Abstract
Background
Cardiopulmonary arrests are a major contributor to mortality and morbidity in pediatric intensive care units (PICUs). Understanding the epidemiology and risk factors for CPR may inform national quality improvement initiatives.
Methods and Results
A retrospective cohort analysis using prospectively collected data from the Paediatric Intensive Care Audit Network database. The Paediatric Intensive Care Audit Network contains data on all PICU admissions in the United Kingdom. We identified children who received cardiopulmonary resuscitation (CPR) in 23 PICUs in England (2013–2017). Incidence rates of CPR and associated factors were analyzed. Logistic regression was used to estimate the size and precision of associations. Cumulative incidence of CPR was 2.2% for 68 114 admissions over 5 years with an incidence rate of 4.9 episodes/1000 bed days. Cardiovascular diagnosis (odds ratio [OR], 2.30; 95% CI, 2.02–2.61), age <1 year (OR, 1.84; 95% CI, 1.65–2.04), the Paediatric Index of Mortality 2 score on admission (OR, 1.045; 95% CI, 1.042–1.047) and longer length of stay (OR, 1.013; 95% CI, 1.012–1.014) were associated with increased odds of receiving CPR. We also found a higher risk of CPR associated with a history of preadmission cardiac arrest (OR, 20.69; [95% CI, 18.16–23.58) and for children with a cardiac condition admitted to a noncardiac PICU (OR, 2.75; 95% CI, 1.91–3.98). Children from Black (OR, 1.68; 95% CI, 1.36–2.07) and Asian (OR, 1.49; 95% CI, 1.28–1.74) racial/ethnic backgrounds were at higher risk of receiving CPR in PICU than White children.
Conclusions
Data from this first multicenter study from England provides a foundation for further research and evidence for benchmarking and quality improvement for prevention of cardiac arrests in PICU.
Keywords: cardiopulmonary resuscitation, critical care, outcome, pediatric, risk
Subject Categories: Pediatrics, Cardiopulmonary Arrest, Cardiopulmonary Resuscitation and Emergency Cardiac Care, Risk Factors
Nonstandard Abbreviations and Acronyms
- NHS
national health service
- PICANet
paediatric intensive care audit network
- PICU
pediatric intensive care unit
- PIM2
paediatric index of mortality 2
Clinical Perspective
What Is New?
This is the first multicenter study from England reporting data on >1500 children having a cardiac arrest after admission to 23 pediatric intensive care units (PICUs) over a 5‐year period.
We found that, overall, only 2 in every 100 admissions to a PICU went on to require cardiopulmonary resuscitation, accounting for about 400 episodes of cardiopulmonary resuscitation every year.
In addition to risk factors reported in the existing literature, such as younger age and underlying cardiac condition, we found a higher risk of CPR in patients from Black and Asian racial/ethnic backgrounds, those presenting with a history of cardiac arrests before admission to a PICU, children with cardiac conditions admitted to noncardiac surgical PICUs, and center volume.
What Are the Clinical Implications?
An association between mortality after discharge from a PICU and race/ethnicity has been previously reported in the United Kingdom, and our findings will support further research to explore higher risks related to race/ethnicity.
The results from this study can be used as evidence for benchmarking and designing large‐scale quality improvement initiatives for early escalation of clinical care and prevention of cardiac arrests in the PICU.
Our findings will also provide a foundation for further collaborative multicenter and multinational research.
Cardiopulmonary arrests are a major contributor to mortality and morbidity in pediatric intensive care units (PICUs) with a reported incidence between 1% and 5.5%. 1 , 2 , 3 , 4 Although survival after cardiopulmonary resuscitation (CPR) in PICU has improved over the past 2 decades from 14% to about 45% in more recent studies, mortality attributable to cardiac arrests in the PICU remains a significant burden and much higher than average mortality of 2% to 3%. 2 , 13
Current evidence suggests that children with cardiac conditions are at higher risk of receiving CPR in the PICU, and a wide range of risk factors have been implicated with risk of cardiac arrest and survival after CPR such as unit volume, patient‐to‐nurse assignment ratios, high unit occupancy, absence of an in‐house senior intensivist, surgical versus nonsurgical patients, availability of mechanical cardiopulmonary support, timing of cardiac arrest, inotropic support, lactate level, and mechanical ventilation. 3 , 21
The United Kingdom has a unique healthcare system in the form of the National Health Service (NHS), with shared financial resources, capacity challenges, rising demand, and uniformity in service standards for clinical care across the country. PICUs are usually located in tertiary centers or specialist hospitals and admit patients who require ventilatory support or support of ≥2 organ systems. Some PICUs act as lead centers with a fuller range of pediatric intensive care services such as cardiac surgery and extracorporeal membrane oxygenation (ECMO). 22 All PICUs in the United Kingdom are integrated with referring hospitals via established critical care networks and transport teams.
None of the multicenter studies reporting epidemiology of cardiac arrests and outcomes after CPR in the PICU have been conducted in the United Kingdom. Since April 2008, all NHS PICUs within England, Wales, and Scotland have been collecting data on consecutive admissions to their units to participate in the Paediatric Intensive Care Audit Network (PICANet). PICANet is commissioned by the Healthcare Quality Improvement Partnership as part of the National Clinical Audit Programme. The core data set of demographic and clinical data on all admissions allows comparison of PICU activity at a local level with national benchmarks. As per PICANet annual report, PICUs across the United Kingdom and Republic of Ireland have approximately 20 000 admissions per year with an associated mortality of 3.5% to 4.0%. 23
We aimed to identify incidence, factors associated with variability of incidence, to understand epidemiology of cardiac arrest in PICUs in England as a basis for future research and quality improvement initiatives.
METHODS
Design and Study Participation
We conducted a retrospective cohort study including all admissions to PICUs in England between January 1, 2013, and December 31, 2017. Only PICUs that provided data for the whole duration of this study were included. Informed consent from individual patients was not required as data were collected from PICANet which is the national repository for all admissions to PICUs.
Data Collection
PICANet prospectively collects data on demographics, diagnoses, severity of illness (Paediatric Index of Mortality 2 [PIM2]), daily interventions including any episode of CPR, and outcomes for patients admitted to PICUs in the United Kingdom and Republic of Ireland. PICANet data are continuously quality controlled via automatic database validation at the point of submission and additionally through on‐site data validation visits by the PICANet team.
Data quality was reviewed in relation to the following variables: age, sex, race/ethnicity, primary diagnosis, prematurity, PIM2 score, 24 length of stay in the PICU, duration of PICU stay since admission when CPR was received, number of days CPR was received, health status at discharge from PICU (dead/alive) and 30 days after discharge from PICU. Data were assessed for completeness, and proportion of any missing data was reported alongside all summary statistics. We planned to exclude variables with more than 5% missing data from analyses; however, because of good quality of data, a complete case analysis was appropriate.
