Abstract
Background:
Non-pharmacological therapies have been shown to be effective in managing challenging behavior in people with dementia. However, the efficacy of art therapy has yet to be determined.
Objective:
In the present systematic review, we evaluate the efficacy of art therapy as a non-pharmacological intervention for dementia and examine whether art therapy improves wellbeing and quality of life while decreasing biological and psychological symptoms of dementia (BPSD).
Methods:
Research undertaken between 2015 and 2020 was examined and a total of seventeen studies met the specified search criteria, with 853 participants (657 people with dementia, 180 formal and informal carers, and 16 volunteers) involved.
Results:
We identified four outcome domains: wellbeing, quality of life, BPSD, and cognitive function. One or more significant outcomes as having an impact on the efficacy of the intervention were reported in 88% (15/17) of the studies, whereas 17% (3/17) demonstrated significant outcomes across quality of life, wellbeing, and BPSD.
Conclusion:
People with dementia benefit from art therapy. These interventions when incorporating elements of being ‘in the moment’ increase opportunities for communication between people with dementia and their caregiver(s) and facilitate person-centered therapeutic activities.
Keywords: Art therapy, behavioral and psychological symptoms of dementia, cognition, dementia, non-pharmacological therapy, systematic review
INTRODUCTION
Globally, 47.5 million people are currently living with dementia, and a further 7.7 million will be diagnosed every year, reaching overall to 152 million individuals diagnosed by 2050 [1]. Dementia pharmacological interventions pose clinical challenges which are becoming increasingly harder to ignore. As patients experience various discouraging side effects, a cycle commences of them being non-compliant with taking their medications, and this in turn will affect their clinical symptoms and the response the drug has overall. Consequently, there has been a rise in non-pharmacological and psychosocial interventions available to enhance quality of life, wellbeing and reducing behavioral and psychological symptoms of dementia (BPSD) [2, 3].
Social interactions and activities positively correlate with older people’s wellbeing and physical health [2, 4] which are essential for the retention of personhood. Personhood is also used as an indicator of wellbeing and quality of life for an individual diagnosed with dementia. Kitwood (1997) defines personhood as ‘a standing or status that is bestowed upon one human being, by others, in the context of relationship and social being; it implies recognition, respect, and trust’ (p.8; [5]). The concept of personhood is the core of the Person-centered care model—it states that there is a need for creativity, self-expression, and social interactions in relation to the needs of the individual [2]. It is now a widely adopted model for both dementia care and other clinical care settings instead of the traditional medical model. It builds upon the notion that every individual should have a fulfilled life independently of the health status [5, 6].
Art therapy for dementia
According to The United Nations Declaration of Human Rights Act (1948) Article 27 “Everyone has the right freely to participate in the cultural life of the community, to enjoy the arts and to share in scientific advancement and its benefits” [7]. Creative expression (as stated in [5]) is part of the ten forms of positive interactions that support positive wellbeing in people with dementia. As such, there has been an increase within dementia care services to engage service users with dementia in therapeutic meaningful activities such as art, music, and storytelling amongst others. These activities allow people with dementia to regain a sense of identity and explore new skills safely, that would otherwise not be possible for them.
Art therapy, as defined by The British Association of Art Therapists (BAAT), is a form of psychotherapy that uses art media as its primary mode of expression and communication [8]. Art therapy presents itself in one of two forms, structured or unstructured, and the sessions are subsequently based on these principles. Structural forms of art therapy are those when facilitators pre-determine a theme, materials and how the session will proceed. Structural sessions are considered better for patients with severe dementia, mobility issues or other concerns. In contrast, unstructured sessions are patient led, and people with dementia are encouraged to choose materials, themes and tools without a facilitator.
Art therapy is considered effective because it can be tailored to meet a range of needs for each individual person. For example, it can be used as a tool for communication [9], helps meet the emotional and psychological needs of patients [10], retains skills [11, 12], and encourages the process of reminiscence. Seifert et al. [13] reported that for patients with dementia, art-based interventions lead to improvements in self-esteem, concentration, and memory.
In 2007, the Museum of Modern Art (MoMA) in New York City launched the innovative “Meet Me at MoMA” program. It was the first gallery to make art accessible to individuals with dementia and their caregivers [14]. The aim of the program was to promote public engagement and enhance quality of life through intellectual stimulation, shared experiences and opportunities for social interactions. Subsequently, it inspired a framework for interventions on delivering and creating art programs for people with dementia and their care partners.
Despite the growing interest in non-pharmacological interventions for dementia, there is still a perceived failure to accurately report the efficacy of these interventions. The studies fail especially in the manner in which they report valid and reliable clinical measures which demonstrate how the intervention affects patients, and how patient’s outcome measures are scored and change over time. In the present study, we provide a review of current research in this area, concentrating on both the efficacy of art therapy as a non-pharmacological intervention for dementia and in improving the wellbeing and quality of life for people with dementia.
METHODS
Literature search
We identified peer-reviewed articles published or translated in the English language, between January 1, 2015 and June 1, 2020. We limited the timeframe to capture the most recent and up to date studies. Using a systematic approach set out by the PRISMA guidelines for reporting systematic reviews (PRISMA [15]), a comprehensive search of following electronic databases was conducted: PubMed, EBSCOhost (searching PsycARTICLES, PsycINFO, AMED and CINAHL), and Google Scholar. Initially the terms Art therapy, Art intervention, Music Therapy, and Music Intervention were paired individually with Dementia or Alzheimer’s. Subsequently, the terms non-pharmacological intervention and psychosocial were added to the searches to generate every possible combination.
