Sir,
Connective tissue nevus (CTN) are dermal hamartomas, formed as a result of an increase in or structural alterations of collagen, elastic fibres and/or mucopolysaccharides. The term was first described by Lewandosky in 1921, and later accepted in 1926 after the review by Gutmann.[1] Pierard and Lapiere classified CTN into reticular and adventitial. Zosteriform nevus is a rare form of reticular CTN.[1] Hereby, we describe a rare case of multidermatomal zosteriform collagenoma in a young male without any systemic involvement along with a detailed review of the literature.
An 18-year-old male presented with multiple asymptomatic skin-coloured to pigmented elevated lesions over the back and right shoulder that had been noticed by his mother since 3 years of age. There was no history of seizure, mental retardation, or any other feature suggestive of systemic involvement. Family history was unremarkable. On cutaneous examination, multiple skin-coloured to reddish-brown soft papules and plaques were noted over the right shoulder, antero-lateral aspect of the neck, upper chest, and left side of the back in a zosteriform distribution involving C2-T3 dermatome on right side and T3-T12 dermatome on left side [Figure 1a-d]. Melanocytic nevi were noticed within the lesions at two places. Other cutaneous, mucosal, general, and systemic examinations were within normal limits. Dermoscopy under polarized mode (Dermlite, DL4, 10X magnification) revealed a cerebriform pattern, comedo-like openings, keratotic plugs, tufts of hair coming out of each follicle, pigment network and fingerprint-like structures (parallel pigmented lines) [Figure 2a-d]. Differential diagnosis of connective tissue nevus and nevus lipomatous superficialis was kept and biopsy was done. Histopathological examination revealed follicular plugging, irregular acanthosis, mild papillomatosis, and increased dermal collagen extending till the subcutaneous tissue [Figure 3a]. Collagen bundles were arranged haphazardly, few bundles were oriented perpendicular to the overlying epidermis [Figure 3b]. Masson-trichome stain highlighted the increased disorganized collagen [Figure 3c and d]. Verhoeff-Van Gieson staining revealed a paucity of elastic fibres along with fragmentation [Figure 3e and f]. A diagnosis of multidermatomal zosteriform collagenoma with non-allelic twin spotting was made. The patient was counselled about the benign nature of the disease and is kept under regular follow-up.
Figure 1.

Multiple skin-coloured to reddish-brown soft papules and plaques were noted over (a) left lower back (b) posterior aspect of right shoulder (c) anterior aspect of right shoulder (d) right deltoid region in a zosterifom distribution
Figure 2.
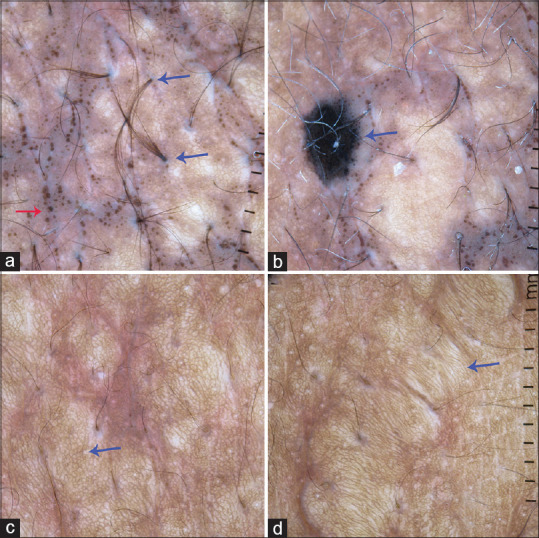
Dermoscopy showing (a) Comedo-like opening (red arrow), and tuft of hairs (blue arrow). (b) Brown-black blotch suggestive of melanocytic nevus (twin spotting, blue arrow). (c) Reticular network pattern (blue arrow). (d) Fingerprint-like structures (blue arrow)
Figure 3.
