Abstract
Brain arteriovenous malformations (bAVMs) are relatively rare, although their potential for secondary intracranial haemorrhage (ICH) makes their diagnosis and management essential to the community. Currently, invasive therapies (surgical resection, stereotactic radiosurgery and endovascular embolisation) are the only interventions that offer a reduction in ICH risk. There is no designated medical therapy for bAVM, although there is growing animal and human evidence supporting a role for bevacizumab to reduce the size of AVMs. In this single-arm pilot study, two patients with large bAVMs (deemed unresectable by an interdisciplinary team) received bevacizumab 5 mg/kg every 2 weeks for 12 weeks. Due to limitations of external funding, the intended sample size of 10 participants was not reached. Primary outcome measure was change in bAVM volume from baseline at 26 and 52 weeks. No change in bAVM volume was observed 26 or 52 weeks after bevacizumab treatment. No clinically important adverse events were observed during the 52-week study period. There were no observed instances of ICH. Sera vascular endothelial growth factor levels were reduced at 26 weeks and returned to baseline at 52 weeks. This pilot study is the first to test bevacizumab for patients with bAVMs. Bevacizumab therapy was well tolerated in both subjects. No radiographic changes were observed over the 52-week study period. Subsequent larger clinical trials are in order to assess for dose-dependent efficacy and rarer adverse drug effects.
Trial registration number: NCT02314377.
Keywords: cerebrovascular, stroke, pharmacology, neurosurgery
Introduction
Brain arteriovenous malformation (bAVM) is a rare disease with a population prevalence of 10–18 per 100 000 people.1–3 These complex tangles of abnormal, dilated vessels are a significant source of intracranial haemorrhage (ICH) with annual risk of rupture estimated to be 1%–2% per year for previously unruptured bAVMs.4–8
ICH is the most significant source of morbidity and mortality in patients with bAVMs.9 Currently, interventional therapies (surgical resection, stereotactic radiosurgery and endovascular embolisation) are the only treatments that reduce risk of bAVM rupture.7 9–11 Unfortunately, an appreciable fraction of patients (≈20%) cannot be offered safe, effective intervention due to the size, location and/or characteristics of the bAVM (eg, large nidus, deep venous drainage, eloquent location).12 13 Furthermore, treatment of unruptured bAVMs—roughly half of all cases—has become increasingly controversial because the natural history for these patients may be less morbid than invasive therapies themselves.8 14 In the prospective, randomised ARUBA trial (A Randomised trial of Unruptured Brain Arteriovenous malformations), death or symptomatic stroke occurred in 10.1% of patients receiving medical (symptomatic) management alone, compared with 30.7% in patients receiving interventional management.14 15 This seminal work shapes our current management of patients with bAVM, encouraging a shift towards conservative management in patients who might have historically undergone partial or palliative intervention.
A growing body of literature demonstrates that bAVMs are dynamically evolving, actively inflammatory, angiogenic lesions, akin to a slow-growing vascular tumour.16–19 Despite the availability of a number of promising drugs targeting angiogenesis, inflammation and vessel integrity, there is currently no medical therapy approved to treat bAVMs. One such promising medical therapy is the angiogenesis inhibitor bevacizumab (Avastin), a recombinant humanised monoclonal antibody that blocks angiogenesis by inhibiting vascular endothelial growth factor (VEGF) A. Bevacizumab is Food and Drug Administration approved for the treatment of several different cancers, but has also been used off-label to successfully treat hereditary haemorrhagic telangiectasia (HHT), an autosomal dominant disease characterised by vascular malformations including bAVMs.20 21 High expression levels of VEGF have been reported both in resected bAVM tissue and in plasma from patients with HHT.22–24 Several studies have reported significant improvements in HHT-related symptoms with bevacizumab use, including decreases in frequency and severity of epistaxis,25 improvement in chronic anaemia and need for blood transfusion20 and improvement in liver AVM-related heart failure.26 A phase II study showed that six doses of bevacizumab administered intravenously over 12 weeks normalised cardiac output in patients with liver AVM-related heart failure, with a roughly 20% reduction in cardiac output compared with pretreatment values.21 This was probably largely due to a decrease in shunting through the liver AVMs, although other possible explanations were not evaluated.
Bevacizumab has been associated with reversal of vascular dysplasia in animal models of bAVM,27 28 and case reports of bevacizumab use in patients with sporadic bAVM for adverse radiation effects have demonstrated a reduction in perilesional oedema by imaging and marked improvement in symptoms.29 30 However, there have been no clinical trials that aim to determine the effect of the anti-VEGF antibody in these patients. The present study fills an important gap in knowledge by determining the feasibility and safety of bevacizumab treatment in two patients with large inoperable bAVMs.
Methods
Study overview
This study is a single-armed pilot study testing the impact of administration of intravenous bevacizumab over the course of 12 weeks. Patients with bAVMs were identified from the prospective University of California, San Francisco Brain AVM Project registry and were reviewed and screened for their ability to comply with all research and clinical procedures. Inclusion and exclusion criteria are outlined in box 1.
