Abstract
Pheochromocytoma/paraganglioma (PPGL)-related hypercatecholaminemic crisis is a rare lethal condition caused by uncontrolled catecholamine secretion, occasionally leading to critical fluctuation in blood pressure (BP). Emergent transcatheter arterial embolization (TAE) has been employed for spontaneous PPGL rupture, but never, to our knowledge, for critical fluctuation in BP associated with PPGL-related hypercatecholaminemic crisis. We describe here our experience utilizing this method to control critical fluctuation in BP associated with this crisis in a 44-year-old man with an unruptured retroperitoneal paraganglioma. The patient experienced sudden severe left abdominal pain and came to our emergency department, where he exhibited severe fluctuation in BP and underwent laboratory testing that showed hypercatecholaminuria and computed tomography (CT) that revealed a left retroperitoneal tumor with no apparent intra- or retroperitoneal hematoma. We performed emergent TAE from the left inferior phrenic artery using gelatin sponge, which stabilized his BP and relieved his abdominal pain. Histologic examination following elective surgical resection of the tumor confirmed our diagnosis of unruptured retroperitoneal paraganglioma. We believe that TAE represents an important option for the emergent treatment of the critical BP fluctuation associated with PPGL-related hypercatecholaminemic crisis.
Keywords: Critical blood pressure fluctuation, Emergent transcatheter arterial embolization, Hypercatecholaminemic crisis, Retroperitoneal paraganglioma
Introduction
Pheochromocytomas and paragangliomas (PPGLs) are rare catecholamine-secreting neuroendocrine tumors that originate from chromaffin cells in the adrenal medulla (pheochromocytomas) and the extra-adrenal autonomic ganglia (paragangliomas) [1], [2], [3], [4], [5], [6]. PPGL-associated hypercatecholaminemic crisis is a rare lethal condition resulting from uncontrolled catecholamine secretion, which may lead to severe hyper- and/or hypotension, multisystem organ failure, and, less frequently, critical fluctuation in blood pressure (BP) [6], [7], [8], [9], [10], [11], [12], [13], [14]. Generally, the first-line treatment for PPGLs is elective surgical tumor resection preceded by antihypertensive therapy using alpha-1 blockade [15]. Surgery carries a high risk of intra- and perioperative morbidity and mortality, whereas patients experiencing hypercatecholaminemic crisis may require emergency surgery [16], [17], [18], [19], [20]. In patients with critical fluctuation in BP, particularly with episodes of severe hypotension, medical control using alpha-1 blockade may be contraindicated [11], [12], [13], [14]. Emergent transcatheter arterial embolization (TAE) has been sometimes performed for spontaneous rupture of PPGLs, but we believe it has not been utilized in patients manifesting severe BP fluctuation associated with hypercatecholaminemic crisis in the absence of rupture [21], [22], [23]. We present the case of a patient with an unruptured retroperitoneal paraganglioma who underwent emergent TAE that successfully controlled critical fluctuation in his BP associated with hypercatecholaminemic crisis.