Selection criteria
The identified articles were individually assessed for inclusion in the present review according to a set criterion. The initial inclusion criteria were as follows: 1) involved individuals diagnosed with any form of dementia, 2) published in a peer-reviewed journal and meeting study design inclusion criteria (see Table 1), 3) identification of treatment and/or exposure to art therapy or music therapy interventions, and 4) containing outcome measures [i.e., BPSD, quality of life (QOL), or wellbeing (subjective or composite)] prior and after the intervention. Articles were excluded if they did not meet the criteria mentioned above in addition to: articles containing combined art-based approaches such as art and dancing, intervention was aimed at caregivers rather than patients and if they did not meet criteria 2 (Table 1). We also decided to extend our exclusion criteria to include articles relating to music interventions, as this both had generated a larger than anticipated scope of research articles and there have already been recent reviews conducted into the efficacy of music-based interventions. The remaining articles included in this review referred to visual arts as defined as the arts of painting and sculpture, rather than literature and music (https://dictionary.cambridge.org/) and did not include ceramic art, printmaking, design, crafts (i.e., knitting, calligraphy, sewing, woodworking, etc.), photography, architecture, film, and video.
Table 1.
Inclusion and exclusion criteria used in the systematic review. The criteria were based on the PICO framework: Patient problem –dementia; Intervention –Creative Visual art; Comparison/Control –participants with no dementia, formal or informal carers, family members; Outcome measures - cognitive function, biological and psychological symptoms of dementia, Wellbeing and Quality of life. We made the difference between pilot and feasibility studies according to Whitehead et al (2014) definition [16]: ‘feasibility’ should be used as an overarching term for preliminary studies and the term ‘pilot’ refers to a specific type of study which resembles the intended trial in aspects such as having a control group and randomization; studies labelled ‘pilot’ should have different aims and objectives to main trials and should also include an intention for future work [16]
| Inclusion criteria | Exclusion criteria |
| Randomized Control Trials | Reviews (narrative, systematic, and meta-analysis |
| Quasi-experimental | Experimental studies containing < 7 participants |
| Qualitative studies | Case studies |
| Observational studies | Applied Behavior Analysis (ABA) studies |
| Pilot studies | Taxonomy studies |
| Exploratory studies Mixed methods studies | Feasibility studies |
Identification of eligible studies
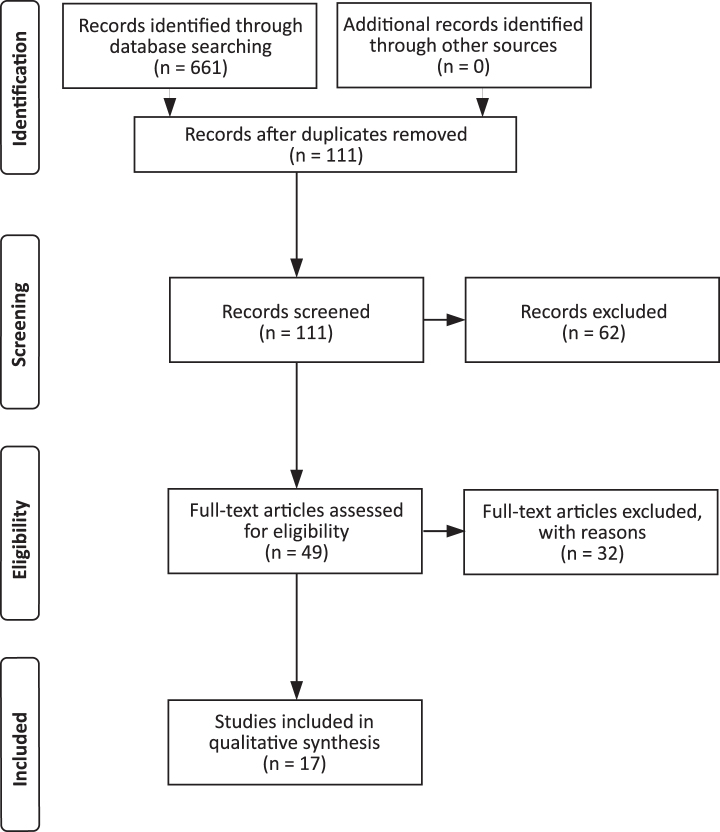
A comprehensive search of the literature yielded a total of 661 studies meeting the search terms. Out of the total of 111 articles eligible for screening meeting the initial inclusion criteria by their title and abstracts, only17 articles from the initial search were eligible for full-text screening and were included in the present review (Fig. 1 for the PRISMA flow diagram of article eligibility). Eligible articles were then coded by contributors according to relevant study characteristics: 1) number of participants, 2) experimental design, 3) clinical measures, 4) effect of QOL and/or BPSD, 5) type of art intervention, 6) benefits to patients, and 7) limitations and implications for future research. Both authors (SYME and EBM-L) reviewed the articles.
Fig. 1.
Flow diagram of articles eligibility for inclusion in the current review.
