Abstract
Introduction
Emergency department (ED) attendances fell across the UK after the ‘lockdown’ introduced on 23rd March 2020 to limit the spread of coronavirus disease 2019 (COVID-19). We hypothesised that reductions would vary by patient age and disease type. We examined pre- and in-lockdown ED attendances for two COVID-19 unrelated diagnoses: one likely to be affected by lockdown measures (gastroenteritis), and one likely to be unaffected (appendicitis).
Methods
We conducted a retrospective cross-sectional study across two EDs in one London hospital Trust. We compared all adult and paediatric ED attendances, before (January 2020) and during lockdown (March/April 2020). Key patient demographics, method of arrival, and discharge location were compared. We used Systemised Nomenclature of Medicine codes to define attendances for gastroenteritis and appendicitis.
Results
ED attendances fell from 1129 per day before lockdown to 584 in lockdown, 51.7% of pre-lockdown rates. In-lockdown attendances were lowest for under-18s (16.0% of pre-lockdown). The proportion of patients admitted to hospital increased from 17.3% to 24.0%, and the proportion admitted to intensive care increased fourfold. Attendances for gastroenteritis fell from 511 to 103, 20.2% of pre-lockdown rates. Attendances for appendicitis also decreased, from 144 to 41, 28.5% of pre-lockdown rates.
Conclusion
ED attendances fell substantially following lockdown implementation. The biggest reduction was for under-18s. We observed reductions in attendances for gastroenteritis and appendicitis. This may reflect lower rates of infectious disease transmission, although the fall in appendicitis-related attendances suggests that behavioural factors were also important. Larger studies are urgently needed to understand changing patterns of ED use and access to emergency care during the coronavirus 2019 pandemic.
INTRODUCTION
The emergence of COVID-19 and subsequent ‘lockdown’ introduced by the British Government on 23rd March 20201 had a substantial impact on emergency department (ED) attendances. Total ED attendances in England in March 2020 fell by 29.4% year-on-year.2 The reasons for this change in ED activity are likely to be multifactorial. To reduce pressure on EDs, patients were instructed to seek advice from online resources and National Health Service (NHS) telephone services. The closure of schools and workplaces is likely to have led to a reduction in the spread of infectious diseases.2 Reductions in organised sports and recreational activity have previously been linked to reductions in physical injuries.3 It is suggested that reductions in children attending EDs reflect parents’ concerns about acquiring nosocomial COVID-19.4 Several authors have highlighted the potential for collateral damage from lockdowns, with patients deterred from seeking help for serious injuries and illnesses at risk of poorer outcomes.5,6
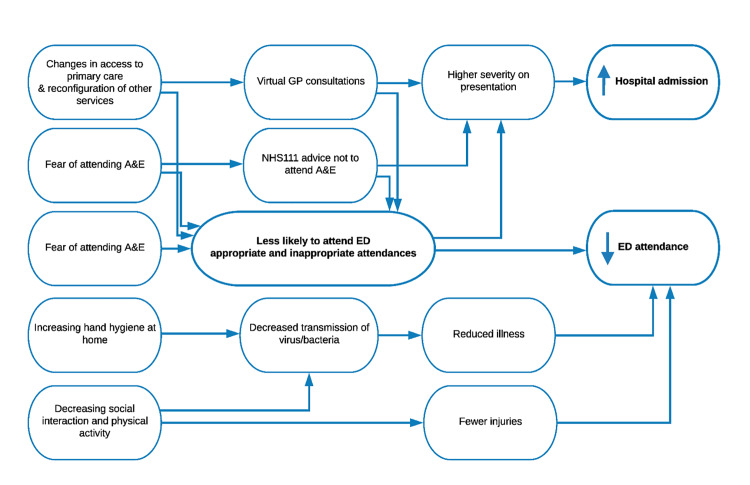
We hypothesised that the impact of the first nationwide lockdown on ED attendance would vary by patient demographics and clinical reason for attendance. We have proposed causal pathways leading to changes in ED attendances and hospital admissions. These are summarised in Figure 1. Using a snapshot of ED data, we examined the number of pre- and in-lockdown ED attendances for two COVID-19 unrelated diagnoses:
Figure 1.
Conceptual framework for changes in emergency department attendance associated with ‘lockdown’ for conditions unrelated to COVID-19.
ED, emergency department.
Gastroenteritis – an infectious disease which we would expect to be affected by lockdown measures.
