Abstract
The Geriatric Emergency Care Applied Research (GEAR) Network (1) conducted a scoping review of the current literature on the identification of and interventions to address elder abuse among patients receiving care in emergency departments and (2) used this review to prioritize research questions for knowledge development. Two questions guided the scoping review: What is the effect of universal emergency department screening compared to targeted screening or usual practice on cases of elder abuse identified, safety outcomes, and health care utilization?; and What is the safety, health, legal, and psychosocial impact of emergency department-based interventions vs. usual care for patients experiencing elder abuse?
We searched five article databases. Additional material was located through reference lists of identified publications, PsychInfo, and Google Scholar. The results were discussed in a consensus conference; and stakeholders voted to prioritize research questions.
No studies were identified that directly addressed the first question regarding assessment strategies; but 4 instruments used for elder abuse screening in the emergency department were identified. For the second question, we located 6 articles on interventions for elder abuse in the emergency department; however, none directly addressed the question of comparative effectiveness. Based on these findings, GEAR participants identified 5 questions as priorities for future research - 2 related to screening, 2 related to intervention, and 1 encompassed both.
In sum, research to identify best practices for elder abuse assessment and intervention in emergency departments is still needed. Although there are practical and ethical challenges, rigorous experimental studies are needed.
Keywords: emergency department, elder abuse, screening, intervention, review
Introduction
The Centers for Disease Control and Prevention define elder abuse as “an intentional act, or failure to act, by a caregiver or another person in a relationship involving an expectation of trust that causes or creates a risk of harm to an older adult (person over the age of 60)” (Centers for Disease Control, 2016). This abuse can be physical, emotional, sexual, financial, or neglectful (National Institute on Aging, 2016). Estimates of prevalence of elder abuse range between 5 and 10 percent in the United States (Acierno et al., 2010; Burnes et al., 2017) and as high as 16 percent globally (Yon et al., 2017). In the US, nearly every state has some form of mandatory reporting, enacted by statute, which is intended to protect older adults (Stiegel, 2017).
Emergency departments offer a unique clinical setting that may position them to be ideal for screening and initiating interventions for elder abuse. Adults aged 65 years and older have rates of emergency department use higher than any other age group (Dufour et al., 2019). Older adults who are victims of abuse often have limited social support (Dong, 2015; Wong & Waite, 2017), and have few interactions with people able to recognize abuse, intervene, and report when the older adult is in an unsafe environment. For many older adults, a visit to the emergency department may represent the only contact with anyone other than caregivers. Additionally, given the extended amount of time that older adults spend in the emergency department during a typical visit (Biber et al., 2013) and, in larger hospitals, the availability of consult services or ancillary professionals like social workers, emergency departments are strongly positioned to screen and intervene. Elder abuse has major health consequences, with one study finding that both elder mistreatment and self-neglect were associated with a significantly increased chance of mortality at a 9 year follow-up (Lachs et al., 1998). Despite the profound negative physical, psychological, and social impacts of elder abuse (Yunus et al., 2019), recognizing elder abuse remains uncommon in emergency departments. Both in coordination and independent of emergency department staff, Emergency Medical Services (EMS) play an important role in the identification and screening of elder abuse. They may have more regular contact with the patient than emergency department providers (Evans, Platts-Mills, et al., 2017) as well as information about the home environment not available to providers. Many EMS providers have little training regarding recognition of elder abuse (Namboodri et al., 2018), so important and clinically relevant information may not be communicated to emergency department providers.
A recent US based retrospective cross-sectional analysis found that elder abuse is formally diagnosed in roughly 0.013% of U.S. emergency department visits for those 60 years and older which is more than 10 times lower than rates of diagnosis of child abuse or domestic violence (Evans, Hunold, et al., 2017). Therefore, a significant opportunity exists to improve care. Previous research agendas, such as a 2008 review and update to The American Geriatric Society’s project New Frontiers in Geriatrics Research (Carpenter & Gerson, 2008), have recognized the importance of research into elder abuse in the emergency department setting but have not provided specific details related to content areas or considerations for undertaking investigations. The present work is intended to both extend and add specificity to previously identified needs in research on this important subject.
The Geriatric Emergency Care Applied Research (GEAR) Network is a foundation and federally funded program (The John A. Hartford Foundation, Gary and Mary West Health Institute, and National Institute on Aging R21AG058926) that used an approach modeled off of the Cornell Institute for Translational Research on Aging (CITRA) model (Sabir et al., 2006) to identify and address high impact research questions for areas with clinically important knowledge gaps. The CITRA model was designed to facilitate dialogue between researchers and practitioners in an effort to align research agendas with the real-world concerns of practitioners. We applied, to elder abuse, the GEAR paradigm of: framing and assessing Patient Intervention Control Outcome (PICO) questions, systematic literature review, and building interdisciplinary stakeholder consensus on best practices and areas of future research. Our primary objective was to examine evidence-based best practices for elder abuse in emergency the emergency care setting and the current state of research on screening and intervention work using a scoping review of the published literature. Our secondary objective was to prioritize high-yield elder abuse research questions for the emergency department setting.
Methods
Study design
GEAR participants from several disciplines were identified by their experience and involvement in geriatric emergency medicine interest groups within Society for Academic Emergency Medicine, American College of Emergency Physicians, American Geriatrics Society, and The Gerontological Society of America. Additional GEAR participants were identified based on their prior publications and content expertise. Funders pre-identified 5 high-impact topics, which became GEAR cores: Cognitive Impairment, Medication Safety, Falls, Elder Abuse, and Care Transitions. Clinicians and researchers joined one or more of these GEAR cores in October 2018. The GEAR Elder Abuse core, which was 9 of the overall 49 members of GEAR, was composed of 3 emergency physicians (TER, TPM, TR) 3 social workers (JK, NMH, SS), an epidemiologist (SC), a geriatric nurse practitioner (KHR), and a research assistant (RS).
Each GEAR core held monthly teleconferences for all core members to discuss and select pertinent PICO questions, prioritize the importance of PICO questions, develop a reproducible search strategy, independently filter the results of the electronic search, extract key study data from the studies that met inclusion criteria, and synthesize the research findings to characterize the current state of research for each selected PICO question. This scoping review was informed by Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews reporting guidelines (Tricco et al., 2018). The study was not pre-registered. The process is also described in a paper published by another GEAR core group (Carpenter et al., 2020).
The GEAR Elder Abuse core also identified one or more articles for each PICO question to illustrate the type of research sought. After the Elder Abuse core attained consensus for the PICO question and exemplar articles, 33 GEAR investigators from all five cores were surveyed to prioritize the top two PICO questions for each core. The top two PICO questions selected as highest priority for the Elder Abuse core were screening and intervention.