Definitions of Variables
CPR was defined as any duration of chest compressions to maintain circulatory flow during cardiac arrest. 25 Index case of CPR was defined as the first episode of CPR during an admission in the PICU. The term CPR admission is used for any PICU admission during which at least 1 episode of CPR was received. Time to CPR was calculated as days since admission in the PICU, and length of stay was calculated as days between date of admission and discharge inclusive. Any stay of <24 hours was counted as 1 day of admission. Data were also collected on whether a child was discharged for palliative care, defined as withdrawal of intensive care at the current level from which it was deemed that the child could no longer benefit. 26
Primary diagnoses were defined as the main diagnosis made throughout the stay in the PICU. For example, a child admitted with cyanotic spells was assigned a primary diagnosis of tetralogy of Fallot even if this was diagnosed after the child had been admitted to the PICU. Diagnoses were classified on the basis of the NHS Coding system (Clinical Terms Version 3) and further categorized into systems: cardiovascular, respiratory, infection, endocrinology, oncology, hematology, neurology, multisystem, and “other.” Center volume was based on number of bed days delivered by a PICU in a given calendar year.
PICU was defined as a clinical facility providing at least level 3 critical care to children according to Paediatric Intensive Care Society standards. 27 Level 3 care can be broadly defined as patients requiring advanced respiratory support alone or monitoring and support for ≥2 organ systems. PICUs were divided into cardiac and noncardiac on the basis of availability of cardiac surgical services in the same hospital, which meant that these PICUs routinely admitted children after cardiac surgical interventions.
Primary Outcomes
Primary outcomes were incidence of cardiac arrest and survival to discharge from the PICU (dead versus alive).
Data Analysis
Univariable multilevel logistic regression (with a random effect for PICU to account for any potential clustering) was used to estimate the level of association and precision for variables such as age, sex, status at discharge, pre‐PICU CPR, cardiac versus noncardiac unit admissions with (1) receiving in‐PICU CPR at least once and (2) in‐PICU mortality following CPR. Pearson's correlation was used to study any association with incidence of CPR and center volume. Descriptive methods were used to study potential seasonal and daily variation in terms of CPR events.
Ethics and Data Handling
PICANet has Research Ethics Committee approval as a research database and is commissioned in England by the Healthcare Quality Improvement Partnership as part of the National Clinical Audit and Patient Outcomes Programme, which granted approval for the data to be shared. Deidentified data were hosted in the University of Leeds's Secure Electronic Environment for Data system, whose data security arrangements are approved as part of NHS Digital's Data Security and Protection Toolkit. STATA version 15 28 was used for reviewing and analysing deidentified data. Access to the data used in this article may be granted following approval of a formal data request by the data controller (the Healthcare Quality Improvement Partnership) as detailed at www.picanet.org.uk.
RESULTS
There were 83 009 admissions (16 601/year) to 28 PICUs (Table S1) across England between January 2013 and December 2017. Data from 5 PICUs were excluded as they did not provide complete data for CPR events for the whole duration of this study (Figure 1). The 2 analysis sets were similar in population demographics including PIM2 scores, age, and race/ethnicity before and after exclusion except the excluded group had a slightly higher proportion of children admitted with cardiac conditions (Table S2). Of all included admissions, 2.24% (1528/68 114) received CPR in PICU. An additional 474 CPR events occurred after the index episode among 17% (269/1528) of these patients, accounting for a total of 2002 episodes of CPR reported over 5 years, equivalent to 4.9 episodes/1000 bed days. Table 1 describes the demographics and characteristics of children who received CPR in the PICU. When compared with the cohort of children who did not receive CPR, there was a higher proportion of Asian (15.3% versus 11.4%) and Black children (7.3% versus 4.8%) who received CPR in the PICU (however, race/ethnicity data were missing for over one‐fifth of admissions in each cohort) and a higher proportion of children aged <1 year (59.4% versus 42.0%). The proportion of male patients was similar in each cohort; however, median PIM2 predicted probability of death (5.7% versus 1.3%), and the proportion of children receiving CPR pre‐PICU (26.9% versus 1.7%) was higher for CPR admissions.
Figure 1. Total number of admissions before and after exclusions.
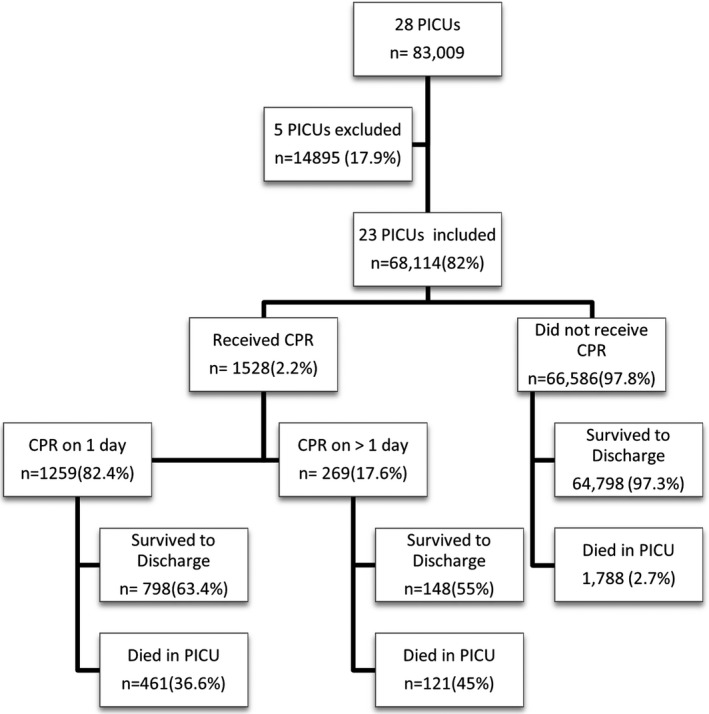
Five PICU excluded as data for CPR was not consistently submitted for the full duration of study. CPR indicates cardiopulmonary resuscitation; and PICUs, pediatric intensive care units.
Table 1.
