Abstract
Melanogenesis is the process leading to the synthesis of melanin, the main substance that influences skin color and plays a pivotal role against UV damage. Altered melanogenesis is observed in several pigmentation disorders. Melanogenesis occurs in specialized cells called melanocytes, physically and functionally related by means of autocrine and paracrine interplay to other skin cell types. Several external and internal factors control melanin biosynthesis and operate through different intracellular signaling pathways, which finally leads to the regulation of microphthalmia-associated transcription factor (MITF), the key transcription factor involved in melanogenesis and the expression of the main melanogenic enzymes, including TYR, TYRP-1, and TYRP-2. Epigenetic factors, including microRNAs (miRNAs), are involved in melanogenesis regulation. miRNAs are small, single-stranded, non-coding RNAs, of approximately 22 nucleotides in length, which control cell behavior by regulating gene expression, mainly by binding the 3′ untranslated region (3′-UTR) of target mRNAs. This review collects data on the miRNAs involved in melanogenesis and how these miRNAs can modulate target gene expression. Bringing to light the biological function of miRNAs could lead to a wider understanding of epigenetic melanogenesis regulation and its dysregulation. This knowledge may constitute the basis for developing innovative treatment approaches for pigmentation dysregulation.
Keywords: melanocyte, melanogenesis, microRNA, skin pigmentation
1. Introduction
Skin represents the primary line of defense against environmental stressors, including chemical stimuli, microbial insults, allergens, and ultraviolet (UV) radiation. Protection from UV rays is essentially based on melanogenesis, the process leading to the synthesis of pigments called melanin, the main substance that influences skin color. Melanin protects the skin from harmful UV rays, as it can absorb UV and visible light and shows antioxidative and radical scavenging abilities, limiting UV-induced effects on cellular macromolecules, mainly DNA, thus protecting cells from genotoxic damage [1]. Therefore, reduced melanogenesis is also a major risk factor for melanoma and other skin cancers [2,3]. Nevertheless, increased melanogenesis and melanin accumulation is associated with hyperpigmentation disorders [4,5]. Skin hyperpigmentation, often associated with aging, hormonal changes, and UVB, is very common in clinical dermatology and includes dermal conditions such as melasma, chloasma, freckles, age spots, and sunspots [5]. In addition, both hyperpigmentation and hypopigmentation, as observed in vitiligo lesions, are frequently the consequence of inflammation, induced by skin stressors [6]. Indeed, the modulation of skin pigmentation still represents a challenge in treating dermatological disorders, despite several studies having investigated potential cures [7,8]. Melanin is produced by highly specialized cells called melanocytes that are in strict contact with other skin cells, especially keratinocytes. The process of skin coloration consists of melanin biosynthesis and the translocation of melanosomes, small organelles containing melanin, from melanocytes into epidermal keratinocytes [6,7,9].
Melanogenesis is a very complex process which includes the development, survival, and differentiation of melanocytes. It involves more than 150 genes and several signaling pathways that operate both at transcriptional and post-transcriptional levels in regulating the main melanogenic molecular players. These include transcription factors, enzymes, and regulatory molecules produced by melanocytes, as well as other skin cells including keratinocytes, dermal fibroblasts, and inflammatory and endocrine cells [6,7,10,11].
Altered gene expression and melanogenic regulatory factor activities are involved in melanogenesis dysfunction [4,11]. Increasingly, studies indicate that gene expression is also influenced by several epigenetic events, including chromatin modification, DNA methylation, and non-coding RNA classes such as long non-coding RNAs (lncRNAs) and microRNAs (miRNAs) [12,13,14,15]. Indeed, the role of miRNAs in melanogenesis has been widely investigated. The aim of this review is to collect recent information concerning the role of miRNAs in melanogenesis and its dysregulation. Studies investigating the role of miRNA in modulating tumor development and growth or metastasis in skin cancers were not included and reviewed by others [16]. Analysis of the biological function of miRNAs will allow for a better understanding of the molecular events involved in regulating skin pigmentation. We suggest that this knowledge may lead to the development of innovative diagnostic tools as well as treatment approaches for pigmentation-related disorders.
2. Melanin Biosynthesis
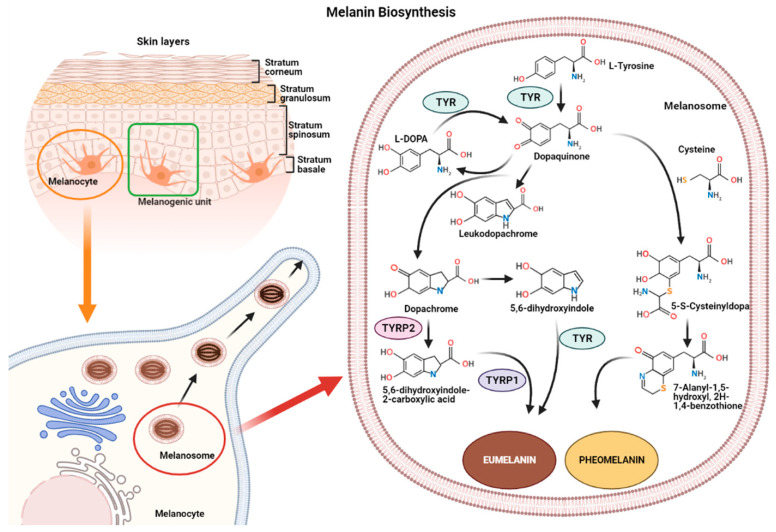
Melanin synthesis occurs in highly specialized cells called melanocytes, localized in the basal layer of the epidermis and hair follicles [17,18]. Melanocytes consist of several ramifications called dendrites that end in keratinocytes, and each melanocyte is strictly connected to more than 30 keratinocytes, constituting the melanogenic unit [19]. During melanogenesis, a series of sequential reactions synthesize melanin, which is translocated into neighboring keratinocytes by means of melanosomes [6,7,9].
Melanin production is controlled by several enzymes including tyrosinase (TYR), tyrosine hydroxylase I (THI), and phenylalanine hydroxylase (PAH) in the initiation phase of melanin synthesis. Tyrosinase-associated protein 1 (TYRP-1) and tyrosinase-associated protein 2 (TYRP-2), also called dopachrome tautomerase (DCT), operate in the later phase [4,20]. TYR is a membrane-bound glycoprotein which plays a key role in the process, as it is considered the rate-limiting enzyme for melanin biosynthesis (Figure 1).
Figure 1.
Representation of the melanogenic unit and melanin synthesis in melanosomes (left). Schematic representation of eumelanin and pheomelanin biosynthetic pathways (right).
The reaction catalyzed by TYR leads to L-tyrosine being transformed into dopaquinone by oxidation [21]. Dopaquinone is highly reactive and can follow two reaction chains from which eumelanin and pheomelanin originate:
-
(1)
In reactions leading to eumelanin production, dopaquinone undergoes intramolecular cyclization to produce leukodopachrome (cyclodopa). Cyclodopa undergoes redox exchange with another molecule of dopaquinone to form dopachrome and DOPA [21]. The dopachrome downstream process is branched in two ways. The first leads to the formation of 5,6-dihydroxyindole-2-carboxylic acid (DHICA) through TYRP-2 intervention and then into eumelanin by TYRP-1 conversion. The second leads to the conversion of dopachrome into 5,6-dihydroxyindole (DHI) and then into eumelanin involving TYR. At the end of this reaction, black-brownish eumelanin is formed.
-
(2)
In reactions leading to pheomelanin production, in the presence of cystein or glutathione, dopaquinone can be converted into 5-S-cysteinyldopa, or glutathionyldopa, which is then converted into quinoline and finally polymerized into red-yellow pheomelanin.
In the skin, both eumelanin and pheomelanin form complex heteropolymers. The total amount of melanin, as well as the ratio between eumelanin to pheomelanin, are considered to determine skin color. Indeed, the role of the ratio between eumelanin and pheomelanin is still under debate, as many authors indicate that it remains unchanged in various phototypes of human skin and, thus, skin color is dependent on total melanin amount [4,22]. Synthesized melanin is collected into melanosomes, which follow a complex maturation process and are transported to keratinocytes along actin filaments in association with motor proteins [4,23].
3. Melanogenesis Regulation
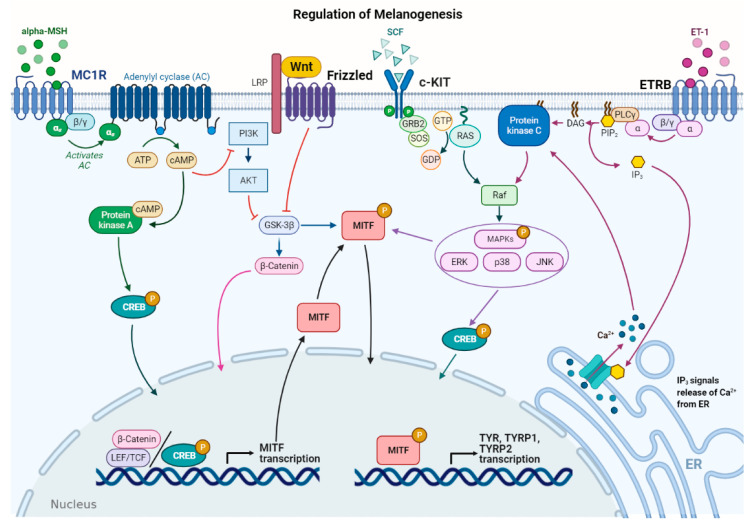
Several stimuli control melanogenesis, including external factors such as UV rays or environmental pollution [11]. Furthermore, a series of endogenous molecules released by melanocytes, keratinocytes, dermal fibroblasts, and immune cells modulate the process paracrinally and autocrinally. These are mainly the α-melanocyte stimulating hormone (α-MSH) and the adrenocorticotropic hormone (ACTH), derived from the cleavage of pro-opiomelanocortin (POMC), from both melanocytes and keratinocytes [11,24]. In addition, stem cell factor (SCF), peptide endothelin 1 (ET-1), hepatocyte growth factor (HGF), keratinocyte growth factor (KGF), basic fibroblast growth factor (bFGF), and inflammatory mediators such as cytokines, prostaglandin E2 (PGE2), and nitric oxide (NO) significantly regulate melanogenesis [25,26]. All these stimuli operate with the activation of several signaling pathways [9,27]. Detailed descriptions of the multiple pathways in melanogenesis have been recently reported by others [6,7,9,11]. Here, the main signaling pathways are briefly summarized (Figure 2).
