Abstract
Background
The addition of hyperthermic intraperitoneal chemotherapy (HIPEC) to interval cytoreductive surgery improves recurrence-free and overall survival in patients with FIGO stage III ovarian cancer who are ineligible for primary cytoreductive surgery. The effect of HIPEC remains undetermined in patients who are candidates for primary cytoreductive surgery.
Primary objective
The primary objective is to evaluate the effect of HIPEC on overall survival in patients with FIGO stage III epithelial ovarian cancer who are treated with primary cytoreductive surgery resulting in no residual disease, or residual disease up to 2.5mm in maximum dimension.
Study hypothesis
We hypothesize that the addition of HIPEC to primary cytoreductive surgery improves overall survival in patients with primary FIGO stage III epithelial ovarian cancer.
Trial design
This international, randomized, open-label, phase III trial will enroll 538 patients with newly diagnosed FIGO stage III epithelial ovarian cancer. Following complete or near-complete (residual disease ≤2.5mm) primary cytoreduction, patients are randomly allocated (1:1) to receive HIPEC or no HIPEC. All patients will receive six courses of platinum-paclitaxel chemotherapy, and maintenance PARP-inhibitor or bevacizumab according to current guidelines.
Major eligibility criteria
Patients with FIGO stage III primary epithelial ovarian, fallopian tube, or primary peritoneal cancer are eligible after complete or nearcomplete primary cytoreductive surgery. Patients with resectable umbilical, spleen, or local bowel lesions may be included. Enlarged extra-abdominal lymph nodes should be negative on FDG-PET or fine-needle aspiration/biopsy.
Primary endpoint
The primary endpoint is overall survival.
Sample size
To detect a HR of 0.67 in favor of HIPEC, 200 overall survival events are required. With an expected accrual period of 60 months and 12 months additional follow-up, 538 patients need to be randomized.
Estimated dates for completing accrual and presenting results
The OVHIPEC-2 trial started in January 2020 and primary analyses are anticipated in 2026.
Trial registration
Introduction
Ovarian cancer has the highest mortality of all gynecologic cancers in the developed world.1 More than 75% of patients are diagnosed with advanced stage disease – disease that has spread beyond the ovaries to the peritoneal surfaces of the pelvis and abdomen. The 10-year survival of women with advanced ovarian cancer (International Federation of Gynecology and Obstetrics (FIGO) stage III and IV) is 10%–15%and has not improved over the past 20 years.2 There is an unmet medical need for therapeutic strategies that prevent or delay disease recurrence and improve survival.
The peritoneal surface is the primary site for ovarian cancer to recur, highlighting the need for therapeutic approaches that specifically target the peritoneal surface. Intraperitoneal delivery of chemotherapy leads to higher intracellular concentrations compared with intravenous delivery and has a penetration depth up to 2.5mm.3,4 Intraperitoneal chemotherapy thus effectively targets microscopic residual disease after macroscopically complete cytoreduction. Previous randomized clinical trials showed significant survival benefit with adjuvant normothermic intraperitoneal/ intravenous chemotherapy cycles administered using a transabdominal catheter.5–8 Increased toxicity, logistic challenges, and catheter-related adverse events limited uptake in clinical practice. Moreover, results of the randomized GOG 252 study suggesting that intraperitoneal delivery is non-superior if bevacizumab is added, have contributed to its underuse.9
Hyperthermic intraperitoneal chemotherapy (HIPEC) is a single procedure in which heated chemotherapy is administered into the peritoneal cavity at the end of the cytoreductive surgery. The elevated temperature enhances the penetration of chemotherapy, causes denaturation of intracellular proteins, and increases the sensitivity to platinum-based chemotherapy by transiently impairing DNA damage repair.10–12 In contrast to intraperitoneal administration using a catheter, HIPEC allows for equal distribution of chemotherapy through the peritoneal cavity without catheter- related complications. The randomized OVHIPEC study provides further evidence that adding HIPEC to interval cytoreductive surgery improves recurrence-free and overall survival in patients with stage III ovarian cancer, who are ineligible for primary cytoreductive surgery due to extensive intraperitoneal disease.13 A 5-year survival benefit of 10% was shown in patients who received HIPEC. For the majority of stage III ovarian cancer patients upfront cytoreductive surgery is feasible and the effect of HIPEC in these patients remains uncertain. We hypothesize that the addition of HIPEC to a complete or nearcomplete primary cytoreductive surgery improves overall survival in patients with FIGO stage III epithelial ovarian, fallopian tube, or primary peritoneal cancer.
