Abstract
Irritability is common in Attention-Deficit Hyperactivity Disorder (ADHD), but little is known about whether irritability predicts the course of ADHD symptoms over time. Adolescence is a dynamic period of emotional development as well as shifts in ADHD symptoms; an important goal is to identify youth at risk of increasing or persisting symptoms. We examined irritability as a longitudinal predictor of change in adolescents’ ADHD symptoms, as well as how this link may differ in females versus males. The sample included 108 youth (72 males) age 12–16 years (M = 14.21 years, SD = 1.44 years), 62 of whom met criteria for ADHD. Approximately 18 months later, 80 participants (48 males) were followed up at Time 2. A dimensional approach was used to examine changes over time in parent-reported inattentive and hyperactive/impulsive symptoms. Longitudinal path analysis revealed that irritability at Time 1 predicted higher relative hyperactive/impulsive symptoms at Time 2 after controlling for age and longitudinal stability in all variables. A multiple-group analysis examining moderation by sex/gender revealed that this association was significant only for females. These results suggest that irritability may play a key role in the persistence and worsening of hyperactive/impulsive symptoms across adolescence for females, with potential implications for the diagnosis and treatment of females with ADHD.
Keywords: Attention-Deficit Hyperactivity Disorder (ADHD), sex, gender, irritability, emotion dysregulation, adolescence
Irritability Predicts Hyperactive/Impulsive Symptoms Across Adolescence for Females The hallmarks of Attention-Deficit Hyperactivity Disorder (ADHD) include symptoms of inattention, hyperactivity, and impulsivity, but these symptoms often show maturational decreases across adolescence (Monuteaux, Mick, Faraone & Biederman, 2010), especially in the hyperactive/impulsive dimension (Biederman, Mick & Faraone, 2000). However, for many youth these symptoms persist (Lee, Lahey, Owens & Hinshaw, 2008; Owens, Hinshaw, Lee & Lahey, 2009), with 40% of young adults still meeting full criteria for ADHD and as many as 90% continuing to show functional impacts (Biederman et al., 2012). ADHD is the most common neurodevelopmental disorder, affecting approximately 5% of U.S. youth and 2.5% of adults (APA, 2013), and is linked with a host of negative long term outcomes, including low academic success, relationship difficulties, vocational impairments, and higher substance use and risk of early death (Breslau, Miller, Chung & Schweitzer, 2011; Barkley & Fischer, 2010; Dalsgaard, Ostergaard, Leckman, Mortensen & Pedersen, 2015; Harty, Gnagy, Pelham, & Molina, 2017). Thus, it is important to identify longitudinal predictors of ADHD symptom trajectories across adolescence.
The heterogeneity of ADHD makes this task difficult. One aspect of heterogeneity is the emotional dysregulation that many but not all individuals with ADHD experience (Faraone et al., 2019). Irritability, a specific aspect of emotion dysregulation, is defined as excessive negative emotional reactivity, including strong anger responses or outbursts, or grumpy mood (Brotman, Kircanski & Leibenluft, 2017; Copeland, Brotman & Costello, 2015). Irritability can be common in individuals with ADHD (Stringaris, Cohen, Pine & Leibenluft, 2009), with estimates ranging from 25% to more than 70% of individuals with ADHD also displaying irritability, even in the absence of mood disorder (Geller et al., 2002; Shaw, Stringaris, Nigg, & Leibenluft, 2014). Importantly, even relatively low levels of irritability predict negative outcomes over time (Copeland et al., 2015). It is not clear how irritability affects the course of ADHD symptoms. It would be clinically relevant, if even modest levels of irritability similarly predict the persistence or worsening of ADHD symptoms, to be able to identify and intervene early with youths showing this constellation of symptoms. In the current study, we examined irritability as a predictor of change in adolescents’ ADHD symptoms over time, with the potential for moderation by gender.
Irritability in ADHD
Irritability by itself predicts long-term risks, including, at the most extreme, higher risk for suicidality (Pickles et al., 2010), but irritability is also overrepresented in youth with ADHD pointing to enmeshment of these conditions. The combination of irritability and ADHD symptoms is associated with particularly poor outcomes, including serious social problems, low global functioning, higher persistence of ADHD symptoms, and suicidal behaviors (Biederman et al., 2012; Galera et al., 2020). Thus, understanding this overlap and identifying early markers has clear importance for disrupting this risky and costly trajectory. Current perspectives highlight multiple factors that are likely at play (Shaw et al., 2014). Developmental studies have pointed to dimensions of temperament – early-emerging and biologically based characteristics of reactivity and regulation – that predict long-term risk for externalizing disorders and ADHD (Eisenberg et al., 2001; Goldsmith, Lemery, & Essex, 2004). For example, Gagne & Goldsmith (2011) documented a genetic influence on the overlap between anger proneness and inhibitory control from 12–36 months, and it may be the persistence of this genetic pathway that is observed later in childhood when ADHD diagnoses are acquired. Importantly, this study also found significant influence by environmental factors, and research has highlighted parenting behaviors and family dynamics that interact with temperament to maintain or exacerbate the co-occurring symptoms of emotion dysregulation, irritability, and ADHD (Fenesy, Teh, & Lee, 2019; Miller, Degnan, Hane, Fox, & Chronis-Tuscano, 2019; Musser et al., 2018). Other work has pointed to shared brain regions that are implicated in emotion regulation and also impacted in ADHD, such as emotion and attention circuits (Shaw et al., 2014; Ochsner, Silvers, & Buhle, 2012), and broad emotion dysregulation, perhaps temperamental in origin, observed in a significant subgroup of ADHD youth (Faraone et al., 2019; Graziano & Garcia, 2016; Karalunas, Gustafsson, Fair, Musser & Nigg, 2019; Nigg et al., 2020).
Irritable youths with ADHD also have more comorbid disorders – or are more likely to acquire them later on – than those with ADHD alone (Ambrosini, Bennett & Elia, 2013; Karalunas et al., 2019). It has been difficult to parse this overlap among ADHD, irritability, and comorbid conditions such as mood disorders and anxiety in order to understand how these factors interact over development. Only a few investigations have examined irritability as a predictor of ADHD symptoms or diagnoses measured longitudinally, and results have been mixed. For example, Leibenluft, Cohen, Gorrindo, Brook, and Pine (2006) showed that chronic irritability in early adolescence predicted ADHD diagnosis two years later, but also predicted later anxiety, depression, mania, and oppositional defiant disorder (ODD). Other studies have not found irritability to predict ADHD longitudinally (Dougherty et al., 2015; Stringaris et al., 2009; Vidal-Ribas, Brotman, Valdivieso, Leibenluft & Stringaris, 2016), but irritability did predict other diagnoses longitudinally, especially anxiety and depressive disorders. The data in the current report come from a larger longitudinal study that aimed to track the development of impulsivity in a low-comorbidity sample, allowing the examination of irritability in the absence of mood disorders and anxiety.