Figure 2.
Main signaling pathways involved in melanogenesis regulation. α-melanocyte stimulating hormone (α-MSH) binds to melanocortin 1 receptor (MC1R), which increases cAMP levels, activating PKA and PI3K/AKT pathway. The former phosphorylates CREB protein, promoting MITF transcription; the latter interplays with Wnt/β-catenin pathway by phosphorylating GSK-3β, which, in turn, releases β-catenin to promote MITF transcription. Stem cell factor (SCF) binds to c-KIT receptor, activating MAPK pathway and phosphorylating CREB. Peptide endothelin 1 (ET-1) binds to its receptor, ETRB, activating PKC and stimulating MITF transcription. MITF is phosphorylated at the post-transcriptional level to promote transcription of the melanogenic enzymes.
In melanocytes, signaling pathways regulating melanogenesis operate through membrane receptors with different molecular activities. These receptors include G protein-coupled receptors (GPCRs) such as the melanocortin-1 receptor (MC1R), which is mainly expressed in melanocytes [28], adrenergic receptors, endothelin type B receptor (ETRB), frizzled receptor (FZD), and tyrosine kinase receptors such as tyrosine kinase receptor KIT, bFGF, and HGF receptors [7,29]. Most signaling pathways lead to the regulation of microphthalmia-associated transcription factor (MITF), a basic helix–loop–helix leucine zipper (bHLH-ZIP) transcription factor. MITF is the dominant transcription factor in melanogenesis as it controls melanocyte development, survival, and proliferation, as well as the steps involved in melanin synthesis [30,31]. MITF induces the transcription of the melanogenic genes, including TYR, TYRP-1, and TYRP-2, by binding to the conserved consensus elements of the promoter regions [31]. Moreover, MITF regulates several other genes involved in melanogenesis, including those required to control melanosome maturation, traffic, and distribution to keratinocytes [32]. Due to the prominent role of MITF, regulation of its expression and activity represents a key event in melanogenesis. At the transcriptional level, MITF expression is regulated by several transcriptional factors that bind the MITF promoter, including cyclic adenosine monophosphate (cAMP)-response element binding protein (CREB), paired box family of transcription factor 3 (PAX3), sex determining region Y-box 9 and 10 (Sox9, Sox10), and Wnt/β-catenin pathway effector lymphoid enhancer-binding factor 1 (LEF-1) [7,31].
Furthermore, MITF activity is regulated at the post-transcriptional level mainly by phosphorylation [33]. MITF may be phosphorylated by several kinases such as MAPK, p38, ribosomal S6 kinase (RSK), and GSK3β [7,11,34,35]. MITF phosphorylation can favor the recruitment of transcriptional coactivator CBP/P300 of CREB, thus increasing the transcription of TYR, TYRP-1, and TYRP-2 melanogenic enzymes [31]. The MAPK signaling pathway can be activated by several extracellular factors, which operate through tyrosine kinase receptors including SCF, a relevant signal produced by keratinocytes and fibroblasts, and HGF and bFGF, mainly produced by keratinocytes [36]. Notably, melanogenesis-related signaling pathways may be positively or negatively modulated by several inflammatory factors that finally regulate skin pigmentation. This regulation is very complex as some molecules have a stimulatory effect on melanogenesis, while others show inhibitory effects. In addition, the production of these inflammatory mediators depends on the communication between several epidermal and dermal cells, as well as specific stimuli inducing inflammation [6].
As mentioned above, UV rays represent external stimuli with significant effects on melanogenic signaling pathways, resulting in increased melanin production. Several cellular and molecular processes are involved in the UV–skin reaction. Indeed, UV irradiation induces MITF expression and consequently melanogenic gene expression [3,31]. Acquired knowledge shows that UV irradiation influences different skin cell types, including melanocytes, keratinocytes, and dermal fibroblasts. UV-induced melanogenesis has been associated with the release of several molecules, including α-MSH, ACTH, SCF, and ET-1, which regulate the signaling pathways described above [25,36,37,38].
4. miRNA Activities and Identification
MicroRNAs (miRNAs) represent a class of non-coding RNAs of approximately 21–23 nucleotides in length. Since their discovery in 1993 [39], miRNAs have been largely studied as essential regulators of gene expression. miRNAs are highly conserved among species and are found in different cell types and organisms, including plants, animals, and viruses [40,41]. It is now estimated that miRNAs target approximately 60% of genes in humans and other mammals [42]. Due to their role in mRNA expression regulation, miRNAs are involved in all cellular activities, including proliferation, differentiation, migration, apoptosis, and immune responses, both in normal and pathological conditions [43,44,45,46]. Several mechanisms ensure high stability in miRNAs. Since they can be easily detected in almost all bodily fluids, miRNAs are now considered important biological markers and potential therapeutic molecules [47]. Inside cells, miRNAs derive from long precursor transcripts which give rise to mature miRNAs through a multi-step process and are then incorporated into an RNA–protein complex known as the RNA-Induced Silencing Complex (RISC) [48]. miRNA activity mainly induces gene expression reduction by binding to sequences in the 3′ untranslated region (3′-UTR) of target genes. This can lead to mRNA target degradation, or inhibition of translation and reduction in protein levels [45]. However, miRNA activities show higher complexity as each miRNA can target different genes and several miRNAs can regulate the same gene’s expression. Moreover, the strict interplay between long non-coding RNAs (lncRNAs) and miRNAs contributes to gene expression regulation [40,45,49].
In general, from a methodological point of view, investigations into miRNA functions and roles in a selected process include a preliminary phase of miRNA identification using high-throughput methods such as microarray, followed by target gene identification with a bioinformatics approach. Finally, target genes need to be validated by 3′-UTR reporter assays and analysis conducted on induced cellular effects following transfection experiments with miRNA mimics and antagomiRs [50]. miRNAs are involved in skin development and functions both in normal and pathological conditions [16]. Furthermore, increasing evidence shows that selected miRNAs regulate specific events occurring in the skin, such as melanogenesis, as detailed below [51,52].
4.1. miRNA Regulating MITF
Due to the key role of MITF as an essential regulator of the melanogenic process, several studies have investigated miRNAs with potential effects on MITF expression and consequent regulation of mRNA levels in melanogenic enzymes [3,30,31,53] (Table 1). Some preliminary studies concerning melanogenesis regulation by miRNAs have been performed in fiber-producing animals, such as alpaca, due to the contribution of melanin synthesis to coat color and the specific interest of alpaca breeders in animal color coat modulation. Differences in miRNA profiles from alpaca skins with different colored coats were identified and most differentially expressed miRNAs showed predicted targets involved in pigmentation [54,55]. These results led to further investigation concerning the functional role of selected miRNAs. Data obtained by Zhu Z et al. (2010) demonstrated the functional role of miR-25 in reducing MITF mRNA and protein, TYR, and TYRP-1 expression in cultured melanocytes. In addition, an inverse relationship was observed between miR-25 level and coat color. Similarly, in alpaca melanocytes, miR508-3p also directly targets MITF, binding to the 3′-UTR of the gene. miR508-3p overexpression downregulated MITF expression, resulting in a decrease in TYR, TYRP-2, and melanin production [56]. Interestingly, in 2012, Dong C. et al. investigated the role of miR-137, another miR-targeting MITF, in a transgenic mice model [57]. Initially investigating melanoma cells lines, where its overexpression downregulated MITF [58], it was found that miR-137 also decreased the expression of the MITF protein and its downstream genes in transgenic mice. Notably, miR-137 had an impact on coat color, demonstrating that modulating a specific miR may significantly regulate melanogenesis, at least in animal models [57].
