Abstract
There are only a limited number of previous reports on clinical cases using tumour tracking with tomotherapy. Therefore, we present two cases of patients treated with tumour tracking with tomotherapy. First, a 74-year-old man with an inoperable lung cancer type T1bN0M0 underwent stereotactic body radiotherapy at a total dose of 48 Gy in four fractions. Second, a 68-year-old man with hepatocellular carcinoma with a portal venous tumour thrombosis and history of liver stereotactic body radiotherapy with fiducial marker implantation received radiotherapy at a total dose of 48 Gy in 20 fractions. The results of patient-specific quality assurance and tracking radiotherapy were sufficient to irradiate tumours. Tumour tracking with tomotherapy successfully delivered radiation in a total of 24 treatment fractions in both patients. Tumour tracking with tomotherapy is feasible in lung and liver cancer treatment. This study’s findings suggest the clinical use of tumour tracking with tomotherapy.
Keywords: Tomotherapy, tumour tracking, lung cancer, stereotactic body radiation therapy, stereotactic ablative radiotherapy
Introduction
Tumour motion management is an important factor in delivering high-dose radiation to the target area without overdosing surrounding normal tissues. 1 Helical tomotherapy is a volumetric image-guided intensity-modulated radiation therapy (IMRT) delivery system with high clinical precision and versatility. 2 The Synchrony Respiratory Tracking System is a real-time respiratory tracking and compensation system that was originally designed for CyberKnife® (Accuray Inc., Sunnyvale, CA, USA) and has recently incorporated Radixact® (Accuray Inc.), which is an updated version of helical tomotherapy.3,4 Previous reports have suggested that tumour tracking with tomotherapy (TTT) is feasible in terms of physical assessment.5–7 However, there have only been a limited number of reports on clinical cases using such tumour tracking. 8 In addition, to the best of our knowledge, TTT for liver tumours has never been documented in patients. Herein, we present two cases of tumour tracking with helical tomotherapy for lung stereotactic body radiotherapy (SBRT) and liver radiotherapy, capturing an early clinical experience of this approach.
Case report
This study was approved by the appropriate institutional review board (approval no. 20200703). All patients provided informed consent prior to radiotherapy. The details of the treatment planning methods are described in Supplementary material 1. Planning target volume (PTV) was created by adding 5 mm margins to gross tumour volume (GTV) in all directions. The prescribed radiation doses were designed to cover 95% of the PTV (D95 prescription).
Tracking simulation and evaluation
Before treatment initiation, a simulation plan was delivered to determine if motion tracking was likely to be successful. In the simulation mode, the behaviour of the gantry, couch, multileaf collimator (MLC), and jaws is the same as that in regular treatment, whereas the treatment beam is disabled. During the simulation, output parameters provide tracking feedback. Several output parameters have configurable thresholds to adopt new motion models or pause treatment. Values of Potential Diff (PD) and Measured Δ (MD) are among the most important output parameters used to determine the quality of the model. PD is a statistical prediction of a three-dimensional (3D) error when the model is used to predict the future target position. MD represents how well the model predicted the fiducial or target locations in the most recent radiograph. These parameters increase if patient’s breathing cycle does not fit the model well, or if the data are not well sampled. Tracking accuracy results were documented during the treatment course. The workflow is shown in Supplementary material 2.
Motion quality assurance procedure
The motion quality assurance (MQA) equipment is shown in Supplementary material 3. The CIRS platform (CIRS Inc., Norfolk, VA, USA) was used to simulate respiratory motion. As a detector, we introduced an SRS MapCHECK® (SMC, Sun Nuclear Corp, Melbourne, FL, USA). The SMC inserted in dedicated phantom was placed on a horizontal motion table, which was rotated 30 degrees around the IEC Z to allow motion prescription in two-dimensional (2D) (IEC X and Y). The light-emitting diode (LED) marker, as a surrogate signal, was positioned on a vertical motion table. To evaluate tracking error, sinusoidal motion sequences were produced by the CIRS software with patient-specific amplitudes and periods assigned from the average motion of each patient, using four-dimensional computed tomography (4DCT)–based analysis. To support fiducial tracking for respiratory motion (FR) and fiducial-free tracking for respiratory motion (FFR) modes, a 2-cm acrylic cube was used to imitate a lung tumour or built-in fiducial markers were set up, respectively (Supplementary materials 3B and 3C). The percent dose error between central diode response of SMC and treatment planning system (TPS)’s calculation was estimated with and without tracking. Similarly, 2D gamma analysis in the coronal plane was performed at 2%/2 mm and 1%/1 mm criteria at a threshold of 10%. Furthermore, detection accuracy of the tracking target, defined as the difference between the predicted and instructed target positions, was evaluated with the root mean square analysis.
