Abstract
Objective:
The purpose of this study was to investigate the changing profile of the phenotypic expression of eating disorders (EDs) and related sociocultural factors in Japan between 1700 and 2020.
Method:
The authors conducted a systematic scoping review in accordance with the PRISMA statement guidelines for scoping reviews.
Results:
Findings indicate that Kampo doctors reported more than 50 patients with restrictive EDs in the 1700s, when Japan adopted a national isolation policy. On the other hand, only a few reports of EDs were found between 1868 and 1944, when rapid Westernization occurred. After World War II, providers began diagnosing patients with anorexia nervosa (AN) around 1960. Patients reported experiencing fat phobia, but did not engage in restriction for achieving slimness. However, after the 1970s, Japan experienced a rise in patients with AN who engaged in restriction to achieve thinness. Cases of patients who engaged in binge/purge symptomatology increased after the 1980s, followed by a steady increase in total ED cases after the 1990s. At various time points, providers attributed family conflicts, internalization of a thin ideal of beauty, changing food environments, and pressures associated with traditional gender roles to the onset and maintenance of EDs in Japan.
Discussion:
Findings reveal that restrictive EDs were present as early as the 18th century; Japanese patients may present with both “typical” and “atypical” forms of AN; ED symptoms can persist in the absence of Western influence; and sociocultural factors, such as gender-specific stressors and family dynamics, may contribute to EDs for Japanese populations.
Keywords: Eating disorders, Epidemiology, Prevalence, Japan, Sociocultural factors, Gender roles, Thin ideal, Westernization, Cross-cultural psychology
1 |. INTRODUCTION
Eating disorders (EDs) are pernicious mental illnesses that are characterized by significant preoccupations with food and weight/shape, and abnormal eating patterns. These health conditions are associated with elevated clinical impairment, medical comorbidities, and mortality rates (American Psychiatric Association, 2013). Most of the research on EDs has focused on young White women from Western cultures, however, disordered eating is known to affect a wider proportion of the global population (Thomas, Lee, & Becker, 2016). Asia is the largest and most populous continent in the world; yet, despite this, relatively limited research has examined the prevalence, risk factors, and presentations of EDs among the diverse groups of people who occupy this region (Pike & Dunne, 2015; Soh & Walter, 2013). Although EDs were initially thought to be “culturally-bound syndromes,” such that they only occurred in countries that had undergone Westernization (Prince, 1985), there have been reports of ED-like presentations in Japan dating back to the 18th century (Kagawa, 1768).
Available epidemiological data suggest that ED prevalence is rising in Japan (Nakai, Nin, & Noma, 2014a; Nakai et al., 2018). However, current prevalence rates may be an underestimate, given that much of our knowledge has been derived from reviews written in English. For instance, other important studies that provide insight into EDs at various time points during Japanese history were initially missed in broad reviews examining EDs in non-Western countries due to language barriers (Cummins, Simmons & Zane, 2005; Keel & Klump, 2003; Makino, Tsuboi, & Dennerstein, 2004). Importantly, these Japanese and Chinese case studies highlight notable differences in clinical presentations of restrictive EDs, as compared to diagnostic criteria outlined in Western nosology (American Psychiatric Association, 2013). For example, around 1960, patients with anorexia nervosa (AN) reported fat phobia; however, they did not engage in restriction for the purpose of achieving a slim figure (Shimosaka, 1961). In contrast, Aoki and colleagues (1976) describe cases of patients with AN who appeared emaciated, but described no fear of fatness. Thus, within the span of a decade, health providers documented vast differences in ED presentations, suggesting that there may be alternative motives for restriction in these groups that could be attributed to cultural shifts during this time period.
There are many cultural differences between Japan and Western countries, including social orientations (e.g., collectivism vs. individualism), food (e.g., Japanese foods tend to be lower in fat content relative to Western diets), family systems (e.g., extended family vs nuclear family), and gender roles (e.g., traditional vs. contemporary gender roles) (Markus & Kitayama, 2010; Mason & Caiger, 1997; Vardaman, 2006). There are some studies which suggest that a combination of these elements from both Japanese and Western cultures contribute to the development of EDs in Japanese populations (Keel & Klump, 2003; Nishizono-Maher, 1998; Pike & Borovoy, 2004). It is currently unclear, however, how these cultural factors have contributed to ED presentations in Japanese populations, especially across different temporal periods. Historically, since EDs were first reported in the 1700s (Kagawa, 1768; Ogino, 1770; Tachibana, 1796), Japan has undergone two revolutionary regimes: the Meiji Restoration in 1868 when Japan transitioned from a feudalist society to a constitutional monarchy, and the end of World War II in 1945 when Japan transitioned from a militaristic regime to a democratic nation (Mason & Caiger, 1997). Given these marked transitions in the nation’s history, it may that cultural shifts associated with these events could provide insight into the onset and maintenance of EDs in Japan.
Although there have been multiple descriptive reviews of ED presentations in Japan (e.g., Chisuwa & O’Dea, 2010; Nishizono-Maher, 1998; Nogami, 1997), no systematic reviews have been conducted with this population. Systematic reviews are considered the standard for synthesizing evidence in healthcare research due to their methodological rigor (Munn et al., 2018). However, given the difficulties of merging data from Chinese and Japanese case reports up until 1980 with epidemiological studies written in English after 1980, scoping reviews provide a useful alternative for interpreting this data. Scoping reviews examine emerging evidence and provide a broader overview of a nascent topic area, with the aims of highlighting current gaps in the literature, and stimulating future research (Munn et al, 2018). Given the disparate, yet vast, body of literature focused on EDs in Japan, the current study aimed to maximize the benefits of both methodological approaches by conducting a systematic scoping review in accordance with extended PRISMA guidelines for scoping reviews (Tricco et al., 2018). Specifically, this study aimed to investigate and map how the phenotypic expression of EDs has changed between 1700 and 2020 in Japan, and how these changes coincided with sociocultural shifts in Japanese history.
2 |. METHOD
2.1 |. Search strategy
We performed a comprehensive literature search in PubMed and CiNii (Citation Information by National Institute of Informatics; https://ci.nii.ac.jp/) in July 2020. We employed several key terms relating to EDs, epidemiology, and sociocultural factors in Japan. CiNii is a data search service system supported by National Institute of Informatics which contains more than 20,630,000 articles, including unpublished academic literature and articles written in both Japanese and English. Search terms were grouped into four categories: (a) Japan, (b) eating disorders (“eating disorder” OR “feeding and eating disorder” OR “anorexia nervosa” OR “bulimia nervosa” OR “binge-eating disorder” OR “avoidant/restrictive food intake disorder”), (c) epidemiology (epidemiology OR prevalence OR incidence), and (d) sociocultural factors. Reference lists of published papers were also screened to identify additional articles.
2.2 |. Selection process
The study selection process is summarized by a PRISMA flowchart presented in Figure 1. The systematic literature search yielded a total of 1957 records after duplicates were removed. After screening titles and abstracts, another 1595 articles were excluded. The main reasons for exclusion at this step were: studies included non-ED samples, an educational article, a conference abstract, niche populations (e.g., athletes, individuals with diabetes), no accurate diagnosis, and sub-threshold EDs. After closer examination of full-text papers, 50 studies were included in the present review. Articles were primarly excluded for the following reasons: insufficient data to answer the proposed research questions (e.g., no description of the methodology used in an ED prevalence study), data were too narrow for answering the current research questions (e.g. the prevalence of hypercholesterolemia in anorexia nervosa), a review article, a case report, and samples did not include Japanese individuals.
FIGURE 1.
