Abstract
Introduction
Alternatives to the classical medial parapatellar (MPP) approach for total knee arthroplasty (TKA) include the mini-medial parapatellar (MMPP), mini-subvastus (MSV), mini-midvastus (MMV) and quadriceps-sparing (QS) approaches. The best approach has been not fully clarified. The purpose of the present study was to conduct a Bayesian network meta-analysis comparing these approaches.
Materials and methods
The present analysis was carried out according to the PRISMA extension statement for reporting systematic reviews incorporating network meta-analyses of healthcare interventions. The databases search was performed in October 2019. All clinical trials comparing two or more approaches for primary TKA were considered for inclusion. The baseline comparability was evaluated through the analysis of variance (ANOVA) test. The statistical analysis was performed through the STATA software/MP. A Bayesian hierarchical random-effects model analysis was adopted in all the comparisons.
Results
Data from 52 articles (4533 patients) were collected. The mean follow-up was 20.38 months. With regard to diagnosis, gender, age and BMI, adequate baseline comparability was detected. The MSV approach ranked better concerning clinical scores (the lowest visual analogic scale, the higher KSS and KSFS) and functional outcomes (the shortest straight leg raise, the greatest degree of flexion and range of motion). Concerning perioperative data, the MSV evidenced the shortest hospital stay, while the MPP the shortest surgical duration and lowest estimated blood loss.
Conclusion
According to the main findings of the present study, the mini-subvastus approach for total knee arthroplasty demonstrated superior overall compared to the other approaches. Orthopaedic surgeons should consider this approach in the light of the evidence and limitations of this Bayesian network meta-analysis.
Keywords: Total knee arthroplasty, Medial parapatellar, Subvastus, Midvastus, Quadriceps sparing
Introduction
While the overall effectiveness of total knee arthroplasty (TKA) is largely unquestionable, the best surgical approach is still to be determined. The medial parapatellar approach, introduced by Von Langenbeck [1], is still regarded as the standard. The main benefit of this approach is that it provides the best exposure of knee surfaces. On the other hand, it has been criticized for introducing massive damage to the articular capsule, patellar and quadriceps tendons, extensor apparatus, soft tissue and vascular structures. Minimally invasive approaches to TKA have been evolved for the purpose of preserving the extensor mechanism as much as possible [2, 3]. The first minimally invasive approach for knee arthroplasty was described by Repicci and Eberle [4] for implantation of a unicompartmental prosthesis. Then came techniques extending to TKA. The mini-subvastus (MSV) approach was introduced by Hoffman et al. [5] in 1991 as a way to minimize extensor damage and preserve the vascular supply to the patella. Furthermore, this approach avoided eversion of the patella, thereby reducing the risk of tendon and cartilage damage [2, 3]. In 1997, Engh et al. [6] described the mini-midvastus (MMV) approach. In addition to the advantages of the MSV, this approach provided better exposure to all knee structures. Finally, Tria et al. [7] introduced the quadriceps-sparing (QS) approach in 2003 and Scudieri et al. the mini-medial parapatellar (MMPP) approach in 2004 [8]. The latter is a shortened version of the MPP. To our knowledge, no study has compared data from all these approaches to establish the best approach for TKA. Hence, the purpose of the present study was to perform a Bayesian network meta-analysis to compare these approaches and determine the most effective. We focused on perioperative data, clinical and functional outcomes.
Materials and methods
Search strategy
The present Bayesian network meta-analysis was carried out according to the PRISMA extension statement for reporting systematic reviews incorporating network meta-analyses of healthcare interventions [9]. To orient the literature search, the following features were defined:
P (population) end-stage knee joint disease;
I (intervention) total knee arthroplasty;
C (comparison) MPP, MMV, MSV, QS, MMPP;
O (outcomes) perioperative data, functional outcomes, clinical scores.
Data source
Two authors (FM and JE) independently performed the initial search. In October 2019, the main databases were accessed: PubMed, Google Scholar, Embase and Scopus. The following keywords were used in combination: total knee arthroplasty, total knee replacement, prosthesis, medial, quadriceps sparing, midvastus, subvastus, mini-medal parapatellar, KSS, KSFS, range of motion, flexion, straight leg raises, hospital duration. All pertinent titles and abstracts were screened, and if matching the topic, the full text was accessed. Bibliographies of the included studies were also cross-referenced. Disagreements between the authors were debated and mutually solved.
Eligibility criteria
All clinical trials comparing two or more approaches for primary TKA were considered for inclusion. According to the Oxford Centre for Evidence-Based Medicine, only articles with levels I and III evidence were considered for the present study. Articles were limited to English, German, Italian, French and Spanish. Case series, case reports, letters, expert opinions and editorials were excluded. No differences concerning the type of implants were made; only the surgical approach was pivotal for inclusion. Missing data under our outcomes of interest warranted exclusion. Disagreements were debated and mutually solved.
Outcomes of interest
Two authors (FM and JE) independently screened all articles resulting from the search. For each approach, study generalities and patient demographics were noted: type of study, number of procedures, duration of follow-up, surgical approach(es), percentage of female and osteoarthritic (OA) patients, mean age and body mass index (BMI). Data concerning the following outcomes of interest were collected: perioperative data (duration of surgery and hospitalization, total estimated blood loss), functional outcomes (range of motion (ROM), flexion, straight leg raise (SLR) [10]) and clinical scores (visual analogic scale (VAS) for pain, the Knee Society Score (KSS) and its related function subscale (KSFS) [11]).
Methodological quality assessment
The methodological quality of the present meta-analysis was evaluated using the PEDro appraisal score (http://www.pedro.org.au/english/downloads/pedro-scale/), which has been validated for this type of study [12]. The PEDro score is an aggregate of dichotomically assigned points given to studies based on the presence or absence of specific endpoints such as eligibility criteria, allocation, baseline comparability, blinding, follow-up, type of analysis, point estimates and variability. Values > 6 points are considered satisfactory.
Statistical analysis
The statistical analyses were performed by the senior author (FM). The baseline comparability was evaluated through the analysis of variance (ANOVA) test. Values of P > 0.5 were considered satisfactory to verify comparability. The statistical analysis was performed through the STATA software/MP 14.1 (Stata Corporation, College Station, TX). A Bayesian hierarchical random-effects model analysis was adopted for all the comparisons. We referred to the generic inverse variance statistic method for continuous data analysis with standardized mean difference effect measure. The edge network plot was performed to analyse connections, contribution weights between studies, and to detect direct and indirect comparisons. To evaluate loop-specific inconsistency, heterogeneity and related inconsistency factor (IF), the if test was performed. To evaluate for overall inconsistency, the equation for global linearity via the Wald test was used. If the P value was > 0.05, the null hypothesis could not be rejected and the consistency assumption could be accepted at the overall level of each treatment. The interval plot was performed to rank the estimated effect (EE) of the endpoints between them. Confidence and percentile intervals (CI and PrI) were each set at 95%. The funnel plot was performed to assess the risk of publication bias for each comparison.
