Lateral flow device (LFD) rapid tests for SARS-CoV-2 antigens are used for asymptomatic testing (including for people who are presymptomatic or paucisymptomatic) in various settings, including in the UK. As of April 9, 2021, LFD tests were made available for twice per week rapid testing to the general population in England. News articles reported pressures within the UK Government to rescind asymptomatic testing due to concerns that, despite high specificity (estimated to be 99·9%),1 the proportion of people testing positive who had COVID-19 (ie, the positive predictive value) was falling in line with the reducing prevalence, leading to greater proportions of individuals having to unnecessarily isolate because of a false-positive test result.2 Asking people to isolate on the basis of what might be a false-positive result is associated with a perceived unfairness and, in some cases, moral indignation.
The risk of people without COVID-19 self-isolating due to false-positive test results is a cost to the individual, their household, and their workplace that needs consideration and mitigation. However, this cost should be considered in the context of the costs of failing to identify true-positive results. In the UK, the epidemic control strategies implemented during the past year, including lockdowns, have all, to varying extents, required people who do not have COVID-19 to isolate or quarantine and to greatly restrict their social contacts, while shutting down entire economic sectors. These restrictions have had massive implications for the incomes, education, and wellbeing of many people, including children and young people.3 Any discussions concerning LFD testing policy should incorporate the trade-off between the negative effects of false positives and the onwards transmission prevented. This trade-off is particularly pertinent when considering the contribution of LFD testing to preventing the need for additional widespread restrictive measures.
Keeping COVID-19 prevalence low is of great public benefit. During the pandemic, all people in the UK have been asked to take measures, which might be personally challenging, to mitigate risk to others, even when they have no symptoms and low likelihood of transmitting the virus. People in the UK generally wear a mask over their nose and mouth in enclosed spaces and self-isolate if they have been in contact with someone known to have COVID-19, even if just an estimated 10–15% of people who come into contact with someone with COVID-19 become infected during a period of high prevalence.4 These measures could be considered analogous to responses to a false-positive test, but the public recognises their value in the reduction of transmission. Most people also recognise that reducing the risk of transmission to others is of benefit to themselves, and the same applies to asymptomatic or community testing.
No measures to control SARS-CoV-2 transmission are without cost or harm, and these costs and harms are not experienced equally across society. If asymptomatic testing is to work and be equitable, it is imperative that more is done to ensure that isolation or quarantine is not an undue sacrifice that disproportionately affects people who cannot work from home and might lose their jobs, incomes, or ability to care for family members.5, 6 A crucial part of the problem is distinguishing between false-positive results and true-positive results and their consequences as an end-to-end system. Much of the harm of false-positive results can be mitigated by taking a second test if the first is positive; if this is done via LFD, it would add only 30 min, and varying test batches (or even tests that detect different antigens) could help address concerns that the chance of receiving a false-positive result might be correlated across tests delivered together, especially if they are from the same batch.7, 8 Although a second test increases specificity of the testing procedure, it can only lower overall sensitivity as neither LFD nor PCR testing is 100% sensitive. The accompanying reduction in true-positive results could also have an effect on transmission.
If COVID-19 prevalence is low and the proportion of false-positive results is judged too high for mass asymptomatic population testing, when considered with the appropriate trade-offs, then LFD testing might be well suited to other applications, including: testing subpopulations with high prevalence, such as people who have been in contact with someone with COVID-19;9, 10 testing in high-transmission settings or where physical distancing is impossible; and testing in areas where variants of concern have been detected. The role of LFD testing in society can, and should, be subject to continuous study (including cost-effectiveness), review, and communication, with policy modifications made accordingly. Furthermore, messaging about LFD test accuracy, interpretation, and importance should be clear, should reach underserved groups, and should be based on the most up-to-date evidence.
Asymptomatic testing interventions should not be dismissed on the basis of numbers of people isolating after false-positive test results alone without assessing their worth in preventing both onwards transmission and more widespread restrictive interventions.