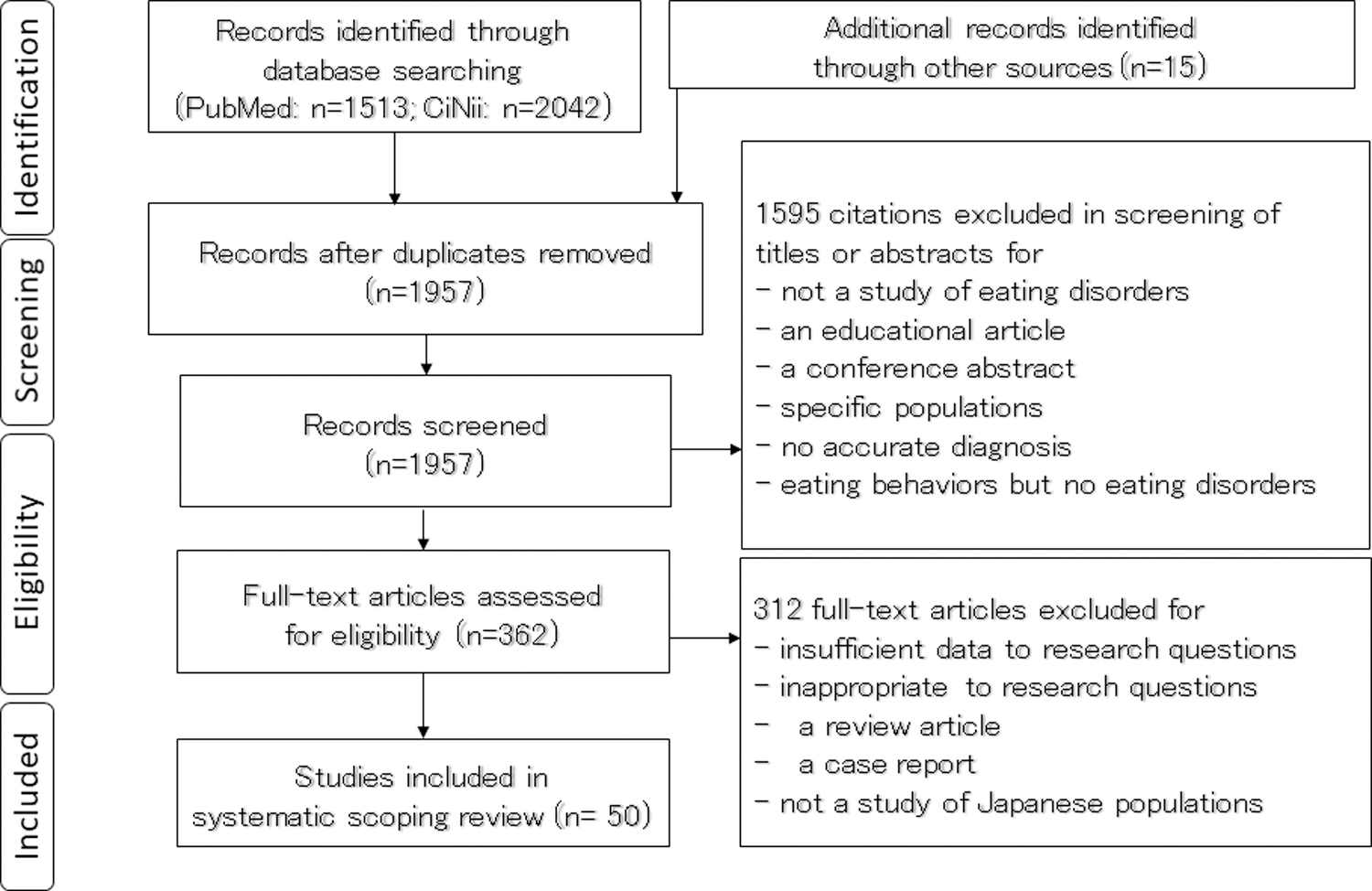
Literature screening process
2.3 |. Charting the data
Data were extracted from all included full-text articles and transferred into a spreadsheet that included information on: the authorship team, year of publication, written language, data collection period, classification tool, sample size, the age of participants, study design, and main findings. A comprehensive summary is presented in a Supplemental Table. Although not required for systematic scoping review articles (Tricco et al., 2018), we conducted a quality assessment to determine the level of bias in studies that met the criteria for the Oxford Centre for Evidence-Based Medicine (2009); this data is also presented in the Supplemental Table that accompanies this review.
3 |. RESULTS
The results of this review are classified according to three distinct time periods in Japanese history: before the Meiji Restoration (1700–1867), between the Meiji Restoration and the end of World War II (1868–1944), and after World War II (1945–2019).
3.1 |. The phenotypic expression of EDs between 1700 and 1867 (pre-Meiji Restoration)
Japanese medicine during the Edo period (1603–1867) mainly focused on Kampo, a simplified, positivistic, and pragmatic version of traditional Chinese medicine (Yu et al., 2006). The books on Kampo medicine were written in Chinese and usually published posthumously. During this time period, Kampo doctors documented cases of Fushoku-byo and Shinsen-ro, which were early ED presentations similar to our modern understanding of restrictive AN presentations (Kagawa; 1768; Tachibana, 1796). However, these doctors did not provide evidence explaining their rationale for classifying these health conditions as early forms of AN (Otsuka, 1955).
To further investigate the nature of these health conditions, Nakai and Nin (2020) compared Fushoku-byo and Shinsen-ro with the diagnostic criteria for feeding and EDs listed in the DSM-5 (American Psychiatric Association, 2013). According to these early Kampo reports, more than 90% of patients with with Fushoku-byo and Shinsen-ro were females, aged 15 to 40 years. All patients exhibited food restriction or avoidance that significantly impaired their physical health and/or psychosocial functioning. These symptoms lasted for months, and sometimes persisted for years. These findings are consistent with the clinical characteristics of feeding and EDs described in the DSM-5 (American Psychiatric Association, 2013). However, upon closer examination, it appears that there was a lot of heterogeneity in cases of Fushoku-byo and Shinsen-ro, such that cases could be classified into either modern AN or avoidant/restrictive food intake disorder (ARFID), as described in Western nosology. For instance, some patients with these conditions closely resembled those with AN during the Victorian era (Habermas, 2005; Keel & Klump, 2003), whereas other patients with Fushoku-byo and Shinsen-ro were similar in presentation to those with ARFID, as classified in the DSM-5 (Nakai & Nin, 2020). Interestingly, while internalization of a thin ideal of beauty has been identified as a robust risk factor for modern EDs (Habermas, 2005; Keel & Klump, 2003; Pike & Dunne, 2015), Kampo doctors did not document any fat phobia or distorted body image in these patients. Rather, they considered these disorders to be caused by psychological distress. These findings suggests that there may be multiple pathways to restrictive eating, depending on patients’ intentions (e.g., AN or ARFID). It is also possible that Fushoku-byo and Shinsen-ro could have been categorized as unspecified feeding or eating disorder (UFED), according to DSM-5 diagnostic criteria, due to an absence of fat phobia and body image concerns (Nakai & Nin, 2020).
Based on a historical review of eating pathology during the Edo period, providers documented approximately 50 cases of patients with Fushoku-byo and Shinsen-ro, when Japan was closed to the outside world (Mason & Caiger, 1997). Based on Kampo doctors’ reports, it is plausible that these disorders were early manifestations of AN and ARFID. These findings challenges early etiological theories of EDs which posit that the development of EDs in non-Western countries is mainly attributed to Western influences (Prince, 1985). In contrast, these findings are consistent with relatively recent literature indicating that AN is not a culturally-bound syndrome (Keel & Klump, 2003).
3.2. Sociocultural factors related to EDs between 1700 and 1867 (pre-Meiji Restoration)
Our systematic review reveals both similarities and differences in sociocultural factors related to EDs between the Edo period and the Victorian era. Similar to their Western counterparts (Habermas, 2005), early Japanese patients were typically from middle and upper class backgrounds and lived in urban environments (Nakai & Nin, 2020). In fact, both Japan and the United Kingdom experienced dramatic economic growth during this time period, which coincided with increased urbanization in both regions. One notable difference, however, was that in contrast to Western countries, Japan remained isolationist (Mason & Caiger, 1997).
Research has consistently documented how family influences and dynamics can contribute to the maintenance and treatment of an ED in both Western and non-Western populations (Cerniglia et al., 2017; Goel, Thomas, Boutte, Kaur, & Mazzeo, 2020)). For instance, providers documented interpersonal conflicts between mothers and daughters among patients with AN during the Victorian era (Vanderycken & van Deth, 1994). Of note, family dynamics may have looked different between the United Kingdom and Japan. For instance, during this time period, British families lived in nuclear households, whereas Japanese households primarily consisted of extended family systems (Mason & Caiger, 1997; Vanderycken & van Deth, 1994). Indeed, Kampo doctors conceptualized individuals’ illnesses as a specific manifestation of psychological distress caused by interpersonal conflict within extended family networks (Kagawa, 1768; Nakai & Nin, 2020; Otsuka, 1955). In this way, providers often attributed the cause of EDs during this time period to familial characteristics.
3.3 |. The phenotypic expression of EDs between 1868 and 1944 (post-Meiji Restoration)
In contrast to the Edo period, our review yielded minimal reports of EDs in Japan after the Meiji Restoration (Nogami, 1997). One book describing Oriental medical practices during this time period described case reports of six young female patients with Fushoku-byo, aged 15 to 23 years (Ohta, 1883). Besides this, no other report on EDs was found in medical journals between 1868 and 1940.
However, just before Japan’s involvement in World War II, Yamaguchi and Ogiwara (1941) published a paper describing two possible cases of AN. In their report, they discuss the symptoms of two young females, aged 13 and 20 years, who had significantly low weight (i.e., body mass index [BMI] < 13.0 kg/m2) due to restrictive eating. They were initially admitted for treatment for possible Simmonds’ disease, which presents similarly to AN (e.g., emaciation, amenorrhea in women). After reviewing the extant diagnostic criteria for both of these health conditions, they proposed a diagnosis of AN for these women (Yamaguchi & Ogiwara, 1941). However, it was common practice for doctors to diagnose patients presenting with these symptoms with functional Simmonds’ disease, rather than an ED.
3.4. Sociocultural factors related to EDs between 1868 and 1944 (post-Meiji Restoration)
Historically, in 1858, the Tokugawa (military) government revoked its isolationist policy, and opened Japan’s borders to the Western world. In 1868, the Tokugawa government was replaced by an imperialist state, headed by the Emperor Meiji. During the Meiji period, Japan implemented a policy of rapid industrialization, modernization, and Westernization in terms of lifestyle, including clothing, housing, and eating habits. Ironically, during this time period when Japan was undergoing rapid industrialization, there were few, if any, reports on EDs (Mason & Caiger, 1997; Ohta, 1883; Yamaguchi & Ogiwara, 1941). Again, these findings directly contradict early developmental theories of EDs, and provide further evidence that EDs can occur both in the absence and presence of Western influences (Keel & Klump, 2003; Prince, 1985).
In the spirit of Westernization, Western medicine was certified as the official form of medical practice after the Meiji Restoration (Mason & Caiger, 1997). As noted above, during this time period, doctors were continuously perplexed by the similar presentations between AN and Simmonds’ disease. Although these disorders had different causal mechanisms (e.g., intentional malnutrition vs. degradation of the pituitary glands), they yielded similar physiological effects, most typically emaciation (Perloff, Lasche, Nodine, Schneeberg, & Vieillard, 1954). Accordingly, it is likely that Japanese doctors practicing Western medicine often misdiagnosed AN as Simmonds’ disease (Yamaguchi & Ogiwara, 1941), further obfuscating our understanding of AN prevalence during this time period.