Descriptive Characteristics of All Patients Admitted to the PICU Between 2013 and 2017
| Characteristics | Had CPR in PICU | No CPR in PICU | All PICU admissions |
|---|---|---|---|
| 1528 (2.2) | 66 586 (97.8) | N=68 114 | |
| Age, y, n (%) | |||
| <1 | 908 (59.4) | 27 942 (42.0) | 28 850 (42.4) |
| 1–4 | 322 (21.1) | 17 815 (26.8) | 18 137 (26.6) |
| 5–10 | 160 (10.5) | 10 064 (15.1) | 10 224 (15.0) |
| 11–15 | 117 (7.7) | 9027 (13.5) | 9135 (13.4) |
| >16 | 21 (1.4) | 1741 (2.6) | 1762 (2.6) |
| Missing | 0 (0.0) | 6 (<0.1) | 6 (<0.1) |
| Sex, n (%) | |||
| Male | 888 (58.1) | 37 812 (56.8) | 38 700 (56.8) |
| Female | 640 (41.9) | 28 766 (43.2) | 29 406 (43.2) |
| Ambiguous* | 0 (0.0) | 8 (<0.1) | 8 (<0.1) |
| Race/Ethnicity, n (%) | |||
| White | 838 (54.8) | 37 996 (57.1) | 38 834 (57.0) |
| Mixed | 49 (3.2) | 2008 (3.0) | 2057 (3.0) |
| Asian | 233 (15.3) | 7601 (11.4) | 7834 (11.5) |
| Black | 111 (7.3) | 3191 (4.8) | 3302 (4.9) |
| Other † /Unknown | 297 (19.4) | 15 790 (23.7) | 16 087 (23.6) |
| Primary diagnosis group, n (%) | |||
| Hematology | 16 (1.1) | 696 (1.2) | 712 (1.1) |
| Cardiovascular | 741 (48.5) | 18 239 (27.4) | 18 981 (27.9) |
| Metabolic/Endocrine | 57 (3.7) | 1883 (2.8) | 1940 (2.9) |
| Infection | 115 (7.5) | 3515 (5.3) | 3630 (5.3) |
| Multisystem | 5 (0.3) | 208 (0.3) | 213 (0.3) |
| Neurology | 81 (5.3) | 7319 (11.0) | 7499 (10.9) |
| Oncology | 20 (1.3) | 2574 (3.9) | 2594 (3.8) |
| Respiratory | 362 (23.7) | 19 253 (28.9) | 19 616 (28.8) |
| Other ‡ | 131 (8.6) | 12 899 (19.4) | 13 028 (19.1) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| PIM2 predicted probability of death | |||
| n (%) | 1528 (100.0) | 66 586 (100.0) | 68 114 (100.0) |
| Mean, % | 15.2 (±22.9) | 3.4 (±7.6) | 3.7 (±8.4) |
| Median, % (range) | 5.7 (0.2–99.8) | 1.3 (0.1–99.6) | 1.3 (0.1–99.8) |
| Pre‐PICU CPR, n (%) | |||
| Yes | 411 (26.9) | 1138 (1.7%) | 1549 (2.3%) |
| No | 1097 (71.8) | 63 199 (94.9%) | 64 296 (94.4%) |
| Missing | 20 (1.3) | 2249 (3.4) | 2269 (3.3) |
| Number of days CPR received | |||
| n (%) | 1528 (100.0) | 1528 (2.2) | |
| Mean | 1.31 (±1.023) | N/A no CPR | 1.31 (±1.023) |
| Median (range) | 1 (1–14) | received | 1 (1–14) |
| Day of admission on first episode of CPR, n (%) | |||
| First day | 743 (48.6) | 743 (48.6) | |
| Second day | 224 (14.7) | N/A–no CPR | 224 (14.7) |
| Third day or later | 561 (36.7) | received | 561 (36.7) |
| Missing | 0 (0.0) | 0 (0.0) | |
| Length of stay (d) | |||
| n (%) | 1528 (100.0) | 66 586 (100.0) | 68 114 (100.0) |
| Mean | 20.12 (±36.37) | 6.39 (±15.81) | 6.69 (±16.68) |
| Median (range) | 9 (1–471) | 3 (1–912) | 3 (1–912) |
CPR indicates cardiopulmonary resuscitation; PICU, pediatric intensive care unit; N/A, not applicable; and PIM2, Paediatric Index of Mortality 2.
Ambiguous refers to a child where either male or female sex cannot be assigned based on phenotype.
Other refers to races/ethnicities not covered.
Body wall and cavities, gastrointestinal, musculoskeletal, trauma, unknown.
Risks for Receiving CPR
Univariable logistic regression analyses examining association between receiving CPR in PICU and various factors are presented in Table 2. Higher PIM2 predicted probability of death on admission (odds ratio [OR], 1.045; 95% CI, 1.042–1.047) and a longer length of stay in the PICU (OR, 1.013; 95% CI, 1.012–1.014) were associated with increased odds of receiving CPR. Children admitted with cardiac conditions were at significantly higher risk of receiving CPR in the PICU (OR, 2.30; 95% CI, 2.02–2.61) compared with those admitted with noncardiac primary diagnosis. The risk of receiving CPR was significantly associated with age, history of preadmission CPR, and race/ethnicity, being highest among children from the Black race/ethnic group (OR, 1.68; 95% CI, 1.36–2.07) followed by the Asian race/ethnic group (OR, 1.49; 95% CI, 1.28–1.74) when compared with White children. Race/ethnicity was not recorded for 17% of individuals.
Table 2.
Univariable Logistic Regression Results for Receiving CPR in the PICU
| Association With Receiving CPR in the PICU | ||||
|---|---|---|---|---|
| OR | 95% CI | P value | ||
| Age, y | ||||
| <1 | Reference group | |||
| 1–4 | 0.61 | 0.53 | 0.69 | <0.01 |
| 5–10 | 0.53 | 0.45 | 0.63 | |
| 11–15 | 0.45 | 0.37 | 0.55 | |
| 16+ | 0.42 | 0.27 | 0.65 | |
| PIM2 probability of death | 1.045 | 1.042 | 1.047 | <0.01 |
| Race/Ethnicity | ||||
| White | Reference group | |||
| Mixed | 1.12 | 0.83 | 1.50 | <0.01 |
| Asian | 1.49 | 1.28 | 1.74 | |
| Black | 1.68 | 1.36 | 2.07 | |
| Other*/Unknown | 1.11 | 0.94 | 1.30 | |
| Sex | ||||
| Female | Reference group | |||
| Male | 1.07 | 0.96 | 1.18 | 0.21 |
| Length of stay, d | 1.013 | 1.012 | 1.014 | <0.01 |
| CPR preadmission | 20.69 | 18.16 | 23.58 | <0.01 |
| Primary diagnosis group | ||||
| Cardiovascular | Reference group | |||
| Hematology | 0.59 | 0.36 | 0.99 | <0.01 |
| Metabolic/Endocrine | 0.80 | 0.60 | 1.06 | |
| Infection | 0.83 | 0.67 | 1.03 | |
| Multisystem | 0.73 | 0.30 | 1.80 | |
| Neurology | 0.29 | 0.23 | 0.37 | |
| Oncology | 0.22 | 0.14 | 0.35 | |
| Respiratory | 0.49 | 0.42 | 0.57 | |
| Other † | 0.28 | 0.23 | 0.34 | |
CPR indicates cardiopulmonary resuscitation; OR, odds ratio; PICU, pediatric intensive care unit; and PIM2, Paediatric Index of Mortality 2.
Other refers to races/ethnicities not covered.
