Abstract
Background:
The United States is currently facing 2 epidemics: sustained morbidity and mortality from substance use and the more recent COVID-19 pandemic. We tested the hypothesis that the pandemic has disproportionately affected individuals with substance use disorder by evaluating average daily 9-1-1 ambulance calls for substance use-related issues compared with all other calls.
Methods:
This was a retrospective cross-sectional analysis of 9-1-1 ambulance calls before and after the start of COVID-19 in Massachusetts. We used consecutive samples of 9-1-1 ambulance calls, categorized into those which were substance-related or not. An interrupted time series analysis was performed to determine if there were changes in numbers of daily calls before a statewide declaration of emergency for COVID-19 (February 15–March 9, 2020), from the emergency declaration until a stay-at-home advisory (March 10–March 22, 2020) and following the stay-at-home advisory (March 23–May 15, 2020).
Results:
Compared with prior to the statewide emergency, the post-statewide emergency average of daily ambulance calls decreased from 2,453.2 to 1,969.6, a 19.7% decrease. Similarly, calls for substance-related reasons decreased by 16.4% compared with prior to the statewide emergency. However, despite an initial decrease in calls, after the stay-at-home advisory calls for substance use began increasing by 0.7 (95% confidence interval (CI) 0.4–1.1) calls/day, while calls for other reasons did not significantly change (+1.2 (95% CI −0.8 to 3.1) calls/day). Refusal of transport for substance-related calls increased from 5.0% before the statewide emergency to 7.5% after the declaration (p < 0.001).
Conclusions:
After an initial decline in substance-related ambulance calls following a statewide declaration of emergency, calls for substance use increased to pre-COVID-19 levels, while those for other reasons remained at a lower rate. The results suggest that COVID-19 is disproportionately affecting individuals with substance use disorder.
Keywords: emergency medical services, substance use, opioids
Background
The United States is experiencing 2 simultaneous epidemics. The opioid epidemic, first proclaimed by the Centers for Disease Control and Prevention (CDC) in 2011 and later as a national public emergency by the White House in 2017, claimed about 400,000 lives between 1999 and 2017 (1, 2). Substance use disorder-related overdose resulted in more than 67,000 deaths in 2018 alone (3). Meanwhile, through mid-August 2020 the COVID-19 pandemic has tragically claimed over 170,000 lives during its rapid spread (4).
The impacts of these 2 epidemics are not mutually exclusive. It can be expected that the consequences of substance use disorder, including instability of housing, jobs and food, will be exacerbated by COVID-19. In addition to the fear, anxiety and personal economic stressors brought on by this pandemic, COVID-19 may make it more difficult for individuals with substance use disorders to receive care and access social supports critical for recovery (5). As in-person group meetings have been limited, the New York Times has labeled the COVID-19 pandemic “a national relapse trigger” (6). There are early signals that COVID-19 has led to a massive 42% decrease in emergency department (ED) visits from its start to the end of April 2020 (7). Although some of this decline was in categories that may have been acceptable to treat in alternative settings such as otitis media and superficial injuries, there are also indications that visits for chest pain and myocardial infarction declined, indicating that patients may be delaying care instead of coming to the emergency department (ED) (7). This may be the case for individuals with substance use disorder and overdose, too. There are further considerations as well. As an example, COVID-19 has changed the landscape of the illicit drug market, including variability in the potency of drugs people are using based on the available supply chain and a shift of drug use to other types of drugs, such as methamphetamine (8).
As society is rapidly trying to understand and mitigate the effects of COVID-19 on individuals with substance use disorders, early data are essential. One important data source is ambulance trip data from emergency medical services (EMS) agencies. Such information can demonstrate epidemiologic shifts in frequency of reported illness and provide information concerning utilization patterns.
In this study, we used the Massachusetts Ambulance Trip Information System (MATRIS), which records all 9-1-1 ambulance calls in the state to determine if COVID-19 had an effect on ambulance calls for drug use and intoxication (substance-related) compared with overall ambulance 9-1-1 calls. We hypothesized that the widespread community shut-down advisory occurring after the statewide declaration of emergency was associated with an increase in substance-related calls but decreases in other common reasons for ambulance use relative to pre-COVID-19 trends.
Methods
This was a retrospective observational study of all 9-1-1 ambulance calls from February 15, 2020 to May 15, 2020 in the state of Massachusetts, where a state of emergency was declared on March 10, 2020 followed by a broad stay-at-home advisory on March 23, 2020 (9). For the purposes of this study, the pre-COVID-19 period was defined as February 15 to March 9, 2020. The COVID-19 period was defined as March 10, 2020 to May 15, 2020. Information for every EMS call during the study period was entered into MATRIS by local EMS agencies. We defined an EMS call as any EMS dispatch for which patient contact occurred, regardless of whether the patient was ultimately transported. The deidentified data were provided to our research team from the state Department of Public Health. The study was deemed “not human subjects research” by the Partners Healthcare Institutional Review Board.