Population intervention comparison (PICO) questions
Following monthly meeting and email correspondence among GEAR taskforce participants from all groups, six PICO questions were proposed. After discussing questions, the GEAR Elder Abuse core derived and subsequently refined the following two PICO questions:
PICO #1
Population:
Emergency department patients ≥ 60 years.
Intervention:
Universal screening for elder abuse.
Comparison:
1. Targeted screening, 2. Usual care / Clinical identification of cases based on EMS, nurse, and physician gestalt and usual practice.
Outcomes:
Total cases identified; accuracy of case identification; long-term safety outcomes including potential harms to the patient, short and long-term legal outcomes, short- and long-term functional outcomes, short- and long-term psychosocial outcomes, impact of screening on healthcare utilization.
Question 1:
What is the effect of universal emergency department screening compared to targeted screening or usual practice on cases of elder abuse identified, accuracy of case identification, long-term safety outcomes including harms, legal, functional, and psychosocial outcomes, and health care utilization?
PICO #2
Population:
Emergency department patients aged ≥ 60 years who are previously known, newly found, or suspected to be victims of elder abuse.
Intervention:
Any emergency department-based or emergency department-initiated intervention including Adult Protective Services (APS) reporting.
Comparison:
Usual care including APS reporting.
Outcomes:
Short- and long-term safety, health, legal, functional, psychosocial outcomes
Question 2:
What is the short and long-term safety, health, legal, functional, psychosocial impact of emergency department-based or emergency department-initiated interventions vs. usual care for emergency department patients previously known, newly found, or suspected to be victims of elder abuse?
Search strategy
A medical librarian member of our research team (MD) designed strategies to search the published literature responsive to each of these PICO questions. The databases used were OVID Medline, EMBASE, CINAHL, Cochrane Central Register of Controlled Trials, and Applied Social Sciences Index and Abstracts. Both searches were completed in November 2018. Both of the search strategies were established using a combination of standardized terms and keywords, employing the controlled vocabulary of each database and plain language. For both searches, multiple variants of terms “aged,” “emergency department,” and “elder abuse” were used. For PICO #1, multiple variants of “screening” were added, and, for PICO #2, variants of “victim,” “safety,” and “identified” were added after “intervention” yielded too few results. The full list of search terms is located in Supplement 1. The final reviewed results were limited to English language studies published after 1959. This search took place on November 28th 2018. We also evaluated reference lists of reviews and retrieved articles to check for additional studies.
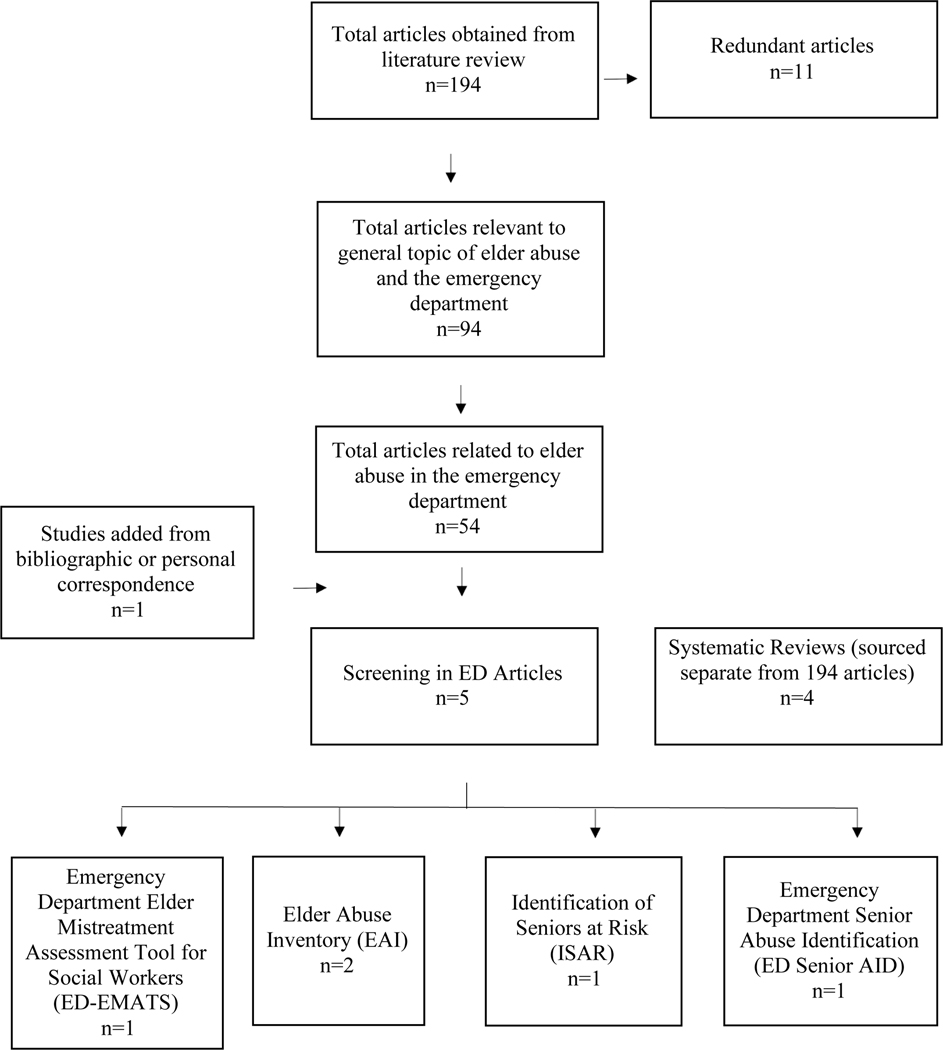
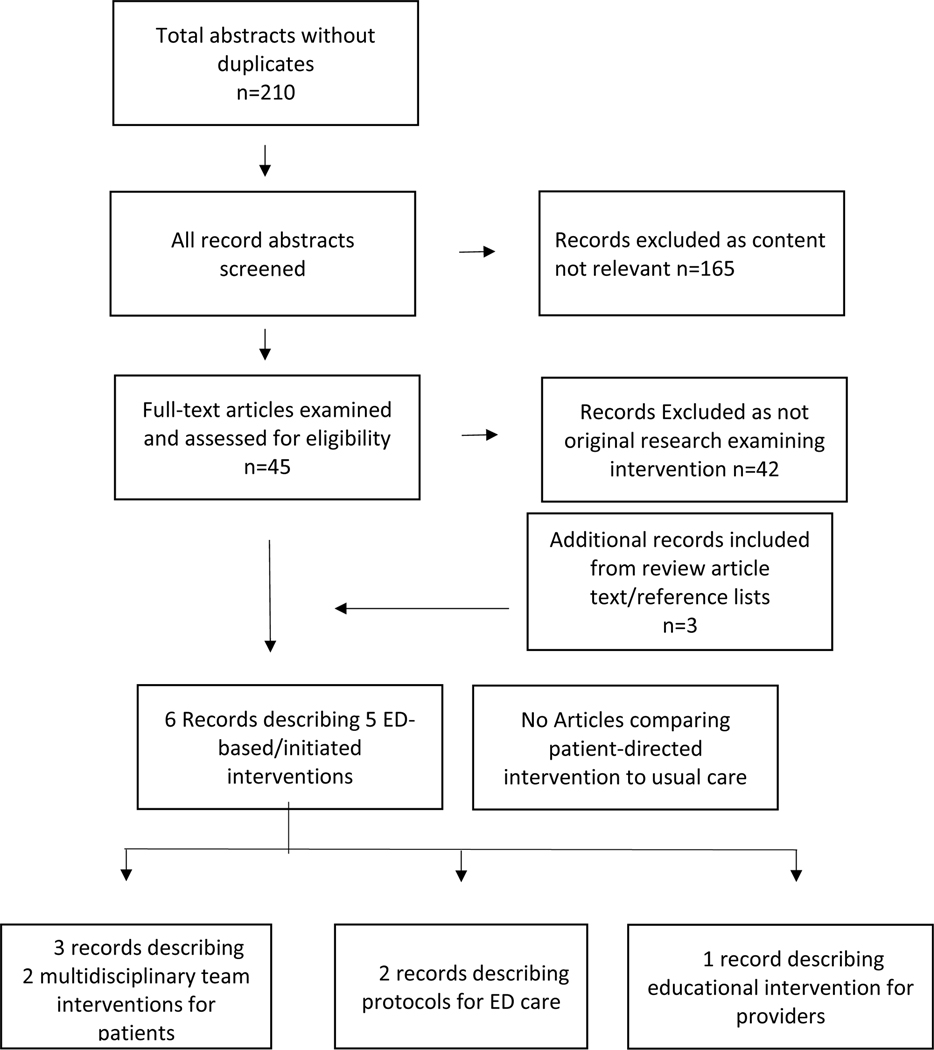
Review process
