Abstract
Morbihan syndrome is a rare entity characterized by persistent erythema and solid edema of upper two-thirds of the face. Although its etiology is poorly understood, it is known to have a wide differential diagnosis and is frequently under-recognized.1–3 We report two such cases of Morbihan syndrome in patients that responded well to treatment with a combination of 2.5% hydrocortisone cream, brimonidine 0.33% topical gel, metronidazole gel and 100 mg doxycycline twice daily. This report emphasizes the necessity of biopsy for clinical correlation in cases of chronic facial edema. It also serves to highlight a potential association of Morbihan syndrome to diabetes mellitus through recently discovered pathophysiology of diabetes on the lymphatic system. It underscores the effectiveness of our therapeutic regimen in the context of other treatment regimen effectiveness. Finally, it highlights novel advances into the diagnosis and treatment of the disease.
Keywords: Dermatology, pathology, inflammatory disease, Morbihan
Introduction
Morbihan syndrome is a rare syndrome that presents with solid facial edema usually in the third or fourth decade of life.1,2 The clinical course of Morbihan syndrome is marked by facial edema that appears slowly and spreads regionally to the forehead, glabella, eyelids, and cheeks. 2 As Morbihan syndrome shares considerable morphological and histological overlap with many granulomatous and inflammatory facial diseases, diagnosis can be challenging. The core symptoms of chronic, local facial edema, and erythema suggest a broad differential diagnosis, including sarcoidosis, Hansen’s disease, systemic lupus erythematosus, cutaneous leishmaniasis, foreign body granuloma, facial granuloma, superior vena cava syndrome, and scleredema of Buschke.1,3 Similarly, adverse drug reactions should be suspected, especially concerning barbiturates, chlorpromazine, diltiazem, and isotretinoin.1–3 The most convincing mimickers are inflammatory dermatoses with facial involvement, including rosaceous lymphedema and Melkersson–Rosenthal syndrome. 2 While not specific to Morbihan syndrome, the slow-onset and chronic course of the disease are important clinical features that can aid in differentiation from other etiologies.
Case report 1
A 67-year-old Caucasian male with a history of non-insulin-dependent diabetes mellitus and ocular rosacea presented with complaints of chronic facial edema and erythema. The facial edema had begun 4 years previously. The Patient denied a history of acne vulgaris. Physical examination revealed periorbital and maxillary facial edema with associated erythema extending over the malar region (Figure 1). A 4-mm punch biopsy showed mild spongiosis with peri-adnexal mixed infiltrate and dermal edema (Figure 2). The dermis showed perivascular and perifollicular lymphoplasmacytic inflammation, solar elastosis, and superficial dermal telangiectasia. No granulomata were observed. Colloidal iron and periodic acid–Schiff (PAS) stains were negative. The patient was initially treated with a regimen of 2.5% hydrocortisone cream, brimonidine 0.33% topical gel, and metronidazole gel. His treatment regimen was later expanded to include 100 mg doxycycline twice daily. This treatment regimen resulted in documented improvement at 3 months following doxycycline initiation with disease resolution at one-year follow-up.
Figure 1.

Case 1—Edema over the periorbital region and cheek with surrounding erythema.
Figure 2.
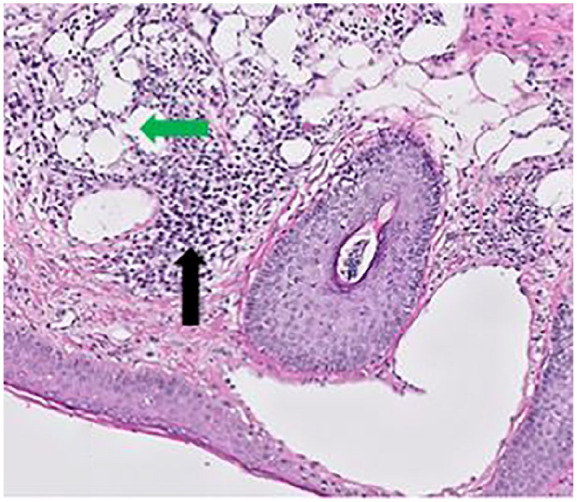
Low power (10×) magnification shows perivascular and perifollicular lymphoplasmacytic inflammatory infiltrate (black arrows) and ectatic superficial dermal blood vessels (green arrow).