To determine the reason for each ambulance call, we programmed a hierarchical schema based on prior work (10). We further collapsed these to create 10 broad categories (Table 1). We were provided with data for dispatch chief complaint (recorded by the 9-1-1 dispatcher), symptom complaint and clinical impression (recorded by the EMS provider). Clinical impression documented by EMS personnel is thought to be the most accurate reason for transport and was used to categorize reason for transport, if present. If not present, then dispatch reason was used, followed by symptom complaint.
Table 1.
Descriptive analysis of reason for ambulance transport before and after the statewide emergency for COVID-19
| Pre-COVID-19* | COVID-19† | ||||
|---|---|---|---|---|---|
| Reason for Transport | n | Average/day | n | Average/day | % change |
| medical | 21,097 | 879.0 | 46,861 | 699.4 | −20.4 |
| trauma | 7,225 | 301.0 | 14,262 | 212.9 | −29.3 |
| neurologic | 6,665 | 277.7 | 14,134 | 211.0 | −24.0 |
| cardiac | 6,080 | 253.3 | 12,582 | 187.8 | −25.9 |
| behavioral | 5,309 | 221.2 | 12,566 | 187.6 | −15.2 |
| respiratory | 5,097 | 212.4 | 13,990 | 208.8 | −1.7 |
| other | 3,859 | 160.8 | 9,395 | 140.2 | −12.8 |
| substance-related | 3,184 | 132.7 | 7,431 | 110.9 | −16.4 |
| obstetrics/gynecology | 239 | 10.0 | 466 | 7.0 | −30.2 |
| missing | 121 | 5.0 | 275 | 4.1 | −18.6 |
| total | 58,876 | 2,453.2 | 131,962 | 1,969.6 | −19.7 |
Pre-COVID-19 is February 15 to March 9, 2020 (24 days).
COVID-19 is March 10 to May 15, 2020 (67 days).
For the category of drug use and intoxication (referred to as “substance-related calls”), we chose all categories related to substance use (Appendix A). Nonspecific reasons, such as “altered mental status” and “weakness” were not included as they are not specific to substance use. This methodology allowed comparison of calls for all substance use-related complaints. To further study the effect of opioid overdose, we also chose a subset of calls that were specific to opioids (boldface in Appendix A) but acknowledge that this likely missed some opioid-related calls that were coded with a nonspecific code (such as “Drug Overdose Accidental (T50.901A)” and “Substance - Unspecified Overdose (T50.90)”). EMS providers are also sometimes unable to determine the exact substance used, and for this sub-analysis we only included those specifically coded as opioid-related.
We analyzed differences in demographics (age and gender) between 9-1-1 calls for substance-related calls and all other reasons, excluding those with missing reasons. We also examined calls where the individual refused transport to determine if there was a difference before and during COVID-19. Categorical variables were compared with Chi-square test and continuous variables were compared with Student’s t-test.
To assess the impact of COVID-19 on trends of substance use and nonsubstance use-related 9-1-1 calls, we conducted a three period interrupted time series analysis (ITSA) that included the pre-COVID-19 period, the period between the statewide emergency and the stay-at-home advisory (March 10, 2020 to March 22, 2020), and the period during COVID-19 following the stay-at-home advisory. ITSA projects the trend from the pre-intervention period into the post-intervention period to hypothesize what would have happened to trends in 9-1-1 calls without the statewide emergency declaration or stay-at-home advisory. We used a segmented ordinary least squares regression with a time variable indicating the number of days from February 15, 2020. We assessed autocorrelation using the Ljung-Box test and added a lag term as indicated. We evaluated if the state of emergency and stay-at-home advisory were associated with changes in level (intercept change or level change) and trend (slope change). We performed this analysis for a) all 9-1-1 calls except for substance-related calls and b) calls for substance-related reasons. As a subset analysis, we performed the analysis for just categories specific to opioid use, recognizing that other categories such as “substance use” also contained EMS runs for opioid use. For this graph, we included all patients who had the variable of interest in any of the clinical impression or dispatch categories. For example, if dispatch reason was “opioid overdose” and clinical impression was “cardiac arrest,” the call would be included. Statistical analyses were performed with Stata IC (version 15.1; StataCorp, College Station, TX, USA) and JMP (version 14; SAS Institute, Cary, NC, USA).
Results
Table 1 demonstrates the reason for EMS calls before and after the statewide emergency declaration for COVID-19. Overall, daily average calls decreased from 2,453.2 to 1,969.6, a 19.7% decrease. The smallest decrease was seen for respiratory complaints (−1.7%) and the largest decrease was for obstetric/gynecological emergencies (−30.2%). Calls for substance-related issues decreased overall by 16.4%.
