Abstract
Purpose:
To introduce the principles and procedure of percutaneous elastic intramedullary nailing (PEIN) as a treatment for symptomatic incomplete atypical femoral fracture (SIAFF).
Methods:
From October 2014 to April 2019, 6 cases of SIAFF were treated with PEIN. Two pre-bent 4-mm stainless-steel nails were used to apply compressive force to the fracture site. The antegrade method was used for proximal fractures and the retrograde method for middle and distal femoral fractures. The femoral bowing angle in the coronal and sagittal planes, and the time required for callus formation and union, were evaluated on plain radiographs in both planes. Thigh pain, tenderness, and complications were also assessed.
Results:
The mean operating time was 65.00 ± 22.64 min. No case progressed to complete atypical fracture. In one case, fracture occurred around the point of nail entry after the patient fell from a chair on postoperative day 7. The incomplete fracture lines were united in 5 cases, after excluding one case with a complication. The time taken to confirm endocortical callus formation, fracture line disappearance, and clinical union was 2.11 ± 0.53, 6.45 ± 4.10, and 6.45 ± 3.65 months, respectively.
Conclusions:
PEIN is a quick, simple but effective treatment for SIAFF that considers the fracture mechanism and is applicable to cases with severe femoral bowing.
Level of evidence:
Level IV, case series.
Keywords: atypical femoral fracture, femoral bowing, prophylactic nailing, intramedullary elastic nailing
Introduction
A rigid intramedullary (IM) nail is mostly used to treat a complete atypical femoral fracture (AFF). However, once a complete fracture occurs, surgical treatment becomes difficult, and there is an increased risk of nonunion or delayed union, which leads to poor clinical outcomes. 1 Therefore, it is crucial to detect and treat symptomatic atypical fractures before a complete fracture develops. However, the treatment of symptomatic incomplete atypical femoral fracture (SIAFF) remains controversial. Prophylactic internal fixation is recommended, since SIAFF is very likely to progress to a complete fracture if left untreated. 1 -4 Fixing the entire femur using a rigid IM nail is the fixation method used most commonly. 5,6 However, it is often difficult to insert the nail into an incomplete fracture because of the geometric mismatch between the nail and femur. Moreover, surgery is complicated since there is a high probability of eccentric reaming due to the hard endosteal callus. 7 This increases the risk of complications, such as an iatrogenic fracture during surgery, protrusion of the distal nail end, or delayed union. 6,8 -11 Various countermeasures have been introduced to resolve this, 12 including modifying the entry, 13 using a nail designed for the contralateral femur, 7 or inserting the femoral nail with external rotation. 7
Rigid IM nails are mainly used because of the convenience of surgery. However, we believe that this method does not fully consider the pathophysiology of AFF, which typically involves a stress or insufficiency fracture. 14 These fractures are caused by lateral tensile and medial compression forces, which become stronger with severe femoral bowing. In recent studies, lateral plate fixation has been limited tried for prophylactic surgery. 15,16 Therefore, as a simple intervention that considers the pathophysiology, we introduced percutaneous elastic intramedullary nailing (PEIN), which we present here.
Materials and Methods
Patient Selection
From October 2014 to April 2019, 33 patients with a diagnosis of AFF underwent surgical treatment, of whom 24 had complete AFF. Preventive surgery was performed on the remaining 9 patients, who were diagnosed with SIAFF with an impending fracture and met all 4 criteria below:
Patients who met the definition of AFF in the 2013 American Society for Bone and Mineral Research Task Force Report 14 ;
Functional pain or tenderness during weight-bearing;
A radiolucent line with cortical thickening present on femoral radiographs;
Progression of the fracture line and symptoms after conservative treatment for at least 3 months.
Rigid IM nailing was performed on 4 of the 9 patients who underwent preventive surgery; the remaining 5 women underwent PEIN (performed 6 times in total) for SIAFF. The patients were followed for at least 1 year (Figures 1 and 2). The study design and protocol were approved by our institutional review board (IRB).