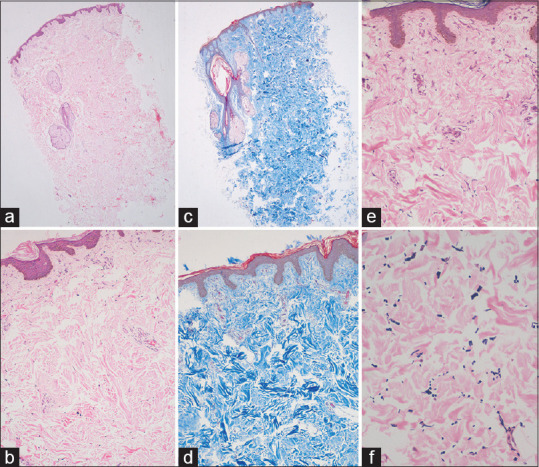
Histopathology showing (a) follicular plugging, irregular acanthosis, mild papillomatosis, and increased dermal collagen extending till the subcutaneous tissue (H and E, 10X). (b) Collagen bundles arranged haphazardly, few bundles were oriented perpendicular to the overlying epidermis (H and E, 40X). (c and d) Masson-trichome stain highlighting the increased disorganized collagen (H and E, 10 and 40X). (e and f) Verhoeff-Van Gieson staining showing paucity of elastic fibres along with fragmentation (H and E, 10 and 40X)
Connective tissue nevi are classified based upon the predominant component, into collagen, elastic, proteoglycan nevi, and nevi of adventitial connective tissue.[2] Clinically, connective tissue nevus presents as firm flesh coloured nodules or plaques with irregular borders, can be polylobulated or cerebriform depending upon the depth. Although difficult to distinguish from collagenoma, elastoma may impart a yellowish hue.[3] A large connective tissue nevus on the lower back resembling peau d' orange may represents a manifestation of tuberous sclerosis, whereas multiple small- to medium-sized lesions on anterior trunk or extremities imparting a yellowish hue favours more towards the Buschke Ollendorff syndrome.[4] Collagen nevi are further classified into hereditary and acquired. The hereditary types inherit as an autosomal dominant pattern and include dermatofibrosis lenticularis disseminata in Buschke–Ollendorff syndrome, familial cutaneous collagenoma, and shagreen patch of tuberous sclerosis. Acquired forms include isolated collagenoma, eruptive collagenoma, linear or zosteriform collagenoma, knuckle pad collagenoma and papulo-linear collagenoma.[2] Collagenoma should raise suspicion for tuberous sclerosis, in absence of which, a prompt consideration of multiple endocrine neoplasia type 1, Brit-Hogg-Dube syndrome, familial cutaneous collagenomas, eruptive collagenoma and storiform collagenomas of Cowden syndrome to be made.[4] The collagenomas in multiple endocrine neoplasia type 1 usually occurs at a later onset, and mostly located on the anterior chest, abdomen, proximal arms and back.[4] In the index case, the lesions had a bilateral asymmetrical multidermal zosteriform distribution without any syndromic association.
The pathogenesis of collagenoma is ambiguous but the key event remains decreased production of collagenase leading to decreased collagen degradation. Besides, the mitosis time for fibroblasts is decreased in collagenoma, which leads to increased accumulation of collagen.[5]
Zosteriform presentation of collagenoma is extremely rare. We found only 14 cases of zosteriform connective tissue nevus has been described in the literature previously [Table 1], with Steiner being the first to describe the condition in 1944.[1,2,6,7,8,9,10,11,12,13,14,15,16,17] Out of the 14 cases described previously, only 7 cases were collagen tissue nevus.
Table 1.