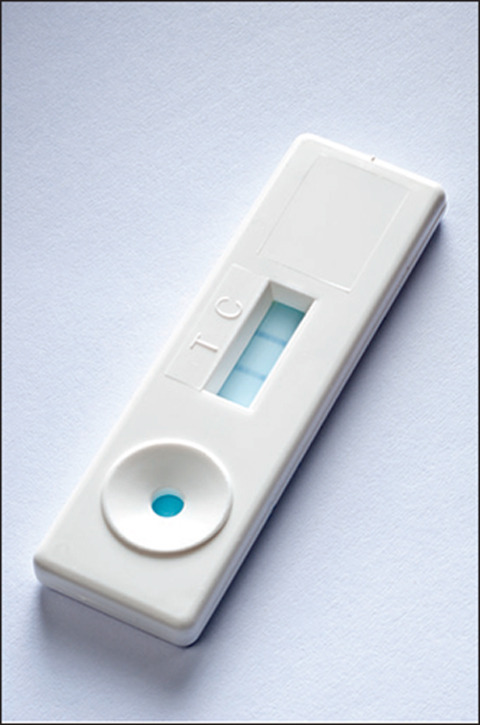
© 2021 Jim Varney/Science Photo Library
IEB has received personal fees from AstraZeneca for his role as a chief data scientist advisor via the University of Liverpool. The other authors declare no competing interests.
References
- 1.Wolf A, Hulmes J, Hopkins S. Lateral flow device specificity in phase 4 (post marketing) surveillance. Department of Health and Social Care. March 10, 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/968095/lateral-flow-device-specificity-in-phase-4.pdf
- 2.Halliday J. Rapid covid testing in England may be scaled back over false positives. April 15, 2021. https://www.theguardian.com/world/2021/apr/15/rapid-covid-testing-in-england-may-be-scaled-back-over-false-positives
- 3.UK Office for National Statistics Coronavirus and the impact on students in higher education in England: September to December 2020. Dec 21, 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/educationandchildcare/articles/coronavirusandtheimpactonstudentsinhighereducationinenglandseptembertodecember2020/2020-12-21
- 4.Public Health England Investigation of novel SARS-CoV-2 variant: variant of concern 202012/01. 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/959361/Technical_Briefing_VOC202012-2_Briefing_2.pdf
- 5.Smith LE, Potts HWW, Amlôt R, Fear NT, Michie S, Rubin GJ. Adherence to the test, trace, and isolate system in the UK: results from 37 nationally representative surveys. BMJ. 2021;372:n608. doi: 10.1136/bmj.n608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fancourt D, Bu F, Mak HW, Steptoe A. COVID-19 Social Study results release 28. Jan 13, 2021. https://b6bdcb03-332c-4ff9-8b9d-28f9c957493a.filesusr.com/ugd/3d9db5_bf013154aed5484b970c0cf84ff109e9.pdf
- 7.Mina MJ, Peto TE, García-Fiñana M, Semple MG, Buchan IE. Clarifying the evidence on SARS-CoV-2 antigen rapid tests in public health responses to COVID-19. Lancet. 2021;397:1425–1427. doi: 10.1016/S0140-6736(21)00425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quilty B, Hellewell J, Clifford S, CMMID COVID-19 Working Group Confirmatory testing with a second lateral flow test may mitigate false positives at low levels of SARS-CoV-2 prevalence in English schools. March 12, 2021. https://cmmid.github.io/topics/covid19/lft_confirm_testing_schools.html
- 9.Love N, Ready D, Turner C, et al. The acceptability of testing contacts of confirmed COVID-19 cases using serial, self-administered lateral flow devices as an alternative to self-isolation. medrxiv. 2021 doi: 10.1101/2021.03.23.21254168. published online March 26. (preprint). [DOI] [PubMed] [Google Scholar]
- 10.Quilty BJ, Clifford S, Hellewell J, et al. Quarantine and testing strategies in contact tracing for SARS-CoV-2: a modelling study. Lancet Public Health. 2021;6:e175–e183. doi: 10.1016/S2468-2667(20)30308-X. [DOI] [PMC free article] [PubMed] [Google Scholar]