Case report
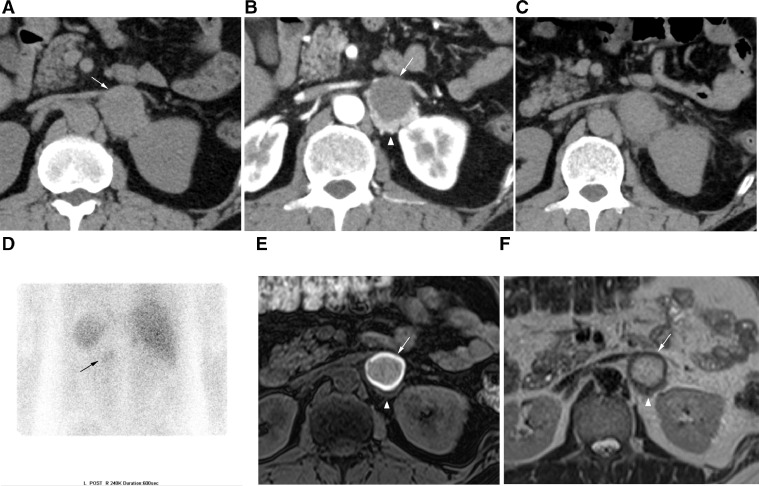
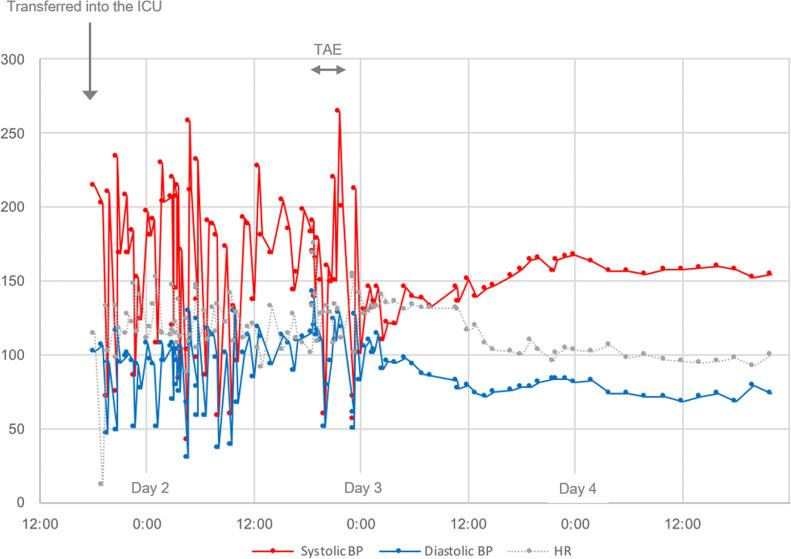
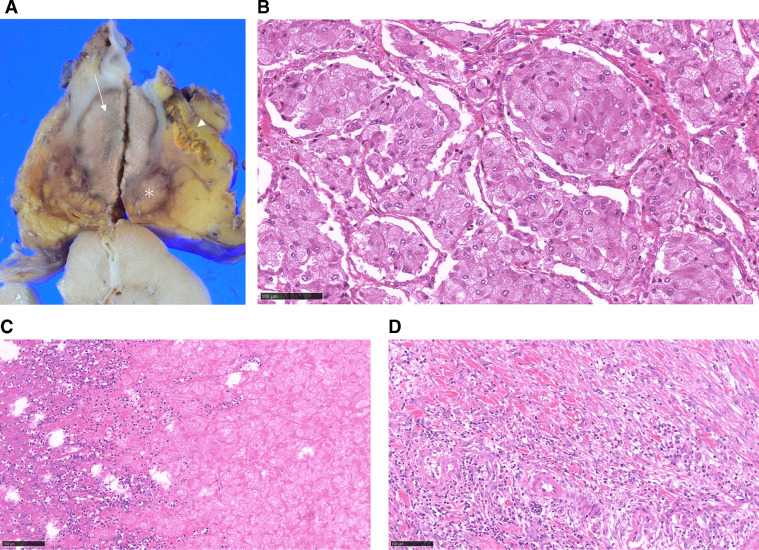
A 44-year-old Japanese man with no notable medical history suddenly experienced severe left abdominal pain when he bent forward during a morning train ride. On admission to our emergency department, he demonstrated peripheral coldness and clamminess in his extremities, and his systolic BP showed severe fluctuation, between 80 and 200 mmHg, with tachycardia of 160 bpm. Blood tests revealed elevated levels of leukocytes (22,400 /μL) and troponin I (927.1 pg/mL), hypokalemia (2.9 mEq/L), and hyperglycemia (368 mg/dL). Pre- and postcontrast computed tomography (CT) disclosed a left retroperitoneal tumor of 4-cm diameter with mild hyperattenuation that showed an area of strong enhancement in its dorsal-dominant part but otherwise poor enhancement (Figs. 1a and 1b). We suspected the patient was experiencing hypercatecholaminemic crisis associated with PPGL and transferred him to our intensive care unit. Twenty-four-hour urinalysis revealed elevated levels of metanephrine (52.7 μg/mgCre) and normetanephrine (34.5 μg/mgCre); his BP continued to demonstrate critical fluctuation with episodes of severe hypotension; and abdominal pain was uncontrolled by analgesics. On Day 2, noncontrast CT disclosed increased attenuation of the peritumoral fat with no apparent intra- or retroperitoneal hematoma, suggesting impending rupture of the PPGL (Figure 1c). Considering the risks associated with both emergent surgical resection of the tumor and medical control using alpha-1 blockade in this patient, we decided to perform emergent TAE under strict monitoring by anesthesiologists as follows. Although selective left inferior phrenic arteriography with a 4-F shepherd hook catheter and a 1.7-F microcatheter inserted via the right common femoral artery revealed no extravasation or pseudoaneurysm, we injected one-mm3 gelatin sponge from the left inferior phrenic artery via the left inferior adrenal artery and then completely eliminated the tumor stain in order to decrease blood flow to the tumor and suppress catecholamine secretion (Fig. 2). During and just after the procedure, the patient's BP continued to fluctuate; but four hours after the procedure, his BP had stabilized, and he reported relief of his abdominal pain (Fig. 3). He then received alpha-1 blockade (doxazosin, 1-6 mg/day) by mouth for 3 weeks and underwent elective surgical tumor resection on Day 24. On Day 4, his levels of urine metanephrine and normetanephrine had returned to normal. On Day 