3.5 |. The phenotypic expression of EDs after 1945 (post World War II)
3.5.1. Descriptive studies
After World War II, providers documented multiple cases of patients with AN. These individuals were typically young women from middle and upper class backgrounds living in the Tokyo metropolitan area in the 1950s (Kaketa & Shimosaka, 1956; Masuda, 1952; Nishimaru, 1956; Yakata, 1951; Yamaguchi et al., 1956). During the 1960s, researchers were beginning to study the psychopathology of AN; however, their manuscripts were written in Japanese, which likely limited the reach of these findings to researchers beyond Japan (Ishikawa Iwata & Hirano, 1960; Kajiyama, 1959; Shimosaka, 1961). Shimosaka (1961) assessed ED psychopathology in 18 patients with AN who presented for treatment at hospitals in Tokyo. These patients mostly engaged in restrictive eating, with a few patients reporting restriction and self-induced vomiting. All patients exhibited fat phobia, however, they did not restrict for the purposes of achieving a thin figure.
During this time period, researchers also focused their efforts on examining how familial characteristics and dynamics within nuclear households may have contributed to AN. For instance, Ishikawa et al. (1960) assessed 18 female patients with AN and described these patients as having mothers who exerted high levels of control, coupled with fathers who were relatively passive. Similarly, Shimosaka (1961) hypothesized that certain parenting styles may induce identity conflicts within children, leading them to engage in dietary restriction as a possible coping strategy. For instance, Shimosaka (1961) consistently observed that his female patients had mothers who appeared protective and often intervened in their child’s life, possibly stifling their child’s ability to psychosocially mature and become independent. As such, Shimosaka (1961) speculated that such attitudes may disturb the ego development of children.
In addition to “typical” presentations of AN, researchers also documented “atypical” presentations of AN around in 1970. Aoki and colleagues (1976) documented cases of patients with AN who engaged in dietary restriction but did not display fat phobia; however, they did not document patients’ intentions for restricting their eating. Furthermore, these patients often complained of somatic symptoms related to ingestion, and did not report any difficulties negotiating their self-identity. Providers considered this form of AN to be a subtype of neurotic anxiety at this point in Japan’s history.
Providers observed an increase in patients with AN engaging in restriction as a motivation for food refusal after the 1970s (Nogami & Yabana, 1997). In addition to dietary restriction, Nogami (1973) documented seven cases of patients presenting with Kibarashi-gui in the Tokyo metropolitan area. This presentation, Kibarashi-gui, was heterogeneous, such that patients could be classified into three probable DSM-5 groups: those with binge eating/purging-type of AN (AN-BP), bulimia nervosa (BN), and binge-eating disorder (BED) (American Psychiatric Association, 2013; Nogami, 1977). Notably, all of these patients experienced binge eating; however, they differed in terms of weight status (e.g., low weight vs. high weight) and additional ED symptoms (e.g., presence or absence of self-induced vomiting). Providers witnessed a marked increase in patients who engaged in binge eating and purging behaviors, such as those with AN-BP and BN, after the 1980s (Kasahara et al., 1985). However, patients presenting with only binge eating (e.g., BED) were not common until the late 1990s (Nakai et al., 2014a; Nakai et al., 2018).
3.5.2. Epidemiological studies with clinical samples
In response to the increase in AN diagnoses, the Ministry of Health and Welfare established a research group in 1980 dedicated to assessing the prevalence and etiology of EDs in Japan (Suematsu, Ishikawa, Kuboki, & Ito,). As such, national surveys of EDs were periodically conducted in hospitals throughout 1980–1981, 1992, 1998, and 2014–2015 (Ando, 2017; Kuboki Nomura, Ide Suematsu & Araki, 1996; Suematsu et al., 1985; Tamaki, Ohno, Kawamura, Hashimoto, & Nagai, 2002). The survey administered in 1980 was the first recorded epidemiological study of EDs in Japan (Suematsu et al., 1985). In this survey, the yearly incidence of AN was fairly low (see Table 1). Furthermore, only 20% of patients displayed features of “typical AN,” such that they met the original diagnostic criteria developed by the Ministry of Health and Welfare’s research group on EDs (Suematsu et al., 1985). Interestingly, 26.5% of patients did not have fat phobia, similar to “non-fat phobic” AN observed throughout other parts of Asia (Pike & Dunne, 2015).
Table 1.
Yearly incidence of eating disorders in medical facilities in Japan
| Year | 1980–1981 | 1992 | 1998 | 2014–15 | 2005 | 2005 |
|---|---|---|---|---|---|---|
| Area of survey conducted | Japan | Japan | Japan | Japan | Kyoto | Kyoto |
| Target medial facilities | Hospitals (> 300beds) | Hospitals (> 200beds) | Hospitals (categorized) | Hospitals (categorized) | Hospitals (categorized) | All facilities (categorized) |
| Number of facilities | 1,030 | 5,057 | 23,401 | 5,220 | 24 | 45 |
| Recovery rate (%) | 33.0 | 37.4 | 61.0 | 49.1 | 55.0 | 51.5 |
| Diagnostic criteria | OCA | rev OCA | DSM-IV | DSM-5 | DSM-IV | DSM-IV |
| Anorexia nervosa | ||||||
| Estimated number | 2,900 | 4,500 | 12,600 | 12,674 | 242 | 422 |
| General population (per 105) | 2.5 | 3.6 | 10.0 | 10.0 | 9.1 | 17.0 |
| Female (aged 10–29; per 105) | 16.2 | 21.8 | 76.4 | 105.6 | 79.1 | 140.7 |
| Bulimia nervosa | ||||||
| Estimated number | 1600 | 6,500 | 4,612 | 144 | 481 | |
| General population (per 105) | 1.3 | 5.1 | 3.6 | 5.4 | 19.5 | |
| Female (aged 10–29; per 105) | 7.8 | 39.4 | 38.4 | 47.1 | 160.3 | |
| Binge eating disorder | ||||||
| Estimated number | 1145 | |||||
| General population (per 105) | 0.9 | |||||
| Female (aged 10–29; per 105) | 9.5 | |||||
| Other eating disorders | ||||||
| Estimated number | 4,200 | 6,075 | 33 | 177 | ||
| General population (per 105) | 3.3 | 4.8 | 1.2 | 7.2 | ||
| Female (aged 10–29; per 105) | 25.5 | 50.6 | 10.8 | 59.0 | ||
| Eating disorders | ||||||
| Estimated number | 23,200 | 24,506 | 419 | 1,080 | ||
| General population (per 105) | 18.3 | 19.3 | 15.8 | 43.8 | ||
| Female (aged 10–29; per 105) | 140.6 | 204.2 | 136.9 | 360.0 | ||
OCA: Original criteria for AN, rev OCA: Revised version of original criteria for AN, categorized: categorized by the number of hospital beds
The latter epidemiological surveys revealed different trends in ED presentations across Japan, such that the yearly incidence of AN and BN increased dramatically in 1998, and then stabilized by 2015 (Table 1). However, the prevalence estimates of BN and BED were extremely low in these national surveys (Table 1). As stated above, these surveys were conducted in hospital settings; however, many patients with BN and BED visited outpatient clinics in Japan (Nakai, 2005). Accordingly, in 2005, researchers conducted a similar survey in all the relevant medical facilities throughout Kyoto to provide more accurate estimates of BN and BED prevalence during this time frame (Nakai et al., 2009). Results indicate that, indeed, the national surveys vastly underestimated the yearly incidence of BN (see Table 1). Thus, it is important to interpret the overall findings from the national surveys with caution, given that they differed dramatically in terms of the selection process of hospitals, and utilized differing ED diagnostic criteria depending on when the survey was administered (see Table 1).
Given these methodological issues, Nakamura et al. (2000) conducted a survey in 1997 to examine the rates of AN and BN in all the relevant medical facilities across Niigata. They found that the estimated point prevalence of AN and BN were 2.65 and 0.52 per 100,000 individuals in the general population, respectively (Nakamura et al., 2000). These statistics suggest that, in contrast to patterns observed in the West (Keel & Klump, 2003), the likelihood of developing AN in Japan is four to five times greater than developing BN. These statistics are often cited as representative prevalence estimates for AN and BN in Japan (Chisuwa & O’Dea, 2010; Galmiche, Dechelotte, Lambert, & Tavolacci, 2019; Keel & Klump, 2003; Makino et al., 2004; Pike & Dunne, 2015). However, these estimates are remarkably lower than the yearly incidence of AN (10.0 per 100,000 general population) and BN (5.1 per 100,000 general population) reported in the national survey conducted in 1998 (Tamaki et al., 2002; see Table 1). This discrepancy may be attributed to two reasons: (a) Nakamura and colleagues (2000) collected data over five days, which were misinterpreted as yearly incidences, and (b) potential regional differences in the prevalence of AN and BN.
3.5.3. EDs in males
During this time period, there have been a few studies that have examined ED presentations among males. Among clinical ED samples, approximately 2.1–5.2% of patients are estimated to be males (Edakubo & Fushimi, 2020; Harada et al., 2016; Nakai et al., 2001; Nakai et al., 2018). While researchers have not identified any significant differences in clinical features between male and female patients with AN (Harada et al., 2016), male patients have a higher mortality rate than their female counterparts. For instance, Edakubo & Fushimi (2020) assessed a mixed-gender sample of patients with AN in acute hospital settings, and found that the adjusted odds ratio of mortality for male patients was two times greater than female patients with AN.
