Highlights
-
•
WHO and ILO are developing joint estimates of work-related burden of disease and injury.
-
•
This paper synthesizes evidence on prevalence of occupational noise exposure.
-
•
65 studies were included (157,370 participants, 54 countries, six WHO regions).
-
•
The prevalence of occupational noise exposure in workers was 0.17.
Keywords: Global burden of disease, Systematic review, Prevalence, Occupational risk factor, Noise
Abstract
Background
The World Health Organization (WHO) and the International Labour Organization (ILO) are developing joint estimates of the work-related burden of disease and injury (WHO/ILO Joint Estimates), with contributions from a large network of individual experts. Evidence from mechanistic and human data suggests that occupational exposure to noise may cause cardiovascular disease. In this paper, we present a systematic review and meta-analysis of the prevalence of occupational exposure to noise for estimating (if feasible) the number of deaths and disability-adjusted life years from cardiovascular disease that are attributable to exposure to this risk factor, for the development of the WHO/ILO Joint Estimates.
Objectives
We aimed to systematically review and meta-analyse estimates of the prevalence of occupational exposure to noise.
Data sources
We searched electronic academic databases for potentially relevant records from published and unpublished studies, including Ovid Medline, PubMed, EMBASE, and CISDOC. We also searched electronic grey literature databases, Internet search engines, and organizational websites; hand-searched reference list of previous systematic reviews and included study records; and consulted additional experts.
Study eligibility and criteria
We included working-age (≥15 years) workers in the formal and informal economies in any WHO Member and/or ILO member State, but excluded children (<15 years) and unpaid domestic workers. We included all study types with an estimate of the prevalence of occupational exposure to noise, categorized into two levels: no (low) occupational exposure to noise (<85dBA) and any (high) occupational exposure to noise (≥85dBA).
Study appraisal and synthesis methods
At least two review authors independently screened titles and abstracts against the eligibility criteria at a first stage and full texts of potentially eligible records at a second stage, followed by extraction of data from qualifying studies. We combined prevalence estimates using random-effect meta-analysis. Two or more review authors assessed the risk of bias and the quality of evidence, using the RoB-SPEO tool and QoE-SPEO approach developed specifically for the WHO/ILO Joint Estimates.
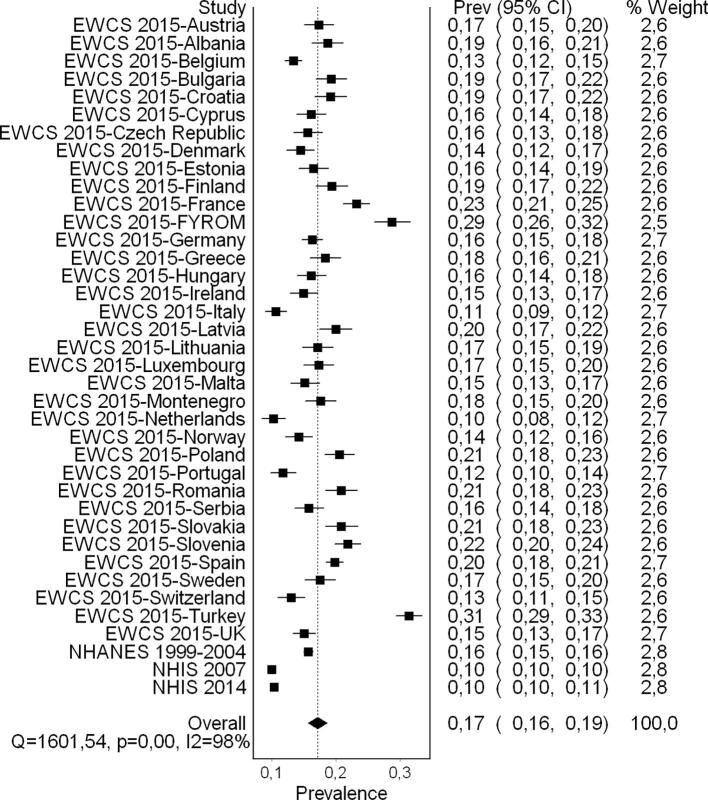
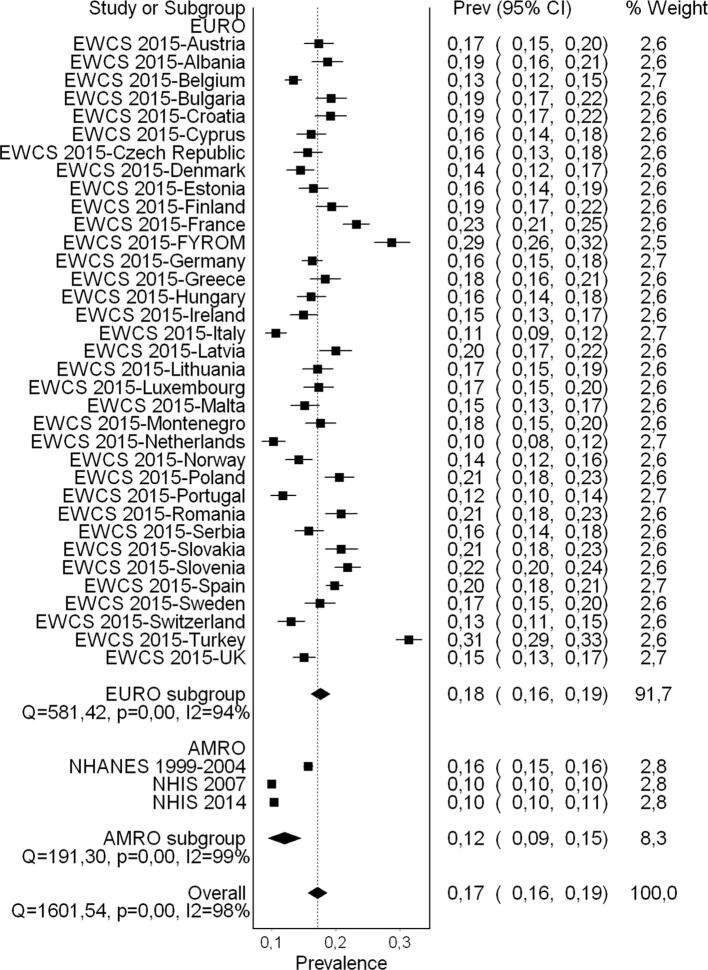
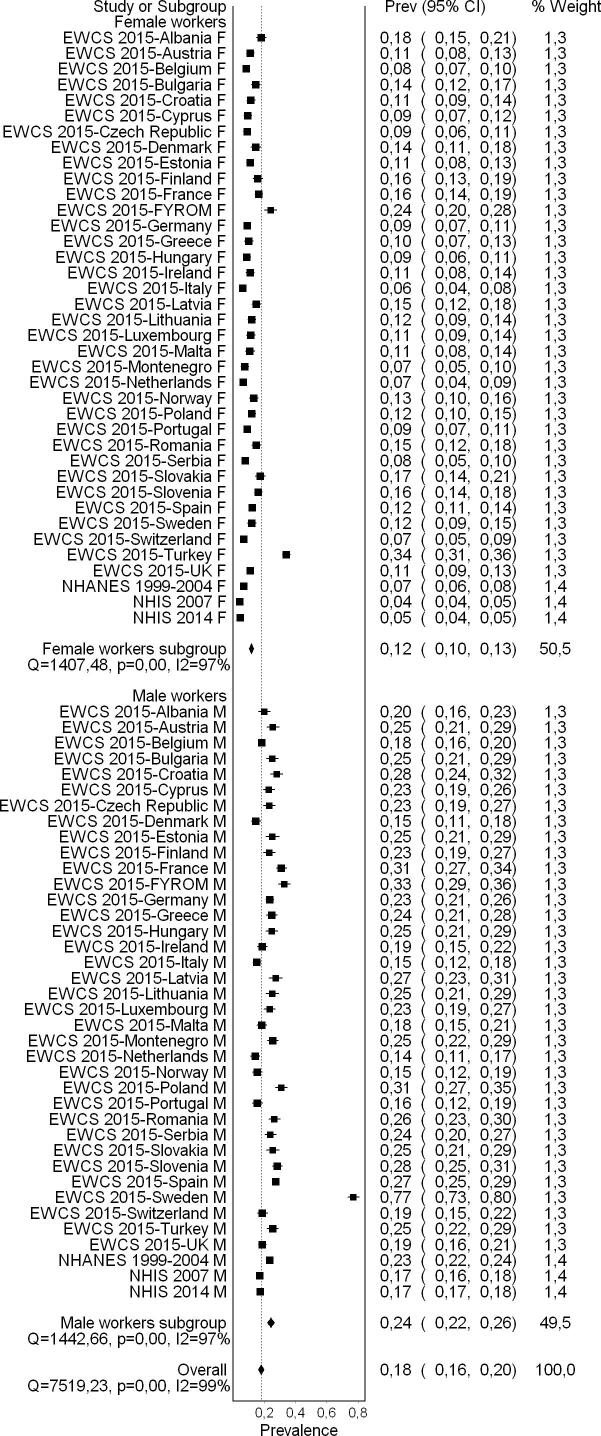
Results
Sixty-five studies (56 cross-sectional studies and nine cohort studies) met the inclusion criteria, comprising 157,370 participants (15,369 females) across 28 countries and all six WHO regions (Africa, Americas, Eastern Mediterranean, Europe, South-East Asia, and Western Pacific). For the main analyses, we prioritized the four included studies that surveyed national probability samples of general populations of workers over the 58 studies of workers in industrial sectors and/or occupations with relatively high occupational exposure to noise. The exposure was generally assessed with dosimetry, sound level meter, or official or company records; in the population-based studies, it was assessed with validated questions. Estimates of the prevalence of occupational exposure to noise are presented for all 65 included studies, by country, sex, 5-year age group, industrial sector, and occupation where feasible. The pooled prevalence of any (high) occupational exposure to noise (≥85dBA) among the general population of workers was 0.17 (95% confidence interval 0.16 to 0.19, 4 studies, 108,256 participants, 38 countries, two WHO regions, I2 98%, low quality of evidence). Subgroup analyses showed that pooled prevalence differed substantially by WHO region, sex, industrial sector, and occupation.
Conclusions
Our systematic review and meta-analysis found that occupational exposure to noise is prevalent among general populations of workers. The current body of evidence is, however, of low quality, due to serious concerns for risk of bias and indirectness. Producing estimates of occupational exposure to noise nevertheless appears evidence-based, and the pooled effect estimates presented in this systematic review are suitable as input data for the WHO/ILO Joint Estimates (if feasible).
Protocol identifier: 10.1016/j.envint.2018.09.040
PROSPERO registration number: CRD42018092272
1. Background
The World Health Organization (WHO) and the International Labour Organization (ILO) are finalizing joint estimates of the work-related burden of disease and injury (WHO/ILO Joint Estimates) (Ryder, 2017). The organizations are estimating the numbers of deaths and disability-adjusted life years (DALYs) that are attributable to exposure to selected occupational risk factors. The WHO/ILO Joint Estimates are based on existing WHO and ILO methodologies for estimating the burden of disease for selected occupational risk factors (Ezzati et al., 2004, International Labour Organization, 1999, International Labour Organization, 2014, Pruss-Ustun et al., 2017). They expand these existing methodologies with estimation of the burden of several prioritized additional pairs of occupational risk factors and health outcomes. For this purpose, population attributable fractions (Murray et al., 2004) are being calculated for each additional risk factor-outcome pair, and these fractions are being applied to the total disease burden envelopes for the health outcome from the WHO Global Health Estimates for the years 2000–2016 (World Health Organization, 2019). Population attributable fractions are the proportional reduction in burden from the health outcome achieved by a reduction of exposure to the risk factor to zero.
The WHO/ILO Joint Estimates may include estimates of the burden of cardiovascular disease attributable to occupational exposure to noise, if feasible, as additional risk factor-outcome pairs whose global burden of disease has not previously been estimated. To select parameters with the best and least biased evidence for our estimation models, we conducted a systematic review and meta-analysis of studies of the prevalence of occupational exposure to noise (Teixeira et al., 2019). In the current paper, we present this systematic review and meta-analysis. WHO and ILO, supported by a large network of individual experts, have in parallel also produced a systematic review of studies estimating the effect of occupational exposure to noise on cardiovascular disease, defined as ischemic heart disease, stroke, and hypertension (Teixeira et al., 2021). The organizations are also concurrently conducting or have completed several other systematic reviews and meta-analyses on other additional risk factor-outcome pairs (Descatha et al., 2018, Descatha et al., 2020, Godderis et al., 2018, Hulshof et al., 2019, Li et al., 2018, Li et al., 2020, Mandrioli et al., 2018, Pachito et al., 2020, Paulo et al., 2019, Pega et al., 2020a, Rugulies et al., 2019, Teixeira et al., 2019, Tenkate et al., 2019; Hulshof et al., 2021b, Hulshof et al., 2021a; Teixeira et al., 2021). To our knowledge, these are the first systematic reviews and meta-analyses (with pre-published protocols) conducted specifically for an occupational burden of disease study (Mandrioli et al., 2018). The WHO and ILO’s joint estimation methodology and the WHO/ILO Joint Estimates are separate from these systematic reviews and will be described in more detail and reported elsewhere.
1.1. Rationale
To consider the feasibility of estimating the burden of cardiovascular disease attributable to occupational exposure to noise, and to ensure that potential estimates of burden of disease are reported in adherence with the guidelines for accurate and transparent health estimates reporting (GATHER) (Stevens et al., 2016), WHO and ILO require a systematic review of studies on the prevalence of relevant levels of occupational exposure to noise. The theoretical minimum risk exposure level is the exposure level that would result in the lowest possible population risk, even if it were not feasible to attain this exposure level in practice (Murray et al., 2004). These prevalence and effect estimates should be tailored to serve as parameters for estimating the burden of cardiovascular disease from occupational exposure to noise. In 2002, WHO carried out an assessment of the global burden of selected diseases (not including cardiovascular disease) from occupational exposure to noise, as part of a larger initiative to assess the impact of 25 risk factors in a standardized manner, in which noise related to work appears as one of the major risk factors to human health (Concha-Barrientos et al., 2004).
In general, the health consequences of a given level of occupational exposure to noise are likely to be similar, regardless of the country or region in which the exposure occurs. A review has therefore been carried out of all well-designed epidemiological studies that link occupational noise exposure to health outcomes, regardless of where the study was conducted (Concha-Barrientos et al., 2004). High levels of occupational exposure to noise remain a problem in all regions of the world, being one of the most common occupational risk factors (Concha-Barrientos et al., 2004, United States Department of Labor, 2013). According to recent evidence (Kerns et al., 2018), 22 million (25%) workers in the general population of the United States of America have a history of occupational exposure to noise (14% exposed in the last year). According to the 6th European Working Conditions Survey (EWCS) in 36 countries in Europe, 28% of workers in 2015 were exposed to excessive noise for at least a quarter of their time at work (Parent-Thirion et al., 2019).
The most serious effect of occupational exposure to noise is irreversible hearing impairment (Concha-Barrientos et al., 2004, Tomprette et al., 2019). This is explained by noise causing mechanical damage to the hair cells and other structures in the cochlea, impaired microcirculation in the inner ear and generation of free radicals, which in turn promote DNA damage, and protein and lipid peroxidation in those structures (Themann and Masterson, 2019). Additionally, according to the World Health Organization (2018), environmental noise exposure can have non-auditory effects on health, such as cardiovascular disease (van Kempen et al., 2018), noise annoyance (Guski et al., 2017), sleep disturbance (Basner and McGuire, 2018), metabolic disorders (van Kempen et al., 2018), cognitive impairment (Clark and Paunovic, 2018a), poor quality of life and mental ill-health (Clark and Paunovic, 2018b), and adverse birth outcomes (Dzhambov and Lercher, 2019, Nieuwenhuijsen et al., 2017). Adverse health effects have also been observed in the occupational environment where noise levels tend to be considerably higher (Themann and Masterson, 2019). For example, a recent systematic review with meta-analysis supported higher risk of some adverse pregnancy outcomes in women exposed to high occupational exposure to noise (Dzhambov et al., 2014). In another meta-analysis (Dzhambov and Dimitrova, 2017), a dose-response relationship was found between occupational exposure to noise and work-related injury risk, based however on a body of evidence the study authors judged to be of “very low” quality. According to Concha-Barrientos et al. (2004), there is limited evidence that occupational exposure to noise impairs performance and entails biochemical, immune, and birth weight effects. In this context, our systematic review and meta-analysis is highly warranted; it contributes a synthesis and assessment of the latest body of evidence from studies estimating the prevalence occupational exposure to noise.
1.2. Description of occupational exposure to noise
Table 1.
Definitions of occupational exposure to noise, its levels, and the minimum risk exposure level.
| Concept | Definition |
|---|---|
| Risk factor | Exposure to occupational noise is the exposure at the workplace to an unpleasant or unwanted sound |
| Risk factor levels |
|
| Theoretical minimum risk exposure level | No occupational exposure to noise (<85dBA) |
Source: (Teixeira et al., 2019).
2. Objectives
To systematically review and meta-analyse evidence on the prevalence of any (high) occupational exposure to noise (≥85dBA) among working-age workers.
3. Methods
3.1. Developed protocol
We applied the Navigation Guide systematic review methodology for systematic reviews in environmental and occupational health as our guiding methodological framework (Woodruff and Sutton, 2014), wherever feasible. The Navigation Guide applies established systematic review methods from clinical medicine, including standard Cochrane Collaboration methods for systematic reviews of interventions, to the field of environmental and occupational health to ensure systematic and rigorous evidence synthesis on environmental and occupational risk factors that reduces bias and maximizes transparency (Woodruff and Sutton, 2014). The need for further methodological development and refinement of the relatively novel Navigation Guide has been acknowledged (Woodruff and Sutton, 2014). Our systematic review may not map well to the Navigation Guide framework (Fig. 1 on page 1009 in Lam et al. (2016)), which is tailored to hazard identification and risk assessment. Nevertheless, steps 1–6 for the stream on human data can be applied to systematically review evidence on the prevalence of exposure to occupational risk factors.
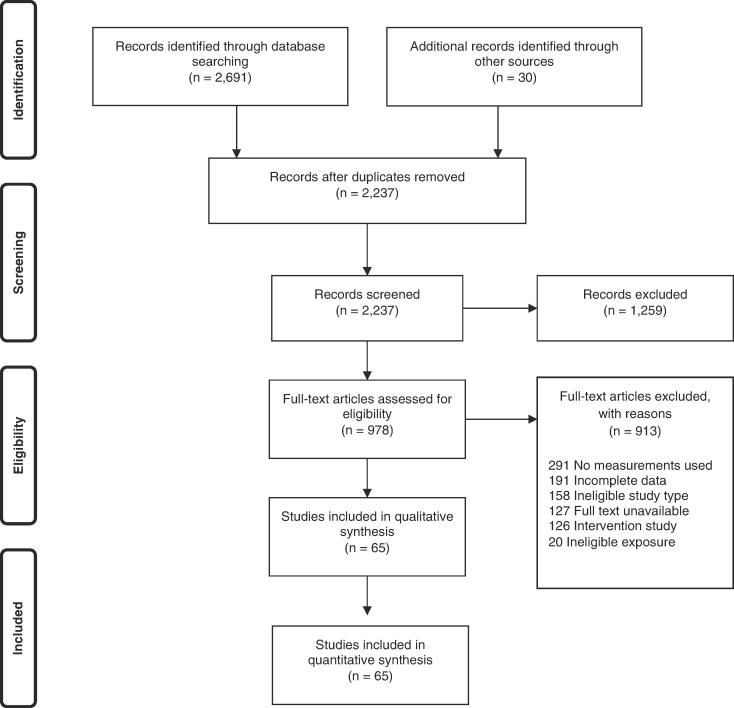
Fig. 1.
Flow diagram of study selection.
We have registered the protocol in PROSPERO under CRD42018092272. This protocol adheres with the preferred reporting items for systematic review and meta-analysis protocols statement (PRISMA-P) (Moher et al., 2015, Shamseer et al., 2015), with the abstract adhering with the reporting items for systematic reviews in journal and conference abstracts (PRISMA-A) (Beller et al., 2013). Any modification of the methods stated in the protocol was registered in PROSPERO and is reported in the systematic review itself (this article). The systematic review is reported to align with the GATHER guidelines (Stevens et al., 2016).