Table 1.
microRNAs regulating MITF in melanogenesis.
| miRNA | Cell Model | Target Gene | Effect on Melanogenesis |
Ref. |
|---|---|---|---|---|
| miR-25 | Alpaca melanocytes | MITF | Negative | [56] |
| miR508-3p | Alpaca melanocytes | MITF | Negative | [56] |
| miR-137 | Alpaca melanocytes | MITF | Negative | [58] |
| miR-675 | Melanocytes of melasma patients, keratinocytes of melasma | MITF | Negative | [5,59,60] |
| miR-218 | Melan-a murine melanocytes, human skin OTC | MITF | Negative | [61] |
| miR-183 | B16 melanoma cells | MITF | Negative | [62] |
| miR-340 | Human epidermal melanocytes (Pig-I) | MITF | Negative | [63,64] |
| miR-200a-3p | B16-4A5 melanoma cells | MITF | Negative | [52] |
| miR-148a-3p | B16-4A5 melanoma cells | MITF | Negative | [52] |
| miR-141-3p | B16-4A5 melanoma cells | MITF | Negative | [52] |
Other studies have identified miRNAs regulating skin pigmentation in human melanocytes. Particular interest has been shown in miR-675, another miR which targets MITF and was to be found expressed at low levels in the hyperpigmented skin of melasma patients. In melanocytes or keratinocytes derived from melasma patients, miR-675 upregulation decreased TYRP-1 and TYRP-2 expression, whereas its knockdown increased their expression. Interestingly, miR-675 was also identified in exosomes released from keratinocytes into the extracellular environment [5,59,60]. Another miR involved in melanogenesis by binding the 3′-UTR in MITF is miR-218, which downregulated TYR, TYRP-1, and DCT mRNA and protein levels, reducing melanin content in immortalized melan-a murine melanocytes. In agreement with these data, miR-218 also suppressed melanogenesis in human pigmented skin organotypic culture (OTC) through MITF repression. Anti-miR-218 was also found to promote melanogenesis in human primary melanocytes [61].
Recently, other miRNAs, including miRNA-183 cluster, miR-340, miR-141-3p, and miR-200a-3p, have been investigated for their role in regulating MITF expression and melanogenesis [62]. Results of this research show that the miRNA-183 cluster targets the 3′-UTR of MITF in B16 mouse melanoma cells. miRNA-183 cluster overexpression decreased MITF, TYR, TYRP-1, and DCT expression and melanin production. Conversely, knockdown of the miRNA-183 cluster increased MITF, TYR, TYRP-1, and DCT expression and, consequently, melanin levels. The miR-183 cluster was also involved in regulating the MEK/ERK signaling pathway implicated in cell proliferation and migration, by modulating mitogen-activated protein kinase 1 (MEK1), extracellular regulated protein kinases1/2 (ERK1/2), and CREB expression [62]. miR-340, which was first identified in melanoma cell lines for its ability to bind specifically to the 3′-UTR of MITF [64], has been also investigated in immortalized human epidermal melanocytes (Pig-1), where it downregulates MITF expression and melanin synthesis [63]. Recently, miR-141-3p and miR-200a-3p have been identified as MITF regulators [52]. In this study, comparing miRNA expression profiles in B16-4A5 mouse melanoma cells which were treated or untreated with α-MSH led to 13 miRNAs being identified as differentially expressed through miRNA array analysis. miR-141-3p, miR-200a-3p, and miR-148a-3p, which target MITF, were downregulated in α-MSH-stimulated cells when compared to untreated cells. Furthermore, miR-141-3p and miR-200a-3p overexpression suppressed MITF expression and TYR activity in B16-4A5 cells. Notably, the inhibitory effect on melanin synthesis was confirmed in a three-dimensional tissue culture model of the human epidermis (3D-MHE model) [52].
4.2. miRNAs Regulating Other Genes in Melanogenesis
Besides the abovementioned studied group of miRNAs, with significant regulatory roles in MITF, other miRNAs are involved in melanogenesis by regulating the expression of other molecular targets, including melanogenic enzymes, transcription factors, or components of the signaling pathways which regulate melanogenesis (Table 2).
Table 2.
Other microRNAs involved in melanogenesis.
| miRNA | Cell Model | Target Gene | Effect on Melanogenesis |
Ref. |
|---|---|---|---|---|
| miR-434-5p | Mouse skin, human skin cell cultures | TYR | Negative | [65] |
| miR-330-5p | Melanoma cells, normal human melanocytes | TYR | Negative | [56,67] |
| miR-203 | Keratinocytes exposed to UV | Kinesin Superfamily Protein 5b | Positive | [67] |
| miR-3196 | Keratinocytes exposed to UV | Unknown target gene | Positive | [67] |
| miR-21a-5p | Human melanocytes | SOX5 | Positive | [68] |
| miR-145 | Murine melan-a melanocytes | Myo5a | Negative | [56] |
| miR-380-3p | Alpaca melanocytes | SOX6 | Negative | [56] |
| miR-200c | Normal human epidermal keratinocytes (NHEK) | SOX1 | Positive | [69] |
| miR-27a-3p | Alpaca and Mouse melanocytes | Wnt3a | Negative | [54,70] |
| miR-379 | Alpaca melanocytes | IGF1R | Negative | [71] |
| miR-143-5p | Human melanocytes | Myo5a | Negative | [72] |
| miR-143-5p | Alpaca melanocytes | TAK1 | Negative | [73] |
| miR-125b | WM266-4 human melanoma cells, MNT1 human melanoma cells | SH3BP4 | Negative | [60] |
Several miRNAs, including miR-450b-5p, miR-1208, miR-326, miR-434-5p, miR330-5p, miR-125, miR-145, and miR-203, have been predicted as targeting TYR and most also target other genes, including MITF [65,66].
Wu et al. used a miR-434-5p homologue to target TYR in cells cultured in vitro as well as in an animal model and showed efficient melanin synthesis reduction. Similarly, miR-330-5p downregulated TYR in melanoma cells and normal melanocytes, inducing depigmentation without affecting cell proliferation [66]. This miR has been also identified in exosomes derived from keratinocytes [56]. In this study, exosomes carrying miR-330-5p caused a decrease in melanin production and TYR expression in melanocytes. Similarly, miR-330-5p overexpression in melanocytes confirmed its inhibitory activity on melanogenesis. Several other miRNAs, such as miR-203, which targets Kinesin Superfamily Protein 5b, involved in melanosome transfer, and miR-3196, with unknown target genes, have been identified in human-derived exosomes from keratinocytes and have shown an ability to increase melanin content in melanocytes [67]. Indeed, exosomes released by Black keratinocytes, as well as Caucasian UV-irradiated keratinocytes, were able to induce increased TYR activity and melanogenic gene expression in melanocytes, at least partly as a result of miR content.
As reported above, several miRNAs which directly target MITF are involved in melanogenesis. Conversely, MITF expression may be subject to more complex regulation. For example, it has been shown that miR-21a-5p overexpression downregulated the SOX5 target, as well as β-catenin and CDK2 protein expression, in normal human melanocytes. In agreement with SOX5 involvement in melanogenesis, its downregulation induced an increase in MITF and melanogenic enzymes’ expression, with consequent stimulation of melanogenesis [68]. Several other miRNAs have been identified as regulators of SOX transcription factors [56,69,74]. miR-145, which was initially identified as a miR regulated by UV treatment and forskolin in murine melan-a melanocytes, significantly modulates several genes involved in pigmentation. miR-145 overexpression or downregulation reduced or increased the expression of several genes involved in melanin biosynthesis, such as SOX9, MITF, TYR, and TYRP-1 [74,75], and in melanosome transfer, such as Myosin Va (Myo5a), Rab27a, and fascin1 (Fscn1), respectively [76]. Notably, miR-145 targeted the 3′-UTR binding site of Myo5a, a molecular motor involved in the intracellular trafficking of vesicles and organelles. A further miR that binds an SOX family component is miR-380-3p, which targets SOX6 by binding to the 3′-UTR region. In alpaca melanocytes, miR-380-3p overexpression downregulated SOX6 and increased β-catenin. Differently from studies indicating that β-catenin induces MITF transcription, in this study, miR-380-3p overexpression caused decreased mRNA levels of melanin-related genes including MITF, TYR, TYRP-1, and DCT, suggesting other SOX6 activities in MITF regulation [56].
Recently, miR-200c has been identified as a SOX1 regulator. Specifically, miR-200c induced SOX1 downregulation by direct binding to the SOX1 3′-UTR, leading to intranuclear β-catenin upregulation and increased expression of MITF-dependent gene expression as well as melanogenesis. These effects were induced in normal human epidermal melanocytes (NHEM) treated with exosomes containing miR-200c, produced by normal human epidermal keratinocytes (NHEK). Notably, miR-200c was found at low levels in exosomes derived from keratinocytes in vitiligo lesions compared to exosomes from NHEK, with a consequent inhibition in melanin production [69]. Some miRNAs have also been involved in modulating the extracellular ligands which regulate melanogenic signaling pathways. An example is miR-27a-3p, which directly targets Wnt3a, a component of the Wnt signaling pathway. miR-27a-3p was found to be expressed at higher levels in alpaca white skin compared to brown skin [54] and was similarly related to skin color in mice [70]. Furthermore, its functional role in downregulating Wnt3a, and thus inhibiting β-catenin and melanogenesis, was confirmed in mouse melanocytes transfected with miR-27a-3p [70]. In addition, miR-379 was shown to modulate insulin-like growth factor receptor I (IGFR1) in alpaca melanocytes. Insulin-like growth factor 1 (IGF1), mainly produced in dermal cells, has been shown to improve melanogenesis through the cAMP pathway. Likewise, miR-379 overexpression reduced melanogenesis by inhibiting the cAMP response element (CRE)-binding protein (CREB)/(MITF) pathway in alpaca melanocytes [71].