Methods
Trial design
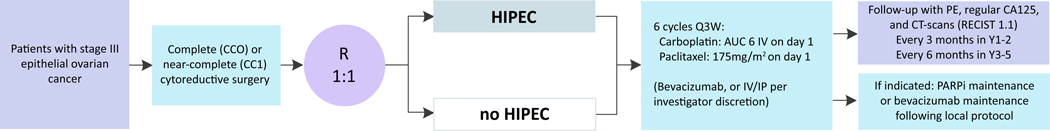
OVHIPEC-2 is an international, randomized, open-label, phase III trial that will enroll 538 patients with newly diagnosed FIGO stage III epithelial ovarian cancer. Following complete or near-complete (residual disease ≤2.5mm) primary cytoreduction, patients are randomly allocated (1:1) to receive HIPEC or no HIPEC. Randomization will take place in the operating room, after cytoreduction has been completed. All patients will receive six courses of platinumpaclitaxel based chemotherapy, and if indicated poly (ADP (ADP)- ribose) polymerase (PARP) inhibition and bevacizumab according to current guidelines (Figure 1). Written informed consent will be collected before any study-related procedures take place. Central randomization will be performed intra-operatively using ALEA online software, after complete or near-complete cytoreduction is achieved.
The trial is executed by the Dutch Gynaecological Oncology Group (DGOG) at 10 participating Dutch sites. Other selected hospitals with deputies in the Gynaecologic Cancer Intergroup (GCIG) and/or the European Network for Gynaecological Oncological Trial groups (ENGOT), and with documented experience in cytoreductive procedures and HIPEC procedures, may participate. The surgical team needs to perform at least 20 cytoreductive procedures for ovarian cancer per year and need to have prior experience of at least 10 HIPEC procedures for ovarian cancer before the start of accrual. Institutional review board approval for the trial has been obtained. The trial is funded by the Dutch Cancer Society (DCS), the Netherlands Organization for Health Research and Development (ZonMW), and the Coverage with Evidence Development (CED) program of the Dutch Ministry of Health.
Procedure
HIPEC will be performed using the open or closed technique. The abdomen is filled with saline, and the suspension is heated to 40°C–41°C, using a heat exchanger. With a flow rate of 1 liter per minute, perfusion with cisplatin 100mg/m2 is started. The HIPEC procedure is estimated to take 120min in total, including the 90-min perfusion period. To prevent nephrotoxicity, sodium thiosulphate will be administered intravenously at the start of perfusion and be continued up until 6 hours after the start of the infusion. The procedure was described previously.13 Patients in both study arms receive six cycles of adjuvant carboplatin-paclitaxel-based chemotherapy. In addition, PARP inhibition or bevacizumab will be administered according to current guidelines. Follow-up will be conducted every 3months for the first 2 years of follow-up, and every 6months in the following 3 years of the follow-up. CA125 will be measured during every follow-up visit, and computed tomography (CT) scans will be performed at end of treatment, and at 6, 12, and 24 months of follow-up.
Participants
Patients with FIGO stage III primary epithelial ovarian, fallopian tube, or primary peritoneal cancer are eligible after they receive complete or near-complete primary cytoreductive surgery. Patients with resectable umbilical lesions, spleen involvement, or local bowel involvement may also be included. Enlarged extra-abdominal lymph nodes should have a negative fluorine-18 fluorodeoxyglucose (FDG) traced positron-emission tomography (PET), or representative fine needle aspiration or biopsy. Pre-operative laparoscopy may be used to evaluate operability. Table 1 shows the full inclusion criteria. If successful primary cytoreductive surgery is not considered feasible, patients will be excluded. Specific criteria for nonresectability are listed in the full exclusion criteria in Table 2. A screening-log of all stage III and IV patients will be held in each participating hospital to monitor patient selection.
Table 1.