Multiple research team members (TER, TPM, and RS for PICO #1 and JK, NMH, and SS for PICO #2) independently screened all search results. Abstracts that were clearly not relevant were excluded, with full text of each potentially relevant article obtained and evaluated independently by reviewers. Eligibility for inclusion was based on responsiveness to elements of the PICO question. Disagreements about any study inclusions were resolved by consensus through clarifying discussions. For PICO #1, Cohen’s kappa was used to quantify inter-rater agreement at this stage of the review process, κ = 0.78 (SE of κ = 0.05 and 95% confidence interval = 0.69–0.87). Records were not maintained for the study inclusion and exclusion decision process of PICO #2, so Cohen’s kappa could not be performed for this group. Flowcharts summarizing the results of this article selection process are shown in Figure 1 (for PICO #1) and Figure 2 (for PICO #2). Abstracted articles related to PICO #1 were compiled (Table 1). For PICO #1, variables included in charting were authors, location, inclusion and exclusion criteria, study design, tools and reference standards, and findings. Abstracted articles related to PICO #2 were compiled (Table 2). For PICO #2, variables included in charting were authors, location, sample size, inclusion and exclusion criteria, study design, intervention or protocol details, and findings.
Figure 1:
PRISMA flow-chart for PICO 1
Figure 2.
PRISMA flow chart for PICO 2
Table 1.
PICO 1 Study Abstraction
| Study | Location and Timeframe | Sample Size | Inclusion/Exclusion Criteria | Study Design | Tool and Reference Standard | Findings |
|---|---|---|---|---|---|---|
| Fulmer et al., 2000 | Large U.S. metropolitan hospital 3 weeks |
N = 36 | Age 70 or older, 18 or greater on MMSE, 20 hours or more per week with caregiver | Pilot study, screening in ED, and tool validation | Elder Assessment Instrument (EAI) Expert panel |
71% true-positive 7% false-positive 93% specificity 29% false-negative |
| Fulmer et al., 2005 | 4 EDs in New York and Tampa 2001–2003 |
N = 405 | Age 70 or older, 18 or greater on MMSE, English or Spanish speaking, 20 hours or more per week of paid/unpaid caregiver and telephone in home | Study to use a dyadic vulnerability/risk-profiling framework for elder neglect | MMSE and EAI | RA diagnosed 5% (n = 22) versus NAT diagnosed 22% (n = 86 of 389) |
| Eulitt, et al., 2014 | Virginia EDs (1 urban and 1 rural) March 2012- August 2012 |
N = 180 patients (90 in each site) | Convenience sample of ED visitors age 65 or older, able to consent, and medically stable. Excluded if positive on Mini-Cog or failed “teach back” test | Cross-sectional survey to identify proportion of patients at risk of mistreatment and associated factors | Modified Identification of Seniors at Risk (ISAR) | OR for being at risk is higher in urban hospital (2.93), higher with less education (2.98), and higher if in a supervised setting (14.24) |
| Platts-Mills et al., 2018 | U.S. academic ED Timeframe not mentioned |
N = 259, drawn from one site | 65+, being seen in ED, present and able to participate. Excluded if acutely ill (Emergency Severity Index score 1), on a psychiatric hold, not English speaking, experiencing IPV, or in another study | Tool development, predictive accuracy and reliability through survey of patients seen in ED | Emergency Department Senior Abuse Identification (ED Senior Aid) Clinical judgement vs combination of survey items |
94% sensitivity 90% specificity good or excellent inter-rater reliability |
| Elman et al., 2020. | U.S. Academic ED NA |
N = 10, not tested on older adults; developed with involvement of 10 experts | NA | Review of existing instruments, Delphi approach with experts, focus group, and expert review | Emergency Department Elder Mistreatment Assessment Tool for Social Workers (ED-EMATS) | First elder abuse assessment tool for use in ED by social workers |
Note. ED = Emergency Department, MMSE = Mini-Mental State Exam, U.S. = United States, NAT = Neglect Assessment Team, IPV = Intimate Partner Violence, RA = Research Assistant, OR = Odds Ratio
Table 2.
