Although atherosclerotic cardiovascular disease (ASCVD) is the leading cause of death among US Hispanic individuals, there is no validated Hispanic ASCVD risk assessment tool. 1 Current guidelines recommend the non‐Hispanic White pooled cohort equation (PCE) for 10‐year ASCVD risk estimation among Hispanic individuals, while the non‐Hispanic Black PCE is recommended when African ancestry is present. 1 The performance of this approach is unknown, and there is no guidance on its clinical implementation.
We evaluated the PCE performance among participants from 2 contemporary, population‐based, multi‐ethnic US cohorts: the DHS (Dallas Heart Study; ages 18–65 years) and the MESA (Multi‐Ethnic Study of Atherosclerosis; ages 45–84 years). 2 , 3 Informed consent was obtained, and institutional review boards approved both studies. Participants were stratified by self‐reported race of non‐Hispanic White, non‐Hispanic Black, and Hispanic individuals. MESA Hispanic individuals were stratified by self‐reported heritage into a group consisting of Mexican and Central and South American individuals and another consisting of Puerto Rican, Dominican, and Cuban individuals based on hypothesized African ancestry. The DHS did not include Hispanic heritage group classification. We included participants aged 40 to 75 years without prior ASCVD or diabetes mellitus, with low‐density lipoprotein cholesterol 70 to 189 mg/dL who were followed for incident adjudicated ASCVD events: fatal and nonfatal myocardial infarctions, strokes, or coronary heart disease deaths. 2 We excluded participants with baseline statin use or missing PCE data. Data will not be made available for purposes of reproducing the results.
We assessed risk discrimination using c‐statistics reflecting the area under the receiver operating characteristic curve. We compared mean 10‐year PCE‐predicted ASCVD incidence to observed 10‐year ASCVD events across baseline 10‐year risk categories: <5%, 5% to <7.5%, 7.5% to <20%, and ≥20%. We assessed calibration by predicted‐to‐observed risk (P/O) ratios using the Grønnesby‐Borgan goodness‐of‐fit test with an ideal P/O ratio of 1. We compared P/O ratios using unpaired t‐tests. We estimated 95% CI for c‐statistics and P/O ratios by dropping the 2.5% smallest and largest values from 1000 sorted nonparametric bootstrap estimates. As an exploratory analysis, we compared risk discrimination using both non‐Hispanic White and non‐Hispanic Black PCEs among MESA Hispanic heritage groups described above. We used SAS 9.4 (SAS Institute Inc., Cary, NC), with 2‐sided P<0.05 considered statistically significant.
We included 1065 Hispanic individuals (86% MESA; mean, 57 years; 53% women), 2159 non‐Hispanic White individuals (79% MESA; mean, 56 years; 53% women), and 1674 non‐Hispanic Black individuals (65% MESA; mean, 57 years, 58% women). At 10 years, there were 295 incident ASCVD events (Hispanic individuals n=61, non‐Hispanic White individuals n=124, non‐Hispanic Black individuals n=110). Similar discrimination was seen with either non‐Hispanic White or non‐Hispanic Black PCE with no significant sex differences in Hispanic individuals (non‐Hispanic White PCE c‐statistic, 0.74; 95% CI, 0.68–0.80; and non‐Hispanic Black PCE c‐statistic, 0.75; 95% CI, 0.70–0.80). Using the non‐Hispanic White PCE in White individuals and the non‐Hispanic Black PCE in Black individuals achieved a c‐statistic of 0.75 (95% CI, 0.71–0.79) and 0.69 (95% CI, 0.65–0.74), respectively.
The P/O ratios of 10‐year ASCVD events according to baseline risk categories (<5%, 5% to <7.5%, 7.5% to <20%, and ≥20%) for Hispanic individuals using the non‐Hispanic White PCE were 1.9 (95% CI, 0.01–3.9), 1.5 (95% CI, 0.0–3.3), 1.4 (95% CI, 0.8–2.0), and 1.4 (95% CI, 0.7–2.1) and using the non‐Hispanic Black PCE were 3.3 (95% CI, 0.0–7.5), 2.0 (95% CI, 0.0–4.5), 1.3 (95% CI, 0.9–1.8), and 1.7 (95% CI, 0.6–2.7), respectively (Figure). There were no significant sex differences in P/O ratios across groups and no difference between P/O ratios in Hispanic individuals across risk categories using the non‐Hispanic White or non‐Hispanic Black PCE (P>0.05).
