Abstract
Candida spondylitis is a relatively rare disease. The primary risk factor is an immunocompromised status. Here, we report an immunocompetent patient who developed Candida spondylitis. The patient was a 70-year-old male. After multiple surgeries, he developed a fever and was diagnosed with chronic pyogenic spondylitis of the lumbar spine, which was treated by long-term antimicrobial therapy. However, his back pain persisted and the inflammatory response was prolonged. We performed posterior thoracolumbar pelvic fixation with a percutaneous pedicle screw system to stabilize the infected vertebral bodies and simultaneously performed a full-endoscopic intervertebral disc biopsy to identify the causative organisms. Candida parapsilosis was identified from a fungal culture of the biopsy specimen. The patient was diagnosed with Candida spondylitis and started on antifungal treatment with fluconazole. His back pain disappeared quickly after surgery, and up to the time of this writing, the patient has continued to receive fluconazole. We attributed the development of Candida spondylitis to the patient’s long-term antibiotic treatment of a postoperative infection of the lumbar spine, which was associated with multiple back surgeries. Fungal spondylitis, including spondylitis caused by Candida spp., should be suspected in patients, even immunocompetent patients, with intractable postoperative spinal infections and pyogenic spondylitis due to microbial substitution. Long-term antimicrobial therapy without definitive identification of the causative organism of a postoperative infection of the lumbar spine that is associated with multiple surgeries can be a cause of Candida spondylitis. A biopsy is strongly recommended for the definitive diagnosis.
Keywords: candida, spondylitis, fluconazole, fungal disease
Introduction
Candida spondylitis is a relatively rare disease, occurring in 0.5% to 1.6% of all types of spondylitis cases. Candida spondylitis is strongly associated with immunocompromise due to conditions such as steroid therapy, neutropenia, and chronic granulomatous disease. In addition, other previously reported possible risk factors for Candida spondylitis are prior use of broad-spectrum antibiotics and central venous access devices. The incidence of Candida spondylitis is estimated to increase because of an aging population and improved diagnostic modalities and techniques [1,2].
Here we report an immunocompetent patient who developed Candida spondylitis after multiple surgeries for a postoperative infection of the lumbar spine.
Case presentation
The patient was a 70-year-old male without a previous history of significant health problems, who underwent a partial lumbar laminectomy (L2/3 to L5/S1) for lumbar spinal stenosis at another hospital about nine years previously. After the initial surgery, a postoperative wound infection developed. Another wound infection occurred after a posterior lumbar interbody fusion (L3/4, L4/5) approximately six years previously. Six months after the second surgery, an anterior lumbar interbody fusion that consisted of a combination of a plate and screw fixation with autologous iliac bone grafting was performed for infectious pseudoarthrosis at L3/4. The patient developed persistent back pain postoperatively. An intraoperative specimen that was cultured after the third surgery was negative for bacteria and the presence of tuberculosis or a fungus was also ruled out by a histopathological examination of the specimen. Two years after the third surgery, all pedicle screws of posterior lumbar interbody fusion of second surgery were removed from the infected posterior implant. Six months before his present admission, the patient developed a fever and was diagnosed with chronic pyogenic spondylitis of the lumbar spine. He was treated with intravenous cefazolin (3 g/day) and clindamycin (1,200 mg/day) followed by an oral course of cefaclor (750 mg/day) and clindamycin (450 mg/day), followed by an oral course of minocycline (100 mg/day). Antimicrobial treatment was administered for a total of six months. The inflammatory response was attenuated temporarily, but resumed.
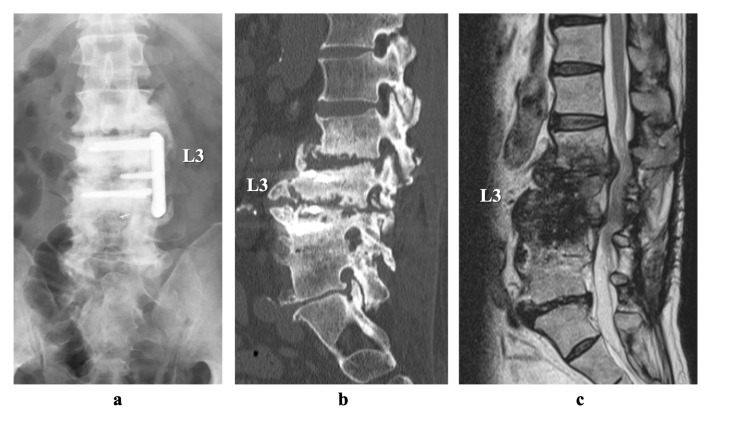
For 9 years, he was referred to our hospital. He had no neurological findings, but the patient’s daily activities were strongly restricted because of persistent back pain. Upon admission, the patient was afebrile, and a peripheral blood sample revealed a mildly increased inflammatory response (white blood cells count 7100/µL, C-reactive protein [CRP] 1.02 mg/dL, and erythrocyte sedimentation rate [ESR] of 36 mm/h). Computed tomography (CT) showed bone destruction of the vertebral endplates and osteosclerosis of the L2-L4 vertebral bodies (Figure 1).