12, 123I-metaiodobenzylguanidine (MIBG) scintigraphy detected its uptake into the tumor (Fig. 1d). On Day 13, noncontrast magnetic resonance imaging (MRI) disclosed T1 shortening primarily in the periphery and T2 elongation throughout most of the mass that had shown poor enhancement on the previous CT (Figs. 1e and 1f). The tumor was histologically diagnosed as an unruptured retroperitoneal paraganglioma with large coagulative necrosis and dorsal-dominant viable cells, no hemorrhage, and peritumoral inflammation (Fig. 4). The patient's postoperative BP remained stable, and he was uneventfully discharged on Day 29.
Fig. 1.
Pre- (a) and postcontrast computed tomography (CT) on admission (b) disclose a left retroperitoneal tumor of 4-cm diameter with mild hyperattenuation (arrow in a) that shows an area of strong enhancement in its dorsal-dominant part (arrowhead in b) but otherwise poor enhancement (arrow in b). Noncontrast CT the next day (c) reveals increased attenuation of peritumoral fat without apparent intra- or retroperitoneal hematoma. Following transcatheter arterial embolization (TAE) for the tumor, posteroanterior view of 123I-metaiodobenzylguanidine (MIBG) scintigraphy (d) detects its uptake into the tumor (arrow), and noncontrast T1- (e) and T2-weighted magnetic resonance imaging (MRI) (f) disclose peripheral-dominant T1 shortening and T2 elongation throughout most of the mass (arrow) that shows poor enhancement on the postcontrast CT (b) except the dorsal-dominant part (arrowhead), strong enhancement.
Fig. 2.
Selective left inferior phrenic arteriography reveals tumor stain (open circle) corresponding to the left retroperitoneal tumor without extravasation or pseudoaneurysm.
Fig. 3.
Line charts representing systolic (red line) and diastolic blood pressure (BP) (blue line) and heart rate (HR) (gray line) before and after transcatheter arterial embolization (TAE) for the tumor. Severe BP fluctuation is noted before the TAE that rapidly disappears thereafter. ICU = intensive care unit.
Fig. 4.
Pathologic findings of the resected retroperitoneal paraganglioma. Macroscopically, the tumor (4.0 × 2.5 × 5.0 cm3 in the diameter) adjacent to the left adrenal gland (arrowhead) shows extensive coagulative necrosis (arrow) with a viable component in the dorsal part (asterisk) (a). Histologically (hematoxylin-eosin stain), tumor cells with amphophilic cytoplasm grow in a nested pattern (b). Ghost tumor cells are noted in the necrotic area with inflammatory reaction at the periphery (left) (c). Peritumoral inflammation and fibrosis are apparent without hemorrhage (d).