Body wall and cavities, gastrointestinal, musculoskeletal, trauma, unknown.
PICU mortality (3.3%–3.7%) and incidence of CPR (2.0%–2.5%) remained consistent over the study period of 5 years. We did not observe any seasonal variation in proportion of admissions with cardiac arrest per month: The highest number of admissions was observed in December, and there was a higher incidence of CPR in April (Figure 2). Overall, the highest number of cardiac arrests occurred on Thursday (16.9%; 339/2002) followed by Saturday (16.3%; 326/2002) and Friday (14.1%; 302/2002).
Figure 2. Monthly variation in PICU admissions and number of CPR events.
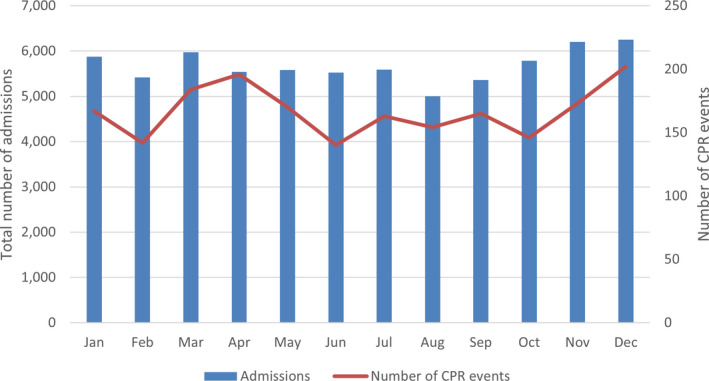
PICU indicates pediatric intensive care unit; and CPR, cardiopulmonary resuscitation.
There was a wide variation in incidence of CPR between PICUs (0.5%–6.5%) and a high positive Pearson's correlation (ρ=0.70) between total bed days and number of admissions for which CPR was received on the basis of individual data for each PICU for each year (Figure 3). This would suggest that PICUs that provided a higher number of bed days (ie, larger units) had a higher proportion of admissions who received CPR. 29
Figure 3. Number of CPR admissions against number of bed days, by PICU.
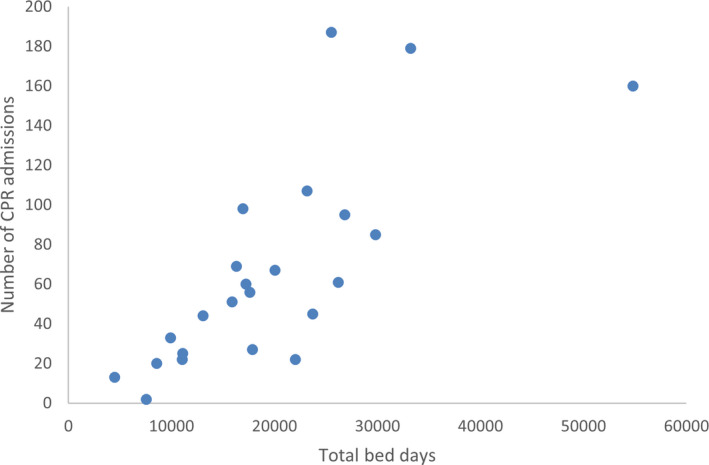
Each dot represents the number of CPR admissions for each unit plotted against number of bed days in the study period for that unit. CPR indicates cardiopulmonary resuscitation; and PICU, pediatric intensive care unit.
Timing of CPR
Of all patients who received CPR in the PICU, 82.4% (1259/1528) received CPR on only 1 day, while 17.6% (269/1528) of patients received CPR on >1 day. Of the 474 subsequent multiple CPR events, 64.1% occurred 1 day after the previous episode. The median number of days between CPR events was 1 (range, 1–134).
Of those with a cardiovascular primary diagnosis who received CPR in the PICU, over half (53.0 %) received CPR on their first day (393/741). These included pre‐ and postsurgical admissions with congenital cardiac anomalies as well as those with medical cardiac diagnoses such as prehospital cardiac arrest, cardiomyopathies, and arrhythmias. Among those who received CPR in the PICU, 26.9% (411/1528) also had a history of cardiac arrest before admission to the PICU in comparison with only 1.7% (1138/68114) of all PICU admissions. Of these patients, 86.6% (356/411) received CPR during the first 24 hours of their admission to the PICU, which was much higher than for those admissions with no history of pre‐PICU CPR (34.1%; 374/1097).
Mortality Associated With CPR
Only 61.9% (946/1528) of patients who received CPR survived to discharge from the PICU compared with 97.3% (64 798/66 586) of those who did not receive CPR in the PICU (Table 3). Of those who received CPR on 1 day, 63.4% (798/1259) survived to discharge, whereas survival for those who received CPR on ≥2 days was only 55% (148/269). In patients who received CPR, the survival to PICU discharge was highest among patients admitted with respiratory conditions (78.2%) and lowest for those admitted because of endocrine/metabolic and infectious conditions (68.4% and 53.9%, respectively). At 30 days after discharge, 3.7% (35/946) of those who received CPR and survived the PICU had died compared with 0.9% (601/64 798) in the non‐CPR group; however, 30‐day status was unknown or missing for >30% of patients in both groups.
Table 3.
Outcomes for All Patients Admitted to the PICU Between 2013 and 2017, n (%)
| Characteristics | Had CPR in PICU | No CPR in PICU | All PICU Admissions |
|---|---|---|---|
| Status at discharge, n (%) | |||
| Alive | 946 (61.9) | 64 798 (97.3) | 65 744 (96.5) |
| Dead | 582 (38.1) | 1788 (2.7) | 2370 (3.5) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Discharge from PICU for palliative care, n (%) | |||
| Yes | 17 (1.8) | 430 (0.7) | 447 (0.7) |
| No | 994 (98.0) | 64 060 (98.9) | 64 987 (98.9) |
| Unknown | 2 (0.2) | 308 (0.5) | 310 (0.5) |
| Status at 30 days' follow‐up for those discharged alive from PICU, n (%) | |||
| Alive | 589 (62.3) | 38 700 (59.7) | 39 289 (59.8) |
| Dead | 35 (3.7) | 601 (0.9) | 636 (1.0) |
| Unknown* | 305 (32.2) | 22 206 (34.3) | 22 511 (34.2) |
| Missing* | 17 (1.8) | 3291 (5.1) | 3308 (5.0) |
CPR indicates cardiopulmonary resuscitation; OR, odds ratio; and PICU, pediatric intensive care unit.
Data for 30 days' follow‐up after PICU discharge were missing or unknown for >30% of admissions in both groups.
Table 4 presents univariable regression analysis for associations between various factors and in‐PICU mortality for those who had CPR. CPR was associated with an increased odds of mortality for patients with a cardiac diagnosis compared with those with a primary respiratory diagnosis (OR, 2.54; 95% CI, 1.86–3.46) and for patients with cardiac conditions in noncardiac PICUs compared with patients with cardiac conditions in cardiac PICUs (OR, 2.40; 95% CI, 1.48–3.88).