Longitudinal studies have generally not examined the developmental interplay between irritability and the separate subtypes or presentations of ADHD. Elevations in irritability have been more often found in the combined presentation of ADHD than in the inattentive-only presentation (Maedgen & Carlson, 2000; Mayes et al., 2019), pointing to a potential specific link with the hyperactivity and impulsivity components of ADHD. The reasons for this specificity are not yet well explored, but could reflect a shared neurobiology, as irritability is hypothesized to be associated with several neurobehavioral differences that more strongly overlap with the hyperactive/impulsive dimension of ADHD, such as greater sensitivity to reward, learning deficits for reward and punishment contingencies, and deficient inhibitory control (Brotman et al., 2017). On the other hand, other work has not shown that irritability is differentially related to ADHD presentation type (Bunford, Evans & Langberg, 2018), but this was a cross-sectional study. One recent study tracked trajectories of irritability and ADHD symptoms across childhood to predict adolescent outcomes (Galera et al., 2020). They found that children with high irritability and high ADHD were more likely to show elevated ADHD symptoms in both the inattentive and hyperactive/impulsive domains, while youths with high irritability but more mild ADHD symptoms were only more likely to show elevated hyperactive/impulsive symptoms in adolescence. The goal of the current study was to examine this question across adolescence. We used a sample of youth with the ADHD-combined presentation type, allowing within-person examination of both inattentive and hyperactive/impulsive symptom categories. Because of this overlap in the ADHD dimensions, an important component of the current analysis is the use of inattentive and hyperactive/impulsive symptoms as simultaneous dependent variables in order to assess specificity.
Adolescence as a Dynamic Developmental Phase
Adolescence is an important developmental phase to capture the emergence of new emotion-related symptoms. It is also a time of dynamic neurodevelopmental change, as systems responsible for regulating attention and behavior are rapidly developing (Casey, Getz & Galvan, 2008). Because of this expectation of fluctuations in irritability and ADHD symptoms over time, we designed our study to capture fluctuations in both directions, including clinical levels of symptoms that may decrease over time as well as initially normative levels that may increase over time. We used a dimensional approach using continuous symptom scores rather than bivariate diagnosis (Kraemer, 2007). We also included a range of youth, spanning those with typical development as well as those clinically diagnosed with ADHD. Indeed, in this study, some parents of typically developing adolescents reported that their adolescents developed ADHD symptoms over time; and some initially diagnosed with ADHD showed a decline in symptoms to normative levels.
Differences by Sex and/or Gender
It is increasingly recognized that the presentation and course of ADHD can differ by sex and/or gender (Gaub & Carlson, 1997; Gershon, 2002). Although “sex” is often used to refer to biological sex, in the current study we did not differentiate reported sex from gender, and so we use the phrase “sex and/or gender” to acknowledge that participants may have reported either of these classifications (additionally, classifications may not be distinct: Rutter, Caspi, & Moffit, 2003). Females are less frequently diagnosed with ADHD (Rucklidge, 2010), but females diagnosed with ADHD appear to have higher comorbidities than males (Ambrosini et al., 2003; Monuteaux et al., 2010) as well as high rates of negative long-term outcomes including risk for self-harm (Hinshaw et al., 2012; Owens, Zalecki, Gillette & Hinshaw, 2017), and mortality (Dalsgaard et al., 2015). In one study, the effects of having high combined ADHD and irritability symptoms in childhood on adolescent outcomes were stronger for females than males (Galera, 2020). Such sex/gender differences in irritability and emotional disorders frequently emerge in adolescence (Leibenluft et al., 2006; Rutter et al., 2003), making this an important developmental phase to examine (Humphreys et al., 2018).
One hypothesis is that females may be more likely than males to experience irritability, which may exacerbate ADHD symptoms. In both community and ADHD samples, female adolescents show higher and more stable levels of irritability (Caprara, Paciello, Gerbino & Cugini, 2007; Humphreys et al., 2018; Leibenluft et al., 2006) or emotional lability/reactivity (Charbonneau, Mezulis & Hyde, 2009; Sobanski et al., 2010) than adolescent males. For example, Riglin and colleagues (2017) identified different trajectories of irritability from middle childhood to adolescence, such that irritability increased for females but decreased for males. Overall, regardless of whether males and females differ in their levels of irritability, the strength of the link between irritability and pathological outcomes is of critical interest. Thus, our second goal is to examine sex and/or gender differences in how irritability and ADHD symptoms are associated across adolescence.
We had two key aims. First, we explored irritability as a predictor, over time, of symptoms of both inattention and hyperactivity/impulsivity. Prior work has demonstrated a stronger concurrent link between irritability and the combined presentation of ADHD (Mayes et al., 2019) and we therefore expected specific predictions from irritability to hyperactive/impulsive symptoms over time. Second, we examined whether sex and/or gender moderated longitudinal associations between irritability and ADHD symptoms. Because irritability is broadly associated with mental-health risk for female adolescents (Humphreys et al., 2018), we expect that irritability will be more strongly related to ADHD symptom development for females than males. To appropriately model the concurrent and longitudinal links among all constructs, including adjusting for stability in symptoms over time, we used path analysis to simultaneously examine multiple dependent variables.
Method
Participants
The data reported here came from a larger and ongoing longitudinal study of the neurodevelopmental trajectory of impulsivity across adolescence using a combination of multi-modal imaging (functional magnetic resonance imaging & diffusion tensor imaging), behavioral, clinical, and academic measures. Participants in this subsample included all 108 adolescents (72 males) aged 12–16 years (M = 14.21 years, SD = 1.44 years), along with their parent(s), who completed a Time 1 visit prior to July 1, 2015. At Time 1, 62 participants (47 males) met criteria for ADHD-Combined Presentation, and 46 participants (25 males) were typically developing. Approximately 18 months later (M = 17.05 months; SD = 2.98 months; range 12–26 months; 71% occurred within 15–21 months), parents completed rating scales again on youth behaviors and symptoms for 80 participants (48 males) at Time 2. Participant ethnicity was 21% Hispanic or Latino; 77% not Hispanic or Latino; and 2% unknown. Participant race was 71.3% White; 3.7% Black or African American; 1.9% Asian; 21.3% more than one race; and 1.8% unknown or other. Parents reported on their educational attainment and income for themselves and partners, if applicable. Most parents had completed a Bachelor’s degree or higher (60.4%); 33.9% reported some college or an Associate’s degree; 5.7% reported some K-12 education or a high school diploma. Income was reported as categorical values representing $25,000 USD increments for each parent, and categorical values were summed to create an estimate of household income. Household income was estimated to be more than $100,000 for 67% of participants, whereas 21.4% fell within $50,000–100,000, and 11.6% fell below $50,000.
Participants were recruited from psychiatric and neurodevelopmental disorders clinics, a university-based institute subject recruitment system, and the community via targeted advertising on flyers and social media. Informed written parental consent and child assent were obtained from all participants by trained research staff during their first encounter, prior to completing the psychological evaluation. Participants were compensated with $50 USD for their time in completing measures and rating scales at each wave. A university Institutional Review Board approved the study.