Table 2 compares characteristics of all calls exclusive of those for drugs/intoxication (n = 179,827) and those for drugs/intoxication (n = 10,615), excluding those with missing reasons for transport (n = 396). For nondrug-related transports, there were small but significant changes in patient demographics (slightly older and more likely to be male in the COVID-19 period). The percentage of patients who refused transport increased from 10.9% to 15.0%, and the percentage of patients who were declared dead at scene doubled (0.6–1.2%). For drug-related transports, there was no detectable difference in patient age or sex. There was also no significant difference in the percentage declared dead at scene. However, refusal of transport increased from 5.0% pre-COVID-19 to 7.5% in the COVID-19 period.
Table 2.
Characteristics of patients and ambulance nonsubstance-related and substance-related calls
| Pre-COVID-19* | COVID-19† | P value | |
|---|---|---|---|
| Nonsubstance-Related Transports (n) | 55,571 | 124,256 | |
| Patient age (mean years, 95% CI) | 51.6 (51.4–51.9) | 52.6 (52.4–52.7) | p < 0.001 |
| Male sex (n, %) | 25,570 (47.5) | 59,916 (49.8) | p < 0.001 |
| Time from dispatch to care complete (mean minutes, 95% CI) | 47.6 (47.4–47.8) | 48.1 (47.9–48.2) | p < 0.001 |
| Patients transported (n, %) | 45,387 (81.7) | 94,532 (76.1) | p < 0.001 |
| Refusal of transport/AMA (n, %) | 6,041 (10.9) | 18,580 (15.0) | p < 0.001 |
| Dead at scene | 348 (0.6) | 1,457 (1.2) | p < 0.001 |
| Substance-Related Transports (n) | 3,184 | 7,433 | |
| Patient age (mean years, 95% CI) | 39.3 (38.7–40.0) | 40.0 (39.6–40.4) | p = 0.113 |
| Male sex (n, %) | 2,195 (69.6) | 5,230 (71.4) | p = 0.067 |
| Time from dispatch to care complete (mean minutes, 95% CI) | 42.7 (42.1–43.4) | 42.1 (41.7–42.6) | p = 0.150 |
| Patient transported (n, %) | 2,883 (90.5) | 6,533 (87.9) | p < 0.001 |
| Refusal of transport/AMA (n, %) | 159 (5.0) | 554 (7.5) | p < 0.001 |
| Dead at scene | 2 (0.1) | 17 (0.2) | p = 0.199 |
AMA = against medical advice.
Pre-COVID-19 is February 15 to March 9, 2020 (24 days).
COVID-19 is March 10 to May 15, 2020 (67 days).