Appendicitis – an acute disorder which we would expect to be largely unaffected by lockdown measures.
METHODS
Emergency department attendance information was provided by the NHS Trust data warehouse team. Information included patient information: age, gender, ethnicity, residential partial postcode, arrival mode at ED, destination at discharge and Systemised Nomenclature of Medicine Clinical Terms (SNOMED-CT)7 diagnostic codes. At the hospital Trust sites, diagnostic codes are entered by the treating ED clinician immediately after conducting a clinical assessment. The code is based on their clinical impression from history and examination, blood tests and, where applicable, specialist imaging investigations. Data was extracted from the ED part of the electronic health system (Cerner Corporation) by the Trust data management team and transferred as a table into a secure analysis environment.
We selected a four-week period (6th January 2020–2nd February 2020) as the pre COVID-19 phase and a four-week period (23nd March 2020–19th April 2020) as the in-lockdown period. We included all ED attendances (children and adults). We compared ED attendances based on patient demographics, and we compared attendances for gastroenteritis and appendicitis, using the SNOMED-CT codes in Appendix 1 to define the study population, in total and by age, to assess examples of one diagnosis likely to be affected and one diagnosis unlikely to be affected by lockdown measures. Differences were assessed using chi-squared test. Analysis was done in R version 3.60 (The R Project for Statistical Computing, Vienna, Austria). This study was granted service evaluation approval through Imperial College London NHS Trust (Ref:228). Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
RESULTS
There were 31,624 ED attendances in the pre-lockdown period and 16,355 in-lockdown, a reduction from 1129 attendances a day pre-lockdown, to 584 a day in-lockdown. Arrivals in ambulances accounted for 61.2% attendances pre- and 51.7% in-lockdown. As a proportion of pre-lockdown attendances, in-lockdown attendances were lowest for under-18s (16.0%) and highest for patients aged 40–60 (76.7%). Male and Asian patients made up a higher proportion of in-lockdown than pre-lockdown attendances. This was also true for patients from postcodes considered the primary catchment for the Trust (77% pre-lockdown and 80% in-lockdown). Pre-lockdown, 17.5% of ED attendances resulted in admission to inpatient wards or intensive care units (ICU), compared to 24.4% in-lockdown. Following lockdown implementation, 4% of admitted patients were admitted directly to ICU, compared to 1% pre-lockdown. Changes in attendances were deemed statistically significant (P<0.0001, chi-squared test). Results are summarised in Table 1.
Table 1.
Characteristics of patients attending two emergency departments in one hospital Trust in North West London.
| Time period | Pre-lockdown | In-lockdown | |
|---|---|---|---|
|
| |||
| n (% of all attendances) | n (% of all attendances) | as % of pre-lockdown attendance | |
| Total number of attendances | 31,624 | 16,355 | 51.7% |
| Male | 15,359 (48.6%) | 8,870 (52.9%) | 57.8% |
| Age | |||
| 0–18 | 7,054 (22.2%) | 1,131 (6.8%) | 16.0% |
| 18–40 | 8,412 (26.6%) | 4,865 (29.0%) | 57.8% |
| 40–50 | 3,073 (9.7%) | 2,368 (14.1%) | 77.1% |
| 50–60 | 3,616 (11.4%) | 2,702 (16.1%) | 74.7% |
| 60–70 | 2,922 (9.2%) | 1,868 (11.1%) | 63.9% |
| 70–85 | 4,563 (14.4%) | 2,797 (16.7%) | 61.3% |
| 85+ | 1,984 (6.3%) | 1,034 (6.2%) | 52.1% |
| Ethnic group | |||
| Any other ethnic group | 7,704 (24.4%) | 3,787 (22.6%) | 49.2% |
| White | 12,576 (39.8%) | 6,342 (38.8%) | 50.4% |
| Black or Black British | 4,256 (13.5%) | 2,239 (13.7%) | 52.6% |
| Asian | 1,499 (4.7%) | 1,208 (7.2%) | 80.6% |
| Not stated | 3,445 (10.9%) | 2,154 (12.9%) | 62.5% |
| Not known | 547 (1.7%) | 594 (3.5%) | 108.6% |
| Catchment area | 24,568 (77.7%) | 13,467 (80.3%) | 54.8% |
| Arrival by ambulance | 19,340 (61.2%) | 7,972 (51.70%) | 41.2% |
| Discharge destination | |||
| Home1 | 20,935 (66.2%) | 10,930 (66.8%) | 52.2% |
| Admitted to hospital | 5,463 (17.3%) | 3,921 (24.0%) | 71.8% |
| Other hospital care2 | 3,945 (12.5%) | 798 (4.9%) | 20.2% |
| Mortuary | 38 (0.1%) | 69 (0.4%) | 181.6% |
| Missing | 259 (0.8%) | 619 (3.7%) | 239.0% |
| Disease profile | |||
| Gastroenteritis | 511 (1.6%) | 103 (0.6%) | 20.2% |
| Appendicitis | 144 (0.5%) | 41 (0.3%) | 28.5% |
Home includes nursing and residential care homes.