Two licensed psychologists in our team with extensive experience in diagnosing ADHD (JFD or JBS) evaluated initial phone screening data to determine eligibility for the study. The phone screen included a checklist of ADHD symptoms and severity, screen for academic or intellectual concerns, learning disability, mood, anxiety and other psychiatric disorders, history of psychiatric diagnosis and medication, presence of metal, physical diagnosis that might interfere with neuroimaging procedures or data interpretation, age and other demographic information. Participants approved as meeting the phone screen criteria for inclusion in the ADHD or typically developing group were invited to proceed to the next phase of the study, which included an in-depth in person psychological evaluation. Participants were then evaluated according to the Diagnostic and Statistical Manual of Mental Disorders – IV-TR or 5th Edition (DSM 5, which was used upon its publication) criteria for ADHD, typical development, and the presence of any other major psychiatric disorder using a diagnostic interview with all participants and one of their parents/caregivers (Diagnostic Interview Schedule for Child and Adolescents; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). The participant diagnostic interview was particularly assessed for presence of self-report internalizing disorders. This structured interview was administered by research coordinators with a bachelor’s degree, clinical psychology graduate students, or master’s level or higher trained clinical psychology staff. The interview assessed ADHD, Oppositional Defiant Disorder (ODD), conduct disorder (CD), phobia, Obsessive Compulsive Disorder (OCD), panic disorder, major depression, bipolar disorder, psychosis, anxiety disorders, substance use disorder, anti-social personality, and Post Traumatic Stress Disorder (PTSD). In accordance with the DSM, participants in the ADHD group needed to exhibit a persistent pattern of clinically significant level of hyperactive/impulsive symptoms and impairment in the home and school setting, exhibit the presence of significant ADHD symptoms before 12 years of age, and the symptoms could not be better explained by another mental disorder (e.g., mood, anxiety disorder). Parents reported on symptoms using the Conners-3 Parent Rating Scale (Conners, 2008). A licensed psychologist (JFD) reviewed all of the diagnostic information to determine final ADHD diagnosis (or typical development or presence of other disorder) based on parent responses to the diagnostic interview, where ADHD-Combined Presentation is indicated by 6 or more current inattentive and hyperactive/impulsive symptoms, and T-scores above 65 on DSM IV TR or DSM-5 Predominantly Inattentive and Predominantly Hyperactive/Impulsive Presentation from the Conners’ parent rating scale. Conners-3 Teacher Rating Scales further informed diagnosis if there were contradictions between interview and parent rating scale data. Attempts were made to collect teacher ratings from three teachers for each participant. However, teachers were not always responsive to participation, particularly for the older adolescents attending high school, and it was not always known whether teachers’ ratings were based on participant behavior in medicated versus unmedicated conditions. Thus, teacher ratings were not a primary source of diagnostic determination. In complex cases (i.e., disagreement between parent and teacher Conners’ ratings and the clinical interview), further follow-up interviews were conducted by JFD, and JFD and JBS were both required to review all diagnostic information to make a final expert diagnosis determination.
Inclusion criteria included IQ ≥ 80 and age between 12 – 28, but age 18 at T2 was the cut-off for the current analyses as we examined only minors whose parents were able to use the Conners-3 Report form at both time points. Additional inclusion criteria for the ADHD group included meeting DSM-IV-TR or 5 criteria for ADHD, Combined Presentation or Hyperactive/Impulsive Presentation. However, all participants in this study met criteria for the Combined Presentation and none for the Hyperactive/Impulsive Presentation. Exclusion criteria included an IQ score < 80, a mathematics or reading learning disability (indicated by scores ≤ 80 on the following subtests from the Weschler Individual Achievement Test (2009): Reading Comprehension, Word Reading, Math Problem Solving, Numerical Operations, and Math Fluency; see Fletcher & Miciak, 2019), history of head trauma, neurological disorder or major medical problem, psychoactive medication besides ADHD medications (i.e., stimulant or atomoxetine), and contraindications for neuroimaging (which was a mandatory aspect of the larger study). Diagnoses of conduct disorder, oppositional defiant disorder, phobia, and ADHD were allowed but the presence of any other DSM-IV-TR or 5 Axis I diagnosis was exclusionary.
Typically developing youth were recruited and assessed using the same diagnostic interview and rating scales as the ADHD group as described above, with the inclusion criterion of a score < 60 on the parent Conners’ 3 ADHD, DSM IV TR or DSM-5 Inattentive and Hyperactive/Impulsive symptoms scales.
Measure
Conners’ Rating Scales - 3 (Conners, 2008), Long Form.
These parent- and self-report rating scales ask about the frequency of behaviors on a scale from 0 (never, seldom) to 3 (very often). The current study used the two DSM-oriented ADHD subscales from the parent-report. The inattentive ADHD symptom scale contained 10 items and showed good internal consistency (T1 α = .97, T2 α = .96). The hyperactive/impulsive ADHD symptom scale contained 11 items and showed good internal consistency (T1 α = .95, Τ2 α = .94). To capture developmental and gender differences, the raw scores were used because normed T-scores obscure these differences. From the parent-report form we created an irritability index containing 5 items that were not included in the above scales: “Loses temper,” “Is angry and resentful,” “Is irritable and easily annoyed by others,” “Temper outbursts,” and “Becomes irritable when anxious.” This subscale showed good internal consistency (T1 α = .93, T2 α = .90). These items were selected based on their similarity in content with the Affective Reactivity Index (Stringaris et al., 2012). Within the larger study, the ARI was added to later years of data collection, and among participants who completed both measures, the irritability indices were highly correlated (r = .96).
From the self-report form, we used the anxiety and depression screener scales at Time 2 as covariates in a post-hoc analysis. These scales contain four items each. Internal consistency was α = .72 for depression; α = .78 for anxiety.
Data Analyses
Hypotheses were tested using a series of path analyses in MPlus Version 7.3, allowing all Time 2 variables to serve as simultaneous dependent variables and explicitly modeling any covariances among variables within time. Fit of each model to the data was evaluated, and we focused on Chi-Square values and the Akaike Information Criterion (AIC) because they facilitate model comparisons; in both cases smaller values indicate better fit. Models that rely on samples less than 200 and have low degrees of freedom have been shown to result in exaggerated estimates of poor fit with standard statistics such as RMSEA (Kenny, Kaniskan, & McCoach, 2015), but we do report them here for transparency. We used a nested model fitting approach to understand whether the inclusion of irritability better explained the patterns present in the data. We first fit a model that simply allowed for stability in all three constructs (inattentive symptoms, hyperactive/impulsive symptoms, and irritability) over time as well as covariances within time. We then compared this to a model that allowed time-lagged predictive paths from irritability to both ADHD symptom domains and noted change in fit.
To examine sex and/or gender differences, we tested structural model invariance using multiple-group analysis. This approach simultaneously fits the model to males and females, and our first model allowed all parameters to be freely estimated (i.e., values could be different for males and females). Sex and/or gender differences were tested using nested models which constrain paths of interest to be equal across males and females. If this results in degraded model fit, it can be concluded that those parameters differ significantly between males and females, equivalent to an interaction effect.
In all models, Time 1 variables were mean-centered prior to entry and age at Time 1 was included as a covariate. Regression diagnostics in SPSS were examined and confirmed that the residuals of the dependent variables were normally distributed, an assumption of path analysis. To further address any non-normality in the data, we utilized bootstrapping with 500 draws with resampling. For ease of interpretation, figures depict standardized estimates.
