Abstract
COVID-19 is an ongoing pandemic and an intermediate analysis of the first 300 cases treated in the Infectious Diseases Clinic from Craiova has been performed. We have found that most of the cases were asymptomatic or mild, but the severity of the symptomatic cases increases with age. The main comorbidities associated mainly with the severe cases were high blood pressure, obesity, other cardiac conditions, diabetes mellitus and malignancies. Inflammation, coagulation and metabolic disorders are significantly more expressed in critically ill patients. Fatality rate is relatively low, death seems to be associated with old age.
Keywords: SARS CoV2, COVID-19, intermediate analysis
Introduction
A cluster of “viral pneumonia” has been recognized in late December 2020 in Wuhan city, Hubei province, Popular Republic of China.
Infection due to the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS CoV2)-later named Coronavirus Infectious Disease 2019 (COVID-19)-has soon spread around the globe.
World Health Organization (WHO) first declared the infection “an international public health emergency” on January 30, 2020, then “a pandemic” on March 11.
On March 7, 2021 there are more than 115 million people infected and more than 2.5 million deaths [1,2].
Romania reported the first case on February 21; until March 6 there are 824995 cases and 20854 deaths [3].
First case diagnosed in the Infectious Diseases Clinic from Craiova was recorded on March 6; until now we have treated more than 5900 patients.
We have performed an intermediate analysis of the first 300 cases admitted in our clinic, highlighting the epidemiological, clinical and evolutive aspects.
Materials and Method
This is a retrospective study (March-July 2020) based on information from the patient transcripts, downloaded into a database.
Epidemiological, clinical and evolutive aspects were noted.
The statistical analysis is based on Chi2 tests (two tails, with Yates’s correction), unpaired t test (Student) and one-way ANOVA with post-hoc Tukey HSD test, the statistical significance being recorded for p<0.05.
The diagnosis of COVID-19 was established following a positive result of a real-time polymerase chain reaction (RT PCR) test for SARS CoV2.
All patients have signed a consent for allowing the use of their personal data.
The study has been approved by the Ethics Committee of the “Victor Babes” Hospital.
Results
We have recorded 89 (29.66%) asymptomatic, 122 (40.66%) mild, 56 (18.66) moderate and 33 (11%) severe cases.
Average age was 40±17.5 years, most patients being adults (274, 91.33%).
Figure 1 shows the average age and standard deviation for each clinical form taken into consideration; there is a statistical difference between data registered for asymptomatic cases (37.22±13.51 years), mild (27.5±19.54 years), moderate (44.5±13.03 year) and severe forms of COVID-19 (63±10.12 years), p<0.0001 (one-way ANOVA).
Figure 1.
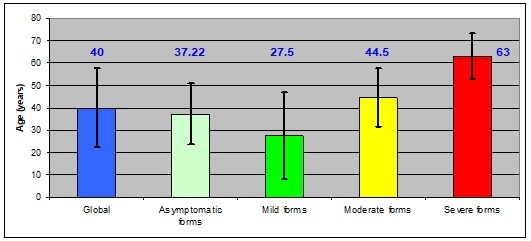
Average age for all cases and for each clinical from taken into consideration
Gender ratio was 167 (males)/133 (females). Most patients were from urban settings (233, 77.66%) and from Dolj county (262, 87.33%).
The peak of this “first wave” was during April and May (97 and 90 cases, respectively).
152 (50.67%) subjects had a previous contact with a confirmed COVID-19 case and 59 (19.67%) have recently returned from abroad (mainly from Italy-8, and Great Britain-2 patients).
We have recorded 4 epidemiological clusters (28, 20, 13 and 9 cases, respectively); 29 subjects were from the medical staff of various departments [4].
Data regarding the personal history of the patients are shown in table 1; when comparing all data with that from the severe forms of COVID-19, there are statistically significant differences for high blood pressure (p=0.026), obesity (p=0.0005), other cardiac conditions (p<0.0001), diabetes mellitus (p<0.0001) and malignancies (p<0.0001).
Table 1.