Case 1: SBRT for lung tumour
A 74-year-old man presented with a history of right upper lobectomy, performed in October 2012, for early stage squamous cell carcinoma (pStage IA). A CT scan performed in May 2020 revealed a 20-mm nodule in the right lower lobe (S8) (Figure 1(a), left). Positron emission tomography with 2-deoxy-2-[fluorine-18]fluoro-D-glucose CT (18F-FDG PET/CT) showed 12.6 of the maximum standardized uptake value (SUVmax) of the tumour without evidence of another abnormal uptake (Figure 1(a), right). The patient had history of severe chronic obstructive pulmonary disease, and used home-based oxygen therapy at 3 L/min. The patient was diagnosed with primary lung cancer, clinical type T1bN0M0, stage IA2, without pathological diagnosis. SBRT for the primary tumour was recommended by a multidisciplinary tumour board at our institute. The total prescribed radiation dose was 48 Gy in four fractions (Figure 1(b)). Synchrony FFR mode was adopted in this case.
Figure 1.
Computed tomography (CT) scanning diagnostic images of lung cancer and the treatment plan. (a) CT images revealed a solitary nodule of 20 mm in diameter in the lower lobe of the right lung (left panel). High 2-deoxy-2-[fluorine-18]fluoro-D-glucose (FDG) uptake by the tumour was observed in contrast imaging with positron emission tomography with FDG integrated with CT (18F-FDG PET/CT) images (right). (b) Stereotactic body radiation therapy (SBRT) plan was generated with a total of 48 Gy in four fractions for planning target volume (PTV). The colour washes indicate the dose distributions. (c) Results of tracking accuracy in stereotactic body radiation therapy for lung tumour (upper left). Tracking results at first simulation without coaching (upper right); results at second simulation with audio coaching (lower left); results at first treatment fraction (lower right) and results at treatment completion (fourth fraction). Findings indicate improvement in tracking accuracy after the first simulation. Parameters of interest (Potential Diff and Measured Δ) did not exceed threshold values for most of the treatment time. Treatment course was successfully completed.
Detection accuracy was within a 1.0-mm margin in the phantom study. The point dose accuracy and the gamma passing rates of 2D doses were within the clinically acceptable range, compared to non-tracking conditions (Table 1). In the first simulation, increasing PD values (near 4 mm) were noted, indicating patient’s irregular breathing. After audio coaching, PD values improved within 3 mm and treatment was successfully completed (Figure 1(c)).
Table 1.
Dosimetric error and motion detection accuracy for two cases.
| Case no. | Delivery time (s) | Motion parameters | Synchrony® (−) | Synchrony® (+) | Detection accuracy | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| A (mm) | P (s) | Dose %diff | Gamma passing rate (%) | Dose %diff | Gamma passing rate (%) | RMS (mm) | ||||
| 2%/2 mm | 1%/1 mm | 2%/2 mm | 1%/1 mm | |||||||
| 1 | 496.3 | 17.6 | 6.0 | −0.43 | 78.6 | 56.7 | −0.18 | 100.0 | 95.0 | 0.87 |
| 2 | 110.5 | 10.8 | 4.0 | 0.51 | 99.3 | 76.4 | 0.43 | 100.0 | 87.8 | 0.53 |
A: peak-to-peak amplitude of respiration; P: period; Dose %diff: dose percent difference; RMS: root mean square.