Box 1. Inclusion and exclusion criteria.
Inclusion criteria
Brain arteriovenous malformations deemed unsuitable for invasive treatment OR patient elected to defer invasive treatment OR failed conventional therapy.
Age >18 years at time of first study drug administration.
Spetzler-Martin grade III–V lesion.
Progressive or disabling signs and symptoms as determined by the study investigators.
Adequate bone marrow function (white blood cells >3000/μL, absolute neutrophil count >1500/mm3, platelet count >100 000/mm3 and haemoglobin >0.1 g/L), adequate liver function (serum glutamic-oxaloacetic transaminase and bilirubin <1.5 times upper limit of normal) and adequate renal function (creatinine <1.5 mg/dL) within 14 days before starting therapy.
Exclusion criteria
Diffuse lesion that cannot be assessed in terms of volume by cross-sectional imaging on MRI.
Inability to undergo MRI scans.
Urine protein >100 mg/dL or >2+ protein (depending on units used in assay).
Coagulation disorders, for example, thrombocytopenia, coagulopathy or anticoagulant therapy (Plavix and aspirin are not excluded).
Unstable medical or psychiatric illness.
Haemorrhagic presentation.
Atrial fibrillation.
Clinically significant thrombotic episode within the last 24 weeks.
Inadequately controlled hypertension (defined as systolic blood pressure >150 mm Hg and/or diastolic blood pressure >100 mm Hg on antihypertensive medications, hypertensive crisis or hypertensive encephalopathy).
Major cardiovascular or peripheral vascular disease.*
Major surgical procedure, open biopsy or significant traumatic injury within 4 weeks of beginning bevacizumab or the anticipation of need for major surgical procedure during the course of the study.
Core biopsy or other minor surgical procedure, within 7 days days prior to bevacizumab.
Serious, non-healing wound, ulcer or bone fracture.
Pregnant or breast feeding. Effective contraception (men and women) must be used in subjects of childbearing potential.
On any other experimental agents/clinical trials.
*New York Heart Association grade II or greater congestive heart failure, myocardial infarction or unstable angina within 12 months prior to study enrolment, symptomatic peripheral vascular disease.
Study procedures
Table 1 outlines the schedule of assessments, examinations and laboratory testing participants underwent during the study interval. Bevacizumab (5 mg/kg every 2 weeks) was administered by intravenous infusion over the course of 12 weeks with observation over a 40-week follow-up period; this dose and schedule was chosen to emulate the HHT hepatic AVM phase II trial given the success that study documented as well as the absence of significant adverse side effects.26 Screening history and physical examination were performed within 14 days of initial treatment, and interim history and physical examination were repeated every other week for 12 weeks prior to bevacizumab infusions. Routine labs were monitored every other week for 12 weeks, and then in follow-up at 26 weeks, and at 52 weeks. Angiogenic and inflammatory markers were monitored at baseline, 12 weeks, 26 weeks and 52 weeks. Patients were followed weekly for toxicities for the first 16 weeks and again at 26 and 52 weeks. All patient records were reviewed weekly by the principal investigator for adverse events.
Table 1.
Schedule of clinical events
| Assessments/Procedures (weeks) |
Screen | W2 #1 |
W4 #2 |
W6 #3 |
W8 #4 |
W10 #5 |
W12 #6 |
W14 | W16 | W26 | W52 |
| Written informed consent/HIPPA | X | ||||||||||
| Inclusion/Exclusion criteria | X | ||||||||||
| Baseline medical history and physical examination | X | ||||||||||
| Physical examination | X | X | X | X | X | X | X | ||||
| Interim history | X | X | X | X | X | X | X | X | |||
| Toxicity assessment, adverse experiences, modified Rankin score | X | X | X | X | X | X | X | X | X | X | X |
| NIH Stroke Scale, Neuro-QoL Questionnaire | X | X | X | X | |||||||
| ECG | X | ||||||||||
| Administer study drug | X | X | X | X | X | X | |||||
| Laboratory evaluation (plasma angiogenic/inflammatory markers): VEGF, FGF2, CRP, ESR, IL-1, IL-2, IL-6, MPO, TNF-α | X | X | X | X | |||||||
| Laboratory evaluations*: complete blood count with differential, creatinine, blood urea nitrogen, liver function tests, prothrombin time, partial thromboplastin time | X | X | X | X | X | X | X | X | X | ||
| Laboratory evaluations*: urine protein/creatinine ratio (urine dipstick for protein prior to infusions) | X | X | X | X | |||||||
| MRI | X | X | X | ||||||||
| Pregnancy test (if applicable) | X | X | X |
*Completed within 3 days of bevacizumab infusion when applicable.
CRP, C reactive protein; ESR, erythrocyte sedimentation rate; FGF2, fibroblast growth factor 2; IL, interleukin; MPO, myeloperoxidase; Neuro-QoL, Quality of Life in Neurologic Disorders; NIH, National Institutes of Health; TNF-α, tumour necrosis factor α; VEGF, vascular endothelial growth factor.