3.2. Searched literature
3.2.1. Information sources and search
3.2.1.1. Electronic bibliographic databases
We searched the following electronic bibliographic databases:
-
(1)
Ovid Medline (1 January 1946 to 21 March 2019 and updated on 25 May 2020)
-
(2)
PubMed (1 January 1946 to 21 March 2019 and updated on 25 May 2020)
-
(3)
Embase (1 January 1947 up to 29 March 2019 and updated on 25 May 2020)
-
(4)
Web of Science (1 January 1945 up to 29 March 2019 and updated on 25 May 2020)
-
(5)
Scopus (1 January 1966 up to 1 April 2019 and updated on 25 May 2020)
-
(6)
Lilacs (1 January 1985 up to 1 April 2019 and updated on 25 May 2020)
The Ovid MEDLINE search strategy was presented in the published protocol (Teixeira et al., 2019). The full search strategies for all databases were revised by an information scientist and are presented in Appendix 1 in the Supplementary data. Searches were performed in electronic databases operated in the English language for most databases, and in Portuguese and Spanish for Lilacs. When we neared completion of the review, we conducted a top-up search of the Ovid Medline and PubMed databases on 31 January 2020 to capture the most recent publications (e.g., publications ahead of print). Deviations from the proposed search strategy and the actual search strategy are documented in Section 8.
3.2.1.2. Electronic grey literature databases and complementary searches
We adapted the search syntax (Appendix 1 in the Supplementary data) to suit grey literature databases and searched the following electronic databases:
-
(1)
CISDOC (up to 3 May 2018)
-
(2)
OpenGrey (up to 3 May 2018)
-
(3)
GreyLit (up to 3 May 2018)
3.2.1.3. Internet search engines.
We also searched Google (www.google.com/) and Google Scholar (www.google.com/scholar/) on 3 May 2018 and screened the first 100 hits for potentially relevant records, as has previously been done in Cochrane Reviews (Pega et al., 2015, Pega et al., 2017).
3.2.1.4. Organizational websites
The websites of the following seven international organizations and national government departments were also searched:
-
(1)
International Labour Organization (www.ilo.org/)
-
(2)
World Health Organization (www.who.int)
-
(3)
European Agency for Safety and Health at Work (https://osha.europa.eu/en)
-
(4)
Eurostat (www.ec.europa.eu/eurostat/web/main/home).
-
(5)
China National Knowledge Infrastructure (http://www.cnki.net/)
-
(6)
Finnish Institute of Occupational Health (https://www.ttl.fi/en/)
-
(7)
National Institute of Occupational Safety and Health of the United States of America, using the institute’s data and statistics gateway (https://www.cdc.gov/niosh/data/)
3.2.1.5. Hand-searching and expert consultation
We hand-searched for potentially eligible studies in:
-
•
Reference lists of previous systematic reviews
-
•
Reference lists of all included study records
-
•
Study records published over the past 24 months in the three peer-reviewed academic journals from which we obtained the largest number of included studies
-
•
Study records that have cited an included study record (identified in the Web of Science citation database)
-
•
Collections of the review authors
Additional individual experts were contacted with a list of included studies, with the request to identify potentially eligible additional studies.
3.2.1.6. National information searches
The review authors from the National Institute for Occupational Health and Poison Control of the Chinese Center for Disease Control and Prevention conducted searches of national and local bibliographic and grey literature databases in Chinese language for the People’s Republic of China.
3.3. Selected studies
Study selection was carried out using Covidence (Covidence systematic review software). All study records identified in the search were downloaded, and duplicates were identified and deleted. Afterwards, two review authors independently and in duplicate screened titles and abstracts (step 1), and then full texts (step 2) of potentially relevant records. A third review author resolved any disagreements between the two review authors. If a study record identified in the literature search was authored by a review author assigned to study selection or if an assigned review author was involved in the study, it was re-assigned to another review author for study selection. The study selection is presented in a flow chart, as per PRISMA guidelines (Liberati et al., 2009).
3.4. Eligibility criteria
The population and exposure criteria are described below.
3.4.1. Types of populations
We included studies of working-age (≥15 years) workers in the formal and informal economies. Studies of children (aged < 15 years) and unpaid domestic workers were excluded. Participants residing in any WHO and/or ILO Member (or member) State and any industrial setting or occupation were included. We note that occupational exposure to noise may potentially have further population reach (e.g. through the release of noise from the workplace into the community) and acknowledge that the scope of our systematic reviews may not be able capture the environmental noise for nearby residents and its impacts on them.
3.4.2. Types of exposures
We included studies that defined occupational exposure to noise in accordance with our standard definition (Table 1). We included studies with measures from any data source, including registry data. All studies of current occupational exposure to noise were included, whether measured objectively (e.g. by means of technology, such as a sound level meter), semi-subjectively (e.g. by means of measurements by experts, such as scientists with subject matter expertise), or based on self-reports by a worker, workplace administrator or manager. If a study reported both objective and subjective measures, we prioritized the objective measure. If a study reported both prevalence of current occupational exposure to noise and history of occupational exposure to noise (i.e., having ever been exposed to high noise levels at work), we prioritized current prevalence. This rule was applied to systematically prioritize prevalence measurements in included studies that collected two or more alternative prevalence measures, such as the National Health Interview Survey (NHIS) (Center for Disease Control and Prevention, 2007, Center for Disease Control and Prevention, 2014) and National Health and Nutrition Examination Survey (NHANES) (Center for Disease Control and Prevention and National Center for Health Statistics, 2020), as described in Appendix 2 in the Supplementary data.
3.4.3. Types of studies
This systematic review included studies of any design reporting quantitative results, including cross-sectional studies. The studies had to be representative (within reason) of the relevant industrial sector(s), occupation(s) or the national population. We excluded qualitative, modelling, and case studies, as well as non-original studies without quantitative data (e.g. letters, commentaries, and perspectives).
Records published in any language were included. Most searches were conducted using English language terms, so that records published in any language that presented essential information (i.e. title and abstract) in English were included. If a record was written in a language other than those spoken by the authors of this review or those of other reviews (Descatha et al., 2018, Descatha et al., 2020, Godderis et al., 2018, Hulshof et al., 2019, Li et al., 2018, Li et al., 2020, Mandrioli et al., 2018, Pachito et al., 2020, Paulo et al., 2019, Pega et al., 2020a, Rugulies et al., 2019, Teixeira et al., 2019, Tenkate et al., 2019; Hulshof et al., 2021b, Hulshof et al., 2021a; Teixeira et al., 2021) in the series (i.e. Arabic, Bulgarian, Chinese, Danish, Dutch, English, French, Finnish, German, Hungarian, Italian, Japanese, Norwegian, Portuguese, Russian, Spanish, Swedish and Thai), then the record was translated into English. Published and unpublished studies were included. Studies conducted using unethical practices were excluded from the review.
3.4.4. Types of prevalence measures
We included studies that reported a prevalence measure. Prevalence is the presence (and often the level) of an exposure to an occupational risk factor in each individual of the study population or in a representative sample at one particular time point (Porta, 2014). The prevalence (as here defined) is usually measured as the number of exposed persons (numerator) divided by the total number of persons (i.e., unexposed persons plus exposed persons) (denominator). It is usually reported as a fraction, in percentage points.
3.5. Extracted data
WHO and ILO developed a standard data extraction sheet. All data extractors piloted this sheet until there was convergence and agreement among them. Most data extractors participated in WHO’s online training for the use of the data extraction sheet. At a minimum, two review authors independently extracted the data on occupational exposure to noise, disaggregated by country, sex, age, and industrial sector and/or occupation. A third review author resolved conflicting extractions. Data were extracted on study characteristics (including study authors, study year, study country, participants, and exposure), study design (including study type, exposure measurement, and type of prevalence estimate), risk of bias (including missing data, as indicated by response rate and other measures), and study context. The prevalence estimates from included studies were entered and managed with the Stata computer software.
Data on potential conflict of interest were also extracted from the included studies, such as financial disclosures, funding sources, and authors’ affiliated organizations. A modification of a previous method was used to identify and assess undisclosed financial interests (Forsyth et al., 2014). If no financial disclosure and conflict of interest statements were provided, other records were searched from this study published in the 36 months prior to the included study record and in other publicly available repositories (Drazen et al., 2010a, Drazen et al., 2010b).
3.6. Requested missing data
We requested the missing data presented in Table 2.
Table 2.
Description of missing data requested and received.
| Study ID | Description of missing data | Person(s) from whom missing data were requested | Date of request(s) | Data received |
|---|---|---|---|---|
| Parent-Thirion 2015 | Data disaggregated by sex, age, and occupation | Open-access database (https://www.eurofound.europa.eu/surveys/european-working-conditions-surveys-ewcs) | Downloaded on 30 January 2020 | Downloaded on 30 January 2020 |
| NHIS 2007 and NHIS 2014 | Data disaggregated by sex, age, occupation, and industrial sector | Open-access database (www.cdc.gov/nchs/nhis/index.htm); Elizabeth Masterson, National Institute for Occupational Safety and Health of the United States of America, advised on the interpretation of measures of self-reported occupational exposure to noise | 30 Jan 2020 | 31 Jan 2020 |
| NHANES 1999–2004 | Data disaggregated by sex, age, occupation, and industrial sector | Open-access database (www.cdc.gov/nchs/nhanes/index.htm); Elizabeth Masterson, National Institute for Occupational Safety and Health of the United States of America, advised on the interpretation of measures of self-reported occupational exposure to noise | 30 Jan 2020 | 31 Jan 2020 |
3.7. Assessed risk of bias
We used the RoB-SPEO tool for assessing risk of bias in studies estimating the prevalence of exposure to occupational risk factors (Pega et al., 2020b). WHO and ILO, in collaboration with a Working Group of individual experts, developed this tool specifically for the systematic reviews conducted for the development of the WHO/ILO Joint Estimates. For each included study, two or more review authors independently assessed risk of bias with RoB-SPEO, and another review author resolved any conflicts between the individual assessments.
3.8. Conducted evidence synthesis (including meta-analysis)
If we found two or more studies with an eligible prevalence estimate, two or more review authors independently assessed the clinical heterogeneity (Deeks et al., 2011) of the studies in terms of population (WHO region and/or distribution by sex, age, industrial sector, and/or occupation) and exposure (definition, measurement methods, and level of exposure), following our protocol (Teixeira et al., 2019). If we judged two or more prevalence estimates to be sufficiently clinically homogenous, we pooled the prevalence estimates of these studies in a quantitative meta-analysis, using the inverse variance method with a random effects model. The output from these meta-analyses is a variance-weighted mean prevalence estimate, which is reported as a fraction. We assessed statistical heterogeneity using the I2 statistic. As recommended elsewhere (Higgins et al., 2019), we did not set specific ranges of I2 to indicate certain levels of statistical heterogeneity, and as described in Section 4.8.1 we expected statistical (and clinical) heterogeneity to be high. The meta-analysis was conducted in Stata 5.0. For our main meta-analysis, we prioritized the included studies that surveyed national probability samples of general populations of workers. We considered the studies of workers in industrial sectors and/or occupations with relatively high occupational exposure to noise as supporting evidence only, but made full use of these for additional analyses (see Section 3.9).
3.9. Conducted additional analyses
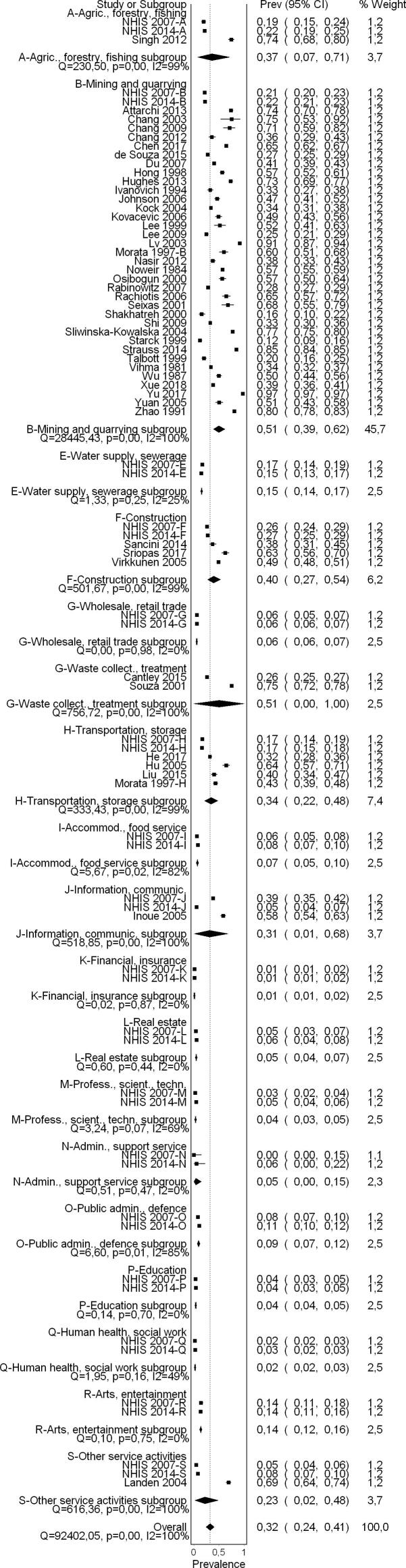
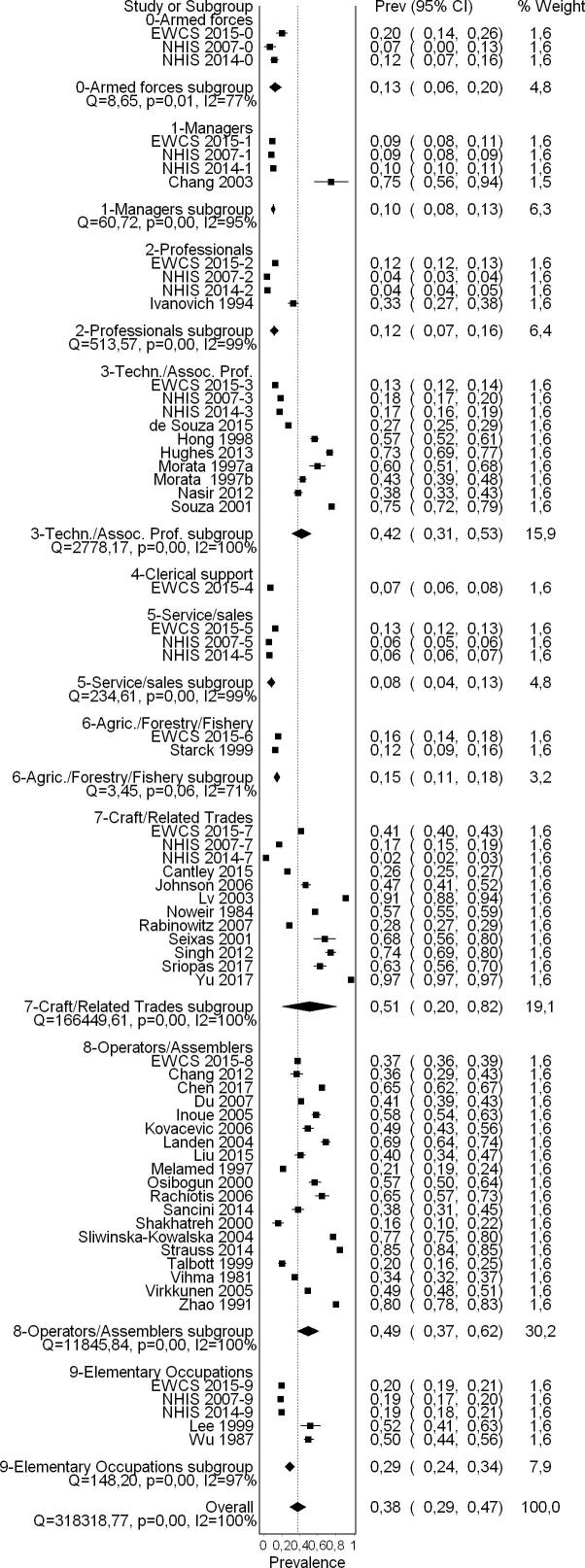
We conducted subgroup analyses by:
-
•
WHO region (and/or country)
-
•
Sex
-
•
Industrial sector
-
•
Occupation
We also planned to conduct subgroup analyses by age group, but did not do so because we did not access the data disaggregated by age.
For the subgroup analyses by sex, we prioritized the included studies that surveyed national probability samples of general populations of workers because these provided the prevalence that we were interested in. However, for the other subgroup analyses, we used all included studies (including those of workers in industrial sectors and/or occupations with relatively high occupational exposure to noise) to estimate prevalence in subgroups, such as defined industrial sectors and occupations, respectively, or if a subgroup had no data available from the prioritized evidence (i.e. general worker population studies). This may have introduced some between-subgroup heterogeneity in our subgroup analyses. Differences between subgroups were assessed with Chi2 tests; for each subgroup analysis, we report the p-value from the test and assume a p-value lower than 0.05 to indicate a significant subgroup difference.
No sensitivity or other analyses were conducted.
3.10. Assessed quality of evidence
We used the QoE-SPEO approach for assessing the quality of evidence in studies estimating the prevalence of exposure to occupational risk factors (Pega et al., submitted for publication). At least two review authors assessed quality of evidence. A third review author resolved conflicting ratings. WHO, supported by a Working Group of individual experts, developed the QoE-SPEO approach specifically for systematic reviews for the WHO/ILO Joint Estimates.
4. Results
4.1. Study selection
A flow diagram of the study selection is presented in Fig. 1. Sixty-five studies (56 cross-sectional studies and nine cohort studies) met the inclusion criteria, comprising 157,370 participants (15,369 females) across 28 countries and all six WHO regions (Africa, Americas, Eastern Mediterranean, Europe, South-East Asia, and Western Pacific). For 30 excluded studies that most closely resembled inclusion criteria, the reasons for exclusion are listed in Appendix 3 in the Supplementary data. All 65 included studies were included in the quantitative meta-analyses, with only four however included in the main meta-analysis.
4.2. Characteristics of included studies
The characteristics of the included studies are summarized in Table 3.
Table 3.