Figure 1. Images on admission.
(a) Lumbar anterior-posterior plain radiograph of the lumbar spine showing the damaged L3/4 plate and L4 screw. (b) Computed tomography scan (sagittal slice) showing bone destruction of the vertebral endplates and osteosclerosis of the L2-4 vertebral bodies. (c) Sagittal T2-weighed magnetic resonance image showing the low-intensity signal of the L2-4 vertebral bodies.
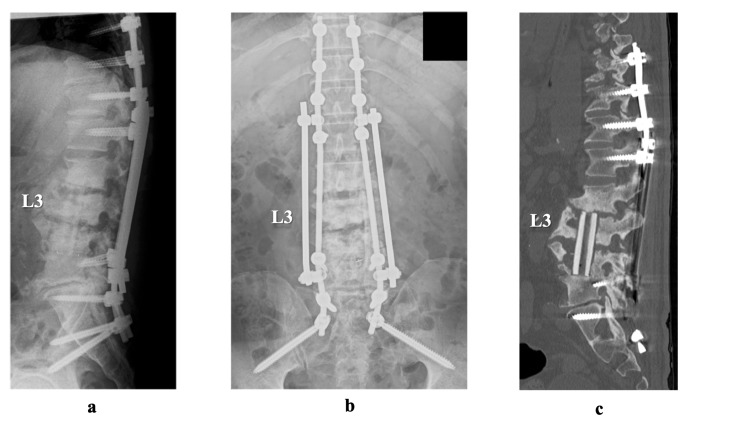
We used a percutaneous pedicle screw system to perform a posterior thoracolumbar pelvic fixation, skipped the infected L2-4 vertebral bodies (Th10 - sacral-alar-iliac), in order to stabilize the infected unstable vertebral bodies, and simultaneously performed a full-endoscopic biopsy of the intervertebral disc of L3/4 to identify the causative organisms. Candida parapsilosis was identified from a fungal culture of the biopsy specimen of the intervertebral disc of L3/4. Altogether, the patient’s findings were diagnosed as Candida spondylitis, and antifungal treatment was started consisting of intravenous fluconazole (800 mg/day) three weeks, followed by an oral administration of fluconazole (400 mg/day). Two weeks after the posterior stabilization and biopsy, we removed the anterior plate and screws and performed curettage of the lesion and a fibula graft via a retroperitoneal approach (Figure 2). The patient’s back pain rapidly resolved after the procedure. At the time of this writing, he has continued to take fluconazole.
Figure 2. Post-operative images.
(a, b, c) Posterior thoracolumbar pelvic fixation with percutaneous pedicle screw system to stabilize the infected unstable vertebral bodies, anterior plate removal, lesion curettage, and fibula graft via retroperitoneal approach.
Discussion
The following magnetic resonance imaging (MRI) findings have been reported to be characteristic of Candida spondylitis: change in the signal and destruction of the vertebral endplate in two adjacent vertebral bodies, a small paraspinal abscess, and low-intensity signal on T2-weighted imaging. By contrast, pyogenic spondylitis and tuberculous spondylitis generally show high-intensity signal on T2-weighted imaging [3]. Because both the characteristic MRI and CT findings are not specific for Candida spondylitis, to differentiate pyogenic spondylitis from Candida spondylitis using imaging findings only is difficult [4].
Guidelines for the diagnosis of pyogenic spondylitis include obtaining two sets of blood cultures for both aerobic and anaerobic bacteria, and obtaining the ESR and the CRP level. Fungal blood cultures are also recommended for patients at risk of fungal infection, such as those with immunocompromised conditions [5].
Candida spondylitis usually progresses more slowly and has fewer symptoms than pyogenic spondylitis. Patients with Candida spondylitis complain of mild back pain and lack signs/symptoms of fever or sepsis. The paucity of clinical signs/symptoms can lead to a delayed diagnosis. Therefore, an adequate biopsy specimen is essential for diagnosis [2,4]. In our patient, a biopsy obtained during a full endoscopic lumbar discectomy was needed for the definitive diagnosis.
Previously, there have been several reports of Candida spondylitis in immunocompetent patients. However, most of these reports were in patients with risk factors such as hepatitis C and prior use of central venous catheterization. There were only four reports of Candida spondylitis in immunocompetent patients without risk factors (Table 1). It took three weeks to four months to make the diagnosis. In all the reports, Candida could be detected not by simple blood culture but by biopsy or intraoperative specimens. Three to six months of antifungal therapy was needed to obtain the cure of Candida spondylitis. Together with the previous cases, the current case suggests that identification of the fungal species by the collection of local specimens is important for the diagnosis of Candida spondylitis and that a longer duration of antifungal therapy was unavoidable until cure.
