Abstract
Background and Aims:
Transmuscular Quadratus Lumborum Block (TQLB) is a novel regional anaesthesia technique, however, its analgesic efficacy as a component of multimodal analgesia (MMA) in Total Laparoscopic Hysterectomy (TLH) is not well studied. The aim of the study was to evaluate the analgesic efficacy of TQLB as a component of MMA for postoperative pain in TLH.
Methods:
A prospective double-blind randomised controlled study was done after approval from the ethical committee and informed patient consent. After randomisation, 37 patients in Group-Q received 20 ml 0.375% ropivacaine and in Group-C, 37 patients received saline in TQLB bilaterally after TLH surgery. All patients received intravenous patient controlled analgesia (IV-PCA) with fentanyl along with diclofenac 75 mg every 12 h. All the patients were assessed at 2, 4, 6, 8, 12, 18, and 24 hours. The primary outcome was the time to first analgesic request. The secondary outcome measures were total fentanyl consumption in 24 hrs, pain scores during rest and movement, postoperative nausea-vomiting, sedation and complications related to local anaesthetic and TQLB procedure.
Results:
The mean [standard deviation (SD)] time to first analgesic request was 7.8 (1.5) hours in Group-Q and 3.2 (1.0) hours in Group-C (P < 0.0001). The mean (SD) dose of fentanyl used in 24 hours was 167.3 (44) μg in Group-Q and 226.5 (41.9) μg in Group-C (P < 0.0001).
Conclusion:
The ultrasound-guided TQLB provides effective postoperative analgesia after TLH surgery in a multimodal analgesia approach. It reduces the fentanyl consumption and improves the visual analogue scale (VAS) score.
Keywords: Analgesia, hysterectomy, laparoscopy, nerve block
INTRODUCTION
The high levels of postoperative pain experienced by patients of total laparoscopic hysterectomy (TLH) is often difficult to control which leads to an increased opioid use and delayed discharge from the hospital.[1] Recently, quadratus lumborum block (QLB) has been incorporated as an adjunct to multimodal analgesia (MMA) for postoperative pain relief and the studies have shown that Transmuscular QLB has better analgesic profile compared to other QLB approaches.[2,3] However, the literature on the TQLB for postoperative analgesia in TLH is still limited. Therefore, we aimed to conduct this study of TQLB to assess the efficacy of TQLB as a part of multimodal analgesic regimen in TLH. The primary objective was to evaluate the duration of pain relief after TQLB and the secondary objectives were to compare the amount of fentanyl consumption, the pain scores, the post-operative nausea vomiting (PONV) and the block related complications in the TQLB group compared to the control group.
METHODS
This was a prospective randomised double blinded case-control study, approved by the ethics and scientific committee of the institution and was conducted during January 2018 to December 2019. A total of 74 female patients aged between 30-60 years with American Society of Anesthesiologists (ASA) physical status class 1 or 2 planned for non-emergency TLH under GA and given the informed consent were included in this study. Patients with history of allergy to local anaesthetic drugs, having contraindications to regional anaesthesia (bleeding disorder, peripheral neuropathy and infection at the site of block), uncontrolled diabetes, hypertension or cardio-respiratory disease were excluded. The subjects were randomly allocated into Group-Q (to receive block with local anaesthetic) and Group-C (control, to receive block with saline) using a computer-generated sequence of random numbers. The group sequence was concealed in sealed opaque envelopes, which were opened only after obtaining informed consent. Two syringes of 20 ml containing either 40 ml saline or 40 ml 0.375% ropivacaine were prepared by an anaesthesiologist who was not involved in the study. The anaesthesiologist, the subjects and the post-operative care providers were blinded to the group assignment. As per hospital practice, injection metoclopramide (10 mg) and ranitidine (50 mg) were given intravenously 1 hr before surgery. In the operation room, vascular access was secured using an 18-gauge intravenous cannula and prophylactic antibiotic was given as per hospital protocol. Standard non-invasive monitors like electrocardiograph (ECG), non-invasive blood pressure (NIBP) monitor, and pulse oximeter were connected and base line values were recorded. Anaesthesia was induced by IV injection of 2-3 mg/kg propofol, 2 μg/kg fentanyl, and vecuronium 0.1 mg/kg body weight as muscle relaxant. Following endotracheal intubation, general anaesthesia was maintained with a mixture of oxygen and nitrous oxide (40:60) and isoflurane (1% end-tidal concentration), maintaining an end-tidal carbon dioxide level of 35–40 mm Hg. The isoflurane concentration was adjusted to maintain blood pressure and heart rate values within 20% of the preoperative measurements, IV bolus of fentanyl (0.5–1 μg/kg) was used for analgesia as necessary. After the surgery, US-guided TQLB was given by one of the expert anaesthetists (AJ/NS/SC) who had >4 years of experience in US-guided regional anaesthesia. After the block, patients were extubated after adequate recovery of consciousness and spontaneous respiration. All the subjects received 75 mg diclofenac IV during skin closure and then at 12 hourly intervals.