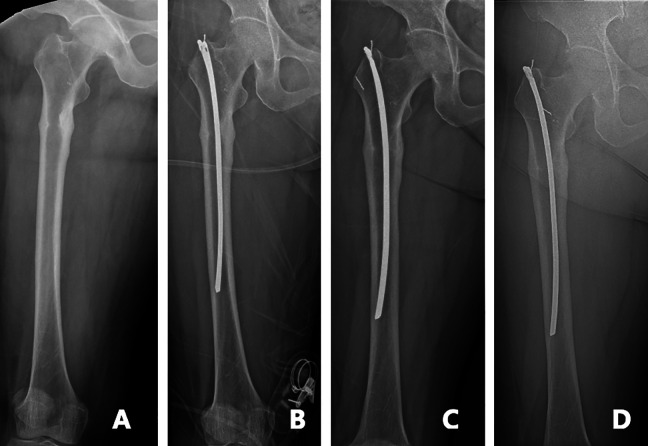
Figure 1.
A, 64-year-old female with atypical fracture in her right femur subtrochanteric area. B, In order to fit the suitable length of nail, we cut the 280 mm-length-nail and pre-overbend for using it. C, For 6-months after the prophylactic IM nailing, the fracture site was healed. D, 18-months after the surgery, the site has remained and she has no pain and tenderness around the fracture site.
Figure 2.
A, 88-year-old female with a crack in her right femur mid-shaft lateral cortex, which means atypical fracture. B, Pre-bending nail is used for fixation. C, 6-weeks after the prophylactic IM nailing, the bone healing process is shown in the radiograph around the fracture site. D, 31-months after the surgery the crack is healed and she has no pain and tenderness around the fracture site.
Operative Techniques and Rehabilitation
Each patient was placed on the fracture table in a supine position. An image amplifier (C-arm) was used to obtain anteroposterior (AP) and lateral views of the femur during the operation, which was performed under general or spinal anesthesia. Two 4.0-mm-diameter stainless steel nails (Ender Nail; Smith & Nephew Richards, USA) were used in 5 cases and a titanium elastic nail (Synthes, USA) was also used in one. The nail length was selected based on fluoroscopy images; where necessary, the nail was cut and bent to match the length of the femur. Pre-bending, which determines the degree of compressive force applied to the fracture site, was performed after considering the diameter of the femur, which was measured at the fracture site with the image amplifier. The flexible nail was pre-bent so that the distance between the line connecting both ends of the nail and apex was twice the diameter of the femur. Because of the nail’s elastic properties, the compression force should be applied to the lateral cortex at the fracture site if one end engages the cortex. The apex was contacted at the posteromedial cortex of the fracture (Figure 3). An approximately 1-cm-long 18-gauge wire was twisted and attached to the nail’s proximal hole to facilitate removal. IM nailing of proximal fractures was performed using the antegrade method, while the nailing of middle and distal fractures was performed using the retrograde method.
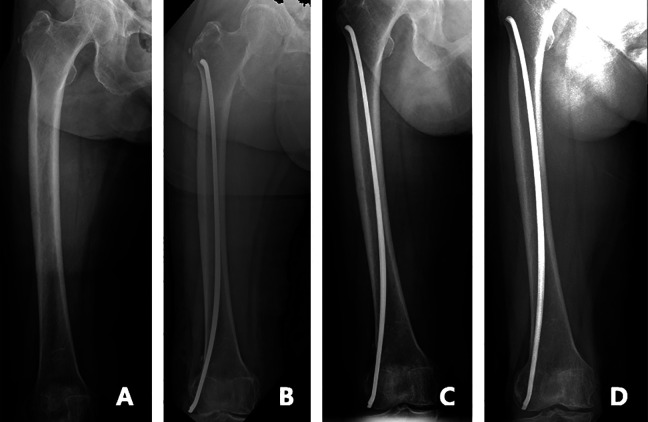
Figure 3.