PICO 2 Study Abstraction
| Study | Location | Sample Size | Inclusion/Exclusion Criteria | Study Design | Intervention or Protocol Details | Findings |
|---|---|---|---|---|---|---|
| Carr et al., 1986 | U.S. academic hospital | N = 50 | Hospitalized patients with suspected elder abuse or neglect | Protocol plus summary of ongoing work | Referral system. Initial assessment by one individual. If concern, then full assessment by RN, MD, and social worker. Cases reviewed and recs made by an Elder Assessment Team | Limited outcome data on 50 cases suggest that the team approach can accurately identify cases. |
| Matlaw & Spence, 1994 | U.S. academic ED | N = 130 | Age 60 and older, plus 2 cases of permanently disabled individuals under age 60. | This study provides results from the protocol initially reported by Carr et al. in 1986 | Multidisciplinary Elder Assessment Team | 130 cases of suspected abuse, 90 (69%) confirmed and reported by EAT. |
| Rosen, Mehta-Naik et al., 2018 | U.S. academic ED | NA | Patient reports elder abuse OR ED staff or EMS suspect abuse | Protocol description | Consultation to the Vulnerable Elder Protection Team. Social worker evaluation, phone consult with MD, consider in-person MD eval, additional hospital and community resources/referrals | Protocol only |
| Jones et al., 1988 | U.S. academic ED | N = 36 | Documented abuse or neglect | Retrospective review | Protocol developed to aid emergency physicians in abuse identification based on history, physical, and psychosocial components | Protocol only |
| Tomita, 1982 | U.S. academic hospital. | NA | Not specified | Protocol | Protocol provides guideline for interviewing patient and caregiver and suggests interventions | Protocol only |
Note. ED = Emergency Department, EAT = Elder Assessment Team, EMS = Emergency Medical Srvices
Consensus conference voting
Based on literature review findings, the GEAR elder abuse subgroup discussed and proposed 19 high priority questions (Supplement 2). These 19 questions highlight a wide range of areas of potential research on elder abuse. This list was presented during an in-person GEAR Consensus Conference of 49 interdisciplinary stakeholder members, the majority (n = 38) attended in person while the remainder (n = 11) participated electronically. The meeting included these participants in addition to 3 support personnel. Participants included emergency physicians, researchers, educators, clinicians, students, geriatricians, nurses, social workers, pharmacists, and patient advocates. The meeting was held in October of 2019.
This group reviewed the findings of the scoping reviews and participated in small group discussions to further reflect on priority issues in elder abuse research. Results of the reviews were provided via presentations at the consensus conference and written summaries of findings. The written portions were made available to participants prior to the start of the conference and all participants were asked to thoroughly review all materials. The original 19 questions were presented and narrowed to 5 through an iterative process of small group discussion, large group debriefs, consolidation, and voting. The in-person conference covering elder abuse and the 4 other high-impact topics took place over a two-day time period. For those not able to attend the conference, voting occurred electronically the week following the conference with 100% participation of task force members. All voting occurred via an online portal in which participants were blinded to the submissions of other participants until after their vote had been submitted. Results of voting were made available to all task force members.
Results
PICO #1 – screening and assessment
We did not find any studies that responded directly to PICO #1 comparing the outcomes of universal screening to targeted screening or usual care. There is, however, research describing the development and evaluation of screening tools for elder abuse, including two recent reviews (Cohen, 2011; McCarthy et al., 2017). Only 4 screening tools for elder abuse have been explicitly described for use in the emergency department: (1) The Elder Assessment Instrument (EAI) (Fulmer et al., 2000; Fulmer et al., 2005; Fulmer et al., 1984), (2) Identifications of Seniors at Risk (ISAR) (Eulitt et al., 2014; McCusker et al., 1999), (3) Emergency Department Senior Abuse Identification (ED-Senior AID) (Platts-Mills et al., 2018), and (4) Emergency Department Elder Mistreatment Assessment Tool for Social Workers (ED-EMATS) (Elman, Rosselli, et al., 2020). Two of these tools (ED-Senior AID and ED-EMATS) are recently developed and are still under active study to further characterize their test characteristics and potential utility.
We noted important differences between these tools, which assess various constructs, including: abuse, neglect, exploitation and abandonment (EAI), mistreatment (ED-EMATS), abuse that includes neglect (ED-Senior AID), and vulnerability to adverse outcomes (ISAR). Some tools have been designed to be used by different disciplines, with the ED-Senior AID intended for nurses and the ED-EMATS for social workers. In contrast, the EAI and ISAR may be used by any ED staff member. The tools use both self-report via direct questioning and clinical observation and inspection for signs of abuse. The ED-EMATS relies on self-report from patients, the EAI relies on clinical observation, and the ED-Senior AID combines self-report and clinical observation. The ISAR was not initially designed to assess for abuse and does not specifically do so. Rather, it assesses for risk factors of a poor outcome for older adults presenting to the emergency department, which may also be risk factors associated with abuse. The choice to include ISAR was made solely on the basis that it has been researched in relation to elder abuse (Eulitt et al., 2014) and is widely used in emergency care. It should be noted that other instruments (e.g., Clinical Frailty Scale) may reflect similar constructs, but were not included because they have not been researched explicitly as an approach to screening for elder abuse. Further work to establish instrument utility of these tools that includes investigations of provider acceptability, potential harms, and patient-centric outcomes in the clinical setting are needed.
PICO #2 - intervention
We did not find any studies that were directly responsive to PICO #2 comparing specific ED-based or ED-initiated interventions for known or suspected elder abuse victims to usual care. Per the PICO question, the intervention could be APS reporting with usual care as a control condition, or APS reporting could have been a control condition if a structured intervention was specified. We did find six articles describing five ED-based/initiated interventions. These included three interventions using multi-disciplinary teams (Carr et al., 1986; Matlaw & Spence, 1994; Rosen, Mehta-Naik, et al., 2018) and two protocols for emergency department care (Jones et al., 1988; Tomita, 1982).
None of these descriptions examined patient outcomes or included a comparison group. One multi-disciplinary team (an ED physician and a social worker and other consult services, as necessary) was based in the emergency department (Rosen, Mehta-Naik, et al., 2018) while the other was hospital-based but received referrals from the emergency department (Carr et al., 1986; Matlaw & Spence, 1994). Both protocols focused on assessment and response, with one targeted towards all health care professionals including emergency department providers (Tomita, 1982) and the other designed specifically for the emergency department and inpatient setting. (Jones et al., 1988) We also found an educational intervention for Emergency Medicine residents that included an overview of elder abuse as well as information about assessment and reporting and that was evaluated using a pre-and post-test (Uva & Guttman, 1996). Notably, other than a single guideline (Geriatric Emergency Department Guidelines, 2014) and suggested list of competencies (Hogan et al., 2010), we did not identify literature describing usual care for emergency department response to elder abuse.