Characteristics of included studies.
| Study | Study population |
Study type |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study ID | Total number of study participants | Number of female study participants | Country of study population | Geographic location | Industrial sector (ISIC-4 code) | Occupation (ISCO-08 code) | Age (in years) | Study design | Study period | Follow-up period |
| Ahmed 2001 | 368 | 0 | Kingdom of Saudi Arabia | Region | 24, 35 | 8121, 7127 | Mean = 32.09; s.d. = 7.70 | Cross-sectional | 1996–1999 | Unclear |
| Attarchi 2012 | 331 | 0 | Islamic Republic of Iran | Local | Unclear | Unclear | Range = 19–55; mean = 38.95 | Cross-sectional | 2010 | Unclear |
| Attarchi 2013 | 471 | 0 | Islamic Republic of Iran | Local | 29 | 3341, 7131, 8211 | Range = 20–58; mean = 32.91 | Cross-sectional | 2010–2011 | Unclear |
| Bauer 1991 | 47,388 | 7,156 | Austria | Local | Unclear | Unclear | Range = 25–55 | Cross-sectional | 1984–1986 | 36 months |
| Cantley 2015 | 9,220 | 989 | United States of America | National | 32 | 7223 | Mean = 44.2; s.d. = 10.5 | Cohort | 1 Jan 2003–31 Dec 2008 | 72 months |
| Chang 2003 | 20 | 0 | People's Republic of China | Local | 45 | 1290 | Mean = 39; s.d. = 7; mean = 45; s.d. = 8 | Panel/Longitudinal | 2000–2001 | Unclear |
| Chang 2009 | 59 | 12 | People's Republic of China | Local | 15 | 7543, 8159, 7322, 9611, 4110, 9329 | Mean = 34.6; s.d. = 7.7; mean = 40.3; s.d. = 5.8 | Cross-sectional | 2005–2006 | Unclear |
| Chang 2012 | 281 | 33 | People's Republic of China | Region | 32 | 8121 | Mean = 32.4; s.d. = 6.4 | Cross-sectional | At the end of 2009 | Unclear |
| Chen 2017 | 1,390 | 0 | People's Republic of China | National | 32 | 8189 | Mean = 33.1; s.d. = 8.7 | Cross-sectional | Unclear | Unclear |
| de Souza 2015 | 1,729 | 144 | Brazil | Local | 6 | 3134 | <30; 30–34; 35–39; 40–44; 45–49; ≥50 | Cross-sectional | 6 months | 6 months |
| Du 2007 | 3,279 | Unclear | People's Republic of China | Region | 13 | 8152 | Range = 21–45; mean = 33.5 | Cross-sectional | Unclear | Unclear |
| Guo 2012 | 60 | 50 | People's Republic of China | Region | 13 | 8159 | Mean = 25.8; s.d. = 8.4 | Cross-sectional | Feb 2010-Jan 2011 | Unclear |
| He 2017 | 531 | 23 | People's Republic of China | Region | 20 | Unclear | Unclear | Cross-sectional | 2016 | Unclear |
| Hong 1998 | 450 | 0 | Republic of Korea | Region | 51 | 3153 | Unclear | Cross-sectional | 1995 | Unclear |
| Hu 2005 | 191 | Unclear | People's Republic of China | Region | 24 | 8121, 3343 | Range = 20–53 | Cross-sectional | Unclear | Unclear |
| Hughes 2013 | 503 | 27 | United States of America | Local | 51 | 3153 | <25; 25–34; 35–44; 45–54; >55 | Cohort | 1 Jan 2001–31 Dec 2007 | 1 Jan 2001–31 Dec 2007 |
| Inoue 2005 | 415 | 0 | Japan | Region | 17 | 8171 | Unclear | Cross-sectional | Unclear | Unclear |
| Ivanovich 1994 | 249 | 249 | Bulgaria | Local | 61 | 2656 | Mean = 34; s.d. = 9.0, Mean = 35.6; s.d. = 9.2, Mean = 40.4; s.d. = 6.5 | Cross-sectional | Unclear | Unclear |
| Johnson 2006 | 313 | 35 | Sweden | Local | 96 | 7315 | Unclear | Cross-sectional | 2002–2006 | 2002–2006 |
| Kock 2004 | 741 | 207 | Denmark | Local | 32 | Unclear | Unclear | Cross-sectional | Unclear | Unclear |
| Kovacevic 2006 | 225 | 111 | Montenegro | Local | 13 | 8152 | Mean = 42.5; s.d. = 8.5; mean = 39.2; s.d. = 8.5; mean = 33.1; s.d. = 9.0; mean = 32.9; s.d. = 7.2 | Cross-sectional | Unclear | Unclear |
| Landen 2004 | 309 | 19 | United States of America | Region | 8 | 8111 | 18–29; 30–39; 40–49; 50–59 ; >60 | Cross-sectional | Unclear | Unclear |
| Lee 1999 | 80 | 16 | Singapore | Local | 96 | 9626 | Range = 17–44; mean = 24.6; s.d. = 6.8; range = 17–45; mean = 23.; s.d. = 5.9 | Cross-sectional | Unclear | Unclear |
| Lee 2009 | 530 | 0 | Republic of Korea | Local | 24 | Unclear | Range = 16–45; mean = 25.6 | Cohort (retrospective) | 1991–1999 | 9 years |
| Liu 2015 | 247 | 48 | People's Republic of China | Region | 32 | 8121 | Mean = 38.0; s.d. = 11.0 | Cross-sectional | Unclear | Unclear |
| Lv 2003 | 319 | 0 | People's Republic of China | Region | Unclear | 7232 | Mean = 33.4; s.d. = 10.3 | Cross-sectional | Unclear | Unclear |
| Maccà 2014 | 285 | 128 | Italy | Local | 13, 25, 32, 41 | 8159, 7211, 9313, 8114 | Mean = 39.9; s.d. = 10 | Cross-sectional | Unclear | Unclear |
| Melamed 1997 | 970 | 624 | Israel | National | 10, 13, 24, 26 | 8121, 8159, 8189, 8212, 8160 | Women = 20–60; men 20–44, ≥45 | Cross-sectional | Unclear | Unclear |
| Morata 1997 | 124 | 0 | Brazil | Local | 32 | 3139 | Range = 21–58; mean = 33.8; s.d. = 8.5 | Cross-sectional | Unclear | Unclear |
| Morata 1997 | 438 | 0 | United States of America | Local | 6 | 3134 | Mean = 44.0; s.d. = 0.9; mean = 40.4; s.d. = 0.6; mean = 41.5; s.d. = 0.9; mean = 43.9; s.d. = 0.4; mean = 42.8; s.d. = 1.4; mean = 40.7; s.d. = 0.7 | Cross-sectional | Jun 1989–1994 | 60 months |
| Nasir 2012 | 358 | 111 | Malaysia | Local | 51 | 3153 | Range = 21–54; mean = 31.9; s.d. = 9.9 | Cross-sectional | Nov 2008-March 2009 | Unclear |
| NHIS 2014 | 34,059 | 18,494 | United States of America | National | General working population | General working population | Range = 18–85+; mean = 49.37; s.d. = 17.99 | Cross-sectional | 2014 | Unclear |
| NHIS 2007 | 20,800 | 11,221 | United States of America | National | General working population | General working population | Range = 18-≥85; mean = 47.15; s.d. = 17.55 | Cross-sectional | 2007 | Unclear |
| NHANES 1999–2004 | 9,721 | 509 | United States of America | National | General working population | General working population | Range = 16-≥85; mean = 37.73; s.d. = 15.57 | Cross-sectional | 1999–2004 | Unclear |
| Noweir 1984 | 2,458 | 0 | Egypt | Other | 13 | 7318 | <25; 25–34; 35–44; 45–54; >55 | Cross-sectional | 1974 (data collected 1975–1976) | 24 months |
| Nyarubeli 2018 | 326 | Unclear | Tanzania | Local | 25 | 7211, 7223 | Unclear | Cohort (prospective) | Unclear | Unclear |
| Osibogun 2000 | 204 | 7 | Nigeria | Local | 13 | 8159 | 16–25; 26–35; 36–45; 46–55 | Cross-sectional | Unclear | Unclear |
| Parent-Thirion 2015 (EWCS) | 43,684 | 26,424 | 35 European countries: Albania, Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Republic of North Macedonia, Germany, Greece, Hungary, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Montenegro, Netherlands, Norway, Poland, Portugal, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey, United Kingdom of Great Britain and Northern Ireland | National | General working population | General working population | 15–65 | Cross-sectional. This is not one cross sectional study across all of Europe-but 35 separate cross-sectional studies with 35 separate data points. | Feb-Dec 2015 | Not applicable |
| Pawlaczy-Luszczynska 2016 | 50 | 0 | Poland | Region | 31 | 8189 | Range = 20–57; mean = 35; s.d. = 8.1 | Cross-sectional | Unclear | Not applicable |
| Rabinowitz 2007 | 6,217 | 397 | United States of America | Local | 32 | 7223 | Mean = 40.8; s.d. = 7.2 | Cohort | 1990–2004 | 7 years |
| Rachiotis 2006 | 145 | 16 | Greece | Local | 26 | 8212 | ≤ 40; > 40 | Cross-sectional | Unclear | Unclear |
| Sancini 2014 | 191 | 0 | Italy | Other | 17 | 8171 | Group A - mean = 38.1; s.d. = 7.7; group B - mean = 38.8; s.d. = 4; group C - mean = 38.8; s.d. = 3.6 | Cross-sectional | Unclear | Unclear |
| Seixas 2001 | 59 | 0 | United States of America | Local | 43 | 7411 | Mean = 34; s.d. = 9 | Cross-sectional | 4 months | 4 months |
| Shakhatreh 2000 | 140 | 26 | Jordan | Local | 32 | 8159 | Exposed group - mean = 38 male and 31.5 female; non-exposed group - mean = 39.7 male and 30.7 female | Cross-sectional | Unclear | Unclear |
| Shi 2009 | 1,170 | 0 | People's Republic of China | Region | 6 | Not applicable | Unclear | Cross-sectional | March-May 2008 | Unclear |
| Singh 2012 | 222 | 222 | India | Region | 24 | 7221 | Exposed group - mean = 30.1; s.d. = 7.8; control group - mean = 32; s.d. = 8.9 | Cross-sectional | Unclear | Unclear |
| Sliwinska-Kowalska 2004 | 906 | 124 | Poland | Local | 3 | 8350 | Range = 20–66 | Cross-sectional | Unclear | Unclear |
| Solecki 2008 | 44 | Unclear | Unclear | Unclear | 1 | 6111 | Range = 33–65; mean = 48.6 | Cross-sectional | 1 year | Not applicable |
| Souza 2001 | 775 | 0 | Brazil | Local | 6 | 3134 | ≤ 38; > 38 | Cross-sectional | 1994 | Unclear |
| Sriopas 2017 | 180 | 0 | Thailand | Local | 45 | 7212 | 20–30; >30–50 | Cross-sectional | Unclear | 1 year |
| Starck 1999 | 370 | 0 | Unclear | Unclear | 43 | 6210 | Range 23–59; mean = 42.7; range 21–60; mean = 38.3 | Cross-sectional | Unclear | Unclear |
| Stokholm 2013 | 11,395 | 2,887 | Denmark | Local | Unclear | Unclear | <25; 25–34; 35–44; 45–54; 55–64; ≥65 | Cohort (prospective) | 1 Jan 2001–31 Dec 2007 | 2001–2007 |
| Strauss 2014 | 40,123 | 0 | South Africa | Local | 7 | 8111 | 16–30; 31–40; 41–50; 51–60; 61–65 | Cohort | 2001–2008 | 8 years |
| Talbott 1999 | 308 | 0 | United States of America | Local | 29 | 8211 | Range = 40–63; mean = 49.6; s.d. = 5.7; mean = 48.7; s.d. = 5.3 | Cross-sectional | Since 1975 | 15 or more years of work |
| Toppila 2001 | 706 | 0 | Finland | Region | Unclear | Unclear | Mean = 40; s.d. = 9 | Cross-sectional | 1995 | Unclear |
| Vihma 1981 | 1,181 | 10 | Finland | Local | 16, 22, 24, 27 | 8121 | Offset printers - mean = 30; relief printers - mean = 41 | Cross-sectional | 1976 | 1977–1980 |
| Virkkunen 2005 | 6,005 | 0 | Finland | National | 96 | 8121 | Beginning of the stud 40–56 ; end of the study 57–63 | Cohort (prospective) | 18 years | 96 months-1985–1994 |
| Whittaker 2014 | 238 | Study group 5.22%; control group 25.2% | Nepal | Local | 7, 55 | 3117, 9112 | Median = 24.0; IQR = 16 | Cross-sectional | Unclear | Unclear |
| Wu 1987 | 316 | 0 | People's Republic of China | Local | 43 | 9329 | Unclear | Cross-sectional | Jun-Aug 1983 | Jun-Aug 1983 |
| Xiao 2008 | 1,906 | 458 | People's Republic of China | Region | Unclear | Unclear | Range = 22–50 | Cross-sectional | Unclear | Unclear |
| Xie 2015 | 98 | 15 | People's Republic of China | Region | 24 | 7223 | Mean = 38.6; s.d. = 5.6 | Cross-sectional | Unclear | Unclear |
| Xue 2018 | 1,813 | 0 | People's Republic of China | Region | 29 | Not applicable | Range = 18–55 | Cross-sectional | Unclear | Unclear |
| Yu 2017 | 6,297 | Unclear | People's Republic of China | Region | 24 | 7213 | Unclear | Cohort (retrospective) | Unclear | Unclear |
| Yuan 2005 | 174 | 0 | People's Republic of China | Region | 32 | 7221, 4110 | Mean = 36.5; s.d. = 9.4, Mean = 37.2; s.d. = 8.6 | Cross-sectional | Unclear | Unclear |
| Zhao 1991 | 1,101 | 1,101 | People's Republic of China | Local | 13 | 8159 | Mean = 38.5; s.d. = 8.1; mean = 37.2; s.d. = 8.6; mean = 33.9; s.d. = 8; mean = 33.9; s.d. = 8.2; mean = 35.5; s.d. = 8.4 | Cross-sectional | 8 Jul-10 Aug 1985 | Unclear |
| Study | Exposure assessment |
|||||||
| Study ID | Exposure definition | Unit for which exposure was assessed | Mode of exposure data collection | Exposure assessment methods | Type of exposure measurement or estimate | Dates covered by exposure assessment (years) | Shortest and longest exposure period | Levels/intensity of exposure (specify unit) |
| Ahmed 2001 | Equivalent continuous noise level (Leq/shift; mean Leq/shift and mean of the total noise immission level (TNIL) | Individual level | Technical device | Dosimeter | Prevalence | 1996–1999 | 12h/day | >85dBA |
| Attarchi 2012 | Leq (equivalent continuous noise level) | Individual level | Technical device | Sound level meter | Prevalence | 2010 | Unclear | Relevant category: >85dBA |
| Attarchi 2013 | Leq (equivalent continuous noise level) | Individual level | Technical device | Sound level meter | Prevalence | 2010–2011 | 8 working hours; repeated through 1 week | Relevant category: >85dBA |
| Bauer 1991 | A-weighted sound-pressure | Individual level | Technical device | Sound level meter | Prevalence | 1984–1986 | Unclear | Relevant category: >85dBA |
| Cantley 2015 | 8h time weighted mean | Individual level | Administrative records | Dosimeter | Prevalence | 2003–2008 | Unclear | <82; 82–84.99; 85–87.99; ≥88dBA |
| Chang 2003 | TWA (Leq) | Individual level | Technical device | Dosimeter | Prevalence | 2000–2001 | 24h monitoring periods | Relevant category: >85dBA |
| Chang 2009 | A-weighted (dBA) and time-weighted average | Individual level | Technical device | Dosimeter | Prevalence | Unclear | 5 min/shift (8am-6pm) | ≥80dBA |
| Chang 2012 | A-weighted decibels (dBA) | Individual level | Technical device | Sound level meter, dosimeter | Prevalence | Dec 2009 | 50–120dBA to all subjects’ noise exposure with 5-min analyse over 8h | Relevant category ≥80dBA |
| Chen 2017 | Equivalent continuous dBA weighted sound pressure levels (LEX,8h) | Group level | Technical device | Sound level meter | Prevalence | Unclear | Unclear | >80dBA |
| de Souza 2015 | A-weighted sound level | Individual level | Technical device | Dosimeter | Prevalence | 2007 | Unclear | Relevant category: >85dBA |
| Du 2007 | A-weighted equivalent sound level (LAeq), peak sound level | Group level | Technical device | Dosimeter | Prevalence | Unclear | Unclear | Relevant category: >85dBA |
| Guo 2012 | A sound level and sound pressure level (SPL), cumulative noise exposure (CNE) | Group level | Technical device | Dosimeter | Prevalence | Unclear (covered 24h on a day after Feb 2010) | Unclear | Relevant category: >85dBA |
| He 2017 | A-weighted equivalent sound level (LAeq) | Group level | Technical device | Dosimeter | Prevalence | Unclear | Unclear | Relevant category: >85dBA |
| Hong 1998 | Time-weighted average | Individual level | Technical device | Dosimeter | Prevalence | Unclear | Daily 8h TWA | Relevant category: >85dBA |
| Hu 2005 | A-weighted equivalent sound level (LAeq) | Group level | Technical device | Dosimeter | Prevalence | Unclear | Unclear | Relevant category: >85dBA |
| Hughes 2013 | Equivalent Cumulative Level (ECL) | Group level | Administrative records | Registry data (industrial hygiene noise exposure monitoring data) | Prevalence | Jan 1, 2001 to Dec 31, 2007 | Unclear | > 85dBA |
| Inoue 2005 | A-weighted sound level | Group level | Administrative records | Sound level meter | Sound level measurement | Twice per year | Unclear | > 92dBA on average |
| Ivanovich 1994 | Equivalent noise level (Leq) | Individual level | Technical device | Sound level meter | Prevalence | Unclear | 15 min intervals during normal working activities | >85dBA |
| Johnson 2006 | 8h Level Equivalent Dosimeter Measurements | Individual level | Technical device | Dosimeter | Prevalence | 4 years | One full shift (at least) | >85dBA |
| Kock 2004 | A-weighted equivalent sound level (LAeq) | Individual level | Technical device | Dosimeter | Prevalence | Unclear (covered 24h on a day after 1 Aug 2001) | Always 24 h | >85dBA |
| Kovacevic 2006 | Equivalent noise levels (Leq) | Group level | Technical device | Noise level analyzer | Prevalence | Unclear | One shift (8h) | Unclear |
| Landen 2004 | Full shift, TWA (dBA) | Individual level | Technical device | Dosimeter | Prevalence | Unclear | Mean = 9h43min; s.d. = 1h11min | > 80dBA |
| Lee 1999 | Time Weighted Average (TWA) level (dBA) | Individual level | Technical device | Dosimeter | Prevalence | Unclear | Whole work shift (7/8pm to 3am) | Relevant category: >85dBA |
| Lee 2009 | TWA (dBA) | Individual level | Technical device | Dosimeter | Incidence | 9 years | 6h/day on demand | Relevant category: >85dBA |
| Liu 2015 | Environmental noise levels and time-weighted noise level | Individual level | Technical device | Sound level meter, dosimeter | Prevalence | Unclear | Unclear | Relevant category: >85dBA |
| Lv 2003 | The 8h equivalent continuous A sound level of each subject (LAeq.8h) | Individual level | Technical device | Unclear | Prevalence | Unclear (covered 24h on a day) | 10h | Relevant category: >85dBA |
| Maccà 2014 | dBA Lep,d | Individual level | Administrative records (supplied by the management of factories) | Sound level meter | Prevalence | Unclear | Unclear | 80–100.7dBA |
| Melamed 1997 | Time-weighted equivalent noise level | Group level | Technical device | Ambient noise levels | Prevalence | Twice each day | 1/2h | Relevant category: >85dBA |
| Morata 1997 | LAEq values in dBA | Individual level | Technical device | Dosimeter | Prevalence | Jun 1989 | Full shift − 8h shifts | ≤80dBA; 81-85dBA; 86-90dBA; ≥91dBA |
| Morata 1997 | Time weighted average | Group level | Technical device | Unclear | Prevalence | Unclear | 2-3h/day in some departments and 8h/shift at others | 78-101dBA, mean = 87dBA; 71-98dBA, mean = 88dBA |
| Nasir 2012 | Time-weighted average | Individual level | Technical device | Dosimeter | Prevalence | >5 years | Occupational exposure to noise >5years, 8h time-weighted average | <85 dBA; 85-89dBA; ≥ 90dBA |
| NHIS 2014 | Exposure to “loud” or “very loud” sounds/ noise | Individual level | Self-reported | Questionnaire | Prevalence | Last 12 months | ≥ 4 h/day, several days/week | “Loud” or “very loud” noise (approx. >85/90dBA) |
| NHIS 2007 | Exposure to “loud” sounds/ noise | Individual level | Self-reported | Questionnaire | Prevalence | Last 12 months | ≥ 4 h/day, several days/week | “Loud” noise (approx. >85dBA) |
| NHANES 1999–2004 | Exposure to “loud” noise | Individual level | Self-reported | Questionnaire | Prevalence | “Currently“ | ≥ 3 months | “Loud” noise (approx. >85dBA) |
| Noweir 1984 | Average value of the A-weighted sound pressure level and sound pressure levels | Group level | Technical device | Sound level meter | Prevalence | Unclear | Unclear | ≥90dBA |
| Nyarubeli 2018 | A-weighted equivalent noise level and the C-weighted peak noise level | Individual level | Technical device | Dosimeter | Incidence | Jun 2016-Jun 2017 | Unclear | “Loud” noise (approx. >85dBA) |
| Osibogun 2000 | Leq 60sec noise (for rapidly fluctuating noise) in the A-Weighted network and slow meter response | Group level | Technical device | Sound level meter | Prevalence | Unclear | Unclear | <85dBA; 85-90dBA; >90dBA |
| Parent-Thirion 2017 (EWCS) | Exposure to “Noise so loud that you would have to raise your voice to talk to people”. Responses ‘never or almost never’ were classified as ‘not occupationally exposed to noise’ and ‘Around 1/4 of the daytime’ or more as “occupationally exposed’ | Individual level | Face-to-face computer-assisted personal interview | Self-reports | Prevalence | Feb-Dec 2015 | At least half of the time at work | “Loud” noise (approx. > 85dBA) |