Results
Identification of eligible studies
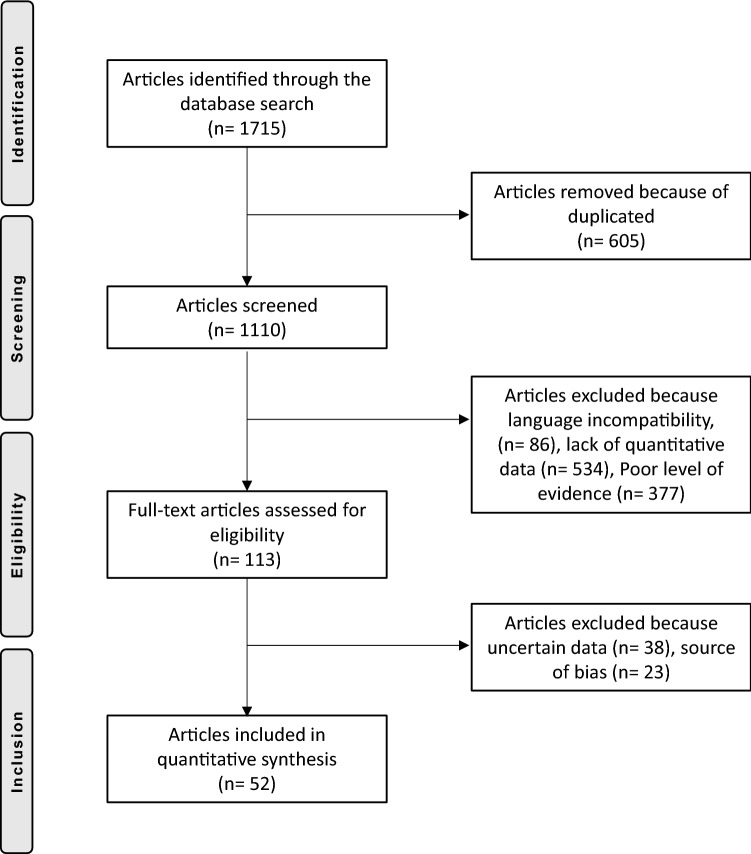
A total of 1715 articles were obtained from the initial search. Of them, 605 were duplicates. A further 377 were rejected because of poor levels of evidence. Another 86 articles were excluded because of language barriers: Chinese, Polish, unknown. Another 534 articles were excluded because they did not report quantitative data under the outcomes of interest. Thirty-eight were excluded because of uncertain data or incomplete results and 23 due to source of publication bias or excessive heterogeneous results. This last operation left 52 articles for review: 34 randomized clinical trials (RCTs), ten prospective cohort studies (PCS), eight retrospective cohort studies (RCS). The flow chart of the literature search is shown in Fig. 1.
Fig. 1.
Flow chart of the literature search
Methodological quality assessment
All included articles stated clearly their eligibility criteria and demonstrated satisfactory baseline comparability. A random and concealed allocation was performed in 32% of the studies. 8% performed a single blinding, and 15% had blinded assessors. Only a third of the included studies performed an adequate follow-up. Almost all the articles performed an adequate analysis, and the intention to treat was satisfied. In the end, the overall PEDro score was 7.42, detecting an optimal quality for the methodological assessment. The PEDro scores across the studies are shown in Table 1.
Table 1.
Demographic baseline of the included studies
| References | Type of study | PEDro score | Knees (n) | Follow-up (months) | Type of approach | Knees (n) | OA patients (%) | Female (%) | Mean age (years) | BMI (kg/m2) |
|---|---|---|---|---|---|---|---|---|---|---|
| Aglietti et al. [13] | RCT | 9 | 60 | 3.00 | MSV | 30 | 60.00 | 70.00 | 28.08 | |
| QS | 30 | 60.00 | 71.00 | 28.07 | ||||||
| Aslam et al. [14] | RCT | 10 | 84 | 12.00 | MMV | 42 | 100.00 | 30.00 | 68.80 | 30.60 |
| MPP | 42 | 100.00 | 57.14 | 68.60 | 30.10 | |||||
| Avci et al. [15] | RCS | 6 | 39 | 23.50 | MMV | 19 | 100.00 | 78.94 | 64.53 | 32.02 |
| MPP | 20 | 100.00 | 90.00 | 67.25 | 32.56 | |||||
| Boerger et al. [2] | PCS | 5 | 120 | 3.00 | MSV | 60 | 100.00 | 77.00 | 69.00 | 28.00 |
| MPP | 60 | 100.00 | 75.00 | 68.00 | 29.00 | |||||
| Bridgman et al. [16] | RCT | 7 | 224 | 13.00 | MSV | 113 | 48.00 | 70.10 | ||
| MPP | 111 | 49.00 | 70.90 | |||||||
| Bonutti et al. [17] | RCT | 9 | 102 | 24.00 | MSV | 51 | 84.00 | 70.00 | 31.00 | |
| MMV | 51 | 84.00 | 70.00 | 31.00 | ||||||
| Chalidis et al. [18] | RCT | 8 | 100 | 24.00 | MMV | 50 | 100.00 | 92.00 | 70.10 | 34.60 |
| MPP | 50 | 100.00 | 88.00 | 71.20 | 34.20 | |||||
| Chiang et al. [11] | RCT | 10 | 75 | 24.00 | QS | 38 | 100.00 | 90.00 | 69.70 | 28.60 |
| MPP | 37 | 100.00 | 90.00 | 69.80 | 29.60 | |||||
| Cho et al. [19] | RCT | 8 | 66 | 12.00 | MMV | 33 | 100.00 | 96.00 | 65.50 | 29.10 |
| MPP | 33 | 100.00 | 93.93 | 67.00 | 28.00 | |||||
| Dabboussi et al. [20] | PCS | 5 | 80 | 3.00 | MMV | 40 | 100.00 | |||
| MPP | 40 | 100.00 | ||||||||
| Feczko et al. [21] | RCT | 7 | 69 | 6.00 | MMV | 36 | 95.00 | 63.88 | 65.14 | 28.26 |
| MPP | 33 | 100.00 | 66.66 | 64.88 | 28.56 | |||||
| Han et al. [22] | RCT | 9 | 30 | 24.00 | MMPP | 15 | 100.00 | 66.00 | 26.90 | |
| MPP | 15 | 100.00 | 64.00 | 26.40 | ||||||
| Heekin et al. [23] | RCT | 9 | 80 | 24.00 | MMV | 40 | 14.00 | 65.13 | 30.98 | |
| MMPP | 40 | 35.00 | 65.13 | 30.98 | ||||||
| Hernandez-Vaquero et al. [24] | RCT | 7 | 62 | 6.00 | MMV | 26 | 100.00 | 80.77 | 70.80 | 32.10 |
| MPP | 36 | 100.00 | 80.33 | 70.50 | 30.80 | |||||
| Huang et al. [25] | RCS | 6 | 96 | 60.00 | MMPP | 35 | 100.00 | 85.71 | 69.20 | 27.00 |
| QS | 31 | 100.00 | 93.55 | 69.30 | 26.90 | |||||
| MPP | 30 | 100.00 | 93.33 | 71.20 | 26.70 | |||||
| Jarvis et al. [26] | RCT | 6 | 53 | 6.00 | MSV | 27 | 100.00 | 87.00 | 69.00 | 31.40 |
| MMV | 26 | 100.00 | 61.54 | 74.20 | 29.80 | |||||
| Jung et al. [27] | PCS | 6 | 40 | 58.40 | MSV | 21 | ||||
| MPP | 19 | |||||||||
| Juosponis et al. [28] | RCT | 8 | 70 | 3.00 | MMV | 35 | 100.00 | 85.71 | 72.00 | 27.95 |
| MPP | 35 | 100.00 | 85.71 | 71.40 | 29.08 | |||||
| Karachalios et al. [29] | RCT | 8 | 100 | 23.00 | MMV | 50 | 92.00 | 62.00 | 71.10 | 32.00 |
| MPP | 50 | 92.00 | 70.00 | 70.80 | 31.50 | |||||
| Karpman et al. [30] | RCT | 8 | 59 | 6.00 | MMV | 20 | 100.00 | 65.00 | 74.00 | 30.00 |
| QS | 20 | 100.00 | 60.00 | 73.00 | 28.00 | |||||
| MPP | 19 | 100.00 | 53.00 | 73.00 | 29.00 | |||||
| Kim [31] | RCT | 10 | 50 | 12.00 | MMV | 23 | 100.00 | 67.00 | 27.10 | |
| MPP | 22 | 100.00 | 68.00 | 28.40 | ||||||
| King et al. [32] | RCS | 5 | 150 | 1.50 | QS | 100 | 95.00 | 52.00 | 67.00 | 30.00 |
| MPP | 50 | 90.00 | 66.00 | 28.00 | 32.00 | |||||
| Laskin et al. [3] | RCS | 5 | 58 | 3.00 | MMV | 26 | 70.00 | 30.00 | ||
| MPP | 26 | 68.00 | 29.00 | |||||||
| Li et al. [33] | RCT | 8 | 50 | 12.00 | MSV | 25 | 100.00 | 64.00 | 69.90 | 25.80 |