Consensus of highest yield ED elder abuse research priorities
During the GEAR Consensus Conference, the following questions were selected as the highest priority for future research (in rank order):
Targeted Screening: Can we effectively identify patients at high risk for elder abuse for whom we can then do targeted screening?
Intervention for Caregivers: Does an intervention to reduce caregiver stress among ED patients with cognitive impairment improve caregiver health and also reduce elder abuse?
Screening and Intervention: Does screening and structured interventions improve outcomes for victims of elder abuse?
EMS Screening: Can a standardized approach to EMS screening for elder abuse increase case identification?
Abuse Specific Interventions: Should interventions that are developed and tested to treat elder abuse in the ED be type-specific, either based on physical, psychological, sexual, financial abuse or neglect or based on specific characteristics such as severity, perpetrator, setting, or resources?
Two of the 5 questions were related to screening, two were related to intervention, and one combined screening and intervention.
Discussion
We present the results of an interdisciplinary effort to summarize existing knowledge regarding screening and interventions for elder abuse in the emergency department and define priority research questions. Though we found promising developments in both assessment and intervention, our scoping review did not reveal any published literature that directly addressed our two PICO questions. Within this context, the priority questions identified tackle overarching issues with the potential to expand future knowledge in important directions.
The consensus conference was held prior to the current COVID-19 pandemic; however, the findings of the group have particular relevance in the context COVID-19. Several scholars have commented on how factors brought on or exacerbated by the pandemic including financial stress, sheltering-in-place, closure of community organizations, and social distancing measures may inadvertently increase risk of abuse and neglect in older adults (Elman, Breckman, et al., 2020; Gardner et al., 2020). Given the potential rise in elder abuse related to COVID-19, it is even more timely and urgent for emergency providers to have evidence-based tools at their disposal to identify abuse and to intervene to address concerns.
Ethical issues associated with screening and reporting must also be considered (Beach et al., 2016; Donovan & Regehr, 2010; Rodriguez et al., 2006). Identification and discussion of abuse may make a situation acutely worse or potentially expose patients to new risks. Further, in some emergency departments, social worker or other personnel familiar with interventions for elder abuse may not be available, and physicians and nurses may not have time or sufficient experience to feel comfortable attempting to address abuse or identify appropriate next steps (Auerbach et al., 2007). Additionally, serious ethical challenges exist when attempting to design comparative studies of interventions versus usual care in this vulnerable population
We found very little literature about emergency department-based or emergency department-initiated interventions for elder abuse victims, and none that included rigorous evaluation. This is consistent with previous reviews (Ayalon et al., 2016; Baker et al., 2016; Rosen, Elman, et al., 2019), which have found that evaluation for elder abuse interventions is uncommon and few elder abuse programs are based in or integrated at acute care hospitals (Rosen, Elman, et al., 2019). Reasons for this absence of rigorously evaluated interventions include limited funding to support elder abuse research, the lengthy period associated with translation research (Morris et al., 2011), and a limited pool of investigators studying acute care for older adults (Rosen, Makaroun, et al., 2019). Low rates of elder abuse identification (Evans, Hunold, et al., 2017; Rosen, Stern, et al., 2018) may also create the false perception that a robust, standardized response is not needed.
We believe that, despite these challenges, formal, high-quality, rigorous studies are needed examining existing or newly developed emergency department interventions using robust patient-oriented outcomes such as goal attainment scaling (Burnes & Lachs, 2017). Ideally these studies would include either usual care as a randomization arm or through comparison with a historical/pre-intervention control period. Randomized control trials that involve a no treatment or intervention arm have a strong potential to contribute meaningful findings, however, they present ethical issues that would need special consideration given the vulnerable nature of research participants (Beach et al., 2016), and may be unfeasible in many cases. Methods used to evaluate pragmatic and complex interventions have particular value in this context (Carpenter & Malone, 2020) The questions selected by GEAR highlight the value of both working interdisciplinarity within the emergency department and partnering with outside providers like EMS and APS.
Many unanswered questions exist regarding what constitutes usual care. It is not clear, if and when elder abuse is identified in the emergency department, if it is critical that an intervention be initiated immediately in the emergency department/hospital setting or if it may be deferred to occur in an outpatient setting. Additionally, more information to characterize the typical involvement of APS following emergency department discharge is necessary. Also requiring further exploration are what criteria should be met for an elder abuse victim to be safely discharged and under what circumstances is hospital admission for safety necessary. Though this was not identified as a priority question, in clinical care in the emergency department, this concern routinely arises. Though recommendations exist, and no clear guidelines have been established (Wong et al., 2020). A potential role for screening and intervention by Emergency Medical Services providers has been suggested but should be explored more deeply (Namboodri et al., 2018; Rosen et al., 2017). A multi-disciplinary team approach, which has been successful in child protection (Hochstadt & Harwicke, 1985; Kistin et al., 2010) and is the most common intervention strategy described in this review, may be particularly promising but is resource intensive. Therefore, data on impact are needed. Screening approaches and interventions for elder abuse in the emergency department can be meaningfully informed by work related to child maltreatment and intimate partner violence (Beach et al., 2016). Relative to elder abuse, a far larger research and practice base exists in these areas; lessons from this work can guide research on elder abuse
Currently, the standard response when elder abuse is suspected or confirmed in many emergency departments is to report to APS as a sole intervention. The overall positive (and potential adverse) impact of mandatory reporting has not been fully evaluated. (US General Accounting Office, 1991) Many experts are not convinced that the benefits of this intervention outweigh harms (Beach et al., 2016), and additional research is needed. The potential harms and danger introduced via screening and interventions should be carefully considered and accounted for in future work. Though interventions are intended to reduce risk, unintended harms (e.g., withdrawal of caregiver support) are possible.
We also believe that in elder abuse work, the growth of research interest and translation to clinical practice in screening and intervention are closely linked. This scoping review highlights gaps in the current literature as well as potential high-impact areas of future work. If emergency departments continue to have low rates of screening, large numbers of cases will continue to be missed. With low rates of recognition, little knowledge can be built around best practices and effective interventions. Further, limited knowledge of intervention options and the absence of an association between elder abuse screening and healthcare outcomes reduces interest in screening among emergency department providers in an already overburdened setting. Robust screening, however, may draw attention to the need for effective interventions and stimulate investment in development and study of response strategies. Also, establishment of effective and impactful responses has the potential to serve as the impetus for increased interest in screening, both by medical providers and in settings outside of the emergency department. Because the causes of elder abuse are multifactorial, screening and interventions research will require interdisciplinary work.
