease profile in patients with multiple sclerosis. Mol Immunol. 2016;75:161–167. doi: 10.1016/j.molimm.2016.05.022. [DOI] [PubMed] [Google Scholar]
- 102.Collard RC, Koehler RP, Mattson DH. Frequency and significance of antinuclear antibodies in multiple sclerosis.; 1997. [DOI] [PubMed]
- 103.Tourbah A, Clapin A, Gout O, et al. Systemic autoimmune features and multiple sclerosis a 5-year follow-up study. http://archneur.jamanetwork.com/. [DOI] [PubMed]
- 104.Filippidou N, Krashias G, Christodoulou C, Pantzaris M, Lambrianides A. Mechanisms of activation induced by antiphospholipid antibodies in multiple sclerosis: Potential biomarkers of disease? J Immunol Methods. 2019;474:112663. doi: 10.1016/j.jim.2019.112663. [DOI] [PubMed] [Google Scholar]
- 105.Stosic M, Ambrus J, Garg N, Weinstock-Guttman B, Ramanathan M, Kalman B, Minagar A, Munschauer FE, Galey TM, Hussein S, Bakshi R, Zivadinov R. MRI characteristics of patients with antiphospholipid syndrome and multiple sclerosis. J Neurol. 2010;257(1):63–71. doi: 10.1007/s00415-009-5264-6. [DOI] [PubMed] [Google Scholar]
- 106.Rovaris M, Viti B, Ciboddo G, Gerevini S, Capra R, Iannucci G, Comi G, Filippi M. Brain involvement in systemic immune mediated diseases: magnetic resonance and magnetisation transfer imaging study. J Neurol Neurosurg Psychiatry. 2000;68:170–177. doi: 10.1136/jnnp.68.2.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ferreira S, D’Cruz DP, Hughes GRV. Multiple sclerosis, neuropsychiatric lupus and antiphospholipid syndrome: Where do we stand? Rheumatology. 2005;44(4):434–442. doi: 10.1093/rheumatology/keh532. [DOI] [PubMed] [Google Scholar]
- 108.Sastre-Garriga J, Reverter J c, Font J, Tintoré M, Espinosa G, Montalban X. Anticardiolipin antibodies are not a useful screening tool in a nonselected large group of patients with multiple sclerosis. Ann Neurol. 2001;49:408–411. doi: 10.1002/ana.81. [DOI] [PubMed] [Google Scholar]
- 109.Kavaliunas A, Manouchehrinia A, Stawiarz L, Ramanujam R, Agholme J, Hedström AK, Beiki O, Glaser A, Hillert J. Importance of early treatment initiation in the clinical course of multiple sclerosis. Mult Scler. 2017;23(9):1233–1240. doi: 10.1177/1352458516675039. [DOI] [PubMed] [Google Scholar]
- 110.Jarius S, Paul F, Weinshenker BG, Levy M, Kim HJ, Wildemann B. Neuromyelitis optica. Nat Rev Dis Prim. 2020;6(1). 10.1038/s41572-020-0214-9. [DOI] [PubMed]
- 111.Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, de Seze J, Fujihara K, Greenberg B, Jacob A, Jarius S, Lana-Peixoto M, Levy M, Simon JH, Tenembaum S, Traboulsee AL, Waters P, Wellik KE, Weinshenker BG, International Panel for NMO Diagnosis International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015;85(2):177–189. doi: 10.1212/WNL.0000000000001729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Iyer A, Elsone L, Appleton R, Jacob A. A review of the current literature and a guide to the early diagnosis of autoimmune disorders associated with neuromyelitis optica. Autoimmunity. 2014;47(3):154–161. doi: 10.3109/08916934.2014.883501. [DOI] [PubMed] [Google Scholar]
- 113.Wingerchuk DM, Weinshenker BG. The emerging relationship between neuromyelitis optica and systemic rheumatologic autoimmune disease. Mult Scler J. 2012;18(1):5–10. doi: 10.1177/1352458511431077. [DOI] [PubMed] [Google Scholar]
- 114.Lee EJ, Lim YM, Kim SY, Lee JK, Kim H, Jin JY, Oh YJ, Kim KK. The clinical and prognostic value of antinuclear antibodies in NMO-IgG seropositive neuromyelitis optica spectrum disorder. J Neuroimmunol. 2019;328:1–4. doi: 10.1016/j.jneuroim.2018.11.012. [DOI] [PubMed] [Google Scholar]
- 115.Long Y, He Y, Zheng Y, Chen M, Zhang B, Gao C. Serum anticardiolipin antibodies in patients with neuromyelitis optica spectrum disorder. J Neurol. 2013;260(12):3150–3157. doi: 10.1007/s00415-013-7128-3. [DOI] [PubMed] [Google Scholar]
