Abstract
Internal carotid artery tadndem lesions are common and are associated with a worse prognosis. There is still no clarity on the endovascular therapy strategy that should be used in the setting of acute cerebrovascular events. We present the case of a patient with acute cerebral ischemia secondary to internal caroid artery tandem lesion, who underwent intracranial thrombectomy and early stenting of the extracranial occlusion, who in a 12-month follow-up did not present complications associated with the procedure, sequelae neurological, thromboembolic recurrence or hemorrhagic events.
Key words: Ischemic stroke, Tandem vascular lesion, Thrombecthomy, Internal carotid artery, Stent
Introduction
Internal carotid artery (ICA) tandem occlussion (TO) is a vascular condition where there is concomitant involvement of its extracranial (EICA) and intracranial (IICA) segments due to thromboembolism, or direct extension of the emboli to major intracranial vessels such as the intracranial internal carotid artery or the middle cerebral artery (MCA). It has poor prognosis and poor response to treatment, especially to thrombolytic therapy alone, possibly secondary to a high thrombotic load that hinders the adequate distribution of the thrombolytic [1]. It corresponds to approximately 15% to 20% of all stroke cases [2,3].
Despite its high technical complexity, mechanical thrombectomy (MT) has emerged as the best treatment option for TO with a high rate of success and safety; however, there is lack of solid evidence. It is not yet clear which approach should be used for proximal obstruction: using a stent is a quick and immediate solution, but it carries an increased risk of bleeding due to the mandatory use of antiplatelet therapy and in some cases of intravenous thrombolysis (IVT); percutaneous transluminal angioplasty avoids the use of antiplatelet therapy but increases the risk of reperfusion injury. Others have advocated treatment of the intracranial injury alone with good results [4].
Another controversial scenario is the order in which obstructions should be addressed. Initial intervention of the intracranial injury represents shorter recanalization time; initial intervention of the extracranial injury defend allows a better state of the collateral vasculature while taking care of the intracranial injury [1].
Wilson et al., found no significant differences in outcomes between these two approaches, however, shorter angiographic time has been reported with initial intervention of intracranial injury [1,4]. They reported a trend towards a better safety profile when the extracranial approach was done first, possibly related to better collateralization.
Coelho et al., concluded that stenting of ICA occlusion did not show clinical benefits, seems to increase the risk of adverse events and prolongs times of intervention with extension of the ischemia. The best recommendation to date is IVT together with avoiding the ICA stent approach [5].
In this article, we present a case report of the treatment of tandem occlusion based on the experience of the interventional radiology group of a reference center in southwestern Colombia.
Case report
A previously asymptomatic 73-year-old man with history of hypertension and a left knee arthroscopic chondroplasty 2 days before, presented to the emergency department with 2 hour onset dysarthria and right hemiparesia. He had no other neurological findings.
A head Computed Tomography (CT) revealed acute thrombosis of the left middle cerebral artery with infarction of its vascular territory. His Alberta Stroke Programme early CT score (ASPECTS) was 7 out of 10 points.
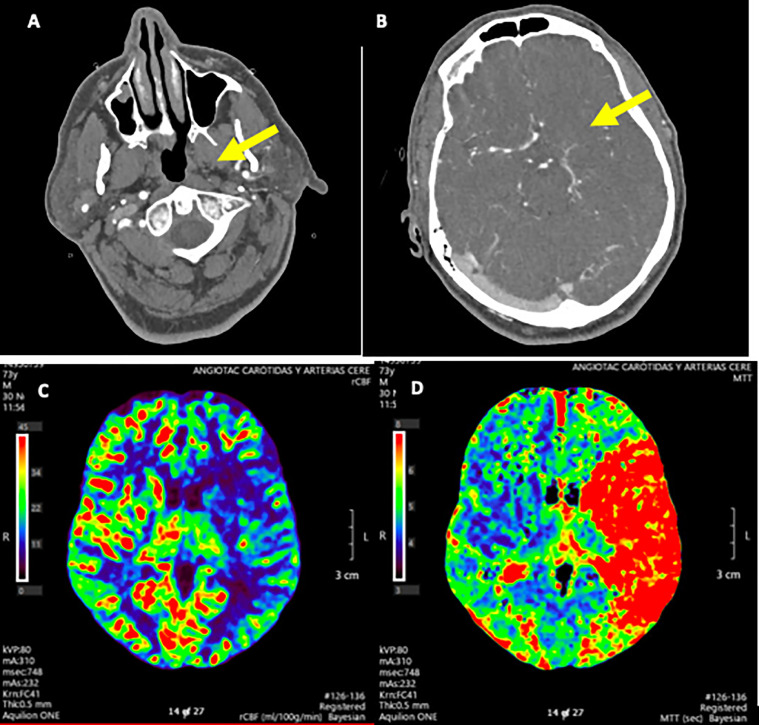
A head CT angioraphy (CTA) confirmed filling defects of the extracranial left ICA and left MCA, with moderate collaterality. The perfusion maps showed decreased Cerebral Blood Flow, increased Mean Transit Time and increased Peak Time in the MCA territory (Fig. 1).