| MPP | 25 | 100.00 | 64.00 | 68.10 | 25.50 | |||||
| Liebensteiner et al. [34] | PCS | 5 | 38 | 2.00 | MMV | 19 | 57.89 | 66.70 | 30.20 | |
| MPP | 19 | 52.63 | 67.60 | 31.50 | ||||||
| Lin et al. [35] | RCT | 9 | 80 | 2.00 | QS | 40 | 100.00 | 67.50 | 69.60 | 28.10 |
| MMPP | 40 | 100.00 | 67.50 | 70.20 | 29.00 | |||||
| Lin et al. [36] | RCT | 9 | 100 | 24.00 | QS | 35 | 100.00 | 86.00 | 67.70 | 26.30 |
| QS | 30 | 100.00 | 87.00 | 70.00 | 25.90 | |||||
| MMPP | 35 | 100.00 | 86.00 | 68.50 | 25.90 | |||||
| Liu et al. [37] | RCT | 8 | 90 | 24.00 | MMV | 45 | ||||
| MPP | 45 | |||||||||
| Maru et al. [38] | PCS | 6 | 77 | 3.00 | MMV | 37 | 100.00 | 51.35 | 71.00 | |
| MPP | 40 | 96.00 | 62.50 | 70.00 | ||||||
| McAllister et al. [39] | PCS | 7 | 180 | 13.00 | MMPP | 91 | 100.00 | 51.64 | 63.00 | |
| MPP | 89 | 100.00 | 49.43 | 63.00 | ||||||
| Mehta et al. [40] | RCT | 7 | 55 | 6.00 | MSV/MMV | 26 | 73.17 | 59.80 | ||
| MPP | 29 | 73.17 | 61.40 | |||||||
| Mukherjee et al. [41] | RCT | 8 | 100 | MMV | 20 | |||||
| MPP | 80 | |||||||||
| Nestor et al. [42] | RCT | 10 | 54 | 3.00 | MMV | 27 | 66.66 | 66.70 | 29.60 | |
| MPP | 27 | 66.66 | 66.70 | 29.60 | ||||||
| Nutton et al. [43] | RCT | 10 | 23 | 6.00 | MMV | 11 | 100.00 | 33.00 | 73.00 | 31.10 |
| MPP | 12 | 100.00 | 50.00 | 70.00 | 29.30 | |||||
| Pescador et al. [44] | RCT | 8 | 96 | 96.00 | MSV | 45 | 68.88 | 71.20 | 28.40 | |
| MPP | 51 | 72.55 | 69.30 | 27.90 | ||||||
| Pongcharoen et al. [45] | RCT | 8 | 60 | 12.00 | MMV | 30 | 100.00 | 83.33 | 67.00 | 27.00 |
| MPP | 30 | 100.00 | 69.69 | 67.00 | 26.00 | |||||
| Rahman et al. [46] | RCS | 5 | 120 | 3.00 | MMPP | 60 | 100.00 | 75.00 | 59.80 | |
| MPP | 60 | 100.00 | 77.00 | 62.00 | ||||||
| Schroer et al. [47] | PCS | 6 | 300 | 24.00 | QS | 150 | 62.00 | 71.00 | 31.00 | |
| MPP | 150 | 61.00 | 70.00 | 32.00 | ||||||
| Seon et al. [48] | PCS | 6 | 84 | 12.00 | MMV | 41 | 100.00 | 80.48 | 64.20 | |
| MPP | 43 | 100.00 | 76.74 | 64.20 | ||||||
| Dayton et al. [49], Stevens-Lapsley et al. [50] | RCT | 8 | 41 | 3.00 | MMPP | 22 | 100.00 | 54.00 | 64.60 | 30.50 |
| MPP | 19 | 45.00 | 64.00 | 31.30 | ||||||
| Tasker et al. [51] | RCT | 8 | 83 | 24.00 | MMV/MSV | 40 | 45.00 | 63.00 | 67.30 | |
| MPP | 43 | 99.00 | 63.00 | 68.20 | ||||||
| Tenholder et al. [52] | RCS | 6 | 118 | MMPP | 69 | 56.00 | 66.80 | 29.30 | ||
| MPP | 49 | 46.94 | 63.50 | 31.50 | ||||||
| Thienpont et al. [53] | RCT | 8 | 300 | 24.00 | MMPP | 150 | 100.00 | 66.66 | 68.00 | 30.40 |
| MPP | 150 | 100.00 | 70.00 | 69.00 | 29.8 | |||||
| Tsuji et al. [54] | PCS | 5 | 20 | 0.50 | MMV | 10 | 100.00 | 60.00 | 68.40 | 28.10 |
| MPP | 10 | 100.00 | 80.00 | 69.80 | 28.90 | |||||
| Unnanuntana et al. [55] | RCS | 6 | 64 | 60.00 | MMPP | 31 | ||||
| MPP | 57 | |||||||||
| Unwin et al. [56] | RCT | 8 | 66 | 72.00 | MMV/MSV | 32 | 75.75 | 67.00 | ||
| MPP | 34 | 75.75 | 67.00 | |||||||
| Varela-Egocheaga et al. [57] | RCT | 8 | 100 | 36.00 | MSV | 50 | 72.00 | 68.02 | 30.97 | |
| MPP | 50 | 74.00 | 70.64 | 30.62 | ||||||
| Watanabe et al. [58] | RCS | 6 | 48 | 48.00 | MMV | 25 | 84.00 | 80.00 | 71.00 | 28.10 |
| MPP | 23 | 78.00 | 73.91 | 71.00 | 26.30 | |||||
| Wegrzyn et al. [59] | RCT | 10 | 36 | 2.00 | MSV | 18 | 100.00 | 72.00 | 67.00 | 30.00 |
| MPP | 18 | 100.00 | 72.00 | 64.00 | 31.00 | |||||
| Wülker et al. [60] | RCT | 8 | 134 | 12.00 | MSV | 66 | 92.00 | 72.70 | 70.20 | 29.30 |
| MPP | 68 | 88.00 | 70.10 | 29.30 | ||||||
| Zhang et al. [61] | RCT | 8 | 82 | 12.00 | MPP | 40 | 54.00 | 65.90 | 26.20 | |
| MMPP | 42 | 50.00 | 64.50 | 24.90 | ||||||
| Zhu et al. [62] | PCS | 6 | 67 | 109.20 | MMPP | 30 | 93.30 | 67.90 | 27.60 | |
| MPP | 37 | 83.80 | 65.30 | 27.70 |
MPP medial parapatellar, MMPP mini-medial parapatellar, QS quadriceps sparing, MMV mini-midvastus, MSV mini-subvastus
Patient demographics
Data from 4533 patients were collected. The mean follow-up was 20.38 (range 3 to 109) months. In the MVV group, a total of 880 patients were analysed. 96% suffered from OA, and 67% were female. Their mean age was 68.64 ± 3.5 years, and mean BMI was 29.46 ± 1.7 kg/m2. In the MPP group, a total of 2026 patients were analysed. 98% suffered from OA, and 69% were female. The mean age was 66.27 ± 7.9 years, and mean BMI was 29.29 ± 1.9 kg/m2. In the MSV group, a total of 604 patients were analysed. 90% suffered from OA, and 70% were female. The mean age was 67.72 ± 3.1 years, and the mean BMI was 29.61 ± 1.5 kg/m2. In the MMPP group, a total of 660 patients were analysed. 100% suffered from OA, and 66% were female. The mean age was 66.31 ± 2.5 years, and mean BMI was 28.00 ± 2.4 kg/m2. In the QS group, a total of 474 patients were analysed. 99% suffered from OA, and 73% were female. The mean age was 70.13 ± 1.9 years, and mean BMI was 29.03 ± 1.4 kg/m2. Among the studies, with regard to diagnosis, gender, age and BMI, adequate baseline comparability was detected (P = 0.7, P = 0.8, P = 0.9, P = 0.8, respectively). Patient demographics for the included studies are shown in Table 1.