3.5.4. ARFID and BED
In 2013, the DSM-IV (American Psychiatric Association, 1994) was replaced by the DSM-5 (American Psychiatric Association, 2013). The DSM-5 made significant changes to ED diagnostic criteria, and formally included ARFID and BED as distinct diagnoses. Importantly, the DSM-5 remarkably reduced the number of diagnoses in the residual category (e.g., distinguishing between other specified feeding or eating disorder [OSFED] and UFED, both of which were formerly collapsed into EDNOS), which allowed Japanese clinicians to more effectively differentiate between ED diagnostic groups (Nakai et al., 2013; Nakai et al., 2017b).
Although only formally recognized by Western nosology in the last decade, Japanese researchers identified probable cases of ARFID in Kyoto as early as 1963 (Nakai et al., 2018). Despite an absence of ARFID cases in the 2014–15 national survey, there have been a few studies examining the prevalence of ARFID in Japan since the mid-20th century. In one study conducted by Nakai and colleagues (2016b), they examined the prevalence of ARFID among a sample of adult patients presenting with DSM-5 EDs. Of the 1029 patients sampled, 95 patients (9.2%) met the criteria for ARFID. Compared to patients with AN, the ARFID group had a shorter illness duration, lower admission history, lower rates of comorbid anxiety disorders, and less severe psychopathology (Nakai, Nin, Noma, Teramukai, & Wonderlich, 2016b). They also reported significantly better treatment outcomes than the AN group (Nakai et al., 2017a). These findings were confirmed by another study, in which researchers conducted a retrospective chart review of hospitalized children and adolescents diagnosed with ARFID and AN restricting-subtype (AN-R) (Kurotori et al., 2019). The recovery rate of the ARFID group was significantly higher than that of the AN-R group. In comparison to their Western counterparts, (Strand, von Hausswolff-Juhlin, & Welch, 2018), these Japanese patients with ARFID were more likely to be women, and experienced better treatment outcomes.
In Japan, the number of patients with BED has markedly increased (Nakai et al., 2014a; Nakai et al., 2018). One study found that, of 251 patients presenting with DSM-5 EDs in a Kyoto clinic, 69 patients (27.5%; 67 women, 2 men) met the criteria for BED (Nakai & Nin, 2016a). Nearly all of these patients (n=67, 97.1%) had a BMI < 30 kg/m2 and experienced psychiatric comorbidities, such as mood and anxiety disorders. Additionally, a majority of these patients (n=59, 85.5%) experienced medical complications, such as dyslipidemia and hypertension. Nearly half of all cases (n=38, 55.1%) had a past history of an ED, such as AN and BN, indicating high rates of diagnostic migration. Notably, all of the female patients (n=67) displayed fat phobia, potentially due to rapid weight gain as a result of frequent binge eating episodes. However, unlike their counterparts with AN and BN, they were not unduly influenced by body shape and weight, suggesting other possible functions of binge eating.
3.5.5. Epidemiological studies with non-clinical samples
In addition to national surveys with clinical samples, other research groups have conducted surveys targeting non-clinical samples and different age groups (e.g., adolescents vs. adults). In studies conducted with adolescents, researchers employed a two-stage screening approach. This two-stage screening approach provides a more comprehensive method for identifying the true prevalence of EDs in a given country (Hoek & van Hoeken, 2003). Researchers used a selection criterion of a BMI < 17.5 kg/m2 for the first stage screening for AN, because the sensitivity and specificity of the Eating Attitudes Test (EAT; Garner & Garfinkel, 1979) were poor for the diagnosis of AN in Japanese samples (Hisamatsu et al., 2000). During the second stage of screening, ED specialists conducted clinical interviews with participants who met this low weight criterion to further evaluate their symptoms.
In 1983 and 1993, researchers followed this two-step approach in order to assess the prevalence of AN in Japanese adolescents (Azuma, 1984; Fujita et al., 1994; Mizuno, Makita, Yamaguchi, Ishii & Mizushima, 1986; Mizushima & Ishii, 1983; Nakai, 1984; Ohzeki, 1984). Table 2 shows regional differences in the point prevalence of AN in female adolescents across various prefecture (e.g., districts) in Japan. Namely, there were low AN prevalence in prefectures with low population densities (e.g., Fukui, Tottori, Shimane), and higher prevalence in prefectures with greater population densities (e.g., Kyoto and Kanagawa). Within Kyoto, 0.42% of female high school students living in the southern area had AN, whereas only 0.04% reported AN in the northern area (Azuma, 1984; Nakai, 1984). In another national survey assessing EDs in adolescents, researchers interviewed Yogo-teachers (i.e., school nurse/health science teachers) in seven Japanese prefectures in 2010–2013 (Hotta et al., 2015). Kamiya and Suematsu (2017) focused their efforts specifically on the Aichi prefecture, observing that the prevalence of AN was particularly high among students attending prestigious high schools. In sum, findings from these reports indicate that the point prevalence of AN was across prefectures remained relatively stable across time (see Table 2).
Table 2.
Point prevalence of anorexia nervosa in adolescents in Japan
| A. Elementary school (aged 10 and 12 years) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Survey year | Prefecture | Female |
Male |
Diagnostic criteria | Rank P, D | Ref | ||
| Sample size | Prevalence | Sample size | Prevalence | |||||
| 2010 | Tokyo | 5,793 | 0.09% | 5,727 | 0.02% | DSM-IV | 1, 1 | 1 |
| 2011 | Kumamoto | 9,857 | 0.01% | 10,234 | 0.00% | DSM-IV | 23, 27 | 1 |
| 2012 | Nagano | 17,375 | 0.09% | 18,388 | 0.02% | DSM-IV | 16, 38 | 1 |
| 2012 | Miyazaki | 2,156 | 0.00% | 2,207 | 0.00% | DSM-IV | 36, 39 | 1 |
| 2013 | Hiroshima | 8,809 | 0.10% | 9,072 | 0.02% | DSM-IV | 12, 17 | 1 |
| 2013 | Yamaguchi | 7,048 | 0.07% | 7,186 | 0.00% | DSM-IV | 25, 28 | 1 |
| B. Junior high school (aged 12 and 15 years) | ||||||||
| Survey year | Prefectures | Female |
Male |
Diagnostic criteria | Rank P, D | Ref | ||
| Sample size | Prevalence | Sample size | Prevalence | |||||
| 1981 | Ishikawa | 21,153 | 0.03% | 22,235 | 0.00% | OCA | 33,32 | 2 |
| 1983 | Fukui | 12,674 | 0.00% | 12,926 | 0.01% | OCA | 45, 36 | 3 |
| 1983 | Kyoto | 5,005 | 0.23% | 4,496 | 0.00% | OCA | 11, 9 | 4 |
| 1983 | Tottori | 6,712 | 0.06% | 7,160 | 0.00% | OCA | 47, 40 | 5 |
| 1983 | Shimane | 11,328 | 0.10% | 11,991 | 0.00% | OCA | 46, 45 | 5 |
| 1993 | Kanagawa | 2,525 | 0.32% | rev OCA | 3,3 | 6 | ||
| 1993 | Tottori | 10,906 | 0.08% | 11,464 | 0.00% | rev OCA | 47,37 | 6 |
| 1993 | Shimane | 12,872 | 0.06% | 13,123 | 0.00% | rev OCA | 46,43 | 6 |
| 2010 | Tokyo | 6,800 | 0.22% | 6,407 | 0.02% | DSM-IV | 1, 1 | 1 |
| 2011 | Kumamoto | 15,379 | 0.11% | 16,218 | 0.00% | DSM-IV | 23, 27 | 1 |
| 2012 | Nagano | 27,480 | 0.17% | 28,889 | 0.02% | DSM-IV | 16, 38 | 1 |
| 2012 | Miyazaki | 1,006 | 0.10% | 1,062 | 0.00% | DSM-IV | 36, 39 | 1 |
| 2013 | Hiroshima | 13,071 | 0.25% | 13,451 | 0.02% | DSM-IV | 12, 17 | 1 |
| 2013 | Yamaguchi | 10,821 | 0.12% | 11,171 | 0.00% | DSM-IV | 25, 28 | 1 |
| 2013 | Hokkaido | 27,141 | 0.11% | 27,932 | 0.02% | DSM-IV | 8, 47 | 1 |
| C. Senior high school (aged 15 and 18 years) | ||||||||
| Survey year | Prefecture (PR) | Female |
Male |
Diagnostic criteria | Rank P, D | Ref | ||
| Sample size | Prevalence | Sample size | Prevalence | |||||
| 1983 | Ishikawa | 15,250 | 0.06% | 15,285 | 0.01% | OCA | 33, 32 | 2 |
| 1986 | Fukui | 15,594 | 0.05% | 11,911 | 0.00% | OCA | 45, 36 | 3 |
| 1984 | Kyoto | 36,581 | 0.21% | 23,000 | 0.00% | OCA | 11, 9 | 4 |
| 1993 | Kyoto | 20,598 | 0.34% | 1,659 | 0.00% | rev OCA | 12, 9 | 6 |
| 2010 | Tokyo | 66,084 | 0.21% | 44,196 | 0.01% | DSM-IV | 1, 1 | 1 |
| 2011 | Kumamoto | 15,381 | 0.25% | 17,543 | 0.03% | DSM-IV | 23, 27 | 1 |
| 2011 | Nagano | 7,629 | 0.20% | 6,923 | 0.00% | DSM-IV | 16, 38 | 1 |
| 2012 | Miyazaki | 12,630 | 0.10% | 13,148 | 0.01% | DSM-IV | 36, 39 | 1 |
| 2013 | Hiroshima | 8,455 | 0.47% | 6,734 | 0.02% | DSM-IV | 12, 17 | 1 |
| 2013 | Yamaguchi | 11,541 | 0.23% | 11,610 | 0.05% | DSM-IV | 25, 28 | 1 |
| 2013 | Hokkaido | 29,419 | 0.14% | 28,391 | 0.01% | DSM-IV | 8, 47 | 1 |
| 2013 | Aichi | 60,850 | 0.13% | 60,069 | 0.01% | DSM-IV | 4, 5 | 7 |
Survey was conducted by the two-stage screening approach or by Yogo-teachers (school nurse/health science teachers), P: Rank of population, D: Rank of population density, OCA: Original criteria for AN, rev OCA: Revised version of original criteria for AN (modified DSM-III-R), Ref: Reference
There have been a few studies on the prevalence of BN and related disorders in non-clinical samples in Japan. Most of them only consisted of administering self-report questionnaires (Kiriike et al., 1988; Nakai et al., 2014a; Nogami, Yamaguchi, Ishiwata, Sakai, & Kusakabe, 1984; Takeda, Suzuki, & Matsushita, 1983). To the best of our knowledge, only one study conducted clinical interviews with their sample. Hisamatsu and colleagues (2000) interviewed 357 female college students in Tokyo and used DSM-IV criteria (American Psychiatric Association, 1994) to estimate the prevalence of AN, BN, and eating disorder not otherwise specified (EDNOS) for the sample. Findings reveal that 1.4% had AN, 1.4% had BN, and 8.7% had EDNOS (Hisamatsu et al., 2000).