Nail pre-bending technique Before insertion nail, measure the diameter of femur and pre-bend the nail, the nails were excessively pre-bended so that the distance between the 2 end of the nail and the apex was twice the diameter of femur. Pre-measuring the direction of nailing is helpful to effective fixation.
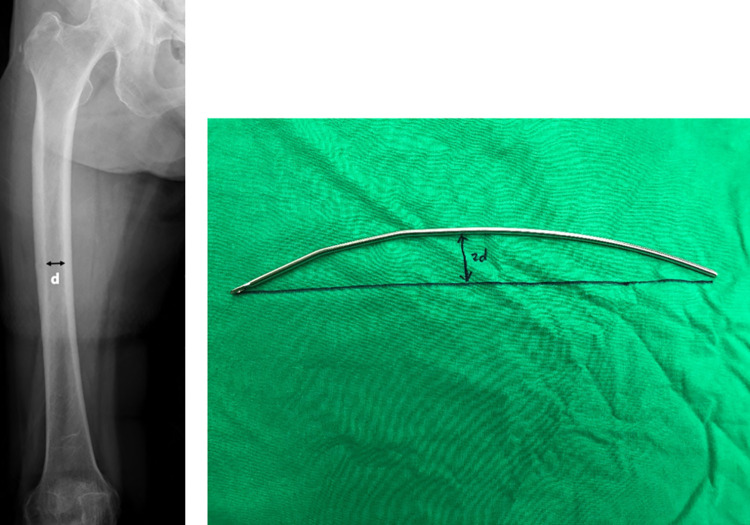
The transverse fracture line of the lateral cortex and location of the insertion site (tip of the greater trochanter and a point just proximal to the lateral epicondyle with the antegrade and retrograde approaches, respectively) were confirmed with the image amplifier. While minimizing percutaneous soft-tissue damage, a single insertion hole was made in the cortical bone using an awl, into which the pre-bent elastic IM nails were inserted (Figures 4 and 5). To maximize the compressive force on the fracture site, we aimed to ensure contact of the nail apex with the posteromedial endocortex at the fracture level. We also ensured that the leading part of the nail was firmly fixed to the lateral cortex to achieve secure 3-point fixation. With antegrade nailing, the lateral cortex of the greater trochanter, posteromedial cortex of the fracture site, and lateral cortex of the distal femur are the points where the nail is most strongly compressed. With retrograde nailing, the lateral cortex of the distal femur, posteromedial cortex of the fracture site, and lateral cortex of the proximal femur are the areas where the nail makes the strongest contact.
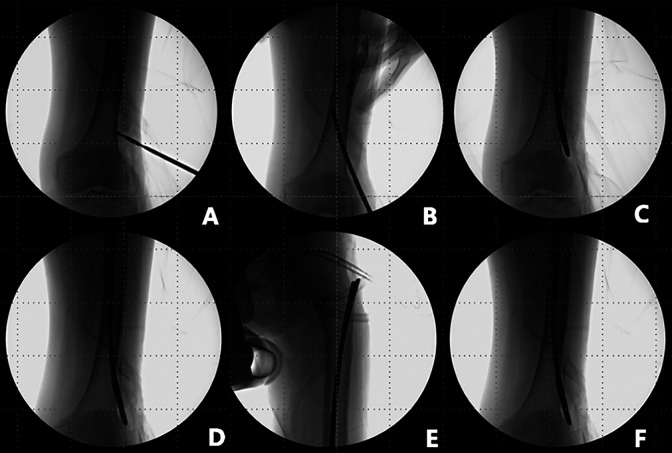
Figure 4.