Outcomes of interest
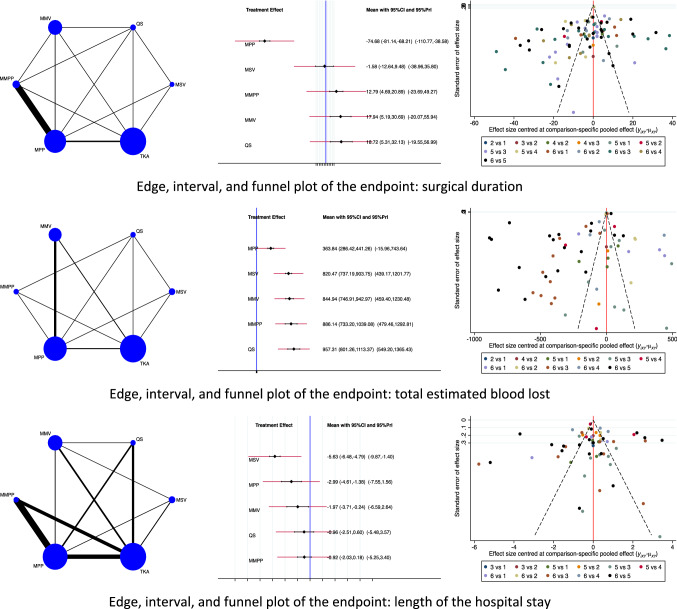
Concerning perioperative data, the MSV approach demonstrated the lowest duration of hospitalization (EE: − 5.63, 95% CI: − 6.48 to − 4.79), followed by the MPP approach (EE: − 2.99, 95% CI: − 4.61 to − 1.38). The MMPP approach reported the highest duration of hospitalization (EE: − 0.92, 95% CI: − 2.03 to 0.18). The test for overall inconsistency scored P = 0.2. The MPP approach demonstrated the lowest value of total estimated blood loss (EE: 363.84, 95% CI: 286.42 to 441.26) followed by the MSV approach (EE: 820.47, 95% CI: 737.19 to 903.75). The QS approach reported the greatest value of total estimated blood loss (EE: 957.31, 95% CI: 801.26 to 1113.37). The test for overall inconsistency scored P = 0.9. The MPP approach demonstrated the shortest surgical duration (EE: − 74.68, 95% CI: − 81.14 to − 68.21) followed by the MPP approach (EE: − 1.58, 95% CI: − 12.64 to 9.48). The QS approach reported the longest surgical duration (EE: 18.72, 95% CI: 5.31 to 32.13). The test for overall inconsistency scored P = 0.9. The network results concerning the endpoint perioperative data are shown in Fig. 2.
Fig. 2.
Results of the network comparison perioperative data
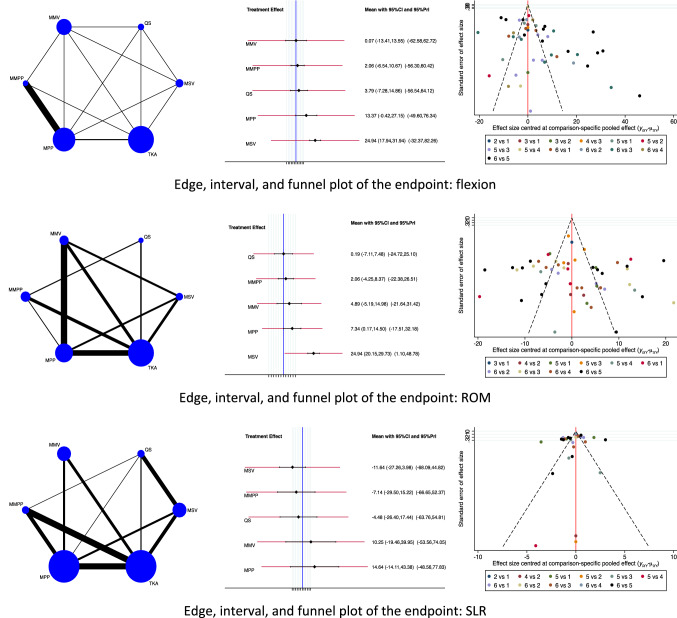
Regarding the functional outcomes, the MSV approach detected the greatest degree of flexion (EE: 24.94, 95% CI: 17.94 to 31.94) followed by the MPP approach (EE: 13.37, 95% CI: − 0.42 to 27.15). The MMV approach reported the lowest degree of flexion (EE: 0.07, 95% CI: − 13.41 to 13.55). The test for overall inconsistency scored P = 0.3. The MSV approach detected the greatest ROM (EE: 24.94, 95% CI: 20.15 to 29.73) followed by the MPP approach (EE: 7.34, 95% CI: 0.17 to 14.50). The QS approach reported the lowest ROM (EE: 0.19, 95% CI: − 7.11 to 7.48). The test for overall inconsistency scored P = 0.5. The MSV approach demonstrated the shortest SLR (EE: − 11.64, 95% CI: − 27.26 to 3.98) followed by the MMPP approach (EE: − 7.14, 95% CI: − 29.50 to 15.22). The MPP approach reported the longest SLR (EE: 14.64, 95% CI: − 14.11 to 43.38). The test for overall inconsistency scored P = 0.6. The network results concerning the endpoint functional outcomes are shown in Fig. 3.
Fig. 3.
Results of the network comparison functional outcomes
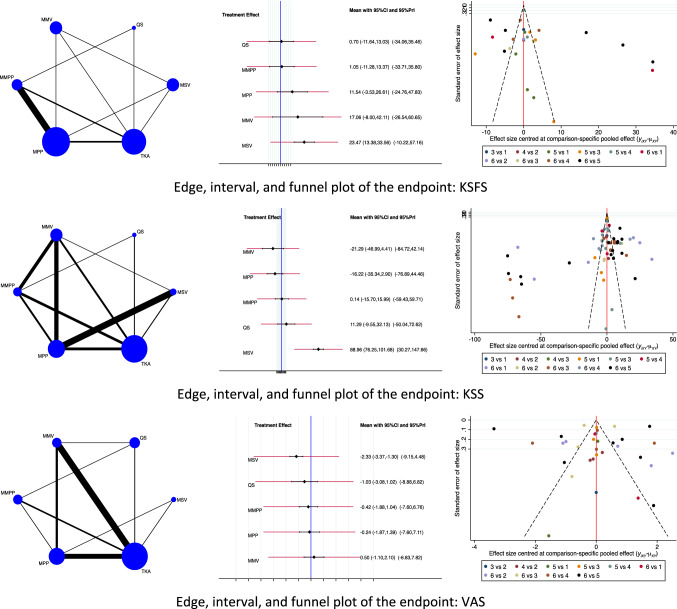
Concerning the clinical scores, the MSV approach demonstrated the highest KSFS scores (EE: 23.47, 95% CI: 13.38 to 33.56) followed by the MMV approach (EE: 17.06, 95% CI: − 8.00 to 42.11). The QS approach reported the lowest value of KSFS (EE: 0.70, 95% CI: − 11.64 to 13.03). The test for overall inconsistency scored P = 0.7. The MSV approach demonstrated the highest KSS scores (EE: 88.96, 95% CI: 76.25 to 101.68) followed by the QS approach (EE: 11.29, 95% CI: − 9.55 to 32.13). The MMV approach reported the lowest KSS scores (EE: − 21.29, 95% CI: − 46.99 to 4.41). The test for overall inconsistency scored P = 0.4. The MSV approach demonstrated the lowest VAS pain score (EE: − 2.33, 95% CI: − 3.37 to − 2.30) followed by the QS approach (EE: − 1.03, 95% CI: − 3.08 to 1.02). The MMV approach reported the highest value of VAS (EE: 0.50, 95% CI: − 1.10 to 2.10). The test for overall inconsistency scored P = 0.05. The network results concerning the endpoint clinical scores are shown in Fig. 4.