P values in bold are statistically significant (p < 0.05).
Figure 1 demonstrates trends in ambulance transports in the 3 specified time periods estimated with ITSA. For nondrug-related calls (Panel A), there was no significant change in daily calls prior to the statewide emergency (+3.6 calls/day, 95% CI −6.5 to 13.7). Between the statewide emergency and stay-at-home advisory, there was a nonsignificant level decrease of −31.7 calls/day (95% CI −230.0 to 166.6) and a decreasing trend of −51.5 (95% CI −64.8 to −38.1) calls/day. After the stay-at-home advisory, relative to the pre-COVID-19 period, there was a level increase of 122.6 (95% CI 2.0 to 243.1) calls/day with no significant trend in calls/day (+1.2 calls/day, 95% CI −0.8 to 3.1).
Figure 1.
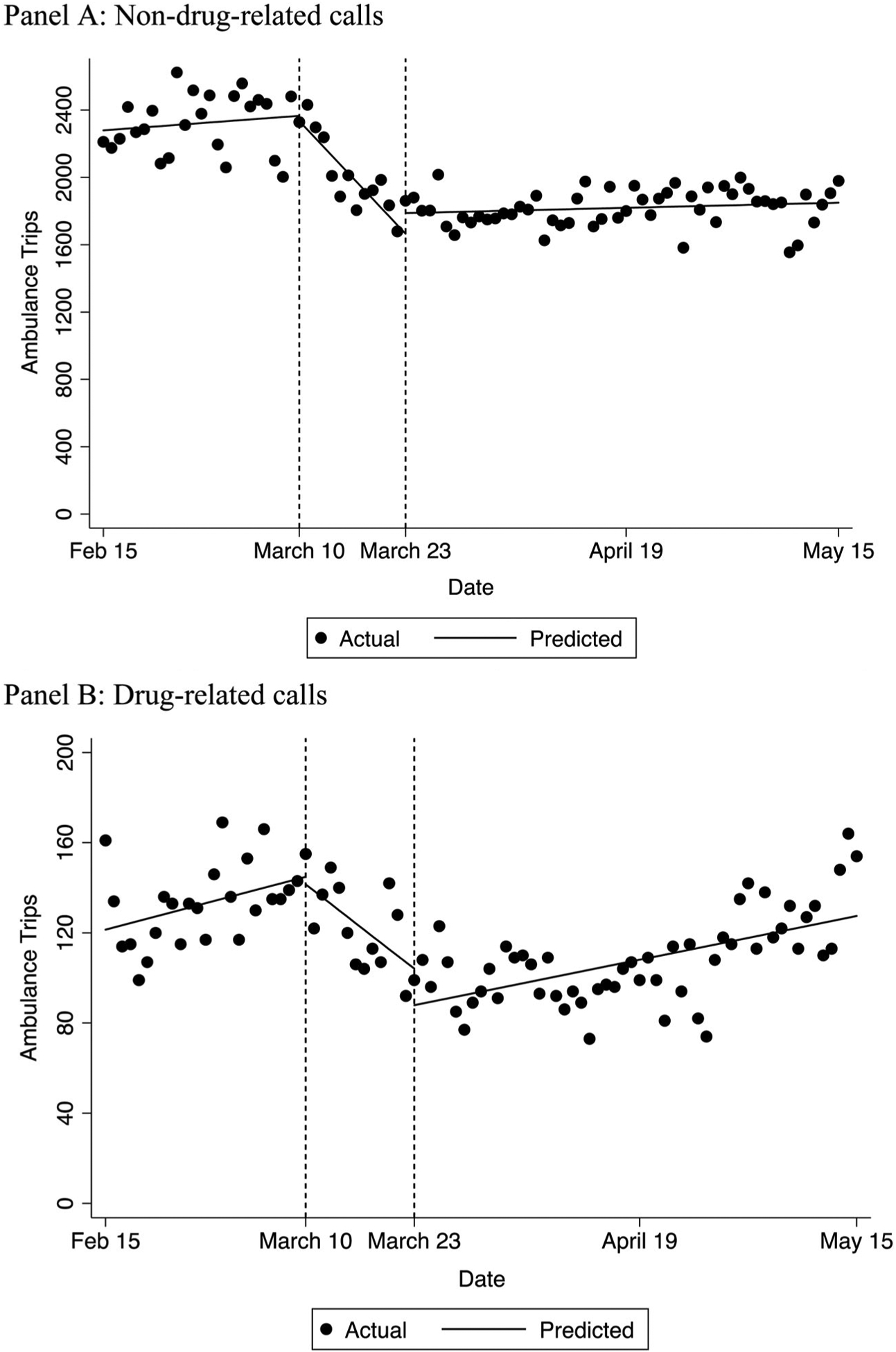
Interrupted time series analysis of the number of ambulance calls prior to COVID-19 (February 15, 2020 to March 9, 2020), between the statewide emergency and the stay-at-home advisory (March 10, 2020 to March 22, 2020) and after the stay-at-home advisory (March 23, 2020 to May 15, 2020), for nonsubstance-related calls (Panel A) and substance-related calls (Panel B).
For substance-related calls (Panel B), there was likewise no significant change in daily EMS calls prior to the statewide emergency (+1.0 calls/day, 95% CI −0.2 to 2.2). Between the statewide emergency and stay-at-home advisory, there was a significant level decrease in the number of calls/day (−3.3, 95% CI −6.4 to −1.3) and a sustained decreasing trend in substance-related calls of −2.9 calls/day (95% CI −5.2 to −0.6). However, after the stay-at-home advisory, there was a nonsignificant decrease in level (−16.2, 95% CI −40.5 to 8.1) followed by an increasing trend of 0.7 calls/day (95% CI 0.4 to 1.1). Near the end of that period, daily average calls had reached similar levels to the pre-COVID-19 period.
Figure 2 demonstrates the number of daily calls for all substance-related issues excluding opioids and those defined specifically as opioid related transports. As previously described, it is almost certain that there are opioid-related transports contained in the category not specific for opioids.
Figure 2.