- 116.Guerra H, Pittock SJ, Moder KG, Froehling DA, Flanagan EP. Neuromyelitis optica spectrum initially diagnosed as antiphospholipid antibody myelitis. J Neurol Sci. 2016;361:204–205. doi: 10.1016/j.jns.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 117.Margoni M, Carotenuto A. Very late-onset recurrent myelitis in a patient diagnosed with antiphospholipid syndrome: a puzzle of autoimmunity. J Neuroimmunol. 2019;337:577051. doi: 10.1016/j.jneuroim.2019.577051. [DOI] [PubMed] [Google Scholar]
- 118.Sherer Y, Hassin S, Shoenfeld Y, et al. Transverse myelitis in patients with antiphospholipid antibodies-the importance of early diagnosis and treatment. [DOI] [PubMed]
- 119.Rodrigues CEM, de Carvalho JF. Clinical, radiologic, and therapeutic analysis of 14 patients with transverse myelitis associated with antiphospholipid syndrome: report of 4 cases and review of the literature. Semin Arthritis Rheum. 2011;40(4):349–357. doi: 10.1016/j.semarthrit.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 120.Peluso S, Antenora A, De Rosa A, et al. Antiphospholipid-related chorea. Front Neurol. 2012:1–8. 10.3389/fneur.2012.00150. [DOI] [PMC free article] [PubMed]
- 121.Cervera R, Asherson RA, Font J, Tikly M, Pallarés L, Chamorro A, Ingelmo M. Chorea in the antiphospholipid syndrome: clinical, radiologic, and immunologic characteristics of 50 patients from our clinics and the recent literature. Med. 1997;76(3):203–212. doi: 10.1097/00005792-199705000-00006. [DOI] [PubMed] [Google Scholar]
- 122.Safarpour D, Buckingham S, Jabbari B. Chorea associated with high titers of antiphospholipid antibodies in the absence of antiphospholipid antibody syndrome. Tremor and Other Hyperkinetic Movements. 2015;5(0):294. doi: 10.5334/tohm.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhang L, Pereira AC. Oromandibular chorea in antiphospholipid syndrome. Pract Neurol. 2018;18(2):132–133. doi: 10.1136/practneurol-2017-001824. [DOI] [PubMed] [Google Scholar]
- 124.Huang YC, Lyu RK, Chen ST, Chu YC, Wu YR. Parkinsonism in a patient with antiphospholipid syndrome - case report and literature review. J Neurol Sci. 2008;267(1-2):166–169. doi: 10.1016/j.jns.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 125.Carecchio M, Comi C, Varrasi C, Stecco A, Sainaghi PP, Bhatia K, Carriero A, Cantello R, Monaco F. Complex movement disorders in primary antiphospholipid syndrome: a case report. J Neurol Sci. 2009;281(1-2):101–103. doi: 10.1016/j.jns.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 126.Chen WH, Chen CH, Chui C, Lui CC, Chen CJ, Yin HL. Antiphospholipid antibodies and cerebellar ataxia: a clinical analysis and literature review. Neuroimmunomodulation. 2014;21(6):283–290. doi: 10.1159/000354614. [DOI] [PubMed] [Google Scholar]
- 127.Ishikawa N, Kobayashi M. Recurrent acute cerebellar ataxia associated with anti-cardiolipin antibodies. Brain and Development. 2010;32(7):588–591. doi: 10.1016/j.braindev.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 128.Jeruc J. Multiple mononeuropathy due to vasculitis associated with anticardiolipin antibodies: a case report. Vol 44.; 2006. [PubMed]
- 129.Nakos G, Tziakou E, Maneta-Peyret L, Nassis C, Lekka ME. Anti-phospholipid antibodies in serum from patients with Guillain-Barré syndrome. Intensive Care Med. 2005;31(10):1401–1408. doi: 10.1007/s00134-005-2736-8. [DOI] [PubMed] [Google Scholar]
- 130.Gilburd B, Stein M, Tomer Y, Tanne D, Abramski O, Chapman Y, Ahiron A, Blank M, Shoenfeld Y. Autoantibodies to phospholipids and brain extract in patients with the guillain-barre syndrome: cross-reactive or pathogenic? Autoimmunity. 1993;16:23–44. doi: 10.3109/08916939309010644. [DOI] [PubMed] [Google Scholar]
- 131.Santos MSF, De Carvalho JF, Brotto M, Bonfa E, Rocha FAC. Peripheral neuropathy in patients with primary antiphospholipid (Hughes) syndrome. Lupus. 2010;19(5):583–590. doi: 10.1177/0961203309354541. [DOI] [PubMed] [Google Scholar]
- 132.Schofield JR. Autonomic neuropathy—in its many guises—as the initial manifestation of the antiphospholipid syndrome. Immunol Res. 2017;65(2):532–542. doi: 10.1007/s12026-016-8889-4. [DOI] [PubMed] [Google Scholar]