Imaging/Volume measurements
MR time-of-flight (TOF) imaging, standard T1-weighted and T2-weighted sequences and iron-sensitive sequences were obtained at the baseline examination, 26 weeks and 52 weeks. A subspecialty-certified neuroradiologist (DLC) reviewed all MRI sequences to assess for bAVM volume, silent haemorrhage and vessel wall changes. bAVM volume was assessed by review of standardised 1.5 mm slices in the axial plane. A cross-sectional area of the bAVM nidus at each slice level was acquired via TOF MR angiography sequences. Volumes were estimated by summing the imputed volume of each slice. Silent haemorrhage was assessed by review of susceptibility-weighted imaging for signal loss from hemosiderin. High-resolution vessel wall imaging MRI was obtained using a black-blood pregadolinium and postgadolinium 0.6 mm isotropic 3D CUBE T1-weighted sequence. Two neuroradiologists (DLC and LE) identified the number of feeding arteries and draining veins and the distribution and degree of AVM postcontrast hyperintensity at and around the vessel wall. Vessel wall hyperintensity inside and outside of the nidus was ranked on a 5-point scale.
Analysis
Safety of bevacizumab treatment was assessed via interim histories, toxicity assessments, physical examination, routine basic laboratory measurements and NIH Stroke Scale Assessments. The preliminary primary efficacy end point of the study was change in bAVM volume from pretreatment MRI at 26 and 52 weeks. A sample size of 10 patients was proposed in order to provide 82% power to detect a 13% change in bAVM volume. A preliminary secondary efficacy outcome was change in serum VEGF level at 12, 26 and 52 weeks. Efficacy end points were compared descriptively. All data were tabulated and descriptive statistics generated using Microsoft Excel.
Results
Subjects
Twenty-one patients were screened and 15 patients screened eligible to participate in the study. Due to limitations of funding unrelated to study design or drug safety, two patients were consented by the research physician to participate in this pilot drug study.
Subject 1 was a middle-aged patient with medical history of obesity and depression who presented with a large, symptomatic, left frontoparietal AVM (Spetzler-Martin grade V), which was formally diagnosed in approximately 30 years prior when the patient began having seizures. Since diagnosis, the patient experienced progressive weakness of the right arm and leg. Seizures were controlled with phenytoin extended-release 400 mg daily and phenobarbitol 100 mg daily. The patient denied all other medical history or neurological symptoms. The patient had neither an AVM-related haemorrhage nor any attempt at definitive AVM treatment prior to start of the trial.
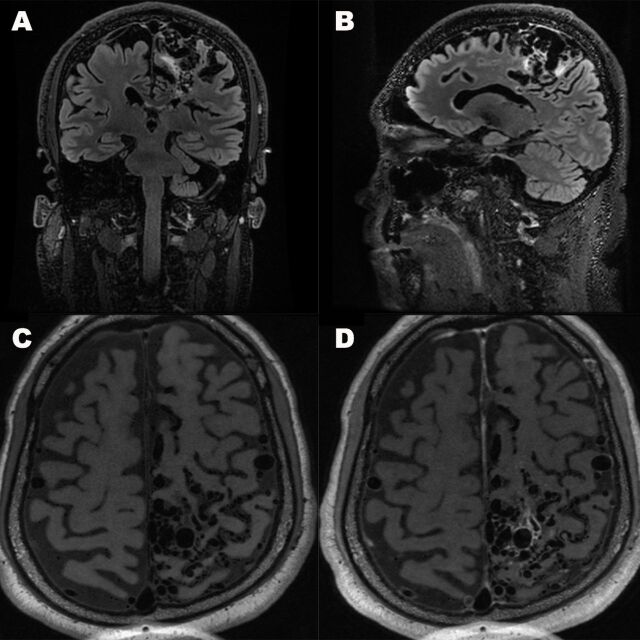
Cerebral angiography 10 years prior to this study revealed a large AVM in the left frontoparietal region with arterial supply from the left anterior cerebral, middle cerebral and posterior cerebral arteries. Baseline MR (figure 1) immediately prior to this study confirmed the presence a large left frontoparietal AVM centred within the paracentral lobule with markedly dilated left anterior and posterior circulation arterial supply and superficial and deep venous drainage.
Figure 1.
Composite image (patient 1) demonstrating representative coronal (A) and sagittal (B) reformats from a three-dimensional whole brain black blood variable flip angle T1-weighted fast spin echo sequence (CUBE). Representative high-resolution T1 precontrast (C) and postcontrast (D) series demonstrating nidal vessel wall enhancement.
Subject 2 was a middle-aged patient who presented with a large, symptomatic, right temporal bAVM (Spetzler-Martin grade IV). The patient reported migraines for 15 years and seizures for 11 years. Seizures reported to occur one to two times per month, refractory to levetiracetam 500 mg two times per day. The patient endorsed light and sound sensitivity, dizziness, nausea and occasional left arm numbness that lasted a few minutes per episode, and denied all other medical history or neurological symptoms. The patient had neither an AVM-related haemorrhage nor any attempt at definitive AVM treatment prior to start of the trial.