Table 1. Reports of Candida spondylitis on immunocompetent patient.
| References | Age | Segments | Spinal intervention | Duration to diagnosis | Cultures | Surgical treatment | Duration of antifungal treatment | Prognosis |
| Torres-Ramos et al. 2004 [6] | 69; female | T8-9 | None | 4 months | Intraoperative cultures | Debridement Fusion | 3 months | cured |
| Cho et al. 2010 [7] | 70; female | L5-S1 | Lumbar discectomy on L5-S1 | 2 months | Intraoperative cultures | Debridement | 4 months | cured |
| Werner et al. 2011 [8] | 40; female | L3-4 | Lumbar discectomy on L5-S1, lumbar epidural steroid injection, lumbar facet injection, lumbar discogram | 3 weeks | Intraoperative cultures | Debridement | 6 months | cured |
| Darrieutort-Laffite et al. 2013 [9] | 22; female | L1-2 | None | 4 months | Biopsy | None | 6 months | cured |
| Current case | 70; male | L2-4 | Multiple spine surgeries | 6 months | Full endoscopic discectomy | Debridement fusion | 9 months | cured |
Our patient did not have any risk factors for Candida spondylitis such as diabetes mellitus, or the use of steroids, prior use of broad-spectrum antibiotics, or a central venous catheter. Our patient’s Candida spondylitis might have been associated with microbial substitution by his long-term antibiotic therapy. There are several possibilities of the origin of candida infection. Both surgical contamination and hematogenous infection originated from the oral cavity are the most likely candidates. We are planning to terminate fluconazole treatment based on the imaging findings of bony union.
Conclusions
Fungal spondylitis due to Candida spp. can develop in association with antibiotic therapy and should be considered for patients, including immunocompetent patients, with intractable postoperative spinal infections and pyogenic spondylitis. Multiple surgeries and long-term antimicrobial therapy without definitive microbial identification of a biopsy specimen can be associated with Candida spondylitis. Therefore, a biopsy is strongly recommended for the definitive diagnosis.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Spondylodiscitis: update on diagnosis and management. Gouliouris T, Aliyu SH, Brown NM. J Antimicrob Chemother. 2010;65:0–24. doi: 10.1093/jac/dkq303. [DOI] [PubMed] [Google Scholar]
- 2.Candida osteomyelitis: analysis of 207 pediatric and adult cases (1970-2011) Gamaletsou MN, Kontoyiannis DP, Sipsas NV, et al. Clin Infect Dis. 2012;55:1338–1351. doi: 10.1093/cid/cis660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Candida spondylitis: comparison of MRI findings with bacterial and tuberculous causes. Lee SW, Lee SH, Chung HW, Kim MJ, Seo MJ, Shin MJ. AJR Am J Roentgenol. 2013;201:872–877. doi: 10.2214/AJR.12.10344. [DOI] [PubMed] [Google Scholar]
- 4.Candida vertebral osteomyelitis (CVO) 28 cases from a 10-year retrospective study in France. Richaud C, De Lastours V, Panhard X, Petrover D, Fantin B, Lefort A. Medicine. 2017;96:0. doi: 10.1097/MD.0000000000007525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.2015 Infectious Diseases Society of America (IDSA) Clinical Practice Guidelines for the diagnosis and treatment of native vertebral osteomyelitis in adults. Berbari EF, Kanj SS, Kowalski TJ, et al. Clin Infect Dis. 2015;61:0–46. doi: 10.1093/cid/civ482. [DOI] [PubMed] [Google Scholar]
- 6.Candida spondylodiscitis: an unusual case of thoracolumbar pain with review of imaging findings and description of the clinical condition. Torres-Ramos FM, Botwin K, Shah CP. https://pubmed.ncbi.nlm.nih.gov/16868600/ Pain Physician. 2004;7:257–260. [PubMed] [Google Scholar]
- 7.Candida parapsilosis spondylodiscitis after lumbar discectomy. Cho K, Lee SH, Kim ES, Eoh W. J Korean Neurosurg Soc. 2010;47:295–297. doi: 10.3340/jkns.2010.47.4.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Candida lusitaniae discitis after discogram in an immunocompetent patient. Werner BC, Hogan MV, Shen FH. Spine J. 2011;11:0–6. doi: 10.1016/j.spinee.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 9.Candida albicans diskitis after body piercing in an immunocompetent patient. Darrieutort-Laffite C, Lassalle C, Chouet-Girard F, Perez L, Dernis E. https://pubmed.ncbi.nlm.nih.gov/31528486/ Joint Bone Spine. 2013;80:226–227. doi: 10.1016/j.jbspin.2012.07.013. [DOI] [PubMed] [Google Scholar]