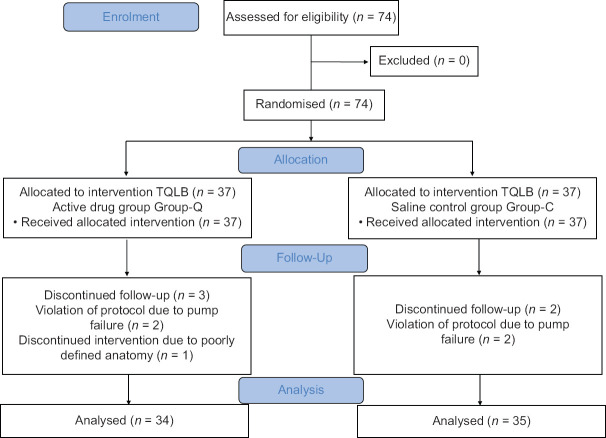
To perform TQLB, patients were turned to left lateral decubitus position. After sterile preparation, low frequency ultrasound probe (2-5 MHz, SonoSite, Turbo- M) was placed just cranial to iliac crest to identify the Shamrock sign. A 21-gauge, 100-mm needle (Stimuplex® A, B. Braun, Melsungen AG) was then inserted in-plane (posterior to anterior direction) and directed to the QL muscle. After the proper position of the needle tip between the psoas major muscle and the QL muscle (the position of needle tip was confirmed with 1-2 ml saline), 20 ml study drug (either of 0.375% ropivacaine (obtained by mixing 10 ml of 0.75% ropivacaine with 10 ml of normal saline) or normal saline (depending upon the allocated group) was injected into the interfascial plane on each side. Precaution was taken such that, the needle tip should always lie posterior to the fascia of psoas muscle and should not pierce the fascial covering of psoas muscle. We used the single decubitus position approach to inject on both sides as described earlier by Jadon et al. [Figure 1a-d].[4]
Figure 1.
(a) The patient in lateral position; curvilinear probe (2-6 MHz) just above and posterior to the iliac crest with the needle entering from the posterior to the anterior direction and its corresponding sonoanatomy (b). (c) Ultrasound probe position and needle entry for quadratus lumborum block of the opposite side and its corresponding sonoanatomy (d). QL – quadratus lumborum, PM – Psoas major, TP – Transverse process (L4), LA – Local anaesthetic.
After extubation patients were shifted to the post-anaesthesia care unit (PACU) and intravenous patient controlled analgesia (IV-PCA) with fentanyl was started with a demand dose of 20 μg, lockout period of 10 minutes and the 4 hr limit of 200 μg. The presence of pain during rest and on movement (on flexion of lower limbs) measured by the Visual Analogue Score (VAS) on the scale of 0-10 (0 = no pain and 10 = worst imaginable pain), pruritus, sedation, nausea, respiratory depression and haemodynamic parameters were assessed systematically in both the groups at 2, 4, 6, 12, 18 and 24 hours after the surgery. Time to first request for analgesia or time when patient had taken fentanyl bolus by PCA pump, and total dose of IV fentanyl consumed over 24 hours were recorded.
Severity of PONV was measured on the 4-point score (0 = absent, 1 = mild, 2 = moderate and 3 = severe or vomiting) and rescue antiemetic (4 mg of IV ondansetron) was given wherever score was >0. Pruritus was treated with injection diphenhydramine (25 mg) intramuscularly. Patients were evaluated for the level of sedation by using a 4-point sedation scale (1 = awake, 2 = sedated response to verbal command, 3 = sedated response to touch, 4 = deeply sedated and response to pain). Presence of respiratory depression was defined if patient had a respiratory rate less than 10/minute; injection naloxone 2-3 μg/kg IV was kept ready for use. At the end of the study period, patients were asked to rate their satisfaction with the pain control regimen using a 3-point scale (1 = highly satisfied, 2 = satisfied, or 3 = dissatisfied).