Case report 2
A 50-year-old Caucasian male with a past medical history significant for latent autoimmune insulin-dependent diabetes mellitus, rosacea, and acne vulgaris presented with chronic periorbital edema (Figure 3). He previously endorsed the presentation of reddish papules in conjunction with swelling that had resolved with oral antibiotic treatment. Physical examination revealed facial edema localized to the right periorbital region and several flesh-colored nodules along the right mandible. A 3-mm punch biopsy showed dermis with perivascular and perifollicular lymphoplasmacytic inflammation, solar elastosis, and superficial dermal telangiectasias (Figure 4). No granulomata were observed. Colloidal iron and PAS stains were negative. The patient was started on doxycycline 100 mg twice daily and once-weekly topical permethrin with partial improvement at 3 months. At this time, permethrin was discontinued and brimonidine 0.33% topical gel and 2.5% hydrocortisone cream were added. Following three additional months, the patient noticed a majority clearance and resolution of edema and erythema. At 1-year follow-up, there was complete resolution of disease with no documented recurrence.
Figure 3.

Case 2—Edema predominantly over the periorbital region.
Figure 4.
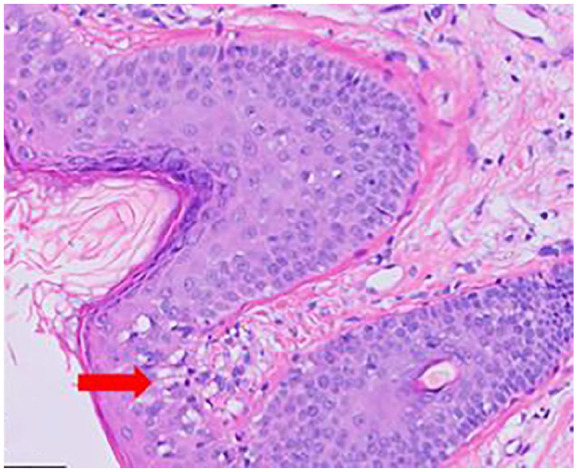
High power (40×) magnification shows spongiosis which is exaggerated in the dermo-epidermal junction (red arrow).
Discussion
In the cases presented, initial clinician suspicion for Morbihan syndrome was high given the past medical history of rosacea in each patient. Other diagnoses were considered, but ultimately lower on the differential diagnosis due to inconsistent histories (e.g. lack of new exposures preceding the development of findings as seen in contact dermatitis) or lack of associated findings (e.g. tongue fissures or facial nerve defects as might be seen in Melkersson–Rosenthal disease). As disease presentation can vary widely, ultimately a biopsy was necessary for clinical correlation. Compared to previous literature, our cases reflect recent revisions in understanding the demographics of a “typical” Morbihan syndrome patient: middle age to elderly Caucasian, male, and a history of acne or rosacea. Previously, the classic Morbihan syndrome patient would have been a woman in her third or fourth decade of life, a hypothesis attributed to the increased prevalence of rosacea among women, which was suggested to be linked to a greater incidence of Morbihan syndrome. Beyond their initial presentation, these patients fit the treatment course defined in recent literature: initiation of tetracycline-based antibiotic therapy with clinical improvement occurring over the following 3 months, if observed. 4 Based on literature findings, the successful resolution of disease in our patients was improbable based on the observed efficacy of other treatment regimens. A literature review of 89 patients diagnosed with Morbihan syndrome who underwent with any treatment regimen found that 72% experienced at least partial response and 14% experiencing complete resolution of disease. However, men with Morbihan syndrome have been shown to have a decreased likelihood of disease resolution with treatment. 4 While both our patients were male, our second patient presented with a history of erythematous papules, which has been correlated with treatment response. 4 One possible reason for the decreased efficacy of treatment in men may be related to the general pattern of decreased willingness to seek care, which could result in an initial presentation at a later disease stage with greater, and less reversible, lymphatic damage. 5 In addition, the duration of treatment with antibiotics has been tied to successful disease resolution, which has led some to suggest that a 4- to 6-month course of antibiotics may be warranted for treatment. These factors may illustrate why our own treatment regimens were successful when others were not: earlier presentation, suggested by the lack of granulomata on histopathology, along with the history of papular/pustular presentation, and strong patient adherence over a 4- to 6-month period.