Fig. 1.
Head CTA (A and B) shows filling defect of the left ICA in its bifurcation (A, arrow) and in the left MCA (B, arrow). Cerebral perfusion maps (C and D) show decreased cerebral blood flow (C) with increased mean transit time (D) in the territory of the MCA.
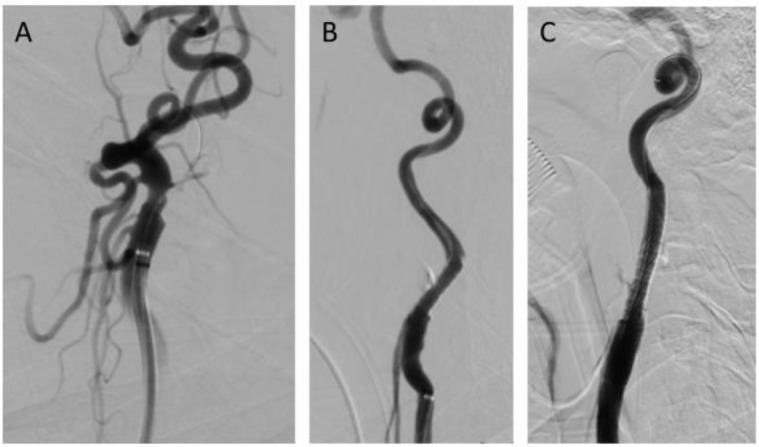
The patient was taken to MT under local anesthesia. Tandem occlusion of the left EICA and IICA in its distal segment were observed (Fig. 2A). The common carotid artery was cannulated with a Neuron Max catheter and a 3 mm balloon angioplasty was performed. MT in the IICA was accomplished with a 4 × 40mm Retriever Solitari stent and penumbra aspiration system with a TICI 3 angiographic result. Afterwards, EICA stenting was carried out with Stent Advanda 5 mm expandable balloon (Fig. 2B). The CT scan showed no signs of hemorrhagic transformation.
Fig. 2.
DSA of the extracranial ICA (A, B and C), shows cannulation of the occlusion (A) and stenting with expandable balloon (B) in the first stage of the procedure. DSA 5 days later shows definitive stent with complete coverage of the previous stent (C).
Improvement of dysarthria and hemiparesis were evidenced after procedure. Control head CT three days later revealed established ischemia in the MCA territory.
Digital sustraction Angiography was performed 5 days later, demonstrating a properly positioned stent with good angiographic result in the EICA and minimal flow to the external carotid artery with collaterality. Complement stenting with a longer definitive Wallstent with complete coverage of the previous stent (Fig. 2C) was performed to reduce the risk of thromboembolism and in-stent stenosis with satisfactory angiographic appearance.
The patient was discharged with rosuvastatin 40 mg, acetylsalicylic acid 100 mg, and clopidogrel 75 mg, with rehabilitation therapies and outpationt follow-up at 12 months without presenting neurological or hemorrhagic novelties.
Discussion
Carotid artery tandem occlussions are conditions associated with ischemic cerebrovascular events in a minority of cases (less than 20%), but they carry a worse prognosis [5]. Despite its relevance, the therapeutic approach to this type of injury is a matter of debate, and there is significant variability among interventional teams when choosing the alternative [8].
In single occlusions, it is clear that the combination of mechanical thrombectomy and stenting in the context of the emergency denotes better results. Regarding tandem occlusions, it is understood that the recanalization rate with intravenous thrombolysis is low (9%) [7]. However, in endovascular management the evidence is contradictory [5,7]. As mentioned, it is generally accepted that thrombectomy is an appropriate choice, but it has not been possible to demonstrate a clear superiority of one therapeutic strategy over another with regard to extracranial injury [6]; especially there is disagreement on the need for implantation of the stent and the time of intervention (before or after thrombectomy, or late at a second time).
