Abstract
Background
Marijuana use is common among patients on long-term opioid therapy (LTOT) for chronic pain, but there is a lack of evidence to guide clinicians’ response.
Objective
To generate expert consensus about responding to marijuana use among patients on LTOT.
Design
Analysis from an online Delphi study.
Setting/Subjects
Clinician experts in pain and opioid management across the United States.
Methods
Participants generated management strategies in response to marijuana use without distinction between medical and nonmedical use, then rated the importance of each management strategy from 1 (not at all important) to 9 (extremely important). A priori rules for consensus were established, and disagreement was explored using cases. Thematic analysis of free-text responses examined factors that influenced participants’ decision-making.
Results
Of 42 participants, 64% were internal medicine physicians. There was consensus that it is not important to taper opioids as an initial response to marijuana use. There was disagreement about the importance of tapering opioids if there is a pattern of repeated marijuana use without clinical suspicion for a cannabis use disorder (CUD) and consensus that tapering is of uncertain importance if there is suspicion for CUD. Three themes influenced experts’ perceptions of the importance of tapering: 1) benefits and harms of marijuana for the individual patient, 2) a spectrum of belief about the overall riskiness of marijuana use, and 3) variable state laws or practice policies.
Conclusions
Experts disagree and are uncertain about the importance of opioid tapering for patients with marijuana use. Experts were influenced by patient factors, provider beliefs, and marijuana policy, highlighting the need for further research.
Keywords: Marijuana, Opioids, Chronic Pain, Delphi Study
Introduction
The United States is in the midst of an epidemic of opioid use disorder and overdose [1], due in part to a rise in opioid prescribing in the past two decades [2]. Clinical guidelines such as the Centers for Disease Control and Prevention (CDC) Guideline for Prescribing Opioids for Chronic Pain recommend that clinicians who prescribe opioids monitor patients regularly for potential harms, which include the use of nonprescribed or illicit substances [3]. Further, guidelines generally recommend that clinicians consider reducing or discontinuing long-term opioid therapy (LTOT) when such use occurs [3–6].
However, current guidelines avoid guidance specific to marijuana use. For example, the CDC guideline acknowledged “uncertainty about the clinical implications” of marijuana use in the context of LTOT [3]. The Washington State Interagency Guideline from 2015 referred to marijuana use as a “complex issue,” and they did not consider it a “red flag,” like amphetamine, cocaine, or nonprescribed benzodiazepine use [6].
This lack of guidance about how to respond to marijuana use in patients on LTOT reflects the concept that the risk/benefit profile of marijuana for patients with chronic pain may differ from that of other federally illicit substances. For example, though known risks of marijuana use include adverse mental health consequences [7, 8] and motor vehicle accidents [9], marijuana use has not been associated with fatal overdose [10]. Further, the past decade has seen a rapid expansion of medical use of marijuana products to treat chronic pain, though few studies have examined long-term outcomes [10–25]. Chronic pain is an indication for certification to receive medical marijuana products in at least 28 US states [26], Canada, and many European countries [27]. Thus, it is not surprising that marijuana use is common among individuals on LTOT for chronic pain. In studies in diverse primary care settings in North America, 11% to 20% of patients on LTOT tested positive for marijuana use [28–32].
Given the increasing use of marijuana and the potential for both harms and benefits, how to respond to marijuana use in patients prescribed LTOT is an important clinical question [33]. Unfortunately, little is known about the harms and benefits of marijuana use in combination with LTOT [34]. Given this lack of evidence and resulting vague language in current clinical guidelines, we sought to generate expert consensus about how clinicians managing chronic pain should respond to marijuana use among patients prescribed LTOT. To provide necessary guidance for front-line clinicians who are often faced with this question, we also explored when and whether tapering opioids is recommended for patients on LTOT who use marijuana.
Methods
Overview
This analysis is part of a Delphi study conducted from March 2015 to August 2016, the purpose of which was to establish consensus about management of concerning behaviors that arise among patients prescribed LTOT. Detailed study methods and outcomes on other common and challenging behaviors, including substance use other than marijuana, were published separately [35,36]. Here, we present methods and results specific to data collection and consensus building about marijuana use. Given perceived differences between marijuana and other substance use, we chose to present these findings separately. This study was approved by the Institutional Review Board of the University of Alabama at Birmingham (UAB).