Table 4.
Univariable Logistic Regression Results
| Association with mortality for those who received CPR in PICU | ||||
|---|---|---|---|---|
| OR | 95% CI | P Value | ||
| Age, y | ||||
| <1 | Reference group | |||
| 1–4 | 1.38 | 1.06 | 1.80 | <0.01 |
| 5–10 | 2.02 | 1.43 | 2.85 | |
| 11–15 | 1.72 | 1.16 | 2.56 | |
| 16+ | 5.02 | 1.91 | 13.24 | |
| PIM2 probability of death | 1.09 | 1.08 | 1.10 | <0.01 |
| Race/Ethnicity | ||||
| White | Reference group | |||
| Mixed | 0.85 | 0.45 | 1.60 | <0.01 |
| Asian | 1.12 | 0.82 | 1.54 | |
| Black | 1.22 | 0.80 | 1.85 | |
| Other*/Unknown | 1.84 | 1.36 | 2.50 | |
| Sex | ||||
| Female | Reference group | |||
| Male | 0.84 | 0.68 | 1.03 | 0.10 |
| Length of stay, d | 0.98 | 0.98 | 0.99 | <0.01 |
| CPR preadmission | 1.49 | 1.17 | 1.89 | <0.01 |
| Primary diagnosis group | ||||
| Cardiovascular | Reference group | |||
| Haematology | 1.17 | 0.43 | 3.22 | <0.01 |
| Metabolic/Endocrine | 2.92 | 1.61 | 5.31 | |
| Infection | 1.66 | 1.10 | 2.50 | |
| Multisystem | Excluded because of small numbers | |||
| Neurology | 1.28 | 0.79 | 2.06 | <0.01 |
| Oncology | 1.35 | 0.54 | 3.37 | |
| Respiratory | 0.39 | 0.29 | 0.54 | |
| Other † | 1.00 | 0.67 | 1.49 | |
CPR indicates cardiopulmonary resuscitation; OR, odds ratio; PICU, pediatric intensive care unit; and PIM2, Paediatric Index of Mortality 2.
Other refers to races/ethnicities not covered.
Body wall and cavities, gastrointestinal, musculoskeletal, trauma, unknown.
Differences Between and Cardiac and Noncardiac PICUs
Of the 23 PICUs included in this analysis, only 9 had local availability of cardiac surgical services including ECMO (Table 5); on average, these had more admissions than noncardiac PICUs (admissions in cardiac units: mean, 3782 [SD, 1846.3], noncardiac units: mean, 2434 [SD, 1024.5]). There was nearly double the incidence of CPR events reported in cardiac PICUs (2.9%; 996/34 039) compared with noncardiac PICUs (1.6%; 532/34 075). Of those who received CPR in a cardiac PICU, 63.5% (632/996) had a cardiovascular primary diagnosis, and 16.0% (159/996) were admitted because of respiratory conditions. Of those who received CPR in a noncardiac PICU, the highest proportion of patients (38.2%; 203/532) had a respiratory diagnosis, and 20.5% (109/532) were admitted because of cardiac conditions. We also found a 2.8‐fold higher risk of CPR for cardiac patients if they were admitted to noncardiac PICUs (OR, 2.75; 95% CI, 1.91–3.98). A higher proportion of those who received CPR in cardiac PICUs were alive at discharge from the PICU (64.0% compared with noncardiac PICU, 58.1%) (Table 6).
Table 5.
Admissions in Cardiac (N=9) and Noncardiac Units (N=14)
| Characteristics | Cardiac Units N=9 | Noncardiac Units N=14 |
|---|---|---|
| Total admissions | n=34 039 | n=34 075 |
| Age, y, n (%) | ||
| <1 | 17 255 (50.7) | 11 595 (34.0) |
| 1–4 | 7954 (23.4) | 10 183 (29.9) |
| 5–10 | 4511 (13.3) | 5713 (16.78) |
| 11–15 | 3668 (10.8) | 5467 (16.0) |
| >16 | 649 (1.9) | 1113 (3.3) |
| Missing | 2 (<0.1) | 4 (<0.1) |
| Sex, n (%) | ||
| Male | 19 225 (56.5) | 19 475 (57.2) |
| Female | 14 812 (43.5) | 14 594 (42.8) |
| Ambiguous* | 2 (<0.1) | 6 (<0.1) |
| Race/Ethnicity, n (%) | ||
| White | 21 254 (62.4) | 17 580 (51.6) |
| Mixed | 1302 (3.8) | 755 (2.2) |
| Asian | 4748 (14.0) | 3086 (9.1) |
| Black | 1778 (5.2) | 1524 (4.5) |
| Other/Unknown | 4957 (14.6) | 11 130 (32.7) |
| Primary diagnosis group | ||
| Haematology | 233 (0.7%) | 479 (1.4%) |
| Cardiovascular | 17 761 (52.2%) | 1220 (3.6%) |
| Metabolic/Endocrine | 557 (1.6%) | 1383 (4.1%) |
| Infection | 1328 (3.9%) | 2302 (6.8%) |
| Multisystem | 89 (0.3%) | 124 (0.4%) |
| Neurology | 2280 (6.7) | 5120 (15.0) |
| Oncology | 965 (2.8) | 1629 (4.8) |
| Respiratory | 6411 (18.8) | 13 205 (38.8) |
| Other † | 4416 (13.0) | 8613 (25.3) |
| Missing | 0 (0.0) | 0 (0.0) |
| PIM2 predicted probability of death | ||
| n (%) | 34 039 (100.0) | 34 075 (100.0) |
| Mean, % | 4.1% (±8.9) | 3.3% (±7.9) |
| Median, % (range) | 1.4% (0.1–99.8) | 1.2% (0.1–99.6) |
| CPR pre‐PICU admission, n (%) | ||
| Yes | 867 (2.6) | 682 (2.0) |
| No | 33 091 (97.2) | 31 205 (91.6) |
| Missing | 81 (0.2) | 2188 (6.4) |
| Received CPR in PICU, n (%) | ||
| Yes | 996 (2.9) | 532 (1.6) |
| No | 33 043 (97.1) | 33 543 (98.4) |
| Missing | 0 (0.0) | 0 (0.0) |
| Number of days CPR received | ||
| n (%) | 996 (100.0) | 532 (100.0) |
| Mean | 1.32 (±1.053) | 1.28 (±0.963) |
| Median (range) | 1 (1–14) | 1 (1–12) |
| Day of admission on first episode of CPR, n (%) | ||
| First day | 492 (49.4) | 251 (47.2) |
| Second day | 142 (14.3) | 82 (15.4) |
| Third day or later | 362 (37.4) | 199 (37.4) |
| Missing | 0 (0.0) | 0 (0.0) |
| Length of stay (days) | ||
| n | 34 039 (100.0) | 34 075 (100.0) |
| Mean | 6.96 (±15.69) | 6.43 (±17.60) |
| Median (range) | 3 (1–747) | 3 (1–912) |
CPR indicates cardiopulmonary resuscitation; PICU, pediatric intensive care unit; and PIM2, Paediatric Index of Mortality 2.