| Pawlaczy-Luszczunska 2016 | Daily noise exposure level (LEX,8h), maximum A-weighted sound pressure level (with time constant Slow) (LAmax) and peak C-weighted sound pressure level (LCpeak) | Group level | Technical device | Sound level meter | Prevalence | Unclear | 3–14 years | LEX,8h: 82.7–94.8dBA, LAmax; 91.9–108.6dBA; LCpeak: 111.5–139.3dBA |
| Rabinowitz 2007 | Time Averaged Equivalent (Leq) | Individual level | Administrative records | Dosimeter | Incidence | 14 years | Unclear | Unclear |
| Rachiotis 2006 | Equivalent continuous Sound Level (Leq dB (A)) | Group level | Technical device | Sound level meter | Prevalence | Uncl | Unclear | 91 (dBA, Leq) |
| Sancini 2014 | Equivalent continuous level noise (LAeq) | Individual level | Technical device | Sound level meter | Prevalence | Unclear | 8h shift | Relevant category: >85dBA |
| Seixas 2001 | Losha (TWA), Leq and Lpeak | Individual level | Technical device | Dosimeter | Prevalence | 4 months | Workday | > 85dBA |
| Shakhatreh 2000 | dB (A) | Group level | Technical device | Sound level meter | Prevalence | Unclear | Unclear | Unclear |
| Shi 2009 | Sound pressure level (SPL);A-weighted equivalent sound level (LAeq) | Group level | Technical device | Dosimeter | Prevalence | Unclear | 8h | >85dBA |
| Singh 2012 | A weighted (Leq) ambient noise and time-weighted average dose | Individual level | Technical device | Dosimeter | Prevalence | Unclear | 8h | ≥90dBA |
| Sliwinska-Kowalska 2004 | A-weighted equivalent sound pressure level | Group level | Technical device | Sound level meter, sound pressure level meter | Prevalence | Unclear | Unclear | Relevant category: >85dBA |
| Solecki 2008 | 8h workday (LEX, 8h) | Individual level | Technical device | Dosimeter and sound level meter | Prevalence | Unclear | Shortest-11 years | lifetime dose (noise emission level) 103.9 dBA; s.d.=1.09 dBA), median= 104 dBA; daily noise exposure level LEX,8h=90.2 dBA, noise exposure (per year): 2.54–4.16 Pa2xh, mean = 3.35; s.d.=1.27) Pa2xh |
| Souza 2001 | Cumulative exposure to noise (dBA) | Individual level | Administrative records | Dosimeter | Prevalence | 10 years | Unclear | Relevant category: >85dBA |
| Sriopas 2017 | Time-weighted average of 8h | Individual level | Technical device | Dosimeter | Prevalence | At least 1 year | Working time for 8h for one time | Relevant category: >85dBA |
| Starck 1999 | A-weighted equivalent level | Group level | Technical device | Unclear | Prevalence | Unclear | Unclear | Relevant category: >85dBA |
| Stokholm 2013 | Full-shift noise exposure levels (LAEq values) | Individual level | Technical device | Dosimeter | Unclear | 2001 and 2009–2010 | Unclear | 70-86dBA |
| Strauss 2014 | Time-weighted average | Individual level | Administrative records | Dosimeter | Incidence | 2001–2008 | Unclear | Relevant category: >85dBA |
| Talbott 1999 | Time-weighted average and Cumulative Exposure Level (Expc) | Individual level | Administrative records | Registry data | Prevalence | 1975–1986 | Unclear | Plant 1: 89–101.6dBA; Plant 2: ≤83dBA |
| Toppila 2001 | 10 min samples calculated A-weighted levels weighted noise exposure level | Individual level | Technical device | Datalogger calibrated | Prevalence | Unclear | Unclear | <90dBA; <100dBA; >100dBA |
| Vihma 1981 | Mean noise level (A filter and predominantly the 200-ms time constant) and Impulse noise (the 35-ms time constant) | Group level | Technical device | Noise meter | Prevalence | Unclear | Unclear | Unclear |
| Virkkunen 2005 | Mean level of exposure among the exposed (level L) by occupation and period | Group level | Administrative records | Registry data (FINJEM database) exposures to continuous and impulse noise | Incidence | 18 years | 1985–1994 (9 years follow-up) | 1 = unexposed, 2 = exposed to 80–85dBA, 3 = exposed to >85dBA |
| Whittaker 2014 | 8h equivalent level | Individual level | Technical device | Workplace noise assessment | Prevalence | Unclear | 1h | Relevant category: >85dBA |
| Wu 1987 | A-weighted sound level | Group level | Technical device | Sound level meter | Prevalence | Jun-Aug 1983 | Unclear | Relevant category: >85dB |
| Xiao 2008 | A-weighted equivalent sound level (LAeq), peak sound level | Group level | Technical device | Dosimeter | Prevalence | Unclear | Unclear | Relevant category: >85dBA |
| Xie 2015 | LAeq8h | Individual level | Technical device | Dosimeter | Prevalence | Unclear | Unclear | Relevant category: >85dBA |
| Xue 2018 | Equivalent continuous A-weighted sound pressure level, LAeq8h | Individual level | Technical device | Dosimeter | Prevalence | Unclear | Unclear | Relevant category: >85dBA |
| Yu 2017 | Cumulative noise exposure | Individual level | Technical device | Dosimeter | Prevalence | Unclear | Unclear | Relevant category: >85dBA |
| Yuan 2005 | A-weighted equivalent sound level (LAeq) | Group level | Technical device | Dosimeter | Prevalence | Unclear | Unclear | Relevant category: >85dBA |
| Zhao 1991 | Time-weighted average | Group level | Technical device | Sound level meter | Prevalence | Unclear | 8h | Relevant category: >85dBA |
| Study | Co-exposure |
Prevalence estimate |
|||||
|---|---|---|---|---|---|---|---|
| Study ID | Exposure definition | Potential co-exposure with other occupational risk factors | Prevalence estimate type | Definition of numerator population | Number of study participants in exposed group | Definition of denominator population | Number of study participants in unexposed group |
| Ahmed 2001 | Equivalent continuous noise level (Leq/shift; mean Leq/shift and mean of the total noise immission level (TNIL) | None | Prevalence | Number of workers above 85 dBA | 202 | All inspected workers | 99 |
| Attarchi 2012 | Leq (equivalent continuous noise level) | Yes | Prevalence | Number of workers above 85 dBA | 167 | All inspected workers | 164 |
| Attarchi 2013 | Leq (equivalent continuous noise level) | Mixed organic solvents | Prevalence | Number of workers above 85 dBA | 347 | All inspected workers | 124 |
| Bauer-1991 | A-weighted sound-pressure | No | Prevalence | Number of workers above 85 dBA | 45,154 | All inspected workers | 2,234 |
| Cantley 2015 | 8h time weighted mean | No | Prevalence | Number of workers above 85 dBA | 2,422 | All inspected workers | 6,798 |
| Chang-2003 | TWA (Leq) | No | Prevalence | Number of workers above 85 dBA | 15 | All inspected workers | 5 |
| Chang 2009 | A-weighted (dBA) and time-weighted average | Organic solvents (DMF and toluene) | Prevalence | Number of workers above 85 dBA | 42 | All inspected workers | 17 |
| Chang 2012 | A-weighted decibels (dBA) | Unclear | Prevalence | Number of workers above 85 dBA | 68 | All inspected workers | 120 |
| Chen 2017 | Equivalent continuous dBA weighted sound pressure levels (LEX,8h) | Unclear | Prevalence | Number of workers above 85 dBA | 900 | All inspected workers | 490 |
| de Souza 2015 | A-weighted sound level | Unclear | Prevalence | Number of workers above 85 dBA | 470 | All inspected workers | 1,259 |
| Du 2007 | A-weighted equivalent sound level (LAeq), peak sound level | Unclear | Prevalence | Number of workers above 85 dBA | 1,342 | All inspected workers | 1,937 |
| Guo 2012 | A sound level and sound pressure level (SPL), cumulative noise exposure (CNE) | No | Prevalence | Number of workers above 85 dBA | 60 | All workers in the position | 0 |
| He 2017 | A-weighted equivalent sound level (LAeq) | No | Prevalence | Number of workers above 85 dBA | 165 | All inspected workers | 348 |
| Hong 1998 | Time-weighted average | None | None | Number of workers above 85 dBA | 255 | All inspected workers | 195 |
| Hu 2005 | A-weighted equivalent sound level (LAeq) | No | Prevalence | Number of workers above 85 dBA | 123 | All inspected workers | 68 |
| Hughes 2013 | Equivalent Cumulative Level (ECL) | toluene, styrene, xylene, benzene | Prevalence | Number of workers above 85 dBA | 368 | All inspected workers | 135 |
| Inoue 2005 | A-weighted sound level | No | Prevalence | Number of workers above 85 dBA | 242 | All inspected workers | 173 |
| Ivanovich 1994 | Equivalent noise level (Leq) | Unclear | Prevalence | Number of workers above 85 dBA | 81 | All inspected workers | 168 |
| Johnson 2006 | 8h Level Equivalent Dosimeter Measurements. | Styrene | Prevalence | Number of workers above 85 dBA | 146 | All inspected workers | 167 |
| Kock 2004 | The A-weighted equivalent sound level (LAeq) | No | Prevalence | Number of workers above 85 dBA | 254 | All workers in the industrial sector | 487 |
| Kovacevic 2006 | Equivalent noise levels (Leq) | No | Prevalence | Number of workers above 85 dBA | 111 | All inspected workers | 114 |
| Landen 2004 | Full shift TWA (dBA) | No | Prevalence | Number of workers above 85 dBA | 213 | All inspected workers | 96 |
| Lee 1999 | Time Weighted Average (TWA) level (dBA) | No | Prevalence | Number of workers above 85 dBA | 40 | All inspected workers | 37 |
| Lee 2009 | TWA (dBA) | No | Incidence | Number of workers above 85 dBA | 133 | All inspected workers | 397 |
| Liu 2015 | Environmental noise levels and time-weighted noise level | Total volatile organic compounds (TVOCs) | Prevalence | Number of workers above 85 dBA | 100 | All inspected workers | 147 |
| Lv 2003 | The 8h equivalent continuous A sound level of each subject (LAeq.8h) | No | Prevalence | Number of workers above 85 dBA | 290 | All workers in the position | 29 |
| Maccà 2014 | dBA Lep,d | No | Prevalence | Number of workers above 85 dBA | 137 | All inspected workers | 148 |
| Melamed 1997 | Time-weighted equivalent noise level | Unclear | Prevalence | Number of workers above 85 dBA | 205 | All inspected workers | 765 |
| Morata 1997 | LAEq values in dBA | Solvents | Prevalence | Number of workers above 85 dBA | 74 | All inspected workers | 50 |
| Morata 1997 | Time weighted average | Solvents | Prevalence | Number of workers above 85 dBA | 189 | All inspected workers | 249 |
| Nasir 2012 | Time-weighted average | No | Prevalence | Number of workers above 85 dBA | 136 | All inspected workers | 222 |
| NHIS 2014 | Exposure to “loud” or “very loud” sounds/ noise | No | Prevalence | Number of workers reporting “loud” or “very loud” noise | 3,543 | All inspected workers | 30,502 |
| NHIS 2007 | Exposure to “loud” sounds/ noise | No | Prevalence | Number of workers reporting “loud” noise | 2,094 | All inspected workers | 18,706 |
| NHANES 1999–2004 | Exposure to “loud” noise | No | Prevalence | Number of workers reporting “loud” noise | 1,523 | All inspected workers | 8,198 |
| Noweir 1984 | Average value of the A-weighted sound pressure level and sound pressure levels | None | Prevalence | Number of workers above 90 dBA | 1,404 | All inspected workers | 1,054 |
| Nyarubeli 2018 | A-weighted equivalent noise level and the C-weighted peak noise level | None | Incidence | Number of workers above 85 dBA | 293 | All inspected workers | 33 |
| Osibogun 2000 | Leq 60sec noise (for rapidly fluctuating noise) in the A-weighted network and slow meter response | No | Prevalence | Number of workers above 85 dBA | 116 | All inspected workers | 71 |
| Parent-Thirion 2017 (EWCS) | Exposure to “Noise so loud that you would have to raise your voice to talk to people”. Responses ‘never or almost never’ were classified as ‘not occupationally exposed to noise’ and ‘Around 1/4 of the day time’ or more as “occupationally exposed’ | Unclear | Prevalence | All participants reporting ‘exposure’ for at least 4 h/day | 7,831 | All participants in the study | 35,805 |
| Pawlaczy-Luszczunska 2016 | Daily noise exposure level (LEX,8h), maximum A-weighted sound pressure level (with time constant Slow) (LAmax) and peak C-weighted sound pressure level (LCpeak) | Organic solvents, tobacco smoking | Prevalence | Number of workers above 85 dBA | 50 | All inspected workers | 0 |
| Rabinowitz 2007 | Time Averaged Equivalent (Leq) | No | Incidence | Number of workers above 85 dBA | 1,759 | All inspected workers | 4,458 |
| Rachiotis 2006 | Equivalent continuous Sound Level (Leq dB (A)) | Unclear | Prevalence | Number of workers above 85 dBA | 94 | All inspected workers | 51 |
| Sancini 2014 | Equivalent continuous level noise (LAeq) | No | Prevalence | Number of workers above 85 dBA | 72 | All inspected workers | 119 |
| Seixas 2001 | Losha (TWA), Leq and Lpeak. | No | Prevalence | Number of workers above 85 dBA | 40 | All inspected workers | 19 |
| Shakhatreh 2000 | dB (A) | No | Prevalence | Number of workers above 85 dBA | 22 | All inspected workers | 70 |
| Shi 2009 | Sound pressure level (SPL);A-weighted equivalent sound level (LAeq) | Unclear | Prevalence | Number of workers above 85 dBA | 385 | All inspected workers | 785 |
| Singh 2012 | A weighted (Leq) ambient noise and time-weighted average dose | None declared | Prevalence | Number of workers above 85 dBA | 165 | All inspected workers | 57 |
| Sliwinska-Kowalska 2004 | A-weighted equivalent sound pressure level | Organic Solvents mixture | Prevalence | Number of workers above 85 dBA | 701 | All inspected workers | 205 |
| Solecki 2008 | 8h work day (LEX, 8h) | Unclear | Prevalence | Number of workers above 85 dBA | 44 | All inspected workers | 0 |
| Souza 2001 | Cumulative exposure to noise (dBA) | No | Prevalence | Number of workers above 85 dBA | 585 | All inspected workers | 190 |
| Sriopas 2017 | Time-weighted average of 8h | No | Prevalence | Number of workers above 85 dBA | 113 | All inspected workers | 67 |
| Starck 1999 | A-weighted equivalent level | Smoke | Prevalence | Number of workers above 85 dBA | 46 | All inspected workers | 324 |
| Stokholm 2013 | Full-shift noise exposure levels (LAEq values) | No | Unclear | Number of workers above 85 dBA | 6,262 | All inspected workers | 5,133 |
| Strauss 2014 | Time-weighted average | No | Incidence | Number of workers above 85 dBA | 33,961 | All inspected workers | 6,162 |
| Talbott 1999 | Time-weighted average and Cumulative Exposure Level (Expc) | No | Prevalence | Number of workers above 85 dBA | 62 | All inspected workers | 246 |
| Toppila 2001 | 10min samples calculated A-weighted levels weighted noise exposure level | No | Prevalence | Number of workers above 85 dBA | 706 | All inspected workers | 0 |
| Vihma 1981 | Mean noise level (A filter and predominantly the 200ms time constant) and Impulse noise (the 35ms time constant) | No | Prevalence | Number of workers above 85 dBA | 404 | All inspected workers | 777 |
| Virkkunen 2005 | Mean level of exposure among the exposed (level L) by occupation and period | Impulsive noise | Incidence | Number of workers above 85 dBA | 2,958 | All inspected workers | 3,047 |
| Whittaker 2014 | 8h equivalent level | No | Prevalence | Number of workers above 85 dBA | 115 | All inspected workers | 123 |
| Wu 1987 | A-weighted sound level | No | Prevalence | Number of workers above 85 dBA | 158 | All inspected workers | 158 |
| Xiao 2008 | A-weighted equivalent sound level (LAeq), peak sound level | No | Prevalence | Number of workers above 85 dBA | 953 | All inspected workers | 953 |
| Xie 2015 | LAeq.8h | Unclear | Prevalence | Number of workers above 85 dBA | 98 | All inspected workers | 0 |
| Xue 2018 | Equivalent continuous A-weighted sound pressure level, LAeq8 h | Unclear | Prevalence | Number of workers above 85 dBA | 700 | All inspected workers | 1,113 |
| Yu 2017 | Cumulative noise exposure | Unclear | Prevalence | Number of workers above 85 dBA | 6,112 | All inspected workers | 185 |
| Yuan 2005 | A-weighted equivalent sound level (LAeq) | No | Prevalence | Number of workers above 85 dBA | 88 | All inspected workers | 86 |
| Zhao 1991 | Time-weighted average | No | Prevalence | Number of workers above 85 dBA | 886 | All inspected workers | 215 |
4.2.1. Study type
Fifty-six included studies were cross-sectional and nine were cohort studies.
4.2.2. Population studied
The included studies captured 157,370 workers (15,369 females, 141,675 males). Thirty-one and 33 studies examined male, and both female and male workers, respectively. No study of females only was found.
By WHO region, most studies examined populations in the Western Pacific (24 studies from 6 countries), followed by populations in Europe (16 studies from 10 countries), Americas (10 studies from 2 countries), Eastern Mediterranean (5 studies from 4 countries), and South-East Asia (3 studies from 3 countries), with fewest studies found from Africa (3 studies from 3 countries). The most commonly studied countries were the People's Republic of China (19 studies) and the United States of America (7 studies).
The industrial sectors most commonly studied were mining and quarrying, other manufacturing (7 studies), manufacture of basic metals (6 studies), manufacture of motor vehicles, trailers and semi-trailers (4 studies) and manufacture of textiles (4 studies).
The occupations included in most studies were plant and machine operators and assemblers (19 studies), followed by craft and related trades workers (10 studies), technicians and associate professionals (seven studies), metal processing plant operators (four studies), and petroleum and natural gas refining plant operators and aircraft pilots and related associate professionals (three studies each).
Half of all studies (31) measured occupational exposure to noise using dosimetry. Nineteen used direct measurements collected with sound level meters. The remaining 12 studies measured exposure indirectly (e.g. by means of proxy through occupation); this included the four studies of general populations of workers (Center for Disease Control and Prevention, 2007, Center for Disease Control and Prevention, 2014, Center for Disease Control and Prevention, 2020, Parent-Thirion et al., 2019) that used self-reported measurements collected in surveys (see Table 3 for description of the survey items).
All studies measures enabled us to differentiate “any” from “no” occupational exposure to noise as per our pre-specified levels (see Table 1).
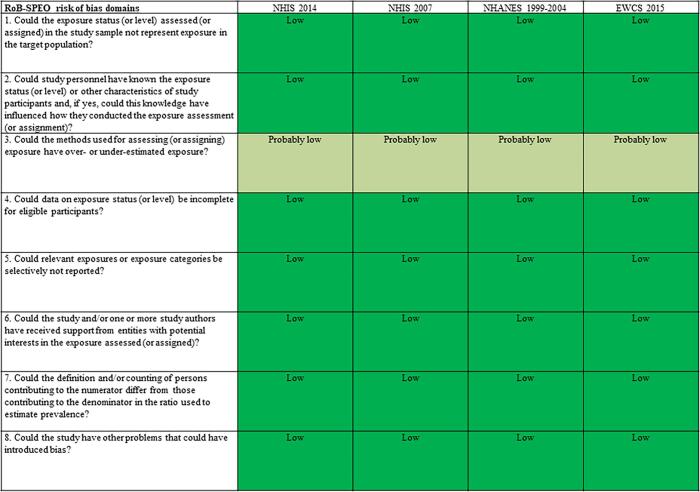
4.3. Risk of bias within studies
The tables of risk of bias of each included study are presented in Appendix 4 in the Supplementary data.