Other hospital care includes ambulatory care centre and short stay wards.
P<0.0001 for all pre- vs in-lockdown comparisons.
Gastroenteritis and Appendicitis Attendances Pre- and In-lockdown
Pre-lockdown, there were 511 attendances with a gastroenteritis code, 1.62% of all attendances, compared to 103 attendances in-lockdown, 0.61% of the total. Total ED attendances with an appendicitis code also decreased over the study period, from 144 (0.46% total) to 41 (0.24% total). Attendances for gastroenteritis in-lockdown were 20.2% of pre-lockdown, compared to 28.5% for appendicitis. While a similar proportion of patients with gastroenteritis were directly discharged home in both time periods (84% before lockdown compared to 83% in lockdown), we observed a threefold increase in discharge rates among patients with appendicitis following lockdown implementation (13% compared to 34%).
Changes in attendances for both diseases varied with age. We observed the most significant reduction in attendances with gastroenteritis amongst children and young people and patients aged over 60.
DISCUSSION
In line with national data,2 we found that overall ED attendances almost halved since the introduction of lockdown. Similar to other reports,6,8 the impact of the lockdown on ED attendance rate was greatest in the under-18’s, suggesting changes in parental health-seeking behaviour. Following lockdown implementation, a higher proportion of ED patients required hospital admission, and there was a fourfold increase in the proportion admitted directly to ICU. These changes may reflect patients attending with more serious conditions, severe COVID-19 and/or the increase in ICU capacity. In contrast, for patients with appendicitis there was a reduction in admissions, which was likely due to a change in clinical management to antibiotics during this time.9
We hypothesised a reduction in gastroenteritis-related attendances following lockdown implementation due to reduced interpersonal contact and spread of infectious diseases. The results show that attendances in-lockdown fell to one-fifth of pre-lockdown rates. A reduction in ED attendances for specific infectious diseases has been described in England2 and Italy.10 However, the decrease in attendances for appendicitis suggests that reduced transmission alone cannot explain the reduction in ED attendances seen after lockdown.
LIMITATIONS
Not all of the differences we have reported are attributable to lockdown. Seasonal variations are seen in a range of infectious diseases, including gastroenteritis. However, seasonal variations alone are unlikely to account for our findings as nationally published data for this hospital Trust suggest April attendances in 2019 were only 5% lower than January 2019.11 Gastrointestinal (GI) symptoms are seen in around 15% of children and adults with confirmed SARS-CoV-2 infection.12 As such, patients with COVID-19 presenting with fever and prominent GI symptoms may be wrongly diagnosed with gastroenteritis, confounding our in-lockdown results. We did not exclude these presentations as we did not know patients’ motivations for attending ED, and testing policy evolved over the study period. Nonetheless, we feel this confounding effect is unlikely to have had a substantial bearing on our results as we observed a fourfold reduction in gastroenteritis attendances during the in-lockdown period. Indeed, if large numbers of patients with GI symptoms secondary to COVID-19 were wrongly labelled as having infectious gastroenteritis, we may have underestimated the extent of the fall in ED attendances for gastroenteritis across the study period.
Treatment pathways have changed during the pandemic as hospitals have sought to minimize non-emergency surgery. This includes an increase in the management of uncomplicated appendicitis with oral antibiotics possibly explaining the fall in appendicitis-related admissions.8 However, this cannot explain the reduction in ED attendances with appendicitis to less than one-third of pre-lockdown levels, as there was no concurrent change in advice to primary care practitioners and patients regarding appendicitis during this time.