Ambiguous refers to a child where either male or female sex cannot be assigned based on phenotype.
Body wall and cavities, gastrointestinal, musculoskeletal, trauma, unknown.
Table 6.
Outcomes for Admissions in Cardiac (n=9) and Noncardiac Units (n=14)
| Characteristics | Cardiac units, n (%) | Noncardiac units, n (%) |
|---|---|---|
| Status at discharge | ||
| Alive | 32 761 (96.3) | 32 983 (96.8) |
| Dead | 1278 (3.8) | 1092 (3.2) |
| Missing | 0 (0.0) | 0 (0.0) |
| Status at discharge for those who had CPR | ||
| Alive | 637 (64.0) | 309 (58.1) |
| Dead | 359 (36.0) | 223 (41.9) |
| Missing | 0 (0.0) | 0 (0.0) |
| Discharge for palliative care (If alive at discharge) | ||
| Yes | 178 (0.5) | 269 (0.8) |
| No | 32 562 (99.9) | 32 425 (98.3) |
| Unknown | 21 (0.1) | 289 (0.9) |
| Status at 30 days follow up | ||
| Alive | 22 053 (67.3) | 17 236 (52.3) |
| Dead | 373 (1.1) | 263 (0.8) |
| Unknown | 8633 (26.4) | 13 878 (42.1) |
| Missing | 1702 (5.2) | 1606 (4.9) |
CPR indicates cardiopulmonary resuscitation.
DISCUSSION
To our knowledge, this is the first multicenter report of incidence of CPR in PICUs in England. In our study population, 2.2% of patients received at least 1 episode of CPR in PICU, with an overall incidence rate of 4.9 episodes/1000 bed days. This was associated with a significantly higher PIM2 score on admission and increased length of stay and mortality before discharge from the PICU. The incidence of CPR and survival at discharge from the PICU was similar to multicenter studies in other countries. 1 , 7 , 15 , 30 In keeping with existing evidence, we also found that the majority of children who received CPR were <1 year old and that a higher number of cardiac arrests happened within 24 hours of admission to the PICU. 1 , 31 Children with cardiac conditions and a history of pre‐PICU cardiac arrest were more likely to receive CPR on the day of admission. Out‐of‐hospital cardiac arrest has been associated with high mortality in children in the United Kingdom, 32 but to our knowledge, no previous multicenter study has reported data for recurrence of cardiac arrests in the PICU for this population. We also found that children who received CPR on the day of admission or on >1 day were at a higher risk of mortality before discharge from the PICU.
A significantly greater risk for receiving CPR in the PICU was noted for children from Black and Asian racial/ethnic backgrounds compared with White children. This association did not persist for mortality before discharge from the PICU. One of the reasons could be that this was a subgroup analysis, and the study was not designed to detect such association. However, data from PICANet have also suggested higher mortality for Asian girls within 30 days of discharge from the PICU. 23 A possible association with social deprivation and inequity in access to specialized services for racial/ethnic minorities should be explored in future research. 33 Another possible explanation is a potential racial/ethnic difference in decisions for limitation of treatment as noted by Burns et al, 8 who found that children of White background were more likely to have a Do Not Attempt CPR agreement in place.
Overall incidence of CPR was higher in cardiac PICUs (2.9% compared with 1.6%), which can be explained by a generally higher incidence of CPR among children with cardiac diseases, as noted in our study population and has also been described in the existing literature. 1 , 5 , 31 , 34
Interestingly, children with cardiac conditions had a significantly higher incidence of CPR and mortality before discharge from the PICU if admitted to a noncardiac PICU. Mortality attributable to cardiac arrest can be affected by level of skills and experience of clinical staff 16 , 35 and initiation of ECMO‐CPR, 5 , 36 , 37 which was only available at cardiac PICUs. Also, specialized PICUs may have better quality control or feedback systems, leading to improved outcomes of CPR. 38 There is a need to consider a possible impact of such factors and the role of training and prevention interventions in both cardiac and noncardiac PICUs and establishing ECMO‐CPR capabilities outside the centers providing cardiac surgical services across the NHS.
Of 109 children with a primary cardiac diagnosis who received CPR in a noncardiac PICU, just over 70% (n=79) had a history of pre‐PICU cardiac arrest. Lipe et al 39 found that adult patients with a history of an out‐of‐hospital cardiac arrest had better outcomes if admitted in cardiac resuscitation centers. We are unable to make similar assumptions based on our data, as the differences in case mix between cardiac admissions to cardiac and noncardiac PICUs will need to be further explored, and further research is needed to study a possibility of such associations in the pediatric population.
The main strengths of this study are its use of multicenter data from a large geographic distribution of an racially/ethnically diverse population with variation in access to specialized services 40 and high case ascertainment levels. 23
We were unable to ascertain if the patient received CPR more than once in a 24‐hour period because of data collection limitations nor to ascertain if a patient had a Do Not Attempt CPR in place. Although this would not change the overall incidence of patients receiving CPR in PICU, we believe that the prevalence of cardiac arrest could be much higher and a larger proportion of children may have received >1 episode of CPR during the 24‐hour data collection period.
Some PICUs were excluded from analysis because they did not collect data for the whole study period, although demographic characteristics of the analysis population did not differ greatly following the exclusions. Other limitations of this study were that we were unable to study specific details such as categorization of patients with cardiac conditions into surgical and nonsurgical cases, duration of CPR and relation to timing of cardiac surgery, provision of ECMO‐CPR, and long‐term outcomes including neurological status for those who survived to discharge from the hospital. We carried out univariable analyses and were unable to adjust for confounders (Tables 2 and 4), which is likely to introduce bias. These should be areas for further research and prospective multicenter studies to evaluate risks, interventions, and outcomes for cardiac arrests in the PICU. We also recommend using causal inference methods and directed acyclic graphs to identify the minimum set of confounders to include in regression models to examine the causal relationship between center volume, incidence of CPR, and in‐PICU mortality.
CONCLUSIONS
In this first multicenter study from England that included data from 23 hospitals, we found a cumulative incidence for CPR of 2.2% among children who were admitted to a PICU.
Cardiac conditions, younger age, and a higher PIM2 score on admission were associated with a higher incidence of CPR, and these children had a significantly prolonged hospital stay and higher mortality in the PICU. We also found a higher risk of CPR associated with race/ethnicity, cardiac versus noncardiac PICUs, and center volume.