Antegrade PEIN technique A, Choice of nail insertion site, find location of GT tip. B, Make entry point in GT tip with awl. C, The first nail is advanced into femoral canal. D, The apex of the curvature should be at the level of the lateral cortex fracture line. E, The second nail are advanced same way with the first nail. F, Successfully 2 nail insertion into femoral canal without any complication.
Figure 5.
Retrograde PEIN technique A, Choice of nail insertion site, find location just proximal point of lateral epicondyle, make entry point in GT tip with awl or drill. B, The first nail is advanced into femoral canal. C, The apex of the curvature should be at the level of the lateral cortex fracture line. When using the retrograde method, care should be taken for fractures of the nail Insertion site. D, The second nail are advanced same way with the first nail. E, Proximal femoral lateral cortex should be compressed by leading part of nail. F, Successfully 2 nail insertion into femoral canal without any complication.
Postoperative Management and Rehabilitation
On the first postoperative day, hip range of motion and quadriceps setting exercises were started. From the second postoperative day, tolerable weight-bearing was initiated through toe-touch ambulation, with a high walker used to support the weight at the elbow level. Gradual increase of the load with a gait-assistance device was encouraged as tolerated. Full weight-bearing was allowed when the pain subsided and partial bone union was confirmed on serial radiographs.
Clinical and Radiological Outcomes
Postoperative clinical evaluation was performed with regular outpatient follow-up (at 6-week intervals). Clinical evaluation of fracture union was based on the presence of pain and tenderness. Clinical union was defined as the absence of pain and tenderness, and the time from surgery to clinical union was noted.
The fracture location was evaluated using preoperative AP and lateral femoral radiographs. The angle made by the 2 lines drawn along the proximal and distal portions of the femoral shaft was assessed on these radiographs using the method of Sasaki et al. 17 We also checked for any change in bowing between before and after surgery. The height of the lesser trochanter in the AP radiograph, and the shape and location of the femoral condyles in the lateral radiograph, were compared to control rotation (Figure 6). The time required for endocortical callus formation and disappearance of the radiolucent line was recorded. Endocortical callus formation was defined as the inner cortical side of the fracture line being completely covered and concealed by the consolidated callus on a follow-up plain radiograph (Figure 7).
Figure 6.
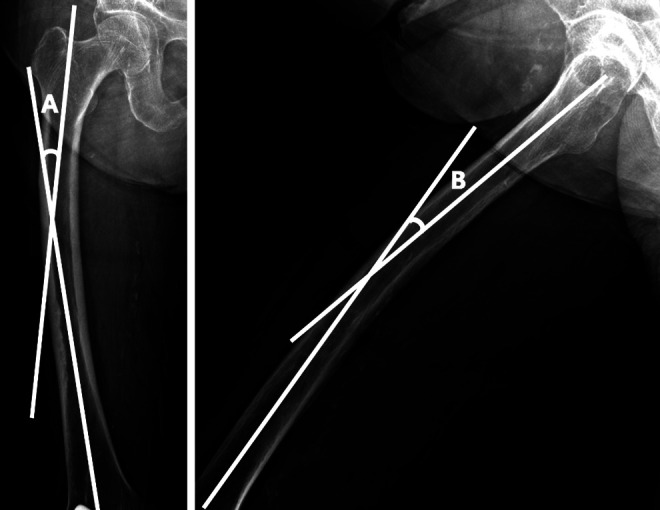
Measurement of femoral curvature Two lines along the proximal and distal portions of the femoral shaft were drawn on (A) antero-posterior and (B) lateral X-rays. Angle A is defined as the angle between the 2 lines on the antero-posterior view and angle B as that on the lateral view.