Fig. 4.
Results of the network comparison clinical scores
Discussion
The main results of this Bayesian network meta-analysis encourage to perform the minimally invasive subvastus approach for total knee arthroplasty. Concerning clinical scores, functional outcomes and length of the hospital stay, the MSV approach outperformed all other approaches. Surgical duration and total estimated blood loss were lower in the MPP approach. The transitivity between studies was always satisfied, and the equation for global linearity via the Wald test found no statistically significant inconsistency among the studies, attesting reliability of the present results.
The intention of the minimally invasive approaches is to provide quicker recovery after TKA by preventing damage to the extensor mechanism. However, the MPP demonstrated a very short length of the hospital stay compared to the other minimally invasive techniques. Regarding perioperative outcomes, the QS approach reported the longest surgical duration and the highest value of total estimated blood loss. This can be explained by the reduced joint exposure of minimally invasive surgeries compared with the traditional approach. Peersman et al. [63], in a retrospective cohort study including 6489 patients, found correlation between an increased surgical duration and an augmented risk of surgical site infection during TKA. Reduced visibility can considerably complicate component installation, prolong the learning curve and generate skin sloughs [52, 64]. The QS approach especially requires more attention to retractor positioning, since they damage bones (particularly when osteoporotic) and soft tissue [13, 30]. The advantage of the QS approach is that it can be easily converted to MMPP or MPP [13].
Concerning clinical scores (KSS, KSFS, VAS), the MSV approach performed better overall. The equation for global linearity via the Wald test evidenced no statistically significant inconsistency among the studies. Thus, the assumption of transitivity can be accepted. The MMV reported the lowest value of KSS and VAS, while the QS the lowest KSFS. Concerning functional outcomes (SLR, ROM, flexion), the MSV approach performed better overall. No statistically significant inconsistency was found through the equation for global linearity via the Wald test; therefore, transitivity between the studies is assumed. As expected, the MPP evidenced the longest SLR, while the MMV the lowest degree of flexion and the QS the lowest ROM.
One of the purposes of minimally invasive TKA is to reduce damage to the quadriceps tendon, in order to guarantee quicker recovery of the extensor mechanism function. The straight leg raise (SLR) is used to assess quadriceps restoration after TKA [65, 66]. SLR times were longer in the traditional MPP group and strongly improved in the other approaches, especially in the MSV approach, confirming reduced damage to the extensor mechanism in these approaches. Several studies have tried to quantify quadriceps destruction in minimally invasive TKA versus the traditional MPP using levels biomarkers indicative of muscle damage (e.g. creatine kinase, interleukin-6, myoglobin). However, their results are contrasting and controversial [67–69].
Comparing the traditional MPP to the other approaches for TKA, we highlight multiple advantages and disadvantages. First, all the other approaches provide a minimally invasive surgery. Second, they aim to preserve patellar vascularization [68], which can reduce the occurrence of patellar fractures, avascular necrosis, subluxations, dislocations, component loosening and rates of anterior knee pain [5, 7]. Third, they are supposed to promote quicker recovery of the quadriceps function and decreased post-operative pain [70, 71]. The MSV, along with the MMV, preserves the vastus medialis insertion [47, 72] and potentially reduces the risk of VMO denervation [71, 73]. Pagnano et al. [74] in a cadaveric study demonstrated that the VMO tendon inserts mostly down to the mild pole of the patella, thus proving that the MSV is the only approach able to preserve the VMO insertion on the patella. Furthermore, the MSV proximally avoids an incision to the descending genicular artery branches (musculoarticular branch) [75, 76]. Fourth, the MSV and MMV almost never require a lateral release [72, 77]. Lateral retinacular release during TKA is not fully understood. It is meant to improve patellar tracking, but can also damage patellar vascularization and reduce joint stability [78, 79]. However, due to difficult execution, a longer learning curve and the need for special instruments, it has not been very popular [13, 80]. The difficulty of execution can result in ligament–patellar maltracking, increased rates of polyethylene wear, loosening, imbalance and instability [81, 82]. To assist the surgeon, the use of a mobile window can facilitate exposure of knee surfaces and dedicated instrumentation should be considered [28, 42]. Not surprisingly, previous studies confirm that the MPP exposure is related to an optimal component positioning [35, 83, 84]. This has discouraged many surgeons from performing minimally invasive TKAs, and the MPP remains the most common approach for TKA. Indeed, our results evidenced that the MPP exposure required less surgical duration and lower estimated blood loss. However, we hypothesize that these results are strongly influenced by the learning curve.
This Bayesian network meta-analysis has several limitations. As previously mentioned, due to reduced visibility and augmented difficulties of installation, minimally invasive TKAs can result in implant malposition. Notwithstanding, implant positioning has not been evaluated, thus representing an important limitation of this study. Implant malposition relates to instability, loosening and consequent joint failure. Further studies should clarify this important endpoint. Another notable limitation of the present study is its lack of analysis for complications. This is due to a lack of data in the included studies under these endpoints. Further studies should implement analyses of complications and evaluate the feasibility of minimally invasive surgeries, especially when it comes to obese patients and patients with previous knee surgeries (e.g. high tibial osteotomies). Points of strength in this Bayesian network meta-analysis are the comprehensive nature of the literature search and the optimal baseline comparability, along with the high number of enrolled studies. To the best of our knowledge, this study represents the first study comparing multiple surgical approaches for TKA. Data from the present network analysis provide evidence in favour of the mini-subvastus approach for total knee arthroplasty. However, the present study represents a data statistical elaboration and, therefore, must be interpreted with caution.
Conclusion
According to the main findings of the present study, the mini-subvastus approach for total knee arthroplasty demonstrated superior overall compared to the other approaches. Orthopaedic surgeons should consider this approach in the light of the evidence and limitations of this Bayesian network meta-analysis.
Funding
Open Access funding enabled and organized by Projekt DEAL. No external source of funding was used.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, informed consent is not required.