3.5.6. Time trends in EDs
Clinical Samples
Of the 50 articles included in this systematic scoping review, a few (e.g., Nadaoka et al.,1996; Nakai et al, 2014a; Nakai et al, 2018) focused on mapping the occurrence of EDs in Japan overtime. In addition to the national surveys described above, Nadaoka et al. (1996) examined 97 patients diagnosed with DSM-III-R EDs at Yamagata University Hospital from 1978–1992 (American Psychiatric Association, 1987). Findings from this study reveal that ED cases quadrupled during 1988–1992, suggesting a marked increase in the number of referrals and diagnoses of EDs over the course of nearly two decades. In addition, Nakai and colleagues (2018) assessed the prevalence and symptomatology of patients presenting for treatment at Kyoto University Hospital between 1963 and 2004. In order to facilitate comparisons, researchers retrospectively assigned DSM-5 ED diagnoses to each patient, when applicable. Patients were categorized based on their admission dates: 1963–1974 (n=26), 1975–1984 (n=97), 1985–1994 (n=540), and 1995–2004 (n=700). Comparisons revealed that the proportion of AN and ARFID decreased across the four time periods, while the proportion of BN and BED cases increased over time. Additionally, the occurrence of fat phobia, body image concerns, binge eating, and purging behaviors increased over time. Interestingly, all patients with AN in the 1960s (n=11) experienced fat phobia and body image concerns; however, none of them engaged in dietary restriction for the purpose of reducing their weight. Notably, AN presentations that were characterized by both fat phobia and dietary restriction for the purpose of achieving slimness, did not occur until the early 1970s. However, the incidence and prevalence of this form of AN increased steadily after the 1970s.
Non-clinical Samples
Nakai et al. (2014a) examined DSM-IV ED symptoms and prevalence among Japanese female students living in the Kyoto prefecture during 1982, 1992, and 2002. Their sample consisted of 10,499 girls and young women, aged 16 to 23 years. Findings indicate that there were significant increases in a fear of weight gain, body dissatisfaction, and maladaptive eating behaviors, such as binge eating and purging behaviors, over this time period. Similarly,, AN, BN, and EDNOS prevalence significantly increased from 1982 to 2002.
Interestingly, despite findings from the national report conducted in 2014–15 indicating low annual incidence rates of BED and no cases of ARFID at hospitals, teachers working with children and adolescents (e.g., elementary school–high school) have reported encountering multiple cases of ARFID and BED amongst their pupils during this time (Seike et al., 2016a, 2016b). This suggests that patients with these disorders avoid professional help or that clinicians in hospitals are unaware of these disorders in Japan. In conjunction with the findings from the Nakai et al. (2014a) study, this may suggest that youth are particularly susceptible to experiencing ED symptoms, but may be less likely to present for treatment at hospital settings.
3.6. Sociocultural factors related to EDs after 1945
3.6.1. National Food Crisis
After World War II, Japan experienced an urban food crisis, resulting in rationing and food insecurity for many citizens (Vardaman, 2006). However, with the stimulus of quick profits from war orders in the Korean peninsula from 1950 to 1953, Japanese industry was at the point of full recovery by 1955 (Vardaman, 2006). During this immediate period following the Second World War, ED cases consisted primarily of AN, and patients were usually wealthy young women living in metropolitan Tokyo (Vardaman, 2006). These patients presented with fat phobia; however, they did not report a desire to be thin. Notably, restriction for the purpose of achieving a thin figure was not common around 1960, mainly due to limited food supplies and differing beauty standards (Hashimoto, 2010). For instance, there were no dieting advertisements in women’s magazines in the 1950s and the 1960s (Morohashi, 1993). Similar to other time periods, psychiatric researchers conceptualized familial characteristics related to the nuclear family as possible etiological factors in the development of AN (Ishikawa et al., 1960; Shimosaka, 1961).
3.6.2. Gender Roles
In 1947, a new law was passed that granted women more rights as citizens, including the right to vote, own property, and inherit property – all of which reflected changing gender norms during this time period. However, these progressive national policies were slow to trickle down to everyday families, such that many traditional gender roles persisted at home. Most women, for instance, were tasked with maintaining their household and attending to children, whereas men were expected to work and maintain their family’s income (Vardaman, 2006). These gender dynamics were reflected in parenting practices, such that mothers were usually considered controlling, whereas fathers were viewed as passive. Indeed, Ishikawa and colleagues (1960) noted these same characteristics amongst families presenting for ED treatment, in which young patients usually came from backgrounds where their mother was described as domineering, and their fathers as relatively permissive (Vardaman, 2006).
3.6.3. Westernization
In 1967, Japanese beauty standards begin to shift after Twiggy, an iconic British model known for her extraordinarily thin figure, visited Japan. After this event, many women’s magazines began to feature more Western-oriented fashion trends and beauty ideals, including an emphasis on a slim physique as the standard of beauty for women (Morohashi, 1993). These ideals became perpetuated further in the form of television shows and movies (Vardaman, 2006). By the 1970s, slimness had become the dominating standard of beauty for Japanese women, and dieting became socially encouraged as a standard method of weight loss (Nakai et al., 2014a).
During this same time, the food environment dramatically changed in Japan, making Western, processed, high-fat foods more readily accessible to Japanese citizens (Ministry of Health, Labor, and Welfare, 2003). For instance, beginning in the 1970s, these types of food were offered at convenient locations that were open throughout the day (e.g., convenience stores, vending machines) (Nakai et al., 2018; Vardaman, 2006). As such, the rates of Japanese adults with overweight steadily increased after the 1980s. Conversely, during this same time period, the rates of young adult women with underweight also increased, reflecting changing beauty ideals (Morohashi, 1993; Nakai et al., 2014a). These paradoxical social messages of encouraging women to lose weight, while simultaneously being surrounded by a changing food environment composed of high-calorie foods, may have contributed to the increase in patients with binge/purge presentations (i.e., AN-BP, BN) after the 1980s (Nakai et al., 2014a; Nakai et al., 2018). A similar phenomena in which individuals are pressured to both lose weight for health reasons while subjected to a pervasive diet culture promoting unhealthy weight regulation strategies has been observed in the West (Taylor, Fitzsimmons-Craft, & Goel, 2018). Furthermore, as EDs became more common in the 1980s, they began to affect individuals across all socioeconomic statuses (Nakai et al., 2018).
In general, EDs became increasingly more common in the 1980s, and there was a steep rise in the late 1990s (Ando, 2017; Nakai et al., 2014a; Tamaki et al., 2002). This increase may be attributable to increased attention to gender inequalities during this period. For instance, women experienced vast gender-based discrimination throughout the latter half of the 20th century, and this only intensified after an economic recession in 1990 (Vardaman, 2006). Furthermore, as Western norms, ideas, and values became increasingly commonplace within Japanese culture, many Japanese women experienced conflicts reconciling Western, individualistic values with Eastern, collectivistic values (Pike & Borovoy, 2004). These cultural-value conflicts have been identified as correlates of eating pathology in other Asian groups (Mustafa, Zaidi, & Weaver, 2017; Reddy & Crowther, 2007; Yu, Pope, & Perez, 2019).
4 |. DISCUSSION
This systematic scoping review charted the changing profile of EDs and their related sociocultural factors in Japan over the course of 300 years. While most reviews including ED data from Japan cite 1980 as the first time when EDs were observed in this nation, this review demonstrates that EDs were first reported as early as the 18th century, prior to modernization (Kagawa, 1768). This review synthesized findings from Chinese, Japanese, and English texts in order to provide a comprehensive overview of the emergence of EDs in Japan and changing trends in EDs, as well as describe how sociocultural influences may have contributed to the rise of EDs during particular time periods throughout Japanese history.
4.1. Tracking ED prevalence over time
To identify and understand these trends, findings were classified according to three distinct time periods: before the Meiji Restoration (1700–1867), between the Meiji Restoration and the end of World War II (1868–1944), and after World War II (1945–2019). During this first historical time period, Kampo doctors documented more than 50 cases of patients who engaged in restrictive eating, but did not express fat phobia or body image concerns (Nakai & Nin, 2020). Notably, when reviewing these reports, Nakai and Nin (2020) determined that these early presentations resemble modern AN and ARFID. Collectively, these early reports indicate that EDs characterized by restriction were present in Japan prior to Westernization and modernization, providing further support that fat phobia is not a necessary precursor to the development of EDs (Becker, Thomas & Pike, 2009; Wildes, Emery & Simons, 2001), and that AN is not a culturally-bound syndrome (Keel & Klump, 2003).