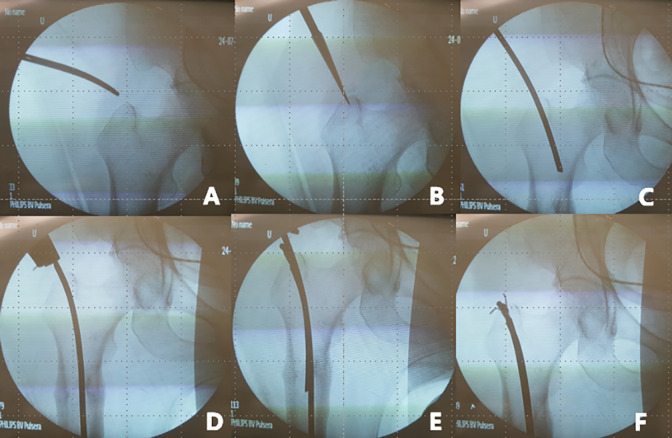
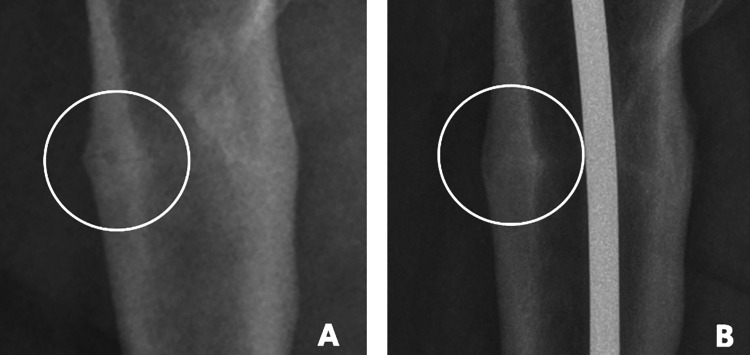
Figure 7.
Endocortical callus formation A, There are some callus on fracture site, but we can see just blurred image at preoperatively. B, For 4 weeks since the PEIN, the radiograph shows ongoing bone healing process, and we can see endocortical callus at the medial side of fracture line. Callus is becoming more radiopaque as a cortical bone’s signal and “completely connecting” the endocortical area.
Statistical Analysis
SPSS software (ver. 20.0; IBM Corp., USA) was used for all statistical analyses. All data are presented as the mean ± standard deviation. The Wilcoxon signed-rank test was used to compare the pre- and postoperative femoral bowing angles. The level of significance was set at p < 0.05.
Results
The PEIN technique was used 6 times in 5 patients (Table 1), all of whom were women. The mean age was 80.00 ± 8.99 years and the mean follow-up duration was 22.48 ± 7.72 months. The mean anterior and lateral bowing was 10.97 ± 5.21° and 14.23 ± 4.84° preoperatively, and 9.02 ± 5.35° and 12.96 ± 4.31° postoperatively, respectively. Both decreased significantly after surgery (both p = 0.043; Table 2).
Table 1.
Patient Demographics.
| Patient No. | Sex | Age (yr) | Side | Duration of bisphosphonate use (mo) | Pre op bowing angle (deg) Anterior | Pre op bowing angle (deg) Lateral | Level of fracture | Callus pattern | Nail entry | Complication | Follow-up (mo) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 75 | L | 108 | 6.99 | 5.40 | Proximal | Endosteal | Antegrade | None | 21.83 |
| 2 | F | 85 | R | None | 17.61 | 16.17 | Middle | Endosteal | Retrograde | None | 15.80 |
| F | 85 | L | None | 14.05 | 19.08 | Proximal | Endosteal | Antegrade | None | 15.80 | |
| 3 | F | 64 | R | None | 4.41 | 15.42 | Proximal | Endosteal | Antegrade | None | 24.30 |
| 4 | F | 83 | L | 41 | 14.77 | 16.91 | Distal | Endosteal | Retrograde | Insertion site fracture | 20.50 |
| 5 | F | 88 | L | 56 | 7.96 | 12.40 | Middle | Periosteal | Retrograde | None | 36.67 |
Abbreviations: Pre op, preoperative; deg, degrees; yr, years; mo, months.
Table 2.