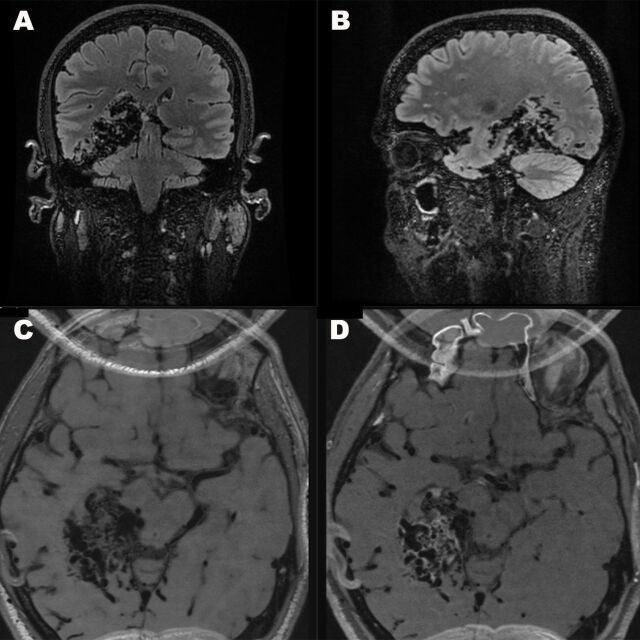
Baseline MR (figure 2) revealed a large right temporal lobe AVM with arterial supply from right middle cerebral artery, right anterior cerebral arteries, right posterior cerebral artery and right external carotid artery. Deep venous drainage of the AVM was identified via the basal vein of Rosenthal into the vein of Galen and straight sinus. Superficial venous drainage into cortical veins over the parietal and occipital lobes was noted.
Figure 2.
Composite image (patient 2) demonstrating representative coronal (A) and sagittal (B) reformats from a three-dimensional whole brain black blood variable flip angle T1-weighted fast spin echo sequence (CUBE). Representative high-resolution T1 precontrast (C) and postcontrast (D) series demonstrating nidal vessel wall enhancement.
Analysis of treatment safety
Bevacizumab treatment was well tolerated in both subjects, as assessed by interim histories, toxicity assessments, physical examination, routine basic laboratory measurements and NIH Stroke Scale Assessments. Subject 2 was noted to have an increase in total bilirubin to a maximum of 2.4 (direct bilirubin remained normal) while the study drug was being administered, which resolved by the 26-week laboratory check. Both patients had seizure events during the study interval which were consistent with their previous pattern of epilepsy. Otherwise, no clinically important adverse events were observed during the 52-week study period.
Analysis of treatment efficacy
The preliminary primary outcome of the study was change in bAVM volume from pretreatment MRI. Baseline MR imaging revealed a bAVM volume of 35.8 cc in subject 1 and 36.9 cc in subject 2. Volume measurements at 26 and 52 weeks revealed no change in bAVM volume.
A preliminary secondary outcome of the study was serum VEGF levels, measured at baseline, 12 weeks, 26 weeks and 52 weeks. Table 2 outlines the inflammatory and angiogenic markers tracked during this study. Notably, both subjects had normal/high VEGF levels at baseline, low VEGF levels at 26 weeks and normal/high VEGF levels at 52 weeks.
Table 2.
Inflammatory/Angiogenic markers
| Marker (reference range) | Baseline | 12 Weeks | 26 Weeks | 52 Weeks |
| VEGF (pg/mL) (31–86) | ||||
| Subject 1 | 57 | 91 (H) | <31 (L) | 74 |
| Subject 2 | 129 (H) | NA* | <3 1 (L) | 93 (H) |
| FGF2 (pg/mL) (≤6.5) | ||||
| Subject 1 | 1.7 | 5.6 | 8.3 (H) | 45 (H) |
| Subject 2 | 30 (H) | NA* | 22.0 (H) | 19.5 (H) |
| CRP (mg/L) (≤3.0) | ||||
| Subject 1 | 0.6 | 6.6 (H) | 0.7 | 0.5 |
| Subject 2 | 5.6 (H) | 6.4 (H) | 0.8 | 2.2 |
| ESR (mm/hour) (≤20) | ||||
| Subject 1 | 2 | 2 | NA* | 2 |
| Subject 2 | 6 | 6 | 2 | NA* |
| IL-2 (pg/mL) (<38) | ||||
| Subject 1 | <38 | <38 | <38 | <38 |
| Subject 2 | <38 | <38 | <38 | <38 |
| IL-6 (pg/mL) (0.31–5.00) | ||||
| Subject 1 | 3.41 | 1.92 | 2.04 | 2.75 |
| Subject 2 | 1.55 | 0.79 | 1.08 | 0.86 |
| IL-1β (pg/mL) (<3.9) | ||||
| Subject 1 | <3.9 | <3.9 | NA* | <3.9 |
| Subject 2 | <3.9 | <3.9 | <3.9 | <3.9 |
| MPO (AI) (<1.0) | ||||
| Subject 1 | <1.0 | <1.0 | <1.0 | <1.0 |
| Subject 2 | <1.0 | <1.0 | <1.0 | <1.0 |
| TNF-α (pg/mL) (0.56–1.40) | ||||
| Subject 1 | <1 (L) | <1 (L) | <1 (L) | <1 (L) |
| Subject 2 | 1.05 | 1.16 | <1 (L) | 1.3 |
*These data were not collected.