The primary outcome measures were the time to first analgesic request and the total dose of fentanyl required in 24 hours. The secondary outcome measures were the VAS scores, PONV scores, pruritus, sedation and respiratory depression and complications of TQLB.
Sample size was calculated by a computer-based software (G power version 3.1.4, Informer Technologies, Inc.) based on results obtained from a pilot study conducted at our institute (time to first analgesic mean (SD) 2.8 h (1.8). Assuming the 50% increase in the time (mean) to first request for analgesia as significant, keeping the power of the study at 80% and significance level of 95%, a total of 65 subjects were required to detect the significant difference. Seventy-four subjects were enroled into the study taking an account for attrition.
Statistical analysis was done using MedCalc® version 19.2.1 (USA). Intra-operative characteristics were assessed using the student's t-test (two tailed, unequal variances) and Chi square test as appropriate. Continuous data was assessed for normality using the “Kolmogorov-Smirnov test” of normality. Normally distributed data (represented as mean ± SD) was assessed using the student's t-test (two-tailed, unequal variances) and non-normally distributed data [represented as median (IQR, 25th & 75th percentile)] was assessed using the Mann-Whitney U-test. Ordinal data were represented as median & IQR and assessed using the Mann-Whitney U-test. A P value < 0.05 was considered significant.
RESULTS
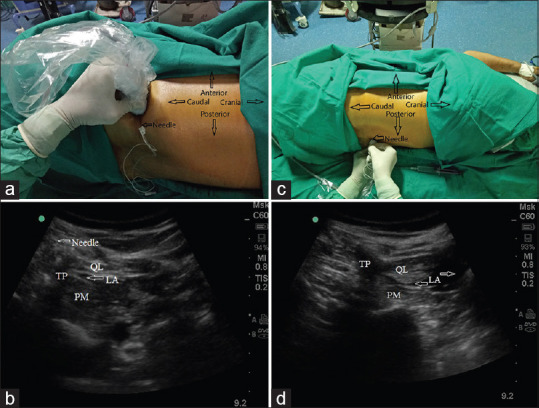
A total of 74 patients (37 in Group-C and 37 in the Group-Q) were enroled into the study. Two patients in the Group-C were excluded (due to violation of protocol). In Group-Q three patients were excluded (two because of violation of protocol and, one because of inability to localise the correct plane for injection). Totally 69 patients (n = 35 Group-C & n = 34 Group-Q) were analysed [Figure 2]. The demographic variables, intraoperative vital parameters, duration of surgery and intraoperative fentanyl consumptions were comparable in both the groups [Table 1]. The mean (SD) time to first analgesic request was 7.8 (1.5) hours in Group-Q and 3.2 (1.0) hours in Group-C, 95% CI (3.9 -5.1) (P < 0.0001) [Table 2]. The mean (SD) dose of fentanyl used in 24 hours was 167.3 (44.0) μg in Group-Q and 226.5 (41.9) μg in Group-C, 95% CI (38.5- 79.8) (P < 0.0001) [Table 2]. At all points during the study, pain scores both at rest and on movement were significantly lower in the Group-Q compared to the Group-C [p < 0.0001, [Table 3]. There was no difference with respect to nausea scores, sedation and pruritus between the two groups [Table 4]. None of the subjects needed naloxone. No patient had any local anaesthetic or block related complication during the block or muscle weakness in the postoperative period.
Figure 2.
Consort diagram of enrolment, randomisation, allocation and follow-up of subjects. TQMB – Transmuscular Quadratus Lumborum Block
Table 1.