Participants
Briefly, the web-based Delphi process engaged clinicians who were experts in chronic pain and opioid prescribing in four sequential rounds of data collection and consensus building. Participants were recruited from professional societies and other expert groups [35,36]. Inclusion criteria were self-report of providing direct outpatient care to adults with chronic pain on LTOT and having expertise in opioid prescribing for chronic pain (e.g., having taught others on this topic, having published on this topic, or being considered a resource for other clinicians on this topic). One participant per round was randomly chosen to receive a $100 gift card.
Data Collection and Analysis
In Round 1, participants were asked to identify all common and challenging concerning behaviors they encounter in patients on LTOT for chronic pain. In Round 2, participants were asked how they would typically manage these behaviors in their clinical practice (“management strategies”). To allow participants to propose distinct management strategies for different substances mentioned in Round 1 (heroin, cocaine, benzodiazepines, alcohol, and marijuana), queries in subsequent rounds were specific to the substance. The findings presented here are specific to marijuana.
In Round 3, participants were presented with management strategies from Round 2 and asked to rate their importance on a scale from 1 (not at all important) to 9 (extremely important). We classified each response as “not important” (1–3), of “uncertain importance” (4–6), or “important” (7–9), and participants were encouraged to clarify their responses with free text. Disagreement occurred if at least one-third of participants indicated that the management strategy was not important (1–3) and at least one-third indicated that it was important (7–9). Consensus was achieved if there was no disagreement [35]. When consensus was achieved, the median value of participant ratings was used to indicate the importance of the strategy using the same classification scheme, that is, not important, of uncertain importance, or important. Analysis of participants’ free-text responses identified “branch points” in decision-making—that is, points at which different clinical circumstances might warrant different management strategies. Two branch points were identified: whether a pattern of repeated marijuana use was present and whether there was clinical suspicion of a cannabis use disorder (CUD).
In Round 4, those management strategies that participants disagreed about were investigated further using a Delphi approach. Participants were provided with their previous response as well as the group’s median response and asked whether they would like to change their response. Management strategies of uncertain importance were investigated using case scenarios constructed based on the identified branch points. We did not define what was meant by “clinical suspicion” of CUD in the case scenarios; this was open to the experts’ interpretation, as would occur in clinical care.
To further understand participants’ decisions about when tapering of opioids in patients on LTOT is an important management strategy in response to marijuana use, we classified each participant based on their responses to three case scenarios. These scenarios differed in terms of whether a pattern of repeated marijuana use was present and whether there was clinical suspicion of CUD.
Specifically, the cases were as follows:
You are seeing a patient in clinic with the following behavior: marijuana use. In the previous round, participants agreed that the following management strategies are an important response to this behavior: Determine if a pattern of behavior has been present (e.g., by talking to the patient or reviewing records). Discuss or assess for a substance use disorder. Refer for addiction treatment or related services. Review opioid treatment agreement with the patient. Order urine toxicology tests more frequently. Now imagine that you have implemented all of the above strategies. Please consider the following cases:
Case 1. You assess the patient. You determine that a pattern of repeated marijuana use HAS NOT been present, and there is NO CLEAR BASIS for a diagnosis of marijuana use disorder.
Case 2. You assess the patient. You determine that a pattern of repeated marijuana use HAS been present, but there is NO CLEAR BASIS for a diagnosis of marijuana use disorder.
Case 3. You assess the patient. You determine that a pattern of repeated marijuana use HAS been present, and YOU STRONGLY SUSPECT a diagnosis of marijuana use disorder.