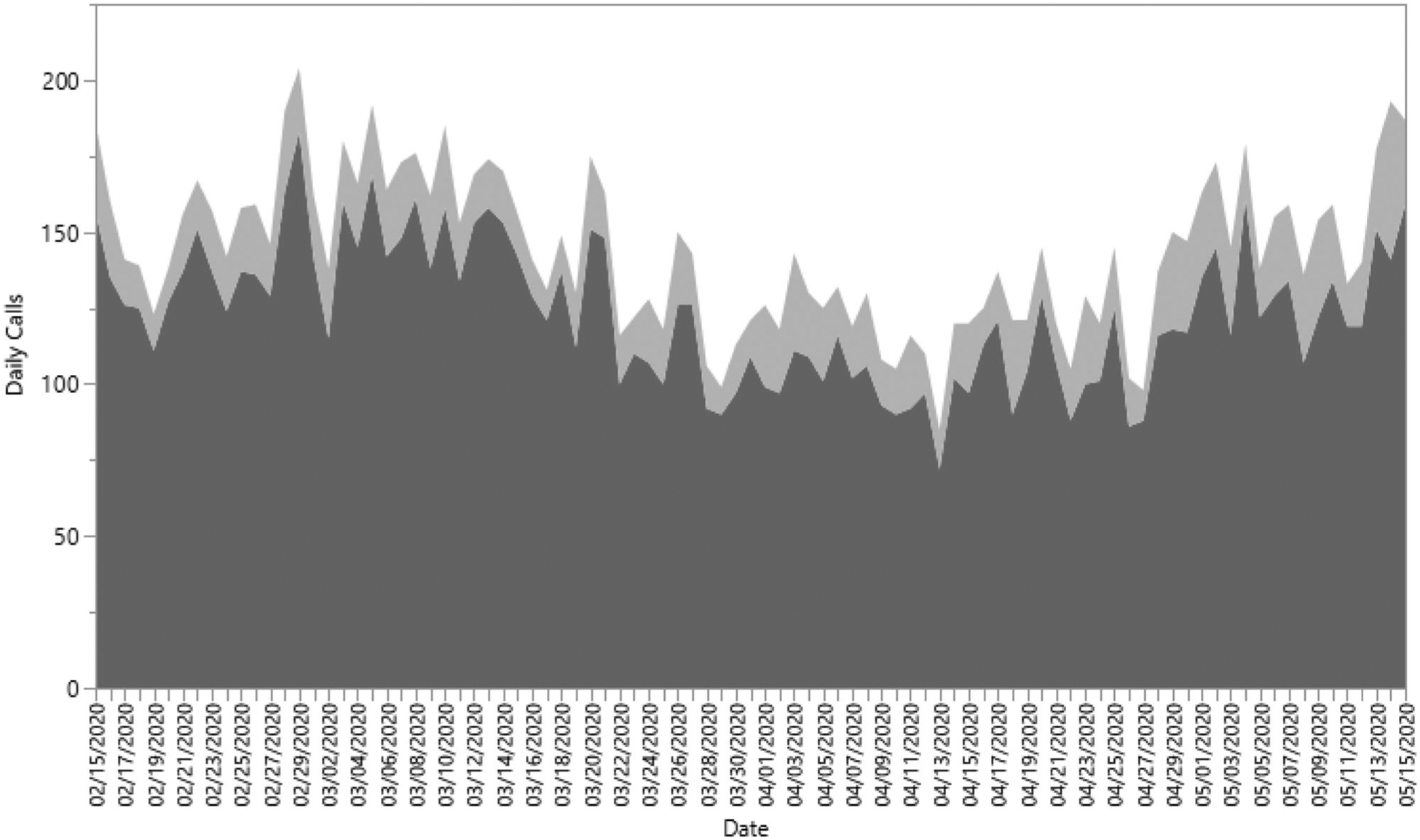
Daily ambulance trips for substance use-related calls, excluding opioids (dark gray), and those specifically for opioids-related reasons (light gray).
Discussion
In this study, evaluating EMS calls before and after a statewide declaration of emergency for COVID-19, we discovered that the trend of daily calls initially decreased, with a significant drop in the number of daily calls after the statewide emergency compared to the pre-COVID-19 period. However, about 2 weeks later, when a stay-at-home advisory was issued, the patterns of substance-related calls and those not related to substance use appear to diverge: calls for nonsubstance-related issues remained at a new, lower level, while those for substance-related issues increased substantially, approaching baseline pre-COVID-19 numbers near the end of the study period.
These results confirm prior hypotheses in the literature (11–13). Given that social stressors that likely disproportionately affect patients with substance use disorders (e.g., homelessness or lack of food or job security) would be expected to increase with COVID-19, so too should ambulance dispatches for these reasons (14). A recent study of patients with HIV and concurrent substance use disorder reported increased illicit substance use and contact with other substance-using individuals and decreased attendance at recovery meetings contemporaneous with COVID-19 (15).
The results of our study are interesting to compare with a study from Kentucky, a state which has also been greatly affected by substance use disorder, demonstrating a 17% increase in the number of EMS opioid-related calls after a statewide COVID-19 emergency declaration (16). The study also demonstrated a 71% higher refusal of transport rate during COVID-19 compared with the prior period. Our refusal rate increased by 50% (from 5.0–7.5%), indicating that in both states patients were hesitant to come to the hospital during the COVID-19 outbreak.
The increase in EMS refusal of transport is consistent with other studies. A survey by the American College of Emergency Physicians/Morning Consult discovered that 80% of individuals surveyed were concerned about contracting COVID-19 from another patient or visitor if they needed to go to the ED (17). While the initial mortality of patients who refuse transport immediately after naloxone reversal is low (18), this increase in refusal rate is nevertheless concerning, and the one-year mortality of individuals who survive an opioid overdose is quite high (19). In part to address this concern, Massachusetts implemented an EMS protocol for “Leave-Behind Naloxone,” in which when a patient refuses transport, the patient and/or an accompanying individual can be given a naloxone kit and instructed on its use (20).