Finally, miRNAs involved in the regulation of melanosome processing and transfer have been also identified. Among them, miR-143-5p targets Myo5a, which belongs to the complex Rab27a/MLPH/Myo5a that connects melanosomes to the actin cytoskeleton in human melanocytes [72]. In a more recent study, Qi S. et al. inhibited miR-143-5p expression using Short Tandem Target Mimics (STTMs) in order to evaluate the functional role of miR-143-5p. As a consequence, increased melanogenic gene expression, including MITF, TYR, and TYRP-1, MLPH, and Rab27, and melanin production were observed [77]. This result indicates the effective possibility of modulating melanin biosynthesis by a miRNA-regulating approach. In addition, miR-143-5p overexpression induces a decrease in TGF-β-activated kinase 1 (TAK1) expression with consequent effects on melanocyte migration and proliferation and MITF downregulation in alpaca melanocytes. Therefore, miR-143-5p may regulate melanogenesis by modulating different gene targets [73]. By means of a bioinformatic approach, followed by experimental validation, miR-125b has also been shown to directly target SRC homology 3 domain-binding protein 4 (SH3BP4), a gene regulated by MITF, which may act by controlling melanogenic enzymes’ distribution to melanosomes or the mTOR signaling pathway. Indeed, when miR-125b was overexpressed in WM266-4 and MNT1 human melanoma cells, decreased levels of the melanogenic enzymes TYR and DCT were observed, although these genes are not direct miR-125b targets [78].
4.3. miRNA Regulated by UV Rays
UV rays can modify intracellular functions in different ways: by directly or indirectly damaging DNA through reactive oxygen species (ROS), inducing apoptosis, cell cycle arrest, and carcinogenesis. The expression profiles of the miRNAs involved in these events are modified by UV irradiation [79,80,81]. Among the UV-induced effects, it is well known that there is a correlation between UVB irradiation and melanogenesis stimulation [1]. miRNA profiling in irradiated mouse melanocytes has been helpful in identifying miRNAs involved in melanogenesis, such as miR-145 [74]. Furthermore, several miRNAs targeting different pigmentation genes have been involved in UV ray effects, including miR-145, miR-137, miR-148, and miR-25 [57,82,83].
miR-340 upregulation was identified in pigmented cells treated with UVB irradiation among miRNAs related to UV irradiation. Studies have shown that miR-340 significantly represses RhoA protein expression and stimulates melanosome transport [81]. Recently, the functional role of miR-340 has been further investigated in immortalized human epidermal melanocytes (Pig-1), confirming that its expression is modulated by UV and that it downregulates MITF expression and melanin synthesis. Notably, miR-340 mimics decreased melanin content in irradiated cells [63]. A further example of a miR potentially being involved in UV-induced pigmentation modulation is miR-21. The latter has been largely investigated in melanoma and shown to be increased by UV radiation in melanocytes, keratinocytes, and fibroblasts [84]. In mouse skin melanocytes, miR-21 has been shown to enhance MITF expression by targeting SOX5 [85]. Inversely, miR-21a-5p has been observed with different levels of activity in UV-irradiated A375.S2 human melanoma and B16F10 melanoma mouse cells. Indeed, in these UV-treated cells, increased melanin content was associated with an increase in α-MSH expression and reduced EGFR and Akt phosphorylation. miR-21 overexpression negatively modulated these UV-induced effects [86]. Interestingly, this miR has been also involved in communication between melanocytes and keratinocytes. Extracellular vesicles derived from UVA-exposed melanocytes modified keratinocyte behavior by inducing miR-21 upregulation and TGF-β and IL-6/STAT3 signaling pathway activation [87]. UVA and UVB rays also induce changes in miRNA produced by keratinocytes [88,89]. Accumulating evidence indicates that exosomes and exosomal miRNAs represent an effective means of communication for melanocytes and keratinocytes [56]. Notably, in Caucasian human keratinocytes, UV rays induce the release of miR, such as hsa-miR-3196, which may stimulate melanin synthesis in melanocytes [67]. Recently, miR-675 production by human keratinocytes has been shown and its role as a paracrine regulator of melanogenesis has been confirmed in vitro, indicating increased exosomal miR-675 in cells irradiated with a 585 nm light emitting diode (LED) and its ability to attenuate melanogenesis in melanocytes [90].
4.4. Common miRNAs in Melanogenesis and Melanomagenesis
Several miRNAs regulating melanogenesis play an important role in melanoma [91]. For instance, miR-340, miR-218, and miR-137, which inhibit melanogenesis, have a tumor suppressor role during melanomagenesis by negatively regulating MITF expression [58,61,64,92]. Other miRNAs which regulate melanogenesis, including miR-379, -200c, -203, -200a-3p, -125b, -183, -508-3p, -675, -143-5p, -141-3p, -145, and -330-5p, can act as tumor suppressors in melanomagenesis, although the target genes may differ from those identified in melanogenesis. On the contrary, miR-21a-5p, -25, and -27a-3p have shown an oncogenic role, being upregulated in metastatic melanoma and during tumor progression [93,94].
Interestingly, some miRNAs involved in both melanogenesis and melanomagenesis, such as miR-21a-3p, -25, -3196, -145, -137, -148, and -675 are induced by UV rays, the main environmental risk factor for melanoma [79,80,81,95].
5. Conclusions
Melanogenesis is the main event involved in regulating skin color and plays a pivotal role in protection from UV rays, as it limits UV damage and genotoxic effects [1]. Melanogenesis dysregulation is observed in several skin pigmentation disorders and has been related to skin cancerogenesis [5]. Therefore, melanogenesis control and regulation play a significant role in skin pathophysiology. Melanogenesis involves different cell types and is regulated by several external and internal factors, including UV rays, hormones, growth factors, and cytokines, which act autocrinally and paracrinally by modulating several cellular signaling pathways [26]. Here, studies showing that several miRNAs participate in the complex regulation of melanogenesis have been reviewed. These data show the significant impact and functional role of miRNAs in the melanogenic process. miRNAs have been identified using different approaches, including miRNA profile evaluation, bioinformatic analysis, and experimental investigation of cellular effects induced by miRNA regulation [48]. Above all, melanocytes and melanoma cell lines were used as they represent the key cell players in melanogenesis. Conversely, since the complex regulation of melanogenesis is based on the strict interplay between melanocytes and keratinocytes, as well other skin cells [6,10,36,96], some studies have investigated miRNAs expressed in keratinocytes, providing relevant information concerning the fine cellular and molecular regulation involved in this process.
Overall, most identified miRNAs, including miR-25, miR508-3p, miR-137, miR-218, miR-183, miR-340, miR-141-3p, and miR-200a-3p, target MITF, leading to a decrease in its gene expression and consequent melanogenesis inhibition [52,58,61,62,63,73]. These miRNAs include miR-137, which was able to modulate coat color in transgenic mice [57]. This result appears to be of particular interest as it demonstrates that modulating miRNA expression may be a way to significantly regulate melanogenesis in vivo. In humans, some miRNAs have also been associated with changes in skin color and pigmentation dysfunction, including miR-675 [60], which was expressed at a low level in the hyperpigmented skin of melasma patients, and miR-200c, which was found at low levels in exosomes obtained from vitiligo patients [69]. In addition, miRNAs can regulate melanogenesis by modulating the expression of genes coding for extracellular mediators such as wnt3a [54,70]; membrane receptors such as IGF-IR [71]; intracellular components of the melanogenic signaling pathways, such as SOX transcription factors; or molecules involved in melanosome transfer, such as Myo5a, Rab27a, and Fscn1 [7,56,69,74,76]. Notably, several miRNAs, including miR-675, miR-330-5p, miR-203, miR-3196, and mir-200c, have been identified in exosomes derived from keratinocytes and their functional role in the regulation of melanocyte activities and melanogenesis has been proven [5,59,60,67,69,97]. This identifies miRNAs as important extracellular molecular mediators, thus increasing our understanding of the close correlation between skin cell types which regulate melanogenesis. In this context, further knowledge on the potential contribution of dermal fibroblasts, as well as inflammatory skin cells, is needed [6,69].
Due to the essential role of UV rays in skin pigmentation, several studies have also investigated miRNAs modulated by UV irradiation, showing that miRNA levels can be changed by UV radiation [79,80,81]. These miRNAs deserve particular attention due to their involvement in skin hyperpigmentation induced by UV rays, and potentially in skin carcinogenesis [84]. Indeed, here, we have reported that several miRNAs can be involved in both melanogenesis and melanomagenesis. Knowledge on miRNAs physiologically involved in melanogenesis is extremely important; alterations in melanocyte miRNA signatures might serve as diagnostic markers for melanoma progression and may help to plan targeted therapies in the future [92].
Several causes and events can lead to altered pigmentation by regulating inflammatory reactions. Therefore, while the role of inflammation in modulating cell behavior and the signaling pathways involved in skin pigmentation is beginning to be elucidated [6], further investigation concerning miRNAs involved in skin inflammation might be helpful. In addition, based on increasing knowledge on the relationship between different classes of non-coding RNAs, new relevant information is expected from studies concerning the interaction and reciprocal regulation of miRNAs and other non-coding RNA classes [14,98]. In conclusion, increasing evidence shows the involvement of miRNAs in melanogenesis and skin pigmentation disorders. Elucidation of the role of melanogenic signaling pathways, as well as intercellular communication, might be improved by a deeper understanding of miRNAs’ activities in controlling and regulating gene targets and melanogenesis and by identifying novel miRNAs. Encouraging data are beginning to show the effective role of miRNAs in the regulation of skin pigmentation, confirming their role in more complex in vitro models such as three-dimensional skin organotypic culture models [61]. Notably, recent topical transfection of miR-141-3p and miR-200a-3p to three-dimensional reconstructed human skin tissue inhibited α-MSH-induced melanin biosynthesis with similar efficiency as obtained by arbutin, a well-known depigmentating molecule [52].