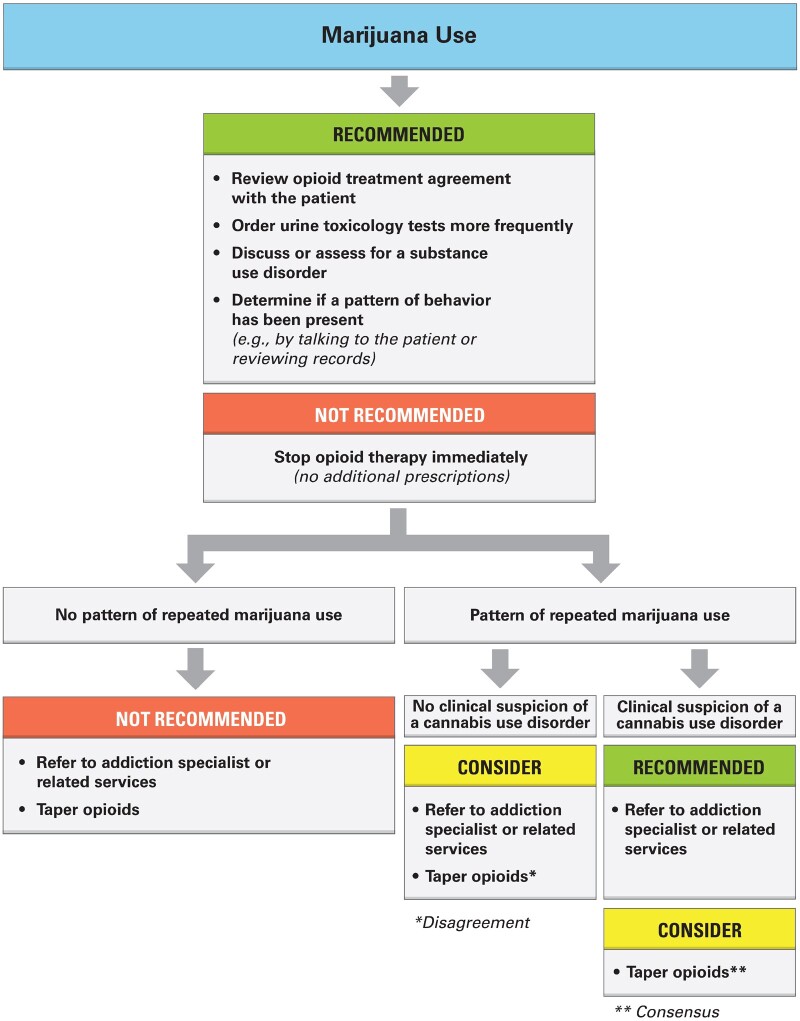
Participants were classified as “opposed” to marijuana use if they rated tapering opioids as important in all three case scenarios (regardless of whether a pattern or suspicion of CUD was present) and “accepting” if they rated tapering as not important in all three cases. We graphically depicted our findings in a proposed treatment algorithm (Figure 1). In the algorithm, a management strategy is “recommended” if there was consensus that it was important, “not recommended” if there was consensus that it was not important, and to be “considered” if there was disagreement about its importance or consensus of uncertain importance.
Figure 1.
Proposed Treatment Algorithm.
Given the richness of the free-text responses about marijuana, and to better understand the disagreement identified in the Delphi process, we also analyzed free-text data about marijuana use from all rounds qualitatively using an inductive thematic analysis approach [37]. Specifically, we extracted all textual data regarding marijuana use and imported them into an Excel spreadsheet. Each of three coders (JS, SRY, JM) developed an initial open coding scheme to classify responses into themes. Through discussion, a consensus coding scheme was created that allowed for merging of similar codes and deletion of overlapping codes. One coder (SRY) re-coded all data based upon the consensus coding scheme developed by the group; the three coders reviewed the coded text and resolved any disagreement. Below, we present the prominent themes identified and provide exemplary quotes from each theme.
Results
Forty-two clinicians participated in the study. Of these, 28 (67%) completed all four rounds. The majority of participants were female (52%), white (83%), and physicians (71%); 84% of physicians were internal medicine physicians. Participants practiced in all regions of the United States (Northeast 31%, Midwest 14%, South 31%, West 24%). Twenty-six (61.9%) practiced in a state with a medical marijuana law.
In Round 3, consensus was achieved that four initial management strategies were important in response to identifying marijuana use among patients prescribed LTOT: reviewing an opioid treatment agreement with the patient, ordering urine toxicology tests more frequently, determining if a pattern of behavior has been present, and discussing or assessing for a substance use disorder (Figure 1). There was consensus that it was not important to stop opioid therapy completely (i.e., to provide no additional prescriptions) as an initial management strategy after identifying marijuana use.
Also in Round 3, the importance of two management strategies, tapering opioids and referring to an addiction specialist or related services, depended on whether the patient had a pattern of repeated marijuana use (vs one-time or occasional use) and whether there was clinical suspicion of CUD. In the case of marijuana use without a pattern of repeated use, there was consensus that it was not important to taper opioids or to refer to an addiction specialist. When there was a pattern of repeated marijuana use but no suspicion of CUD, there was disagreement about whether to taper opioids and consensus that referring to an addiction specialist was of uncertain importance. When there was clinical suspicion of CUD, there was consensus that tapering opioids was of uncertain importance and that it was important to refer to an addiction specialist.