We examined correlates of attrition and found that participants who did not return for Time 2 (n=28) did not differ from those who did return in terms of age or irritability reported (t values < 1.15; all p > .25) or in terms of family income (t(101) = 1.82, p = .07; 5 parents did not report income at T1). Non-returners had significantly higher inattentive (t(106) = 2.49, p = .01) and hyperactive/impulsive symptoms (t(106) = 2.00, p = .05) and were more likely to be male (t(106) = −2.54, p = .01), although the sex/gender ratio was similar at each time point (67% and 60% males at T1 and T2, respectively). To account for missing data, we used full information maximum likelihood (FIML) estimation, which is the least biased approach to handling missingness, even when missing is not at random (Widaman, 2006). All primary analyses were thus conducted using the full sample (n = 108). The elapsed time between Time 1 and Time 2 was examined as a covariate but did not substantially impact results (see supplementary material).
Results
Descriptive Statistics
Descriptive statistics and sex differences are shown in Table 1. At both time points, parents rated males higher than females on inattentive and hyperactive symptoms. Irritability was not significantly different by gender at either time point. Longitudinally, among participants with complete data at both time points, parent-reported symptoms decreased (inattentive t(79) = 2.89, p = .005; hyperactive/impulsive t(79) = 4.49, p < .001) and irritability decreased with marginal significance (t(79) = 1.77, p = .08). Repeated measures ANOVAS, with sex/gender as a between subjects factor, showed that there were not sex/gender differences in these changes (sex*time interaction terms F(1,78) = 0.85, p = .36 and F(1,78) = 2.70, p = .10).
Table 1.
Descriptive Statistics for Study Variables
| Full Sample | Males | Females | Gender Difference | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | N | Mean | SD | t(df), p | |
| Time 1 | ||||||||||
| Age | 108 | 14.21 | 1.44 | 72 | 14.26 | 1.50 | 36 | 14.12 | 1.34 | .49(106), .63 |
| Inattentive Symptoms | 108 | 14.56 | 10.49 | 72 | 16.61 | 10.06 | 36 | 10.47 | 10.27 | 2.97(106), .004 |
| Hyperactive/Impulsive Symptoms | 108 | 11.47 | 9.68 | 72 | 13.57 | 9.94 | 36 | 7.28 | 7.68 | 3.33(106), .001 |
| Irritability | 108 | 4.59 | 4.27 | 72 | 5.03 | 4.19 | 36 | 3.72 | 4.35 | 1.51(106), .14 |
| Time 2 | ||||||||||
| Age | 80 | 15.61 | 1.48 | 48 | 15.69 | 1.55 | 32 | 15.49 | 1.39 | .56(78), .58 |
| Inattentive Symptoms | 80 | 11.63 | 9.42 | 48 | 13.35 | 9.70 | 32 | 9.03 | 8.48 | 2.051(78), .044 |
| Hyperactive/Impulsive Symptoms | 80 | 7.53 | 7.92 | 48 | 8.98 | 8.27 | 32 | 5.34 | 6.93 | 2.052(78), .044 |
| Irritability | 80 | 3.80 | 3.85 | 48 | 4.27 | 3.77 | 32 | 3.094 | 3.92 | 1.35(78), .18 |
Note. All measures are parent-reported. Inattentive, hyperactive/impulsive, and irritability symptoms all reported on the Conners 3 Rating Scale. Age reported in years.
Path Analyses
Stability Model.
This path analysis allowed stability paths for each construct over time (e.g., T1 irritability -> T2 irritability), covariances between constructs within time (e.g., r (T1 irritability with T1 inattentive), and T1 age as a covariate. Fit statistics were χ2(6) = 19.89, p = .003; RMSEA = .15 [.08–.22], p = .01; CFI = .96; TLI = .91; and AIC = 4237.28. Variables showed strong, significant stability over time and significant covariances within time. Age at T1 showed a small, negative association with inattentive symptoms at T2 (β = −.14, p = .01).
Irritability Prediction Model.
This path analysis added two paths from T1 irritability to T2 inattentive symptoms and T2 hyperactive/impulsive symptoms. Adding these paths significantly improved model fit (Δχ2 (Δdf = 2)= 9.40, p < .01; AIC = 4231.89). However, the path predicting T2 inattentive symptoms from T1 irritability was not significant (Unstd. B = 0.09, p = .51, 95% CI −0.18–0.36; β = .04). Removing this path produced a smaller AIC (4230.44) and did not significantly decrease model fit (Δχ2 (Δdf = 1)= 0.55, p =.46), so this more parsimonious model was retained as the final model. Final fit statistics were χ2(5) = 11.04, p = .05; RMSEA = .11 [.00–.19], p = .12; CFI = .98; TLI = .95.
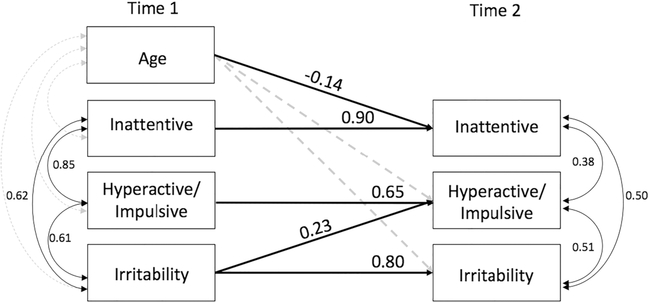
Figure 1 shows the final path analysis for parent-reported variables for the full sample. Irritability at T1 predicted higher relative levels of hyperactivity/impulsivity at T2 (Unstd. B = 0.41, p = .03; 95% CI 0.03–0.79; β = .23).
Figure 1.
Full sample: Longitudinal links between irritability and ADHD symptoms.
Standardized estimates shown. All depicted values are significant at p < .05; non-significant paths retained in the model are depicted by a grey dashed line.
Cross-Lagged Model.
A cross-lagged analysis was also explored, allowing inattentive and hyperactive/impulsive symptoms at T1 to predict irritability at T2. These paths were not significant (B = 0.01, β = .04, p = .78; and B = −0.03, β = −.08, p = .53, respectively) and model fit was worse for this model than the final model (AIC = 4235.36, CFI = .98, TLI = .84, RMSEA = .19 [.09–.32], p = .02, χ2(2) = 9.97, p = .01) so these paths were removed.
Sex and/or Gender Differences.
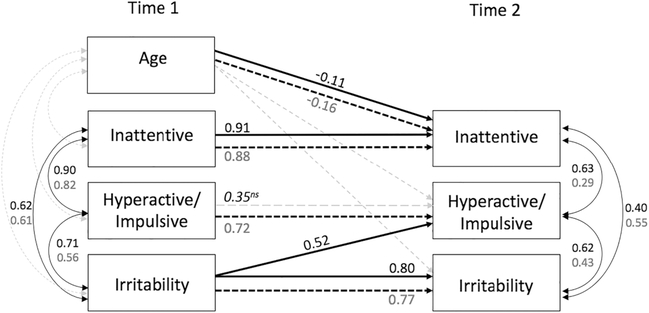
Figure 2 shows the results of the multiple-group analysis, allowing all parameter estimates to differ by gender. Fit statistics were χ2(10) = 23.31, p = .01; RMSEA = .16 [.07–.24], p = .02; CFI = .96; TLI = .89; and AIC = 4234.29. For females, the stability path from T1 to T2 hyperactivity/impulsivity became non-significant (p = .12) due to the significant amount of variance predicted by T1 irritability. T1 irritability predicted higher relative hyperactivity/impulsivity for females (Unstd. B = 0.83, p = .02; 95% CI 0.12–1.54; β = .52) but not for males (Unstd. B = 0.26, p = .27; 95% CI −0.20–0.73; β = .14). Fixing this path to be equal across males and females resulted in significantly decreased model fit (Δχ2 (Δdf = 1)= 4.39, p =.04; AIC = 4236.69), indicating that, equivalent to an interaction effect, these path estimates differ significantly between males and females. The effect size for females for the regression of T2 hyperactivity/impulsivity on T1 irritability means that every 1 point higher on the irritability scale predicted 0.83 points higher on the hyperactive/impulsive symptom scale at Time 2.