In contrast to the 18th and early 19th centuries, there exists only a few reports of EDs while Japan underwent rapid industrialization and Westernization after 1868. However, due to the adoption of Western medicine during this time, it could be that many true cases of EDs, especially AN, were mistakenly diagnosed as Simmonds’ disease, which presents similarly (e.g., emaciation). In 1960, AN appeared to only affect young, wealthy women (Shimosaka, 1961). While these women presented with fat phobia, “non-fat phobic” AN did not express a desire to lose weight. At this point in time, this “non-fat phobic” AN was conceptualized as a manifestation of anxiety (Aoki et a., 1970). Similar cases of “non-fat phobic” AN have been documented throughout Asia, including Hong Kong, Malaysia, and the Indian subcontinent (Becker et al., 2009; Pike & Dunne, 2015).
Beginning in the early 1970s, researchers began documenting cases of “typical” AN manifestations characterized by fat phobia and restriction with the purpose of achieving thinness (Nakai et al., 2018). Additionally, with the changing food landscape and increased focus on reducing overweight in the 1980s, providers also witnessed a rise in patients presenting with binge/purse symptomology (Nakai et al., 2018). Thus, in contrast to patients with restrictive EDs during the Edo period prior to the Meiji restoration, the number of patients with AN-BP and BN increased during the latter half of the 20th century, possibly due to shifting beauty ideals and accessibility to high-fat, Western foods. Interestingly, the incidence of EDs, particularly BN and BED, further increased after the 1990s. This is inconsistent with trajectories from other countries, where the prevalence of AN usually stabilizes, while BN decreases overtime (Hoek & van Hoeken, 2003; Tseng, Tu, Hsieh, & Chang, 2020). During this time, researchers attributed these trends to gender-based discrimination, and women attempting to negotiate between different cultural values (Nakai et al., 2018).
After the Second World War, similar to Western countries, Japan observed high prevalence of patients with AN in the 1950s, followed by increases in patients with BN and BED in the 1970s and the 1980s. In addition to charting changes in the incidence and prevalence of particular EDs across Japan, this review also highlights significant regional differences in how these EDs manifest. For instance, EDs tend to be lower in sparse regions along the Japan Sea coast, such as Niigata, Tottori and Shimane, compared with high-density regions along the Pacific side, such as Tokyo, Kanagawa, and Kyoto. As such, it may be misleading to generalize ED prevalence estimates across Japan; rather, researchers should aim to further investigate the possible reasons for these stark differences.
4.2. Reconciling the Issue of “Atypical” and “Typical” Presentations of AN
Throughout Japanese history, Kampo doctors and Western medical doctors alike have documented varying forms of AN. However, despite recommendations to do so (e.g., Becker et al., 2009), the DSM-5 does not currently include guidance for how to classify “atypical” forms of AN that consist of dietary restraint in the absence of fat phobia or weight/shape concerns. Within the OSFED category, for instance, the DSM-5 recognizes only one form of “atypical AN,” which is reserved for individuals who meet all diagnostic criteria for traditional AN except that their weight is within or above the BMI normal range (American Psychiatric Association, 2013). However, Japanese women have presented with “atypical” forms of AN along with more “typical” manifestations of AN since the latter half of the 20th century (Nakai & Nin, 2020). Furthermore, Nakai and colleagues (2014b) have provided further evidence suggesting that these presentations are distinct syndromes that vary in terms of ED psychopathology (Becker et al., 2009). As stated elsewhere, these atypical, “non-fat phobic” presentations of AN are also common in other Asian populations (e.g. Pike & Dunne, 2015), possibly pointing to cultural factors that may make this presentation more prevalent in these regions. Thus, we encourage future researchers to continue to investigate these nuanced AN presentations in Japanese populations, as well as potentially consider acknowledging these syndromes within future iterations of the DSM and other psychiatric texts. Maintaining the status quo may preclude proper diagnosis and recognition of these disorders in Japanese samples living both within and outside of Japan.
4.3. Strengths & Limitations
This is the first systematic scoping review to provide a comprehensive overview of ED presentations in Japan. Strengths of this study include: inclusion and interpretation of texts written in languages other than English (e.g., Chinese and Japanese), a rigorous methodological design guided by extended PRISMA guidelines for scoping reviews, and assessment of EDs within non-White, Western samples. However, this review should be interpreted within the context of its limitations. Many of the studies that were surveyed in this review included data from self-report questionnaires, rather than clinical interview data. Furthermore, our findings are primarily based on cross-sectional data, rather than prospective data. Further, given the nature of this review, such that we assessed reports dating back as early as the 18th century, the quality of our interpretations, and those of other researchers who conducted retrospective analyses on these case reports, is dependent upon the quality of the original clinical documentation. Thus, findings dating back to the Edo period, for instance, should be interpreted with caution.
While it is a general strength that researchers have conducted multiple national, epidemiological surveys in Japan, these surveys often targeted hospitals and used differing ED diagnostic criteria. However, findings from other studies included in this review suggest that patients with BN and BED, for instance, may not present to traditional hospital settings, obfuscating our full understanding of the actual prevalence estimates of these health conditions. As such, we encourage future researchers to conduct a rigorous, population-based survey to reassess the current prevalence of EDs across diverse medical, community, and school settings in Japan.
4.3. Conclusions
This is the first systematic scoping review documenting the prevalence, incidence, and sociocultural correlates of EDs in Japan from 1700 to 2020. Findings reveal that (a) restrictive EDs were present as early as the 18th century; (b) Japanese patients may present with both “typical” and “atypical” forms of AN; (c) ED symptoms can persist in the absence of Western influence; and (d) sociocultural factors, such as an emphasis on thinness, pressures associated with traditional gender roles, a shifting food environment, and family dynamics, may contribute to EDs for Japanese populations. Future research should continue to investigate EDs within Japan, with a particular emphasis on advancing our understanding of the true prevalence estimates of EDs (especially BN, BED, and ARFID), identifying possible biological and cultural correlates of EDs for these groups, and developing culturally-responsive treatments for at-risk groups, such as school children and young women.
Supplementary Material
Footnotes
CONFLICT OF INTEREST
The authors confirm there are no conflicts of interest.
REFERENCES
- American Psychiatric Association, (1987). Diagnostic and Statistical Manual of Mental Disorders (3rd rev ed.). Washington, DC.: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association, (1994). Diagnostic and Statistical Manual of Mental Disorders (4th ed.). Washington, DC.: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association, (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, DC.: American Psychiatric Association. [Google Scholar]
- Ando T (2017). Research on the guideline for the improvement of medical care system of eating disorders—An interim result of the national survey of eating disorders. In: Ando T (Ed.), Report of the research on the improvement of medical care system of eating disorders. (pp.29–40). The Ministry of Health, Labor and Welfare, Tokyo, Japan: (in Japanese). [Google Scholar]
- Aoki H, Suematsu H, Esaki M, Kurokawa N, Tamai H, Takesue T, & Tohyama N (1976). A psychosomatic consideration of pathoplastic mechanisms in anorexia nervosa. Japanese Journal of Psychosomatic Medicine, 16, 30–38 (in Japanese). [Google Scholar]
- Azuma T (1984). The epidemiology of anorexia nervosa in public senior high school students in Kyoto prefecture. In: Research group for eating disorders (Ed.), Annual report of anorexia nervosa. (pp.40–46). The Ministry of Health and Welfare, Tokyo, Japan: (in Japanese). [Google Scholar]
- Becker AE, Thomas JJ, & Pike KM (2009). Should non-fat phobic anorexia nervosa be included in the DSM-V? International Journal of Eating Disorders, 42, 620–635. 10.1002/eat.20727 [DOI] [PubMed] [Google Scholar]