RESULTS
We present a summary of the findings according to creative art interventions, capturing the efficacy of each individual form and the impact it has on patients with dementia (Table 2). A total of 853 subjects (657 people with dementia, 180 formal and informal carers, and 16 volunteers) participated in these studies including two long-term secure care facilities (76 total residents, 54–102 years of age, of which 20 partook in the study; [11]). Across the included studies, we identified three different forms of Creative Art therapy: Visual Art Making (seven studies [11–13, 19–21, 25]), Art Appreciation (six studies, [3, 4, 9, 17, 22, 23], and a combination of both (four studies [2, 10, 18, 24]) (Table 2). 88% of articles (15/17) reported clinical measures pre-and post-intervention. These studies used quantitative measures of cognition (Mini-Mental State Exam (MMSE); Alzheimer’s Disease Assessment Scale-Cognitive Subscale, Mini-Addenbrooke’s Cognitive Examination), Activities of Daily Living, Neuropsychiatric Inventory, The Cohen-Mansfield Agitation Inventory (a 29-item scale to assess agitation completed by a proxy, i.e., family carer or staff member), Geriatric Depression Scale, outcome measures for quality of life for people with dementia (DEMOQOL) etc. (see Table 2, with the full list of rating scales and assessments completed in the reviewed studies). Graham and Fabricius [11] and Mondoro et al. [21] were the only two of the seventeen studies that used a qualitative approach. Graham and Fabricius [11] protocol consisted of observations and field notes which were later translated and analyzed following inductive thematic analysis. Although Mondro et al. study used a questionnaire, this was to be completed by the caregivers and results were analyzed using thematic analysis [21]. The approach in these two studies enabled extraction of themes, a method which lends itself to capturing the essence of an experience.
Table 2.
Summary of eligible studies
| Author (y) | Summary | Description of art therapy | Clinical measures | Effect on QOL/BPSD | Findings/Benefits |
| Loizeau et al. 2015 [17] | A mixed method study that utilized TimeSlips to encourage persons living with dementia to create stories. It was conducted at the Kunsthaus Museum in Switzerland. Participants were four people with dementia and their caregivers and four volunteers, who supported the people with dementia during the sessions. | Art appreciation: Museum visits with storytelling sessions. | CBS DAS-D Interviews SFAS | Yes / Yes | There was a statistically significant positive effect on all participants’ mood (all participants: Z = –4.84, p < 0.001; people with dementia: Z = –3.57, p < 0.001; Caregivers: Z = –3.34, p < 0.001). No significant differences in the caregivers’ and volunteers’ attitudes towards dementia or Caregiver Burden Inventory were found. All caregivers and most of the volunteers reported a positive change in their attitude towards dementia. People with dementia reported that they welcomed the opportunity to contribute and express their thoughts. All participants were highly satisfied with their experience. |
| Hazzan et al. (2016) [18] | Pilot study with 8 male participants with dementia diagnosis. | Art appreciation and art making sessions across several art domains. | MMSE CMAI ADL | Yes / Yes | Increase in meaningful communication and engagement with care partners. |
| Sauer et al. (2016) [2] | Exploratory study using video data on 38 people with dementia living in long-term care. | A person-centered and intergenerational art making activity program called Opening Minds through Art (OMA), including traditional visual arts activities (e.g., coloring books, scrapbooking). | GCCWOT | Yes / Not tested | Descriptive results indicated a high percentage of moderate or high intensities of well-being during OMA sessions, with little to no ill-being. Paired-sample t-tests comparing OMA showed significantly higher intensity scores in the domains of engagement and pleasure, as well as significantly lower intensity scores for disengagement when compared to traditional visual arts activities alone. |
| Johnson et al. (2017) [3] | Quasi-experimental crossover design study investigating impact of museum activities on subjective wellbeing. | Art appreciation: object handling and art viewing. | VAS | Yes / Not tested | Significant increase in subjective wellbeing during the session, irrespective of the order activities were presented, for both people with dementia and their caregivers. An end of intervention questionnaire indicated that experiences of the session were positive. |
| Participants were people with early to middle stage dementia and their caregivers (66 in total: 36 people with dementia and 30 caregivers). | |||||
| Seifert et al. (2017) [13] | Pilot study on 12 people dementia (n = 6 each in experimental and control group), examining how a sculpture-based therapy influences wellbeing. | Visual Art Sculpture making for experimental and control group; they also participated in singing, painting and playing board games. | MMSE NPI | Yes / Yes | The experimental (sculptural activity) group showed improvements in wellbeing across all five domains: mental state and concentration, corporeal memory, self-reliance, self-esteem and physicality. |
| Tyack et al. (2017) [4] | Quasi-experimental study exploring technology assisted art therapy. 12 pairs of volunteers with dementia and informal caregivers were recruited (n = 24). | Art appreciations using technology, i.e., touchscreen tablet device displaying art images. | VAS QOL-AD | Yes / On mood and behavior | Well-being subdomains generally increased with number of sessions. Qualitative positive findings included changes in cognition, behavior, mood and relationships. |
| Graham and Fabricius (2018) [11] | Qualitative study examining effect of a live mural painting in two long-term care dementia facilities (n = 76). | Visual art painting of institutional (i.e., care home, hospital) doors into a mural. | Qualitative study | Yes / Yes | Reduction in exit-seeking behavior; benefits in sustained attention, aesthetic awareness, memory, gender identity and community building. |
| Hammani and Khadhar (2018) [19] | Observational study investigating the impact of art therapy on behavior in 12 people with a diagnosis of Alzheimer’s disease dementia. | Visual art: Painting workshops. | MMSE | Yes / Yes | Improvements in motivation and concentration, with reduction in agitation and aggressive behavior. |
| Mondro et al. (2018) [20] | 30 dyads of carers-dementia participants took part in the 8 weeks Retaining Identity Program. Study was based on a qualitative analysis. | Visual art: Art making sessions and discussions. | Questionnaire | Yes / Not tested | The main themes that emerged from the survey were: caregiver growth, caregiver awareness, and creative discovery. The participants’ artwork supports that art making has the potential to encourage an equitable exchange and outcome for people with memory loss and their caregivers. |