4.3.1. Cohort studies
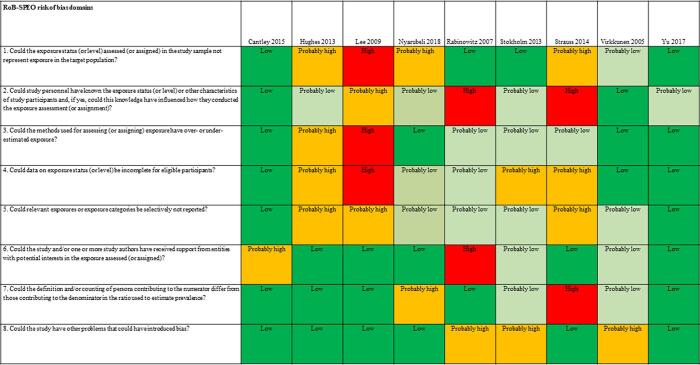
Fig. 2 presents an overview of risk of bias in included cohort studies. Each study was rated along RoB-SPEO’s eight risk of bias domains (Pega et al., 2020b).
Fig. 2.
Summary of risk of bias, cohort studies.
4.3.1.1. Bias in selection of participants into the study
We assessed risk of bias in this domain based on whether the groups being compared were the same in all relevant ways (or as close to this as possible) apart from the exposure. Of the nine included studies, the risk of selection bias was rated to be high for one study due to the study records not providing sufficient detail for target population, study sample, criteria for eligibility for individuals to participate in the study, sampling, recruitment and enrolment procedures, rate of participation in the study, and rate of participation in the exposure assessment (Lee et al., 2009). Three studies were rated as ”probably high” because indirect evidence suggests that inclusion/exclusion criteria, recruitment and enrolment procedures, and participation/response rates differed across groups exposure (Hughes and Hunting, 2013, Strauss et al., 2014). One study was rated as “probably low” because the authors declared the inclusion of white-collar analyses would impact the results (Virkkunen et al., 2005) (Fig. 2).
4.3.1.2. Performance bias
For the eight included studies, this bias was rated “high” for two studies due to exposure assessors and study personnel not being blinded or being incompletely blinded, and the exposure assessment was likely to have been influenced by the lack of blinding (e.g., exposure was systematically assessed differentially for subgroups defined by participant characteristics) (Rabinowitz et al., 2007, Strauss et al., 2014). For one study the risk was deemed “probably high” because the information on blinding was insufficient to permit a rating of risk of bias (Lee et al., 2009). Four studies were rated as “probably low” because indirect evidence suggests that the exposure assessors and study personnel were adequately blinded or blinding was unlikely to influence exposure assessment (Hughes and Hunting, 2013, Stokholm et al., 2013, Yu et al., 2017) (Fig. 2).
4.3.1.3. Bias due to exposure misclassification
For the eight included studies, this bias was rated high for one study, due to direct evidence suggesting that the method adopted in the study for the exposure assessment and assignment does not produce valid, accurate and reliable exposure data, ideally based on direct quantitative exposure measures (Lee et al., 2009); one “probably high” because the information on blinding is insufficient to permit a rating of risk of bias (Lee et al., 2009); another was rated as “probably high” because as described in the report, noise exposure data may overestimate the true exposure to noise among the subjects due to use of hearing protection as per occupational standards and HCPs regulations (Hughes and Hunting, 2013); and three studies were rated as “probably low” because insufficient information existed about the exposure assessment and assignment method to permit rating the risk of bias (Rabinowitz et al., 2007, Stokholm et al., 2013, Strauss et al., 2014) (Fig. 2).
4.3.1.4. Bias due to incomplete exposure data
For the eight included studies, this bias was rated “high” for one study due to insufficient information about the completeness of exposure data (Lee et al., 2009). Three studies were rated as “probably high” because data on exposure level were not shown for all participants (Hughes and Hunting, 2013, Stokholm et al., 2013, Strauss et al., 2014). Two studies was rated as “probably low” because time trend analysis was used to estimate temporal trends for noise exposures within particular standardised job titles (Rabinowitz et al., 2007) (Fig. 2).
4.3.1.5. Bias due to selective reporting of exposures
For the eight included studies, this bias was rated “probably high” for three studies, due to the control group possibly including persons with some previous exposure to occupational exposure to noise, since information on the previous work history of participants was not available; additionally uncontrolled confounders and possible misclassifications due to employment status could have introduced some degree of uncertainty (Hughes and Hunting, 2013, Lee et al., 2009, Strauss et al., 2014). Four studies received a “probably low” rating because the noise was not directly measured, there was indirect evidence that exposure measurement methods were accurate or dosimetry was performed in a small group and broken down for all study participants (Rabinowitz et al., 2007, Stokholm et al., 2013, Virkkunen et al., 2005) (Fig. 2).
4.3.1.6. Bias due to conflict of interest
For the eight included studies, this bias was rated “high” for one study due to two researchers providing consultant services/work to industry (Rabinowitz et al., 2007). One study was rated as “probably high” because the research was funded by grant from industry (Cantley et al., 2015). Two studies were rated as “probably low” because there was indirect evidence which suggested the study was free of support from a company, study author or other entity having a financial interest in the outcome of the study (Stokholm et al., 2013, Virkkunen et al., 2005) (Fig. 2).
4.3.1.7. Bias due to differences in numerator and denominator
For the eight included studies, this bias was rated “probably high” for two studies due to insufficient information provided in study records and our requests for missing data about exposure and control group (including unclear total numbers of study participants for some included studies) were unanswered; it is unclear whether the authors studied all workers (Strauss et al., 2014);. The risk of bias was rated as “probably low” for two studies that dropped some participants from the analysis without clarifying if these were dropped from the numerator and/or denominator (Stokholm et al., 2013, Virkkunen et al., 2005) (Fig. 2).
4.3.1.8. Other bias
For the eight included studies, this bias was rated “probably high” for three studies; for one this due to the declaration that the inclusion of white-collar analyses would impact the results (Virkkunen et al., 2005). Stokholm et al. (2013) declared that individual information on the use of hearing protection devices was not available, which possibly reduced the power to detect an effect. Rabinowitz et al. (2007) did not consider the combined effects of noise (Fig. 2).
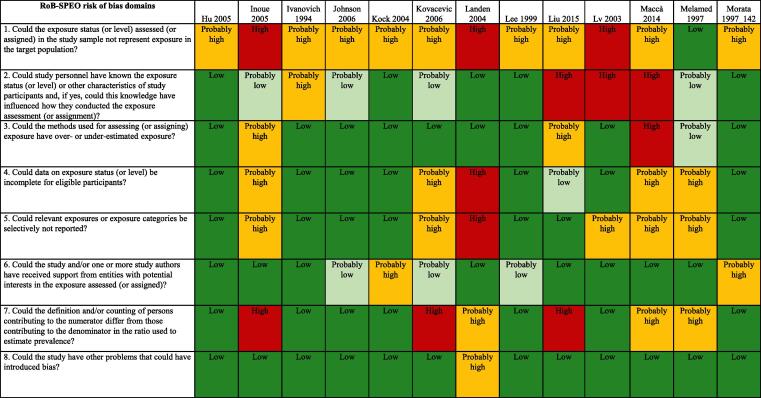
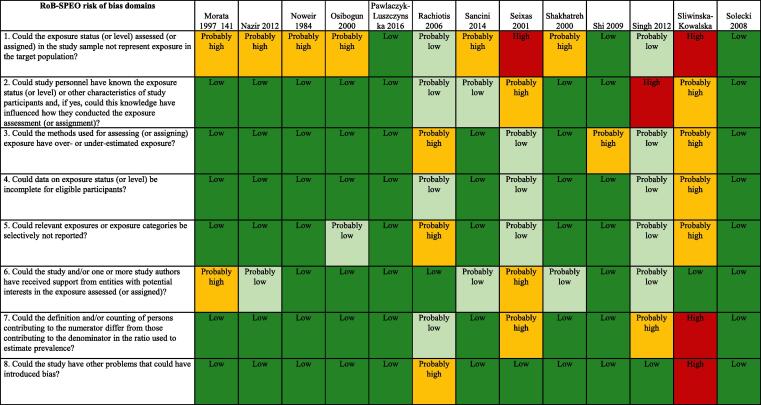
4.3.2. Cross-sectional studies
Fig. 3 presents an overview of risk of bias in included cross-sectional studies rated along RoB-SPEO’s eight risk of bias domains (Pega et al., 2020b).
Fig. 3.
Summary of risk of bias, cross-sectional studies.
4.3.2.1. Bias in selection of participants into the study
We assessed risk of bias in this domain based on whether the groups being compared were the same in all relevant ways (or as close to this as possible) apart from the exposure. Of the 52 included studies, the risk of selection bias was rated to be high for seven studies due to the study records not providing sufficient descriptions of the target population, inclusion/exclusion criteria, recruitment and enrolment procedures, participation/response rates, and/or data on the distribution of relevant study sample and population characteristics (Inoue et al., 2005, Landen et al., 2004, Seixas et al., 2001, Sliwinska-Kowalska et al., 2004, Xie et al., 2015, Xue et al., 2018). Twenty six studies were rated as “probably high” because the recruitment and/or enrolment procedures were not representative of the target population (Attarchi et al., 2012, Chang et al., 2003, Du et al., 2007, Guo et al., 2012, He et al., 2017, Hu et al., 2005, Ivanovich et al., 1994, Johnson et al., 2006, Kock et al., 2004, Kovacevic and Belojevic, 2006, Lee, 1999, Liu et al., 2015, Macca et al., 2015, Morata et al., 1997a, Morata et al., 1997b, Nasir and Rampal, 2012, Noweir, 1984, Osibogun et al., 2000, Sancini et al., 2014, Shakhatreh et al., 2000, Starck et al., 1999, Talbott et al., 1999, Whittaker et al., 2014, Wu et al., 1987, Xiao et al., 2008, Yuan et al., 2005). Nine studies were rated as “probably low” for this item, in general, because indirect evidence suggested that inclusion/exclusion criteria, recruitment and enrolment procedures, and participation/response rates were similar across groups (Bauer et al., 1991, Chang and Chang, 2009, de Souza et al., 2015, Rachiotis et al., 2006, Singh et al., 2012, Souza et al., 2001, Toppila et al., 2001, Vihma, 1981, Zhao et al., 1991). Finally, ten articles were rated as “low” risk of bias for this domain because, in general, the descriptions of the target population, inclusion/exclusion criteria, recruitment and enrolment procedures, participation/response rates were adequately detailed (Ahmed et al., 2001, Attarchi et al., 2013, Chang et al., 2012, Chen et al., 2017, Hong et al., 1998, Melamed et al., 1997, Pawlaczyk-Luszczynska et al., 2016, Shi, 2009, Solecki, 2008, Sriopas et al., 2017) (Fig. 3).
4.3.2.2. Performance bias
From the 52 cross-sectional included studies, the performance bias was rated “high” for four studies, due to exposure assessors and study personnel were not blinded or were incompletely blinded, and the exposure assessment was likely to be influenced by the lack of blinding(Liu et al., 2015, Macca et al., 2015, Singh et al., 2012). Seven studies received a “probably high” rating because indirect evidence suggested that the exposure assessors and study personnel were not adequately blinded (Du et al., 2007, Hong et al., 1998, Ivanovich et al., 1994, Seixas et al., 2001, Sliwinska-Kowalska et al., 2004, Talbott et al., 1999, Whittaker et al., 2014). Eighteen studies were rated as “probably low” because, although the information on blinding was insufficient to permit a rating of “low” risk of bias, indirect evidence indicated that the exposure assessors and study personnel were adequately blinded (Ahmed et al., 2001, Attarchi et al., 2013, Bauer et al., 1991, Chang and Chang, 2009, Chang et al., 2003, de Souza et al., 2015, Guo et al., 2012, Inoue et al., 2005, Johnson et al., 2006, Kovacevic and Belojevic, 2006, Melamed et al., 1997, Rachiotis et al., 2006, Sancini et al., 2014, Souza et al., 2001, Starck et al., 1999, Vihma, 1981, Xiao et al., 2008, Zhao et al., 1991). Lastly, the remaining twenty three studies were rated as “low” because exposure assessors and study personnel were blinded to relevant participant characteristics (e.g. occupation and/or disease status), and the blinding was probably not broken (Attarchi et al., 2012, Chang et al., 2012, Chen et al., 2017, He et al., 2017, Hu et al., 2005, Kock et al., 2004, Landen et al., 2004, Lee, 1999, Morata et al., 1997a, Morata et al., 1997b, Nasir and Rampal, 2012, Noweir, 1984, Osibogun et al., 2000, Pawlaczyk-Luszczynska et al., 2016, Shakhatreh et al., 2000, Shi, 2009, Solecki, 2008, Sriopas et al., 2017, Toppila et al., 2001, Wu et al., 1987, Xie et al., 2015, Xue et al., 2018, Yuan et al., 2005) (Fig. 3).
4.3.2.3. Bias due to exposure misclassification
For the 52 included cross-sectional studies, this bias was rated “high” for only one study (Macca et al., 2015) because it was unclear how exposure assessment was performed and exposure measures were obtained, and there was evidence for concern about the exposure measurement method used. Eight studies were rated as “probably high” because, in general, there was insufficient information about the exposure measurement methods to permit a rating of “high” risk of bias but there was indirect evidence that suggested that the methods were not robust, as described by the criteria for a rating of high risk of bias (de Souza et al., 2015, Inoue et al., 2005, Liu et al., 2015, Rachiotis et al., 2006, Shi, 2009, Sliwinska-Kowalska et al., 2004, Talbott et al., 1999, Xiao et al., 2008). Fifteen studies were rated as “probably low” because there was insufficient information about the exposure measurement methods to permit a rating of “low” risk of bias. However, there was indirect evidence that exposure measurement methods were accurate, as described by the criteria for a rating of “low” risk of bias (Attarchi et al., 2013, Bauer et al., 1991, Chang and Chang, 2009, Chang et al., 2003, Chen et al., 2017, Du et al., 2007, Guo et al., 2012, Melamed et al., 1997, Seixas et al., 2001, Singh et al., 2012, Souza et al., 2001, Starck et al., 1999, Vihma, 1981, Whittaker et al., 2014, Zhao et al., 1991). Lastly, twenty eight studies (Ahmed et al., 2001, Attarchi et al., 2012, Chang et al., 2012, He et al., 2017, Hong et al., 1998, Hu et al., 2005, Ivanovich et al., 1994, Johnson et al., 2006, Kock et al., 2004, Kovacevic and Belojevic, 2006, Landen et al., 2004, Lee, 1999, Lv et al., 2003, Morata et al., 1997a, Morata et al., 1997b, Nasir and Rampal, 2012, Noweir, 1984, Osibogun et al., 2000, Pawlaczyk-Luszczynska et al., 2016, Sancini et al., 2014, Shakhatreh et al., 2000, Solecki, 2008, Sriopas et al., 2017, Toppila et al., 2001, Wu et al., 1987, Xie et al., 2015, Xue et al., 2018, Yuan et al., 2005) were classified as low risk of bias because, in general, the reviewers considered direct evidence that exposure was consistently assessed, using well-established methods that directly measure exposure (Fig. 3).
4.3.2.4. Bias due to incomplete exposure data
For the 52 cross-sectional included studies, this bias was rated high for one study because participation in the study was low enough to possibly introduce bias (Landen et al., 2004). Seven studies were rated as “probably high” because data on exposure level are not shown for all participants (Chen et al., 2017, de Souza et al., 2015, Inoue et al., 2005, Kovacevic and Belojevic, 2006, Macca et al., 2015, Melamed et al., 1997, Sliwinska-Kowalska et al., 2004). Sixteen studies were rated as “probably low” because, in general, the proportion of study participants who participated in the exposure assessment was acceptable and the reasons for non-participation in exposure assessment were acceptable (Ahmed et al., 2001, Attarchi et al., 2013, Bauer et al., 1991, Chang et al., 2003, Hong et al., 1998, Liu et al., 2015, Rachiotis et al., 2006, Seixas et al., 2001, Singh et al., 2012, Souza et al., 2001, Starck et al., 1999, Talbott et al., 1999, Vihma, 1981, Whittaker et al., 2014, Wu et al., 1987, Zhao et al., 1991). The remaining 28 studies were rated as “low” for this item because, on the whole, data on exposure status (or level) seemed complete for eligible participants (Attarchi et al., 2012, Chang and Chang, 2009, Chang et al., 2012, Du et al., 2007, Guo et al., 2012, He et al., 2017, Hu et al., 2005, Ivanovich et al., 1994, Johnson et al., 2006, Kock et al., 2004, Lee, 1999, Lv et al., 2003, Morata et al., 1997a, Morata et al., 1997b, Nasir and Rampal, 2012, Noweir, 1984, Osibogun et al., 2000, Pawlaczyk-Luszczynska et al., 2016, Sancini et al., 2014, Shakhatreh et al., 2000, Shi, 2009, Solecki, 2008, Sriopas et al., 2017, Toppila et al., 2001, Xiao et al., 2008, Xie et al., 2015, Xue et al., 2018, Yuan et al., 2005) (Fig. 3).
4.3.2.5. Bias due to selective reporting of exposures
For the 52 included studies, this bias was rated as “high” for three studies, because there was insufficient information about selective exposure reporting to permit a judgment of “low” or “probably low” risk of bias but there was sufficient evidence, which suggests the study was not free of selective exposure reporting (Attarchi et al., 2013, Chen et al., 2017, Landen et al., 2004). There were fourteen studies rated as “probably high” because, in general, there was indirect evidence, which suggested the study was not free of selective exposure reporting (Ahmed et al., 2001, de Souza et al., 2015, Inoue et al., 2005, Kovacevic and Belojevic, 2006, Lv et al., 2003, Macca et al., 2015, Melamed et al., 1997, Rachiotis et al., 2006, Sliwinska-Kowalska et al., 2004, Sriopas et al., 2017, Vihma, 1981, Whittaker et al., 2014, Wu et al., 1987, Zhao et al., 1991). Ten studies were classified as “probably low” for this item because, in general, the exposure assessment was based on individual exposure measurements (Chang and Chang, 2009, Chang et al., 2003, Guo et al., 2012, Hong et al., 1998, Osibogun et al., 2000, Seixas et al., 2001, Singh et al., 2012, Souza et al., 2001, Starck et al., 1999, Talbott et al., 1999). Finally, the remaining 25 studies were considered as “low” risk of bias because of sufficient information about exposure selective reporting (Attarchi et al., 2012, Bauer et al., 1991, Chang et al., 2012, Du et al., 2007, He et al., 2017, Hu et al., 2005, Ivanovich et al., 1994, Johnson et al., 2006, Kock et al., 2004, Lee, 1999, Liu et al., 2015, Morata et al., 1997a, Morata et al., 1997b, Nasir and Rampal, 2012, Noweir, 1984, Pawlaczyk-Luszczynska et al., 2016, Sancini et al., 2014, Shakhatreh et al., 2000, Shi, 2009, Solecki, 2008, Toppila et al., 2001, Xiao et al., 2008, Xie et al., 2015, Xue et al., 2018, Yuan et al., 2005) (Fig. 3).
4.3.2.6. Bias due to conflict of interest
From the 52 cross-sectional included articles, this bias was rated as “high” for only one study because the authors received funding from a company (ford.com) which could represent a potential interest in the study’s results (Talbott et al., 1999). For five studies the bias was rated “probably high” because, in general, there was indirect evidence which suggests the study was not free of support from a company, study author or other entity having a financial interest in the outcome of the study (Chang et al., 2012, Kock et al., 2004, Morata et al., 1997a, Morata et al., 1997b, Seixas et al., 2001). Seventeen studies were classified as “probably low” because, in general, there was insufficient information to permit a rating of low risk of bias but there is indirect evidence which suggests the study was free of support from a company, study author or other entity having a financial interest in the outcome of the study, as described by the criteria for a rating of low risk of bias (Attarchi et al., 2012, Attarchi et al., 2013, Bauer et al., 1991, Chang and Chang, 2009, Chang et al., 2003, Chen et al., 2017, de Souza et al., 2015, Du et al., 2007, Guo et al., 2012, He et al., 2017, Hong et al., 1998, Hu et al., 2005, Inoue et al., 2005, Ivanovich et al., 1994, Johnson et al., 2006, Kovacevic and Belojevic, 2006, Landen et al., 2004, Lee, 1999, Liu et al., 2015, Lv et al., 2003, Macca et al., 2015, Melamed et al., 1997, Nasir and Rampal, 2012, Noweir, 1984, Osibogun et al., 2000, Pawlaczyk-Luszczynska et al., 2016, Rachiotis et al., 2006, Sancini et al., 2014, Shakhatreh et al., 2000, Shi, 2009, Singh et al., 2012, Sliwinska-Kowalska et al., 2004, Solecki, 2008, Souza et al., 2001, Sriopas et al., 2017, Starck et al., 1999, Toppila et al., 2001, Vihma, 1981, Whittaker et al., 2014, Wu et al., 1987, Xiao et al., 2008, Xie et al., 2015, Xue et al., 2018, Yuan et al., 2005, Zhao et al., 1991. Lastly, twenty nine studies were considered as low risk of bias for this item because, in general, there was sufficient evidence which suggests they were free of competing interest between authors and funding entities {Ahmed et al., 2001 #1597) (Fig. 3).