Inclusion criteria
| Eligible patients must meet all of the following criteria to be included in the OVHIPEC-2 trial: | |
|---|---|
| 1. | signed and written informed consent |
| 2. | age ≥18 |
| 3. | histological proven FIGO stage III primary epithelial ovarian, fallopian tube, or extra-ovarian cancer, treated with primary complete cytoreduction, or primary cytoreduction with no more than 2.5 mm residual disease |
| a. in case of extra-abdominal enlarged lymph nodes, representative cytology/histology or FDG-PET scan must be negative; | |
| b. resectable, local bowel involvement or spleen or umbilical lesions are allowed; | |
| c. in case no histological proof is available before surgery, patients can be randomized during surgery based on histological proof on intraoperative frozen section material | |
| 4. | fit for major surgery, World Health Organization performance status 0–2 |
| 5. | adequate bone marrow function (hemoglobin level >5.5 mmol/L; neutrophils >1.5 × 109/L; platelets >100 × 109 /L) |
| 6. | adequate hepatic function (ALT, AST and bilirubin <2.5 times upper limit of normal) |
| a. in case of Gilbert’s disease: bilirubin <5 times upper limit of normal | |
| 7. | adequate renal function (creatinine clearance using Cockcroft –Gault formula ≥ 60 ml/min) |
| 8. | baseline health-outcome questionnaire should be completed before randomization |
| 9. | able to understand the patient information and questionnaires |
Table 2.
Exclusion criteria
| A potential subject who meets any of the following criteria will be excluded from participation in this study: | |
|---|---|
| 1. | history of previous malignancy treated with chemotherapy |
| 2. | history of previous malignancy within five years prior to inclusion, with the exception of carcinoma in situ of the cervix, radically excised basal cell or squamous cell cancer of the skin or synchronal endometrial carcinoma FIGO IA G1/2 |
| 3. | if complete primary cytoreduction is not feasible, for the following reasons: |
| a. diffuse deep infiltration of the root of small bowel mesentery, and/or; | |
| b. diffuse carcinomatosis of the small bowel that requires resection that leads to short bowel syndrome (remaining bowel <1.5 meter), and/or; | |
| c. diffuse involvement/deep infiltration of stomach/duodenum, and/or; | |
| d. diffuse involvement/deep infiltration of head or middle part of pancreas, and/or; | |
| e. involvement of truncus coeliacus , hepatic arteries or left gastric artery, and/or; | |
| f. non-resectable enlarged (larger than 10 mm short axis) lymph nodes | |
| 4. | in case of a known psychiatric disorder, substance abuse disorder, or high suspicion of a mental disorder that could interfere with cooperation or compliance with the requirements of the trial |
| 5. | when opting for fertility sparing surgery |
| 6. | in case of 6a known history of Human Immunodeficiency Virus (HIV, or HIV 1/2 antibodies) |
| 7. | in case of known active Hepatitis B (e.g., HBsAg reactive) or Hepatitis C (e.g., HCV RNA [qualitative]) |
| 8. | patients who received prior treatment for the current malignancy |
Endpoints
The primary endpoint of this study is overall survival. Overall survival is defined as the time from randomization to the date of death from any cause. For subjects who are alive, their survival time will be censored at the date of last contact. Overall survival will be censored for subjects at the date of randomization if they were randomized but had no follow-up. Survival status will be updated for long-term overall survival for life. Secondary endpoints are recurrence-free survival, time to start of the first subsequent anticancer treatment after the first recurrence, and the incidence and grade of toxicity and morbidity. The definition of recurrence-free survival is specified as the time from randomization to the date of documented progression/recurrence, as determined by the Gynaecologic Cancer Intergroup criteria in combination with clinical and/or radiological assessments, or death due to any cause, whichever occurs first.14 Time to start of the first subsequent anticancer treatment after the first recurrence is an intermediate endpoint between recurrence-free survival and overall survival, considering time between recurrence and start of the next treatment line. Standardization of the follow-up with regular CA125 measurements and CT-scans at specific time points will be strictly adhered to in order to prevent bias in the measurement of secondary endpoints from the open-label design of the study. Exploratory endpoints are the time to second subsequent anticancer treatment after progressive disease, health-related quality of life, and cost-effectiveness. Pre-specified subgroup analyses will be performed based on the stratification factors (institute, peritoneal cancer index at start of surgery, and for completeness of surgery), histologic subtype, and BRCA mutation.