| Ramsey et al. 2018 [12] | Quasi-experimental study investigating structured and unstructured art activities and the use of scaffolding in 8 people with dementia. | Visual art: painting and drawing | DEMOQOL | Yes (not significant) / Not tested | Structured scaffolding optimized individuals’ success during sessions. The use of dementia-tailored scaffolding for art activity sessions allowed people to use their retained skills in visual art production (painting and drawing). |
| Structured and unstructured activities. | |||||
| Schall et al. (2018) [10] | A randomized controlled study on the influence of the ARTEMIS intervention on the emotional state, well-being, and quality of life of dementia patients. People with mild-to-moderate dementia (n = 44) and their care partners (n = 44) participated in once a week museum visits on six pre-arranged occasions. | A weekly museum visits once a week on six pre-arranged occasions. The intervention consisted of six different guided art tours (60 min), followed by art-making in the studio (60 min). Independent museum visits served as a control condition. | MMSE QOL-AD GDS ADAS-COG NPI FAHW | Yes / Yes | Art museum-based art interventions are able to improve the subjective well-being, mood, and quality of life in people with dementia. In particular, improvements in participants’ self-rated quality of life (p < 0.05) and a statistically significant positive changes with medium effect sizes (dcorr = 0.74–0.77). The total NPI score as well as the affective (depressed mood and anxiety) and apathy subscales were significantly lower after the ARTEMIS intervention (NPI total = 2.43; NPI affective = 2.24; NPI apathy = 2.52; p < 0.05). |
| Windle et al. (2018) [21] | A mixed method longitudinal study included 125 participants with dementia and explored the impact of visual art program on QOL, wellbeing and communication. | Visual art program with variety of art making tasks. | GCCWBOT DEMQOL HCS | Yes (not significant) / Not tested | Scores for the well-being domains of interest (attention, pleasure, self-esteem, negative affect, and sadness) were significantly better in the art program than the alternative condition. Proxy-reported QoL significantly improved between baseline and 3-month follow-up, but no improvements in QoL were reported by the participants with dementia. |
| Camic et al. (2019) [22] | Quasi-experimental study looking at the impact of object handling. 80 participants diagnosed with early to moderate stage dementia took part. | Art appreciation: object handling. | CWS VAS | Yes / Not tested | People with early and moderate impairment had positive increases in wellbeing, regardless of the type of dementia, but those with early stage dementia showed larger positive increases in their wellbeing. |
| D’Cunha et al. (2019) [23] | A quasi-experimental, exploratory study investigating cortisol levels, QOL and BPSD in 25 people with dementia (mean age 84.6±7.27 years), 22 provided viable saliva samples. 6 weeks duration. | Art appreciation: Art appreciation sessions with discussions as part of the Art and Dementia program at the National Gallery of Australia’s (NGA). | BADL DEMOQOL DMOQOLC GDS M-ACE GWO Handgrip measure | No /Yes | Improvement in hypothalamic-pituitary-adrenal axis function. The waking to evening salivary cortisol ratio was higher post-intervention (p = 0.033), but no change in Interleukin-6 levels. No improvements in QoL (DEMQOL-Carer) between baseline and post-intervention (p = 0.076). However, self-reported depressive symptoms decreased post-intervention compared with baseline (p = 0.015), and memory (immediate recall) (p = 0.009) and verbal fluency (p = 0.027) improved between the same timepoints. |
| Hendriks et al. (2019) [9] | Cross-sectional observational study 144 people, 72 with dementia and 72 caregivers, examined responsiveness to artwork. | Art appreciation: Museum tour guided by trained professional. | GDS BCRS INTERACT Scale | Yes / Not tested | The appreciative and active responsiveness and interaction with others during the program appeared related to the severity of dementia, to specific cognitive impairments and to type of artworks. People with more severe dementia responded less to art than people with mild dementia. Artworks with more natural elements revealed less interaction with others. Artifacts (i.e., objects not originally meant as artworks) evoked more reactions than artworks. |
| Humphrey et al. (2019) [24] | A pilot study on 8 men diagnosed with dementia. | Art appreciation and art making activities. | MMSE CMAI ADL | Yes / Yes | Supportive communication and positive engagement. |
| Lokon et al. (2019) [25] | Exploratory study investigating impact of activity in 67 people with dementia living in care homes. | Comparison of five different activities on the well-being of institutionalized people with dementia: The intergenerational art program OMA, art and music therapies, creative activities, non-creative activities, and no activities at all. | SM-GCCWOT | Yes / Not tested | People with dementia showed the highest well-being scores during OMA compared to all other activities. Although no significant well-being differences were found between creative activities led by licensed art/music therapist versus regular activity staff, or between creative and non-creative activities (led by regular activity staff), people with dementia benefited from participating in activities, regardless of the type (creative or non-creative), or who conducted them (licensed therapists or activity staff). |
ADAS-Cog, Alzheimer’s Disease Assessment Scale; ADL, Activities of Daily Living; BCRS, Brief Cognitive Rating Scale; BADL, Bristol Activities of Daily Living Scale for dementia; BPSD, Behavioral and Psychological Symptoms of Dementia; CBS, Cornell-Brown Scale for Quality of Life; CMAI, The Cohen-Mansfield Agitation Inventory; CWS, Carer Well-Being and Support Questionnaire; DAS-D, Dementia Attitudes Scale; DEMOQOL, Dementia Quality of Life Instrument; DEMOQOLC, DEMOQOL-Carer; FAHW, Questionnaire of General Habitual Well-being; VAS, Visual Analogue Scale; GCCWBOT, The Greater Cincinnati Chapter Well-Being Observation Tool; GDS, Geriatric Depression Scale; GWQ, General Wellbeing Questionnaire; HCS, Holden Communication Scale; M-ACE, Mini-Addenbrooke’s Cognitive Examination; MMSE, Mini-Mental State Examination; NPI, Neuropsychiatric Inventory; QOL, Quality of Life; QOL-AD, Quality of Life in Alzheimer’s Disease; SFAS, Smiley-Face Assessment Scale; SM-GCCWOT, The Scripps Modified Greater Cincinnati Chapter Well-Being Observational Tool.