Data regarding the personal history of the patients
|
|
Global |
Asymptomatic forms |
Mild forms |
Moderate forms |
Severe forms |
|
High blood pressure |
100 |
28 |
34 |
20 |
18 |
|
Obesity |
48 |
10 |
12 |
12 |
14 |
|
Other heart conditions |
41 |
9 |
6 |
8 |
18 |
|
Diabetes mellitus |
29 |
2 |
3 |
9 |
15 |
|
Malignancies |
11 |
1 |
1 |
2 |
7 |
|
Chronic respiratory conditions |
10 |
0 |
1 |
3 |
6 |
|
Chronic kidney disease |
7 |
0 |
6 |
1 |
0 |
|
Tuberculosis |
1 |
0 |
1 |
0 |
0 |
|
HIV infection |
1 |
0 |
1 |
0 |
0 |
The main complaints of the patients when admitted into the hospital are shown in Figure 2. No statistical differences were noticed between the clinical forms of the disease.
Figure 2.
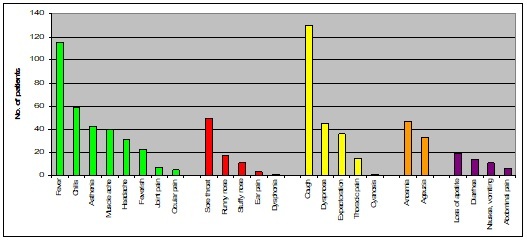
Main complaints of the patients from the study group; legend: green-general symptoms, red-upper respiratory tract infection symptoms, yellow-lower respiratory tract symptoms, orange-neurologic symptoms, purple-digestive symptoms
Most physical findings do not differentiate between clinical forms, except for dyspnea, cyanosis, oxygen saturation below 90%, coma or necessity for intubation, commonly encountered and defining for the severe form of infection due to SARS CoV2. After hospital admission, the newly emerged symptoms are shown in Figure 3.
Figure 3.
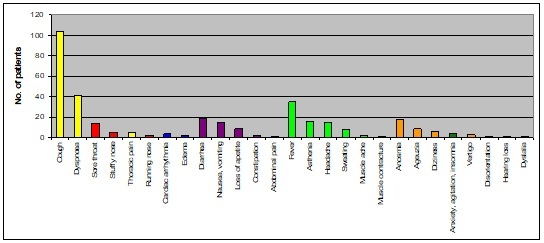
Newly recognized symptoms after hospital admission; legend: green-general symptoms, red-upper respiratory tract infection symptoms, yellow-lower respiratory tract symptoms, orange-neurologic symptoms, purple-digestive symptoms, blue-cardiologic symptoms, dark green-psychiatric symptoms
Overall, the laboratory data show (average): leukocyte number 7003.35±3116.41/ cubic millimeter (mm3), erythrocytes sedimentation rate/1 hour (1h) 25.46±28.49 millimeter (mm), blood glucose 123.2±56.3 milligram per deciliter (mg/dL), serum lactate 1.68±0.39 milliequivalent per liter (mEq/L), troponin 13.11±20.59 micrograms per liter (µg/L; number of tests, n=27), D dimers 753.39±980.6 micrograms per milliliter (µg/mL; n=55).
By comparison the following values (on average) were noted for severe cases: leukocyte number 8666.67±4565.88/mm3 (p=0.006), erythrocytes sedimentation rate (1h) 43.05±28.9mm (p=0.0008), blood glucose 304.45±273.58mg/dL (p<0.0001), serum lactate 3.47±3.84mEq/L (p<0.0001), troponin 90.81±202.08µg/L (n=5, p=0.04), D dimers 1314.22±1347.54µg/mL (n=23, p=0.04).
As regarding the blood glucose, the number of patients with values above 120mg/dL vas 47 in total, but 24 of them have severe form of COVID-19 (p<0.0001).
No statistically significant differences were noted for the laboratory data in asymptomatic, mild or moderate forms of COVID-19.
Table 2 summarizes the aspects of lung imaging (all vs. critical cases).
Table 2.