Sample size
Assuming a median overall survival after optimal or complete primary cytoreductive surgery in patients with stage III epithelial ovarian cancer of 49.7 months, a two-sided experiment-wise α=0.05 logrank test procedure requires 200 overall survival events to show a statistically significant difference in overall survival.5 This is calculated with set 80% power, when the true HR of the experimental arm to the control arm is similar to what was previously observed in patients after interval cytoreductive surgery (0.67).13 This sample size calculation accounts for two interim analyses after 67 and 133 events, with alpha spending function according to O’Brien–Fleming.15 Assuming that accrual will be completed in 60 months, and adding 12 months additional follow-up, 538 patients need to be randomized. In case of misspecification of the median survival for the control arm, the number of enrolled patients or minimum follow-up period may be changed during the course of the study to achieve the required number of events.
Randomization
Patients will be registered before surgery, and randomized during surgery after primary cytoreduction, when there is no more than2.5mm residual disease. If primary complete, or near-complete (≤2.5mm) cytoreduction is not feasible, patients will be considered a screening failure, and will not be randomized. Randomization with equal probability of assignment to each treatment regimen will be performed centrally by the method of minimization with a random element, using online ALEA software. Randomization will be stratified for institute, for low (0–15), intermediate (16–30), or high (31–45) ovarian peritoneal cancer index at the start of surgery, and for the completeness of surgery: complete cytoreduction or residual disease up to 2.5mm.
Statistical methods
The final analysis of the overall survival of patients in the trial will be conducted after 200 deaths have been observed. The outcome will be considered significant if the two-sided p-value is <0.045, to ensure overall type 1 error at 5%. The primary analysis will include tabulation of all cases entered, the distribution of important prognostic baseline variables, and observed results with respect to the primary and secondary endpoints. All randomized patients will be included in the analysis for overall survival according to the intention to treat principle. A sensitivity analysis will be carried out for the effect of HIPEC on overall survival excluding the patients who received adjuvant intraperitoneal/intravenous chemotherapy. The analysis of recurrence-free survival, and time to first subsequent anticancer treatment after first recurrent disease will be carried out similarly as the primary study parameter. The analysis of overall survival, recurrence-free survival, and time to first subsequent anticancer treatment after first recurrent disease will be based on Kaplan–Meier procedures, and the primary hypothesis will be evaluated by using the stratified logrank test. To adjust for random differences in baseline covariates, we will also estimate the treatment effect by Cox’s proportional hazard regression model, given that the proportional hazards assumptions are valid. Two interim analyses for efficacy of the primary endpoint are planned after 67 and 133 events for overall survival at a one-sided nominal P-value of 0.003 and 0.0071, respectively.
Recurrence-free survival as determined by the Gynaecologic Cancer Intergroup criteria, treatment-related toxicity and morbidity are secondary endpoints. Safety and tolerability will be measured by the incidence of adverse events, serious adverse events, adverse events leading to discontinuation, selected adverse events, and specific laboratory abnormalities (worst grade) in each treatmentgroup. Adverse events and laboratory abnormalities will be gradedusing the National Cancer Institute Common Terminology Criteria for Adverse Events version 5.0, and the Clavien–Dindo classification.16 An interim safety-run will be performed to evaluate the safety of HIPEC and adjuvant intraperitoneal/intravenous chemotherapy following 10 patients treated with HIPEC and intraperitoneal/intravenous adjuvant chemotherapy.
Discussion
The OVHIPEC trial showed that the addition of HIPEC to interval cytoreductive surgery is safe and improves recurrence-free survival and overall survival for patients with stage III ovarian cancer, who are ineligible for primary cytoreductive surgery due to the extent of disease.13 To determine if HIPEC has a similar effect when added to primary cytoreductive surgery, we initiated the randomized phase III OVHIPEC-2 trial. This trial randomizes patients who are treated with primary complete, or near-complete cytoreductive surgery to receive HIPEC or no HIPEC with the same treatment schedule that was administered in the OVHIPEC trial. The hyperthermia and the intraperitoneal chemotherapy may act synergistically, since the elevated temperature contributes to the penetration of chemotherapy and to the sensitivity to platinum-based chemotherapy. In in-vitro studies, the elevated temperature degrades BRCA2 and thereby inhibits homologous recombination, which in combination with double strand breaks caused by platinum-based chemotherapy, results in tumor cell death.10–12,17
The OVHIPEC-2 trial design does not allow us to disentangle the effects of hyperthermia and intraperitoneal delivery of chemotherapy. However, hyperthermia does not add major toxicity and a multi-arm trial that also includes arms with intraperitoneal heated saline or normal temperature intraperitoneal chemotherapy requires thousands of patients.