There are several additional findings of note. The first is that the demographics of substance-related calls appear to be lower than those of nonsubstance-related transports. The average age for substance-related calls was around 40 and over two-thirds were male, while for nonsubstance-related calls the average age was over 50 and had about equal sex distribution for nonsubstance-related calls. We were also curious to see if transport times varied given the need for EMS providers to don personal protective equipment. For substance-related transports, there was no difference from dispatch to care complete (about 42 minutes in both periods). Although the finding was not significant, the percentage of patients declared dead at scene was 0.1% in the pre-COVID-19 period and 0.2% in the COVID-19 period. The fact that this doubling did not reach statistical significant may be due to small sample size but does warrant further study, particularly evaluating if providers were more hesitant to provide naloxone or to perform CPR for fear of aerosolization.
This study has several limitations that must be considered. The study was retrospective and based on administrative data completed during a prehospital encounter, which were then divided into categories. Misclassification errors are possible. This is statewide data and may not necessarily reflect trends in other states or regions of the United States due to differences in baseline opioid use disorder rates and policies. We were not able to separate the reason for substance-related calls, as EMS providers generally choose nonspecific reasons for transport, such as “overdose” or “substance use.” For the opioid-related analysis, we likely missed cases that were coded as nonspecific, for example “overdose” or “substance use.” Finally, our data only extend through May 15, 2020 and further trends after this time may have developed.
Conclusions
After an initial decline in substance-related ambulance calls following a statewide declaration of emergency, calls for substance use increased while calls for other reasons remained lower than pre-COVID-19 levels. These findings confirmed our hypothesis that patients with substance use disorders are likely disproportionately affected by the secondary effects of the COVID-19 pandemic, reaching pre-COVID-19 levels of EMS use while overall EMS use remained low. Communities should be aware of these vulnerable patients and can consider providing continuing access to treatment and support groups (even if only virtual) and novel interventions such as leave-behind naloxone.
Acknowledgments
This work was funded by National Institutes of Health grant 1-R01-DA044167. Additional support for statistical analysis was provided by Harvard Catalyst. The funding sources were not involved in the study design, collection, analysis or interpretation of the data, writing of the report, or decision to submit the report for publication. The conclusions in this article are those of the authors and do not necessarily represent the official position of the funders.
Appendix A.
List of clinical impressions, complaints and dispatch reasons defined as substance-related calls. Definitions in bold represent those specific to opioids
Adverse effect of other drugs, medicaments and biological substances, initial encounter (T50.995A)
Adverse effect of other primarily systemic and hematological agents (T45.8 × 5)
Adverse effect of unspecified agents primarily affecting the gastrointestinal system (T47.95)
Adverse effect of unspecified drugs primarily affecting the autonomic nervous system (T44.905)
Adverse effect of unspecified drugs, medicaments and biological substances, initial encounter (T50.905A)
Adverse effect of unspecified nonopioid analgesic, antipyretic and antirheumatic, initial encounter (T39.95XA)
Adverse effect of unspecified primarily systemic and hematological agent (T45.95)
Adverse effect of unspecified systemic antibiotic (T36.95)
Alcohol abuse (F10.1)
Alcohol abuse with intoxication (F10.120)
Alcohol abuse with intoxication, unspecified (F10.129)
Alcohol abuse with other alcohol-induced disorder (F10.188)
Alcohol abuse, uncomplicated (F10.10)
Alcohol dependence (F10.2)
Alcohol dependence with alcohol-induced psychotic disorder with delusions (F10.250)
Alcohol dependence with alcohol-induced psychotic disorder with hallucinations (F10.251)
Alcohol dependence with intoxication delirium (F10.221)
Alcohol dependence with intoxication, unspecified (F10.229)
Alcohol dependence with withdrawal (F10.23)
Alcohol dependence with withdrawal delirium (F10.231)
Alcohol dependence with withdrawal, uncomplicated (F10.230)
Alcohol dependence, uncomplicated (F10.20)
Alcohol detox/withdrawal
Alcohol intoxication
Alcohol related disorders (F10)
Alcohol use, unspecified (F10.9)
Alcohol use, unspecified with intoxication, unspecified (F10.929)
Alcohol use, unspecified with other alcohol-induced disorder (F10.988)
Cannabis abuse (marijuana) (F12.10)
Cannabis related disorders (F12)
Cannabis use, unspecified, uncomplicated (F12.90)
Cocaine abuse (F14.10)
Cocaine related disorders (F14)
Drug induced acute dystonia (G24.02)
Drug overdose accidental (T50.901A)
Drug overdose intentional (T50.902A)
Drug use effects (T88.7)
Dystonic reaction (G24.0)
EENT - Pin point pupils (H57.03)
ETOH abuse
Ingestion/poisoning
Intoxication, alcohol (F10.92)