Radiological Evaluation for the Femoral Curvature.
| Mean ± standard deviation | |||
|---|---|---|---|
| Pre-operative | Post-operative | P-value | |
| Anterior bowing angle (degree) | 10.97 ± 5.21 | 9.02 ± 5.37 | 0.043* |
| Lateral bowing angle (degree) | 14.23 ± 4.84 | 12.96 ± 4.31 | 0.043* |
* Statistically significant.
The mean duration of surgery, including the time taken for draping and pre-bending of the nail, was 65.00 ± 22.64 min. There were no iatrogenic fractures during the surgical procedure. However, one patient who underwent the retrograde technique fell from a chair on postoperative day 7 and sustained a complete fracture at the point of nail entry; this fracture healed after lateral plate fixation. Complete union was achieved in the remaining cases after an average of 6.45 months. The average time for endocortical callus formation and disappearance of the fracture line was 2.1 ± 0.53 and 6.45 ± 4.10 months, respectively. Thigh pain and fracture site tenderness disappeared at 6.45 ± 3.65 months postoperatively in all cases. There was no hardware removal due to symptoms and no case of infection.
Discussion
Despite first being reported in 2005 by Odvina et al., 18 treatment guidelines have not been established for all types of AFF. The most controversial treatment is that for SIAFF. In 2017, Koh et al. published a meta-analysis of 834 cases of AFF. 3 They found that conservative treatment of incomplete fractures ultimately failed in 47% of patients, while 97% of the patients who underwent preventive surgery successfully progressed to fracture union. Most studies concluded that prophylactic surgery should be considered for incomplete fractures with intractable pain. 3 Many preventive surgical methods have been proposed; the currently preferred method is prophylactic internal fixation using rigid nails. 3,9,19 Although this method has overall good outcomes, 3 the use of rigid nails is based on empirical data rather than the specific mechanism of atypical fractures. 15 Furthermore, Asians have small bodies with more pronounced anterolateral bowing of the femur. Therefore, it is often difficult to insert a rigid nail with a straight geometry or lateral offset. Moreover, given that the surgery is performed in this challenging situation, the risk of complications is high. This surgery might also be too major to be suitable as preventive surgery. Theoretically, PEIN has the following advantages over rigid IM nailing. First, based on the nature of the pre-bent flexible nail used to restore the original arc, compression force can be applied to the anterolateral cortex to counteract the fracture mechanism. Thus, this method has the physiological advantage of promoting fracture healing compared to rigid IM nailing. Second, PEIN is technically easy, fast, and minimally invasive surgery. 20,21 Third, it can preserve the endosteal circulation. 22 -24 Fourth, because pre-bent nails are used, there is almost no risk of iatrogenic fracture caused by femoral bowing and a rigid nail system. 10,11 Lastly, it can shorten the hospital stay. 2,15,25
Patient and caregiver satisfaction were high due to the rapid postoperative rehabilitation, short operating time, and absence of systemic complications. According to Koh et al. 3 fracture union when preventive surgery was performed using the conventional method took an average of 7 months (range: 1.5-20 months). This was comparable to the average fracture union time in our PEIN patients, of 6.45 ± 4.10 months. There were also changes in the pre- and postoperative bowing angles, which both decreased significantly.
It is thought that the flexible nail, which is bent laterally in the femoral canal, effectively exerts a continuous compressive force on the lateral cortex, which affects the femoral curvature. This might help reduce the fracture risk during continuous weight-bearing. The antegrade method was used for proximal femoral fractures to apply a compression force to the fracture site and minimize endosteal damage in the femoral canal. By contrast, the retrograde method was used for distal and mid-shaft femoral fractures.