Data on lung imaging of patients; legend: NS=not statistically significant
|
Chest X ray aspects |
Global |
Critical forms |
p |
|
normal lung imagery |
158 |
2 |
<0.0001 |
|
consolidation |
62 |
18 |
<0.0001 |
|
interstitial aspect |
50 |
3 |
NS |
|
"ground-glass" opacities |
21 |
6 |
0.057 |
|
bronchopneumonia |
5 |
3 |
0.04 |
|
pleural effusion |
3 |
0 |
NS |
|
abscesses |
1 |
1 |
NS |
Patients have been treated according to the national guidelines and the following antiviral regimens have been used: Lopinavir/Ritonavir, 200/50 milligrams (mg)/capsule, 2 capsules every 12 hours, 7-10 days-39 patients, Hydroxychloroquine, 200mg/pill, 800mg for the first day, then 400mg/day for another 4 days-57 cases, combination of Hydroxychloroquine and Lopinavir/Ritonavir-42 cases and Remdesivir, 100mg/vial, 200mg intravenously for the first day, then 100mg for another 4 days-1 case.
All patients with moderate and severe forms received steroids (Dexamethasone, vials, 8 mg/day intravenously, 10 days) and anticoagulant therapy (Enoxaparin, prefilled syringe, 4 to 6 milliliters subcutaneously, once or twice a day, depending on the patient’s body weight, throughout the hospitalization).
The median length of hospital stay was 13 days [limits between 2 and 35 days].
The results of hospitalization is shown in Figure 4.
Figure 4.
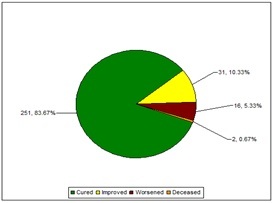
Result of hospitalization
All 16 patients with worsen condition have been transferred to another clinic, but unfortunately 14 of them died; thus, the mortality ratio was 5.33%.
The average age of deceased patients was 72.33±7.57 years (p<0.0001 as compared with average age of all cases).
Discussion
Most of our cases were asymptomatic or mild form of COVID-19 and, fortunately, only 11% of cases were severe, with a fatality ratio of 5.33% which, at that time, was in accordance with the data from the medical literature [5,6,7,8,9,10].
The age of the patients seems to be the most important factor influencing the severity of the disease and death; it should be noted that there are a 13 years difference between the average age of the patients diagnosed with moderate and severe forms and 10 years difference between the average age of patients with severe forms and those who died.
We did not register severe forms in our pediatric patients, however they represented only a minority of the total cases.
Globally there is only a small predominance of males versus female patients (M vs. F ratio=1.25) and the ratio increases for moderate (2.29) and severe forms respectively (1.75), however without statistical significance, probably due to the small number of patients taken into account.
A similar result is shown in the medical literature [5,6,7,8].
Our patients had multiple comorbidities and, as expected due to the increased age of the patients, most of them were detected in severe cases. Similar results were published on this matter [5,6,7,8,9,10], raising the question of their impact on COVID-19 evolution.
Indeed, these sufferings are among the most common causes of morbidity and mortality around the globe [11], however there are a series of data showing that they may contribute to the worsening of the infection due to the novel coronavirus and, possibly, to the death of the patients [12,13,14,15].
As demonstrated by other studies [5,8,9,10], the main complaints of the patients, prior to hospital admission, are cough, fever, chills, sore throat, dyspnea and anosmia; after admission, cough, dyspnea and fever predominate.
Laboratory data show that inflammation, coagulation and metabolic disorders predominate in severely ill patients.
Current data suggest that the hyperinflammatory response-also known as the cytokine storm-of the host (and not the virus itself) is responsible for the disease severity and, possibly, death of the patients [16] and, also there is an interplay between inflammation and coagulation disorders [17].
The lungs seem to be the main organs affected by the disease, but recent data show that COVID-19 might be a multisystemic disease, at least in severe cases; in that respect, the higher troponin level seen in critically ill patients might be a sign of myocardial involvement, although the exact mechanism is not known [18].
Lung imagery shows that consolidation and bronchopneumonia’s aspect predominate in severe cases, but we have not confirmed any bacterial superinfection; thus, the role of antibacterial therapy remains controversial.
The majority of the patients with COVID-19 gets cured and the fatality rate is rather low; old patients are at high risk of death, in accordance with other studies [5,7,8].
Conclusions
1. Most of the cases were asymptomatic or mild;
2. Severity of the symptomatic cases increases with age;
3. Half of the patients had a previous contact with a confirmed case and almost 20% came from abroad;
4. High blood pressure, obesity, other cardiac condition, diabetes mellitus or malignancies are the main comorbidities associated with severe cases;
5. Inflammation, coagulation and metabolic disorders are significantly more expressed in severe cases;
6. Fatality rate is relatively low; deceased patients had a significantly higher age than other patients diagnosed with COVID-19.