Review of zosteriform connective tissue nevus reported in literature highlighting the case reports with zosteriform collagenoma
| Case | Age in years/Gender | Site of the lesion | Histopathological features | Associated systemic disease |
|---|---|---|---|---|
| Steiner[6] (1944) | 5/F | Right lower chest and back | Abnormal collagen and elastic tissue | None |
| Kozminsky et al.[7] (1985) | 23/F | Left upper dorsum and dorsum of left arm | Alterations of elastic tissue | None |
| Yeh et al.[8] (2003) | 3/M | Right side of abdomen and flank | Sparse, and fragmented elastic tissue | None |
| Amjadi et al.[9] (2007) | 25/M | Right lower lumbar and upper gluteal region | Increased collagen | Segmental neurofibromatosis |
| Brazzelli et al.[10] (2007) | 8/F | Right lumbosacral area | Thickened and sclerotic collagen and thinned elastic fibres | None |
| Chang et al.[11] (2003) | 14/M | Lower back | Increased proteoglycan and absent collagen and elastic fibres | None |
| Asano et al.[12] (2007) | 8/M | Right forearm, right lower limb and right side of abdomen | Abnormal collagen and increased, and fragmented elastic fibres | None |
| Choi et al.[13] (2011) | 1 year 8 months/F | Left side of chest and abdomen | Increased collagen and decreased elastic fibre | None |
| Castalleno-Gonzalez et al.[14] (2012) | 14/F | Right deltoid and lower back | Reduced and fragmented elastic fibres | None |
| Dubiel et al.[15] (2014) | 20/F | Right leg | Increased collagen and decreased elastic fibres | None |
| Topal et al.[16] (2014) | 10/M | Right arm | Increased collagen bundles, decreased elastic fibres | None |
| Cerman et al.[1] (2016) | 8/F | Right buttock | Increased collagen, and diminished elastic fibres | None |
| Das et al.[2] (2017) | 4/M | Bilateral lumbosacral, and right shoulder and thigh | Thickened collagen | None |
| Lee et al.[17] (2018) | 34/M | Right lower back | Reduced elastic fibre and mucin deposition | None |
| Present case | 18/M | Right shoulder and left back region | Increased collagen, and sparse and fragmented elastic fibres | None |
Reddish brown strands with white dots giving a cobblestone appearance[18] and yellowish globules of different sizes against a brown background[19] has been reported in the dermoscopy of shagreen patch.
Histopathologically, accumulation of dense and coarse collagen with a relative decrease in elastic fibers in the dermis are the diagnostic features of collagenoma. The alteration in elastic fibers is probably as a result of a dilution phenomenon.[3] The closest differential diagnoses are, nevus lipomatosus superficialis and segmental neurofibromatosis.[9] The presence of ectopic fat in the dermis is pathognomonic for nevus lipomatosus superficialis.[9]
As the disease remains asymptomatic, treatment is only for cosmetic concerns. Although there are no specific guidelines, careful personal and family history should be taken in all the cases of connective tissue nevus, to rule out a syndromic association.[3] Surgical removal of lesions remains the mainstay of treatment. Satisfactory treatment of collagenoma has been observed with intralesional triamcinolone acetonide. The therapeutic response is attributed to a decrease in the production of transforming growth factor β1 and increased production of basic fibroblast growth factor by fibroblasts, leading to inhibition of fibroblast mitosis and collagen synthesis.[5]
In conclusion, Zosteriform connective tissue nevus is very rare. We report a rare case of bilateral multidermatomal zosteriform collagenoma in a young male without any syndromic association.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Aksu Çerman A, Aktaş E, Kıvanç Altunay IK, Demirkesen C. Zosteriform collagen nevus in an infant. Acta Dermatovenerol Croat. 2016;24:148–9. [PubMed] [Google Scholar]