Footnotes
The original online version of this article was revised due to a retrospective Open Access order.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
6/14/2021
A Correction to this paper has been published: 10.1007/s00590-021-03026-9
References
- 1.Langenbeck B. Zur Resection des Kniegelenks. Verhandlungen der Deutschen Gesellschaft für Chirurgie. 1878;8:23. [Google Scholar]
- 2.Boerger TO, Aglietti P, Mondanelli N, Sensi L. Mini-subvastus versus medial parapatellar approach in total knee arthroplasty. Clin Orthop Relat Res. 2005;440:82–87. doi: 10.1097/01.blo.0000185755.09777.2d. [DOI] [PubMed] [Google Scholar]
- 3.Laskin RS, Beksac B, Phongjunakorn A, Pittors K, Davis J, Shim JC, Pavlov H, Petersen M. Minimally invasive total knee replacement through a mini-midvastus incision: an outcome study. Clin Orthop Relat Res. 2004;428:74–81. doi: 10.1097/01.blo.0000148582.86102.47. [DOI] [PubMed] [Google Scholar]
- 4.Repicci JA, Eberle RW. Minimally invasive surgical technique for unicondylar knee arthroplasty. J South Orthop Assoc. 1999;8(1):20–27. [PubMed] [Google Scholar]
- 5.Hofmann AA, Plaster RL, Murdock LE. Subvastus (Southern) approach for primary total knee arthroplasty. Clin Orthop Relat Res. 1991;269:70–77. [PubMed] [Google Scholar]
- 6.Engh GA, Holt BT, Parks NL. A midvastus muscle-splitting approach for total knee arthroplasty. J Arthroplasty. 1997;12(3):322–331. doi: 10.1016/S0883-5403(97)90030-9. [DOI] [PubMed] [Google Scholar]
- 7.Tria AJ, Jr, Coon TM. Minimal incision total knee arthroplasty: early experience. Clin Orthop Relat Res. 2003;416:185–190. doi: 10.1097/01.blo.0000093030.56370.d9. [DOI] [PubMed] [Google Scholar]
- 8.Scuderi GR, Tenholder M, Capeci C. Surgical approaches in mini-incision total knee arthroplasty. Clin Orthop Relat Res. 2004;428:61–67. doi: 10.1097/01.blo.0000148574.79874.d0. [DOI] [PubMed] [Google Scholar]
- 9.Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, Mulrow C, Catala-Lopez F, Gotzsche PC, Dickersin K, Boutron I, Altman DG, Moher D. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 10.Urban LM. The straight-leg-raising test: a review. J Orthop Sports Phys Ther. 1981;2(3):117–133. doi: 10.2519/jospt.1981.2.3.117. [DOI] [PubMed] [Google Scholar]
- 11.Migliorini F, Eschweiler J, Tingart M, Rath B. Posterior-stabilized versus cruciate-retained implants for total knee arthroplasty: a meta-analysis of clinical trials. Eur J Orthop Surg Traumatol. 2019;29(4):937–946. doi: 10.1007/s00590-019-02370-1. [DOI] [PubMed] [Google Scholar]
- 12.de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55(2):129–133. doi: 10.1016/S0004-9514(09)70043-1. [DOI] [PubMed] [Google Scholar]
- 13.Aglietti P, Baldini A, Sensi L. Quadriceps-sparing versus mini-subvastus approach in total knee arthroplasty. Clin Orthop Relat Res. 2006;452:106–111. doi: 10.1097/01.blo.0000238789.51972.16. [DOI] [PubMed] [Google Scholar]
- 14.Aslam MA, Sabir AB, Tiwari V, Abbas S, Tiwari A, Singh P. Approach to total knee replacement: a randomized double blind study between medial parapatellar and midvastus approach in the early postoperative period in asian population. J Knee Surg. 2017;30(8):793–797. doi: 10.1055/s-0036-1597978. [DOI] [PubMed] [Google Scholar]
- 15.Avci CC, Gulabi D, Erdem M, Kurnaz R, Gunes T, Bostan B. Minimal invasive midvastus versus standard parapatellar approach in total knee arthroplasty. Acta Orthop Traumatol Turc. 2013;47(1):1–7. doi: 10.3944/AOTT.2013.2801. [DOI] [PubMed] [Google Scholar]
- 16.Bridgman SA, Walley G, MacKenzie G, Clement D, Griffiths D, Maffulli N. Sub-vastus approach is more effective than a medial parapatellar approach in primary total knee arthroplasty: a randomized controlled trial. Knee. 2009;16(3):216–222. doi: 10.1016/j.knee.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 17.Bonutti PM, Zywiel MG, Ulrich SD, Stroh DA, Seyler TM, Mont MA. A comparison of subvastus and midvastus approaches in minimally invasive total knee arthroplasty. J Bone Jt Surg Am. 2010;92(3):575–582. doi: 10.2106/JBJS.I.00268. [DOI] [PubMed] [Google Scholar]
- 18.Chalidis BE, Petsatodis G, Christodoulou AG, Christoforidis J, Papadopoulos PP, Pournaras J. Is obesity a contraindication for minimal invasive total knee replacement? A prospective randomized control trial. Obes Surg. 2010;20(12):1633–1641. doi: 10.1007/s11695-009-9968-6. [DOI] [PubMed] [Google Scholar]
- 19.Cho KY, Kim KI, Umrani S, Kim SH. Better quadriceps recovery after minimally invasive total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1759–1764. doi: 10.1007/s00167-013-2556-2. [DOI] [PubMed] [Google Scholar]
- 20.Dabboussi N, Sakr M, Girard J, Fakih R. Minimally invasive total knee arthroplasty: a comparative study to the standard approach. N Am J Med Sci. 2012;4(2):81–85. doi: 10.4103/1947-2714.93381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feczko P, Engelmann L, Arts JJ, Campbell D. Computer-assisted total knee arthroplasty using mini midvastus or medial parapatellar approach technique: a prospective, randomized, international multicentre trial. BMC Musculoskelet Disord. 2016;17:19. doi: 10.1186/s12891-016-0872-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Han I, Seong SC, Lee S, Yoo JH, Lee MC. Simultaneous bilateral MIS-TKA results in faster functional recovery. Clin Orthop Relat Res. 2008;466(6):1449–1453. doi: 10.1007/s11999-008-0216-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heekin RD, Fokin AA. Mini-midvastus versus mini-medial parapatellar approach for minimally invasive total knee arthroplasty: outcomes pendulum is at equilibrium. J Arthroplasty. 2014;29(2):339–342. doi: 10.1016/j.arth.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 24.Hernandez-Vaquero D, Noriega-Fernandez A, Suarez-Vazquez A. Total knee arthroplasties performed with a mini-incision or a standard incision. Similar results at six months follow-up. BMC Musculoskelet Disord. 2010;11:27. doi: 10.1186/1471-2474-11-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang AB, Wang HJ, Yu JK, Yang B, Ma D, Zhang JY. Are there any clinical and radiographic differences between quadriceps-sparing and mini-medial parapatellar approaches in total knee arthroplasty after a minimum 5 years of follow-up? Chin Med J (Engl) 2015;128(14):1898–1904. doi: 10.4103/0366-6999.160521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jarvis SL, Onstot BR, Bhowmik-Stoker M, Jacofsky MC, Jacofsky DJ. Differences between midvastus and subvastus TKA surgical approaches in the tasks of sitting and standing. J Knee Surg. 2013;26(5):333–341. doi: 10.1055/s-0033-1333904. [DOI] [PubMed] [Google Scholar]
- 27.Jung YB, Lee YS, Lee EY, Jung HJ, Nam CH. Comparison of the modified subvastus and medial parapatellar approaches in total knee arthroplasty. Int Orthop. 2009;33(2):419–423. doi: 10.1007/s00264-007-0510-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Juosponis R, Tarasevicius S, Smailys A, Kalesinskas RJ. Functional and radiological outcome after total knee replacement performed with mini-midvastus or conventional arthrotomy: controlled randomised trial. Int Orthop. 2009;33(5):1233–1237. doi: 10.1007/s00264-008-0630-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karachalios T, Giotikas D, Roidis N, Poultsides L, Bargiotas K, Malizos KN. Total knee replacement performed with either a mini-midvastus or a standard approach: a prospective randomised clinical and radiological trial. J Bone Jt Surg Br. 2008;90(5):584–591. doi: 10.1302/0301-620X.90B5.20122. [DOI] [PubMed] [Google Scholar]