AI, antibody index; CRP, C reactive protein; ESR, erythrocyte sedimentation rate; FGF2, fibroblast growth factor 2; H, high; IL, interleukin; L, low; MPO, myeloperoxidase; TNF-α, tumour necrosis factor α; VEGF, vascular endothelial growth factor.
Vessel wall imaging
Iron-sensitive imaging revealed no bleeding beyond that found in baseline imaging. Neither subject had perivascular enhancement outside of the nidus. There were no observed changes in vessel wall hyperintensity.
Discussion
In the first clinical trial to date of anti-VEGF therapy in patients with bAVM, we found that bevacizumab treatment was not associated with adverse events in two patients with large, unresectable bAVMs. Given the substantial percentage of patients with bAVM with unresectable lesions due to bAVM size, location and/or other characteristics, there has been increasing interest in disease-modifying medical therapies to reduce the risk of bAVM haemorrhage. Despite the clear need for medical therapeutics, a recent study identifies 38 active bAVM clinical trials, only the present trial has investigated medical management.31
Currently, therapeutic targets are largely being aimed at the underlying pathways known to impact the bAVM life-cycle and the integrity of surrounding brain parenchyma. Specifically, in vitro studies have focused on bAVM mechanisms for growth and rupture including overexpression of angiogenic factors,32 33 stabilising the blood-brain barrier34 35 and inhibition of matrix metalloproteinases.36 37 Anti-angiogenic agents have been quickest to use in patients with bAVM, given the growing collection of series documenting the presence of RAS and RAS-related gene mutations in brain and spine AVMs.33 38–42 The RAS signalling pathway includes the RAF-MEK-MAPK/ERK cascade, which has been shown to impact VEGF expression and vice versa.43 44 As such, therapeutics targeting RAS-opathies, whether through inhibiting VEGF (bevacizumab), BRAF (vemurafenib)or MEK (trametinib), have gained increasing interest. These efforts are encouraging, such that RAS-modifying medications are now used in specific, compassionate use instances. For example, Edwards et al described a quantitative response to the MEK inhibitor, trametinib, in a child with a large, thoracic metameric AVM.32 As promising as RAS-based therapies for AVMs might be, RAS superfamily mutations are not identified in a fraction of cases. This may be related to tissue heterogeneity but may also indicate that there are multiple genetic drivers of AVM formation, growth and rupture. Promising studies of thalidomide and rapamycin for AVM indicate a role for therapeutic targets outside of the RAS superfamily.35 45 Further study is needed to characterise the genomic and somatic drivers of bAVMs and to aid in identifying subpopulations more and less susceptible to medical and potential gene therapies.
There have been several case reports of bevacizumab use in patients with sporadic bAVM for treatment of adverse radiation effects after radiosurgery.29 30 Treatment with bevacizumab (2.5 mg/kg, followed 1 week later by 7.5 mg/kg) resulted in marked improvement in symptoms (severe headache and hemiparesis refractory to steroid therapy and pain management) and resolution of perilesional oedema by imaging.30 Interestingly, 1 year after gamma knife radiosurgery and 10 weeks after bevacizumab treatment, angiography demonstrated nidus obliteration and no evidence of arteriovenous shunting. The relative contribution of the radiosurgical effect and any potential anti-VEGF effect cannot be separated, but it commonly takes several years for nidus obliteration to be achieved after radiosurgery. Deibert et al similarly reported mean reductions in adverse radiation effects as measured by contrast enhancement and T2 hyperintensity in four patients with bAVMs who received an average dose of 4.4 mg/kg of bevacizumab for an average of 2.5 doses.29 The authors did not report change in bAVM volume, as it was not the scope of the research, although all four patients improved clinically and no adverse events were reported.
There has been concern over the use of bevacizumab in patients with intracranial disease because of the potential increased risk of bleeding. Case reports have described instances of ICH in patients with small cell carcinoma and colon cancer treated with bevacizumab.46 47 Until recently, these concerns have led to the routine exclusion of patients with brain metastases from bevacizumab trials, despite larger studies that have found no relationship between bevacizumab treatment and ICH.48 A similar argument has been made to exclude patients with bAVMs from bevacizumab trials. In a trial of bevacizumab for patients with liver-AVM-related heart failure, bevacizumab was found to normalise cardiac output, but patients with bAVMs were excluded from this trial.21 Currently, there is no literature noting an increased rate of AVM-related haemorrhage with bevacizumab therapy; the present study is consistent with the existing, although limited data.