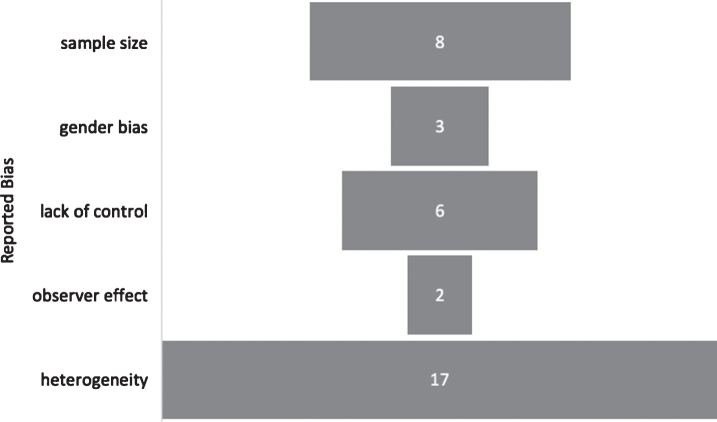
Bias in eligible studies
The presence of bias was examined in two ways: 1) as a whole, for the review process and then 2) within each individual article. We looked at how each study reported being impacted by the risk of bias (see Fig. 2 for a summary of the reported biases).
Fig. 2.
Summary of Report Bias.
The articles reported several limitations and biases that would have influenced their generalizability and efficacy of the intervention. The limitation that was most often reported among all the studies was the heterogeneity of the analyzed sample. However, this was to be expected with specificity of the condition. Thereafter, in eight of the seventeen studies it was reported that there were instances of selection bias, sample size and gender (see Table 2).
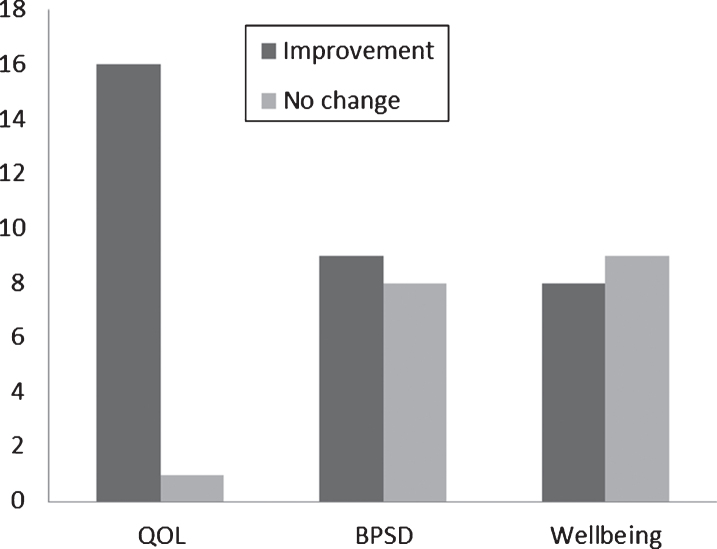
Efficacy of creative art therapy
In order to compare the potential benefits of different creative arts interventions we calculated the proportion of studies that reported statistically significant effect/outcome. Fifteen out of seventeen of the studies (88%) reported at least one outcome to be of statistical significance, whereas all three outcomes were considered statistically significant in three out of the seventeen studies (17%) (Fig. 3).
Fig. 3.
Summary of intervention effects. Columns denote number of studies. QOL, quality of life; BPSD, behavioral and psychological symptoms of dementia.
The following outcome measures were more frequently commented on during creative art interventions: mood (including depression), agitation, well-being, concentration, communication, apathy, motivation, and attention. Of primary interest we decided to focus on Quality of life, wellbeing, and general reduction in BPSD: 16 of the 17 studies (94%) reported improvements in quality of life, 9 (53%) reported reduction in BPSD, and 8 (47%) found improvements to patient wellbeing specifically (Fig. 3). Interestingly, one study reported only positive changes in two specific BPSD symptoms, mood and agitation [4].
Figure 3 demonstrates the general trend in efficacy of creative art interventions, with improving quality of life being most effective, whereas there was no real indication of efficacy in improving wellbeing. It is difficult to make general inferences about the overall impact of creative art interventions on BPSD from the eligible articles since majority of the papers either do not report effects on BPSD or do so inconclusively. Moreover, most of the studies failed to report well-being measures.
Visual art therapy refers to any activity where patients are making or producing art [8]. In the current review, out of the seventeen studies, seven were intervention based around visual art therapy. The majority of these were painting (see Table 2, column six). The exception to this is the Seifert et al. study [13] that used sculpture making to form the basis of their intervention group, while implementing a control group that participated in non-art-based activities. They observed continuous positive improvements in several subscales of wellbeing: mental state and concentration, self-reliance, self-esteem and enhancing individual’s physicality [13]. The results of their stud indicate that the intervention was effective in producing multi-dimensional effects and could potentially improve other areas of psychological functioning.