The current trial is designed as open-label trial, introducing potential open-label biases. Several measures are taken to limit these. Randomization takes place at the latest possible moment during surgery, after complete or almost complete (lesions up to 2.5mm) resection is reached. Surgical bias will thereby be minimized. To also minimize open-label bias during follow-up, scheduled follow-up visits with CA125 measurements and CT scans will be strictly adhered to.
To guarantee high surgical quality, requirements are in place for hospitals to participate in the trial: participating hospitals need to be involved in a national or regional trial group with a deputy in the Gynaecologic Cancer Intergroup, or the European Network for Gynaecological Oncological Trial group, and should have experience in cytoreductive procedures combined with HIPEC procedures for ovarian cancer.
Since HIPEC is a treatment strategy that is added to the primary surgical intervention, participation in the trial does not avert other adjuvant options. All patients in the trial are scheduled to receive six adjuvant cycles of carboplatin and paclitaxel. Patients may also receive maintenance treatment with PARP inhibition after first-line chemotherapy, according to local protocols.18–20 The same approach applies to other upfront strategies, for example, adjuvant intraperitoneal and intravenous chemotherapy, or maintenance bevacizumab. All first-line cancer treatment strategies and maintenance strategies that are administered during follow-up will be registered and closely monitored. The first line of treatment after the first recurrent disease will be registered.
Since BRCA mutational status and the histology type is not always known before start of the primary cytoreductive surgery, patients cannot be stratified for these characteristics. Central histological review will be performed for all participants and will be registered and reported. Pre-specified subgroup analysis will be performed for high-grade serous ovarian cancer vs other histological types. If somatic and/or germline BRCA testing is performed, these results will be registered for all patients and subgroup analysis will also be performed for somatic and germline BRCA mutations. The OVHIPEC-2 trial will elucidate whether the addition of HIPEC to primary cytoreductive surgery improves overall and recurrence-free survival in patients with stage III epithelial ovarian cancer. The results of this trial could potentially change practice for women with advanced stage ovarian cancer who still represent a patient population with a great unmet medical need.
Acknowledgements
D. Baars, M. Schrier, H. van Tinteren, A. Torres, V. Verwaal. Collaborators The International OVHIPEC-2 Steering Committee (in alphabetical order): N Bakrin, S Banerjee, S Barry, DP Barton, D Brennan, PE Colombo, M Deraco, WJ van Driel, A Fagotti, R Farrell, R Grisham, BJ Mosgaard, I McNeish, L Perrin, GS Sonke, O Zivanovic. The Dutch OVHIPEC group (in alphabetical order): HJG Arts, I Boere, GJ Creemers, WJ van Driel, KN Gaarenstroom, M van Gent, M van Ham, B Hellebrekers, R Hermans, I de Hingh, SN Koole, JR Kroep, CD de Kroon, R Lalisang, S Lambrechts, P Ottevanger, N Reesink, V Retel, AKL Reyners, EM Roes, HWR Schreuder, GS Sonke, RM van Stein, A Thijs, A Westermann, PO Witteveen, A Wymenga, R Yigit. Dutch Gynaecological Oncology Group (DGOG), Dutch Peritoneal Oncology Group (DPOG).
Funding The trial is funded by the Dutch Cancer Society (DCS), the Netherlands Organization for Health Research and Development (ZonMW), and the Coverage with Evidence Development (CED) program of the Dutch Ministry of Health.