Discussion
Hypercatecholaminemic crisis associated with PPGL is a rare and potentially lethal condition that results from uncontrolled catecholamine secretion. Various triggers, including a forward-bending posture, can induce this crisis and occasionally lead to critical fluctuation in BP, such as that manifested by our patient [[12], [13], [14],24,25]. Ohara and colleagues reported acute attacks of critical fluctuation in BP in a patient with a pheochromocytoma with spontaneous large coagulative necrosis [11]. They surmised that catecholamine-induced vasoconstriction had produced acute infarcts in the tumor under chronic ischemia that progressed through repetitive massive releases of catecholamines into the circulation, resulting in extensive necrosis [11]. Similarly in our patient, histological examination confirmed a large area of coagulative necrosis without hemorrhage within the paraganglioma. CT of the necrosis showed mild hyperattenuation and poor enhancement, and MRI following TAE demonstrated peripheral-dominant T1 shortening. Indeed, increased attenuation in CT has been associated with increased cellular density without liquefaction in coagulative necrosis, and extensive coagulative necrosis without hemorrhage can show entire T1 shortening, such as that reported in uterine leiomyomas with red degeneration [26,27]. In our patient, the viable area of the tumor that showed strong enhancement on CT on admission preserved its uptake of MIBG even after TAE, so we speculate that the necrosis might not be attributable to the non-superselective TAE using the temporary embolic material.
Prior to surgical tumor resection, spontaneous remission of hypercatecholaminemic crisis associated with pheochromocytomas with extensive necrosis has been attributed to exhaustion of catecholamine secretion [11]. Ohara and colleagues reported spontaneous resolution of severe BP fluctuation within 2 weeks after the onset, with normalization of plasma catecholamine levels and no uptake of MIBG into the tumor, secondary to completion of the extensive necrosis [11]. Otherwise, particularly when emergent surgery and medical control using alpha-1 blockade bear high risk, treatment might comprise mechanical circulatory support with a cardiopulmonary device or intra-aortic balloon pump and/or removal of catecholamines by continuous hemodiafiltration [28], [29], [30], [31], [32]. Alternatively, we chose to perform emergent TAE, which swiftly controlled the critical BP fluctuation, and ultimately performed elective surgical tumor resection. To our knowledge, emergent TAE has never been performed to address the critical BP fluctuation associated with unruptured PPGL-related hypercatecholaminemic crisis, but we believe its use could rapidly decrease blood flow to the paraganglioma and suppress catecholamine secretion, leading to swift stabilization of BP and symptom relief. Thus, though TAE is theoretically regarded as a potential trigger of hypercatecholaminemic crisis, in this clinical scenario in which other methods are contraindicated, emergent TAE under strict monitoring may represent an important treatment option [28]. Actually, similarly in our patient, this procedure has been described to successfully rescue unruptured PPGL-related catecholamine-induced cardiogenic shock as a bridge to surgical tumor resection [28]. We used gelatin sponge as temporary embolic material instead of polyvinyl alcohol as permanent embolic material, because the latter was not clinically approved in our country. Although critical BP fluctuation associated with hypercatecholaminemic crisis can recur following TAE using the temporary embolic material, this procedure appears acceptable at least as a bridge to elective surgical tumor resection.
Conclusion
We believe this is the first report of emergent TAE performed to control critical fluctuation in BP associated with hypercatecholaminemic crisis in a patient with an unruptured retroperitoneal paraganglioma and that TAE represents an important treatment option for such cases by rapidly decreasing blood flow to the tumor and thus suppressing catecholamine secretion, particularly when emergent surgery and medical control using alpha-1 blockade bear high risk.
Footnotes
Competing Interests: We have no conflict of interest to disclose.