Figure 2.
Gender effects: Multiple group analysis of longitudinal links between irritability and ADHD symptoms.
Effects for females depicted by solid black lines, black font, and top values. Effects for males depicted by dashed black lines, grey font, and bottom values. Standardized estimates shown. All depicted values are significant at p < .05 unless noted; non-significant paths retained in the model are depicted by a grey dashed line.
The stability path between hyperactive/impulsive symptoms at Time 1 and Time 2 was significant for females (B = .65, β = .74, p < .001) in the absence of the predictive path from Time 1 irritability.
ns non-significant
Post hoc Examination of Anxiety and Depression.
While clinical diagnoses of anxiety or depression were exclusionary at Time 1, we performed a post-hoc analysis to explore whether the development of new anxiety or depression were impacting these findings. Youth self-reports on the Conners’ Rating Scale – 3 anxiety and depression screener scales (4 items each) at Time 2 were included as covariates in the final models with all Time 2 variables and with each other (For females, Manxiety = 3.85, SD = 2.82; Mdepression = 2.62, SD = 2.61; For males, Manxiety = 3.68, SD = 2.34; Mdepression = 2.10, SD = 1.99). Results did not differ meaningfully, and all betas changed by 0.02 or less, except that the prediction from Time 1 irritability to Time 2 hyperactive/impulsive symptoms for females was slightly reduced (B = 0.75; β = .47; p = .03). Model fit statistics were χ2(26) = 39.40, p = .04; RMSEA = .10 [.02–.16], p = .12; CFI = .97; TLI = .92; AIC = 4765.89; and not significantly different from the primary model (Δχ2 (Δdf = 16)= 16.09, p =.45). This suggests that while anxiety and depression appear to become involved with this constellation of factors, the predictive link between earlier irritability and the development of hyperactive/impulsive symptoms was not obscured by the development of anxiety or depression symptoms.
Discussion
This study examined the role that irritability may play in the course of ADHD symptoms over adolescence. Adolescents with ADHD and adolescents following typical development both exhibit changes in emotionality, attention, hyperactivity, and impulsivity, making this an important developmental phase for understanding how these components interact. Given noted sex and/or gender differences in ADHD, we examined whether sex and/or gender moderated the link between irritability and future ADHD symptoms. We found that higher levels of irritability at baseline predicted higher relative hyperactive/impulsive symptoms 18 months later, but this link was significant only for females.
This study extended previous findings of links between irritability and the hyperactive/impulsive dimension of ADHD symptoms (observed in the combined presentation type; Maedgen & Carlson, 2000; Mayes et al., 2019) to show that this association is predictive over time. Irritability is hypothesized to be associated with several neurobehavioral differences that more strongly overlap with the hyperactive/impulsive dimension of ADHD, such as greater sensitivity to reward, learning deficits for reward and punishment contingencies, and deficient inhibitory control (Brotman et al., 2017). This may point to a potential shared neurophysiological source of both irritability and hyperactivity/impulsivity. The current study adds an important time-ordered consideration to this conceptualization because it indicates that irritability plays an exacerbating role over time. Importantly, irritability was only a significant longitudinal predictor for females.
This is the first report that we are aware of that found differences by sex and/or gender in the longitudinal link between irritability and hyperactive/impulsive symptoms. The examination of sex and/or gender as a moderator of the link was important because males and females did not differ in their mean levels of irritability at either time point; rather, it was the strength of the association between earlier irritability and later ADHD symptoms that was significantly stronger for females. For every 1 point increase on the irritability scale at Time 1 (e.g., endorsing an item as “pretty much true” instead of “just a little true”), hyperactive/impulsive symptoms were expected to be 0.83 points higher at Time 2 for females. Thus, for example, a 2-point increase in irritability predicts more than 1.5 points higher on hyperactive/impulsive symptoms which could be clinically significant given that this raw score increase typically translates to an increase of at least 3 in T-scores, depending on the age norming.
The reason for this association is unknown. Possibly, female adolescents with higher levels of irritability have a more difficult time regulating negative emotions, resulting in more frequent expressions of impulsive, unregulated behaviors and emotions. For example, Bunford and colleagues (2018) found that female and male adolescents with ADHD generally shared similar patterns of emotional dysregulation compared to a community sample, but females with ADHD were more likely to report poor strategies for dealing with their emotions when upset. In contrast, males with ADHD were more likely to lack clarity about their experienced emotions compared to a community samples. For females, these poor regulatory strategies may be compounded by high social expectations: In Western cultures, irritability and poor emotion regulation are less tolerated in females than males, and this is reflected in peer and parent perceptions of behavior (Root & Denham, 2010; Sobanski et al., 2010). Low acceptance for negative emotions in females paired with poor regulatory abilities could result in more frequent outbursts of impulsive behavior. This scenario could also impact parent ratings: if irritability and hyperactive/impulsive behavior are more salient to parents of females than to parents of males, then they would give higher ratings on these items (Rutter et al., 2003).
Future work should replicate this link and examine the mechanisms of this irritability-impulsivity link for female adolescents. For example, emotion regulation abilities may play a mediating role. It will also be important to explore the kinds of impulsive and hyperactive behaviors that are displayed by irritable adolescents, and females specifically. It is possible that these behaviors may be more emotional in nature (e.g., emotional impulsivity and hyperactive or fidgeting behaviors that are attempts at self-soothing), but this will require more nuanced measures of ADHD symptomatology.
More nuanced and multi-method measures of ADHD symptoms are also needed to further probe the potential specificity of the association between irritability and hyperactive/impulsive symptoms. In the current study, inattentive symptoms were highly stable over time (β = .87 and .91 for males and females, respectively, in a stability-only model), which statistically leaves little variance to be predicted. Hyperactive/impulsive symptoms were not as highly stable over time (β = .75 and .74 for males and females, respectively, in a stability-only model), allowing more variability to be predicted by irritability. However, this issue does not explain the sex and/or gender difference in the prediction by irritability given the nearly identical degree of stability between males and females. For females, the inclusion of irritability as a predictor of hyperactive/impulsive symptoms reduced the estimate of stability to non-significance, suggesting that the presence of irritability partly drives the continuation of hyperactive/impulsive symptoms.