Opioid abuse (F11.10)
Opioid dependence with withdrawal (F11.23)
Opioid related disorders (F11)
Opioid use, unspecified with unspecified opioid-induced disorder (F11.99)
Opioid use, unspecified with withdrawal (F11.93)
Other psychoactive substance abuse with intoxication, unspecified (F19.129)
Other psychoactive substance abuse, uncomplicated (F19.10)
Other psychoactive substance dependence with intoxication, uncomplicated (F19.220)
Other psychoactive substance dependence, uncomplicated (F19.20)
Other psychoactive substance related disorders (F19)
Other psychoactive substance use, unspecified with intoxication, unspecified (F19.929)
Other psychoactive substance use, unspecified with unspecified psychoactive substance-induced disorder (F19.99)
Other psychoactive substance use, unspecified with withdrawal (F19.93)
Other psychoactive substance use, unspecified with withdrawal, unspecified (F19.939)
Other psychoactive substance use, unspecified, uncomplicated (F19.90)
Other stimulant use, unspecified with intoxication, uncomplicated (F15.920)
Overdose
Overdose, drugs/poisoning (T50.904)
Overdose/poisoning/ingestion
Poisoning by 4-aminophenol derivatives, intentional self-harm, initial encounter (T39.1X2A)
Poisoning by amphetamines, undetermined (T43.624)
Poisoning by cannabis (derivatives), accidental (unintentional), initial encounter (T40.7X1A)
Poisoning by cannabis (derivatives), undetermined (T40.7 × 4)
Poisoning by cocaine, accidental (unintentional), initial encounter (T40.5X1A)
Poisoning by cocaine, undetermined (T40.5 × 4)
Poisoning by diagnostic agents, accidental (unintentional), initial encounter (T50.8X1A)
Poisoning by diagnostic agents, intentional self-harm, initial encounter (T50.8X2A)
Poisoning by heroin, accidental (unintentional), initial encounter (T40.1X1A)
Poisoning by heroin, undetermined (T40.1 × 4)
Poisoning by methadone, undetermined (T40.3 × 4)
Poisoning by opium, undetermined (T40.0 × 4)
Poisoning by other drugs, medicaments and biological substances, undetermined (T50.994)
Poisoning by other opioids, accidental (unintentional), initial encounter (T40.2X1A)
Poisoning by other opioids, accidental (unintentional), sequela (T40.2X1S)
Poisoning by other opioids, undetermined (T40.2 × 4)
Poisoning by other synthetic narcotics, undetermined (T40.4 × 4)
Poisoning by salicylates, undetermined (T39.094)
Poisoning by unspecified antidepressants, intentional self-harm, initial encounter (T43.202A)
Poisoning by unspecified antiepileptic and sedative-hypnotic drugs, undetermined (T42.74)
Poisoning by unspecified drugs, medicaments and biological substances, accidental (unintentional), initial encounter (T50.901A)
Poisoning by unspecified drugs, medicaments and biological substances, intentional self-harm (T50.902)
Poisoning by unspecified drugs, medicaments and biological substances, undetermined (T50.904)
Poisoning by unspecified drugs, medicaments and biological substances, undetermined, initial encounter (T50.904A)
Poisoning by unspecified narcotics, accidental (unintentional), initial encounter (T40.601A)
Poisoning by unspecified narcotics, intentional self-harm, initial encounter (T40.602A)
Poisoning by unspecified narcotics, undetermined (T40.604)
Poisoning by unspecified narcotics, undetermined, initial encounter (T40.604A)
Poisoning by unspecified psychodysleptics [hallucinogens], undetermined (T40.904)
Poisoning by unspecified psychostimulants, accidental (unintentional) (T43.601)
Poisoning by unspecified psychotropic drug, undetermined (T43.94)
Poisoning by, adverse effect of and underdosing of amphetamines (T43.62)
Poisoning by, adverse effect of and underdosing of benzodiazepines (T42.4)
Poisoning by, adverse effect of and underdosing of diuretics and other and unspecified drugs, medicaments and biological substances (T50)
Poisoning by, adverse effect of and underdosing of other and unspecified drugs, medicaments and biological substances (T50.9)
Poisoning by, adverse effect of and underdosing of other and unspecified narcotics (T40.6)
Poisoning by, adverse effect of and underdosing of other drugs, medicaments and biological substances (T50.99)
Poisoning/drug ingestion
Psychoactive substance abuse (F19.10)
Substance - Alcohol dependence with withdrawal (F10.239)
Substance - Alcohol use, with intoxication (F10.92)
Substance - Cannabis related (F12.9)
Substance - Cocaine related (F14.9)
Substance - Hallucinogen related (F16.9)
Substance - Heroin overdose (T40.1)
Substance - Inhalant related (F18.9)
Substance - Nonspecified sedative, hypnotic or anxiolytic related (F13.9)
Substance - Opioid related (F11.9)
Substance - Poisoning by cannabis derivatives/synthetic (K2) (T40.7)
Substance - Poisoning: Overdose of medication (intentional self-harm/suicidal) (T50.992)
Substance - Poisoning: Overdose of unspecified medication/substance (accidental) (T50.901)
Substance - Psychoactive substance related (F19.9)
Substance - Unspecified overdose (T50.90)
Substance - Drug abuse
Substance - Drug abuse
Toxic effect of unspecified substance, intentional self-harm, initial encounter (T65.92XA)
Unspecified adverse effect of drug or medicament, initial encounter (T88.7XXA)
References
- 1.Centers for Disease Control and Prevention. Prescription painkiller overdoses at epidemic levels. November 1, 2011. Available from: https://www.cdc.gov/media/releases/2011/p1101_flu_pain_killer_overdose.html.