Demographic Characteristics of Patients, Duration of Surgery and Intraoperative Fentanyl Used in Group-C and Group-Q
| Parameter | Group-Q (n=34) | Group-C (n=35) | P |
|---|---|---|---|
| Age (year) | 43.5 (7.9) | 43.5 (4.4) | 0.989 |
| Weight (kg) | 61.3 (7.5) | 63.2 (8.2) | 0.302 |
| Height (cm) | 150.8 (4.9) | 151.6 (5.7) | 0.505 |
| ASA (I/II) | 6/28 | 8/27 | 0.765 |
| Heart Rate (/min) Mean (SD) | 77.5 (8.3) | 81.2 (7.5) | 0.053 |
| MAP (mmHg) | 74.5 (6.5) | 75.6 (7.4) | 0.52 |
| SpO2 (%) | 99.6 (0.6) | 99.6 (0.7) | 0.836 |
| Duration of Surgery min | 153 (38) | 150 (42) | 0.756 |
| Intra-operative fentanyl used Mean (SD) µg | 124.8 (29.2) | 125.9 (27.6) | 0.873 |
ASA-American Society of Anesthesiologists;SD-Standard Deviation; SpO2- Peripheral oxygen saturation; MAP-Mean arterial pressure; *All measured values are presented as mean and standard deviation (SD)
Table 2.
Time to First Analgesic Request and The Dose of Fentanyl Used in 24 h in Group-Q and Group-C
| Group-Q (n=34) | Group-C (n=35) | 95% CI | P |
|---|---|---|---|
| Time to first analgesic request, mean (SD) hours | |||
| 7.8 (1.5) | 3.2 (1.0) | 3.9-5.1 | P<0.0001 |
| Fentanyl used in 24 h, mean (SD) µg | |||
| 167.3 (44.0) | 226.5 (41.9) | 38.5-79.8 | P<0.0001 |
Table 3.
Comparative VAS score during rest and movement in Group-Q and Group-C at various time points from 2 h-24 h
| Variable | Group Q (n=34) median (IQR) | Group C (n=35) median (IQR) | P |
|---|---|---|---|
| VAS Score at rest | |||
| 2 h | 1 (1.5,4) | 3 (2,5) | <0.0001 |
| 4 h | 1 (0,1) | 3 (2,4) | <0.0001 |
| 6 h | 1 (1,2) | 2 (1.5,5) | <0.0001 |
| 12 h | 1 (1,2) | 2 (2,3) | <0.0001 |
| 18 h | 1 (1,2) | 2.5 (2,3) | <0.0001 |
| 24 h | 1 (1,2) | 2 (1,2.5) | 0.0001 |
| VAS Score on movement | |||
| 2 h | 1 (0,1) | 4 (3,6) | <0.0001 |
| 4 h | 2 (1,2) | 4.5 (3,6) | <0.0001 |
| 6 h | 2 (2,3) | 3 (2,7) | <0.0001 |
| 12 h | 2 (2,2) | 4 (3,5) | <0.0001 |
| 18 h | 2 (1.25,2) | 3 (2.5,4) | <0.0001 |
| 24 h | 2 (1,2) | 3 (2,3.5) | <0.0001 |
The difference was significant P<0.0001 at all times. VAS-Visual analogue scale
Table 4.
Incidence of Post-Operative Nausea and Vomiting, Sedation, and Pruritus in Group-Q and Group-C
| Variables | Group-Q (n=34) | Group-C (n=35) | P |
|---|---|---|---|
| Nausea and Vomiting (Score) | |||
| Absent (1) | 26 | 20 | 0.836 |
| Mild (2) | 5 | 6 | |
| Moderate (3) | 2 | 7 | |
| Severe (4) | 1 | 2 | |
| Level of Sedation (Score) | |||
| Fully awake (1) | 25 | 20 | 0.350 |
| Respond to Verbal (2) | 7 | 11 | |
| Respond to Touch (3) | 2 | 4 | |
| Respond to Pain (4) | 0 | 0 | |
| Pruritus | |||
| Present | 1 | 2 | 0.572 |
| Absent | 33 | 33 |
*No significant differences between Group-Q and Group-C (P>0.05)
DISCUSSION
In this study we observed that TQLB provided effective pain relief compared to control group. Patients in the Group-Q had significantly prolonged time to first request to analgesia, reduced fentanyl requirement in 24 hours and lower VAS scores compared to Group-C.