A small number of studies combined Visual Art Making and Art Appreciation [10, 18, 24, 25]. Art Appreciation encompasses all those interventions whereby art is being viewed in a variety of forms such as galleries or museums [3, 9, 17, 22], tablets [4], and care facilities [10, 13, 25]. Some of the observed benefits are that it allows for people with dementia to reconcile former memories with the artwork being exhibited, thus improving their mood, self-esteem and reducing the strain of caregivers. The studies we reviewed [10, 18, 24, 25] all reported similar findings: meaningful engagements and improvements across clinical measures. All the interventions were able to break the figurative walls of silence and increase communication between caregivers and patients.
DISCUSSION
Creative arts therapies have been investigated as supplementary non-pharmacological interventions for dementia with somewhat conflicting findings. To date, there is no consensus which specific approach of creative art therapy lends itself to be the most effective. As such, this warrants further investigation into which approach is the most effective in alleviating distressing challenging dementia symptoms and improving wellbeing. For the purpose of this review, we have grouped outcome measures together to form coherent themes. In general, the results from this review showed that people with dementia were improving during creative arts therapies across four domains:
-
1.
Cognitive function (included outcomes relating to changes in attention, concentration, and memory);
-
2.
Biological and psychological symptoms of dementia (outcomes relating to changes in motivation, mood, apathy, instances of aggressive behavior or agitation and sadness);
-
3.
Wellbeing with outcomes related or encompassed all subdomains of wellbeing, with outcome measures often redefined for every study; and
-
4.
Quality of life (outcomes relating to changes in communication, fulfilment, engagement as well as general quality of life measures).
One separate theme emerged throughout the data analysis and that was the notion of ‘in the moment’ interventions. Hazzan et al. (2016) program on ‘Artful Moments’ highlighted the feasibility of implementing an art-based intervention in care homes [18]. This study revealed increased levels of engagement between both caregivers and patients, which in turn improved their ability to communicate.
The majority of the studies had one aim, to produce good quality data, whether that be in support or not of evidence-based practice guidelines. Two of the papers from this review discussed novel and innovative concepts: one addressed the possibility of changing how to view art therapy as a global entity [12], whereas the second introduced the idea of testing physiological responses [23]. Ramsey et al. (2018) study outlined a potential new direction for creative art therapy in dementia care [12]. Namely, the proposition is to move away from the concept that creative art therapy should be used as a medical intervention with the purpose of alleviating symptoms and caregiver burden and, instead, incorporate art production as an activity for the purpose of life fulfilment and creative expression [12]. This should lead to the focus being on more person-centered care outcomes such as quality of life and wellbeing [12]. D’Cunha et al. (2019) studied the physiological responses in people living with dementia during art appreciation intervention [23]. They found that elevated cortisol levels were associated with cognitive impairment, whereas diurnal variations in cortisol rhythms were associated with greatest frailty. As participants engaged with the art appreciation intervention their hypothalamic-pituitary-adrenal (HPA) axis function improved. This study is among the few that investigated the impact of creative art intervention upon physiological outcomes, highlighting that the positive effects of art appreciation upon mental and physical wellbeing as re underpinned by dynamic physiological response. Whether this response is sustainable beyond the duration of the intervention (i.e., 6 weeks, [23]), remains to be determined in longer duration studies.
Our study has limitations. Firstly, the study population in the analyzed studies was rather modest (as low as 8 people and did not include a control group [12, 18, 24]). In addition, we identified only one randomized control trial (RCT) study [10]. This was due to the majority of RCTs being on the topic of music. We are aware that this increased the risk of sampling bias as well as any occurrence of detection bias related to the outcome of quality of life. Therefore, without the rigor keenly associated with the process of randomization and concealed allocation in RCTs we are increasing the likelihood of bias. In addition, except for one study that included participants with Alzheimer’s disease only [19], heterogeneity of the dementia etiology appears not to have been considered critical, since the art impact upon the mental attributes, such as mental and cognitive state, was not expected to be dementia subtype-specific [13].
During the review process, it became apparent that it was not possible to review all the literature on art therapies available to patients with dementia. To name a few: music, dance, photography, and writing were among those that were not within the scope of this review. The recent scoping review on creative arts, including visual arts, literary arts, comedy, music, and dance identified only 26 studies [26], providing further support that this field remains largely under researched. Nevertheless, there is strong evidence in support of using participatory and participating arts for both people with dementia [26] and their informal carers [27], irrespectively of the art form. Despite the emerging extensive body of literature over the last five years, there is a lack of consensus in defining quality of life for people with dementia, or what actually encompasses it. During the review process, we decided that all variations of the definition would be accepted as long as studies clearly outlined the definition they utilized in their protocol.
CONCLUSIONS
Retaining the principles of a systematic review we examined the existing knowledge about art therapy for people with dementia. The handful of art studies as an adjunction to standard dementia care (including both pharmacological and non-cognitive/behavioral treatments) although showing some therapeutic efficacy (i.e., upon cognition, affect and emotional well-being, social functioning, behavior, and quality of life) are limited to a small number of participants and have been described of low quality [28]. The latest systematic review, similarly, found art therapy in general or specific art therapies (i.e., performing or creative arts) to have a rather modest cognitive impact on people with dementia [29]. However, all these studies included poorly defined samples, were conducted over a brief period of time (for up to 5–10 weeks), with standardized cognitive tests (i.e., MMSE, ACE-III) used to assess the therapeutic outcomes [29] that may not capture the benefit of treatment in people with dementia over a brief period of time [30]. These shortcomings seem to have been addressed in a most recent randomized control feasibility study conducted on participants with mild cognitive impairment. who were assessed with a more elaborate battery of neurocognitive assessments, including the Rey Auditory Verbal Learning, Delayed Recall and Recognition Trial, tasks from the Wechsler Adult intelligence Scale-3rd edition (WAIS-III), and Colour Trails Test. In this study, participants in the art therapy group had significant improvement in memory domains which were sustained at 9 months [31].