- 2.Centers for Medicare and Medicaid Services. Ongoing emergencies and disasters. October 23, 2020. Available from: https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/Current-Emergencies/Ongoing-emergencies.
- 3.National Institute on Drug Abuse. Overdose death rates. October 23, 2020. Available from: https://www.drugabuse.gov/drug-topics/trends-statistics/overdose-death-rates.
- 4.Centers for Disease Control and Prevention. Cases and deaths in the US. October 23, 2020. Available from: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/us-cases-deaths.html.
- 5.Volkow ND. Collision of the COVID-19 and addiction epidemics. Ann Intern Med. 2020;173(1):61–2. doi: 10.7326/M20-1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoffman J With meetings banned, millions struggle to stay sober on their own. New York Times. March 26, 2020. https://www.nytimes.com/2020/03/26/health/coronavirus-alcoholics-drugs-online.html. [Google Scholar]
- 7.Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, Gundlapalli AV, National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 Pandemic on Emergency Department Visits - United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.United Nations Office on Drugs and Crime. COVID-19 and the drug supply chain: from production and trafficking to use. Available from: https://www.unodc.org/documents/data-and-analysis/covid/Covid-19-and-drug-supply-chain-Mai2020.pdf.
- 9.Commonwealth of Massachusetts. Order assuring continued operation of essential services in the Commonwealth, closing certain workplaces, and prohibiting gatherings of more than 10 people. October 23, 2020. Available from: https://www.mass.gov/doc/march-23-2020-essential-services-and-revised-gatherings-order/download.
- 10.Munjal KG, Silverman RA, Freese J, Braun JD, Kaufman BJ, Isaacs D, Werner A, Webber M, Hall CB, Prezant DJ. Utilization of emergency medical services in a large urban area: description of call types and temporal trends. Prehosp Emerg Care. 2011;15(3):371–80. doi: 10.3109/10903127.2011.561403. [DOI] [PubMed] [Google Scholar]
- 11.Becker WC, Fiellin DA. When epidemics collide: Coronavirus Disease 2019 (COVID-19) and the Opioid Crisis. Ann Intern Med. 2020;173(1):59–60. doi: 10.7326/M20-1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alexander GC, Stoller KB, Haffajee RL, Saloner B. An epidemic in the midst of a pandemic: Opioid use disorder and COVID-19. Ann Intern Med. 2020;173(1):57–8. doi: 10.7326/M20-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wakeman SE, Green TC, Rich J. An overdose surge will compound the COVID-19 pandemic if urgent action is not taken. Nat Med. 2020;26(6):819–20. doi: 10.1038/s41591-020-0898-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Melamed OC, Hauck TS, Buckley L, Selby P, Mulsant BH. COVID-19 and persons with substance use disorders: inequities and mitigation strategies. Subst Abus. 2020;41(3):286–91. doi: 10.1080/08897077.2020.1784363. [DOI] [PubMed] [Google Scholar]
- 15.Hochstatter KR, Akhtar WZ, Dietz S, Pe-Romashko K, Gustafson DH, Shah DV, Krechel S, Liebert C, Miller R, El-Bassel N, et al. Potential influences of the COVID-19 pandemic on drug use and HIV care among people living with HIV and substance use disorders: experience from a pilot mHealth intervention. AIDS Behav. 2020;23:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slavova S, Rock P, Bush HM, Quesinberry D, Walsh SL. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214:108176. doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American College of Emergency Physicians. Public poll: emergency care concerns amidst COVID-19. April 2020. Available from: https://www.emergencyphysicians.org/globalassets/emphysicians/all-pdfs/acep-mc-covid19-april-poll-analysis.pdf.
- 18.Levine M, Sanko S, Eckstein M. Assessing the risk of prehospital administration of naloxone with subsequent refusal of care. Prehosp Emerg Care. 2016;20(5):566–9. doi: 10.3109/10903127.2016.1142626. [DOI] [PubMed] [Google Scholar]
- 19.Weiner SG, Baker O, Bernson D, Schuur JD. One-year mortality of patients after emergency department treatment for nonfatal opioid overdose. Ann Emerg Med. 2020;75(1):13–7. doi: 10.1016/j.annemergmed.2019.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Commonwealth of Massachusetts. Leave-behind naloxone. October 23, 2020.Available from: https://www.mass.gov/doc/emergency-release-of-613-leave-behind-naloxone/download.