References
- 1.Whalen RK, Althausen AF, Daniels GH. Extra-adrenal pheochromocytoma. J Urol. Jan 1992;147(1):1–10. doi: 10.1016/s0022-5347(17)37119-7. PMID:1729490. doi: 10.1016/s0022-5347(17)37119-7. [DOI] [PubMed] [Google Scholar]
- 2.Sahdev A, Sohaib A, Monson JP, Grossman AB, Chew SL, Reznek RH. CT and MR imaging of unusual locations of extra-adrenal paragangliomas (pheochromocytomas) Eur Radiol. Jan 2005;15(1):85–92. doi: 10.1007/s00330-004-2412-3. Epub 2004 Jul 28. PMID: 15290072. [DOI] [PubMed] [Google Scholar]
- 3.Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. Jun 2014;99(6):1915–1942. doi: 10.1210/jc.2014-1498. PMID: 24893135. [DOI] [PubMed] [Google Scholar]
- 4.Turchini J, Cheung VKY, Tischler AS, De Krijger RR, Gill AJ. Pathology and genetics of phaeochromocytoma and paraganglioma. Histopathology. Jan 2018;72(1):97–105. doi: 10.1111/his.13402. PMID: 29239044. [DOI] [PubMed] [Google Scholar]
- 5.Tevosian SG, Ghayee HK. Pheochromocytomas and Paragangliomas. Endocrinol Metab Clin North Am. Dec 2019;48(4):727–750. doi: 10.1016/j.ecl.2019.08.006. PMID: 31655773. [DOI] [PubMed] [Google Scholar]
- 6.Aygun N, Uludag M. Pheochromocytoma and Paraganglioma: From Epidemiology to Clinical Findings. Sisli Etfal Hastan Tip Bul. Jun 2020;54(2):159–168. doi: 10.14744/SEMB.2020.18794. PMID: 32617052; PMCID: PMC7326683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guerrero MA, Schreinemakers JM, Vriens MR, Suh I, Hwang J, Shen WT. Clinical spectrum of pheochromocytoma. J Am Coll Surg. Dec 2009;209(6):727–732. doi: 10.1016/j.jamcollsurg.2009.09.022. PMID: 19959041. [DOI] [PubMed] [Google Scholar]
- 8.Kantorovich V, Pacak K. Emergencies Related to Pheochromocytoma/Paraganglioma Syndrome. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, Dungan K, Grossman A, Hershman JM, Hofland J, Kalra S, Kaltsas G, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, McGee EA, McLachlan R, Morley JE, New M, Purnell J, Sahay R, Singer F, Stratakis CA, Trence DL, Wilson DP, editors. Endotext [Internet] MDText.com, Inc.; South DartmouthMA: 2019. p. 2000. Aug 29. –. PMID: 25905361. [Google Scholar]
- 9.Patel D, Phay JE, Yen TWF, Dickson PV, Wang TS, Garcia R. Update on Pheochromocytoma and Paraganglioma from the SSO Endocrine/Head and Neck Disease-Site Work Group. Part 1 of 2: Advances in Pathogenesis and Diagnosis of Pheochromocytoma and Paraganglioma. Ann Surg Oncol. May 2020;27(5):1329–1337. doi: 10.1245/s10434-020-08220-3. Epub 2020 Feb 28. PMID: 32112212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kiernan CM, Solórzano CC. Pheochromocytoma and Paraganglioma: Diagnosis, Genetics, and Treatment. Surg Oncol Clin N Am. Jan 2016;25(1):119–138. doi: 10.1016/j.soc.2015.08.006. PMID: 26610778. [DOI] [PubMed] [Google Scholar]
- 11.Ohara N, Uemura Y, Mezaki N, Kimura K, Kaneko M, Kuwano H. Histopathological analysis of spontaneous large necrosis of adrenal pheochromocytoma manifested as acute attacks of alternating hypertension and hypotension: a case report. J Med Case Rep. Oct 2016;10(1):279. doi: 10.1186/s13256-016-1068-3. PMID: 27729064; PMCID: PMC5059976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ganguly A, Grim CE, Weinberger MH, Henry DP. Rapid cyclic fluctuations of blood pressure associated with an adrenal pheochromocytoma. Hypertension. Mar-Apr 1984;6(2 Pt 1):281–284. PMID: 6724665. [PubMed] [Google Scholar]