An important aspect of this study is that participants were excluded for several comorbid disorders (other than ODD, CD, and phobia) at Time 1, but ADHD is commonly comorbid with other conditions such as anxiety and depression (Vidal-Ribas et al., 2016). We did not examine whether participants met criteria for new diagnoses at Time 2 (this information is being examined in later years of this ongoing study), but the inclusion of self-reported anxiety and depression symptoms did not substantially change the main findings of the current study. Disentangling the overlap between irritability, ADHD, and co-occurring conditions is an important aim of future work. There is evidence that, compared to males, females with ADHD show a broader range of outcomes in adolescence and adulthood (Hinshaw et al., 2012; Owens et al., 2017). Indeed, many of the more negative outcomes for females seem to indicate an increasing enmeshment of ADHD with mood disorders (Humphreys et al., 2018; Riglin et al., 2017), and particular risk for anxiety and depression (Eyre et al., 2019; Stringaris et al., 2009). The exclusion of anxiety and mood disorders in the current study limits our ability to extend these findings to youth experiencing these comorbidities with ADHD. However, the current results suggest that the exacerbation of ADHD symptoms by earlier irritability is not attributable to anxiety or mood disorders and warrants consideration even in the absence of these additional diagnoses. Further, these long term risks for females with ADHD should draw our attention to gender differences in this disorder, even if females have less severe ADHD symptoms than males, as they did in the current study.
This analysis showed that the inclusion of irritability measures resulted in models that better explained the data, as well supported the hypothesis that links between irritability and ADHD vary over time by gender. However, this study also had several limitations. These models and hypotheses now should be tested in other, large samples with greater diversity in race, ethnicity, and socioeconomic status, as household income was high in the current sample. It would be important to examine whether these effects persist or change in contexts of greater economic or environmental stress. Future work should also examine these questions in both ADHD presentations, as the current study excluded the inattentive-only presentation. In particular, developmental changes in the prevalence of the presentations have been noted, with some work showing that the combined presentation becomes less common across adolescence (Willcutt, 2012; Ramtekkar, Reiersen, Todorov, & Todd, 2010). In this case, it is possible that our sample of predominately combined presentation represents a more extreme group of adolescents who persisted in hyperactive/impulsive symptoms. However, some studies also show rates of the combined presentation that are equivalent to, or greater than, rates of the inattentive presentation in adolescence and adulthood (Neuman et al., 2005; Wilens et al., 2009). Importantly, the current study utilized a dimensional approach, and irritability and hyperactive/impulsive symptoms were significantly correlated (r range .37–.54) even in the typically-developing adolescents, suggesting that this effect is not limited to severe cases of ADHD. Whether irritability would predict ADHD persistence for the inattentive-only presentation is an important question for future work.
The retention rate between Time 1 and Time 2, at 74%, was not as high as we would have hoped, and reflects a gap in funding as well as typical difficulties engaging adolescents in an ongoing, time-intensive study. However, we used a statistical estimating approach that in effect retained the whole sample, and is robust even the case of 33% missing data (Widaman, 2006). Non-returners had elevated ADHD symptoms at Time 1, and we followed best practice for missing data by including these predictors of attrition in our model (Graham, 2009). However, the true impact of attrition in this study is unknown. Replication in larger samples is an important future aim. In particular, studies with large numbers of females with ADHD symptoms are needed to further examine questions of sex and/or gender differences in the course of ADHD.
Finally, this study relied on parent-reported measures of symptoms on a single questionnaire, and this shared method and shared rater variance may have impacted results. This methodological choice may have impacted the degree of stability in constructs over time, which in the case of inattentive symptoms is particularly high. As noted, this likely limited our ability to predict further variance in Time 2 inattentive symptoms. Multi-method designs should be applied in future work. The use of adolescent self-report for emotional domains such as irritability should also be considered, as with age, parents may become less likely to observe these behaviors. More nuanced indices of irritability should also be explored in future work because the scale used here resulted in relatively low mean irritability scores, and this is common in other measures such as the ARI (Tseng et al., 2019), which has a possible range of 12 but a cutoff score of >3 can indicate clinical significance. Thus, while the current results fit within the existing literature, the current results should be interpreted in light of this restricted range.
Together, the current results suggest that irritability may play an important role in the persistence and worsening of hyperactive/impulsive symptoms across adolescence for females. The potential clinical implications include a consideration of symptoms of irritability in adolescent females as a risk factor for steady or increasing patterns of hyperactive/impulsive symptoms, as well as the need for interventions that address irritability together with ADHD symptoms.
Supplementary Material
Acknowledgments
This work was supported by grant numbers 2 R01 MH 091068 from the National Institutes of Mental Health (Schweitzer), U54 HD079125, the MIND Institute Intellectual and Developmental Disabilities Research Center award from the National Institutes of Child Health and Human Development, and T32HP30037 from the Health Resources and Services Administration (HRSA) through the Quality, Safety, and Comparative Effectiveness Research Training – Primary Care (QSCERT-PC) Program.
Footnotes
Ethical approval All procedures performed were in accordance with the ethical standards of the institutional research committee (protocol number 405204-65) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- Ambrosini PJ, Bennett DS, & Elia J (2013). Attention deficit hyperactivity disorder characteristics: II. Clinical correlates of irritable mood. Journal of Affective Disorders, 145(1), 70–76. doi: 10.1016/j.jad.2012.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Barkley RA, & Fischer M (2010). The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. Journal of the American Academy of Child & Adolescent Psychiatry, 49(5), 503–513. doi: 10.1097/00004583-201005000-00011 [DOI] [PubMed] [Google Scholar]
- Biederman J, Mick E, & Faraone SV (2000). Age-dependent decline of symptoms of attention deficit hyperactivity disorder: Impact of remission definition and symptom type. American Journal of Psychiatry, 157(5), 816–818. doi: 10.1176/appi.ajp.157.5.816 [DOI] [PubMed] [Google Scholar]
- Biederman J, Spencer TJ, Petty C, Hyder LL, O’Connor KB, Surman CB, & Faraone SV (2012). Longitudinal course of deficient emotional self-regulation CBCL profile in youth with ADHD: Prospective controlled study. Neuropsychiatric Disease and Treatment, 8, 267–276. doi: 10.2147/NDT.S29670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Miller E, Chung JWJ, & Schweitzer JB (2011). Childhood and adolescent onset psychiatric disorders, substance use, and failure to graduate high school on time. Journal of Psychiatric Research, 45(3), 295–301. doi: 10.1016/j.jpsychires.2010.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brotman MA, Kircanski K, & Leibenluft E (2017). Irritability in children and adolescents. Annual Review of Clinical Psychology, 13(1), 317–341. doi: 10.1146/annurev-clinpsy-032816-044941 [DOI] [PubMed] [Google Scholar]