Conflict of interests
None to declare.
Acknowledgments
Acknowledgments
LIG developed the study design and performed the analysis of the data.
FD, ACS, LD were responsible for data collection.
LIG, FD, ACS, LD wrote the first draft of the manuscript. All authors read and approved the final manuscript.
The authors would like to thank to the department involved and, particularly, to the resident doctors for the collaboration.
References
- 1.World Health Organisation, 2021, WHO Coronavirus Diseases (COVID-19) dashboard [online] Available at: covid19.who.int .
- 2.World Health Organisation, 2020, Timeline of WHO’s response to COVID-19 [online] Available at: who. int/news-room/detail/29-06-2020-covidtimeline .
- 3.Grupul de Comunicare Strategică, 2020, Informare COVID-19, Grupul de Comunicare Strategică, 6 martie 2021 [online] Available at: www.mai.gov.ro/informare-covid-19-grupul-de-comunicare-strategica .
- 4.Dumitrescu F, Turcu AA, Dragonu L, Stoian AC, Diaconescu I, Diaconu R, Giubelan L. The epidemiological, clinical and evolutive aspects of the SARS-COV-2 infection-an intermediary analysis of the cases from "Victor Babes" Clinical Hospital in Craiova, Romania. Ro J Infect Dis. 2020;23(2):91–96. [Google Scholar]
- 5.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K, Xu D, Yu H, Wang H, Wang T, Guo W, Chen J, Ding C, Zhang X, Huang J, Han M, Li S, Luo X, Zhao J, Ning Q. Clinical characteristics of 113 deceased patients with coronavirus diseases 2019: retrospective study. BMJ. 2020;368:m1091–m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xie P, Ma W, Tang H, Liu D. Severe COVID-19: a review of recent progress with a look toward the future. Front Public Health. 2020;8:189–189. doi: 10.3389/fpubh.2020.00189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang B, Zhou X, Qiu Y, Song Y, Feng F, Feng J, Song Q, Jia Q, Wang J. Clinical characteristics of 82 cases of death from COVID-19. PloS ONE. 2020;15(7):e0235458–e0235458. doi: 10.1371/journal.pone.0235458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, the Nortwell COVID-19 Research Consortium Presenting characteristics, comorbidities and outcome among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang C, Wang X, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xio J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guan W, Ni Z, Hu Y. Clinical features of coronavirus diseases 2019 in China. NEJM. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization, 2016, Global Health Observatory (GHO) data, Top 10 causes of death [online] Available at: who.int/gho/mortality_burden_disease/causes_death/top_10/en/
- 12.Yahai H. Adiposity is the crucial enhancer of COVID-19. Cardiol Res. 2020;11(5):353–354. doi: 10.14740/cr1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yanai H. A significance of high prevalence of diabetes and hypertension in severe COVID-19 patients. J Clin Med Res. 2020;12(6):389–392. doi: 10.14740/jocmr4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Costa de Luceno TM, Fernandes da Silva Santos A, Regina de Lima B, Borborema eduarda de Albuquerque M, Silva JA. Mechanism of inflammatory response in associated comorbidities in COVID-19. Diabetes Metab Syndr. 2020;14(4):597–600. doi: 10.1016/j.dsx.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanchis-Gomar F, Lavie CJ, Mehra MJ. Obesity and the outcome in COVID-19: when an epidemic and pandemic collide. Mayo Clin Proc. 2020;95(7):1445–1453. doi: 10.1016/j.mayocp.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20(6):355–362. doi: 10.1038/s41577-020-0331-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ricardo JJ, Ari M. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir Med. 2020;8(6):e46–e47. doi: 10.1016/S2213-2600(20)30216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Imazio M, Klingel K, Kinderman I, Brucato A, De Rosa FG, Adler Y, De Ferrari GM. COVID-19 pandemic and troponin: indirect myocardial injury, myocardial inflammation or myocarditis. Heart. 2020;106(5):1127–1131. doi: 10.1136/heartjnl-2020-317186. [DOI] [PubMed] [Google Scholar]