- 13.Ionescu CN, Sakharova OV, Harwood MD, Caracciolo EA, Schoenfeld MH, Donohue TJ. Cyclic rapid fluctuation of hypertension and hypotension in pheochromocytoma. J Clin Hypertens (Greenwich) Dec 2008;10(12):936–940. doi: 10.1111/j.1751-7176.2008.00046.x. PMID: 19120720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kobal SL, Paran E, Jamali A, Mizrahi S, Siegel RJ, Leor J. Pheochromocytoma: cyclic attacks of hypertension alternating with hypotension. Nat Clin Pract Cardiovasc Med. Jan 2008;5(1):53–57. doi: 10.1038/ncpcardio1054. PMID: 18094673. [DOI] [PubMed] [Google Scholar]
- 15.Kinney MA, Narr BJ, Warner MA. Perioperative management of pheochromocytoma. J Cardiothorac Vasc Anesth. Jun 2002;16(3):359–369. doi: 10.1053/jcan.2002.124150. PMID: 12073213. [DOI] [PubMed] [Google Scholar]
- 16.Uchida N, Ishiguro K, Suda T, Nishimura M. Pheochromocytoma multisystem crisis successfully treated by emergency surgery: report of a case. Surg Today. Oct 2010;40(10):990–996. doi: 10.1007/s00595-009-4165-8. Epub 2010 Sep 25. PMID: 20872207. [DOI] [PubMed] [Google Scholar]
- 17.Salinas CL, Gómez Beltran OD, Sánchez-Hidalgo JM, Bru RC, Padillo FJ, Rufián S. Emergency adrenalectomy due to acute heart failure secondary to complicated pheochromocytoma: a case report. World J Surg Oncol. May 2011;9:49. doi: 10.1186/1477-7819-9-49. PMID: 21569521; PMCID: PMC3107160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scholten A, Cisco RM, Vriens MR, Cohen JK, Mitmaker EJ, Liu C. Pheochromocytoma crisis is not a surgical emergency. J Clin Endocrinol Metab. Feb 2013;98(2):581–591. doi: 10.1210/jc.2012-3020. Epub 2013 Jan 2. PMID: 23284003. [DOI] [PubMed] [Google Scholar]
- 19.Murai N, Azami T, Iida T, Mikura K, Imai H, Kaji M. A case of pheochromocytoma with a marked decrease in catecholamine levels after rupture in which a good outcome was achieved by elective surgery. Endocr J. Nov 2018;65(11):1093–1099. doi: 10.1507/endocrj.EJ18-0071. Epub 2018 Aug 4. PMID: 30078826. [DOI] [PubMed] [Google Scholar]
- 20.Whitelaw BC, Prague JK, Mustafa OG, Schulte KM, Hopkins PA, Gilbert JA. Phaeochromocytoma crisis. Clin Endocrinol (Oxf) Jan 2014;80(1):13–22. doi: 10.1111/cen.12324. Epub 2013 Oct 17. Erratum in: Clin Endocrinol (Oxf). 2013 Mar;80(3):468. PMID: 24102156. doi: 10.1111/cen.12324. [DOI] [PubMed] [Google Scholar]
- 21.Di Daniele N, Canale MP, Tesauro M, Rovella V, Gandini R, Schillaci O. Preoperative embolization reduces the risk of cathecolamines release at the time of surgical excision of large pelvic extra-adrenal sympathetic paraganglioma. Case Rep Endocrinol. 