- Bunford N, Evans SW, & Langberg JM (2018). Emotion dysregulation is associated with social impairment among young adolescents with ADHD. Journal of Attention Disorders, 22(1), 66–82. doi: 10.1177/1087054714527793 [DOI] [PubMed] [Google Scholar]
- Caprara GV, Paciello M, Gerbino M, & Cugini C (2007). Individual differences conducive to aggression and violence: Trajectories and correlates of irritability and hostile rumination through adolescence. Aggressive Behavior, 33(4), 359–374. doi: 10.1002/ab.20192 [DOI] [PubMed] [Google Scholar]
- Casey B, Getz S, & Galvan A (2008). The adolescent brain. Developmental Review, 28(1), 62–77. doi: 10.1016/j.dr.2007.08.003.The [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charbonneau AM, Mezulis AH, & Hyde JS (2009). Stress and emotional reactivity as explanations for gender differences in adolescents’ depressive symptoms. Journal of Youth and Adolescence, 38(8), 1050–1058. doi: 10.1007/s10964-009-9398-8 [DOI] [PubMed] [Google Scholar]
- Conners KC (2008). Conners 3rd edition manual. New York: Multi-Health Systems, Inc. [Google Scholar]
- Copeland WE, Brotman MA, & Costello EJ (2015). Normative irritability in youth: Developmental findings from the Great Smoky Mountains Study. Journal of the American Academy of Child and Adolescent Psychiatry, 54(8), 635–642. doi: 10.1016/j.jaac.2015.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalsgaard S, Ostergaard SD, Leckman JF, Mortensen PB, & Pedersen MG (2015). Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: A nationwide cohort study. The Lancet, 385(9983), 2190–2196. doi: 10.1016/S0140-6736(14)61684-6 [DOI] [Google Scholar]
- Dougherty LR, Smith VC, Bufferd SJ, Kessel E, Carlson GA, & Klein DN (2015). Preschool irritability predicts child psychopathology, functional impairment, and service use at age nine. Journal of Child Psychology and Psychiatry and Allied Disciplines, 56(9), 999–1007. doi: 10.1111/jcpp.12403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL, Fabes RA, Shepard SA, Reiser M, … Guthrie IK (2001). The relations of regulation and emotionality to children’s externalizing and internalizing problem behavior. Child Development, 72(4), 1112–1134. doi: 10.1111/1467-8624.00337 [DOI] [PubMed] [Google Scholar]
- Eyre O, Riglin L, Leibenluft E, Stringaris A, Collishaw S, & Thapar A (2019). Irritability in ADHD: Association with later depression symptoms. European Child & Adolescent Psychiatry, 28(10), 1375–1384. doi: 10.1007/s00787-019-01303-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Rostain AL, Blader J, Busch B, Childress AC, Connor DF, & Newcorn JH (2019). Practitioner Review: Emotional dysregulation in attention-deficit/hyperactivity disorder – implications for clinical recognition and intervention. Journal of Child Psychology and Psychiatry and Allied Disciplines, 60(2), 133–150. doi: 10.1111/jcpp.12899 [DOI] [PubMed] [Google Scholar]
- Fenesy MC, Teh SE & Lee SS (2019). Negative parenting moderates the prospective association of ADHD symptoms and youth social problems. Journal of Abnormal Child Psychology, 47, 1583–1597. Doi: 10.1007/s10802-019-00542-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher JM, & Miciak J (2019). The identification of specific learning disabilities: A summary of research on best practices. Austin, TX: Texas Center for Learning Disabilities [Google Scholar]
- Gagne JR, & Goldsmith HH (2011). A longitudinal analysis of anger and inhibitory control in twins from 12 to 36 months of age. Developmental Science, 14(1), 112–124. doi: 10.1111/j.1467-7687.2010.00969.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galera C, Orri M, Vergunst F, Melchior M, Van der Waerden J, Bouvard MP, … Côté SM (2020). Developmental profiles of childhood attention-deficit/hyperactivity disorder and irritability: association with adolescent mental health, functional impairment, and suicidal outcomes. Journal of Child Psychology and Psychiatry and Allied Disciplines, 5. doi: 10.1111/jcpp.13270 [DOI] [PubMed] [Google Scholar]
- Gaub M, & Carlson CL (1997). Gender differences in ADHD: A meta-analysis and critical review. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 1036–1046. [DOI] [PubMed] [Google Scholar]
- Geller B, Zimerman B, Williams M, Delbello MP, Bolhofner K, Craney JL, … & Nickelsburg MJ (2002). DSM-IV mania symptoms in a prepubertal and early adolescent bipolar disorder phenotype compared to attention-deficit hyperactive and normal controls. Journal of Child and Adolescent Psychopharmacology, 12, 11–25. [DOI] [PubMed] [Google Scholar]
- Gershon J (2002). A meta-analytic review of gender differences in ADHD. Journal of Attention Disorders, 5, 143–154. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH, Lemery KS, & Essex MJ (2004). Temperament as a Liability Factor for Childhood Behavioral Disorders: The Concept of Liability. In Behavior genetics principles: Perspectives in development, personality, and psychopathology. (pp. 19–39). Washington, DC, US: American Psychological Association [Google Scholar]
- Graham JW (2009). Missing Data Analysis: Making It Work in the Real World. Annual Review of Psychology, 60(1), 549–576. doi: 10.1146/annurev.psych.58.110405.085530 [DOI] [PubMed] [Google Scholar]
- Graziano PA, & Garcia A (2016). Attention-deficit hyperactivity disorder and children’s emotion dysregulation: A meta-analysis. Clinical Psychology Review, 46, 106–123. doi: 10.1016/j.cpr.2016.04.011 [DOI] [PubMed] [Google Scholar]
- Harty SC, Gnagy EM, Pelham WE Jr., Molina BSG (2017). Anger-irritability as a mediator of attention deficit hyperactivity disorder risk for adolescent alcohol use and the contribution of coping skills. Journal of Child Psychology and Psychiatry, 58(5), 555–563. doi: 10.1111/jcpp.12668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado AJ, Schrodek E, & Swanson EN (2012). Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: Continuing impairment includes elevated risk for suicide attempts and self-injury. Journal of Consulting and Clinical Psychology, 80(6), 1041–1051. doi: 10.1037/a0029451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, Schouboe SNF, Kircanski K, Leibenluft E, Stringaris A, & Gotlib IH (2018). Irritability, externalizing, and internalizing psychopathology in adolescence: Cross-sectional and longitudinal associations and moderation by sex. Journal of Clinical Child and Adolescent Psychology, 1–9. doi: 10.1080/15374416.2018.1460847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karalunas SL, Gustafsson HC, Fair D, Musser ED, & Nigg JT (2019). Do we need an irritable subtype of ADHD? Replication and extension of a promising temperament profile approach to ADHD subtyping. Psychological Assessment, 31(2), 236–247. doi: 10.1037/pas0000664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA, Kaniskan B, & McCoach DB (2015). The performance of RMSEA in models with small degrees of freedom. Sociological Methods and Research, 44(3), 486–507. doi: 10.1177/0049124114543236 [DOI] [Google Scholar]
- Kraemer HC (2007), DSM categories and dimensions in clinical and research contexts. International Journal of Methods in Psychiatry Research, 16, S8–S15. doi: 10.1002/mpr.211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SS, Lahey BB, Owens EB, & Hinshaw SP (2008). Few preschool boys and girls with ADHD are well adjusted during adolescence. Journal of Abnormal Child Psychology, 36, 373–383. [DOI] [PubMed] [Google Scholar]