Further investigations using advanced in vitro models, such as co-culture of skin cells and organotypic skin culture, are to be encouraged in order to better clarify the essential role of miRNAs in melanogenesis, taking into account the strict correlation among cells that participate in the process [99]. Epigenetic regulation of melanogenesis provides a novel insight into the melanogenesis mechanism and suggests potential therapeutic approaches for the unsolved problem of skin pigmentation disorders [7], based on the use of miRNA mimics and antagomiRs [52,100].
Acknowledgments
We thank Georgia Emma Gili for revising the English text of the manuscript.
Abbreviations
| 3′-UTR | three prime untranslated region |
| 3D-MHE model | three-dimensional tissue culture model of human epidermis |
| ACTH | adrenocorticotrophic hormone |
| AKT | protein kinase B |
| bFGF | basic fibroblast growth factor |
| bHLH-ZIP | basic helix-loop-helix leucine zipper |
| cAMP | cyclic adenosine monophosphate |
| CDK2 | cyclin-dependent kinase 2 |
| CREB | cAMP-responsive element binding protein |
| DAG | diacyglycerol |
| DCT | dopachrome tautomerase |
| ERK1/2 | extracellular regulated protein kinases1/2 |
| ETRB | endothelin type B receptor |
| Fscn1 | fascin1 |
| FZD | frizzled receptor |
| GPCRs | G protein-coupled receptors |
| GSK3β | glycogen synthase kinase 3β |
| HGF | hepatocyte growth factor |
| IGF-1R | insulin-like growth factor receptor I |
| IL-6 | interleukin-6 |
| IP3 | inositol triphosphate |
| KGF | keratinocyte growth factor |
| L-DOPA | dihydroxyphenylalanine |
| LED | light emitting diode |
| LEF-1 | lymphoid enhancer-binding factor 1 |
| LEF-TCF | lymphoid enhancing factor-1/T-cell factor |
| lncRNA | long non-coding RNAs |
| MAPK | mitogen-activated protein kinase |
| MC1R | melanocortin 1 receptor |
| MEK1 | mitogen-activated protein kinase 1 |
| miRNAs | microRNAs |
| MITF | microphthalmia-associated transcription factor |
| MLPH | melanophilin |
| MYO5A | myosin VA |
| NHEK | normal human epidermal keratinocytes |
| NHEM | normal human epidermal melanocytes |
| NO | nitric oxide |
| OTC | skin organotypic culture |
| PAX3 | paired box family of transcription box 3 |
| PGE2 | prostaglandin E2 |
| PI3K | phosphoinositide-3 kinase |
| Pig-1 | immortalized human epidermal melanocytes |
| PIP2 | phosphatidylinositol 4,5-bisphosphate |
| PKA | protein kinase A |
| PLCγ | activated phospholipase Cγ |
| POMC | proopiomelanocortin |
| RISC | RNA-Induced Silencing Complex |
| RNA | ribonucleic acid |
| ROS | reactive oxygen species |
| RSK | ribosomal S6 kinase |
| SCF | stem cell factor |
| SH3BP4 | SRC homology 3 domain-binding protein 4 |
| SOX | sex-determining region Y-box |
| SOX1 | sex determining region Y-box 1 |
| SOX10 | sex determining region Y-box 10 |
| SOX5 | sex determining region Y-box 5 |
| SOX6 | sex determining region Y-box 6 |
| SOX9 | sex determining region Y-box |
| STAT3 | signal transducer and activator of transcription 3 |
| STTMs | short tandem target mimic |
| TAK1 | TGF-β-activated kinase 1 |
| TGF-β | transforming growth factor-β |
| TYR | tyrosinase |
| TYRP-1 | tyrosinase-related protein 1 |
| TYRP-2 | tyrosinase-related protein 2 |
| UV | ultraviolet |
| UVA | ultraviolet A |
| UVB | ultraviolet B |
| WNT3A | Wnt family member 3A |
| α-MSH | α-melanocyte stimulating hormone |
Author Contributions
Conceptualization, Y.H., M.D.M. and F.M.; writing—original draft preparation, Y.H., I.B. and M.D.M.; figure and table preparation, L.O.-G., G.D.M., I.B.; writing—review and editing, Y.H., M.D.M. and F.M. supervision, M.D.M., F.M., M.T.; funding acquisition, M.D.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the University of Ferrara FAR (M.D.M. and F.M., 2020) and PRIN 2017 (F.M.), while M.D.M. received a financial contribution from Morgan Srl, Monteviale (VI), ITALY.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. Y.H. is an employee of Morgan Srl.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.D’Orazio J., Jarrett S., Amaro-Ortiz A., Scott T. UV Radiation and the Skin. Int. J. Mol. Sci. 2013;14:2222. doi: 10.3390/ijms140612222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller A.J., Mihm M.C. Melanoma. N. Engl. J. Med. 2006;355:51–65. doi: 10.1056/NEJMra052166. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen N.T., Fisher D.E. MITF and UV Responses in Skin: From Pigmentation to Addiction. Pigment. Cell Melanoma Res. 2019;32:224–236. doi: 10.1111/pcmr.12726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hida T., Kamiya T., Kawakami A., Ogino J., Sohma H., Uhara H., Jimbow K. Elucidation of Melanogenesis Cascade for Identifying Pathophysiology and Therapeutic Approach of Pigmentary Disorders and Melanoma. Int. J. Mol. Sci. 2020;21:6129. doi: 10.3390/ijms21176129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee A.-Y. Recent Progress in Melasma Pathogenesis. Pigment Cell Melanoma Res. 2015;28:648–660. doi: 10.1111/pcmr.12404. [DOI] [PubMed] [Google Scholar]
- 6.Fu C., Chen J., Lu J., Yi L., Tong X., Kang L., Pei S., Ouyang Y., Jiang L., Ding Y., et al. Roles of Inflammation Factors in Melanogenesis (Review) Mol. Med. Rep. 2020;21:1421–1430. doi: 10.3892/mmr.2020.10950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pillaiyar T., Manickam M., Jung S.-H. Recent Development of Signaling Pathways Inhibitors of Melanogenesis. Cell Signal. 2017;40:99–115. doi: 10.1016/j.cellsig.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Madireddy S., Crane J.S. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2021. Hypopigmented Macules. [PubMed] [Google Scholar]
- 9.D’Mello S.A.N., Finlay G.J., Baguley B.C., Askarian-Amiri M.E. Signaling Pathways in Melanogenesis. Int. J. Mol. Sci. 2016;17:1144. doi: 10.3390/ijms17071144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yamaguchi Y., Passeron T., Watabe H., Yasumoto K., Rouzaud F., Hoashi T., Hearing V.J. The Effects of Dickkopf 1 on Gene Expression and Wnt Signaling by Melanocytes: Mechanisms Underlying Its Suppression of Melanocyte Function and Proliferation. J. Investig. Dermatol. 2007;127:1217–1225. doi: 10.1038/sj.jid.5700629. [DOI] [PubMed] [Google Scholar]
- 11.Serre C., Busuttil V., Botto J.-M. Intrinsic and Extrinsic Regulation of Human Skin Melanogenesis and Pigmentation. Int. J. Cosmet. Sci. 2018;40:328–347. doi: 10.1111/ics.12466. [DOI] [PubMed] [Google Scholar]
- 12.Horsburgh S., Fullard N., Roger M., Degnan A., Todryk S., Przyborski S., O’Reilly S. MicroRNAs in the Skin: Role in Development, Homoeostasis and Regeneration. Clin. Sci. 2017;131:1923–1940. doi: 10.1042/CS20170039. [DOI] [PubMed] [Google Scholar]
- 13.Yamada T., Hasegawa S., Iwata Y., Arima M., Kobayashi T., Numata S., Nakata S., Sugiura K., Akamatsu H. UV Irradiation-Induced DNA Hypomethylation around WNT1 Gene: Implications for Solar Lentigines. Exp. Dermatol. 2019;28:723–729. doi: 10.1111/exd.13949. [DOI] [PubMed] [Google Scholar]
- 14.Jiang L., Huang J., Hu Y., Lei L., Ouyang Y., Long Y., Li H., Li S., Yang L., Yang Y., et al. Identification of the CeRNA Networks in α-MSH-Induced Melanogenesis of Melanocytes. Aging. 2020;13:2700–2726. doi: 10.18632/aging.202320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lanzillotti C., De Mattei M., Mazziotta C., Taraballi F., Rotondo J.C., Tognon M., Martini F. Long Non-Coding RNAs and MicroRNAs Interplay in Osteogenic Differentiation of Mesenchymal Stem Cells. Front. Cell Dev. Biol. 2021;9:646032. doi: 10.3389/fcell.2021.646032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neagu M., Constantin C., Cretoiu S.M., Zurac S. MiRNAs in the Diagnosis and Prognosis of Skin Cancer. Front. Cell Dev. Biol. 2020;8:71. doi: 10.3389/fcell.2020.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Slominski A., Wortsman J., Plonka P.M., Schallreuter K.U., Paus R., Tobin D.J. Hair Follicle Pigmentation. J. Investig. Dermatol. 2005;124:13–21. doi: 10.1111/j.0022-202X.2004.23528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Slominski A., Tobin D.J., Shibahara S., Wortsman J. Melanin Pigmentation in Mammalian Skin and Its Hormonal Regulation. Physiol. Rev. 2004;84:1155–1228. doi: 10.1152/physrev.00044.2003. [DOI] [PubMed] [Google Scholar]