Of the 28 respondents in Round 4, five (17%) indicated that tapering opioids was not important even if there was a pattern of use or suspicion of CUD (i.e., “accepting” of marijuana use among patients on LTOT). Four (14%) indicated that tapering opioids was important in response to marijuana use regardless of whether there was a pattern of use or suspicion of CUD (“opposed”). The five who were accepting of marijuana practiced in the Northeast, Western, and Southern regions of the United States, and four practiced in states with medical marijuana laws at the time of the survey. Of the four who were opposed to marijuana, three worked in US Department of Veterans Affairs (VA) clinic settings, and they practiced in the South (two), Midwest (one), and Northeast (one) regions of the United States. The remaining 19 practiced in all regions of the United States.
Qualitative analysis of free-text data revealed three prominent themes that describe the most prominent influences on clinical decisions about responding to marijuana use among patients on LTOT: 1) benefits and harms of marijuana for the individual patient, 2) a spectrum of beliefs about the overall riskiness of marijuana use, and 3) variable state laws or practice policies. Exemplary quotes for each theme are presented in Table 2. In addition, prominent interplay between these themes revealed ambivalence and uncertainty about how to respond to marijuana use. For example, one participant wrote, “I consider marijuana much lower risk than other illicit drugs. However, if there is a clinic policy then I would adhere to this.” Another wrote, “The response may differ, in part, on whether the marijuana is in a state where it is legal. But marijuana use may not be causing problems, and to me, it would not be an indication to stop the prescription medication just because of any marijuana use.” One participant summarized a common sentiment, “Given the shifts in society, I am still uncertain about the role of marijuana in the management of chronic pain.”
Table 2.
Major influences on expert response to marijuana use and exemplary quotes
| Theme | Quotes |
|---|---|
| Benefits and harms of marijuana for the individual patient | [It is] important to understand how/why [the] patient is using marijuana; what the effects are and how it is used in relation to opioids. |
| It would be important to clarify exactly what these benefits are for this patient … . If on a given day, I do not believe the patient is experiencing significant harms, I remain concerned about future harms and repeat this decision-making process with each refill and each visit. | |
| While I don’t necessarily agree this is ideal, if they are not experiencing harm, do not appear to have addiction, and I have counseled them appropriately, I would be willing to work with the patient and try to minimize but not necessarily stop opioids if overall the benefits seem to outweigh the harms/risks. | |
| Belief about the overall riskiness of marijuana use | I would not mix opioids and marijuana. |
| Since there are drug/drug interactions with the cannabis and opioids, the opioids should be tapered if [the patient] continues with the marijuana. | |
| [I] consider marijuana much lower risk than other illicit drugs. | |
| I do not believe that tapering opioids is an appropriate clinical response to nondisordered marijuana use. | |
| State laws or practice policy | [It] depends on the laws regarding marijuana use in the state that the patient lives in. If recreational marijuana is legal there, I do not think that it should factor in to the opioid decision as long as there is no evidence of harm. However, if it is only approved for medicinal uses and it is not being certified/authorized/prescribed by me, then this represents increased risk. Similarly, if the use of marijuana is illegal in the state in which the patient lives, it needs to be treated as an illicit substance and other controlled substances should be prescribed with caution, if at all. |
| My toleration for marijuana in a [urine toxicology test] is related, in part, to whether MJ is legal in the state where I am practicing and/or, in the case of medical marijuana, whether the patient has a medical MJ card. | |
| [I] consider marijuana much lower risk than other illicit drugs. However, if there is a clinic policy then [I] would adhere to this. |
Table 1.