4.3.2.7. Bias due to differences in numerator and denominator
For the 52 included cross-sectional studies, this bias was rated as “high” for five studies (Hong et al., 1998, Inoue et al., 2005, Kovacevic and Belojevic, 2006, Liu et al., 2015, Sliwinska-Kowalska et al., 2004) because, in general, the numerator and denominator are defined and/or counted differently, and/or the shortest prevalence period was inappropriate (e.g. too short to detect exposure). Seven studies were rated as “probably high” for this bias item because, in general, indirect evidence suggests that the numerator and denominator for the prevalence estimate did not seem appropriate (Chang et al., 2003, Chen et al., 2017, Landen et al., 2004, Macca et al., 2015, Melamed et al., 1997, Seixas et al., 2001, Singh et al., 2012). Eleven studies were classified as “probably low” because, in general, the proportion of persons invited to participate in the study who in fact did participate was acceptable (Bauer et al., 1991, Chang and Chang, 2009, Du et al., 2007, Rachiotis et al., 2006, Souza et al., 2001, Starck et al., 1999, Talbott et al., 1999, Vihma, 1981, Whittaker et al., 2014, Xiao et al., 2008, Zhao et al., 1991). Finally, twenty nine studies were rated as “low” because differences in numerator and denominator seem appropriate (Ahmed et al., 2001, Attarchi et al., 2012, Attarchi et al., 2013, Chang et al., 2012, de Souza et al., 2015, Guo et al., 2012, He et al., 2017, Hu et al., 2005, Ivanovich et al., 1994, Johnson et al., 2006, Kock et al., 2004, Lee, 1999, Lv et al., 2003, Morata et al., 1997a, Morata et al., 1997b, Nasir and Rampal, 2012, Noweir, 1984, Osibogun et al., 2000, Pawlaczyk-Luszczynska et al., 2016, Sancini et al., 2014, Shakhatreh et al., 2000, Shi, 2009, Solecki, 2008, Sriopas et al., 2017, Toppila et al., 2001, Wu et al., 1987, Xie et al., 2015, Xue et al., 2018, Yuan et al., 2005) (Fig. 3)
4.3.2.8. Other bias
From the 52 cross-sectional studies, one was rated as “high” (Sliwinska-Kowalska et al., 2004) because the authors did not study the impact of the use of personal protective equipment on hearing function and did not control for occupational co-exposures to ototoxic chemical agents. Three were rated as “probably high” because there was indirect evidence suggesting the study was not free of other potential sources of bias (Landen et al., 2004, Rachiotis et al., 2006, Starck et al., 1999). Two were rated as “probably low” because there was insufficient information to permit a rating of “low” risk of bias but there was indirect evidence, which suggests the study was free of other potential sources of bias (Sriopas et al., 2017, Whittaker et al., 2014). The vast majority of studies (46) were classified as “low” risk of bias for this item because they appeared to be free of other potential sources of bias (Fig. 3).
4.3.3. Population-based cross-sectional survey
For the eight domains of risk of bias for the population-based cross-sectional survey, only the bias due to exposure misclassification was rated “probably low” for all studies because the method of assessing occupational noise exposure was subjective (Fig. 4).
Fig. 4.
Summary of risk of bias, Population-based cross-sectional surveys.
4.4. Synthesis of results
4.4.1. All prevalence estimates
A data sheet with all prevalence estimates is provided in Appendix 5 in the Supplementary data. If available to us, the prevalence estimates are presented fully disaggregated by country, sex, age group and industrial sector or occupation. The data in the sheet is prepared in a convenient format for ready use as input data for modelling occupational exposure to noise.
4.4.2. Pooled prevalence estimate
For our main meta-analysis, we prioritized the included studies that surveyed national probability samples of general populations of workers. These are the European Working Condition Survey (EWCS) (Parent-Thirion et al., 2019); National Health Interview Survey (NHIS) (Center for Disease Control and Prevention, 2007, Center for Disease Control and Prevention, 2014) and National Health and Nutrition Examination Survey (NHANES) (Center for Disease Control and Prevention and National Center for Health Statistics 2020). We judged the other 60 included studies to capture workers in (selected) industrial sectors and/or occupations with relatively high occupational exposure to noise that did not equally represent exposure in the general population of workers, and therefore we excluded these studies from the main meta-analysis. The main meta-analysis therefore included four studies with a total of 108,256 participants from 38 countries in two WHO regions (Americas and Europe) that reported estimates of the prevalence of occupational exposure to noise among workers (general population) using self-reported, subjective measurements collected in large-scale, official surveys. These four studies were thus relatively homogenous in population and exposure. The forest plot from the meta-analysis is presented in Fig. 5. The pooled prevalence of any occupational exposure to noise was 0.17 (95% CI 0.16 to 0.19, 4 studies, 108,256 participants, 38 countries). The statistical heterogeneity was high, with an I2 of 98%.
Fig. 5.
Main meta-analysis, Is occupationally exposed to noise (≥85dBA), studies of general populations of workers.
4.5. Additional analyses
4.5.1. Subgroup analyses
We conducted subgroup analyses using all studies included in the systematic review, where results were disaggregated by the relevant variable, including the population-based studies.
4.5.1.1. By WHO region and/or country
By WHO region, the pooled prevalence estimates for studies of the general population of workers is presented in Fig. 6 and Table 4 and for studies of studies of workers in selected occupations and/or industrial sectors with higher exposure is presented in Fig. 7 and Table 5. In both analyses, the prevalence estimates differed substantially between the WHO regions included in the respective subgroup analyses (test for subgroup differences p < 0.001).
Fig. 6.
Subgroup analysis by WHO region, Is occupationally exposed to noise (≥85dBA), studies of the general population of workers.
Table 4.
Subgroup analysis by WHO region, Is occupationally exposed to noise, studies of the general population of workers.
| WHO region | Prevalence (95% confidence interval) | Number of studies2 |
|---|---|---|
| Africa | – | – |
| Americas | 0.12 (0.09–0.15) | 3 studies |
| Eastern Mediterranean | – | – |
| Europe | 0.18 (0.16–0.19) | 1 study |
| South-East Asia | – | – |
| Western Pacific | – | – |
Footnotes: Test for subgroup differences found p < 0.001.
Fig. 7.
Subgroup analysis by WHO region, Is occupationally exposed to noise (≥85dBA), all included studies.
Table 5.
Subgroup analysis by WHO region, Is occupationally exposed to noise, studies of workers in selected occupations and/or industrial sectors with higher exposure.
| WHO region | Prevalence (95% confidence interval) | Number of studies |
|---|---|---|
| Africa | 0.74 (0.51–0.96) | 2 studies |
| Americas | 0.39 (0.34–0.45) | 13 studies |
| Eastern Mediterranean | 0.60 (0.51–0.68) | 5 studies |
| Europe | 0.26 (0.13–0.39) | 15 studies |
| South-East Asia | 0.62 (0.46–0.77) | 3 studies |
| Western Pacific | 0.54 (0.40–0.69) | 21 studies |
Footnotes: Test for subgroup differences found p < 0.001.
4.5.1.2. By sex
As noted above (see Section 3.9), for the subgroup analyses by sex, we prioritized evidence from the included studies that surveyed national probability samples of general populations of workers. The reason for this was that these studies provided the prevalence that we were interested in. The subgroup analysis (Fig. 8) found that the prevalence of occupational exposure to noise was lower among females with 0.12 (95% CI 0.10 to 0.13) than among males with 0.24 (95% CI 0.21 to 0.26)). The test of subgroup differences was statistically significant (p < 0.001).
Fig. 8.
Subgroup analysis by sex, Is occupationally exposed to noise (≥85dBA).
4.5.1.3. By industrial sector
By industrial sector, the pooled prevalence estimates for ISIC codes at one-digit level with available data are presented in Fig. 9 and Table 6. Prevalence estimates differed substantially between industrial sectors (test for subgroup differences p < 0.001) (see Table 6).
Fig. 9.
Subgroup analysis by industrial sector, Is occupationally exposed to noise (≥85dBA), studies of general populations of workers.
Table 6.
Subgroup analysis by industrial sector, Is occupationally exposed to noise, studies of general populations of workers.
| Industrial sector (ISIC code) | Prevalence (95% confidence interval) | Number of studies |
|---|---|---|
| A Agriculture, forestry and fishing | 0.37 (0.07–0.17) | 3 studies |
| B Mining and quarrying | 0.51 (0.39–0.62) | 38 studies |
| E Water supply; sewerage, waste management and remediation activities | 0.15 (0.14–0.17) | 2 studies |
| F Construction | 0.40 (0.27–0.54) | 5 studies |
| G Wholesale and retail trade; repair of motor vehicles and motorcycles | 0.06 (0.06–0.07) | 2 studies |
| H Transportation and storage | 0.34 (0.22–0.48) | 6 studies |
| I Accommodation and food service activities | 0.07 (0.05, 0.10) | 2 studies |
| J Information and communication activities | 0.31 (0.01–0.68) | 3 studies |
| K Financial and insurance activities | 0.01 (0.01–0.02) | 2 studies |
| L Real estate activities | 0.05 (0.04–0.07) | 2 studies |
| M Professional, scientific and technical activities | 0.04 (0.03–0.05) | 2 studies |
| N Administrative and support service activities | 0.05 (0.00–0.15) | 2 studies |
| O Public administration and defence; compulsory social security | 0.11 (0.08–0.14) | 2 studies |
| P Education | 0.04 (0.04–0.05) | 2 studies |
| Q Human health and social work activities | 0.03 (0.02–0.03) | 2 studies |
| S Other service activities | 0.23 (0.02–0.48) | 3 studies |
Footnotes: Test for subgroup differences found p < 0.001.
4.5.1.4. By occupation
By occupation, the pooled prevalence for ISCO codes (at one-digit level) with available data are presented in Fig. 10. For studies that did not report ISCO codes, we coded occupations ourselves based on the information reported in the study records or other study documentation that we accessed, such as study protocols and questionnaires. Evidence included within subgroups defined by occupation may be heterogeneous. Different studies may have coded the same occupations differently. Exposure might differ in the same occupation. For example, in the People's Republic of China, large enterprises often use automated machines which decrease the exposure time of noise for workers, whereas small and medium-sized enterprises may not use these more expensive, newer machines, suggesting that occupational exposure to noise differs by enterprise size even within occupation. The forest plot of the subgroup analysis (Fig. 10) shows that prevalence estimates differed substantially between the nine groups of occupations captured in the body of evidence included in this systematic review (test for subgroup differences p < 0.001) (see Table 7).
Fig. 10.
Subgroup analysis by occupation, Is occupationally exposed to noise (≥85dBA).
Table 7.
Subgroup analysis by occupation, Is occupationally exposed to noise.
| Industrial sector (ISIC code) | Prevalence (95% confidence interval) | Number of studies |
|---|---|---|
| 0 Armed forces occupations | 0.13 (0.06–0.20) | 3 studies |
| 1 Managers | 0.10 (0.08–0.13) | 4 studies |
| 2 -Professionals | 0.12 (0.07–0.16) | 4 studies |
| 3 Technicians and Associate Professionals | 0.42 (0.31–0.53) | 10 studies |
| 4 Clerical support workers | 0.07 (0.06–0.08) | 1 study |
| 5 Service and sales workers | 0.08 (0.04–0.13) | 3 studies |
| 6 Skilled Agricultural, Forestry and Fishery Workers | 0.15 (0.11–0.18) | 2 studies |
| 7 Craft and Related Trades Workers | 0.51 (0.20–0.82) | 12 studies |
| 8 Plant and Machine Operators and Assemblers | 0.49 (0.37–0.62) | 19 studies |
| 9 Elementary Occupations | 0.29 (0.24–0.34) | 5 studies |
Footnotes: Test for subgroup differences found p < 0.001.
4.6. Quality of evidence
Using the QoE-SPEO approach for assessing quality of evidence of the entire body of evidence, which WHO developed specifically for the WHO/ILO Joint Estimates (forthcoming), we judged the body of evidence used in the main meta-analysis. This is the prioritized evidence from the four population-based studies of the general population of workers.
4.6.1. Expected heterogeneity
The expected heterogeneity is defined as “the actual, real and non-spurious variability in the prevalence of exposure within or between individual workers” (Pega et al., submitted for publication). We anticipated heterogeneity both within and between workers, based on different levels of occupational exposure to noise between and within occupations, work sites, regulations and compliance, use of personal protective equipment, job tasks, and technology and tools used. Consequently, we rated expected heterogeneity as “high”.
4.6.2. Risk of bias
The use of survey questions may have introduced serious risk of bias across studies in the third RoB-SPEO domain (Pega et al., 2020a, Pega et al., 2020b): misclassification bias in the assessment of the exposure to the risk factor. Such bias could have occurred even though the survey questions that are used in the included studies are standardized and validated against objective, individual measurements. We downgraded the quality of evidence by one level (−1) due to our serious concerns in this QoE-SPEO domain.
4.6.3. Indirectness
Evidence is limited to populations in 38 countries in two WHO regions. All of these countries are high-income countries. We have serious concerns that this study population does not match the population of interest. We downgraded the quality of evidence for “serious” concerns for indirectness by one level (−1).
4.6.4. Inconsistency, imprecision, and publication bias
We did not have any serious concerns in the domains of inconsistency, imprecision or publication bias. We had rated expected heterogeneity as “high” and found high statistical variability across studies (I2 98%), and therefore we were not concerned for inconsistency. Although expected heterogeneity was “high”, the 95% CI of the pooled prevalence estimate is narrow, but the pooled body of evidence includes a large sample (108,256 participants), and this probably explains the relatively narrow CI even if heterogeneity is expected to be high between and within studies. No evidence was found for publication bias, and the body of evidence consists of established, large studies conducted by producers of official statistics. Therefore, we did not downgrade for any of these three QoE-SPEO domains (+/- 0).
4.6.5. Final decision on quality of evidence
The grading started from a rating of “high”. We downgraded the quality of evidence by one grade each for risk of bias and indirectness. Our final rating was therefore that the body of evidence was of “low quality”; further research is very likely to have an important impact on our confidence in the estimate of prevalence and is likely to change the estimate.
5. Discussion
5.1. Summary of evidence
As shown in the table of summary of findings (Table 8), the pooled prevalence of any occupational exposure to noise was 0.17 (95% CI 0.16 to 0.19, 4 studies, 108,256 participants, 38 countries, I2 98%). By region, the pooled prevalence was 0.74 for Africa (95% CI 0.51 to 0.96, 2 studies); 0.39 for the Americas (95% CI 0.34 to 0.45, 13 studies); 0.60 for the Eastern Mediterranean (95% CI 0.51 to 0.68, 5 studies); 0.26 for Europe (95% CI 0.13 to 0.39, 15 studies); for South-East Asia was 0.62 (95% CI 0.46 to 0.77, 3 studies); and 0.54 for the Western Pacific (95% CI 0.40 to 0.69, 21 studies) (test for subgroup differences p < 0.001). Subgroup analyses showed that pooled prevalence also differed by sex, industrial sector and occupation.
Table 8.
Summary of findings.
| Prevalence of any occupational exposure to noise | ||||
|---|---|---|---|---|
|
Population: Any workers Settings: All countries and work settings Exposure: Occupational exposure to noise (>85dBA) | ||||
| Outcome | Prevalence estimate (95% CI) | No. of participants (studies) | QoE-SPEO quality of the evidence rating | Comments |
| Any occupational exposure to noise (defined as ≥ 85 dBA; measured using indirect (survey) measurements) | 0.17 (0.16, 0.19) | 108,256 participants (4 studies) | ⊕⊕⊝⊝ a,b,c Low |
The other 60 studies not included in the main meta-analysis generally support this estimate but indicated higher prevalence because they studied non-general populations at higher risk (defined by occupations and industrial sectors with known high occupational exposure to noise). |
| CI: confidence interval | ||||
| QoE-SPEO quality of evidence ratings: High quality: Further research is very unlikely to change our confidence in the estimate of prevalence. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of prevalence and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of prevalence and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
aExpected heterogeneity was rated as “high”.
bDowngraded by one grade because of serious concern for risk of bias (primarily for bias in the exposure assessment).
cDowngraded by one grade because of serious concern for indirectness.
5.2. Comparison with previous systematic reviews evidence
To our knowledge, there is no prior systematic review or meta-analytic evidence that we could compare our systematic review and meta-analysis against.
6. Use of evidence for burden of disease estimation
This systematic review and meta-analysis was conducted by WHO and ILO, supported by a large network of experts, for the development of the WHO/ILO Joint Estimates. More specifically, it provides the crucial evidence base for both organizations to consider producing global health estimates of occupational exposure to noise. The systematic review found a large body of evidence comprising many studies. Overall, we judged this body of evidence to be of low quality (at least the prioritized evidence that contributed the main analysis). Producing estimates of occupational exposure to noise appears to be evidence-based and warranted, and the pooled prevalence estimate from the main and subgroup analyses appear suitable as input data for WHO/ILO Joint Estimates.
7. Conclusions
Our systematic review and meta-analysis found that occupational exposure to noise is prevalent among general populations of workers. The current body of evidence is, however, of low quality, due to serious concerns for risk of bias and indirectness. Producing estimates occupational exposure to noise nevertheless appears evidence-based, and the pooled effect estimates presented in this systematic review are suitable as input data for the WHO/ILO Joint Estimates.
8. Differences between protocol and systematic review
-
●
We intended to use a modified version of the Navigation Guide risk of bias tool, but then developed a tool specifically for assessing risk of bias in studies estimating prevalence of exposure with occupational exposure to noises (RoB-SPEO; Pega et al., 2020b) and applied this dedicated tool in our systematic review.
-
●
We intended to use a modified version of the Navigation Guide approach for assessing quality of evidence, but then WHO, with a Working Group of individual experts, developed the QoE-SPEO approach specifically for assessing quality of evidence in studies estimating prevalence of exposure to occupational risk factors (Pega et al., submitted for publication) and then applied this dedicated tool in our systematic review.
-
●
In our protocol we planned to conduct sensitivity analyses, but we did not conduct these.
-
●
We did not intend to quantitatively meta-analyse prevalence estimates but did so in the systematic review because the health estimation will require pooled estimates, rather than individual estimates only.
Financial support
All authors are salaried staff members of their respective institutions. The publication was prepared with financial support from the World Health Organization cooperative agreement with the Centres for Disease Control and Prevention National Institute for Occupational Safety and Health of the United States of America (Grant 1E11OH0010676-02; Grant 6NE11OH010461-02-01; and Grant 5NE11OH010461-03-00); the German Federal Ministry of Health (BMG Germany) under the BMG-WHO Collaboration Programme 2020-2023 (WHO specified award ref. 70672); and the Spanish Agency for International Cooperation (AECID) (WHO specified award ref. 71208).
Sponsors
The sponsors of this systematic review are the World Health Organization and the International Labour Organization.
Author contributions
Had the idea for this systematic review: FP, Ivan Ivanov (WHO), Nancy Leppink (ILO).
Selected the lead reviewers and gathered the review teams: FP, Ivan Ivanov, Nancy Leppink.
Coordinated the entire series of systematic reviews: FP, Yuka Ujita (ILO).
Were the lead reviewers of this systematic review: LT, DS.
Led the design of the systematic review including developed the standard methods: FP.