This study provides not only the foundations for further multicenter and multinational research but also evidence for the need for benchmarking and designing large‐scale quality improvement initiatives for early escalation of clinical care and prevention of cardiac arrests in the PICU.
Sources of Funding
None.
Disclosures
Dr Scholefield is funded by a National Institute for Health Research (Clinical Scientist) Fellowship award. However, this project was not funded by the National Institute for Health Research. The views expressed are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, or the Department of Health and Social Care. The remaining authors have no disclosures to report.
Supporting information
Tables S1–S2
Acknowledgments
Lee Norman (Database Manager, PICANet) contributed to data collection and management. He has provided consent to be named in the acknowledgements.
(J Am Heart Assoc. 2021;10:e018177. DOI: 10.1161/JAHA.120.018177.)
Supplementary Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.120.018177
For Sources of Funding and Disclosures, see page 11.
References
- 1. Alten J, Klugman D, Raymond T, Cooper D, Donohue J, Zhang W, Pasquali S, Gaies M. Epidemiology and outcomes of cardiac arrest in pediatric cardiac ICUs. Pediatr Crit Care Med. 2017;18:935–943. DOI: 10.1097/PCC.0000000000001273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Berg RA, Sutton RM, Holubkov R, Nicholson CE, Dean JM, Harrison R, Heidemann S, Meert K, Newth C, Moler F, et al. Ratio of PICU versus ward cardiopulmonary resuscitation events is increasing. Crit Care Med. 2013;41:2292–2297. DOI: 10.1097/CCM.0b013e31828cf0c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gupta P, Tang X, Gall C, Lauer C, Rice T, Wetzel R. Epidemiology and outcomes of in‐hospital cardiac arrest in critically ill children across hospitals of varied center volume: a multi‐center analysis. Resuscitation. 2014;85:1473–1479. DOI: 10.1016/j.resuscitation.2014.07.016. [DOI] [PubMed] [Google Scholar]
- 4. Gupta P, Jacobs JP, Pasquali SK, Hill KD, Gaynor JW, O'Brien SM, He M, Sheng S, Schexnayder SM, Berg RA, et al. Epidemiology and outcomes after in‐hospital cardiac arrest after pediatric cardiac surgery. Ann Thorac Surg. 2014;98:2138–2144. DOI: 10.1016/j.athoracsur.2014.06.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. De Mos N, van Litsenburg R, McCrindle B, Bohn D, Parshuram C. Pediatric in‐intensive‐care‐unit cardiac arrest: incidence, survival, and predictive factors. Crit Care Med. 2006;34:1209–1215. DOI: 10.1097/01.CCM.0000208440.66756.C2. [DOI] [PubMed] [Google Scholar]
- 6. Slonim A, Patel K, Ruttimann U, Pollack M. Cardiopulmonary resuscitation in pediatric intensive care units. Crit Care Med. 1997;25:1951–1955. DOI: 10.1097/00003246-199712000-00008. [DOI] [PubMed] [Google Scholar]
- 7. Tibballs J, Kinney S. A prospective study of outcome of in‐patient paediatric cardiopulmonary arrest. Resuscitation. 2006;71:310–318. DOI: 10.1016/j.resuscitation.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 8. Burns J, Sellers D, Meyer E, Lewis‐Newby M, Truog R. Epidemiology of death in the PICU at five U.S. teaching hospitals. Crit Care Med. 2014;42:2101–2108. DOI: 10.1097/CCM.0000000000000498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Irie H, Okamoto H, Uchino S, Endo H, Uchida M, Kawasaki T, Kumasawa J, Tagami T, Shigemitsu H, Hashiba E, et al. The Japanese Intensive care PAtient database (JIPAD): a national intensive care unit registry in Japan. J Crit Care. 2019;55:86–94. DOI: 10.1016/j.jcrc.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 10. Kalzén H, Larsson B, Eksborg S, Lindberg L, Edberg K, Frostell C. Survival after PICU admission: the impact of multiple admissions and complex chronic conditions. PLoS One. 2018;13:e0193294. 10.1371/journal.pone.0193294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pollack MM, Holubkov R, Funai T, Berger JT, Clark AE, Meert K, Berg RA, Carcillo J, Wessel DL, Moler F, et al. Simultaneous prediction of new morbidity, mortality, and survival without new morbidity from pediatric intensive care. Crit Care Med. 2015;43:1699–1709. DOI: 10.1097/CCM.0000000000001081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Parra D, Totapally B, Zahn E, Jacobs J, Aldousany A, Burke R, Chang A. Outcome of cardiopulmonary resuscitation in a pediatric cardiac intensive care unit. Crit Care Med. 2000;28:3296–3300. DOI: 10.1097/00003246-200009000-00030. [DOI] [PubMed] [Google Scholar]
- 13. Ortmann L, Prodhan P, Gossett J, Schexnayder S, Berg R, Nadkarni V, Bhutta A, Mancini ME, Berg RA, Allen E, et al. Outcomes after in‐hospital cardiac arrest in children with cardiac disease. Circulation. 2011;124:2329–2337. DOI: 10.1161/CIRCULATIONAHA.110.013466. [DOI] [PubMed] [Google Scholar]
- 14. Bacon MK, Conrad SJ, Hatch BC, Hughes JD, Terrell MK, Maynord PO, Smith AH. Resource demands and the incidence of cardiopulmonary resuscitation within a pediatric cardiac intensive care unit. Circulation. 2014;130(suppl 2):A11345. Available at: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=yrovftp&NEWS=N&AN=00003017‐201411251‐00515 Accessed April 8 2021. [Google Scholar]
- 15. Berg RA, Nadkarni VM, Clark AE, Moler F, Meert K, Harrison RE, Newth CJL, Sutton RM, Wessel DL, Berger JT, et al. Incidence and outcomes of cardiopulmonary resuscitation in PICUs. Crit Care Med. 2016;44:798–808. DOI: 10.1097/CCM.0000000000001484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hansen M, Fleischman R, Meckler G, Newgard C. The association between hospital type and mortality among critically ill children in US EDs. Resuscitation. 2013;84:488–491. DOI: 10.1016/j.resuscitation.2012.07.032. [DOI] [PubMed] [Google Scholar]
- 17. Maskell KF, Ferguson NM, Bain J, Wills BK. Survival after cardiac arrest: ECMO rescue therapy after amlodipine and metoprolol overdose. Cardiovasc Toxicol. 2017;17:223–225. DOI: 10.1007/s12012-016-9362-2. [DOI] [PubMed] [Google Scholar]
- 18. Narayanan A, Dominguez T, Hsia T, Thiruchelvam T, Leavey B, Banks V. Patient demographics and early outcomes after cardiopulmonary resuscitation in paediatric cardiac intensive care unit. Cardiol Young. 2017;27:S352–S353. DOI: 10.1017/S104795111700110X. [DOI] [Google Scholar]
- 19. Ofoma UR, Basnet S, Berger A, Kirchner HL, Girotra S, Abella B, Anderson ML, Bradley SM, Chan PS, Edelson DP, et al. Trends in survival after in‐hospital cardiac arrest during nights and weekends. J Am Coll Cardiol. 2018;71:402–411. DOI: 10.1016/j.jacc.2017.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rodríguez‐Núñez A, López‐Herce J, García C, Carrillo A, Domínguez P, Calvo C, Delgado M. Effectiveness and long‐term outcome of cardiopulmonary resuscitation in paediatric intensive care units in Spain. Resuscitation. 2006;71:301–309. DOI: 10.1016/j.resuscitation.2005.11.020. [DOI] [PubMed] [Google Scholar]
- 21. Lasa JJ, Rogers RS, Localio R, Shults J, Raymond T, Gaies M, Thiagarajan R, Laussen PC, Kilbaugh T, Berg RA, et al. Extracorporeal cardiopulmonary resuscitation (E‐CPR) during pediatric in‐hospital cardiopulmonary arrest is associated with improved survival to discharge. Circulation. 2016;133:165–176. DOI: 10.1161/CIRCULATIONAHA.115.016082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. NHS England . Service specifications. 2015; Available at: https://www.england.nhs.uk/commissioning/wp‐content/uploads/sites/12/2015/01/e07‐sa‐paed‐inten‐care.pdf Accessed 29 January 2020.