Participant characteristics (N = 42)
| Characteristic | No. (%) |
|---|---|
| Female | 22 (52) |
| Age, mean (SD), y | 48 (11.6) |
| Geographic region of the US | |
| Northeast | 13 (31) |
| South | 13 (31) |
| Midwest | 6 (14) |
| West | 10 (24) |
| Practiced in state with medical marijuana law enacted before 1/1/2016* | 26 (61.9) |
| Race | |
| White | 35 (83) |
| Black | 2 (5) |
| Other | 5 (12) |
| VA setting | 20 (48) |
| Discipline | |
| Physician (MD or DO) | 32 (76) |
| Nurse practitioner | 7 (17) |
| Clinical pharmacologist | 1 (2) |
| Registered nurse | 1 (2) |
| Clinical nurse specialist | 1 (2) |
| Physician specialty (of 32 physicians) | |
| Internal medicine | 27 (84) |
| Physical medicine & rehab | 3 (9) |
| Neurology | 3 (9) |
| Anesthesiology | 1 (3) |
| Psychiatry | 1 (3) |
Discussion
In this study, experts agreed that it is not important to taper or discontinue LTOT in response to one-time or occasional marijuana use. However, there was disagreement about whether to taper opioids for patients with a pattern of repeated use, and uncertainty about whether to taper opioids even when the clinician has suspicion of a CUD. Experts agreed that reviewing the opioid treatment agreement and increasing frequency of urine drug testing are always important for patients on LTOT who use marijuana, and that it is important to refer patients to an addiction specialist or related services if there is clinical suspicion of a CUD. Most experts were neither fully accepting nor fully opposed to marijuana use among patients on LTOT. Qualitative analysis revealed that decisions about how to respond to marijuana use in patients on LTOT are influenced by the benefits and harms of marijuana for the individual patient, provider beliefs about the overall riskiness of marijuana use, and state laws or practice policies. Taken together, these findings demonstrate substantial disagreement and clinical uncertainty about the optimal response to marijuana use among patients on LTOT, provide a heuristic for developing a response based on the pattern of use and presence of a CUD, and generate hypotheses for future research.
Disagreement among the study participants and vagueness of guidelines about how to respond to marijuana use in the absence of a CUD reflect limited evidence about the harms and benefits of marijuana use among patients on LTOT. Regarding potential harms, cross-sectional studies have found an association between marijuana use and prescription opioid misuse among patients on LTOT [32,34, 38,39]. However, the nature of the association is unknown (i.e., whether marijuana use leads to or may be a risk factor for opioid misuse, opioid use disorder, or overdose is not yet known) [34]. In addition, though there is concern for central nervous system depression in patients on LTOT when marijuana is introduced, studies are lacking. Regarding potential benefits, recent retrospective and cross-sectional studies found that marijuana use is associated with decreased opioid use in patients with chronic pain [40–43], and there may be analgesic synergism between marijuana and opioids [44]. Recent epidemiologic studies have found a relationship between medical marijuana laws and reduced opioid overdose at a state level [43,45–48]. However, existing research is limited due in part to US federal restrictions on marijuana research, and rigorous prospective studies about the impact of marijuana use on individuals’ pain or opioid use outcomes are lacking.
Consistent with our qualitative findings, a reasonable approach in the absence of evidence is to consider the relative benefits and harms of marijuana use for the individual patient on LTOT before deciding how best to respond. This framework of weighing the benefits vs risks or actual harms parallels the framework promoted by the CDC guideline for decisions about opioid management more broadly [3]. Notably, it can be challenging to tease out the benefits and harms of marijuana from those of LTOT, and further research is needed to guide practice.
In this study, we found that a clinical suspicion of CUD prompted participants to suggest referral to an addiction specialist or related services and consider tapering opioids. This is largely consistent with guidelines such as the Veterans Affairs/Department of Defense recommendation to avoid LTOT in patients with an untreated substance use disorder [49]. In national surveys, the prevalence of CUD is 30% among US adults who reported past-year marijuana use [50]. However, primary care providers, who prescribe the majority of opioids for chronic pain in the United States, are not well trained in identifying or treating substance use disorders [51,52]. Further, in contrast to opioid use disorder, there are few options for treating CUD, and their effectiveness is limited [53]. The lack of treatment options likely reduces primary care providers’ motivation to make the diagnosis.
Finally, the findings suggest that state laws or practice policies influence providers’ perspectives on how to manage marijuana use among patients on LTOT. This may reflect provider concerns about liability or potential risks to their medical license or career. It may also reflect that loosening of medical marijuana laws can lead to positive provider perception of marijuana’s benefits relative to its risks. Given the lack of evidence and uncertainty about the risks and benefits of marijuana use in patients with LTOT, provider beliefs about the overall riskiness of marijuana and state or practice policies may have a disproportionate impact on provider decisions. Participants in this study described that health systems and practices have created policies about concomitant use of marijuana and prescription opioids that could help standardize care. Notably, though the Washington State guideline states that “it would be prudent to have a policy regarding the concomitant use of cannabis and opioids,” the guideline does not indicate what that policy should be, noting that this is a “complex issue” [6]. Our findings do not support the tapering or discontinuing of LTOT in response to a first episode of marijuana use, in contrast to recommendations in some practice policies.