The difficulties in diagnosis and treatment can be attributed to poor understandings of disease pathophysiology. However, a common course has been established; edema has been suggested to result from poor lymphatic flow via lymphatic obstruction or post-inflammatory dermal fibrosis. At the histological level, the destruction of elastic connective tissue in the perivascular area leads to decreased vascular wall integrity and subsequent edema from exudation of fluid.2,6 Recent literature has rarely attempted to comment on or identify individual triggers that have led to the associated histological findings—likely due to the difficulty in identifying a trigger that precedes the insidious onset associated with the disease. Previously, inflammatory reactions to cosmetic product use or Demodex infestation have been suggested to be possible inciting factors for Morbihan syndrome.2,7 More recently, discoveries made in understanding the pathophysiology of non-insulin-dependent diabetes mellitus have shown how impaired nitric oxide signaling can disrupt lymphatic vascular integrity, which has important associations to the pathophysiology of Morbihan syndrome. 8 This new study supports findings from previous studies on diabetic rats, which revealed induced lymphatic flow abnormalities that were restored following insulin-based control of blood glucose. 9 Taken together, it is possible that disruptions to the lymphatic system resulting from diabetes mellitus could contribute to the formation of facial edema that characterizes Morbihan syndrome.
New advances in imaging may shed light on the anatomic changes that occur in the lymphatic system in association with Morbihan syndrome, and as a result, may allow inferences into the disease’s pathophysiology. Thus far, imaging has rarely been used in the diagnosis of Morbihan syndrome. Rarely, imaging has been utilized to assist in process of disease differentiation. Cerebrofacial magnetic resonance imaging (MRI) has been used in at least one case to rule out tumor compression or regional infectious causes as contributing mechanisms. 10 However, emerging technologies such as near-infrared (NIR) imaging and non-invasive contrast agent-free imaging systems (such as optical coherence tomography (OCT), optical frequency domain imaging (OFDI), and multispectral imaging) may be powerful tools for imaging of the lymphatic system and narrowing the broad differential that currently challenges clinicians. 11
Likewise, treatment effectiveness is often unsatisfactory. Inconsistent treatment efficacy, variation in medication dosage, and the loss of patients to follow-up are some commonly identified contributing factors. Current therapies tend to be focused around antibiotic-, corticosteroid-, or isotretinoin-based therapies—with combination therapies showing no advantage in efficacy. 4 Recent treatment modalities favor the use of antibiotics (e.g. doxycycline), brimonidine gels, and surgical correction. Treatment regimens have also been attempted with cyclin therapy, X-ray irradiation, lymphatic massage, interferon-gamma injections, antihistamines, and high-dose antibiotic only therapies. However, these generally fail to provide symptomatic resolution.6,10
In cases resistant to mainstay therapies, novel therapies including omalizumab, complex decongestive therapy (CDT), CO2 blepharoplasty, and surgical eyelid debulking may be used, and have shown some potential for symptomatic improvement.12–14 However among available cases, disease recurrence was noted within 6 months after treatment with CO2 blepharoplasty and eyelid debulking regimens.12,15 In two cases of isotretinoin-resistant disease, CDT was documented as providing improvement and later led to symptomatic resolution in one of these cases. 12 In addition, monthly omalizumab injections led to complete resolution in one case of steroid-resistant disease. 13 Recent application of surgical techniques such as lymphaticovenous anastomosis in conjunction with eyelid debulking has shown greater promise for the improvement of the most severe medication-resistant cases. Due to the rarity of the disease, better documentation is required moving forward to assess and recommend treatment regimens based on patient demographics, presentation, and histopathological findings.