Contributed substantially to the design of the systematic review: LT, TA, WA, MA, MM, DS.
Conducted the search: LT, FP, TA, WA, MA, MM, WH, XS, MZ, DS.
Selected studies: LT, TA, WA, MA, MM, WH, XS, MZ, DS.
Extracted data: LT, TA, WA, MA, MM, WH, XS, MZ, DS, AMD.
Requested missing data: LT, DS, AMD.
Assessed risk of bias: LT, TA, MA, MM, WH, XS, MZ, DS.
Conducted the meta-analyses: LT, FP, CA, AMD, DS.
Assessed quality of evidence: LT, FP, AMD, DS.
Developed the standards and wrote the template for all systematic reviews in the series: FP.
Wrote the first draft of the manuscript using the template: LT, FP, AMD, DS.
Revised the manuscript critically for important intellectual content: LT, FP, AMD, TA, WA, MA, MM, DS.
Ensured tailoring of the systematic review for WHO/ILO estimation purposes: FP.
Ensured harmonization across systematic reviews in the series: FP.
Approved the final version of the systematic review to be published: All authors.
Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: All authors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank Paul Whaley (Lancaster University, United Kingdom of Great Britain and Northern Ireland) and Tim Driscoll (University of Sydney, Australia) for the editorial guidance and support. We also thank Ivan Ivanov (WHO), Nancy Leppink (ILO) and Yuka Ujita (ILO) for their coordination and other support for this systematic review; Marco A.N. de Araújo (Oswaldo Cruz Foundation, Brazil) for the contributions at an early stage of the systematic review; Carel TJ Hulshof (University of Amsterdam, The Netherlands), Grace Sembajwe (Hofstra University, United States of America), Flavia Torreão Thiemann (Physics Institute of São Carlos, University of São Paulo, Brazil), and Otavio Henrique Thiemann (Physics Institute of São Carlos, University of São Paulo, Brazil) for retrieving selected full-text articles; Talita Monsores Paixão (Oswaldo Cruz Foundation, Brazil) for assisting with the inclusion of references and formatting tables and figures; and Natalie Momen (WHO) for technically editing the manuscript. Elizabeth Masterson (Centers for Disease Control and Prevention, United States of America) assisted with the preparation of the data from the NHIS and NHANES, and Carel TJ Hulshof and Subas Neupane (Tampere University, Finland) assisted with the preparation of the data from the EWCS. The authors alone are responsible for the views expressed in this article, and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
Handling Editor: Paul Whaley
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envint.2021.106380.
Contributor Information
Liliane R. Teixeira, Email: lilianeteixeira@ensp.fiocruz.br.
Frank Pega, Email: pegaf@who.int.
Wagner de Abreu, Email: abreu.wagner41@gmail.com.
Marcia S. de Almeida, Email: soalheir@ensp.fiocruz.br.
Carlos A.F. de Andrade, Email: carlos.andrade@ensp.fiocruz.br.
Tatiana M. Azevedo, Email: tamaze@gmail.com.
Angel M. Dzhambov, Email: angelleloti@gmail.com.
Weijiang Hu, Email: huwj@niohp.chinacdc.cn.
Marta R.V. Macedo, Email: mribeiro@fiocruz.br.
Martha S. Martínez-Silveira, Email: martha.silveira@gmail.com.
Xin Sun, Email: sunxin@niohp.chinacdc.cn.
Meibian Zhang, Email: mbzhang@cdc.zj.cn.
Siyu Zhang, Email: zhangsy@niohp.chinacdc.cn.
Denise T. Correa da Silva, Email: denisetorreao@gmail.com.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- Ahmed H.O., Dennis J.H., Badran O., Ismail M., Ballal S.G., Jerwood D. Occupational noise exposure and hearing loss of workers in two plants in eastern saudi Arabia. Ann. Occup. Hyg. 2001;45:371–380. [PubMed] [Google Scholar]
- Attarchi M., Dehghan F., Safakhah F., Nojomi M., Mohammadi S. Effect of exposure to occupational noise and shift working on blood pressure in rubber manufacturing company workers. Ind. Health. 2012;50:205–213. doi: 10.2486/indhealth.ms1321. [DOI] [PubMed] [Google Scholar]
- Attarchi M., Golabadi M., Labbafinejad Y., Mohammadi S. Combined effects of exposure to occupational noise and mixed organic solvents on blood pressure in car manufacturing company workers. Am. J. Ind. Med. 2013;56:243–251. doi: 10.1002/ajim.22086. [DOI] [PubMed] [Google Scholar]
- Basner, M., McGuire, S., 2018. WHO environmental noise guidelines for the european region: a systematic review on environmental noise and effects on sleep. Int. J. Environ. Res. Public Health 15. [DOI] [PMC free article] [PubMed]
- Bauer P., Korpert K., Neuberger M., Raber A., Schwetz F. Risk factors for hearing loss at different frequencies in a population of 47,388 noise-exposed workers. J. Acoust. Soc. Am. 1991;90:3086–3098. doi: 10.1121/1.401418. [DOI] [PubMed] [Google Scholar]
- Beller, E.M., Glasziou, P.P., Altman, D.G., Hopewell, S., Bastian, H., Chalmers, I., Gøtzsche, P.C., Lasserson, T., Tovey, D., Group, f.t.P.f.A., 2013. PRISMA for abstracts: reporting systematic reviews in journal and conference abstracts. PLoS Med. 10, e1001419. [DOI] [PMC free article] [PubMed]
- Cantley L.F., Galusha D., Cullen M.R., Dixon-Ernst C., Rabinowitz P.M., Neitzel R.L. Association between ambient noise exposure, hearing acuity, and risk of acute occupational injury. Scand. J. Work Environ. Health. 2015;41:75–83. doi: 10.5271/sjweh.3450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention; National Center for Health Statistics, 2007. National Health Interview Survey: 2007 Data Release ed^eds. Atlanta: CDC.
- Center for Disease Control and Prevention; National Center for Health Statistics, 2014. National Health Interview Survey: 2014 Data Release ed^eds. Atlanta: CDC.
- Center for Disease Control and Prevention; National Center for Health Statistics, 2020. National Health and Nutrition Examination Survey: Questionnaires, Datasets, and Related Documentation: 1999-2000, 2001-2003, 2003-2004. ed^eds. Atlanta: CDC.
- Chang S.J., Chang C.K. Prevalence and risk factors of noise-induced hearing loss among liquefied petroleum gas (LPG) cylinder infusion workers in Taiwan. Ind. Health. 2009;47:603–610. doi: 10.2486/indhealth.47.603. [DOI] [PubMed] [Google Scholar]
- Chang T.Y., Jain R.M., Wang C.S., Chan C.C. Effects of occupational noise exposure on blood pressure. J. Occup. Environ. Med. 2003;45:1289–1296. doi: 10.1097/01.jom.0000100003.59731.3d. [DOI] [PubMed] [Google Scholar]
- Chang T.Y., Liu C.S., Young L.H., Wang V.S., Jian S.E., Bao B.Y. Noise frequency components and the prevalence of hypertension in workers. Sci. Total Environ. 2012;416:89–96. doi: 10.1016/j.scitotenv.2011.11.071. [DOI] [PubMed] [Google Scholar]
- Chen S., Ni Y., Zhang L., Kong L., Lu L., Yang Z., Yang L., Zhang X., Zhu Y. Noise exposure in occupational setting associated with elevated blood pressure in China. BMC Public Health. 2017;17:107. doi: 10.1186/s12889-017-4050-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark C., Paunovic K. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and cognition. Int. J. Environ. Res. Public Health. 2018 doi: 10.3390/ijerph15020285. 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark C., Paunovic K. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and quality of life, wellbeing and mental health. Int. J. Environ. Res. Public Health. 2018;15 doi: 10.3390/ijerph15112400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Concha-Barrientos M., Campbell-Lendrum D.H., Steenland K. World Health Organization; Geneva: 2004. Occupational noise: assessing the environmental burden of disease from work-related impairment at national and local levels ed^eds. [Google Scholar]
- Covidence systematic review software, V.H.I., Melbourne, Australia. Available at www.covidence.org.
- de Souza T.C., Perisse A.R., Moura M. Noise exposure and hypertension: investigation of a silent relationship. BMC Public Health. 2015;15:328. doi: 10.1186/s12889-015-1671-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeks, J., Higgins, J., Altman, D., 2011. Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins, J., Green, S., eds. Cochrane Handbook for Systematic Reviews of Interventions Version 510 [updated March 2011] The Cochrane Collaboration.
- Descatha A., Sembajwe G., Baer M., Boccuni F., Di Tecco C., Duret C., Evanoff B.A., Gagliardi D., Ivanov I.D., Leppink N., Marinaccio A., Magnusson Hanson L.L., Ozguler A., Pega F., Pell J., Pico F., Prüss-Üstün A., Ronchetti M., Roquelaure Y., Sabbath E., Stevens G.A., Tsutsumi A., Ujita Y., Iavicoli S. WHO/ILO work-related burden of disease and injury: Protocol for systematic reviews of exposure to long working hours and of the effect of exposure to long working hours on stroke. Environ. Int. 2018;119:366–378. doi: 10.1016/j.envint.2018.06.016. [DOI] [PubMed] [Google Scholar]
- Descatha A., Sembajwe G., Pega F., Ujita Y., Baer M., Boccuni F., Di Tecco C., Duret C., Evanoff B.A., Gagliardi D., Godderis L., Kang S.-K., Kim B.J., Li J., Hanson L.M., Marinaccio A., Ozguler A., Pachito D., Pell J., Pico F., Ronchetti M., Roquelaure Y., Rugulies R., Schouteden M., Siegrist J., Tsutsumi A., Iavicoli S. The effect of exposure to long working hours on stroke: a systematic review and meta-analysis from the WHO/ILO Work-Related Burden of Disease and Injury. Environ. Int. 2020;142:105746. doi: 10.1016/j.envint.2020.105746. [DOI] [PubMed] [Google Scholar]
- Drazen J.M., de Leeuw P.W., Laine C., Mulrow C., DeAngelis C.D., Frizelle F.A., Godlee F., Haug C., Hebert P.C., James A., Kotzin S., Marusic A., Reyes H., Rosenberg J., Sahni P., Van der Weyden M.B., Zhaori G. Toward more uniform conflict disclosures: the updated ICMJE conflict of interest reporting form. JAMA. 2010;304:212–213. doi: 10.1001/jama.2010.918. [DOI] [PubMed] [Google Scholar]
- Drazen J.M., Van der Weyden M.B., Sahni P., Rosenberg J., Marusic A., Laine C., Kotzin S., Horton R., Hebert P.C., Haug C., Godlee F., Frizelle F.A., de Leeuw P.W., DeAngelis C.D. Uniform format for disclosure of competing interests in ICMJE journals. JAMA. 2010;303:75–76. doi: 10.1001/jama.2009.1542. [DOI] [PubMed] [Google Scholar]
- Du H., Liu L., Zhang B., Ma H., Song L. Investigation on the effect of noise hazards on health of workers in textile industry in Fuxin. J. Occup. Health Damage. 2007;22:39–41. [Google Scholar]
- Dzhambov Angel, Dimitrova Donka. Occupational noise exposure and the risk for work-related injury: a systematic review and meta-analysis. Ann. Work Expo. Health. 2017;61(9):1037–1053. doi: 10.1093/annweh/wxx078. [DOI] [PubMed] [Google Scholar]
- Dzhambov A.M., Dimitrova D.D., Dimitrakova E.D. Noise exposure during pregnancy, birth outcomes and fetal development: meta-analyses using quality effects model. Folia Med. (Plovdiv) 2014;56:204–214. doi: 10.2478/folmed-2014-0030. [DOI] [PubMed] [Google Scholar]
- Dzhambov, A.M., Lercher, P., 2019. Road traffic noise exposure and birth outcomes: an updated systematic review and meta-analysis. Int. J. Environ. Res. Public Health 16. [DOI] [PMC free article] [PubMed]
- Ezzati M., Lopez A.D., Rodgers A., Murray C.J.L. WHO; Geneva, Switzerland: 2004. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors ed^eds. [Google Scholar]
- Forsyth S.R., Odierna D.H., Krauth D., Bero L.A. Conflicts of interest and critiques of the use of systematic reviews in policymaking: an analysis of opinion articles. Syst. Rev. 2014;3:122. doi: 10.1186/2046-4053-3-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godderis L., Bakusic J., Boonen E., Delvaux E., Ivanov I.D., Lambrechts M.-C., Latorraca C.O., Leppink N., Martimbianco A.L., Pega F., Prüss-Üstün A.M., Riera R., Ujita Y., Pachito D.V. WHO/ILO work-related burden of disease and injury: Protocol for systematic reviews of exposure to long working hours and of the effect of exposure to long working hours on alcohol use and alcohol use disorder. Environ. Int. 2018;120:22–33. doi: 10.1016/j.envint.2018.07.025. [DOI] [PubMed] [Google Scholar]
- Guo Y., Han S., Xu Y. Investigation on the relationship between hearing loss and length of service and cumulative noise exposure of noise-exposed workers in a textile mill. China Modern Med. 2012;19:150–154. [Google Scholar]
- Guski, R., Schreckenberg, D., Schuemer, R., 2017. WHO environmental noise guidelines for the european region: a systematic review on environmental noise and annoyance. Int. J. Environ. Res. Public Health 14. [DOI] [PMC free article] [PubMed]
- He J., Zhao W., Wang S. Investigation on hearing loss of noise workers in a large chemical plant. Occup. Health Emergency Rescue. 2017;35:44–45. [Google Scholar]
- Higgins J., Thomas J., Chandler J., Cumpston M., Li T., Page M., Welch V., editors. Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. John Wiley & Sons; Chichester, UK: 2019. [Google Scholar]
- Hong O.S., Chen S.P., Conrad K.M. Noise induced hearing loss among male airport workers in Korea. Aaohn J. 1998;46:67–75. [PubMed] [Google Scholar]
- Hu J., He J., Lin B., Ceng Y. Investigation and analysis of hearing loss of noise workers in steel tube mills. Chin. J. Metall. Ind. Med. 2005;22:614–615. [Google Scholar]
- Hughes H., Hunting K.L. Evaluation of the effects of exposure to organic solvents and hazardous noise among US Air Force Reserve personnel. Noise Health. 2013;15:379–387. doi: 10.4103/1463-1741.121224. [DOI] [PubMed] [Google Scholar]
- Hulshof C.T.J., Colosio C., Daams J.G., Ivanov I.D., Prakash K.C., Kuijer P., Leppink N., Mandic-Rajcevic S., Masci F., van der Molen H.F., Neupane S., Nygard C.H., Oakman J., Pega F., Proper K., Pruss-Ustun A.M., Ujita Y., Frings-Dresen M.H.W. WHO/ILO work-related burden of disease and injury: Protocol for systematic reviews of exposure to occupational ergonomic risk factors and of the effect of exposure to occupational ergonomic risk factors on osteoarthritis of hip or knee and selected other musculoskeletal diseases. Environ. Int. 2019;125:554–566. doi: 10.1016/j.envint.2018.09.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulshof C.T.J., Pega F., Neupane S., Colosio C., Daams J.G., Kc P., Kuijer P.P.F.M., Mandic-Rajcevic S., Masci F., van der Molen H.F., Nygård C-H., Oakman J., Proper K.I., Frings-Dresen M.H.W. The effect of occupational exposure to ergonomic risk factors on osteoarthritis of hip or knee and selected other musculoskeletal diseases: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021 doi: 10.1016/j.envint.2020.106349. [DOI] [PubMed] [Google Scholar]
- Hulshof C.T.J., Pega F., Neupane S., van der Molen H.F., Colosio C., Daams J.G., Descatha A., Kc P., Kuijer P.P.F.M., Mandic-Rajcevic S., Masci F., Morgan R.L., Nygård C-H., Oakman J., Proper K.I., Solovieva S., Frings-Dresen M.H.W. The prevalence of occupational exposure to ergonomic risk factors: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021;146(106157) doi: 10.1016/j.envint.2020.106157. [DOI] [PubMed] [Google Scholar]
- Inoue M., Laskar M.S., Harada N. Cross-sectional study on occupational noise and hypertension in the workplace. Arch. Environ. Occup. Health. 2005;60:106–110. doi: 10.3200/AEOH.60.2.106-110. [DOI] [PubMed] [Google Scholar]
- International Labour Organization . ILO; Geneva: 1999. ILO estimates over 1 million work-related fatalities each year ed^eds. [Google Scholar]
- International Labour Organization . International Labour Organization; Geneva: 2014. Safety and health at work : a vision for sustainable prevention: XX World Congress on Safety and Health at Work 2014: Global Forum for Prevention, 24–27 August 2014, Frankfurt, Germany. [Google Scholar]
- Ivanovich E., Kolarova D., Enev S., Tzenova B., Topalova M. Noise evaluation and estimation of some specific and non-specific health indicators in telephone operators. Rev. Environ. Health. 1994;10:39–46. doi: 10.1515/reveh.1994.10.1.39. [DOI] [PubMed] [Google Scholar]
- Johnson A.C., Morata T.C., Lindblad A.C., Nylen P.R., Svensson E.B., Krieg E., Aksentijevic A., Prasher D. Audiological findings in workers exposed to styrene alone or in concert with noise. Noise Health. 2006;8:45–57. doi: 10.4103/1463-1741.32467. [DOI] [PubMed] [Google Scholar]
- Kerns E., Masterson E.A., Themann C.L., Calvert G.M. Cardiovascular conditions, hearing difficulty, and occupational noise exposure within US industries and occupations. Am. J. Ind. Med. 2018;61:477–491. doi: 10.1002/ajim.22833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kock S., Andersen T., Kolstad H.A., Kofoed-Nielsen B., Wiesler F., Bonde J.P. Surveillance of noise exposure in the Danish workplace: a baseline survey. Occup. Environ. Med. 2004;61:838–843. doi: 10.1136/oem.2004.012757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacevic M., Belojevic G. Tooth abrasion in workers exposed to noise in the Montenegrin textile industry. Ind. Health. 2006;44:481–485. doi: 10.2486/indhealth.44.481. [DOI] [PubMed] [Google Scholar]
- Lam, J., Sutton, P., Halladay, A., Davidson, L.I., Lawler, C., Newschaffer, C.J., Kalkbrenner, A., Health, J.J.Z.S.o.P., Windham, G.C., Daniels, N., Sen, S., Woodruff, T.J., 2016. Applying the navigation guide systematic review methodology case study #4: association between developmental exposures to ambient air pollution and autism. PLoS One 21.