- 19.Nordlund J.J. The Melanocyte and the Epidermal Melanin Unit: An Expanded Concept. Dermatol. Clin. 2007;25:271–281. doi: 10.1016/j.det.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 20.Schallreuter K.U., Kothari S., Chavan B., Spencer J.D. Regulation of Melanogenesis—Controversies and New Concepts. Exp. Dermatol. 2008;17:395–404. doi: 10.1111/j.1600-0625.2007.00675.x. [DOI] [PubMed] [Google Scholar]
- 21.Land E.J., Ramsden C.A., Riley P.A. Quinone Chemistry and Melanogenesis. Methods Enzym. 2004;378:88–109. doi: 10.1016/S0076-6879(04)78005-2. [DOI] [PubMed] [Google Scholar]
- 22.Del Bino S., Ito S., Sok J., Nakanishi Y., Bastien P., Wakamatsu K., Bernerd F. Chemical Analysis of Constitutive Pigmentation of Human Epidermis Reveals Constant Eumelanin to Pheomelanin Ratio. Pigment Cell Melanoma Res. 2015;28:707–717. doi: 10.1111/pcmr.12410. [DOI] [PubMed] [Google Scholar]
- 23.Chang H., Choi H., Joo K.-M., Kim D., Lee T.R. Manassantin B Inhibits Melanosome Transport in Melanocytes by Disrupting the Melanophilin-Myosin Va Interaction. Pigment. Cell Melanoma Res. 2012;25:765–772. doi: 10.1111/pcmr.12002. [DOI] [PubMed] [Google Scholar]
- 24.Wakamatsu K., Graham A., Cook D., Thody A.J. Characterisation of ACTH Peptides in Human Skin and Their Activation of the Melanocortin-1 Receptor. Pigment Cell Res. 1997;10:288–297. doi: 10.1111/j.1600-0749.1997.tb00688.x. [DOI] [PubMed] [Google Scholar]
- 25.Tagashira H., Miyamoto A., Kitamura S.-I., Tsubata M., Yamaguchi K., Takagaki K., Imokawa G. UVB Stimulates the Expression of Endothelin B Receptor in Human Melanocytes via a Sequential Activation of the P38/MSK1/CREB/MITF Pathway Which Can Be Interrupted by a French Maritime Pine Bark Extract through a Direct Inactivation of MSK1. PLoS ONE. 2015;10:e0128678. doi: 10.1371/journal.pone.0128678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Imokawa G. Melanocyte Activation Mechanisms and Rational Therapeutic Treatments of Solar Lentigos. Int. J. Mol. Sci. 2019;20:3666. doi: 10.3390/ijms20153666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin J.Y., Fisher D.E. Melanocyte Biology and Skin Pigmentation. Nature. 2007;445:843–850. doi: 10.1038/nature05660. [DOI] [PubMed] [Google Scholar]
- 28.Roberts D.W., Newton R.A., Beaumont K.A., Helen Leonard J., Sturm R.A. Quantitative Analysis of MC1R Gene Expression in Human Skin Cell Cultures. Pigment Cell Res. 2006;19:76–89. doi: 10.1111/j.1600-0749.2005.00286.x. [DOI] [PubMed] [Google Scholar]
- 29.Mosca S., Cardinali G., Flori E., Briganti S., Bottillo I., Mileo A.M., Maresca V. The PI3K Pathway Induced by AMSH Exerts a Negative Feedback on Melanogenesis and Contributes to the Release of Pigment. Pigment Cell Melanoma Res. 2021;34:72–88. doi: 10.1111/pcmr.12910. [DOI] [PubMed] [Google Scholar]
- 30.Levy C., Khaled M., Fisher D.E. MITF: Master Regulator of Melanocyte Development and Melanoma Oncogene. Trends Mol. Med. 2006;12:406–414. doi: 10.1016/j.molmed.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 31.Vachtenheim J., Borovanský J. “Transcription Physiology” of Pigment Formation in Melanocytes: Central Role of MITF. Exp. Dermatol. 2010;19:617–627. doi: 10.1111/j.1600-0625.2009.01053.x. [DOI] [PubMed] [Google Scholar]
- 32.Ohbayashi N., Fukuda M. Recent Advances in Understanding the Molecular Basis of Melanogenesis in Melanocytes. F1000Research. 2020;9 doi: 10.12688/f1000research.24625.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hsiao J.J., Fisher D.E. The Roles of Microphthalmia-Associated Transcription Factor and Pigmentation in Melanoma. Arch. Biochem. Biophys. 2014;563:28–34. doi: 10.1016/j.abb.2014.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khaled M., Larribere L., Bille K., Aberdam E., Ortonne J.-P., Ballotti R., Bertolotto C. Glycogen Synthase Kinase 3beta Is Activated by CAMP and Plays an Active Role in the Regulation of Melanogenesis. J. Biol. Chem. 2002;277:33690–33697. doi: 10.1074/jbc.M202939200. [DOI] [PubMed] [Google Scholar]
- 35.Saha B., Singh S.K., Sarkar C., Bera R., Ratha J., Tobin D.J., Bhadra R. Activation of the Mitf Promoter by Lipid-Stimulated Activation of P38-Stress Signalling to CREB. Pigment Cell Res. 2006;19:595–605. doi: 10.1111/j.1600-0749.2006.00348.x. [DOI] [PubMed] [Google Scholar]
- 36.Wang Y., Viennet C., Robin S., Berthon J.-Y., He L., Humbert P. Precise Role of Dermal Fibroblasts on Melanocyte Pigmentation. J. Dermatol. Sci. 2017;88:159–166. doi: 10.1016/j.jdermsci.2017.06.018. [DOI] [PubMed] [Google Scholar]
- 37.Chakraborty A.K., Funasaka Y., Slominski A., Ermak G., Hwang J., Pawelek J.M., Ichihashi M. Production and Release of Proopiomelanocortin (POMC) Derived Peptides by Human Melanocytes and Keratinocytes in Culture: Regulation by Ultraviolet B. Biochim. Biophys. Acta. 1996;1313:130–138. doi: 10.1016/0167-4889(96)00063-8. [DOI] [PubMed] [Google Scholar]
- 38.Cui R., Widlund H.R., Feige E., Lin J.Y., Wilensky D.L., Igras V.E., D’Orazio J., Fung C.Y., Schanbacher C.F., Granter S.R., et al. Central Role of P53 in the Suntan Response and Pathologic Hyperpigmentation. Cell. 2007;128:853–864. doi: 10.1016/j.cell.2006.12.045. [DOI] [PubMed] [Google Scholar]
- 39.Lee R.C., Feinbaum R.L., Ambros V. The C. Elegans Heterochronic Gene Lin-4 Encodes Small RNAs with Antisense Complementarity to Lin-14. Cell. 1993;75:843–854. doi: 10.1016/0092-8674(93)90529-Y. [DOI] [PubMed] [Google Scholar]
- 40.Finotti A., Fabbri E., Lampronti I., Gasparello J., Borgatti M., Gambari R. MicroRNAs and Long Non-Coding RNAs in Genetic Diseases. Mol. Diagn. Ther. 2019;23:155–171. doi: 10.1007/s40291-018-0380-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rotondo J.C., Mazzoni E., Bononi I., Tognon M., Martini F. Association Between Simian Virus 40 and Human Tumors. Front. Oncol. 2019;9:670. doi: 10.3389/fonc.2019.00670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pradhan A.K., Bhoopathi P., Talukdar S., Scheunemann D., Sarkar D., Cavenee W.K., Das S.K., Emdad L., Fisher P.B. MDA-7/IL-24 Regulates the MiRNA Processing Enzyme DICER through Downregulation of MITF. Proc. Natl. Acad. Sci. USA. 2019;116:5687–5692. doi: 10.1073/pnas.1819869116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Correia de Sousa M., Gjorgjieva M., Dolicka D., Sobolewski C., Foti M. Deciphering MiRNAs’ Action through MiRNA Editing. Int. J. Mol. Sci. 2019;20:6249. doi: 10.3390/ijms20246249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huang W. MicroRNAs: Biomarkers, Diagnostics, and Therapeutics. Methods Mol. Biol. 2017;1617:57–67. doi: 10.1007/978-1-4939-7046-9_4. [DOI] [PubMed] [Google Scholar]