Severe postoperative pain after TLH often requires aggressive management to avoid unnecessary suffering and delay in the discharge from the hospital.[1,5] MMA is the standard practice and the recent PROSPECT recommendations also suggest to use MMA to minimise the opioid use and its adverse effects.[6,7] Currently, truncal blocks became an important component of MMA. Initially, transversus abdominis plane (TAP) block was used for analgesia in TLH however, due limited extent of blockade and lack of visceral analgesia, their role in providing analgesia in TLH is debatable.[8,9,10]
In recent times, the QLB which is an evolution of the TAP block has been found to be superior than TAP block.[11,12,13] The exact mechanism of QLB is poorly understood, however the spread of local anaesthetic (LA) into the paravertebral space and the effect on sympathetic fibres are probable reasons for superior analgesia.[2,11,14]
There are many approaches of QLB and each approach has the variable spread of LA and variable clinical effects.[2,10,14,15,16,17] One recent study has also suggested that posterior QLB significantly reduces postoperative pain following laparoscopic gynaecological surgery.[18] However, the clinical studies evaluating the efficacy of TQLB for postoperative analgesia in TLH are lacking. Therefore, we conducted this study to evaluate the analgesic efficacy of TQLB in TLH surgery.
We preferred TQLB over other approaches of QLB because of extensive spread of LA in TQLB as shown in the various studies and also this approach has a definitive end point during needle placement.[16,19]
Many studies have observed and compared the pain relief beyond 24 hrs; however, we limited our study period for 24 hrs as that is the most painful period following TLH. Choi et al.,[20] observed that in TLH, visceral and the incisional pains were most intense on the day of operation and then decreased following surgery.
Studies have shown that morphine PCA is more effective than fentanyl PCA in controlling pain of laparoscopy surgery; however, we used fentanyl as PCA because fentanyl PCA has reduced incidence of PONV.[21] In our study, PONV was comparable between Group-C and Group-Q even when, subjects in Group-C used significantly higher amount of fentanyl than the subjects of Group-Q (p < 0.0001) [Table 2]. The postulation is that, pain itself may be a larger contributor for PONV than fentanyl per se[21] or it may be an incidental finding.
Sensory loss and motor weakness in the lower limbs have been reported in the studies of TQLB. Initially it was observed as a complication and later used as anaesthetic technique to provide analgesia in lower limb surgery.[3,22,23] However, we did not find any sensory loss or motor weakness in the lower limbs as reported in other studies. The spread of local anaesthetic over lumbar plexus leading to sensory changes and motor weakness of lower limb is decided by the position of needle during block. If block needle pierces the fascia of psoas muscle, the chances of motor weakness increases due to involvement of the lumbar plexus.[3,22,23] In our block technique, we were cautious to avoid the puncture of the psoas muscle fascia. However, this is just an assumption and may require further studies focussed on this particular aspect.
Early recovery after surgery is always the desirable goal and role of QLB is also evaluated in enhanced recovery after surgery (ERAS) protocols.[24] Our prospective double blinded randomised study provided evidence that, TQLB provides an effective analgesia in TLH and may be researched further with the objective to assess the Quality of Recovery (QoR).
TQLB requires a lateral decubitus position and positioning for bilateral blocks remains a challenge, particularly in the anaesthetised patient. Bilateral block while patient is lying on one side (either right or left lateral position) has been described earlier.[4] We used the same technique and found it suitable for our patients.
The strength of our study was its uniqueness as, this is one of the first studies where the efficacy of TQLB has been evaluated for analgesia in TLH. However, our study has many limitations. Firstly, no sensory mapping was done after TQLB; however, it was not done to avoid bias, as saline block would have shown the differentiable sensory changes to observer. Secondly, we did not describe the success and failure of the block, however expected the direct impact of failed block on the requirement of early rescue drug and higher requirement of fentanyl.
Every new block should have been evaluated for the safety profile. However, this study was not adequately powered to evaluate the safety concerns. Last but not the least, it can be argued that, although, VAS scores were significantly higher in Group-C than Group-Q, differences were not too high to have clinical relevance [Table 3]. Why should one venture into an invasive block like TQLB? This can simply be explainedby the fact that, we used IV-PCA in both the groups and previous studies have already proved the effectiveness of IV-PCA.[25] However, the extra advantage of TQLB is, the duration and quality of relief, which was better with TQLB. Moreover, the role of various nerve blocks in the prevention of chronic pain and persistent pain after surgery are the areas for further research which open the avenues for further research to find out the role of TQLB.[26]
To summarise our findings, the TQLB is a novel technique which can be used as an adjunct to multimodal analgesia for TLH. Group-Q patients had prolonged and better pain relief and required less fentanyl over 24 hours than patients of Group-C. Although, the calculated effect size (Hedges' g) was large enough for two important parameters to prove superiority of TQLB analgesia in TLH (3.47 for first request for analgesia and 1.37 for fentanyl used in 24 hours). However, before generalising the results and assuming its superiority on previously existing blocks used for pain relief in TLH, a comparative study with large participants is warranted.