In one patient who underwent the retrograde method, a fracture occurred around the pin insertion site at 1 week post-surgery. Although this patient fell from a chair, the fracture was thought to have initiated from a minor cortical injury at nail entry. When applying the retrograde method in an AFF with brittle characteristics due to insufficient bone quality, care should be taken to avoid cortical bone microfracture at the pin insertion site. Moreover, fixation using the antegrade method is safe for midshaft fractures. Another problem is that the PEIN method uses pre-bent nails. Therefore, if the femoral curvature is severe, additional fractures could occur since the full length of the femur cannot be fixed. Entry may also increase stress. When inserting the nail, care should be taken not to damage the endocortex and create a stress riser. In the past, stainless steel was used because of its high strength and elasticity. Recently, however, titanium nails have mainly been used, as in one of our patients. However, since titanium is weaker than stainless steel, implant failure is possible. Thus, it is advisable to use a thick nail or increase the number thereof.
This study had several limitations. First, it was a retrospective study. Second, it is difficult to compare the outcomes obtained with the PEIN technique with those of existing methods because of the small sample size and short follow-up period. However, the surgical technique was simple and prevented transformation of SIAFF to a complete fracture. Moreover, fracture union occurred in all cases, except the patient who experienced a complication. We believe that the introduction of this new treatment method is clinically meaningful. A multicenter prospective study including more cases will help evaluate the new technique accurately.
In summary, the PEIN technique in patients with SIAFF is simple and can be used even when the canal is narrow or bowing is severe. It does not predispose the patient to iatrogenic fractures and promotes bone union via compressive pressure exerted at the fracture site. Moreover, this technique has many biomechanical advantages that lower the potential fracture risk by reducing postoperative femoral bowing. The PEIN technique can be a beneficial alternative to prevent progression to complete fracture.
Footnotes
Authors’ Note: This study was approved by Kyung Hee University Hospital Institutional Review Board (KHUH 2020-10-041).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Yoon Je Cho, MD, PhD  https://orcid.org/0000-0001-8951-1066
https://orcid.org/0000-0001-8951-1066
References
- 1. Min BW, Koo KH, Park YS, et al. Scoring system for identifying impending complete fractures in incomplete atypical femoral fractures. J Clin Endocrinol Metab. 2017;102(2):545–550. [DOI] [PubMed] [Google Scholar]
- 2. Banffy MB, Vrahas MS, Ready JE, Abraham JA. Nonoperative versus prophylactic treatment of bisphosphonate-associated femoral stress fractures. Clin Orthop Relat Res. 2011;469(7):2028–2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Koh A, Guerado E, Giannoudis PV. Atypical femoral fractures related to bisphosphonate treatment: issues and controversies related to their surgical management. Bone Joint J. 2017;99-B(3):295–302. [DOI] [PubMed] [Google Scholar]
- 4. Wang K, Moaveni A, Dowrick A, Liew S. Alendronate-associated femoral insufficiency fractures and femoral stress reactions. J Orthop Surg (Hong Kong). 2011;19(1):89–92. [DOI] [PubMed] [Google Scholar]
- 5. Shane E, Burr D, Ebeling PR, et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2010;25(11):2267–2294. [DOI] [PubMed] [Google Scholar]
- 6. Park JH, Lee Y, Shon OJ, Shon HC, Kim JW. Surgical tips of intramedullary nailing in severely bowed femurs in atypical femur fractures: simulation with 3D printed model. Injury. 2016;47(6):1318–1324. [DOI] [PubMed] [Google Scholar]