This study has several limitations. The scoping reviews conducted was focused specifically on screening and interventions to address elder abuse during emergency care. This represents only a small subset of the overall work in screening and intervention for elder abuse in the healthcare setting. Recently published complementary work includes a broad review of elder abuse in emergency care; a review of screening tools to identify elder abuse across healthcare in general; and recent systematic reviews of the prevalence of elder abuse (Gallione et al., 2017; Mercier et al., 2020; Yon et al., 2019; Yon et al., 2017). We limited our search to articles written in English, and thus may have missed relevant work from non-English speaking countries (Morrison et al., 2012). Though taskforce members represented diverse disciplines and professional backgrounds, the process would have benefited from the additional presence of prehospital providers, adult protective services workers, and patient advocates. Two patient advocates participated in the GEAR process and voting but were not members of the Elder Abuse core. Though our review was comprehensive, the date of the search, November of 2018, prevented examination of instruments developed or tested after that time. One known example of this, an evaluation of an EMS-based screening tool, the Detection of Elder Mistreatment Through Emergency Care Technicians (DETECT), was published in 2019 (Cannell et al., 2019) and is not included in this systematic review. A validation study of the ED Senior AID (Platts-Mills et al., 2020) was also not included in this review due to time of publication
Several topics that could greatly improve management of elder abuse were absent from the literature: information on the identification of modifiable risk factors for elder abuse (e.g. caregiver stress), emergency department-based or initiated interventions to prevent elder abuse, and work describing appropriate theoretical models that would serve as a foundation to derive or assess interventions to treat elder abuse in the emergency department. We also did not identify any work related to examinations of cultural or community factors that might inform the manifestation or treatment of elder abuse in the emergency department. When the evidence base is sufficient to identify optimal or close-to-optimal approaches for emergency department elder abuse screening and intervention, randomized trials or methods to evaluate complex interventions may be necessary to accurately characterize the clinical impact. In conclusion, we believe additional research on elder abuse is essential to improve our understanding of how to optimally identify and serve these vulnerable older adults. We hope that the gaps in research revealed through the work of GEAR will be used to direct future research efforts.
Supplementary Material
Summary of all search terms used for both PICO 1 and PICO 2
Full listing of candidate questions for consensus conference voting
Affirmation:
I affirm that I have listed everyone who has contributed significantly to the work and have obtained written consent from all contributors who are not authors and are named in the acknowledgement section
Impact Statement:
We certify that this work is novel. This work contains a detailed scoping review of findings related to screening and intervention of elder abuse specifically in the emergency department setting. Using this work and the input of an interdisciplinary team assembled at a consensus conference, we provide suggestions to guide future investigations in the form of high priority research questions.
Acknowledgments
Funding: The John A. Hartford Foundation, Gary and Mary West Health Institute, and National Institute on Aging (R21AG058926)
References
- Acierno R, Hernandez MA, Amstadter AB, Resnick HS, Steve K, Muzzy W, & Kilpatrick DG (2010). Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health, 100(2), 292–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institue on Aging (2016). Elder Abuse. In National Institue on Aging. Health; (Ed.). [Google Scholar]
- Auerbach C, Mason SE, & Heft Laporte H. (2007). Evidence that supports the value of social work in hospitals. Soc Work Health Care, 44(4), 17–32. 10.1300/J010v44n04_02 [DOI] [PubMed] [Google Scholar]
- Ayalon L, Lev S, Green O, & Nevo U. (2016). A systematic review and meta-analysis of interventions designed to prevent or stop elder maltreatment. Age Ageing, 45(2), 216–227. 10.1093/ageing/afv193 [DOI] [PubMed] [Google Scholar]
- Baker PR, Francis DP, Hairi NN, Othman S, & Choo WY (2016). Interventions for preventing abuse in the elderly. Cochrane Database of Systematic Reviews. 10.1002/14651858.CD010321.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach SR, Carpenter CR, Rosen T, Sharps P, & Gelles R. (2016). Screening and detection of elder abuse: Research opportunities and lessons learned from emergency geriatric care, intimate partner violence, and child abuse. J Elder Abuse Negl, 28(4–5), 185–216. 10.1080/08946566.2016.1229241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biber R, Bail HJ, Sieber C, Weis P, Christ M, & Singler K. (2013). Correlation between age, emergency department length of stay and hospital admission rate in emergency department patients aged ≥70 years. Gerontology, 59(1), 17–22. 10.1159/000342202 [DOI] [PubMed] [Google Scholar]
- Burnes D, Henderson CR Jr., Sheppard C, Zhao R, Pillemer K, & Lachs MS (2017). Prevalence of Financial Fraud and Scams Among Older Adults in the United States: A Systematic Review and Meta-Analysis. Am J Public Health, 107(8), e13–e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnes D, & Lachs MS (2017). The Case for Individualized Goal Attainment Scaling Measurement in Elder Abuse Interventions. J Appl Gerontol, 36(1), 116–122. 10.1177/0733464815581486 [DOI] [PubMed] [Google Scholar]
- Cannell B, Gonzalez JMR, Livingston M, Jetelina KK, Burnett J, & Weitlauf JC (2019). Pilot testing the detection of elder abuse through emergency care technicians (DETECT) screening tool: results from the DETECT pilot project. J Elder Abuse Negl, 31(2), 129–145. 10.1080/08946566.2018.1564104 [DOI] [PubMed] [Google Scholar]