- 23. PICANet . 2019. Picanet.org.uk. Available at: https://www.picanet.org.uk/wpcontent/uploads/sites/25/2019/12/PICANet‐2019‐Annual‐Report‐Summary_v1.0.pdf. Accessed 18 December 2019.
- 24. Slater A, Shann F, Pearson G, & PIM Study Group . PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med. 2003;29:278–285. DOI: 10.1007/s00134-002-1601-2. [DOI] [PubMed] [Google Scholar]
- 25. Maconochie IK, Bingham R, Eich C, López‐Herce J, Rodríguez‐Núñez A, Rajka T, Van de Voorde P, Zideman DA, Biarent D, Monsieurs KG, et al. European resuscitation council guidelines for resuscitation 2015. Resuscitation. 2015;95:223–248. DOI: 10.1016/j.resuscitation.2015.07.028. [DOI] [PubMed] [Google Scholar]
- 26. PICANet . PICANet web admission dataset manual version 5.2. 2017; Picanet.org.uk. Available at: https://picsociety.uk/wp‐content/uploads/2015/10/PICS_Standards_Appendix_2010.pdf Accessed 28 January 2020.
- 27. Paediatric Intensive Care Society . Appendices to standards for the care of critically ill children. 2010; Available at: https://picsociety.uk/wp‐content/uploads/2015/10/PICS_Standards_Appendix_2010.pdf. Accessed 28 January 2020.
- 28. StataCorp . Stata Statistical Software. Release 15. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 29. Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24:69–71. DOI: 10.1093/ije/dyw341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Niles DE, Duval‐Arnould J, Skellett S, Knight L, Su F, Raymond TT, Sweberg T, Sen AI, Atkins DL, Friess SH, et al. Characterization of pediatric in‐hospital cardiopulmonary resuscitation quality metrics across an international resuscitation collaborative. Pediatr Crit Care Med. 2018;19:421–432. DOI: 10.1097/PCC.0000000000001520. [DOI] [PubMed] [Google Scholar]
- 31. Gupta P, Rettiganti M, Jeffries H, Scanlon M, Ghanayem N, Daufeldt J, Rice T, Wetzel R. Risk factors and outcomes of in‐hospital cardiac arrest following pediatric heart operations of varying complexity. Resuscitation. 2016;105:1–7. DOI: 10.1016/j.resuscitation.2016.04.022. [DOI] [PubMed] [Google Scholar]
- 32. Scholefield B, Raman S, Hussey A, Haigh F, Kanthimathinathan H, Skellett S, Peters M, Duncan H, Morris K. 152 predictive factors for survival after paediatric out‐of‐hospital cardiac arrest: a UK multicentre cohort study. Arch Dis Child. 2012;97:A43. DOI: 10.1136/archdischild-2012-302724.0152. [DOI] [Google Scholar]
- 33. Gov.uk . People living in deprived neighbourhoods. 2018; Ethnicity‐facts‐figures.service.gov.uk. Available at: https://www.ethnicity‐facts‐figures.service.gov.uk/uk‐population‐by‐ethnicity/demographics/people‐living‐in‐deprived‐neighbourhoods/latest. Accessed 18 December 2019.
- 34. Dhillon G, Lasa J, Aggarwal V, Checchia P, Bavare A. Cardiac arrest in the pediatric cardiac ICU. Pediatr Crit Care Med. 2019;20:233–242. DOI: 10.1097/PCC.0000000000001810. [DOI] [PubMed] [Google Scholar]
- 35. Gaies M, Clarke N, Donohue J, Gurney J, Charpie J, Hirsch J. Personnel and unit factors impacting outcome after cardiac arrest in a dedicated pediatric cardiac intensive care unit. Pediatr Crit Care Med. 2012;13:583–588. DOI: 10.1097/PCC.0b013e318238b272. [DOI] [PubMed] [Google Scholar]
- 36. Freeman C, Bennett T, Casper T, Larsen G, Hubbard A, Wilkes J, Bratton S. Pediatric and neonatal extracorporeal membrane oxygenation. Crit Care Med. 2014;42:512–519. DOI: 10.1097/01.ccm.0000435674.83682.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Stub D, Bernard S, Pellegrino V, Smith K, Walker T, Sheldrake J, Hockings L, Shaw J, Duffy SJ, Burrell A, et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation. 2015;86:88–94. DOI: 10.1016/j.resuscitation.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 38. Niles DE, Duval‐Arnould J, Skellett S, Knight L, Su F, Raymond TT, Sweberg T, Sen AI, Atkins DL, Friess SH, et al. Characterization of pediatric in‐hospital cardiopulmonary resuscitation quality metrics across an international resuscitation collaborative*. Pediatric Critical Care Medicine. 2018;19:421–432. DOI: 10.1097/PCC.0000000000001520. [DOI] [PubMed] [Google Scholar]
- 39. Lipe D, Giwa A, Caputo N, Gupta N, Addison J, Cournoyer A. Do out‐of‐hospital cardiac arrest patients have increased chances of survival when transported to a cardiac resuscitation center? J Am Heart Assoc. 2018;7:e011079. DOI: 10.1161/JAHA.118.011079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. NHS England . NHS England, Paediatric critical care and surgery in children review: Summary report. 2019; Available at: https://www.england.nhs.uk/publication/paediatric‐critical‐care‐and‐surgery‐in‐children‐review‐summary‐report/. Accessed 18 December 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S2