- Landen D., Wilkins S., Stephenson M., McWilliams L. Noise exposure and hearing loss among sand and gravel miners. J. Occup. Environ. Hyg. 2004;1:532–541. doi: 10.1080/15459620490476503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.H., Kang W., Yaang S.R., Choy N., Lee C.R. Cohort study for the effect of chronic noise exposure on blood pressure among male workers in Busan, Korea. Am. J. Ind. Med. 2009;52:509–517. doi: 10.1002/ajim.20692. [DOI] [PubMed] [Google Scholar]
- Lee L.T. A study of the noise hazard to employees in local discotheques. Singapore Med. J. 1999;40:571–574. [PubMed] [Google Scholar]
- Li J., Brisson C., Clays E., Ferrario M.M., Ivanov I.D., Landsbergis P., Leppink N., Pega F., Pikhart H., Prüss-Üstün A.M., Rugulies R., Schnall P.L., Stevens G.A., Tsutsumi A., Ujita Y., Siegrist J. WHO/ILO work-related burden of disease and injury: Protocol for systematic reviews of exposure to long working hours and of the effect of exposure to long working hours on ischaemic heart disease. Environ. Int. 2018;119:558–569. doi: 10.1016/j.envint.2018.06.022. [DOI] [PubMed] [Google Scholar]
- Li J., Pega F., Ujita Y., Brisson C., Clays E., Descatha A., Ferrario M.M., Godderis L., Iavicoli S., Landsbergis P.A., Metzendorf M.I., Morgan R.L., Pachito D.V., Pikhart H., Richter B., Roncaioli M., Rugulies R., Schnall P.L., Sembajwe G., Trudel X., Tsutsumi A., Woodruff T.J., Siegrist J. The effect of exposure to long working hours on ischaemic heart disease: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2020;142 doi: 10.1016/j.envint.2020.105739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gotzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y.W., Wang H.J., Weng S.F., Su W.J., Wang X., Guo Y.F., Yu D., Du L.L., Zhou T., Chen W.H., Shi T.M. Occupational hearing loss among Chinese municipal solid waste landfill workers: a cross-sectional study. PLoS ONE. 2015;10:10. doi: 10.1371/journal.pone.0128719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lv S., Shao L., Wang J., Yang Y., Huang Y., Zhu W., Zhao Y. Dose-response relationship between noise exposure and prevalence of hearing loss in male aircraft maintenance workers. Chin. J. Ind. Med. 2003;16:277–279. [Google Scholar]
- Macca I., Scapellato M.L., Carrieri M., Maso S., Trevisan A., Bartolucci G.B. High-frequency hearing thresholds: effects of age, occupational ultrasound and noise exposure. Int. Arch. Occup. Environ. Health. 2015;88:197–211. doi: 10.1007/s00420-014-0951-8. [DOI] [PubMed] [Google Scholar]
- Mandrioli D., Schlunssen V., Adam B., Cohen R.A., Colosio C., Chen W., Fischer A., Godderis L., Goen T., Ivanov I.D., Leppink N., Mandic-Rajcevic S., Masci F., Nemery B., Pega F., Pruss-Ustun A., Sgargi D., Ujita Y., van der Mierden S., Zungu M., Scheepers P.T.J. WHO/ILO work-related burden of disease and injury: Protocol for systematic reviews of occupational exposure to dusts and/or fibres and of the effect of occupational exposure to dusts and/or fibres on pneumoconiosis. Environ. Int. 2018;119:174–185. doi: 10.1016/j.envint.2018.06.005. [DOI] [PubMed] [Google Scholar]
- Melamed S., Froom P., Kristal-Boneh E., Gofer D., Ribak J. Industrial noise exposure, noise annoyance, and serum lipid levels in blue-collar workers–the CORDIS Study. Arch. Environ. Health. 1997;52:292–298. doi: 10.1080/00039899709602201. [DOI] [PubMed] [Google Scholar]
- Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P., Stewart, L.A., 2015. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. System. Rev. 4. [DOI] [PMC free article] [PubMed]
- Morata T.C., Engel T., Durao A., Costa T.R., Krieg E.F., Dunn D.E., Lozano M.A. Hearing loss from combined exposures among petroleum refinery workers. Scand. Audiol. 1997;26:141–149. doi: 10.3109/01050399709074987. [DOI] [PubMed] [Google Scholar]
- Morata T.C., Fiorini A.C., Fischer F.M., Colacioppo S., Wallingford K.M., Krieg E.F., Dunn D.E., Gozzoli L., Padrao M.A., Cesar C.L. Toluene-induced hearing loss among rotogravure printing workers. Scand. J. Work Environ. Health. 1997;23:289–298. doi: 10.5271/sjweh.222. [DOI] [PubMed] [Google Scholar]
- Murray C.J.L., Ezzati M., Lopez A.D., Rodgers A., Vander Hoorn S. Comparative quantification of health risks: conceptual framework and methodological issues. In: Ezzati M., Lopez A.D., Rodgers A., Murray C.J.L., editors. Comparative Quantification of Health Risks: Global and Regional Burdedn of Disease Attributable to Selected Major Risk Factors. World Health Organization; Geneva: 2004. [Google Scholar]
- Nasir H.M., Rampal K.G. Hearing loss and contributing factors among airport workers in Malaysia. Med. J. Malaysia. 2012;67:81–86. [PubMed] [Google Scholar]
- Nieuwenhuijsen, M.J., Ristovska, G., Dadvand, P., 2017. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and adverse birth outcomes. Int. J. Environ. Res. Public Health 14. [DOI] [PMC free article] [PubMed]
- Noweir M.H. Noise exposure as related to productivity, disciplinary actions, absenteeism, and accidents among textile workers. J. Saf. Res. 1984;15:163–174. [Google Scholar]
- Osibogun A., Igweze I.A., Adeniran L.O. Noise-induced hearing loss among textile workers in Lagos metropolis. Niger Postgrad Med. J. 2000;7:104–111. [PubMed] [Google Scholar]
- Pachito D.V., Pega F., Bakusic J., Boonen E., Clays E., Descatha A., Delvaux E., De Bacquer D., Koskenvuo K., Kroger H., Lambrechts M.C., Latorraca C.O.C., Li J., Cabrera Martimbianco A.L., Riera R., Rugulies R., Sembajwe G., Siegrist J., Sillanmaki L., Sumanen M., Suominen S., Ujita Y., Vandersmissen G., Godderis L. The effect of exposure to long working hours on alcohol consumption, risky drinking and alcohol use disorder: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related burden of disease and injury. Environ. Int. 2020;146:106205. doi: 10.1016/j.envint.2020.106205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parent-Thirion, A., Biletta, I., Cabrita, J., Vargas Llave, O., Vermeylen, G., Wilczyńska, A., Wilkens, M., 2019. Sixth European Working Conditions Survey: Overview report. Updated 29 October 2019. ed^eds. Dublin: Eurofound.
- Paulo M.S., Adam B., Akagwu C., Akparibo I., Al-Rifai R.H., Bazrafshan S., Gobba F., Green A.C., Ivanov I., Kezic S., Leppink N., Loney T., Modenese A., Pega F., Peters C.E., Pruss-Ustun A.M., Tenkate T., Ujita Y., Wittlich M., John S.M. WHO/ILO work-related burden of disease and injury: Protocol for systematic reviews of occupational exposure to solar ultraviolet radiation and of the effect of occupational exposure to solar ultraviolet radiation on melanoma and non-melanoma skin cancer. Environ. Int. 2019;126:804–815. doi: 10.1016/j.envint.2018.09.039. [DOI] [PubMed] [Google Scholar]
- Pawlaczyk-Luszczynska M., Dudarewicz A., Czaja N., Bortkiewicz A. Do hearing threshold levels in workers of the furniture industry reflect their exposure to noise? Med. Pr. 2016;67:337–351. doi: 10.13075/mp.5893.00337. [DOI] [PubMed] [Google Scholar]
- Pega F., Chartres N., Guha N., Modenese A., Morgan R.L., Martinez-Silveira M.S., Loomis D. The effect of occupational exposure to welding fumes on trachea, bronchus and lung cancer: A protocol for a systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2020;145 doi: 10.1016/j.envint.2020.106089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pega, F., Liu, S.Y., Walter, S., Lhachimi, S.K., 2015. Unconditional cash transfers for assistance in humanitarian disasters: effect on use of health services and health outcomes in low- and middle-income countries. Cochrane Database Syst. Rev. 9, CD011247. [DOI] [PMC free article] [PubMed]
- Pega, F., Liu, S.Y., Walter, S., Pabayo, R., Saith, R., Lhachimi, S.K., 2017. Unconditional cash transfers for reducing poverty and vulnerabilities: effect on use of health services and health outcomes in low- and middle-income countries. Cochrane Database Syst. Rev. 11, CD011135. [DOI] [PMC free article] [PubMed]
- Pega, F., Norris, S.L., Backes, C., Bero, L.A., Descatha, A., Gagliardi, D., Godderis, L., Loney, T., Modenese, A., Morgan, R.L., Pachito, D., Paulo, M.B.S., Scheepers, P.T.J., Schlünssen, V., Sgargi, D., Silbergeld, E.K., Sørensen, K., Sutton, P., Tenkate, T., Torreão Corrêa da Silva, D., Ujita, Y., van Deventer, E., Woodruff, T.J., Mandrioli, D., 2020b. RoB-SPEO: A tool for assessing risk of bias in studies estimating the prevalence of exposure to occupational risk factors from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 135, 105039. [DOI] [PMC free article] [PubMed]
- Porta, M., 2014. A Dictionary of Epidemiology.6 ed^eds. New York: Oxford University Press.
- Pega, F., Gagliardi, D., Bero, L.A., Boccuni, F., Chartres, N., Descatha, A., Godderis, L., Loney, T., Mandrioli, D., Modenese, A., Morgan, R.L., Pachito, D., Paulo, M.S., Scheepers, P.T.J, Tenkate, T., Norris, S.L., submitted for publication. QoE-SPEO: An approach for assessing the quality of evidence in studies estimating prevalence of exposure to occupational risk factors from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int.. [DOI] [PMC free article] [PubMed]
- Pruss-Ustun A., Wolf J., Corvalan C., Bos R., Neira M. World Health Organization; Geneva: 2017. Preventing disease through healthy environments: a global assessment of the burden of disease from enviornmental risks. [Google Scholar]
- Rabinowitz P.M., Galusha D., Dixon-Ernst C., Slade M.D., Cullen M.R. Do ambient noise exposure levels predict hearing loss in a modern industrial cohort? Occup. Environ. Med. 2007;64:53–59. doi: 10.1136/oem.2005.025924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachiotis G., Alexopoulos C., Drivas S. Occupational exposure to noise, and hearing function among electro production workers. Auris Nasus Larynx. 2006;33:381–385. doi: 10.1016/j.anl.2006.03.008. [DOI] [PubMed] [Google Scholar]
- Rugulies R., Ando E., Ayuso-Mateos J.L., Bonafede M., Cabello M., Di Tecco C., Dragano N., Durand-Moreau Q., Eguchi H., Gao J., Garde A.H., Iavicoli S., Ivanov I.D., Leppink N., Madsen I.E.H., Pega F., Pruss-Ustun A.M., Rondinone B.M., Sorensen K., Tsuno K., Ujita Y., Zadow A. WHO/ILO work-related burden of disease and injury: Protocol for systematic reviews of exposure to long working hours and of the effect of exposure to long working hours on depression. Environ. Int. 2019;125:515–528. doi: 10.1016/j.envint.2018.11.011. [DOI] [PubMed] [Google Scholar]
- Ryder, G., 2017. Welcome address from the Director General of the International Labour Organization. XXI World Congress on Safety and Health at Work. Sands Expo and Convention Centre, Singapore.
- Sancini A., Caciari T., Rosati M.V., Samperi I., Iannattone G., Massimi R., Loreti B., Scala B., Sacco C., Tomei F., Tomei G. Can noise cause high blood pressure? Occupational risk in paper industry. Clin. Ter. 2014;165:e304–e311. [PubMed] [Google Scholar]
- Seixas N.S., Ren K., Neitzel R., Camp J., Yost M. Noise exposure among construction electricians. Aihaj. 2001;62:615–621. doi: 10.1080/15298660108984661. [DOI] [PubMed] [Google Scholar]
- Shakhatreh F.M., Abdul-Baqi K.J., Turk M.M. Hearing loss in a textile factory. Saudi Med. J. 2000;21:58–60. [PubMed] [Google Scholar]
- Shamseer L., Moher D., Clarke M., Ghersi D., Liberati A., Petticrew M., Shekelle P., Stewart L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350 doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- Shi Y.I. Investigation on the influence of production noise on electrocardiogram of male workers in oil production plants. Ind Hlth Occup Dis. 2009;35:293–295. [Google Scholar]
- Singh L.P., Bhardwaj A., Deepak K.K. Prevalence of permanent hearing threshold shift among workers of Indian iron and steel small and medium enterprises: A study. Noise & Health. 2012;14:119–128. doi: 10.4103/1463-1741.97256. [DOI] [PubMed] [Google Scholar]
- Sliwinska-Kowalska M., Zamyslowska-Szmytke E., Szymczak W., Kotylo P., Fiszer M., Wesolowski W., Pawlaczyk-Luszczynska M., Bak M., Gajda-Szadkowska A. Effects of coexposure to noise and mixture of organic solvents on hearing in dockyard workers. J. Occup. Environ. Med. 2004;46:30–38. doi: 10.1097/01.jom.0000105912.29242.5b. [DOI] [PubMed] [Google Scholar]
- Solecki L. Relationship between the level of total exposure to noise among private farmers and the degree of hearing loss. Med. Pr. 2008;59:149–158. [PubMed] [Google Scholar]
- Souza, N.S.S., Carvalho, F.M., de Cassia Pereira Fernandes, R., 2001. [Arterial hypertension among oil-drilling workers exposed to noise]. Cad Saude Publica 17, 1481–1488. [PubMed]
- Sriopas A., Chapman R.S., Sutammasa S., Siriwong W. Occupational noise-induced hearing loss in auto part factory workers in welding units in Thailand. J. Occup. Health. 2017;59:55–62. doi: 10.1539/joh.15-0291-OA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starck J., Toppila E., Pyykko I. Smoking as a risk factor in sensory neural hearing loss among workers exposed to occupational noise. Acta Otolaryngol. 1999;119:302–305. doi: 10.1080/00016489950181288. [DOI] [PubMed] [Google Scholar]
- Stevens, G.A., Alkema, L., Black, R.E., Boerma, J.T., Collins, G.S., Ezzati, M., Grove, J.T., Hogan, D.R., Hogan, M.C., Horton, R., Lawn, J.E., Marušić, A., Mathers, C.D., Murray, C.J.L., Rudan, I., Salomon, J.A., Simpson, P.J., Vos, T., Welch, V., Group), T.G.W., 2016. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet (London, England) 388, e19–e23. [DOI] [PubMed]
- Stokholm Z.A., Bonde J.P., Christensen K.L., Hansen A.M., Kolstad H.A. Occupational noise exposure and the risk of hypertension. Epidemiology. 2013;24:135–142. doi: 10.1097/EDE.0b013e31826b7f76. [DOI] [PubMed] [Google Scholar]
- Strauss S., Swanepoel D.W., Becker P., Eloff Z., Hall J.W., 3rd. Noise and age-related hearing loss: a study of 40 123 gold miners in South Africa. Int. J. Audiol. 2014;53(Suppl 2):S66–S75. doi: 10.3109/14992027.2013.865846. [DOI] [PubMed] [Google Scholar]
- Talbott E.O., Gibson L.B., Burks A., Engberg R., McHugh K.P. Evidence for a dose-response relationship between occupational noise and blood pressure. Arch. Environ. Health. 1999;54:71–78. doi: 10.1080/00039899909602239. [DOI] [PubMed] [Google Scholar]
- Teixeira, L.R., Azevedo, T.M., Bortkiewicz, A., Correa da Silva, D.T., de Abreu, W., de Almeida, M.S., de Araujo, M.A.N., Gadzicka, E., Ivanov, I.D., Leppink, N., Macedo, M.R.V., de, S.M.E.M.G., Pawlaczyk-Luszczynska, M., Pega, F., Pruss-Ustun, A.M., Siedlecka, J., Stevens, G.A., Ujita, Y., Braga, J.U., 2019. WHO/ILO work-related burden of disease and injury: protocol for systematic reviews of exposure to occupational noise and of the effect of exposure to occupational noise on cardiovascular disease. Environ. Int. 125, 567–578. [DOI] [PubMed]
- Teixeira L., Pega F., Dzhambov A., Bortkiewicz A., Correa da Silva D.T., de Andrade C.A.F., Gadzicka E., Hadkhale K., Iavicoli S., Martinez-Silveira M.S., Pawlaczyk-Łuszczyńska M., Rondinone B.M., Siedlecka J., Valenti A., Gagliardi D. The effect of occupational exposure to noise on ischaemic heart disease, stroke and hypertension: a systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021 doi: 10.1016/j.envint.2021.106387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenkate T., Adam B., Al-Rifai R.H., Chou B.R., Gobba F., Ivanov I.D., Leppink N., Loney T., Pega F., Peters C.E., Pruss-Ustun A.M., Silva Paulo M., Ujita Y., Wittlich M., Modenese A. WHO/ILO work-related burden of disease and injury: Protocol for systematic reviews of occupational exposure to solar ultraviolet radiation and of the effect of occupational exposure to solar ultraviolet radiation on cataract. Environ. Int. 2019;125:542–553. doi: 10.1016/j.envint.2018.10.001. [DOI] [PubMed] [Google Scholar]
- Themann C.L., Masterson E.A. Occupational noise exposure: A review of its effects, epidemiology, and impact with recommendations for reducing its burden. J. Acoust. Soc. Am. 2019;146:3879. doi: 10.1121/1.5134465. [DOI] [PubMed] [Google Scholar]
- Tomprette, N., Chatillon, J., Chevret, J., 2019. Dossier Bruit au travail : De l’évaluation à la prévention des risques Savoir & Actualités Hygiène et sécurité du travail 254.
- Toppila E., Pyykko I., Starck J. Age and noise-induced hearing loss. Scand. Audiol. 2001;30:236–244. doi: 10.1080/01050390152704751. [DOI] [PubMed] [Google Scholar]
- United States Department of Labor, 2013. Occupational Safety and Health Administration: Technical Manual. Section III: Chapter 5.
- van Kempen E., Casas M., Pershagen G., Foraster M. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int. J. Environ. Res. Public Health. 2018;15:379. doi: 10.3390/ijerph15020379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vihma T. Health hazards and stress factors in small industry: Prevalence study in the Province of Uusimaa, Finland, with special reference to the type of industry and the occupational title as classifications for the description of occupational health problems. Scand. J. Work Environ. Health. 1981;7:9–149. [PubMed] [Google Scholar]
- Virkkunen H., Kauppinen T., Tenkanen L. Long-term effect of occupational noise on the risk of coronary heart disease. Scand. J. Work Environ. Health. 2005;31:291–299. doi: 10.5271/sjweh.885. [DOI] [PubMed] [Google Scholar]
- Whittaker J.D., Robinson T., Acharya A., Singh D., Smith M. Noise-induced hearing loss in small-scale metal industry in Nepal. J. Laryngol. Otol. 2014;128:871–880. doi: 10.1017/S0022215114001728. [DOI] [PubMed] [Google Scholar]
- Woodruff T.J., Sutton P. The Navigation Guide Systematic Review Methodology: A Rigorous and Transparent Method for Translating Environmental Health Science into Better Health Outcomes. Environ. Health Perspect. 2014;122:1007–1014. doi: 10.1289/ehp.1307175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . WHO; Copenhagen: 2018. Environmental noise guidelines for the European region ed^eds. [Google Scholar]
- World Health Organization . WHO; Geneva: 2019. Disease burden and mortality estimates: disease burden, 2000–2016 ed^eds. [Google Scholar]
- Wu T.N., Ko Y.C., Chang P.Y. Study of noise exposure and high blood pressure in shipyard workers. Am. J. Ind. Med. 1987;12:431–438. doi: 10.1002/ajim.4700120408. [DOI] [PubMed] [Google Scholar]
- Xiao Q., Xiao C., Du W. Effect of occupational noise exposure on the cardiovascular system. Occup. Health Saf. 2008;24:11–12. [Google Scholar]
- Xie H.W., Tang S.-C., Zhou L.-F., Quan C.-J., Zhang M.-B. Relationship between Cumulative Noise Exposure and Human Hearing Loss Caused by Non-stationary Noise. J. Environ. Occup. Med. 2015;32:56–60. [Google Scholar]
- Xue C.H., Tao Z.M., Su Y.W., Li E.B., Zhou M., Bao M.Y., Liu Y.M. Analysis on hearing status and related influencing factors in workers exposed to noise in an automobile manufacture enterprise. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2018;36:204–207. doi: 10.3760/cma.j.issn.1001-9391.2018.03.011. [DOI] [PubMed] [Google Scholar]
- Yu S.F., Chen G.S., Jiao J., Gu G.Z., Zhang H.L., Wang X.M., Zhou W.H., Wu H., Li Y.H., Zheng Y.X. A cohort study on occupational noise induced hearing loss in workers at an iron and steel plant. Zhonghua Yu Fang Yi Xue Za Zhi. 2017;51:13–19. doi: 10.3760/cma.j.issn.0253-9624.2017.01.005. [DOI] [PubMed] [Google Scholar]
- Yuan J., Yang M., Yao H., Zheng J., Yang Q., Chen S., Wei Q., Tanguay R.M., Wu T. Plasma antibodies to heat shock protein 60 and heat shock protein 70 are associated with increased risk of electrocardiograph abnormalities in automobile workers exposed to noise. Cell Stress Chaperones. 2005;10:126–135. doi: 10.1379/CSC-95R.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y., Zhang S., Selvin S., Spear R.C. A dose response relation for noise induced hypertension. Br. J. Ind. Med. 1991;48:179–184. doi: 10.1136/oem.48.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.