The case presented illustrates that a completely endovascular approach with intracranial thrombectomy followed by early stenting of the EICA, improved distal perfusion and clinical response in a 12-month follow-up of a patient with tandem occlusion, without being associated to extension of brain damage, technical complications of the procedure, intracranial hemorrhages, recurrence of the thromboembolic event or in-stent stenosis.
This case provides the literature with evidence of the success of early stenting of the extracranial lesion of the ICA in a patient with a potentially very poor prognosis, and added to other cases it could help to characterize the patients who benefit from this type of procedure.
Acknowledgments
Contributorship
Conception or design of the work: ECGP, CFMD, VMQ, EAFP. Data acquisition and analysis: ECGP, CFMD, VMQ, EAFP. Interpretation of data: ECGP, CFMD, EAFP. Drafting the work: ECGP, CFMD, VMQ. Revising the work for valuable intellectual content: ECGP, CFMD. Final approval of the version: ECGP, CFMD, VMQ, EAFP
Data sharing statement
The relevant anonymized patient-level data are available via request from the authors.
Ethical approval and Informed consent
The report case was reviewed and approved. Following our institutional guidelines, all protected health information was removed, and individual patient consent was not required for the analysis.
Footnotes
Acknowledgment: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Competing Interest: The authors declare no conflicts of interest in the publication of this article.
References
- 1.Wilson MP, Murad MH, Krings T, Pereira VM, O'Kelly C, Rempel J. Management of tandem occlusions in acute ischemic stroke - intracranial versus extracranial first and extracranial stenting versus angioplasty alone: a systematic review and meta-analysis. J Neurointerventional Surg. 2018;10(8):721–728. doi: 10.1136/neurintsurg-2017-013707. [DOI] [PubMed] [Google Scholar]
- 2.Rangel-Castilla L, Rajah GB, Shakir HJ, Shallwani H, Gandhi S, Davies JM. Management of acute ischemic stroke due to tandem occlusion: should endovascular recanalization of the extracranial or intracranial occlusive lesion be done first? Neurosurg Focus. 2017;42(4):E16. doi: 10.3171/2017.1.FOCUS16500. [DOI] [PubMed] [Google Scholar]
- 3.Papanagiotou P, Haussen DC, Turjman F, Labreuche J, Piotin M, Kastrup A. Carotid stenting with antithrombotic agents and intracranial thrombectomy leads to the highest recanalization rate in patients with acute stroke with tandem lesions. JACC Cardiovasc Interv. 2018;11(13):1290–1299. doi: 10.1016/j.jcin.2018.05.036. 09. [DOI] [PubMed] [Google Scholar]
- 4.Blassiau A, Gawlitza M, Manceau P-F, Bakchine S, Serre I, Soize S. Mechanical thrombectomy for tandem occlusions of the internal carotid artery—results of a conservative approach for the extracranial lesion. Front Neurol [Internet] 2018 doi: 10.3389/fneur.2018.00928. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6230960/ [cited 2020 Nov 13]9Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grigoryan M, Haussen DC, Hassan AE, Lima A, Grossberg J, Rebello LC. Endovascular treatment of acute ischemic stroke due to tandem occlusions: large multicenter series and systematic review. Cerebrovasc Dis Basel Switz. 2016;41(5–6):306–312. doi: 10.1159/000444069. [DOI] [PubMed] [Google Scholar]
- 6.Jadhav Ashutosh P., Zaidat Osama O., Liebeskind David S., Yavagal Dileep R., Haussen Diogo C., Hellinger Frank R. Emergent management of tandem lesions in acute ischemic stroke. Stroke. 2019;50(2):428–433. doi: 10.1161/STROKEAHA.118.021893. [DOI] [PubMed] [Google Scholar]
- 7.Assis Z, Menon BK, Goyal M, Demchuk AM, Shankar J, Rempel JL. Acute ischemic stroke with tandem lesions: technical endovascular management and clinical outcomes from the ESCAPE trial. J Neurointerventional Surg. 2018;10(5):429–433. doi: 10.1136/neurintsurg-2017-013316. [DOI] [PubMed] [Google Scholar]
- 8.Coelho A.P., Lobo M., Gouveia R., Silveira D., Campos J., Augusto R. Overview of evidence on emergency carotid stenting in patients with acute ischemic stroke due to tandem occlusions: a systematic review and meta-analysis. J cardiovascular surgery. 2019;60(6):693–702. doi: 10.23736/S0021-9509.18.10312-0. [DOI] [PubMed] [Google Scholar]