These clinical findings parallel those of neuroradiological and neurophysiological studies that showed reorganization of prefrontal white matter to accompany the visual artistic creativity, i.e., drawing, painting, with multivariate patterns of cortical and cerebellar activity evoked by these tasks [32]. Likewise, activation of prefrontal and parietal lobes was seen in visual artistic creativity (drawing and painting) and aesthetic appreciation of both representational and abstract art, respectively [33]. Similar neuroplastic changes, as demonstrated with enhanced visual and auditory evoked potentials, were recently confirmed in visual and/or music therapy study and these were sustained for up to 3 months [34]. These studies provide further evidence that art provokes plasticity in neural pathways that mediate creative cognition and perceptuomotor integration [32]. More importantly, these studies show the involvement of the fronto-parietal network that is involved in executive function and goal-directed behavior. Bearing in mind that apathy, a decrease in motivation and goal-directed behavior, is the most common neuropsychiatric symptom in people with preclinical [35] and overt dementia [36], art can find its place in both prevention and potential treatment of this syndrome.
In general, many of the studies reviewed here were designed to be observational or as pilot studies opting for the recruitment of smaller samples that met the very specific criteria of the diagnosis. We observed that the mode of delivery had less of an impact on outcome measures then initially assumed. Whether an individual was passively interacting with the artwork itself in an act of appreciation, or actively partaking in developing a piece of artwork seemed to have no influence—it was the creative element of the intervention that had the positive effects on people with dementia.
Viewed as a limitation in many ways as the results cannot be generalized, this form of research is vital in paving the way for future larger studies. Future research would benefit from including larger samples, follow-up after the intervention to measure whether there is a sustained benefit and looking at the influence of intervention on symptom change overtime. It would be beneficial to compare how quality of life changes along the evolution of the disease and how patients respond to creative art therapies. Finally, interventions should look at incorporating more elements of person-centered therapeutic activities and being ‘in the moment’. This will help foster an environment for communication that is meaningful and fulfilling between caregiver and patient dyads.
ACKNOWLEDGMENTS
We would like to thank Dr. Vladimir B. Ladinski for his help with Figure 1.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
REFERENCES
- [1].Alzheimer Disease International (2020) World Alzheimer Report 2020. https://www.alzint.org/resource/world-alzheimer-report-2020/, Accessed on December 27, 2020.
- [2]. Sauer PE, Fopma-Loy J, Kinney JM, Lokon E (2016) “It makes me feel like myself”: Person-centered versus traditional visual arts activities for people with dementia. Dementia 15, 895–912. [DOI] [PubMed] [Google Scholar]
- [3]. Johnson J, Culverwell A, Hulbert S, Robertson M, Camic PM (2017) Museum activities in dementia care: Using visual analog scales to measure subjective wellbeing. Dementia 16, 591–610. [DOI] [PubMed] [Google Scholar]
- [4]. Tyack C, Camic PM, Heron MJ, Hulbert S (2017) Viewing art on a tablet computer: A well-being intervention for people with dementia and their caregivers. J Appl Gerontol 36, 864–894. [DOI] [PubMed] [Google Scholar]
- [5]. Kitwood T (1997) Dementia reconsidered: The person comes first. Open University Press, Berkshire, UK. [Google Scholar]
- [6]. Fazio S, Pace D, Flinner J, Kallmyer B (2018) The fundamentals of person-centered care for individuals with dementia. Gerontologist 58(Suppl 1), S10–S19. [DOI] [PubMed] [Google Scholar]
- [7].The United Nations Universal Declaration of Human Rights Act (1948) lhttps://www.un.org/en/universal-declaration-human-rights/index.html, Accessed on December 27, 2020.
- [8].The British Association of Art Therapists. Retrieved from https://www.baat.org/About-Art-Therapy2020, Accessed December 2020.