Due to limitations of funding and patient recruitment, our study did not meet the goal of 10 patients. Thus, while this is a major step in the medical management of bAVMs, our study is underpowered to detect the hypothesised change in bAVM volume. Our safety data, and specifically the lack of ICH noted in our patients, is an important data point, but future larger trials are warranted to more comprehensively assess this risk. With respect to funding, this trial was designed with support from industry sponsors, which was ultimately withdrawn for reasons unrelated to study design or drug safety, leading to inadequate funding to support a larger trial. While recruitment was not the limiting factor, this trial had very narrow inclusion criteria which could be broadened to increase catchment in future trials. Additionally, given the relatively large volume bAVMs in our study participants, it may be more difficult to appreciate small changes in bAVM volume. Future trials might consider including patients with smaller bAVMs. A final limitation of this trial is the use of only one dosing schedule, limiting the ability to assess the efficacy of bevacizumab in reducing ICH risk in patients with bAVM.
This single-arm pilot study is the first to test anti-VEGF therapy in patients with bAVM, and one of very few studies to attempt medical therapy of any kind in this patient population. Results from this pilot study lay the foundation for larger trials, with the goal of broadening bAVM management strategies and offering, for the first time, a medical therapy for patients with bAVMs that are not amenable to surgical management.
Acknowledgments
The authors would like to thank the patients for enrolling in this trial and William L. Young, MD, deceased, for his seminal contributions to AVM research and for laying the foundation for translational research.
Footnotes
Contributors: RM: data analysis, manuscript composition. HS, HK: trial design, data analysis, manuscript composition. NK, WS, PKS, JLC: data safety monitoring, trial design and manuscript composition. MAD: clinical research coordinator. JN, CEMcC: trial design, manuscript composition. DAS, LE: imaging data analysis, manuscript composition. DLC: all of the above, study oversight.
Funding: This work was supported by the American Heart Association (16GRNT30420016), the National Institutes of Health (R01 HL122774, NS027713 and NS112819) and the Michael Ryan Zodda Foundation (no award number available).
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Approval was obtained through the institutional review board at the University of California, San Francisco (UCSF). All patients provided written informed consent.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: The data that support the findings of this study are available from the corresponding author, on reasonable request.
References
- 1.Berman MF, Sciacca RR, Pile-Spellman J, et al. The epidemiology of brain arteriovenous malformations. Neurosurgery 2000;47:389–97. 10.1097/00006123-200008000-00023 [DOI] [PubMed] [Google Scholar]
- 2.Al-Shahi R, Fang JSY, Lewis SC, et al. Prevalence of adults with brain arteriovenous malformations: a community based study in Scotland using capture-recapture analysis. J Neurol Neurosurg Psychiatry 2002;73:547–51. 10.1136/jnnp.73.5.547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gabriel RA, Kim H, Sidney S, et al. Ten-Year detection rate of brain arteriovenous malformations in a large, multiethnic, defined population. Stroke 2010;41:21–6. 10.1161/STROKEAHA.109.566018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Komiyama M. Pathogenesis of brain arteriovenous malformations. Neurol Med Chir 2016;56:317–25. 10.2176/nmc.ra.2016-0051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rutledge WC, Ko NU, Lawton MT, et al. Hemorrhage rates and risk factors in the natural history course of brain arteriovenous malformations. Transl Stroke Res 2014;5:538–42. 10.1007/s12975-014-0351-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yamada S, Takagi Y, Nozaki K, et al. Risk factors for subsequent hemorrhage in patients with cerebral arteriovenous malformations. J Neurosurg 2007;107:965–72. 10.3171/JNS-07/11/0965 [DOI] [PubMed] [Google Scholar]
- 7.Brown RD, Wiebers DO, Forbes G, et al. The natural history of unruptured intracranial arteriovenous malformations. J Neurosurg 1988;68:352–7. 10.3171/jns.1988.68.3.0352 [DOI] [PubMed] [Google Scholar]
- 8.Al-Shahi Salman R, White PM, Counsell CE, et al. Outcome after conservative management or intervention for unruptured brain arteriovenous malformations. JAMA 2014;311:1661–9. 10.1001/jama.2014.3200 [DOI] [PubMed] [Google Scholar]