- 30.Karpman RR, Smith HL. Comparison of the early results of minimally invasive vs standard approaches to total knee arthroplasty: a prospective, randomized study. J Arthroplasty. 2009;24(5):681–688. doi: 10.1016/j.arth.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 31.Kim JG, Lee SW, Ha JK, Choi HJ, Yang SJ, Lee MY. The effectiveness of minimally invasive total knee arthroplasty to preserve quadriceps strength: a randomized controlled trial. Knee. 2011;18(6):443–447. doi: 10.1016/j.knee.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 32.King J, Stamper DL, Schaad DC, Leopold SS. Minimally invasive total knee arthroplasty compared with traditional total knee arthroplasty. Assessment of the learning curve and the postoperative recuperative period. J Bone Jt Surg Am. 2007;89(7):1497–1503. doi: 10.2106/jbjs.f.00867. [DOI] [PubMed] [Google Scholar]
- 33.Li Z, Cheng W, Sun L, Yao Y, Cao Q, Ye S, Qi L, Xu S, Wu X, Jing J. Mini-subvastus versus medial parapatellar approach for total knee arthroplasty: a prospective randomized controlled study. Int Orthop. 2018;42(3):543–549. doi: 10.1007/s00264-017-3703-z. [DOI] [PubMed] [Google Scholar]
- 34.Liebensteiner MC, Krismer M, Koller A, Semenitz B, Mayr E. Does minimally invasive total knee arthroplasty improve isokinetic torque? Clin Orthop Relat Res. 2012;470(11):3233–3239. doi: 10.1007/s11999-012-2545-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin WP, Lin J, Horng LC, Chang SM, Jiang CC. Quadriceps-sparing, minimal-incision total knee arthroplasty: a comparative study. J Arthroplasty. 2009;24(7):1024–1032. doi: 10.1016/j.arth.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 36.Lin SY, Chen CH, Fu YC, Huang PJ, Lu CC, Su JY, Chang JK, Huang HT. Comparison of the clinical and radiological outcomes of three minimally invasive techniques for total knee replacement at two years. Bone Jt J. 2013;95(7):906–910. doi: 10.1302/0301-620x.95b7.29694. [DOI] [PubMed] [Google Scholar]
- 37.Liu H, Mei X, Zhang Z, Sun J. Mini-midvastus versus mini-medial parapatellar approach in simultaneous bilateral total knee arthroplasty with 24-month follow-up. Acta Orthop Traumatol Turc. 2015;49(6):586–592. doi: 10.3944/AOTT.2015.15.0078. [DOI] [PubMed] [Google Scholar]
- 38.Maru M, Akra G, McMurtry I, Port A. A prospective comparative study of the midvastus and medial parapatellar approaches for total knee arthroplasty in the early postoperative period. Eur J Orthop Surg Traumatol. 2009;19(7):473–476. doi: 10.1007/s00590-009-0452-8. [DOI] [Google Scholar]
- 39.McAllister CM, Stepanian JD. The impact of minimally invasive surgical techniques on early range of motion after primary total knee arthroplasty. J Arthroplasty. 2008;23(1):10–18. doi: 10.1016/j.arth.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 40.Mehta NBM, Goyal A, Mishra P, Joshi D, Chaudhary D. Quadriceps sparing (subvastus/midvastus) approach versus the conventional medial parapatellar approach in primary knee arthroplasty. J Arthrosc J Surg. 2017;4(1):15–20. doi: 10.1016/j.jajs.2017.02.004. [DOI] [Google Scholar]
- 41.Mukherjee P, Press J, Hockings M. Mid-vastus vs medial para-patellar approach in tota knee replacement—time to discharge. Iowa Orthop J. 2009;29:19–22. [PMC free article] [PubMed] [Google Scholar]
- 42.Nestor BJ, Toulson CE, Backus SI, Lyman SL, Foote KL, Windsor RE. Mini-midvastus vs standard medial parapatellar approach: a prospective, randomized, double-blinded study in patients undergoing bilateral total knee arthroplasty. J Arthroplasty. 2010;25(6 Suppl):5–11. doi: 10.1016/j.arth.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 43.Nutton RW, Wade FA, Coutts FJ, van der Linden ML. Short term recovery of function following total knee arthroplasty: a randomised study of the medial parapatellar and midvastus approaches. Arthritis. 2014;2014:173857. doi: 10.1155/2014/173857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pescador D, Moreno AA, Blanco JF, Garcia I. Long-term analysis of minimally invasive surgery in knee arthroplasty. Acta Ortop Mex. 2011;25(6):353–358. [PubMed] [Google Scholar]
- 45.Pongcharoen B, Yakampor T, Charoencholvanish K. Patellar tracking and anterior knee pain are similar after medial parapatellar and midvastus approaches in minimally invasive TKA. Clin Orthop Relat Res. 2013;471(5):1654–1660. doi: 10.1007/s11999-012-2778-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rahman OAM. Less invasive versus standard total knee replacement: comparison of early outcome. J Pak Med Assoc. 2015;65:82–86. [PubMed] [Google Scholar]
- 47.Schroer WC, Diesfeld PJ, Reedy ME, LeMarr AR. Mini-subvastus approach for total knee arthroplasty. J Arthroplasty. 2008;23(1):19–25. doi: 10.1016/j.arth.2006.12.100. [DOI] [PubMed] [Google Scholar]
- 48.Seon JK, Song EK, Yoon TR, Park SJ, Bae BH, Cho SG. Comparison of functional results with navigation-assisted minimally invasive and conventional techniques in bilateral total knee arthroplasty. Comput Aided Surg. 2007;12(3):189–193. doi: 10.1080/10929080701311861. [DOI] [PubMed] [Google Scholar]
- 49.Dayton MR, Bade MJ, Muratore T, Shulman BC, Kohrt WM, Stevens-Lapsley JE. Minimally invasive total knee arthroplasty: surgical implications for recovery. J Knee Surg. 2013;26(3):195–201. doi: 10.1055/s-0032-1327449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stevens-Lapsley JE, Bade MJ, Shulman BC, Kohrt WM, Dayton MR. Minimally invasive total knee arthroplasty improves early knee strength but not functional performance: a randomized controlled trial. J Arthroplasty. 2012;27(10):1812–1819. doi: 10.1016/j.arth.2012.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tasker A, Hassaballa M, Murray J, Lancaster S, Artz N, Harries W, Porteous A. Minimally invasive total knee arthroplasty; a pragmatic randomised controlled trial reporting outcomes up to 2 year follow up. Knee. 2014;21(1):189–193. doi: 10.1016/j.knee.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 52.Tenholder M, Clarke HD, Scuderi GR. Minimal-incision total knee arthroplasty: the early clinical experience. Clin Orthop Relat Res. 2005;440:67–76. doi: 10.1097/01.blo.0000185450.89364.10. [DOI] [PubMed] [Google Scholar]
- 53.Thienpont E. Faster recovery after minimally invasive surgery in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2412–2417. doi: 10.1007/s00167-012-1978-6. [DOI] [PubMed] [Google Scholar]
- 54.Tsuji S, Tomita T, Fujii M, Laskin RS, Yoshikawa H, Sugamoto K. Is minimally invasive surgery-total knee arthroplasty truly less invasive than standard total knee arthroplasty? A quantitative evaluation. J Arthroplasty. 2010;25(6):970–976. doi: 10.1016/j.arth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 55.Unnanuntana A, Pornrattanamaneewong C, Mow CS. Minimally invasive and standard total knee arthroplasty result in similar clinical outcomes at a minimum of five-year follow-up. J Med Assoc Thail. 2012;95(Suppl 9):S29–S35. [PubMed] [Google Scholar]
- 56.Unwin O, Hassaballa M, Murray J, Harries W, Porteous A. Minimally invasive surgery (MIS) for total knee replacement; medium term results with minimum five year follow-up. Knee. 2017;24(2):454–459. doi: 10.1016/j.knee.2017.01.010. [DOI] [PubMed] [Google Scholar]