- 133.Tektonidou MG, Andreoli L, Limper M, Amoura Z, Cervera R, Costedoat-Chalumeau N, Cuadrado MJ, Dörner T, Ferrer-Oliveras R, Hambly K, Khamashta MA, King J, Marchiori F, Meroni PL, Mosca M, Pengo V, Raio L, Ruiz-Irastorza G, Shoenfeld Y, Stojanovich L, Svenungsson E, Wahl D, Tincani A, Ward MM. EULAR recommendations for the management of antiphospholipid syndrome in adults. Ann Rheum Dis. 2019;78(10):1296–1304. doi: 10.1136/annrheumdis-2019-215213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Arnaud L, Mathian A, Ruffatti A, Erkan D, Tektonidou M, Cervera R, Forastiero R, Pengo V, Lambert M, Martinez-Zamora MA, Balasch J, Zuily S, Wahl D, Amoura Z. Efficacy of aspirin for the primary prevention of thrombosis in patients with antiphospholipid antibodies: an international and collaborative meta-analysis. Autoimmun Rev. 2014;13(3):281–291. doi: 10.1016/j.autrev.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 135.Cohen H, Hunt BJ, Efthymiou M, et al. Rivaroxaban versus warfarin to treat patients with thrombotic antiphospholipid syndrome, with or without systemic lupus erythematosus (RAPS): a randomised, controlled, open-label, phase 2/3, non-inferiority trial. Lancet Haematol. 2016;3(9):e426–e436. doi: 10.1016/S2352-3026(16)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Pengo V, Denas G, Zoppellaro G, et al. Rivaroxaban vs warfarin in high-risk patients with antiphospholipid syndrome. Blood. 2018;132(13):1365–1371. doi: 10.1182/blood-2018-04-848333. [DOI] [PubMed] [Google Scholar]
- 137.Bala MM, Celinska-Lowenhoff M, Szot W, et al. Antiplatelet and anticoagulant agents for secondary prevention of stroke and other thromboembolic events in people with antiphospholipid syndrome. Cochrane Database Syst Rev. 2020;2020(10). 10.1002/14651858.CD012169.pub3. [DOI] [PMC free article] [PubMed]
- 138.Pengo V, Denas G, Zoppellaro G, Jose SP, Hoxha A, Ruffatti A, Andreoli L, Tincani A, Cenci C, Prisco D, Fierro T, Gresele P, Cafolla A, de Micheli V, Ghirarduzzi A, Tosetto A, Falanga A, Martinelli I, Testa S, Barcellona D, Gerosa M, Banzato A. Rivaroxaban vs warfarin in high-risk patients with antiphospholipid syndrome. Blood. 2018;132(13):1365–1371. doi: 10.1182/blood-2018-04-848333. [DOI] [PubMed] [Google Scholar]
- 139.Woller SC, Stevens SM, Kaplan DA, et al. Apixaban for the secondary prevention of thrombosis among patients with antiphospholipid syndrome: study rationale and design (ASTRO-APS) Clin Appl Thromb Off J Int Acad Clin Appl Thromb. 2016;22(3):239–247. doi: 10.1177/1076029615615960. [DOI] [PubMed] [Google Scholar]
- 140.Woller S, Stevens S, Kaplan D, Rondina M. Protocol modification of apixaban for the secondary prevention of thrombosis among patients with antiphospholipid syndrome study. Clin Appl Thromb. 2017;24:107602961772921. doi: 10.1177/1076029617729214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Fazili M, Stevens SM, Woller SC. Direct oral anticoagulants in antiphospholipid syndrome with venous thromboembolism: Impact of the European Medicines Agency guidance. Res Pract Thromb Haemost. 2020;4(1):9–12. doi: 10.1002/rth2.12287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Andreoli L, Bertsias GK, Agmon-Levin N, Brown S, Cervera R, Costedoat-Chalumeau N, Doria A, Fischer-Betz R, Forger F, Moraes-Fontes MF, Khamashta M, King J, Lojacono A, Marchiori F, Meroni PL, Mosca M, Motta M, Ostensen M, Pamfil C, Raio L, Schneider M, Svenungsson E, Tektonidou M, Yavuz S, Boumpas D, Tincani A. EULAR recommendations for women’s health and the management of family planning, assisted reproduction, pregnancy and menopause in patients with systemic lupus erythematosus and/or antiphospholipid syndrome. Ann Rheum Dis. 2017;76(3):476–485. doi: 10.1136/annrheumdis-2016-209770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sammaritano LR, Bermas BL, Chakravarty EE, Chambers C, Clowse MEB, Lockshin MD, Marder W, Guyatt G, Branch DW, Buyon J, Christopher-Stine L, Crow-Hercher R, Cush J, Druzin M, Kavanaugh A, Laskin CA, Plante L, Salmon J, Simard J, Somers EC, Steen V, Tedeschi SK, Vinet E, White CW, Yazdany J, Barbhaiya M, Bettendorf B, Eudy A, Jayatilleke A, Shah AA, Sullivan N, Tarter LL, Birru Talabi M, Turgunbaev M, Turner A, D'Anci KE. 2020 American College of Rheumatology Guideline for the management of reproductive health in rheumatic and musculoskeletal diseases. Arthritis Care Res. 2020;72(4):461–488. doi: 10.1002/acr.24130. [DOI] [PubMed] [Google Scholar]