Case 2: IMRT for liver tumour
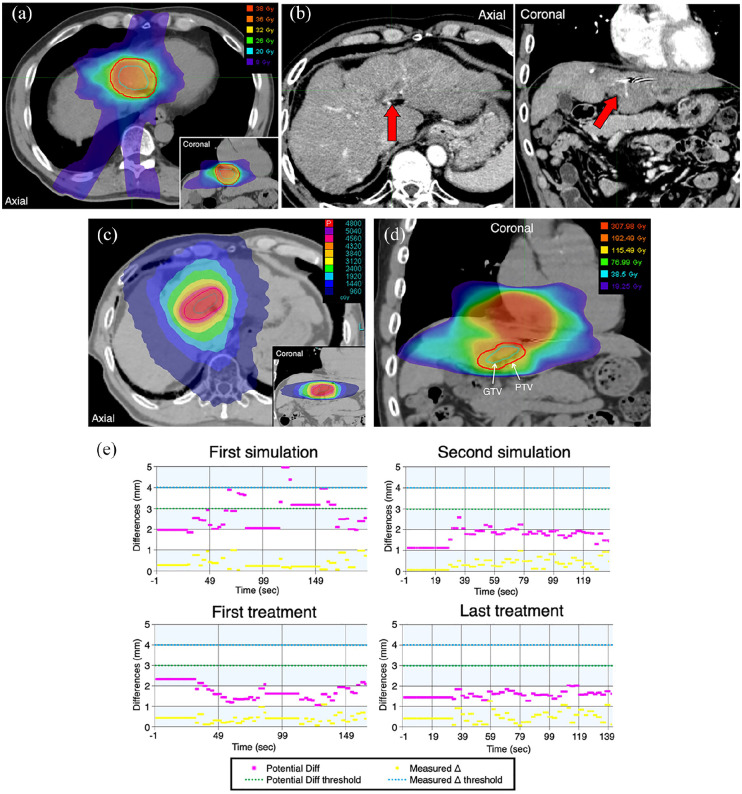
A 68-year-old man presented with a history of alcoholic cirrhosis and treatments for hepatocellular carcinoma (HCC) administered between March 2016 and February 2020, including SBRT following implantation of a fiducial marker in March 2016 (Figure 2(a)). Contrast-enhanced CT scan was performed in June 2020, revealing multiple intrahepatic failures in the left lobe of the liver with portal venous tumour thrombosis (PVTT) in the left branch of the hepatic portal vein (Figure 2(b)). The Child–Pugh score and grade were 8 and B, respectively. We prescribed radiation at a total dose of 48 Gy in 20 fractions for PVTT (Figure 2(c) and (d)). Synchrony FR mode, using the old implanted fiducial marker, was adopted.
Figure 2.
Diagnostic images and treatment plan for liver tumour. (a) The previous SBRT was prescribed at a dose of 40 Gy in five fractions (D95) for pathologically confirmed HCC in S4 of the liver. Dose distribution of previous stereotactic body radiation therapy was represented in the MIM Maestro version 7.0.3 (MIM Software Inc., Cleveland, OH, USA) from the digital imaging and communications in medicine-radiation therapy (DICOM-RT). (b) Portal venous tumour thrombosis (PVTT) observed close to the previously irradiated area in contrast-enhanced computed tomography (indicated by arrows). (c) Treatment plan with intensity-modulated radiation therapy for PVTT was generated at a total of 48 Gy in 20 fractions for planning target volume (PTV). (d) Combined dose distributions of previous and present radiotherapy defined in terms of biologically effective dose (BED), using a linear-quadratic model with an assumed α/β ratio of 2 Gy for liver (BED2) (MIM Maestro). (e) Results of tracking accuracy in radiotherapy for liver tumour (upper left). The first simulation resulted in an unstable model (upper right); a stable model was achieved after changing the LED marker position from the chest wall to abdominal wall (lower left); results at first treatment fraction (lower right) and results at treatment completion (20th fraction). Parameters of interest (Potential Diff and Measured Δ) never exceeded threshold values, except for the first simulation. Treatment was successfully completed.
Detection accuracy was within a 1.0-mm margin in the phantom study. The point dose accuracy and the gamma passing rates of 2D doses were within the clinically acceptable range, compared to non-tracking conditions (Table 1). In the first simulation, we observed increasing PD values (over 4 mm). However, after changing the LED position from the chest wall to the abdominal wall, PD values improved within 3 mm, and the treatment was successfully completed (Figure 2(e)).
Discussion
This report presented two patients treated using TTT, including the first case of a liver tumour treated with TTT, showing MQA and treatment validation findings in lung and liver tumours using a total of 24 fractions.
According to AAPM-TG 101, patient-specific MQA should be established, using a moving phantom that simulates respiratory motion. 9 Chen et al. 7 reported that for fiducial tracking for non-respiratory motion (FNR) and FR, signal from diodes could be interpreted as fiducials, precluding their accurate detection and that subtraction of kV dose for diode measurements in gamma analysis was crucial. Therefore, to avoid the above defects, we verified integration of Synchrony with SMC. Our results indicate that target detection accuracy of Synchrony with an internal–external correlation is well within 1.5 mm, suggesting tolerance for these phantom studies under the clinical-like condition. The point dose accuracy and the gamma passing rates of 2D doses were within the clinically acceptable range. Thus, SMC is an MQA tool with accurate dosimetry and spatial resolution.
We showed that coaching patients improved the accuracy of motion tracking. Furthermore, tracking errors were reduced by changing the LED position from the chest wall to the abdominal wall as previously reported in the CyberKnife Synchrony system. 10 Careful simulation and continuous assessment of motion were paramount to achieving accurate beam delivery and continuous treatment.