- 9.Halim AX, Johnston SC, Singh V, et al. Longitudinal risk of intracranial hemorrhage in patients with arteriovenous malformation of the brain within a defined population. Stroke 2004;35:1697–702. 10.1161/01.STR.0000130988.44824.29 [DOI] [PubMed] [Google Scholar]
- 10.van Beijnum J, Lovelock CE, Cordonnier C, et al. Outcome after spontaneous and arteriovenous malformation-related intracerebral haemorrhage: population-based studies. Brain 2009;132:537–43. 10.1093/brain/awn318 [DOI] [PubMed] [Google Scholar]
- 11.Fults D, Kelly DL. Natural history of arteriovenous malformations of the brain: a clinical study. Neurosurgery 1984;15:658–62. 10.1227/00006123-198411000-00003 [DOI] [PubMed] [Google Scholar]
- 12.Han PP, Ponce FA, Spetzler RF. Intention-to-treat analysis of Spetzler-Martin grades IV and V arteriovenous malformations: natural history and treatment paradigm. J Neurosurg 2003;98:3–7. 10.3171/jns.2003.98.1.0003 [DOI] [PubMed] [Google Scholar]
- 13.Khaw AV, Mohr JP, Sciacca RR, et al. Association of infratentorial brain arteriovenous malformations with hemorrhage at initial presentation. Stroke 2004;35:660–3. 10.1161/01.STR.0000117093.59726.F9 [DOI] [PubMed] [Google Scholar]
- 14.Mohr JP, Parides MK, Stapf C, et al. Medical management with or without Interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet 2014;383:614–21. 10.1016/S0140-6736(13)62302-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohr JP, Overbey JR, Hartmann A, et al. Medical management with Interventional therapy versus medical management alone for unruptured brain arteriovenous malformations (ARUBA): final follow-up of a multicentre, non-blinded, randomised controlled trial. Lancet Neurol 2020;19:573–81. 10.1016/S1474-4422(20)30181-2 [DOI] [PubMed] [Google Scholar]
- 16.Davidson AS, Morgan MK. The embryologic basis for the anatomy of the cerebral vasculature related to arteriovenous malformations. J Clin Neurosci 2011;18:464–9. 10.1016/j.jocn.2010.12.004 [DOI] [PubMed] [Google Scholar]
- 17.Stapleton CJ, Armstrong DL, Zidovetzki R, et al. Thrombospondin-1 modulates the angiogenic phenotype of human cerebral arteriovenous malformation endothelial cells. Neurosurgery 2011;68:1342–53. 10.1227/NEU.0b013e31820c0a68 [DOI] [PubMed] [Google Scholar]
- 18.Jabbour MN, Elder JB, Samuelson CG, et al. Aberrant angiogenic characteristics of human brain arteriovenous malformation endothelial cells. Neurosurgery 2009;64:139–48. 10.1227/01.NEU.0000334417.56742.24 [DOI] [PubMed] [Google Scholar]
- 19.Mouchtouris N, Jabbour PM, Starke RM, et al. Biology of cerebral arteriovenous malformations with a focus on inflammation. J Cereb Blood Flow Metab 2015;35:167–75. 10.1038/jcbfm.2014.179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flieger D, Hainke S, Fischbach W. Dramatic improvement in hereditary hemorrhagic telangiectasia after treatment with the vascular endothelial growth factor (VEGF) antagonist bevacizumab. Ann Hematol 2006;85:631–2. 10.1007/s00277-006-0147-8 [DOI] [PubMed] [Google Scholar]
- 21.Dupuis-Girod S, Ginon I, Saurin J-C, et al. Bevacizumab in patients with hereditary hemorrhagic telangiectasia and severe hepatic vascular malformations and high cardiac output. JAMA 2012;307:948–55. 10.1001/jama.2012.250 [DOI] [PubMed] [Google Scholar]
- 22.Sadick H, Naim R, Sadick M, et al. Plasma level and tissue expression of angiogenic factors in patients with hereditary hemorrhagic telangiectasia. Int J Mol Med 2005;15:591–6. 10.3892/ijmm.15.4.591 [DOI] [PubMed] [Google Scholar]
- 23.Hashimoto T, Emala CW, Joshi S, et al. Abnormal pattern of Tie-2 and vascular endothelial growth factor receptor expression in human cerebral arteriovenous malformations. Neurosurgery 2000;47:910–9. 10.1097/00006123-200010000-00022 [DOI] [PubMed] [Google Scholar]
- 24.Cirulli A, Liso A, D'Ovidio F, et al. Vascular endothelial growth factor serum levels are elevated in patients with hereditary hemorrhagic telangiectasia. Acta Haematol 2003;110:29–32. 10.1159/000072411 [DOI] [PubMed] [Google Scholar]
- 25.Epperla N, Hocking W. Blessing for the bleeder: bevacizumab in hereditary hemorrhagic telangiectasia. Clin Med Res 2015;13:32–5. 10.3121/cmr.2013.1205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitchell A, Adams LA, MacQuillan G, et al. Bevacizumab reverses need for liver transplantation in hereditary hemorrhagic telangiectasia. Liver Transpl 2008;14:210–3. 10.1002/lt.21417 [DOI] [PubMed] [Google Scholar]
- 27.Walker EJ, Su H, Shen F, et al. Arteriovenous malformation in the adult mouse brain resembling the human disease. Ann Neurol 2011;69:954–62. 10.1002/ana.22348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walker EJ, Su H, Shen F, et al. Bevacizumab attenuates VEGF-induced angiogenesis and vascular malformations in the adult mouse brain. Stroke 2012;43:1925–30. 10.1161/STROKEAHA.111.647982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deibert CP, Ahluwalia MS, Sheehan JP, et al. Bevacizumab for refractory adverse radiation effects after stereotactic radiosurgery. J Neurooncol 2013;115:217–23. 10.1007/s11060-013-1214-3 [DOI] [PubMed] [Google Scholar]