- 57.Varela-Egocheaga JR, Suarez-Suarez MA, Fernandez-Villan M, Gonzalez-Sastre V, Varela-Gomez JR, Rodriguez-Merchan C. Minimally invasive subvastus approach: improving the results of total knee arthroplasty: a prospective, randomized trial. Clin Orthop Relat Res. 2010;468(5):1200–1208. doi: 10.1007/s11999-009-1160-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Watanabe T, Muneta T, Ishizuki M. Is a minimally invasive approach superior to a conventional approach for total knee arthroplasty? Early outcome and 2- to 4-year follow-up. J Orthop Sci. 2009;14(5):589–595. doi: 10.1007/s00776-009-1383-2. [DOI] [PubMed] [Google Scholar]
- 59.Wegrzyn J, Parratte S, Coleman-Wood K, Kaufman KR, Pagnano MW. The John Insall award: no benefit of minimally invasive TKA on gait and strength outcomes: a randomized controlled trial. Clin Orthop Relat Res. 2013;471(1):46–55. doi: 10.1007/s11999-012-2486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wulker N, Lambermont JP, Sacchetti L, Lazaro JG, Nardi J. A prospective randomized study of minimally invasive total knee arthroplasty compared with conventional surgery. J Bone Jt Surg Am. 2010;92(7):1584–1590. doi: 10.2106/JBJS.H.01070. [DOI] [PubMed] [Google Scholar]
- 61.Zhang Z, Gu B, Zhu W, Zhu L, Li Q, Du Y. Minimally invasive and computer-assisted total knee arthroplasty versus conventional technique: a prospective, randomized study. Eur J Orthop Surg Traumatol. 2014;24(8):1475–1479. doi: 10.1007/s00590-013-1313-z. [DOI] [PubMed] [Google Scholar]
- 62.Zhu M, Ang CL, Yeo SJ, Lo NN, Chia SL, Chong HC. Minimally invasive computer-assisted total knee arthroplasty compared with conventional total knee arthroplasty: a prospective 9-year follow-up. J Arthroplasty. 2016;31(5):1000–1004. doi: 10.1016/j.arth.2015.11.023. [DOI] [PubMed] [Google Scholar]
- 63.Peersman G, Laskin R, Davis J, Peterson MG, Richart T. Prolonged operative time correlates with increased infection rate after total knee arthroplasty. HSS J. 2006;2(1):70–72. doi: 10.1007/s11420-005-0130-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dalury DF, Dennis DA. Mini-incision total knee arthroplasty can increase risk of component malalignment. Clin Orthop Relat Res. 2005;440:77–81. doi: 10.1097/01.blo.0000185757.17401.7b. [DOI] [PubMed] [Google Scholar]
- 65.Cheng T, Liu T, Zhang G, Peng X, Zhang X. Does minimally invasive surgery improve short-term recovery in total knee arthroplasty? Clin Orthop Relat Res. 2010;468(6):1635–1648. doi: 10.1007/s11999-010-1285-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zan P, Wu Z, Yu X, Fan L, Xu T, Li G. The effect of patella eversion on clinical outcome measures in simultaneous bilateral total knee arthroplasty: a prospective randomized controlled trial. J Arthroplasty. 2016;31(3):637–640. doi: 10.1016/j.arth.2015.09.040. [DOI] [PubMed] [Google Scholar]
- 67.Wohlrab D, Gutteck N, Hildebrand M, Zeh A, Hein W. Influence of the surgical approach on postoperative rehabilitation after TKA. Z Orthop Unfallchirurgie. 2008;146(2):200–205. doi: 10.1055/s-2008-1038398. [DOI] [PubMed] [Google Scholar]
- 68.Niki Y, Mochizuki T, Momohara S, Saito S, Toyama Y, Matsumoto H. Is minimally invasive surgery in total knee arthroplasty really minimally invasive surgery? J Arthroplasty. 2009;24(4):499–504. doi: 10.1016/j.arth.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 69.Huang Z, Shen B, Ma J, Yang J, Zhou Z, Kang P, Pei F. Mini-midvastus versus medial parapatellar approach in TKA: muscle damage and inflammation markers. Orthopedics. 2012;35(7):e1038–e1045. doi: 10.3928/01477447-20120621-17. [DOI] [PubMed] [Google Scholar]
- 70.Cila E, Guzel V, Ozalay M, Tan J, Simsek SA, Kanatli U, Ozturk A. Subvastus versus medial parapatellar approach in total knee arthroplasty. Arch Orthop Trauma Surg. 2002;122(2):65–68. doi: 10.1007/s004020100319. [DOI] [PubMed] [Google Scholar]
- 71.Engh GA, Parks NL. Surgical technique of the midvastus arthrotomy. Clin Orthop Relat Res. 1998;351:270–274. doi: 10.1097/00003086-199806000-00032. [DOI] [PubMed] [Google Scholar]
- 72.Pan WM, Li XG, Tang TS, Qian ZL, Zhang Q, Zhang CM. Mini-subvastus versus a standard approach in total knee arthroplasty: a prospective, randomized, controlled study. J Int Med Res. 2010;38(3):890–900. doi: 10.1177/147323001003800315. [DOI] [PubMed] [Google Scholar]
- 73.Jojima H, Whiteside LA, Ogata K. Anatomic consideration of nerve supply to the vastus medialis in knee surgery. Clin Orthop Relat Res. 2004;423:157–160. doi: 10.1097/01.blo.0000128642.61260.b3. [DOI] [PubMed] [Google Scholar]
- 74.Pagnano MW, Meneghini RM, Trousdale RT. Anatomy of the extensor mechanism in reference to quadriceps-sparing TKA. Clin Orthop Relat Res. 2006;452:102–105. doi: 10.1097/01.blo.0000238788.44349.0f. [DOI] [PubMed] [Google Scholar]
- 75.Faure BT, Benjamin JB, Lindsey B, Volz RG, Schutte D. Comparison of the subvastus and paramedian surgical approaches in bilateral knee arthroplasty. J Arthroplasty. 1993;8(5):511–516. doi: 10.1016/S0883-5403(06)80216-0. [DOI] [PubMed] [Google Scholar]
- 76.Scheibel MT, Schmidt W, Thomas M, von Salis-Soglio G. A detailed anatomical description of the subvastus region and its clinical relevance for the subvastus approach in total knee arthroplasty. Surg Radiol Anat. 2002;24(1):6–12. doi: 10.1007/s00276-002-0004-y. [DOI] [PubMed] [Google Scholar]
- 77.Alcelik I, Sukeik M, Pollock R, Misra A, Naguib A, Haddad FS. Comparing the mid-vastus and medial parapatellar approaches in total knee arthroplasty: a meta-analysis of short term outcomes. Knee. 2012;19(4):229–236. doi: 10.1016/j.knee.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 78.Ritter MA, Herbst SA, Keating EM, Faris PM, Meding JB. Patellofemoral complications following total knee arthroplasty. Effect of a lateral release and sacrifice of the superior lateral geniculate artery. J Arthroplasty. 1996;11(4):368–372. doi: 10.1016/S0883-5403(96)80024-6. [DOI] [PubMed] [Google Scholar]
- 79.Archibeck MJ, Camarata D, Trauger J, Allman J, White RE., Jr Indications for lateral retinacular release in total knee replacement. Clin Orthop Relat Res. 2003;414:157–161. doi: 10.1097/01.blo.0000079260.91782.96. [DOI] [PubMed] [Google Scholar]
- 80.Liu Z, Yang H. Comparison of the minimally invasive and standard medial parapatellar approaches for total knee arthroplasty: systematic review and meta-analysis. J Int Med Res. 2011;39(5):1607–1617. doi: 10.1177/147323001103900503. [DOI] [PubMed] [Google Scholar]
- 81.Li XG, Tang TS, Qian ZL, Huang LX, Pan WM, Zhu RF. Comparison of the mini-midvastus with the mini-medial parapatellar approach in primary TKA. Orthopedics. 2010;33(10):723. doi: 10.3928/01477447-20100826-04. [DOI] [PubMed] [Google Scholar]
- 82.Khakha RS, Chowdhry M, Norris M, Kheiran A, Patel N, Chauhan SK. Five-year follow-up of minimally invasive computer assisted total knee arthroplasty (MICATKA) versus conventional computer assisted total knee arthroplasty (CATKA)—a population matched study. Knee. 2014;21(5):944–948. doi: 10.1016/j.knee.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 83.Peng X, Zhang X, Cheng T, Cheng M, Wang J. Comparison of the quadriceps-sparing and subvastus approaches versus the standard parapatellar approach in total knee arthroplasty: a meta-analysis of randomized controlled trials. BMC Musculoskelet Disord. 2015;16:327. doi: 10.1186/s12891-015-0783-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chiang H, Lee CC, Lin WP, Jiang CC. Comparison of quadriceps-sparing minimally invasive and medial parapatellar total knee arthroplasty: a 2-year follow-up study. J Formos Med Assoc. 2012;111(12):698–704. doi: 10.1016/j.jfma.2011.11.025. [DOI] [PubMed] [Google Scholar]