This study has limitations. Participants were asked about how they would respond to discrete behaviors, such as marijuana use, among patients on LTOT. We are therefore unable to draw conclusions regarding how they would respond when marijuana use occurs along with other concerning behaviors. We did not examine the converse situation, that is, how experts would respond to requests to initiate medical marijuana among patients on LTOT, or to initiate opioids among patients already using marijuana. We did not stratify each scenario according to whether marijuana use was authorized under a medical marijuana program. Participants all self-reported that they were pain and opioid experts; however, additional information about their experience and scope of practice (e.g., patient panel size or composition, or expertise in diagnosing and treating substance use disorders) was not collected. Finally, expert responses were based on hypothetical cases and may not be consistent with their actual behaviors.
When faced with a lack of evidence and clinical uncertainty, clinicians rely on expert opinion. In this study, experts agreed about monitoring strategies but disagreed about whether to taper LTOT in response to repeated marijuana use in the absence of a cannabis use disorder among patients on LTOT for chronic pain. Further research is urgently needed to guide clinical decision-making regarding marijuana use in patients on LTOT.
Funding sources: The authors received support from the National Institutes of Health: K24DA046309 (Starrels), R01DA039046 (Starrels), K23MH104073 (Merlin), and K12DA033312 (Edelman).
Conflicts of interest: Dr. Starrels has received research and travel support from the Opioid Post-marketing Requirement Consortium for work on a Food and Drug Administration–mandated observational study of the risks of opioids, has consulted for Venebio Group LLC, and has served as a Core Expert for the Centers for Disease Control Guideline for Prescribing Opioids for Chronic Pain.
Prior presentation: Findings from this study were presented as a poster at the Society of General Internal Medicine’s annual meeting in Denver, Colorado, on April 13, 2018.
References
- 1. Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. MMWR Morb Mortal Wkly Rep 2016;64(50–51):1378–82. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Annual Surveillance Report of Drug-Related Risks and Outcomes—United States, 2017. Surveillance Special Report 1. Atlanta: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2017.
- 3. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep 2016;65(1):1–49. [DOI] [PubMed] [Google Scholar]
- 4. Chou R, Fanciullo GJ, Fine PG, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain 2009;10(2):113–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Federation of State Medical Boards. Model Policy on the Use of Opioid Analgesics in the Treatment of Chronic Pain. United States: Federation of State Medical Boards; 2013.
- 6.Washington State Agency Medical Directors’ Group. Interagency Guideline on Prescribing Opioids for Pain. United States: Washington State Agency Medical Directors' Group; 2015. Available at: http://www.agencymeddirectors.wa.gov/Files/2015AMDGOpioidGuideline.pdf. (accessed June 28, 2019)
- 7. De Aquino JP, Sherif M, Radhakrishnan R, Cahill JD, Ranganathan M, D'Souza DC. The psychiatric consequences of cannabinoids. Clin Ther 2018;40:1448–56. [DOI] [PubMed] [Google Scholar]
- 8. Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem 2013;59(3):478–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sewell RA, Poling J, Sofuoglu M. The effect of cannabis compared with alcohol on driving. Am J Addict 2009;18(3):185–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nugent SM, Morasco BJ, O'Neil ME, et al. The effects of cannabis among adults with chronic pain and an overview of general harms: A systematic review . Ann Intern Med 2017;167(5):319–31. [DOI] [PubMed] [Google Scholar]