- 144.Legault K, Schunemann H, Hillis C, Yeung C, Akl EA, Carrier M, Cervera R, Crowther M, Dentali F, Erkan D, Espinosa G, Khamashta M, Meerpohl JJ, Moffat K, O'Brien S, Pengo V, Rand JH, Rodriguez Pinto I, Thom L, Iorio A. McMaster RARE-Bestpractices clinical practice guideline on diagnosis and management of the catastrophic antiphospholipid syndrome. J Thromb Haemost. 2018;16:1656–1664. doi: 10.1111/jth.14192. [DOI] [PubMed] [Google Scholar]
- 145.Helms J, Tacquard C, Severac F, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46(6):1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan. China JAMA Neurol. 2020;77(6):683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Beyrouti R, Adams ME, Benjamin L, Cohen H, Farmer SF, Goh YY, Humphries F, Jäger HR, Losseff NA, Perry RJ, Shah S, Simister RJ, Turner D, Chandratheva A, Werring DJ. Characteristics of ischaemic stroke associated with COVID-19. J Neurol Neurosurg Psychiatry. 2020;91(8):889–891. doi: 10.1136/jnnp-2020-323586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Baldini T, Asioli G, Romoli M, et al. Cerebral venous thrombosis and severe acute respiratory syndrome coronavirus-2 infection: a systematic review and meta-analysis. Eur J Neurol. 2021. 10.1111/ene.14727. [DOI] [PMC free article] [PubMed]
- 149.Harzallah I, Debliquis A, Drénou B. Lupus anticoagulant is frequent in patients with Covid-19. J Thromb Haemost. 2020;18(8):2064–2065. doi: 10.1111/jth.14867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Siguret V, Voicu S, Neuwirth M, et al. Are antiphospholipid antibodies associated with thrombotic complications in critically ill COVID-19 patients? Thromb Res. 2020;195:74–76. doi: 10.1016/j.thromres.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Abdel-Wahab N, Talathi S, Lopez-Olivo MA, Suarez-Almazor ME. Risk of developing antiphospholipid antibodies following viral infection: a systematic review and meta-analysis. Lupus. 2018;27(4):572–583. doi: 10.1177/0961203317731532. [DOI] [PubMed] [Google Scholar]
- 152.Schouwers SME, Delanghe JR, Devreese KMJ. Lupus Anticoagulant (LAC) testing in patients with inflammatory status: does C-reactive protein interfere with LAC test results? Thromb Res. 2010;125(1):102–104. doi: 10.1016/j.thromres.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 153.Olsen NJ, Schleich MA, Karp DR. Multifaceted effects of hydroxychloroquine in human disease. Semin Arthritis Rheum. 2013;43(2):264–272. doi: 10.1016/j.semarthrit.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 154.Borghi MO, Beltagy A, Garrafa E, Curreli D, Cecchini G, Bodio C, Grossi C, Blengino S, Tincani A, Franceschini F, Andreoli L, Lazzaroni MG, Piantoni S, Masneri S, Crisafulli F, Brugnoni D, Muiesan ML, Salvetti M, Parati G, Torresani E, Mahler M, Heilbron F, Pregnolato F, Pengo M, Tedesco F, Pozzi N, Meroni PL. Anti-phospholipid antibodies in COVID-19 are different from those detectable in the anti-phospholipid syndrome. Front Immunol. 2020;11:584241. doi: 10.3389/fimmu.2020.584241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Gatto M, Perricone C, Tonello M, Bistoni O, Cattelan AM, Bursi R, Cafaro G, de Robertis E, Mencacci A, Bozza S, Vianello A, Iaccarino L, Gerli R, Doria A, Bartoloni E. Frequency and clinical correlates of antiphospholipid antibodies arising in patients with SARS-CoV-2 infection: findings from a multicentre study on 122 cases. Clin Exp Rheumatol. 2020;38(4):754–759. [PubMed] [Google Scholar]