Figure 1. Baseline PCE variables and risk calibration of the non‐Hispanic White and the non‐Hispanic Black PCE among participants from the DHS and MESA.
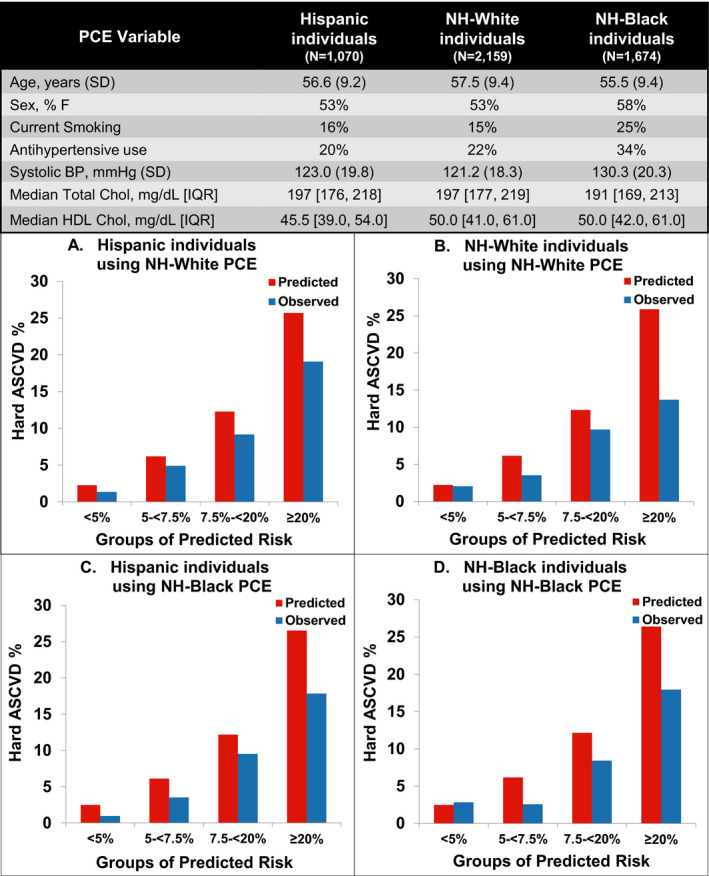
There were statistically significant differences (P<0.05) in mean age, sex, mean systolic BP, median total cholesterol, median HDL cholesterol, smoking prevalence, and antihypertensive use across groups. The non‐Hispanic White PCE led to similar risk overprediction in non‐Hispanic White individuals and in Hispanic individuals (A and B). The non‐Hispanic Black PCE led to similar risk overprediction in non‐Hispanic Black individuals and Hispanic individuals (C and D). ASCVD indicates atherosclerotic cardiovascular disease; BP, blood pressure; DHS, Dallas Heart Study; HDL, high‐density lipoprotein; MESA, Multi‐Ethnic Study of Atherosclerosis; N‐H, non‐Hispanic; and PCE, pooled cohort equation.
An exploratory analysis of 887 MESA Hispanic participants showed Mexican and Central and South American descendants (n=621) had 41 ASCVD events with c‐statistics of 0.78 and 0.76 using the non‐Hispanic White and non‐Hispanic Black PCEs, respectively. Alternatively, a group of Puerto Rican, Dominican, and Cuban descendants (n=272) experienced 14 ASCVD events with c‐statistics of 0.68 and 0.69 using the non‐Hispanic White and non‐Hispanic Black PCE, respectively.