Footnotes
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement Data will be available upon request
References
- 1.Bray F, Sankila R, Ferlay J, et al. Estimates of cancer incidence and mortality in Europe in 1995. Eur J Cancer 2002;38:99–166. [DOI] [PubMed] [Google Scholar]
- 2.Timmermans M, Sonke GS, Van de Vijver KK, et al. No improvement in long-term survival for epithelial ovarian cancer patients: a population-based study between 1989 and 2014 in the Netherlands. Eur J Cancer 2018;88:31–7. [DOI] [PubMed] [Google Scholar]
- 3.Dedrick RL, Myers CE, Bungay PM, et al. Pharmacokinetic rationale for peritoneal drug administration in the treatment of ovarian cancer. Cancer Treat Rep 1978;62:1–11. [PubMed] [Google Scholar]
- 4.Los G, Mutsaers PH, van der Vijgh WJ, et al. Direct diffusion of cis-diamminedichloroplatinum(II) in intraperitoneal rat tumors after intraperitoneal chemotherapy: a comparison with systemic chemotherapy. Cancer Res 1989;49:3380–4. [PubMed] [Google Scholar]
- 5.Armstrong DK, Bundy B, Wenzel L, et al. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med 2006;354:34–43. [DOI] [PubMed] [Google Scholar]
- 6.Tewari D, Java JJ, Salani R, et al. Long-term survival advantage and prognostic factors associated with intraperitoneal chemotherapy treatment in advanced ovarian cancer: a Gynecologic Oncology Group study. JCO 2015;33:1460–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wright AA, Cronin A, Milne DE, et al. Use and effectiveness of intraperitoneal chemotherapy for treatment of ovarian cancer. JCO 2015;33:2841–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jaaback K, Johnson N, Lawrie TA, et al. Intraperitoneal chemotherapy for the initial management of primary epithelial ovarian cancer. Cochrane DB Syst Rev 2011;11:1–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walker JL, Brady MF, Wenzel L, et al. Randomized trial of intravenous versus intraperitoneal chemotherapy plus bevacizumab in advanced ovarian carcinoma: an NRG Oncology/Gynecologic Oncology Group study. JCO 2019;37:1380–90. 1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ohno S, Siddik ZH, Kido Y, et al. Thermal enhancement of drug uptake and DNA adducts as a possible mechanism for the effect of sequencing hyperthermia on cisplatin-induced cytotoxicity in L1210 cells. Cancer Chemother Pharmacol 1994;34:302–6. [DOI] [PubMed] [Google Scholar]
- 11.Spratt JS, Adcock RA, Muskovin M, et al. Clinical delivery system for intraperitoneal hyperthermic chemotherapy. Cancer Res 1980;40:256–60. [PubMed] [Google Scholar]
- 12.van de Vaart PJM, van der Vange N, Zoetmulder FAN, et al. Intraperitoneal cisplatin with regional hyperthermia in advanced ovarian cancer: pharmacokinetics and cisplatin–DNA adduct formation in patients and ovarian cancer cell lines. Eur J Cancer 1998;34:148–54. [DOI] [PubMed] [Google Scholar]
- 13.van Driel WJ, Koole SN, Sikorska K, et al. Hyperthermic intraperitoneal chemotherapy in ovarian cancer. N Engl J Med 2018;378:230–40. [DOI] [PubMed] [Google Scholar]
- 14.Rustin GJS, Vergote I, Eisenhauer E, et al. Definitions for response and progression in ovarian cancer clinical trials incorporating RECIST 1.1 and Ca 125 agreed by the gynecological cancer intergroup (GCIG). Int J Gynecol Cancer 2011;21:419–23. [DOI] [PubMed] [Google Scholar]
- 15.Kumar A, Chakraborty BS. Interim analysis: a rational approach of decision making in clinical trial. J Adv Pharm Technol Res 2016;7:118–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187–96. [DOI] [PubMed] [Google Scholar]
- 17.Krawczyk PM, Eppink B, Essers J, et al. Mild hyperthermia inhibits homologous recombination, induces BRCA2 degradation, and sensitizes cancer cells to poly (ADP-ribose) polymerase-1 inhibition. Proc Natl Acad Sci U S A 2011;108:9851–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moore K, Colombo N, Scambia G, et al. Maintenance olaparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med 2018;379:2495–505. [DOI] [PubMed] [Google Scholar]
- 19.Coleman RL, Fleming GF, Brady MF, et al. Veliparib with first-line chemotherapy and as maintenance therapy in ovarian cancer. N Engl J Med 2019;381:2403–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.González-Martín A, Pothuri B, Vergote I, et al. Niraparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med 2019;381:2391–402. [DOI] [PubMed] [Google Scholar]