- [9]. Hendriks I, Meiland FJM, Slotwinska K, Kroeze R, Weinstein H, Gerritsen DL, Dröes RM (2019) How do people with dementia respond to different types of art? An explorative study into interactive museum programs. Inter Psychogeriatr 31, 857–868. [DOI] [PubMed] [Google Scholar]
- [10]. Schall A, Tesky VA, Adams AK, Pantel J (2018) Art museum-based intervention to promote emotional well-being and improve quality of life in people with dementia: The ARTEMIS project. Dementia 17, 728–743. [DOI] [PubMed] [Google Scholar]
- [11]. Graham ME, Fabricius A (2018) Painting in situ: The benefits of live mural painting for residents on two secure long-term care dementia units. Arts Health 10, 257–273. [Google Scholar]
- [12]. Ramsey A, Webb S, Ellis M (2018) Scaffolding for artistic success: Comparing structured and unstructured art activity for people with dementia. J Dement Care 26, 20–23. [Google Scholar]
- [13]. Seifert K, Spottke A, Fliessbach K (2017) Effects of sculpture based art therapy in dementia patients - A pilot study. Heliyon 3, e00460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. Rosenberg F (2009) The MoMA Alzheimer’s project: Programming and resources for making art accessible to people with Alzheimer’s disease and their caregivers. Arts Health 1, 93–97. [Google Scholar]
- [15]. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidia JP Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaborate. PLoS Med 6, e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16]. Whitehead AL, Benjamin GO, Sully BGO, Campbell MJ (2014) . Pilot and feasibility studies: is there a difference from each other and from a randomised controlled trial?. Contemp Clin Trials 38, 130–133. [DOI] [PubMed] [Google Scholar]
- [17]. Loizeau A. Kündig Y, Oppikofer S (2015) ’Awakened art stories’-Rediscovering pictures by persons living with dementia utilising TimeSlips: A pilot study. Geriatr Ment Health Care 3, 13–20. [Google Scholar]
- [18]. Hazzan AA, Humphrey J, Kilgour-Walsh L, Moros KL, Murray C, Stanners S, Montemuro M, Giangregorio A, Papaioannou A (2016) Impact of the “artful moments” intervention on persons with dementia and their care partners: A pilot study. Canad Geriatr J 19, 58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19]. Hammami S, Khadhar G (2018) Impacts of art therapy and Alzheimer’s disease. Middle East J Age Aging 15, 29. [Google Scholar]
- [20]. Mondro A, Connell CM, Li L, Reed E (2018) Retaining identity: Creativity and caregiving. Dementia 9, 1641–1656. [DOI] [PubMed] [Google Scholar]
- [21]. Windle G, Joling KJ, Howson-Griffiths T, Woods B, Jones CH, Van De Ven PM, Newman A, Parkinson C (2018) The impact of a visual arts program on quality of life, communication, and well-being of people living with dementia: A mixed-methods longitudinal investigation. Int Psychogeriatr 30, 409–423. [DOI] [PubMed] [Google Scholar]
- [22]. Camic PM, Hulbert S, Kimmel J (2019) Museum object handling: A health-promoting community-based activity for dementia care. J Health Psychol 24, 787–798. [DOI] [PubMed] [Google Scholar]
- [23]. D’Cunha N, McKune A Isbel S, Kellett J Georgousopoulou E, Naumovski N (2019) Psychophysiological responses in people living with dementia after an art gallery intervention: An exploratory study. J Alzheimers Dis 72, 549–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24]. Humphrey J, Montemuro M, Coker E, Kilgour-Walsh L, Moros K, Murray C, Stanners S (2019) Artful Moments: A framework for successful engagement in an arts-based programme for persons in the middle to late stages of dementia. Dementia 18, 2340–2360. [DOI] [PubMed] [Google Scholar]
- [25]. Lokon E, Sauer P, Li Y (2019) Activities in dementia care: A comparative assessment of activity types. Dementia 18, 471–489. [DOI] [PubMed] [Google Scholar]
- [26]. Ward MC, Milligan C, Rose E, Elliott M, Wainwright BR (2020) The benefits of community-based participatory arts activities for people living with dementia: A thematic scoping review. Arts Health, doi: 10.1080/17533015.2020.1781217 [DOI] [PubMed]
- [27]. Irons JY, Garip G, Cross AJ, Sheffield D, Bird J (2020) An integrative systematic review of creative arts interventions for older informal caregivers of people with neurological conditions. PLoS One 15, e0243461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28]. Deshmukh SR, John Holmes J, Cardno A (2018) Art therapy for people with dementia. Cochrane Database Syst Rev 9, CD011073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29]. Young R, Camic PM, Tischler V (2016) The impact of community-based arts and health interventions on cognition in people with dementia: A systematic literature review. Aging Ment Health 20, 337–351. [DOI] [PubMed] [Google Scholar]
- [30].NICE guideline [NG97] (2018) Dementia: Assessment, management and support for people living with dementia and their carers. https://www.nice.org.uk/guidance/ng97, Accessed February 28, 2021. [PubMed]
- [31]. Lee R, Wong J, Shoon W, Gandhi M, Feng L, EH, K, Rawtaer I, Mahendran R (2018) Art therapy for the prevention of cognitive decline. Arts Psychother 64, 20–25. [Google Scholar]
- [32]. Schlegel A, Alexander P, Fogelson SV, Li X, Lu Z, Kohler PJ, Riley E, Tse PU, Meng M (2015) The artist emerges: Visual art learning alters neural structure and function. Neuroimage 105, 440–451. [DOI] [PubMed] [Google Scholar]
- [33]. Cattaneo Z, Lega C, Gardelli C, Merabet LB, Cela-Conde CJ, Marcos Nadal M (2014) The role of prefrontal and parietal cortices in esthetic appreciation of representational and abstract art: A TMS study. Neuroimage 99, 443–450. [DOI] [PubMed] [Google Scholar]
- [34]. Alain C, Moussard A, Singer J, Lee Y, Bidelman GM, Moreno S (2019) Music and visual art training modulate brain activity in older adults. Front Neurosci 13, 182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35]. Umucu E, Wyman M, Lee B, Zuelsdorff M, Benton SF, Nystrom N, Johnson SC, Carlsson CM, Asthana S, Gleason CE (2019) Apathy in preclinical Alzheimer’s disease: Psychometric validation of the apathy evaluation scale. Am J Alzheimers Dis Other Demen 34, 16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36]. Zhao QF, Tan L, Wang HF, Jiang T, Tan MS, Tan L, Xu W, Li JQ, Wang J, Lai TJ (2016) The prevalence of neuropsychiatric symptoms in Alzheimer’s disease: Systematic review and meta-analysis. J Affect Disord 190, 264–271. [DOI] [PubMed] [Google Scholar]