- Carpenter CR, & Gerson LW (2008). Geriatric Emergency Medicine. The American Geriatrics Society. [Google Scholar]
- Carpenter CR, Hammouda N, Linton EA, Doering M, Ohuabunwa UK, Ko KJ, Hung WW, Shah MN, Lindquist LA, Biese K, Wei D, Hoy L, Nerbonne L, Hwang U, & Dresden SM (2020). Delirium Prevention, Detection, and Treatment in Emergency Medicine Settings: A Geriatric Emergency Care Applied Research (GEAR) Network Scoping Review and Consensus Statement. Acad Emerg Med. 10.1111/acem.14166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter CR, & Malone ML (2020). Avoiding Therapeutic Nihilism from Complex Geriatric Intervention “Negative” Trials: STRIDE Lessons. J Am Geriatr Soc, 68(12), 2752–2756. 10.1111/jgs.16887 [DOI] [PubMed] [Google Scholar]
- Carr K, Dix G, Fulmer T, & al, e. (1986). An elder abuse assessment team in an acute hospital setting. The Beth Israel Hospital Elder Assessment Team. Gerontologist, 26, 115–118. [DOI] [PubMed] [Google Scholar]
- Cohen M. (2011). the Identification of Elder Abuse. Journal of Clinical Outcomes Management, 18, 261–270. [Google Scholar]
- Centers for Disease Conttol. (2016). Understanding Elder Abuse. [Google Scholar]
- Dong XQ (2015). Elder Abuse: Systematic Review and Implications for Practice. J Am Geriatr Soc, 63(6), 1214–1238. 10.1111/jgs.13454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan K, & Regehr C. (2010). Elder Abuse: Clinical, Ethical, and Legal Considerations in Social Work Practice. Clinical Social Work Journal, 38(2), 174–182. 10.1007/s10615-010-0269-2 [DOI] [Google Scholar]
- Dufour I, Chouinard MC, Dubuc N, Beaudin J, Lafontaine S, & Hudon C. (2019). Factors associated with frequent use of emergency-department services in a geriatric population: a systematic review. BMC Geriatr, 19(1), 185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elman A, Breckman R, Clark S, Gottesman E, Rachmuth L, Reiff M, Callahan J, Russell LA, Curtis M, Solomon J, Lok D, Sirey JA, Lachs MS, Czaja S, Pillemer K, & Rosen T. (2020). Effects of the COVID-19 Outbreak on Elder Mistreatment and Response in New York City: Initial Lessons. J Appl Gerontol, 39(7), 690–699. 10.1177/0733464820924853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elman A, Rosselli S, Burnes D, Clark S, Stern ME, LoFaso VM, Mulcare MR, Breckman R, & Rosen T. (2020). Developing the Emergency Department Elder Mistreatment Assessment Tool for Social Workers Using a Modified Delphi Technique Health Soc Work. 10.1093/hsw/hlz040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eulitt PJ, Tomberg RJ, Cunningham TD, Counselman FL, & Palmer RM (2014). Screening elders in the emergency department at risk for mistreatment: a pilot study. J Elder Abuse Negl, 26(4), 424–435. 10.1080/08946566.2014.903549 [DOI] [PubMed] [Google Scholar]
- Evans CS, Hunold KM, Rosen T, & Platts-Mills TF (2017). Diagnosis of Elder Abuse in U.S. Emergency Departments. J Am Geriatr Soc, 65(1), 91–97. 10.1111/jgs.14480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans CS, Platts-Mills TF, Fernandez AR, Grover JM, Cabanas JG, Patel MD, Vilke GM, & Brice JH (2017). Repeated Emergency Medical Services Use by Older Adults: Analysis of a Comprehensive Statewide Database. Ann Emerg Med, 70(4), 506–515.e503. 10.1016/j.annemergmed.2017.03.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulmer T, Paveza G, Abraham I, & Fairchild S. (2000). Elder neglect assessment in the emergency department. J Emerg Nurs (6), 436–443. 10.1067/men.2000.110621 [DOI] [PubMed] [Google Scholar]
- Fulmer T, Paveza G, Vandeweerd C, Guadagno L, Fairchild S, Norman R, Abraham I, & Bolton-Blatt M. (2005). Neglect assessment in urban emergency departments and confirmation by an expert clinical team. J Gerontol A Biol Sci Med Sci (60), 1002–1006. 10.1093/gerona/60.8.1002 [DOI] [PubMed] [Google Scholar]
- Fulmer T, Street S, & Carr K. (1984). Abuse of the elderly: screening and detection. J Emerg Nurs, 10(3), 131–140. [PubMed] [Google Scholar]
- Gallione C, Dal Molin A, Cristina FVB, Ferns H, Mattioli M, & Suardi B. (2017). Screening tools for identification of elder abuse: a systematic review. J Clin Nurs, (26), 2154–2176. 10.1111/jocn.13721 [DOI] [PubMed] [Google Scholar]
- Gardner W, States D, & Bagley N. (2020). The Coronavirus and the Risks to the Elderly in Long-Term Care. J Aging Soc Policy, 1–6. 10.1080/08959420.2020.1750543 [DOI] [PubMed] [Google Scholar]
- Geriatric Emergency Department Guidelines. (2014). Ann Emerg Med, 63(5), e7–25. 10.1016/j.annemergmed.2014.02.008 [DOI] [PubMed] [Google Scholar]
- Hochstadt NJ, & Harwicke NJ (1985). How effective is the multidisciplinary approach? A follow-up study. Child Abuse Negl, 9(3), 365–372. [DOI] [PubMed] [Google Scholar]
- Hogan TM, Losman ED, Carpenter CR, Sauvigne K, Irmiter C, Emanuel L, & Leipzig RM (2010). Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med, 17(3), 316–324. 10.1111/j.1553-2712.2010.00684.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones J, Dougherty J, Schelble D, & Cunningham W. (1988). Emergency department protocol for the diagnosis and evaluation of geriatric abuse. Ann Emerg Med, 17(10), 1006–1015. [DOI] [PubMed] [Google Scholar]
- Kistin CJ, Tien I, Bauchner H, Parker V, & Leventhal JM (2010). Factors that influence the effectiveness of child protection teams. Pediatrics, 126(1), 94–100. 10.1542/peds.2009-3446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachs MS, Williams CS, O’Brien S, Pillemer KA, & Charlson ME (1998). The mortality of elder mistreatment. JAMA, 280(5), 428–432. 10.1001/jama.280.5.428 [DOI] [PubMed] [Google Scholar]
- Matlaw JR, & Spence DM (1994). The hospital elder assessment team - a protocol for suspected cases of elder abuse and neglect. J Elder Abuse Negl, 6(2), 23–37. 10.1300/J084v06n02_03 [DOI] [Google Scholar]
- McCarthy L, Campbell S, & Penhale B. (2017). Elder abuse screening tools: a systematic review. Journal of Adult Protection, 19(6), 368–379. 10.1108/JAP-10-2016-0026 [DOI] [Google Scholar]
- McCusker J, Bellavance F, Cardin S, Trépanier S, Verdon J, & Ardman O. (1999). Detection of older people at increased risk of adverse health outcomes after an emergency visit: the ISAR screening tool. J Am Geriatr Soc, 47(10), 1229–1237. 10.1111/j.1532-5415.1999.tb05204.x [DOI] [PubMed] [Google Scholar]