- 45.Mazziotta C., Lanzillotti C., Iaquinta M.R., Taraballi F., Torreggiani E., Rotondo J.C., Otòn-Gonzalez L., Mazzoni E., Frontini F., Bononi I., et al. MicroRNAs Modulate Signaling Pathways in Osteogenic Differentiation of Mesenchymal Stem Cells. Int. J. Mol. Sci. 2021;22:2362. doi: 10.3390/ijms22052362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Iaquinta M.R., Lanzillotti C., Mazziotta C., Bononi I., Frontini F., Mazzoni E., Oton-Gonzalez L., Rotondo J.C., Torreggiani E., Tognon M., et al. The Role of MicroRNAs in the Osteogenic and Chondrogenic Differentiation of Mesenchymal Stem Cells and Bone Pathologies. Theranostics. 2021 doi: 10.7150/thno.55664. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nedaeinia R., Manian M., Jazayeri M.H., Ranjbar M., Salehi R., Sharifi M., Mohaghegh F., Goli M., Jahednia S.H., Avan A., et al. Circulating Exosomes and Exosomal MicroRNAs as Biomarkers in Gastrointestinal Cancer. Cancer Gene. Ther. 2017;24:48–56. doi: 10.1038/cgt.2016.77. [DOI] [PubMed] [Google Scholar]
- 48.O’Brien J., Hayder H., Zayed Y., Peng C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018;9:402. doi: 10.3389/fendo.2018.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wawrzyniak O., Zarębska Ż., Rolle K., Gotz-Więckowska A. Circular and Long Non-Coding RNAs and Their Role in Ophthalmologic Diseases. Acta Biochim. Pol. 2018;65:497–508. doi: 10.18388/abp.2018_2639. [DOI] [PubMed] [Google Scholar]
- 50.Grillone K., Riillo C., Scionti F., Rocca R., Tradigo G., Guzzi P.H., Alcaro S., Di Martino M.T., Tagliaferri P., Tassone P. Non-Coding RNAs in Cancer: Platforms and Strategies for Investigating the Genomic “Dark Matter”. J. Exp. Clin. Cancer Res. 2020;39:117. doi: 10.1186/s13046-020-01622-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mione M., Bosserhoff A. MicroRNAs in Melanocyte and Melanoma Biology. Pigment Cell Melanoma Res. 2015;28:340–354. doi: 10.1111/pcmr.12346. [DOI] [PubMed] [Google Scholar]
- 52.Itoh T., Fukatani K., Nakashima A., Suzuki K. MicroRNA-141-3p and MicroRNA-200a-3p Regulate α-Melanocyte Stimulating Hormone-Stimulated Melanogenesis by Directly Targeting Microphthalmia-Associated Transcription Factor. Sci. Rep. 2020;10:2149. doi: 10.1038/s41598-020-58911-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen T., Zhao B., Liu Y., Wang R., Yang Y., Yang L., Dong C. MITF-M Regulates Melanogenesis in Mouse Melanocytes. J. Dermatol. Sci. 2018;90:253–262. doi: 10.1016/j.jdermsci.2018.02.008. [DOI] [PubMed] [Google Scholar]
- 54.Tian X., Jiang J., Fan R., Wang H., Meng X., He X., He J., Li H., Geng J., Yu X., et al. Identification and Characterization of MicroRNAs in White and Brown Alpaca Skin. BMC Genom. 2012;13:555. doi: 10.1186/1471-2164-13-555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhu Z., He J., Jia X., Jiang J., Bai R., Yu X., Lv L., Fan R., He X., Geng J., et al. MicroRNA-25 Functions in Regulation of Pigmentation by Targeting the Transcription Factor MITF in Alpaca (Lama Pacos) Skin Melanocytes. Domest. Anim. Endocrinol. 2010;38:200–209. doi: 10.1016/j.domaniend.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 56.Liu X., Du B., Zhang P., Zhang J., Zhu Z., Liu B., Fan R. MiR-380-3p Regulates Melanogenesis by Targeting SOX6 in Melanocytes from Alpacas (Vicugna Pacos) BMC Genom. 2019;20:962. doi: 10.1186/s12864-019-6343-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dong C., Wang H., Xue L., Dong Y., Yang L., Fan R., Yu X., Tian X., Ma S., Smith G.W. Coat Color Determination by MiR-137 Mediated down-Regulation of Microphthalmia-Associated Transcription Factor in a Mouse Model. RNA. 2012;18:1679–1686. doi: 10.1261/rna.033977.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bemis L.T., Chen R., Amato C.M., Classen E.H., Robinson S.E., Coffey D.G., Erickson P.F., Shellman Y.G., Robinson W.A. MicroRNA-137 Targets Microphthalmia-Associated Transcription Factor in Melanoma Cell Lines. Cancer Res. 2008;68:1362–1368. doi: 10.1158/0008-5472.CAN-07-2912. [DOI] [PubMed] [Google Scholar]
- 59.Valadi H., Ekström K., Bossios A., Sjöstrand M., Lee J.J., Lötvall J.O. Exosome-Mediated Transfer of MRNAs and MicroRNAs Is a Novel Mechanism of Genetic Exchange between Cells. Nat. Cell Biol. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 60.Kim N.-H., Choi S.-H., Kim C.-H., Lee C.H., Lee T.R., Lee A.-Y. Reduced MiR-675 in Exosome in H19 RNA-Related Melanogenesis via MITF as a Direct Target. J. Investig. Dermatol. 2014;134:1075–1082. doi: 10.1038/jid.2013.478. [DOI] [PubMed] [Google Scholar]
- 61.Guo J., Zhang J., Wang W., Cheung F.W., Lu Y., Ng C., Kung H., Liu W. MicroRNA-218 Inhibits Melanogenesis by Directly Suppressing Microphthalmia-Associated Transcription Factor Expression. RNA Biol. 2014;11:732–741. doi: 10.4161/rna.28865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Du B., Liu X., Khan A., Wan S., Guo X., Xue J., Fan R. MiRNA-183∼96∼182 Regulates Melanogenesis, Cell Proliferation and Migration in B16 Cells. Acta Histochem. 2020;122:151508. doi: 10.1016/j.acthis.2020.151508. [DOI] [PubMed] [Google Scholar]
- 63.Yang Y., Wei X., Bai J., Huang M., Hao T., Hao Y., Wang Y., Li C. MicroRNA-340 Is Involved in Ultraviolet B-Induced Pigmentation by Regulating the MITF/TYRP1 Axis. J. Int. Med. Res. 2020;48:300060520971510. doi: 10.1177/0300060520971510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Goswami S., Tarapore R.S., Poenitzsch Strong A.M., TeSlaa J.J., Grinblat Y., Setaluri V., Spiegelman V.S. MicroRNA-340-Mediated Degradation of Microphthalmia-Associated Transcription Factor (MITF) MRNA Is Inhibited by Coding Region Determinant-Binding Protein (CRD-BP) J. Biol. Chem. 2015;290:384–395. doi: 10.1074/jbc.M114.590158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wu D.T., Chen J.S., Chang D.C., Lin S.-L. Mir-434-5p Mediates Skin Whitening and Lightening. Clin. Cosmet. Investig. Dermatol. 2008;1:19–35. doi: 10.2147/ccid.s4181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rambow F., Bechadergue A., Saintigny G., Morizot F., Mahé C., Larue L. MiR-330-5p Targets Tyrosinase and Induces Depigmentation. J. Investig. Dermatol. 2014;134:2846–2849. doi: 10.1038/jid.2014.231. [DOI] [PubMed] [Google Scholar]
- 67.Lo Cicero A., Delevoye C., Gilles-Marsens F., Loew D., Dingli F., Guéré C., André N., Vié K., van Niel G., Raposo G. Exosomes Released by Keratinocytes Modulate Melanocyte Pigmentation. Nat. Commun. 2015;6:7506. doi: 10.1038/ncomms8506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Aguennouz M., Guarneri F., Oteri R., Polito F., Giuffrida R., Cannavò S.P. Serum Levels of MiRNA-21-5p in Vitiligo Patients and Effects of MiRNA-21-5p on SOX5, Beta-Catenin, CDK2 and MITF Protein Expression in Normal Human Melanocytes. J. Dermatol. Sci. 2021;101:22–29. doi: 10.1016/j.jdermsci.2020.10.014. [DOI] [PubMed] [Google Scholar]
- 69.Zhao C., Wang D., Wang X., Mao Y., Xu Z., Sun Y., Mei X., Song J., Shi W. Down-Regulation of Exosomal MiR-200c Derived from Keratinocytes in Vitiligo Lesions Suppresses Melanogenesis. J. Cell Mol. Med. 2020;24:12164–12175. doi: 10.1111/jcmm.15864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhao Y., Wang P., Meng J., Ji Y., Xu D., Chen T., Fan R., Yu X., Yao J., Dong C. MicroRNA-27a-3p Inhibits Melanogenesis in Mouse Skin Melanocytes by Targeting Wnt3a. Int. J. Mol. Sci. 2015;16:921. doi: 10.3390/ijms160510921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu B., Zhang J., Hu S., Qi S., Jia Q., Yang W., Yang S., Ji K., Liu X., Dong C., et al. MicroRNA-379 Mediates Pigmentation, Migration and Proliferation of Melanocytes by Targeting the Insulin-like Growth Factor 1 Receptor. Exp. Dermatol. 2020;29:467–476. doi: 10.1111/exd.14095. [DOI] [PubMed] [Google Scholar]
- 72.Alves C.P., Yokoyama S., Goedert L., Pontes C.L.S., Sousa J.F., Fisher D.E., Espreafico E.M. MYO5A Gene Is a Target of MITF in Melanocytes. J. Investig. Dermatol. 2017;137:985–989. doi: 10.1016/j.jid.2016.11.026. [DOI] [PubMed] [Google Scholar]