CONCLUSION
Ultrasound-guided TQLB with thelocal anaesthetic ropivacaine prolongs the first request to analgesia, provides effective postoperative analgesia during rest as well as on movement after TLHand reduces fentanyl use compared to saline. We suggest further studies to evaluate the effect of TQLB on chronic pain and the safety profile of TQLB.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ekstein P, Szold A, Sagie B, Werbin N, Klausner JM, Weinbroum AA. Laparoscopic surgery may be associated with severe pain and high analgesia requirements in the immediate postoperative period. Ann Surg. 2006;243:41–6. doi: 10.1097/01.sla.0000193806.81428.6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dam M, Moriggl B, Hansen CK, Hoermann R, Bendtsen TF, Børglum J. The pathway of injectate spread with the transmuscular quadratus lumborum block: A cadaver study. Anesth Analg. 2017;125:303–12. doi: 10.1213/ANE.0000000000001922. [DOI] [PubMed] [Google Scholar]
- 3.Ueshima H, Yoshiyama S, Otake H. The ultrasound-guided continuous transmuscular quadratus lumborum block is an effective analgesia for total hip arthroplasty. J Clin Anesth. 2016;31:35. doi: 10.1016/j.jclinane.2015.12.033. [DOI] [PubMed] [Google Scholar]
- 4.Jadon A, Jain P, Dhanwani L. Bilateral transmuscular quadratus lumborum block performed in single lateral decubitus position without changing position to the contralateral side. Indian J Anaesth. 2018;62:314–5. doi: 10.4103/ija.IJA_750_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009;3:CD003677. [Google Scholar]
- 6.Refaat S, Mawgood AA, Sonbaty MA, Gamal M, Ahmed A. Multi-modal analgesic technique for pain control in patients undergoing diagnostic gynecological laparoscopy: Randomized controlled clinical trial. Open Access Maced J Med Sci. 2019;7:1324–9. doi: 10.3889/oamjms.2019.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lirk P, Thiry J, Bonnet M, Joshi GP, Bonnet F. Pain management after laparoscopic hysterectomy: Systematic review of literature and PROSPECT recommendations. Reg Anesth Pain Med. 2019;44:425–36. doi: 10.1136/rapm-2018-100024. [DOI] [PubMed] [Google Scholar]
- 8.Regmi S, Srinivasan S, Badhe AS, Satyaprakash MV, Adinarayanan S, Mohan VK. Comparison of analgesic efficacy of continuous bilateral transversus abdominis plane catheter infusion with that of lumbar epidural for postoperative analgesia in patients undergoing lower abdominal surgeries. Indian J Anaesth. 2019;63:462–8. doi: 10.4103/ija.IJA_20_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kane SM, Garcia-Tomas V, Alejandro-Rodriguez M, Astley B, Pollard RR. Randomised trial of transversus abdominis plane block at total laparoscopic hysterectomy: Effect of regional analgesia on quality of recovery. Am J Obstet Gynecol. 2012;207:e1–5. doi: 10.1016/j.ajog.2012.06.052. [DOI] [PubMed] [Google Scholar]
- 10.Chen Y, Shi K, Xia Y, Zhang X, Papadimos TJ, Xu X, et al. Sensory assessment and regression rate of bilateral oblique subcostal transversus abdominis plane block in volunteers. Reg Anesth Pain Med. 2018;43:174–9. doi: 10.1097/AAP.0000000000000715. [DOI] [PubMed] [Google Scholar]
- 11.Blanco R, Ansari T, Girgis E. Quadratus lumborum block for postoperative pain after caesarean section: A randomised controlled trial. Eur J Anaesthesiol. 2015;32:812–8. doi: 10.1097/EJA.0000000000000299. [DOI] [PubMed] [Google Scholar]