- Cerniglia L, Cimino S, Tafa M, Marzilli E, Ballarotto G, & Bracaglia F (2017). Family profiles in eating disorders: Family functioning and psychopathology. Psychology Research and Behavior Management, 10, 305–312. 10.2147/PRBM.S145463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisuwa N, & O’Dea JA (2010). Body image and eating disorders amongst Japanese adolescents. A review of the literature. Appetite, 54, 5–15. [DOI] [PubMed] [Google Scholar]
- Cummins L, Simmons A, & Zane N (2005). Eating disorders in Asian populations: A critique of current approaches to the study of culture, ethnicity, and eating disorders. American Journal of orthopsychiatry, 75, 553–574. [DOI] [PubMed] [Google Scholar]
- Edakubo S, & Fushimi K (2020). Mortality and risk assessment for anorexia nervosa in acute-care hospitals: a nationwide administrative database analysis. BMC Psychiatry, 20, 19, doi: 10.1186/s12888-020-2433-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita T, Inaba H, Sasaki D, Nakai Y, Azuma T, Mizushima N, … Ishida Y (1994). The epidemiology of anorexia nervosa and bulimia nervosa in junior and senior high school students in Japan. In: Research group for eating disorders (Ed.), Annual report of anorexia nervosa. (pp.30–33). The Ministry of Health and Welfare, Tokyo, Japan: (in Japanese). [Google Scholar]
- Galmiche M, Dechelotte P, Lambert G, & Tavolacci MP (2019). Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. American Journal of Clinical Nutrition, 109, 1402–1413. [DOI] [PubMed] [Google Scholar]
- Garner DM & Garfinkel PE (1979). The Eating Attitudes Test: An index of the symptoms of anorexia nervosa. Psychological Medicine, 9, 273–279. [DOI] [PubMed] [Google Scholar]
- Goel NJ, Thomas B, Boutte RL, Kaur B, & Mazzeo SE (2020). Body image and eating disorders among South Asian American women: What are we missing? Manuscript under review. [DOI] [PubMed]
- Habermas T (2005). On the uses of history in psychiatry: Diagnostic implications for anorexia nervosa. International Journal of Eating Disorders, 38, 167–182. [DOI] [PubMed] [Google Scholar]
- Harada T, Yamauchi T, Kodama Y, Miyamoto S, Kiriike N, & Inoue K (2016). Clinical features of Japanese males with anorexia nervosa. Osaka City Medical Journal, 62, 85–93. [PubMed] [Google Scholar]
- Hashimoto K (2010). Postwar Japanese history of the family and the gap. Tokyo, Japan, Seikyusha. (in Japanese). [Google Scholar]
- Hisamatsu Y, Tuboi K, Tsutsui S, & Sinoda T (2000). A study on primary screening method for eating disorder in female university students. Japanese Journal of Psychosomatic Medicine, 40, 325–331 (in Japanese with English abstract). [Google Scholar]
- Hoek HW, & van Hoeken D (2003). Review of the prevalence and incidence of eating disorders. International Journal of Eating Disorders, 34, 383–396, DOI: 10.1002/eat.10222. [DOI] [PubMed] [Google Scholar]
- Hotta M, Horikasa R, Mabe H, Yokoyama S, Sugiyama E, Yonekawa T, … Ogawa Y (2015). Epidemiology of anorexia nervosa in Japanese adolescents. Biopsychosocial Medicine, 9, 17, doi: 10.1186/s13030-015-0044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikawa K, Iwata Y, & Hirano G (1960). Studies on the symptoms and the pathology of anorexia nervosa. Psychiatria et Neurologia Japonica, 62, 1203–1221 (In Japanese). [Google Scholar]
- Kagawa S (1768). Ippondo Koyo Igen, Tokyo, Japan: Waseda University Library; (in Chinese). [Google Scholar]
- Kajiyama S (1959). Anorexia nervosa - A clinical psychiatric study of 20 cases. Psychiatria et Neurologia Japonica, 61, 2256–2272 (in Japanese). [Google Scholar]
- Kaketa K, & Shimosaka K (1956). Anorexia nervosa. Clinic All-round, 5, 1903–1910 (In Japanese). [Google Scholar]
- Kamiya Y, & Suematsu H (2017). The epidemiological survey of the eating disorders in high school students in Aichi prefecture and actual conditions survey of correspondence by Yogo-teachers. Japan Journal of School Health, 59, 107–115 (in Japanese). [Google Scholar]
- Kasahara T, Yasuda M, Hayashishita T, Koyama T, Hukatsu R, & Yamauchi T (1985). Studies on bulimia: some characteristics of clinical symptoms. Psychiatria et Neurologia Japonica, 87, 521–545 (in Japanese). [PubMed] [Google Scholar]
- Keel P, & Klump K (2003). Are eating disorders culture-bound syndromes? Implications for conceptualizing their etiology. Psychological Bulletin, 129, 747–769. [DOI] [PubMed] [Google Scholar]
- Kiriike N, Nagata T, Tanaka M, Nishiwaki S, Takeuchi N, & Kawakita Y (1988). Prevalence of binge-eating and bulimia among adolescent women in Japan. Psychiatry Research, 26, 163–169. [DOI] [PubMed] [Google Scholar]
- Kuboki T, Nomura S, Ide M, Suematsu H & Araki S (1996). Epidemiological data on anorexia nervosa in Japan. Psychiatry Research, 62, 11–16. [DOI] [PubMed] [Google Scholar]
- Kurotori I, Shioda K, Abe T, Kato R, Ishikawa S, & Suda S (2019). An inpatient observational study: Characteristics and outcomes of avoidant/restrictive food intake disorder (ARFID) in children and adolescents in Japan. Neuropsychiatric Disease and Treatment, 15, 3313–3321, doi: 10.2147/NDT.S218354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Ho TP, & Hsu LK (1993). Fat phobic and non-fat phobic anorexia nervosa: a comparative study of 70 Chinese patients in Hong Kong. Psychological Medicine, 23, 999–1017. [DOI] [PubMed] [Google Scholar]
- Makino M, Tsuboi K, & Dennerstein L (2004). Prevalence of eating disorders: A comparison of Western and non-Western countries. Medscape General Medicine, 6, 49. [PMC free article] [PubMed] [Google Scholar]
- Markus HR, & Kitayama S (2010). Cultures and selves: A cycle of mutual constitution. Perspectives on Psychological Science, 5, 420–430. doi: 10.1177/1745691610375557 [DOI] [PubMed] [Google Scholar]
- Mason RHP, & Caiger JG (1997). A history of Japan, Tokyo, Japan, Tuttle publishing. [Google Scholar]
- Masuda M (1952). The 17-ketosteroids. Japanese Journal of Urology, 43, 41–51 (in Japanese with English abstract). [Google Scholar]
- Ministry of Health, Labor and Welfare (2003). The National Nutrition Survey in Japan, 2001, Tokyo, Japan, Dai-ichi-Suppan Publishing. (in Japanese). [Google Scholar]
- Mizuno Y, Makita H, Yamaguchi N, Ishii Y, & Mizushima Y (1986). The epidemiological study of anorexia nervosa in junior and senior high school students in Fukui Prefecture. Japanese Journal of Psychosomatic Medicine, 26, 409–419 (in Japanese). [Google Scholar]
- Mizushima N, & Ishii Y (1983). The epidemiology of anorexia nervosa in junior and senior high school students in Ishikawa prefecture. Japanese Journal of Psychosomatic Medicine, 23, 311–319 (in Japanese). [Google Scholar]
- Morohashi T (1993). The culture of women’s magazines: a study of gender image. Tokyo, Japan, Akashi Shoten; (in Japanese). [Google Scholar]
- Munn Z, Peters MDJ, Sterm C, Tufanaru C, McArthur A, & Aromataris E (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18, 143, 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustafa N, Zaidi AU, & Weaver RR (2017). Conspiracy of silence: cultural conflict as a risk factor for the development of eating disorders among second-generation Canadian South Asian women. South Asian Diaspora, 9(1), 33–49. 10.1080/19438192.2016.1199421 [DOI] [Google Scholar]
- Nadaoka T, Oiji A, Takahashi S, Morioka Y, Kashiwakura M, & Totsuka S (1996). An epidemiological study of eating disorders in a northern area of Japan. Acta Psychiatrica Scandinavica, 93, 305–310. [DOI] [PubMed] [Google Scholar]
- Nakai Y (1984). The epidemiology of anorexia nervosa in junior and senior high school students in Kyoto prefecture. In: Research group for eating disorders (Ed.), Annual report of anorexia nervosa. (pp.34–39). The Ministry of Health and Welfare, Tokyo, Japan: (in Japanese). [Google Scholar]
- Nakai Y, Fujita T, Kuboki T, Nozoe S, Kubo C, Yoshimasa Y, … Nakao K (2001). Nationwide survey of eating disorders in Japan. Clinical Psychiatry, 43, 1373–1378 (in Japanese). [Google Scholar]
- Nakai Y (2005). Epidemiology of eating disorders. Psychosomatic medicine, 9, 299–305 (in Japanese). [Google Scholar]
- Nakai Y, Hamagaki S, Noma S, Takao T, Yamashita T, Fujita M, … Ishikawa T (2009). Survey of eating disorders among medical facilities in Kyoto City. Clinical Psychiatry, 51, 681–683 (in Japanese). [Google Scholar]
- Nakai Y (2012). Epidemiology. In Guideline of eating disorders. (ed. Japan Society for Eating Disorders), pp.18–22, Igakushoin, Tokyo, Japan: (in Japanese). [Google Scholar]
- Nakai Y, Fukushima M, Taniguchi A, Nin K, & Teramukai S (2013). Comparison of DSM-IV versus proposed DSM-5 diagnostic criteria for eating disorders in a Japanese sample. European Eating Disorders Review, 21, 8–14, doi: 10.1002/erv.2203. [DOI] [PubMed] [Google Scholar]
- Nakai Y, Nin K, & Noma S (2014a). Eating disorder symptoms among Japanese female students in 1982, 1992 and 2002. Psychiatry Research, 209, 151–156. [DOI] [PubMed] [Google Scholar]
- Nakai Y, Nin K, Teramukai S, Taniguchi A, Fukushima M, & Wonderlich S (2014b). Typical and atypical anorexia nervosa in a Japanese sample. International Journal of Eating Disorders, 47, 130–137. doi: 10.1002/eat.22208. [DOI] [PubMed] [Google Scholar]
- Nakai Y, & Nin K (2016a). Clinical symptoms in patients with binge-eating disorder. Japanese journal of clinical psychiatry, 45, 235–239 (in Japanese).. [Google Scholar]