Conclusion
Morbihan syndrome is a rare disease of unknown etiology presenting with erythema and edema of the upper two-thirds of the face. We report and discuss two such case presentations that showed disease resolution after quadrivalent treatment regimens of hydrocortisone cream, topical brimonidine, metronidazole, and oral doxycycline. For retinoid-resistant disease, several novel therapies exist that have been able to provide clinical improvement, and rarely, resolution of disease. This report emphasizes the necessity of biopsy clinical correlation to rule out similar conditions and suggests how recent discoveries in diabetes mellitus pathophysiology may contribute to Morbihan syndrome.
Footnotes
Authors’ note: This material was presented at the American Society of Dermatopathology national conference in October 2019, Orlando, FL, USA.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Joseph Nenow  https://orcid.org/0000-0002-4153-7969
https://orcid.org/0000-0002-4153-7969
References
- 1. Batra M, Bansal C, Tulsyan S. Granulomatous rosacea: unusual presentation as solitary plaque. Dermatol Online J 2011; 17: 9. [PubMed] [Google Scholar]
- 2. Wohlrab J, Lueftl M, Marsch WC. Persistent erythema and edema of the midthird and upper aspect of the face (morbus Morbihan): evidence of hidden immunologic contact urticaria and impaired lymphatic drainage. J Am Acad Dermatol 2005; 52(4): 595–602. [DOI] [PubMed] [Google Scholar]
- 3. Vasconcelos RC, Eid NT, Eid RT, et al. Morbihan syndrome: a case report and literature review. An Bras Dermatol 2016; 91(5 Suppl. 1): 157–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Boparai RS, Levin AM, Lelli GJ., Jr. Morbihan disease treatment: two case reports and a systematic literature review. Ophthalmic Plast Reconstr Surg 2019; 35(2): 126–132. [DOI] [PubMed] [Google Scholar]
- 5. Thompson AE, Anisimowicz Y, Miedema B, et al. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract 2016; 17: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Veraldi S, Francia C, Persico M. Morbihan syndrome. Indian Dermatol Online J 2013; 4: 122–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hu SW, Robinson M, Meehan SA, et al. Morbihan disease. Dermatol Online J 2012; 18: 27. [PubMed] [Google Scholar]
- 8. Scallan JP, Hill MA, Davis MJ. Lymphatic vascular integrity is disrupted in type 2 diabetes due to impaired nitric oxide signalling. Cardiovasc Res 2015; 107: 89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moriguchi P, Sannomiya P, Lara PF, et al. Lymphatic system changes in diabetes mellitus: role of insulin and hyperglycemia. Diabetes Metab Res Rev 2005; 21(2): 150–157. [DOI] [PubMed] [Google Scholar]
- 10. Aboutaam A, Hali F, Baline K, et al. Morbihan disease: treatment difficulties and diagnosis: a case report. Pan Afr Med J 2018; 30: 226–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Munn LL, Padera TP. Imaging the lymphatic system. Microvasc Res 2014; 96: 55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bechara FG, Jansen T, Losch R, et al. Morbihan’s disease: treatment with CO2 laser blepharoplasty. J Dermatol 2004; 31(2): 113–115. [DOI] [PubMed] [Google Scholar]
- 13. Kafi P, Edén I, Swartling C. Morbihan syndrome successfully treated with omalizumab. Acta Derm Venereol 2019; 99: 677–678. [DOI] [PubMed] [Google Scholar]
- 14. Renieri G, Brochhausen C, Pfeiffer N, et al. Chronisches Lidödem assoziiert mit Rosazea (morbus Morbihan): Differenzialdiagnostische Schwierigkeiten und Therapieoptionen. Klin Monbl Augenheilkd 2011; 228: 19–24. [DOI] [PubMed] [Google Scholar]
- 15. Hattori Y, Hino H, Niu A. Surgical lymphoedema treatment of Morbihan disease. Ann Plast Surg 2021; 86: 547–550. [DOI] [PubMed] [Google Scholar]