- Mercier E, Nadeau A, Brousseau AA, Emond M, Lowthian J, Berthelot S, Costa AP, Mowbray F, Melady D, Yadav K, Nickel C, & Cameron PA (2020). Elder Abuse in the Out-of-Hospital and Emergency Department Settings: A Scoping Review. Ann Emerg Med, 75(2), 181–191. 10.1016/j.annemergmed.2019.12.011 [DOI] [PubMed] [Google Scholar]
- Morris ZS, Wooding S, & Grant J. (2011). The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med, 104(12), 510–520. 10.1258/jrsm.2011.110180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison A, Polisena J, Husereau D, Moulton K, Clark M, Fiander M, Mierzwinski-Urban M, Clifford T, Hutton B, & Rabb D. (2012). The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int J Technol Assess Health Care, 28(2), 138–144. 10.1017/s0266462312000086 [DOI] [PubMed] [Google Scholar]
- Namboodri BL, Rosen T, Dayaa JA, Bischof JJ, Ramadan N, Patel MD, Grover J, Brice JH, & Platts-Mills TF (2018). Elder Abuse Identification in the Prehospital Setting: An Examination of State Emergency Medical Services Protocols. J Am Geriatr Soc, 66(5), 962–968. 10.1111/jgs.15329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platts-Mills TF, Dayaa JA, Reeve BB, Krajick K, Mosqueda L, Haukoos JS, Patel MD, Mulford CF, McLean SA, Sloane PD, Travers D, & Zimmerman S. (2018). Development of the Emergency Department Senior Abuse Identification (ED Senior AID) tool. J Elder Abuse Negl, 30(4), 247–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platts-Mills TF, Hurka-Richardson K, Shams RB, Aylward A, Dayaa JA, Manning M, Mosqueda L, Haukoos JS, Weaver MA, Sloane PD, Travers D, Hendry PL, Norse A, Jones CW, McLean SA, Reeve BB, Zimmerman S, Davenport K, Bynum D, Frederick E, Lassiter-Fisher K, Stuckey A, Daley-Placide R, Hoppens M, Betterton J, Owusu S, Flemming C, & Colligan A. (2020). Multicenter Validation of an Emergency Department-Based Screening Tool to Identify Elder Abuse. Ann Emerg Med, 76(3), 280–290. 10.1016/j.annemergmed.2020.07.005 [DOI] [PubMed] [Google Scholar]
- Rodriguez MA, Wallace SP, Woolf NH, & Mangione CM (2006). Mandatory reporting of elder abuse: between a rock and a hard place. Ann Fam Med, 4(5), 403–409. 10.1370/afm.575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen T, Elman A, Dion S, Delgado D, Demetres M, Breckman R, Lees K, Dash K, Lang D, Bonner A, Burnett J, Dyer CB, Snyder R, Berman A, Fulmer T, & Lachs MS (2019). Review of Programs to Combat Elder Mistreatment: Focus on Hospitals and Level of Resources Needed. J Am Geriatr Soc, 67(6), 1286–1294. 10.1111/jgs.15773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen T, Lien C, Stern ME, Bloemen EM, Mysliwiec R, McCarthy TJ, Clark S, Mulcare MR, Ribaudo DS, Lachs MS, Pillemer K, & Flomenbaum NE (2017). Emergency Medical Services Perspectives on Identifying and Reporting Victims of Elder Abuse, Neglect, and Self-Neglect. J Emerg Med, 53(4), 573–582. 10.1016/j.jemermed.2017.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen T, Makaroun LK, Conwell Y, & Betz M. (2019). Violence In Older Adults: Scope, Impact, Challenges, And Strategies For Prevention. Health Aff (Millwood), 38(10), 1630–1637. 10.1377/hlthaff.2019.00577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen T, Mehta-Naik N, Elman A, Mulcare MR, Stern ME, Clark S, Sharma R, LoFaso VM, Breckman R, Lachs M, & Needell N. (2018). Improving Quality of Care in Hospitals for Victims of Elder Mistreatment: Development of the Vulnerable Elder Protection Team. Jt Comm J Qual Patient Saf, 44(3), 164–171. 10.1016/j.jcjq.2017.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen T, Stern ME, Elman A, & Mulcare MR (2018). Identifying and Initiating Intervention for Elder Abuse and Neglect in the Emergency Department. Clin Geriatr Med, 34(3), 435–451. 10.1016/j.cger.2018.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabir M, Breckman R, Meador R, Wethington E, Reid MC, & Pillemer K. (2006). The CITRA research-practice consensus-workshop model: exploring a new method of research translation in aging. Gerontologist, 46(6), 833–839. 10.1093/geront/46.6.833 [DOI] [PubMed] [Google Scholar]
- Stiegel LA (2017). Legal Basics: Elder Abuse (pp. 1–5). National Center on Law & Elder Rights. [Google Scholar]
- Tomita S. (1982). Detection and treatment of elderly abuse and neglect: A protocol for health care professionals. 2(2), 37–51. [Google Scholar]
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tuncalp O, & Straus SE (2018). PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation (Ann Intern Med (Vol. 169, pp. 467–473). 10.7326/m18-0850 [DOI] [PubMed] [Google Scholar]
- US General Accounting Office. (1991). Elder Abuse: Effectiveness of Reporting Laws and Other Factors. https://www.gao.gov/assets/220/214127.pdf
- Uva JL, & Guttman T. (1996). Elder abuse education in an emergency medicine residency program [Letter]. Acad Emerg Med, 3(8), 817–819. [PubMed] [Google Scholar]
- Wong J, & Waite L. (2017). Elder mistreatment predicts later physical and psychological health: Results from a national longitudinal study. J Elder Abuse Negl, 29(1), 15–42. 10.1080/08946566.2016.1235521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong SP, Sharda N, Zietlow KE, & Heflin MT (2020). Planning for a Safe Discharge: More Than a Capacity Evaluation. J Am Geriatr Soc, 68(4), 859–866. 10.1111/jgs.16315 [DOI] [PubMed] [Google Scholar]
- Yon Y, Mikton C, Gassoumis ZD, & Wilber KH (2019). The Prevalence of Self-Reported Elder Abuse Among Older Women in Community Settings: A Systematic Review and Meta-Analysis. Trauma Violence Abuse, 20(2), 245–259. 10.1177/1524838017697308 [DOI] [PubMed] [Google Scholar]
- Yon Y, Mikton CR, Gassoumis ZD, & Wilber KH (2017). Elder abuse prevalence in community settings: a systematic review and meta-analysis (Lancet Glob Health (5), e147–e156. 2017 10.1016/s2214-109x(17)30006-2 [DOI] [PubMed] [Google Scholar]
- Yunus RM, Hairi NN, & Choo WY (2019). Consequences of Elder Abuse and Neglect: A Systematic Review of Observational Studies. Trauma Violence Abuse, 20(2), 197–213. 10.1177/1524838017692798 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Summary of all search terms used for both PICO 1 and PICO 2
Full listing of candidate questions for consensus conference voting