- Nakai Y, Nin K, Noma S, Teramukai S, & Wonderlich S (2016b). Characteristics of avoidant/restrictive food intake disorder in a cohort of adult patients. European Eating Disorders Review, 24, 528–530, doi: 10.1002/erv.2476. [DOI] [PubMed] [Google Scholar]
- Nakai Y, Nin K, Noma S, Hamagaki S, Takagi R, Teramukai S, & Wonderlich S (2017a). Clinical presentation and outcome of avoidant/restrictive food intake disorder in a Japanese sample. Eating Behaviors, 24, 49–53, doi: 10.1016/j.eatbeh.2016.12.004. [DOI] [PubMed] [Google Scholar]
- Nakai Y, Nin K, Noma S, Teramukai S,Fujikawa K, & Wonderlich S (2017b). The impact of DSM-5 on the diagnosis and severity indicator of eating disorders in a treatment-seeking sample. International Journal of Eating Disorders, 50, 1247–1257. doi: 10.1002/eat.22777. [DOI] [PubMed] [Google Scholar]
- Nakai Y, Nin K, Noma S, Teramukai S, Fujikawa K, & Wonderlich SA (2018). Changing profile of eating disorders between 1963 and 2004 in a Japanese sample. International Journal of Eating Disorders, 51, 953–958, 10.1002/eat.22935 [DOI] [PubMed] [Google Scholar]
- Nakai Y, & Nin K (2020). Eating disorders during the Edo period between 1603 and 1867 in Japan. International Journal of Eating Disorders, doi: 10.1002/eat.23387. [DOI] [PubMed] [Google Scholar]
- Nakamura K, Yamamoto M, Yamazaki O, Kawashima Y, Muto K, Someya T, … Nozoe S (2000). Prevalence of anorexia nervosa and bulimia nervosa in a geographically defined area in Japan. International Journal of Eating Disorders, 28, 173–180. [DOI] [PubMed] [Google Scholar]
- Nishimaru S (1956). Anorexia nervosa. Clinic All-round, 5, 1897–1902 (In Japanese). [Google Scholar]
- Nishizono-Maher A (1998). Eating disorders in Japan: finding the right context. Psychiatry and Clinical Neuroscience, 52, S320–S323. [DOI] [PubMed] [Google Scholar]
- Nogami Y (1973). On the “binge-eating” in adolescence. Nichidai Igaku Zasshi, 32, 218–227 (In Japanese). [Google Scholar]
- Nogami Y, & Yabana F (1977). On Kibarashi-gui (binge eating). Folia Psychiatrica et Neurologica Japonica, 31, 294–295 (in Japanese with English abstract). [PubMed] [Google Scholar]
- Nogami Y, Yamaguchi T, Ishiwata H, Sakai T, & Kusakabe Y (1984). The prevalence of binge eating among the Japanese university population. Nichidai Igaku Zasshi, 43, 749–752 (In Japanese). [Google Scholar]
- Nogami Y (1997). Eating disorders in Japan; A review of the literature. Psychiatry and Clinical Neurosciences, 51, 339–346. [DOI] [PubMed] [Google Scholar]
- Ogino T (1770). Taishuen-Zuihitu, Kyoto University Rare Materials Digital Archive, Kyoto, Japan: (in Chinese). [Google Scholar]
- Ohta M (1883). Wakan-Irinshinshi, Kyoto, Japan, Kyousha, Kyoto University Rare Materials Digital Archive. (in Chinese). [Google Scholar]
- Ohzeki T (1984). The epidemiology of anorexia nervosa in junior high school students in Tottori and Shimane prefectures. In: Research group for eating disorders (Ed.), Annual report of anorexia nervosa. (pp. 50–58). The Ministry of Health and Welfare, Tokyo, Japan: (in Japanese). [Google Scholar]
- Ohzeki T, Hanaki K, Motozumi H, Ishitani N, Matsuda-Ohtahara H, Sunaguchi M, & Shiraki K (1990). Prevalence of obesity, leanness and anorexia nervosa in Japanese boys and girls aged 12–14 years. Annals of Nutrition and Metabolism, 34, 208–212, doi: 10.1159/000177588. [DOI] [PubMed] [Google Scholar]
- Otsuka K (1955). On Fushoku-byo of the Edo period. Nihon Toyo Igakukai Zasshi (Kampo Medicine), 6, 10–14 (in Japanese). [Google Scholar]
- Oxford Centre for Evidence-Based Medicine. (2009). Levels of evidence. Oxford, UK: Oxford Centre for Evidence-Based Medicine. [Google Scholar]
- Perloff WH, Lasche EM, Nodine JH, Schneeberg NG, & Vieillard CB (1954). The starvation state and functional hypopituitarism. J. A. M. A, 155, 1307–1313. [DOI] [PubMed] [Google Scholar]
- Pike KM, & Borovoy A (2004). The rise of eating disorders in Japan: Issues of culture and limitations of the model of “Westernization”. Culture, Medicine, and Psychiatry, 28, 493–531. doi: 10.1007/s11013-004-1066-6. [DOI] [PubMed] [Google Scholar]
- Pike KM, & Dunne PE (2015). The rise of eating disorders in Asia: a review. Journal of Eating Disorders, 3, 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince R (1985). The concept of culture-bound syndromes: Anorexia nervosa and brain-fag. Social Science & Medicine, 21, 197–203. [DOI] [PubMed] [Google Scholar]
- Reddy SD, & Crowther JH (2007). Teasing, acculturation, and cultural conflict: Psychosocial correlates of body image and eating attitudes among South Asian women. Cultural Diversity and Ethnic Minority Psychology, 13(1), 45–53. 10.1037/1099-9809.13.1.45 [DOI] [PubMed] [Google Scholar]
- Seike K, Hanazawa H, Ohtani T, Takamiya S, Sakuta R, & Nakazato M (2016a). A questionnaire survey of the type of support required by Yogo teachers to effectively manage students suspected of having eating disorders. BioPsychoSocial Medicine, 10, 15, doi: 10.1186/s13030-016-0065-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seike K, Nakazato M, Hanazawa H, Ohtani T, Niitsu T, Ishikawa S, … Sakuta R (2016b). A questionnaire survey regarding the support needed by Yogo teachers to take care of students suspected of having eating disorders (second report). BioPsychoSocial Medicine, 10, 28, doi: 10.1186/s13030-016-0079-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimosaka K (1961). Psychiatric studies on anorexia nervosa. Psychiatria et Neurologia Japonica, 63, 1041–1082 (In Japanese with German abstract). [PubMed] [Google Scholar]
- Soh NL, & Walter T (2013). Publications on cross-cultural aspects of eating disorders. Journal of Eating Disorders, 1, 4, doi: 10.1186/2050-2974-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strand M, von Hausswolff-Juhlin Y, & Welch E (2018). A systematic scoping review of diagnostic validity in avoidant/restrictive food intake disorder. International Journal of Eating Disorders, 52, 331–360. [DOI] [PubMed] [Google Scholar]
- Suematsu H, Ishikawa H, Kuboki T, & Ito T (1985). Statistical studies on anorexia nervosa in Japan: Detailed clinical data on 1,011 patients. Psychotherapy and Psychosomatics, 43, 96–103. doi: 10.1159/000287865 [DOI] [PubMed] [Google Scholar]
- Tachibana N (1796). Toyuki, Tokyo, Japan: National Diet Library; (in Chinese). [Google Scholar]
- Takeda A, Suzuki K, & Matsushita S (1983). Prevalence of bulimia nervosa (DSM-III-R) among male and female high school students. Clinical Psychiatry, 35, 1273–1278 (in Japanese). [Google Scholar]
- Tamaki A, Ohno Y, Kawamura T, Hashimoto S, & Nagai M (2002). Nationwide epidemiological survey of intractable diseases with no subsidy for treatment. IRYO, 56, 51–58 (in Japanese). [Google Scholar]
- Taylor CB, Fitzsimmons-Craft EE, & Goel NJ (2018). Prevention: Current status and underlying theory. In Agras WS & Robinson A (Eds.), Oxford handbook of eating disorders (2nd ed., pp. 247–270). New York, NY: Oxford University Press. [Google Scholar]
- Thomas JJ, Lee S, & Becker AE (2016). Updates in the epidemiology of eating disorders in Asia and the Pacific. Current Opinion in Psychiatry, 29, 354–362. 10.1097/YCO.0000000000000288. [DOI] [PubMed] [Google Scholar]
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, …Straus S,E(2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169, 467–473, doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- Tsai G (2000). Eating disorders in the far east. Eating and Weight disorders, 5, 183–197. [DOI] [PubMed] [Google Scholar]
- Tseng MM, Tu CY, Hsieh SF, & Chang CH (2020). Rates and trends in healthcare-detected incidence of anorexia nervosa and bulimia nervosa: A national health insurance claim data study in Taiwan, 2002–2013. International journal of eating disorders, 53(3), 331–338. doi: 10.1002/eat.23203. [DOI] [PubMed] [Google Scholar]
- Vandereycken W, & van Deth R (1994). From fasting saints to anorexic girls: The history of self-starvation. New York: New York University Press. [Google Scholar]
- Vardaman JM (2006). Contemporary Japanese History: Since 1945. Tokyo, Japan, IBC [Google Scholar]
- Wildes JE, Emery RE, & Simons AD (2001). The roles of ethnicity and culture in the development of eating disturbance and body dissatisfaction: A meta-analytic review. Clinical Psychology Review, 21(4), 521–551. [DOI] [PubMed] [Google Scholar]
- Yakata M (1951). Two cases of anorexia nervosa. Niigata Medical Journal, 65, 620–623. (in Japanese). [Google Scholar]
- Yamaguchi Y, & Ogiwara K (1941). So called anorexia nervosa and its two cases. Japanese Journal of Gastroenterology, 40, 13–138 (in Japanese). [Google Scholar]
- Yamaguchi Y, Tsuchiya M, & Akiba T (1956). Treatment of anorexia nervosa. Clinic All-round, 5, 1916–1924 (In Japanese). [Google Scholar]
- Yu K, Pope SC, & Perez M (2019). Clinical treatment and practice recommendations for disordered eating in Asian Americans. Professional Psychology: Research and Practice. Advance online publication. 10.1037/pro0000244 [DOI] [Google Scholar]
- Yu F, Takahashi T, Moriya J, Kawaura K, Yamakawa J, Kusaka K, … Kanda T (2006). Traditional Chinese medicine and Kampo: A review from the distant past for the future. The Journal of International Medical Research, 36, 231–239. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