The Synchrony system specification suggests that to achieve potential targeting accuracy of 1.5 mm, threshold values of PD and MD should be set to 2.0 and 4.0 mm, respectively. 7 Our PD threshold was set to 3.0 mm for both patients to minimize treatment pauses. Future studies should verify whether a 5-mm PTV margin is necessary and sufficient to compensate for dose coverage.
Conclusion
We reported on two clinical cases of TTT, including the first case of liver tumour treatment with TTT, and demonstrated the clinical feasibility of this technique. Motion tracking and compensation system with the Synchrony and Radixact technology ensured clinical safety and efficacy when used to correct respiratory motion.
Supplemental Material
Supplemental material, sj-pdf-1-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-2-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-3-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-4-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-5-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-6-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-7-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-8-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Acknowledgments
The authors thank Dr Toshiyuki Imagumbai from the Department of Therapeutic Radiology, Kobe City Medical Center General Hospital (Hyogo, Japan) for providing clinical information and Ms Fuyumi Kobayashi from Accuray Japan K.K. (Tokyo, Japan) for providing technical assistance. The authors acknowledge Editage (www.editage.jp) for English language editing.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from the institutional review board at the Takarazuka City Hospital (approval no. 20200703).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by a Grant JSPS KAKENHI grant number JP20K08093.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Hiroshi Doi  https://orcid.org/0000-0003-3237-2119
https://orcid.org/0000-0003-3237-2119
Supplemental material: Supplemental material for this article is available online.
References
- 1. Shirato H, Seppenwoolde Y, Kitamura K, et al. Intrafractional tumor motion: lung and liver. Semin Radiat Oncol 2004; 14(1): 10–18. [DOI] [PubMed] [Google Scholar]
- 2. Saw CB, Katz L, Gillette C, et al. 3D treatment planning on helical tomotherapy delivery system. Med Dosim 2018; 43(2): 159–167. [DOI] [PubMed] [Google Scholar]
- 3. Ozhasoglu C, Saw CB, Chen H, et al. Synchrony – CyberKnife respiratory compensation technology. Med Dosim 2008; 33(2): 117–123. [DOI] [PubMed] [Google Scholar]
- 4. Chao EH, Lucas D, Schnarr E. Evaluation of TomoTherapy dose calculations with intrafractional motion and motion compensation. Med Phys 2018; 45(1): 18–28. [DOI] [PubMed] [Google Scholar]
- 5. Schnarr E, Beneke M, Casey D, et al. Feasibility of real-time motion management with helical tomotherapy. Med Phys 2018; 45(4): 1329–1337. [DOI] [PubMed] [Google Scholar]
- 6. Price A, Chen J, Chao E, et al. Compensation of intrafractional motion for lung stereotactic body radiotherapy (SBRT) on helical TomoTherapy. Biomed Phys Eng Express 2019; 5: 025043. [Google Scholar]
- 7. Chen GP, Tai A, Keiper TD, et al. Technical note: comprehensive performance tests of the first clinical real-time motion tracking and compensation system using MLC and jaws. Med Phys 2020; 47: 2814–2825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chen GP, Tai A, Puckett L, et al. Clinical implementation and initial experience of real-time motion tracking with jaws and multileaf collimator during helical tomotherapy delivery. Pract Radiat Oncol. Epub ahead of print 10 February 2021. DOI: 10.1016/j.prro.2021.01.010. [DOI] [PubMed] [Google Scholar]
- 9. Benedict SH, Yenice KM, Followill D, et al. Stereotactic body radiation therapy: the report of AAPM Task Group 101. Med Phys 2010; 37(8): 4078–4101. [DOI] [PubMed] [Google Scholar]
- 10. Akino Y, Sumida I, Shiomi H, et al. Evaluation of the accuracy of the CyberKnife synchrony™ respiratory tracking system using a plastic scintillator. Med Phys. Epub ahead of print 1 June 2018. DOI: 10.1002/mp.13028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-2-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-3-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-4-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-5-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-6-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-7-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports
Supplemental material, sj-pdf-8-sco-10.1177_2050313X211023688 for A first report of tumour-tracking radiotherapy with helical tomotherapy for lung and liver tumours: A double case report by Wataru Okada, Hiroshi Doi, Masao Tanooka, Keisuke Sano, Kenji Nakamura, Yusuke Sakai, Mayuri Shibata and Masahiro Tanaka in SAGE Open Medical Case Reports