- Leibenluft E, Cohen P, Gorrindo T, Brook JS, & Pine DS (2006). Chronic versus episodic irritability in youth: A community-based, longitudinal study of clinical and diagnostic associations. Journal of Child and Adolescent Psychopharmacology, 16(4), 456–466. doi: 10.1089/cap.2006.16.456 [DOI] [PubMed] [Google Scholar]
- Maedgen JW, & Carlson CL (2000). Social functioning and emotional regulation in the attention deficit hyperactivity disorder subtypes. Journal of Clinical Child Psychology, 29(1), 30–42. doi: 10.1207/S15374424jccp2901 [DOI] [PubMed] [Google Scholar]
- Mayes SD, Calhoun SL, Waxmonsky JG, Kokotovich C, Baweja R, Lockridge R, & Bixler EO (2019). Demographic differences in disruptive mood dysregulation disorder symptoms in ADHD, autism, and general population samples. Journal of Attention Disorders, 23(8), 849–858. doi: 10.1177/1087054716664409 [DOI] [PubMed] [Google Scholar]
- Miller NV, Degnan KA, Hane AA, Fox NA, & Chronis-Tuscano A (2019). Infant temperament reactivity and early maternal caregiving: Independent and interactive links to later childhood attention-deficit/hyperactivity disorder symptoms. Journal of Child Psychology and Psychiatry, 60(1), 43–53. doi: 10.1111/jcpp.12934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monuteaux MC, Mick E, Faraone SV, & Biederman J (2010). The influence of sex on the course and psychiatric correlates of ADHD from childhood to adolescence: A longitudinal study. Journal of Child Psychology and Psychiatry and Allied Disciplines, 51(3), 233–241. Doi: 10.1111/j.1469-7610.2009.02152.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musser ED, Lugo Y, Ward AR, Tenenbaum RB, Morris S, Brijmohan N, & Martinez J (2018). Parent emotion expression and autonomic-linked emotion dysregulation in childhood ADHD. Journal of Psychopathology and Behavioral Assessment, 40(4), 593–605. doi: 10.1007/s10862-018-9685-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuman RJ, Sitdhiraksa N, Reich W, Ji THC, Joyner CA, Sun L-W, & Todd RD (2005). Estimation of Prevalence of DSM-IV and Latent Class-Defined ADHD Subtypes in a Population-Based Sample of Child and Adolescent Twins. Twin Research and Human Genetics, 8(4), 392–401. doi: 10.1375/twin.8.4.392 [DOI] [PubMed] [Google Scholar]
- Nigg JT, Karalunas SL, Gustafsson HC, Bhatt P, Ryabinin P, Mooney MA, … Wilmot B (2020). Evaluating chronic emotional dysregulation and irritability in relation to ADHD and depression genetic risk in children with ADHD. Journal of Child Psychology and Psychiatry and Allied Disciplines, 61(2), 205–214. doi: 10.1111/jcpp.13132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochsner KN, Silvers JA, & Buhle JT (2012). Functional imaging studies of emotion regulation: a synthetic review and evolving model of the cognitive control of emotion. Annals of the New York Academy of Sciences, 1251(1), E1–E24. doi: 10.1111/j.1749-6632.2012.06751.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens EB, Hinshaw SP, Lee SS, & Lahey BB (2009). Few girls with childhood attention-deficit/hyperactivity disorder show positive adjustment during adolescence. Journal of Clinical Child and Adolescent Psychology, 38(1), 132–143. doi: 10.1080/15374410802575313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens EB, Zalecki C, Gillette P, & Hinshaw SP (2017). Girls with childhood ADHD as adults: Cross-domain outcomes by diagnostic persistence. Journal of Consulting and Clinical Psychology, 85(7), 723–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickles A, Aglan A, Collishaw S, Messer J, Rutter M, & Maughan B (2010). Predictors of suicidality across the life span: The Isle of Wight study. Psychological Medicine, 40(9), 1453–1466. doi: 10.1017/S0033291709991905 [DOI] [PubMed] [Google Scholar]
- Psychological Corporation (2009). Wechsler Individual Achievement Test Manual; 3rd edition. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Riglin L, Eyre O, Cooper M, Collishaw S, Martin J, Langley K, … Thapar A (2017). Investigating the genetic underpinnings of early-life irritability. Translational Psychiatry, 7(9), e1241. doi: 10.1038/tp.2017.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramtekkar UP, Reiersen AM, Todorov AA, & Todd RD (2010). Sex and Age Differences in Attention-Deficit/Hyperactivity Disorder Symptoms and Diagnoses: Implications for DSM-V and ICD-11. Journal of the American Academy of Child & Adolescent Psychiatry, 49(3), 217–228.e3. doi: 10.1016/j.jaac.2009.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Root AK, & Denham SA (2010). The role of gender in the socialization of emotion: Key concepts and critical issues. New Directions for Child and Adolescent Development, 2010(128), 1–9. doi: 10.1002/cd.265 [DOI] [PubMed] [Google Scholar]
- Rucklidge JJ (2010). Gender Differences in Attention-Deficit/Hyperactivity Disorder. Psychiatric Clinics of North America, 33(2), 357–373. doi: 10.1016/j.psc.2010.01.006. [DOI] [PubMed] [Google Scholar]
- Rutter M, Caspi A, & Moffitt TE (2003). Using sex differences in psychopathology to study causal mechanisms: Unifying issues and research strategies. Journal of Child Psychology and Psychiatry and Allied Disciplines, 44(8), 1092–1115. doi: 10.1111/1469-7610.00194 [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, & Schwab-Stone ME (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry, 39(1), 28–38. doi: 10.1097/00004583-200001000-00014 [DOI] [PubMed] [Google Scholar]
- Shaw P, Stringaris A, Nigg J, & Leibenluft E (2014). Emotion dysregulation in attention deficit hyperactivity disorder. The American Journal of Psychiatry, 171(3), 276–293. doi: 10.1176/appi.ajp.2013.13070966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobanski E, Banaschewski T, Asherson P, Buitelaar J, Chen W, Franke B, … Faraone SV (2010). Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): Clinical correlates and familial prevalence. Journal of Child Psychology and Psychiatry and Allied Disciplines, 51(8), 915–923. doi: 10.1111/j.1469-7610.2010.02217.x [DOI] [PubMed] [Google Scholar]
- Stringaris A, Cohen P, Pine DS, & Leibenluft E (2009). Adult outcomes of youth irritability: A 20-year prospective community-based study. American Journal of Psychiatry, 166(9), 1048–1054. doi: 10.1176/appi.ajp.2009.08121849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris A, Goodman R, Ferdinando S, Razdan V, Muhrer E, Leibenluft E, & Brotman MA (2012). The Affective Reactivity Index: A concise irritability scale for clinical and research settings. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 53(11), 1109–1117. doi: 10.1111/j.1469-7610.2012.02561.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng WL, Deveney CM, Stoddard J, Kircanski K, Frackman AE, Yi JY, … Leibenluft E (2019). Brain mechanisms of attention orienting following frustration: Associations with irritability and age in youths. American Journal of Psychiatry, 176(1), 67–76. doi: 10.1176/appi.ajp.2018.18040491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidal-Ribas P, Brotman MA, Valdivieso I, Leibenluft E, & Stringaris A (2016). The status of irritability in psychiatry: A conceptual and quantitative review. Journal of the American Academy of Child and Adolescent Psychiatry, 55(7), 556–570. doi: 10.1016/j.jaac.2016.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widaman K (2006). Missing data: What to do with or without them. Monographs of the Society for Research in Child Development, 71(3), 42–64. doi: 10.1111/j.1540-5834.2006.00404.x [DOI] [Google Scholar]
- Wilens TE, Biederman J, Faraone SV, Martelon M, Westerberg D, & Spencer TJ (2009). Presenting ADHD symptoms, subtypes, and comorbid disorders in clinically referred adults with ADHD. The Journal of clinical psychiatry, 70(11), 1557–1562. doi: 10.4088/JCP.08m04785pur [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcutt EG (2012). The prevalence of DSM-IV Attention-Deficit/Hyperactivity Disorder: A meta-analytic review. Neurotherapeutics, 9(3), 490–499. doi: 10.1007/s13311-012-0135-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.