- 30.Williams BJ, Park DM, Sheehan JP. Bevacizumab used for the treatment of severe, refractory perilesional edema due to an arteriovenous malformation treated with stereotactic radiosurgery. J Neurosurg 2012;116:972–7. 10.3171/2012.1.JNS111627 [DOI] [PubMed] [Google Scholar]
- 31.Raper DMS, Winkler EA, Rutledge WC, et al. An update on medications for brain arteriovenous malformations. Neurosurgery 2020;87:871–8. 10.1093/neuros/nyaa192 [DOI] [PubMed] [Google Scholar]
- 32.Edwards EA, Phelps AS, Cooke D, et al. Monitoring arteriovenous malformation response to genotype-targeted therapy. Pediatrics 2020;146:e20193206. 10.1542/peds.2019-3206 [DOI] [PubMed] [Google Scholar]
- 33.Al-Olabi L, Polubothu S, Dowsett K, et al. Mosaic Ras/MAPK variants cause sporadic vascular malformations which respond to targeted therapy. J Clin Invest 2018;128:1496–508. 10.1172/JCI98589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Winkler EA, Birk H, Burkhardt J-K, et al. Reductions in brain pericytes are associated with arteriovenous malformation vascular instability. J Neurosurg 2018;129:1464–74. 10.3171/2017.6.JNS17860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhu W, Chen W, Zou D, et al. Thalidomide reduces hemorrhage of brain arteriovenous malformations in a mouse model. Stroke 2018;49:1232–40. 10.1161/STROKEAHA.117.020356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hashimoto T, Matsumoto MM, Li JF, et al. Suppression of MMP-9 by doxycycline in brain arteriovenous malformations. BMC Neurol 2005;5:1. 10.1186/1471-2377-5-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frenzel T, Lee CZ, Kim H, et al. Feasibility of minocycline and doxycycline use as potential vasculostatic therapy for brain vascular malformations: pilot study of adverse events and tolerance. Cerebrovasc Dis 2008;25:157–63. 10.1159/000113733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nikolaev SI, Vetiska S, Bonilla X, et al. Somatic activating KRAS mutations in arteriovenous malformations of the brain. N Engl J Med 2018;378:250–61. 10.1056/NEJMoa1709449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hong T, Yan Y, Li J, et al. High prevalence of KRAS/BRAF somatic mutations in brain and spinal cord arteriovenous malformations. Brain 2019;142:23–34. 10.1093/brain/awy307 [DOI] [PubMed] [Google Scholar]
- 40.Goss JA, Huang AY, Smith E, et al. Somatic mutations in intracranial arteriovenous malformations. PLoS One 2019;14:e0226852. 10.1371/journal.pone.0226852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Priemer DS, Vortmeyer AO, Zhang S, et al. Activating KRAS mutations in arteriovenous malformations of the brain: frequency and clinicopathologic correlation. Hum Pathol 2019;89:33–9. 10.1016/j.humpath.2019.04.004 [DOI] [PubMed] [Google Scholar]
- 42.Oka M, Kushamae M, Aoki T, et al. Kras G12D or G12V mutation in human brain arteriovenous malformations. World Neurosurg 2019;126:e1365–73. 10.1016/j.wneu.2019.03.105 [DOI] [PubMed] [Google Scholar]
- 43.Meadows KN, Bryant P, Pumiglia K. Vascular endothelial growth factor induction of the angiogenic phenotype requires Ras activation. J Biol Chem 2001;276:49289–98. 10.1074/jbc.M108069200 [DOI] [PubMed] [Google Scholar]
- 44.Sohn SJ, Sarvis BK, Cado D, et al. Erk5 MAPK regulates embryonic angiogenesis and acts as a hypoxia-sensitive repressor of vascular endothelial growth factor expression. J Biol Chem 2002;277:43344–51. 10.1074/jbc.M207573200 [DOI] [PubMed] [Google Scholar]
- 45.Chelliah MP, Do HM, Zinn Z, et al. Management of complex arteriovenous malformations using a novel combination therapeutic algorithm. JAMA Dermatol 2018;154:1316–9. 10.1001/jamadermatol.2018.3039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tanvetyanon T, Murtagh R, Bepler G. Rupture of a cerebral arteriovenous malformation in a patient treated with bevacizumab. J Thorac Oncol 2009;4:268–9. 10.1097/JTO.0b013e318195a642 [DOI] [PubMed] [Google Scholar]
- 47.Nishimura T, Furihata M, Kubo H, et al. Intracranial hemorrhage in patients treated with bevacizumab: report of two cases. World J Gastroenterol 2011;17:4440–4. 10.3748/wjg.v17.i39.4440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang L, Chen C-J, Guo X-L, et al. Bevacizumab and risk of intracranial hemorrhage in patients with brain metastases: a meta-analysis. J Neurooncol 2018;137:49–56. 10.1007/s11060-017-2693-4 [DOI] [PMC free article] [PubMed] [Google Scholar]