Our results suggest that the non‐Hispanic White and non‐Hispanic Black PCEs perform similarly among MESA/DHS Hispanic individuals as they do among White and Black individuals. Furthermore, both the non‐Hispanic White and non‐Hispanic Black PCEs showed good risk discrimination but suboptimal risk calibration among MESA/DHS Hispanic participants. Similarly, a retrospective analysis of an insured Hispanic population showed systematic risk overestimation. 4 In our study, calibration was best in the clinically relevant intermediate risk groups (7.5%–20%) where pharmacotherapeutic decisions (ie, statins) are made; however, there was substantial risk overestimation of nearly 30% to 40% in this group similar to a prior MESA analysis where only the non‐Hispanic White PCE was tested in Hispanic participants. 3
Our exploratory analysis in MESA Hispanic individuals suggests that the non‐Hispanic White and non‐Hispanic Black PCEs perform similarly among Hispanic heritage groups. Nonetheless, a retrospective analysis from northern California electronic health records suggests heterogeneity across Hispanic heritage groups. 5 This heterogeneity could be explained by different contribution of African ancestry, variable migration and acculturation patterns, and differences in risk factor contribution to ASCVD events among Hispanic individuals. 1
Our analysis was limited by few events in some risk categories and in Hispanic heritage groups. Additionally, Hispanic individuals in the MESA/DHS do not entirely encompass the diversity of Hispanic heritage in the United States, and this may limit the generalizability of our findings. The impact of medication initiation during follow‐up is not accounted for.
In conclusion, the PCE performance on Hispanic individuals shows good risk discrimination but suboptimal risk calibration, similar to its performance among non‐Hispanic White and non‐Hispanic Black individuals. As acknowledged in recent guidelines, better understanding of Hispanic ancestral heterogeneity may lead to more appropriate cardiovascular risk estimates in US Hispanic individuals.
Sources of Funding
The Multi‐Ethnic Study of Atherosclerosis is supported by contracts N01‐HC‐95159, N01‐HC‐95160, N01‐HC‐95161, N01‐HC‐95162, N01‐HC‐95163, N01‐HC‐95164, N01‐HC‐95165, N01‐HC‐95166, N01‐HC‐95167, N01‐HC‐95168, N01‐HC‐95169, and HHSN268201500003I from the National Heart, Lung, and Blood Institute and by grants UL1‐RR‐024156 and UL1‐RR‐025005 from the National Center for Research Resources. The Dallas Heart Study was funded by a grant from the Donald W. Reynolds Foundation.
Disclosures
Dr Joshi reports grant support from the American Heart Association, NovoNordisk, National Aeronautics and Space Administration; consulting from Regeneron and Bayer; and Equity G3 Therapeutics. The remaining authors have no disclosures to report.
Acknowledgments
The authors thank the other investigators, the staff, and the participants of the MESA and the DHS for their valuable contributions. A full list of MESA investigators and institutions can be found at http://www.mesa‐nhlbi.org.
(J Am Heart Assoc. 2021;10:e018410. DOI: 10.1161/JAHA.120.018410.)
For Sources of Funding and Disclosures, see page 3.
References
- 1. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella‐Tommasino J, Forman DE, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol. Circulation. 2018;138:e1082–e1143. DOI: 10.1161/CIR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Victor RG, Haley RW, Willett DL, Peshock RM, Vaeth PC, Leonard D, Basit M, Cooper RS, Iannacchione VG, Visscher WA, et al. The Dallas Heart Study: a population‐based probability sample for the multidisciplinary study of ethnic differences in cardiovascular health. Am J Cardiol. 2004;93:1473–1480. DOI: 10.1016/j.amjcard.2004.02.058. [DOI] [PubMed] [Google Scholar]
- 3. DeFilippis AP, Young R, McEvoy JW, Michos ED, Sandfort V, Kronmal RA, McClelland RL, Blaha MJ. Risk score overestimation: the impact of individual cardiovascular risk factors and preventive therapies on the performance of the American Heart Association–American College of Cardiology–Atherosclerotic Cardiovascular Disease risk score in a modern multi‐ethnic cohort. Eur Heart J. 2017;38:598–608. DOI: 10.1093/eurheartj/ehw301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rana JS, Tabada GH, Solomon MD, Lo JC, Jaffe MG, Sung SH, Ballantyne CM, Go AS. Accuracy of the atherosclerotic cardiovascular risk equation in a large contemporary, multiethnic population. J Am Coll Cardiol. 2016;67:2118–2130. DOI: 10.1016/j.jacc.2016.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rodriguez F, Chung S, Blum MR, Coulet A, Basu S, Palaniappan LP. Atherosclerotic cardiovascular disease risk prediction in disaggregated Asian and Hispanic subgroups using electronic health records. J Am Heart Assoc. 2019;8:e011874. DOI: 10.1161/JAHA.118.011874. [DOI] [PMC free article] [PubMed] [Google Scholar]