- 73.Ji K., Zhang P., Zhang J., Fan R., Liu Y., Yang S., Hu S., Liu X., Dong C. MicroRNA 143-5p Regulates Alpaca Melanocyte Migration, Proliferation and Melanogenesis. Exp. Dermatol. 2018;27:166–171. doi: 10.1111/exd.13480. [DOI] [PubMed] [Google Scholar]
- 74.Dynoodt P., Mestdagh P., Van Peer G., Vandesompele J., Goossens K., Peelman L.J., Geusens B., Speeckaert R.M., Lambert J.L.W., Van Gele M.J.L. Identification of MiR-145 as a Key Regulator of the Pigmentary Process. J. Investig. Dermatol. 2013;133:201–209. doi: 10.1038/jid.2012.266. [DOI] [PubMed] [Google Scholar]
- 75.Harris M.L., Baxter L.L., Loftus S.K., Pavan W.J. Sox Proteins in Melanocyte Development and Melanoma. Pigment Cell Melanoma Res. 2010;23:496–513. doi: 10.1111/j.1755-148X.2010.00711.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Van Gele M., Geusens B., Schmitt A.-M., Aguilar L., Lambert J. Knockdown of Myosin Va Isoforms by RNAi as a Tool to Block Melanosome Transport in Primary Human Melanocytes. J. Investig. Dermatol. 2008;128:2474–2484. doi: 10.1038/jid.2008.100. [DOI] [PubMed] [Google Scholar]
- 77.Qi S., Liu B., Zhang J., Liu X., Dong C., Fan R. Knockdown of MicroRNA-143-5p by STTM Technology Affects Eumelanin and Pheomelanin Production in Melanocytes. Mol. Med. Rep. 2019;20:2649–2656. doi: 10.3892/mmr.2019.10492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kim K.-H., Bin B.-H., Kim J., Dong S.E., Park P.J., Choi H., Kim B.J., Yu S.J., Kang H., Kang H.H., et al. Novel Inhibitory Function of MiR-125b in Melanogenesis. Pigment Cell Melanoma Res. 2014;27:140–144. doi: 10.1111/pcmr.12179. [DOI] [PubMed] [Google Scholar]
- 79.Jayanthy A., Setaluri V. Light-Regulated MicroRNAs. Photochem. Photobiol. 2015;91:163–172. doi: 10.1111/php.12386. [DOI] [PubMed] [Google Scholar]
- 80.Guo L., Huang Z.-X., Chen X.-W., Deng Q.-K., Yan W., Zhou M.-J., Ou C.-S., Ding Z.-H. Differential Expression Profiles of MicroRNAs in NIH3T3 Cells in Response to UVB Irradiation. Photochem. Photobiol. 2009;85:765–773. doi: 10.1111/j.1751-1097.2008.00482.x. [DOI] [PubMed] [Google Scholar]
- 81.Jian Q., An Q., Zhu D., Hui K., Liu Y., Chi S., Li C. MicroRNA 340 Is Involved in UVB-Induced Dendrite Formation through the Regulation of RhoA Expression in Melanocytes. Mol. Cell Biol. 2014;34:3407–3420. doi: 10.1128/MCB.00106-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jiang S., Yu X., Dong C. MiR-137 Affects Melanin Synthesis in Mouse Melanocyte by Repressing the Expression of c-Kit and Tyrp2 in SCF/c-Kit Signaling Pathway. Biosci. Biotechnol. Biochem. 2016;80:2115–2121. doi: 10.1080/09168451.2016.1200455. [DOI] [PubMed] [Google Scholar]
- 83.Cha H.J., Kim O.-Y., Lee G.T., Lee K.S., Lee J.H., Park I.-C., Lee S.-J., Kim Y.R., Ahn K.J., An I.-S., et al. Identification of Ultraviolet B Radiation-induced MicroRNAs in Normal Human Dermal Papilla Cells. Mol. Med. Rep. 2014;10:1663–1670. doi: 10.3892/mmr.2014.2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Melnik B.C., John S.M., Carrera-Bastos P., Schmitz G. MicroRNA-21-Enriched Exosomes as Epigenetic Regulators in Melanomagenesis and Melanoma Progression: The Impact of Western Lifestyle Factors. Cancers. 2020;12:2111. doi: 10.3390/cancers12082111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wang P., Zhao Y., Fan R., Chen T., Dong C. MicroRNA-21a-5p Functions on the Regulation of Melanogenesis by Targeting Sox5 in Mouse Skin Melanocytes. Int. J. Mol. Sci. 2016;17:959. doi: 10.3390/ijms17070959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lin K.-Y., Chen C.-M., Lu C.-Y., Cheng C.-Y., Wu Y.-H. Regulation of MiR-21 Expression in Human Melanoma via UV-Ray-Induced Melanin Pigmentation. Environ. Toxicol. 2017;32:2064–2069. doi: 10.1002/tox.22421. [DOI] [PubMed] [Google Scholar]
- 87.Wäster P., Eriksson I., Vainikka L., Öllinger K. Extracellular Vesicles Released by Melanocytes after UVA Irradiation Promote Intercellular Signaling via MiR21. Pigment Cell Melanoma Res. 2020;33:542–555. doi: 10.1111/pcmr.12860. [DOI] [PubMed] [Google Scholar]
- 88.Zhou B., Xu Y., Permatasari F., Liu W., Li W., Guo X., Huang Q., Guo Z., Luo D. Characterization of the MiRNA Profile in UVB-Irradiated Normal Human Keratinocytes. Exp. Dermatol. 2012;21:317–319. doi: 10.1111/j.1600-0625.2012.01465.x. [DOI] [PubMed] [Google Scholar]
- 89.Kraemer A., Chen I.-P., Henning S., Faust A., Volkmer B., Atkinson M.J., Moertl S., Greinert R. UVA and UVB Irradiation Differentially Regulate MicroRNA Expression in Human Primary Keratinocytes. PLoS ONE. 2013;8:e83392. doi: 10.1371/journal.pone.0083392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jin S., Chen L., Xu Z., Xing X., Zhang C., Xiang L. 585 Nm Light-Emitting Diodes Inhibit Melanogenesis through Upregulating H19/MiR-675 Axis in LEDs-Irradiated Keratinocytes by Paracrine Effect. J. Dermatol. Sci. 2020;98:102–108. doi: 10.1016/j.jdermsci.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 91.Sabarimurugan S., Royam M.M., Das A., Das S., Gothandam K.M., . Jayaraj R. Systematic Review and Meta-Analysis of the Prognostic Significance of MiRNAs in Melanoma Patients. Mol. Diagn. Ther. 2018;22:653–669. doi: 10.1007/s40291-018-0357-5. [DOI] [PubMed] [Google Scholar]
- 92.Möller K., Sigurbjornsdottir S., Arnthorsson A.O., Pogenberg V., Dilshat R., Fock V., Brynjolfsdottir S.H., Bindesboll C., Bessadottir M., Ogmundsdottir H.M., et al. MITF Has a Central Role in Regulating Starvation-Induced Autophagy in Melanoma. Sci. Rep. 2019;9:1055. doi: 10.1038/s41598-018-37522-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Varrone F., Caputo E. The MiRNAs Role in Melanoma and in Its Resistance to Therapy. Int. J. Mol. Sci. 2020;21:878. doi: 10.3390/ijms21030878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tang H., Xu X., Xiao W., Liao Y., Xiao X., Li L., Li K., Jia X., Feng H. Silencing of MicroRNA-27a Facilitates Autophagy and Apoptosis of Melanoma Cells through the Activation of the SYK-dependent MTOR Signaling Pathway. J. Cell. Biochem. 2019;120:13262–13274. doi: 10.1002/jcb.28600. [DOI] [PubMed] [Google Scholar]
- 95.Melnik B.C. MiR-21: An Environmental Driver of Malignant Melanoma? J. Transl. Med. 2015;13 doi: 10.1186/s12967-015-0570-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Takano K., Hachiya A., Murase D., Tanabe H., Kasamatsu S., Takahashi Y., Moriwaki S., Hase T. Quantitative Changes in the Secretion of Exosomes from Keratinocytes Homeostatically Regulate Skin Pigmentation in a Paracrine Manner. J. Dermatol. 2020;47:265–276. doi: 10.1111/1346-8138.15202. [DOI] [PubMed] [Google Scholar]
- 97.Liu Y., Xue L., Gao H., Chang L., Yu X., Zhu Z., He X., Geng J., Dong Y., Li H., et al. Exosomal MiRNA Derived from Keratinocytes Regulates Pigmentation in Melanocytes. J. Dermatol. Sci. 2019;93:159–167. doi: 10.1016/j.jdermsci.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 98.Brahmbhatt H.D., Gupta R., Gupta A., Rastogi S., Misri R., Mobeen A., Ghosh A., Kothari P., Sitaniya S., Scaria V., et al. The Long Noncoding RNA MALAT1 Suppresses MiR-211 to Confer Protection from Ultraviolet-Mediated DNA Damage in Vitiligo Epidermis by Upregulating Sirtuin 1. Br. J. Dermatol. 2020 doi: 10.1111/bjd.19666. [DOI] [PubMed] [Google Scholar]
- 99.Randall M.J., Jüngel A., Rimann M., Wuertz-Kozak K. Advances in the Biofabrication of 3D Skin in Vitro: Healthy and Pathological Models. Front. Bioeng. Biotechnol. 2018;6:154. doi: 10.3389/fbioe.2018.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gerloff D., Sunderkötter C., Wohlrab J. Importance of MicroRNAs in Skin Oncogenesis and Their Suitability as Agents and Targets for Topical Therapy. Skin Pharmacol. Physiol. 2020;33:270–279. doi: 10.1159/000509879. [DOI] [PMC free article] [PubMed] [Google Scholar]