- 7. Park YC, Song HK, Zheng XL, Yang KH. Intramedullary nailing for atypical femoral fracture with excessive anterolateral bowing. J Bone Joint Surg Am. 2017;99(9):726–735. [DOI] [PubMed] [Google Scholar]
- 8. Egol KA, Park JH, Rosenberg ZS, Peck V, Tejwani NC. Healing delayed but generally reliable after bisphosphonate-associated complete femur fractures treated with IM nails. Clin Orthop Relat Res. 2014;472(9):2728–2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Oh CW, Oh JK, Park KC, Kim JW, Yoon YC. Prophylactic nailing of incomplete atypical femoral fractures. Sci World J. 2013:450148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Prasarn ML, Ahn J, Helfet DL, Lane JM, Lorich DG. Bisphosphonate-associated femur fractures have high complication rates with operative fixation. Clin Orthop Relat R. 470(8):2295–2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lim HC, Bae JH, Yi JW, Park JH. Bilateral stress fracture of the femoral shaft after total knee arthroplasty: a case report. Knee. 2011;18(5):354–357. [DOI] [PubMed] [Google Scholar]
- 12. Lee KJ, Min BW. Surgical treatment of the atypical femoral fracture: overcoming femoral bowing. Hip Pelvis. 2018;30(4):202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kim JW, Kim H, Oh CW, et al. Surgical outcomes of intramedullary nailing for diaphyseal atypical femur fractures: is it safe to modify a nail entry in bowed femur? Arch Orthop Trauma Surg. 2017;137(11):1515–1522. [DOI] [PubMed] [Google Scholar]
- 14. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;l29(1):1–23. [DOI] [PubMed] [Google Scholar]
- 15. Kharazmi M, Michaelsson K, Hallberg P, Schilcher J. Lateral fixation: an alternative surgical approach in the prevention of complete atypical femoral fractures. Eur J Orthop Surg Traumatol. 2018;28(2):299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tsuchie H, Miyakoshi N, Nishi T, Abe H, Segawa T, Shimada Y. Combined effect of a locking plate and teriparatide for incomplete atypical femoral fracture: two case reports of curved femurs. Case Rep Orthop. 2015;2015:213614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sasaki S, Miyakoshi N, Hongo M, Kasukawa Y, Shimada Y. Low-energy diaphyseal femoral fractures associated with bisphosphonate use and severe curved femur: a case series. J Bone Miner Metab. 2012;30(5):561–567. [DOI] [PubMed] [Google Scholar]
- 18. Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005;90(3):1294–1301. [DOI] [PubMed] [Google Scholar]
- 19. Bogdan Y, Tornetta P, III, Einhorn TA, et al. Healing time and complications in operatively treated atypical femur fractures associated with bisphosphonate use: a multicenter retrospective cohort. J Orthop Trauma. 2016;30(4):177–181. [DOI] [PubMed] [Google Scholar]
- 20. Yamaji T, Ando K, Nakamura T, Washimi O, Terada N, Yamada H. Femoral shaft fracture callus formation after intramedullary nailing: a comparison of interlocking and ender nailing. J Orthop Sci. 2002;7(4):472–476. [DOI] [PubMed] [Google Scholar]
- 21. Browner BD, Burgess AR, Robertson RJ, Baugher WH, Freedman MT, Edwards CC. Immediate closed antegrade ender nailing of femoral fractures in polytrauma patients. J Trauma. 1984;24(11):921. [DOI] [PubMed] [Google Scholar]
- 22. Haas N, Krettek C, Schandelmaier P, Frigg R, Tscherne H. A new solid unreamed tibial nail for shaft fractures with severe soft tissue injury. Injury. 1993;24(1):49–54. [DOI] [PubMed] [Google Scholar]
- 23. Gregory P, Sanders R. The treatment of closed, unstable tibial shaft fractures with unreamed interlocking nails. Clin Orthop Relat Res. 1995;(315):48–55. [PubMed] [Google Scholar]
- 24. Neviaser AS, Lane JM, Lenart BA, Edobor-Osula F, Lorich DG. Low-energy femoral shaft fractures associated with alendronate use. J Orthop Traum. 2008;22(5):346–350. [DOI] [PubMed] [Google Scholar]
- 25. Morris D, Shaikh W III, Morris S, IV. Signs of insufficiency fractures overlooked in a patient receiving chronic bisphosphonate therapy. J Am Board Fam Med. 2016;29(3):404–407. [DOI] [PubMed] [Google Scholar]