2012;2012 doi: 10.1155/2012/481328. Epub 2012 Sep 4. PMID: 22988529; PMCID: PMC3439941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Apentchenko Eriutina N, Castellón Pavón CJ, García Vásquez C, Gonzalo Montesinos I, Jiménez de Los Galanes S, Pacheco Martínez PA. Retroperitoneal paraganglioma-Is preoperative embolization useful? Int J Surg Case Rep. 2017;39:64–68. doi: 10.1016/j.ijscr.2017.07.038. Epub 2017 Aug 5. PMID: 28806623; PMCID: PMC5554985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Edo N, Yamamoto T, Takahashi S, Mashimo Y, Morita K, Saito K. Optimizing Hemodynamics with Transcatheter Arterial Embolization in Adrenal Pheochromocytoma Rupture. Intern Med. Jul 2018;57(13):1873–1878. doi: 10.2169/internalmedicine.9907-17. Epub 2018 Feb 28. PMID: 29491290; PMCID: PMC6064710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guzik P, Wykretowicz A, Wesseling IK, Wysocki H. Adrenal pheochromocytoma associated with dramatic cyclic hemodynamic fluctuations. Int J Cardiol. Sep 2005;103(3):351–353. doi: 10.1016/j.ijcard.2004.08.071. PMID: 16098406. [DOI] [PubMed] [Google Scholar]
- 25.Oishi S, Sasaki M, Ohno M, Umeda T, Sato T. Periodic fluctuation of blood pressure and its management in a patient with pheochromocytoma. Case report and review of the literature. Jpn Heart J. May 1988;29(3):389–399. doi: 10.1536/ihj.29.389. PMID: 3050197. [DOI] [PubMed] [Google Scholar]
- 26.Nakai G, Yamada T, Hamada T, Atsukawa N, Tanaka Y, Yamamoto K. Pathological findings of uterine tumors preoperatively diagnosed as red degeneration of leiomyoma by MRI. Abdom Radiol (NY) Jul 2017;42(7):1825–1831. doi: 10.1007/s00261-017-1126-3. PMID: 28389786; PMCID: PMC5486831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shiino A, Ito R, Nakasu S, Handa J. Metastatic adenocarcinoma presenting as a homogeneously high density mass on CT. J Comput Assist Tomogr. Jan-Feb 1998;22(1):130–132. doi: 10.1097/00004728-199801000-00024. PMID: 9448776. [DOI] [PubMed] [Google Scholar]
- 28.Houari N, Touzani S, Salhi H, Alaoui Lamrani MY, Ibnmajdoub K, El Ouahabi H. Retroperitoneal Paraganglioma-Induced Cardiogenic Shock Rescued by Preoperative Arterial Embolization. Case Rep Crit Care. Jul 2018;2018 doi: 10.1155/2018/4058046. PMID: 30073095; PMCID: PMC6057417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou X, Liu D, Su L, Long Y, Du W, Miao Q. Pheochromocytoma crisis with severe cyclic blood pressure fluctuations in a cardiac pheochromocytoma patient successfully resuscitated by extracorporeal membrane oxygenation: a case report. Medicine (Baltimore) May 2015;94(17):e790. doi: 10.1097/MD.0000000000000790. PMID: 25929929; PMCID: PMC4603056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dang Van S, Hamy A, Hubert N, Fouquet O. Cardiogenic shock induced by a voluminous phaeochromocytoma rescued by concomitant extracorporeal life support and open left adrenalectomy. Eur J Cardiothorac Surg. Oct 2016;50(4):782–783. doi: 10.1093/ejcts/ezw122. Epub 2016 Apr 10. PMID: 27068551. [DOI] [PubMed] [Google Scholar]
- 31.Bouabdallaoui N, Bouchard D, Jolicoeur EM, Chronopoulos A, Garneau PY, Lamarche Y. Extracorporeal membrane oxygenation in pheochromocytoma-induced cardiogenic shock. Asian Cardiovasc Thorac Ann. May 2018;26(4):314–316. doi: 10.1177/0218492317727995. Epub 2017 Aug 21. PMID: 28823181. [DOI] [PubMed] [Google Scholar]
- 32.Koizumi G, Saiki R, Kurokawa I, Mikura K, Iida T, Murai N, Kaji M. Continuous Hemodiafiltration for Pheochromocytoma Crisis with a Positive Outcome. Intern Med. NOV 2019;58(21):3113–3119. doi: 10.2169/internalmedicine.2991-19. Epub 2019 Jul 10. PMID: 31292390; PMCID: PMC6875466. [DOI] [PMC free article] [PubMed] [Google Scholar]