- 2.Das A, Kumar P. Multidermatomal zosteriform collagen nevus. Indian J Paediatr Dermatol. 2017;18:142–3. [Google Scholar]
- 3.McCuaig CC, Vera C, Kokta V, Marcoux D, Hatami A, Thuraisingam T, et al. Connective tissue nevi in children: Institutional experience and review. J Am Acad Dermatol. 2012;67:890–7. doi: 10.1016/j.jaad.2012.01.036. [DOI] [PubMed] [Google Scholar]
- 4.Bongiorno MA, Nathan N, Oyerinde O, Wang JA, Lee CR, Brown G, et al. Clinical characteristics of connective tissue nevi in tuberous sclerosis complex with special emphasis on shagreen patches. JAMA Dermatol. 2017;153:660–5. doi: 10.1001/jamadermatol.2017.0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saki N, Dorostkar A, Heiran A, Aslani FS. Satisfactory treatment of a large connective tissue nevus with intralesional steroid injection. Dermatol Pract Concept. 2018;8:12–4. doi: 10.5826/dpc.0801a03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steiner K. Connective tissue nevus. Arch Dermatol Syphilol. 1944;50:183–90. [Google Scholar]
- 7.Kozminsky ME, Bronson DM, Barsky S. Zosteriform connective tissue nevus. Cutis. 1985;36:77–8. [PubMed] [Google Scholar]
- 8.Yeh SW, Magalhaes AM, Vasconcellos MR, Michalany NS, Tomimori Yamashita J. Zosteriform connective tissue nevus: A case report. Int J Dermatol. 2003;42:720–22. doi: 10.1046/j.1365-4362.2003.01774.x. [DOI] [PubMed] [Google Scholar]
- 9.Amjadi M, Khorrami-Arani N, Mashman G, Allen PW. Zosteriform connective tissue nevus: A case report. Am J Dermatopathol. 2007;29:303–5. doi: 10.1097/DAD.0b013e3180465694. [DOI] [PubMed] [Google Scholar]
- 10.Brazzelli V, Muzio F, Barbagallo T, Fornara L, Donadini F, Guerci B, et al. Zosteriform connective tissue nevus in a pediatric patient. Pediatr Dermatol. 2007;24:557–8. doi: 10.1111/j.1525-1470.2007.00520.x. [DOI] [PubMed] [Google Scholar]
- 11.Chang SE, Kang SK, Kim ES, Lee MW, Choi JH, Sung KJ, et al. A case of congenital mucinous nevus: A connective tissue nevus of the proteoglycan type. Pediatr Dermatol. 2003;20:229–31. doi: 10.1046/j.1525-1470.2003.20309.x. [DOI] [PubMed] [Google Scholar]
- 12.Asano Y, Ihn H, Tamaki K. Linear connective tissue nevus. Pediatr Dermatol. 2007;24:439–41. doi: 10.1111/j.1525-1470.2007.00477.x. [DOI] [PubMed] [Google Scholar]
- 13.Choi YJ, Lee SJ, Choi CW, Kim WS, Lee GY. Multiple unilateral zosteriform connective tissue nevi on the trunk. Ann Dermatol. 2011;23(Suppl 2):S243–6. doi: 10.5021/ad.2011.23.S2.S243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Castellanos-González M, Petiti-Martín G, Postigo C, Rodriguez-Peralto JL. Zosteriform connective tissue nevus: A new case report. Actas Dermosifiliogr. 2012;103:640–2. doi: 10.1016/j.ad.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Dubiel W, Kiehlmann I, Happle R. Linear collagen naevus: An unusual connective tissue disorder. Acta Derm Venereol. 2014;94:361–2. doi: 10.2340/00015555-1747. [DOI] [PubMed] [Google Scholar]
- 16.Topal IO, Kamali GH, Gungor S, Goncu OE. Zosteriform collagen nevus in a young boy. Dermatol Online J. 2014;20:13030/qt52c8120x. [PubMed] [Google Scholar]
- 17.Lee MY, Byun JY, Choi HY, Choi YW. Mucinous Nevus. Ann Dermatol. 2018;30:465–7. doi: 10.5021/ad.2018.30.4.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gundalli S, Ankad BS, Ashwin PK, Kolekar R. Dermoscopy of shagreen patch: A first report. Our Dermatol Online. 2015;6:331–3. [Google Scholar]
- 19.Gajjar PC, Mehta HH, Gosai M. Dermoscopy of congenital dermatoses in pediatric age group: An observational study. Indian J Paediatr Dermatol. 2019;20:219–26. [Google Scholar]