- 11. Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: A systematic review and meta-analysis. JAMA 2015;313(24):2456–73. [DOI] [PubMed] [Google Scholar]
- 12. Ellis RJ, Toperoff W, Vaida F, et al. Smoked medicinal cannabis for neuropathic pain in HIV: A randomized, crossover clinical trial. Neuropsychopharmacology 2009;34(3):672–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nurmikko TJ, Serpell MG, Hoggart B, Toomey PJ, Morlion BJ, Haines D. Sativex successfully treats neuropathic pain characterised by allodynia: A randomised, double-blind, placebo-controlled clinical trial. Pain 2007;133(1):210–20. [DOI] [PubMed] [Google Scholar]
- 14. Abrams DI, Jay CA, Shade SB, et al. Cannabis in painful HIV-associated sensory neuropathy: A randomized placebo-controlled trial. Neurology 2007;68(7):515–21. [DOI] [PubMed] [Google Scholar]
- 15. Wilsey B, Marcotte T, Tsodikov A, et al. A randomized, placebo-controlled, crossover trial of cannabis cigarettes in neuropathic pain. J Pain 2008;9(6):506–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Skrabek RQ, Galimova L, Ethans K, Perry D. Nabilone for the treatment of pain in fibromyalgia. J Pain 2008;9(2):164–73. [DOI] [PubMed] [Google Scholar]
- 17. Narang S, Gibson D, Wasan AD, et al. Efficacy of dronabinol as an adjuvant treatment for chronic pain patients on opioid therapy. J Pain 2008;9(3):254–64. [DOI] [PubMed] [Google Scholar]
- 18. Wissel J, Haydn T, Muller J, et al. Low dose treatment with the synthetic cannabinoid Nabilone significantly reduces spasticity-related pain: A double-blind placebo-controlled cross-over trial. J Neurol 2006;253(10):1337–41. [DOI] [PubMed] [Google Scholar]
- 19. Blake DR, Robson P, Ho M, Jubb RW, McCabe CS. Preliminary assessment of the efficacy, tolerability and safety of a cannabis-based medicine (Sativex) in the treatment of pain caused by rheumatoid arthritis. Rheumatology 2006;45(1):50–2. [DOI] [PubMed] [Google Scholar]
- 20. Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: A clinical review. JAMA 2015;313(24):2474–83. [DOI] [PubMed] [Google Scholar]
- 21. Berman JS, Symonds C, Birch R. Efficacy of two cannabis based medicinal extracts for relief of central neuropathic pain from brachial plexus avulsion: Results of a randomised controlled trial. Pain 2004;112(3):299–306. [DOI] [PubMed] [Google Scholar]
- 22. Andreae MH, Carter GM, Shaparin N, et al. Inhaled cannabis for chronic neuropathic pain: A meta-analysis of individual patient data. J Pain 2015;16(12):1221–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Karst M, Salim K, Burstein S, Conrad I, Hoy L, Schneider U. Analgesic effect of the synthetic cannabinoid CT-3 on chronic neuropathic pain: A randomized controlled trial. JAMA 2003;290(13):1757–62. [DOI] [PubMed] [Google Scholar]
- 24. Langford RM, Mares J, Novotna A, et al. A double-blind, randomized, placebo-controlled, parallel-group study of THC/CBD oromucosal spray in combination with the existing treatment regimen, in the relief of central neuropathic pain in patients with multiple sclerosis. J Neurol 2013;260(4):984–97. [DOI] [PubMed] [Google Scholar]
- 25. Rog DJ, Nurmikko TJ, Friede T, Young CA. Randomized, controlled trial of cannabis-based medicine in central pain in multiple sclerosis. Neurology 2005;65(6):812–9. [DOI] [PubMed] [Google Scholar]
- 26. ProCon.org. 25 legal medical marijuana states and DC. Published June 28, 2016. Available at: http://medicalmarijuana.procon.org/view.resource.php? resourceID=000881 (accessed September 1, 2016).