- 12.Verma K, Malawat A, Jethava D, Jethava DD. Comparison of transversus abdominis plane block and quadratus lumborum block for post-caesarean section analgesia.A randomised clinical trial. Indian J Anaesth. 2019;63:820–6. doi: 10.4103/ija.IJA_61_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yousef NK. Quadratus lumborum block versus transversus abdominis plane block in patients undergoing total abdominal hysterectomy: A randomised prospective controlled trial. Anesth Essays Res. 2018;12:742–7. doi: 10.4103/aer.AER_108_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carline L, McLeod GA, Lamb C, Colvin L. A cadaver study comparing spread of dye and nerve involvement after three different quadratus lumborum blocks. Br J Anaesth. 2016;117:387–94. doi: 10.1093/bja/aew224. [DOI] [PubMed] [Google Scholar]
- 15.El-Boghdadly K, Elsharkawy H, Short A, Chin KJ. Quadratus lumborum block nomenclature and anatomical considerations. Reg Anesth Pain Med. 2016;41:548–9. doi: 10.1097/AAP.0000000000000411. [DOI] [PubMed] [Google Scholar]
- 16.Elsharkawy H, El-Boghdadly K, Barrington M. Quadratus lumborum block: Anatomical concepts, mechanisms, and techniques. Anesthesiology. 2019;130:322–35. doi: 10.1097/ALN.0000000000002524. [DOI] [PubMed] [Google Scholar]
- 17.Elsharkawy H, El-Boghdadly K, Kolli S, Esa WAS, DeGrande S, Soliman LM, et al. Injectate spread following anterior subcostal and posterior approaches to the quadratus lumborum block: A comparative cadaveric study. Eur J Anaesthesiol. 2017;34:587–95. doi: 10.1097/EJA.0000000000000680. [DOI] [PubMed] [Google Scholar]
- 18.Ishio J, Komasawa N, Kido H. Evaluation of ultrasound-guided posterior quadratus lumborum block for postoperative analgesia after laparoscopic gynecological surgery. J Clin Anesth. 2017;41:1–4. doi: 10.1016/j.jclinane.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 19.Kang W, Lu D, Yang X, Zhou Z, Chen X, Chen K, et al. Postoperative analgesic effects of various quadratus lumborum block approaches following caesarean section: A randomised controlled trial. J Pain Res. 2019;12:2305–12. doi: 10.2147/JPR.S202772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choi JB, Kang K, Song MK, Seok S, Kim YH, Kim JE. Pain characteristics after total laparoscopic hysterectomy. Int J Med Sci. 2016;13:562–8. doi: 10.7150/ijms.15875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Niiyama Y, Matsuoka N, Sugimoto R, Yamakage M. Efficacy of intravenous patient-controlled analgesia (IV-PCA) using fentanyl compared with IV-PCA using morphine after abdominal surgery: A prospective randomized study. J Anesth Clin Res. 2016;7:598. [Google Scholar]
- 22.Ueshima H, Hiroshi O. Incidence of lower-extremity muscle weakness after quadratus lumborum block. J Clin Anesth. 2018;44:104. doi: 10.1016/j.jclinane.2017.11.020. [DOI] [PubMed] [Google Scholar]
- 23.Stuart GM, Ryan HC, Iqbal U, Olabisi IO, Hurd B. Transmuscular quadratus lumborum block reduces length of stay in patients receiving total hip arthroplasty? Anesth Pain Med. 2018;8:e80233. doi: 10.5812/aapm.80233. doi: 10.5812/aapm. 80233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akerman M, Pejcic N, Velickovic I. A review of the quadratus lumborum block and ERAS. Front Med (Lausanne) 2018;5:44. doi: 10.3389/fmed.2018.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hudcova J, McNicol E, Quah C, Lau J, Carr DB. Patient controlled opioid analgesia versus conventional opioid analgesia for postoperative pain. Cochrane Database Syst Rev. 2006;4:CD003348. doi: 10.1002/14651858.CD003348.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Albrecht E, Chin KJ. Advances in regional anaesthesia and acute pain management: A narrative review. Anaesthesia. 2020;75:e101–10. doi: 10.1111/anae.14868. [DOI] [PubMed] [Google Scholar]