CONCLUSION
We have developed a conceptual causal framework proposing various factors which may lead to lower ED attendances during the COVID-19 pandemic. These factors include deterred care seeking due to fears of acquiring infection in hospital settings and patients seeking health advice from other services. Future studies, using larger, more generalisable data from across whole healthcare systems must aim to untangle the relative contributions of these different factors and ensure that sick patients have timely and equitable access to emergency care.
Supplementary Information
ACKNOWLEDGMENTS
This research was funded by the NIHR Imperial Biomedical Research Centre (BRC). The research was conducted using National Institute of Health Research Health Informatics Collaborative data resources. Data management was provided by the Big Data and Analytical Unit (BDAU) at the Institute of Global Health Innovation (IGHI).
Imperial College London is grateful for support from the NW London NIHR Applied Research Collaboration. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Footnotes
Section Editor: Patrick Meloy, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. This report is independent research funded by the UK National Institute for Health Research (NIHR) Biomedical Research Centre NIHR-BRC-P68711. KH and PE are supported by the NIHR Imperial Biomedical Research Centre (BRC). CC is supported by a personal NIHR Career Development Fellowship (NIHR-2016-090-015). GSC is supported by NIHR Research Professorship. RGN is supported by NIHR academic clinical lecturer award (ACL-2018-21-007). ChC’s work as a Clinical Research Fellow in Integrated Care is supported by a grant from the Imperial Health Charity. Ethics for this study was granted service evaluation approval through Imperial College London NHS Trust (Ref:228).
REFERENCES
- 1.UK Parliament. UK Parliament Health Secretary gives update on new ‘lockdown’ measures announced to tackle coronavirus. 2020. [Accessed February 16, 2021]. Available at: https://www.parliament.uk/business/news/2020/march/update-on-coronavirus-24-march-2020.
- 2.Kelly E, Firth Z. How is COVID-19 changing the use of emergency care? The Health Foundation; 2020. [Accessed June 5, 2020]. Available at: www.health.org.uk/news-and-comment/charts-and-infographics/how-is-covid-19-changing-the-use-of-emergency-care. [Google Scholar]
- 3.Buddhdev P, Gille H, Ibrahin Y. The paediatric burden of UK lockdown – early results in the COVID-19 era. 2020. [Accessed June 9, 2020]. Available at: https://www.boa.ac.uk/policy-engagement/journal-of-trauma-orthopaedics/journal-of-trauma-orthopaedics-and-coronavirus/the-paediatric-trauma-burden-of-uk-lockdown-early.html.
- 4.Wong LE, Hawkins JE, Langness S, et al. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care | Catalyst non-issue content. 2020. [Accessed June 9, 2020]. Available at: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0193.
- 5.Crawley E, Loades M, Feder G, et al. Wider collateral damage to children in the UK because of the social distancing measures designed to reduce the impact of COVID-19 in adults. BMJ Paediatr Open. 2020;4(1):e000701. doi: 10.1136/bmjpo-2020-000701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bavli I, Sutton B, Galea S. Harms of public health interventions against Covid-19 must not be ignored. BMJ. 2020;371:m4074. doi: 10.1136/bmj.m4074. [DOI] [PubMed] [Google Scholar]
- 7.United Kingdom National Health Service. NHS Digital SNOMED CT 2020. 2020. [Accessed June 9, 2020]. Available at: https://digital.nhs.uk/services/terminology-and-classifications/snomed-ct.
- 8.Isba R, Edge R, Jenner R, et al. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch Dis Child. 2020;105(7):704. doi: 10.1136/archdischild-2020-319385. [DOI] [PubMed] [Google Scholar]
- 9.Collard M, Lakkis Z, Loriau J, et al. Antibiotics alone as an alternative to appendectomy for uncomplicated acute appendicitis in adults: Changes in treatment modalities related to the COVID-19 health crisis. J Visc Surg. 2020;157(3S1):S33–S42. doi: 10.1016/j.jviscsurg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Angoulvant F, Ouldali N, Dawei Yang D, et al. COVID-19 pandemic: impact caused by school closure and national lockdown on pediatric visits and admissions for viral and non-viral infections, a time series analysis. Clin Infect Dis. 2021;72(2):319–22. doi: 10.1093/cid/ciaa710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NHS England. A&E Attendances. 2020. [Accessed June 5, 2020]. Available at: www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/
- 12.Mao R, Qiu Y, He JS, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(7):667–78. doi: 10.1016/S2468-1253(20)30126-6. Erratum in: Lancet Gastroenterol Hepatol 2020; 5(7):e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.