- 27. Azofeifa A, Mattson ME, Schauer G, McAfee T, Grant A, Lyerla R. National estimates of marijuana use and related indicators—National Survey on Drug Use and Health, United States, 2002–2014. MMWR Surveill Summ 2016;65(11):1–28. [DOI] [PubMed] [Google Scholar]
- 28. Hariharan J, Lamb GC, Neuner JM. Long-term opioid contract use for chronic pain management in primary care practice. A five year experience. J Gen Intern Med 2007;22(4):485–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fleming MF, Balousek SL, Klessig CL, Mundt MP, Brown DD. Substance use disorders in a primary care sample receiving daily opioid therapy. J Pain 2007;8(7):573–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ives TJ, Chelminski PR, Hammett-Stabler CA, et al. Predictors of opioid misuse in patients with chronic pain: A prospective cohort study. BMC Health Serv Res 2006;6:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Turner JA, Saunders K, Shortreed SM, et al. Chronic opioid therapy urine drug testing in primary care: Prevalence and predictors of aberrant results. J Gen Intern Med 2014;29(12):1663–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nugent SM, Yarborough BJ, Smith NX, et al. Patterns and correlates of medical cannabis use for pain among patients prescribed long-term opioid therapy. Gen Hosp Psychiatry 2018;50:104–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cushman PA, Liebschutz JM, Hodgkin JG, et al. What do providers want to know about opioid prescribing? A qualitative analysis of their questions. Subst Abus 2017;38(2):222–9. [DOI] [PubMed] [Google Scholar]
- 34. Reisfield GM, Wasan AD, Jamison RN. The prevalence and significance of cannabis use in patients prescribed chronic opioid therapy: A review of the extant literature. Pain Med 2009;10(8):1434–41. [DOI] [PubMed] [Google Scholar]
- 35. Merlin JS, Young SR, Azari S, et al. Management of problematic behaviours among individuals on long-term opioid therapy: Protocol for a Delphi study. BMJ Open 2016;6(5):e011619.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Merlin JS, Young SR, Starrels JL, et al. Managing concerning behaviors in patients prescribed opioids for chronic pain: A Delphi study. J Gen Intern Med 2018;33(2):166–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3(2):77–101. [Google Scholar]
- 38. Degenhardt L, Lintzeris N, Campbell G, et al. Experience of adjunctive cannabis use for chronic non-cancer pain: Findings from the Pain and Opioids IN Treatment (POINT) study. Drug Alcohol Depend 2015;147:144–50. [DOI] [PubMed] [Google Scholar]
- 39. Hefner K, Sofuoglu M, Rosenheck R. Concomitant cannabis abuse/dependence in patients treated with opioids for non-cancer pain. Am J Addict 2015;24(6):538–45. [DOI] [PubMed] [Google Scholar]
- 40. Reiman A, Welty M, Solomon P. Cannabis as a substitute for opioid-based pain medication: Patient self-report. Cannabis Cannabinoid Res 2017;2(1):160–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Reiman A. Cannabis as a substitute for alcohol and other drugs. Harm Reduct J 2009;6:35.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Boehnke KF, Litinas E, Clauw DJ. Medical cannabis use is associated with decreased opiate medication use in a retrospective cross-sectional survey of patients with chronic pain. J Pain 2016;17(6):739–44. [DOI] [PubMed] [Google Scholar]
- 43. Sohler NL, Starrels JL, Khalid L, et al. Cannabis use is associated with lower odds of prescription opioid analgesic use among HIV-infected individuals with chronic pain. Subst Use Misuse 2018;53:1602–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Abrams DI, Couey P, Shade SB, Kelly ME, Benowitz NL. Cannabinoid-opioid interaction in chronic pain. Clin Pharmacol Ther 2011;90(6):844–51. [DOI] [PubMed] [Google Scholar]
- 45. Cooper ZD, Bedi G, Ramesh D, Balter R, Comer SD, Haney M. Impact of co-administration of oxycodone and smoked cannabis on analgesia and abuse liability. Neuropsychopharmacology 2018;43:2046–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Intern Med 2014;174(10):1668–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wen H, Hockenberry JM. Association of medical and adult-use marijuana laws with opioid prescribing for Medicaid enrollees. JAMA Intern Med 2018;178:673–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Powell D, Pacula RL, Jacobson M. Do medical marijuana laws reduce addictions and deaths related to pain killers? J Health Econ 2018;58:29–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Department of Veterans Affairs Department of Defense. VA/DoD Clinical Practice Guideline for Opioid Therapy for Chronic Pain. United States: Department of Veterans Affairs Department of Defense; 2017.
- 50. Hasin DS, Saha TD, Kerridge BT, et al. Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry 2015;72(12):1235–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wood E, Samet JH, Volkow ND. Physician education in addiction medicine. JAMA 2013;310(16):1673–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Association AP. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 53. Sherman BJ, McRae-Clark AL. Treatment of cannabis use disorder: Current science and future outlook. Pharmacotherapy 2016;36(5):511–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.The National Organization for the Reform of Marijuana Laws. Medical marijuana state laws. Available at: https://norml.org/legal/medical-marijuana-2 (accessed July 2, 2018).