ABSTRACT
Background: The adverse consequences of the COVID-19 pandemic on mental health have been widely studied in recent months. However, few studies have examined the protective psychological factors that may explain how individuals are coping with the COVID-19 pandemic and its forced confinements.
Objective: This study analyzes the impact of confinement due to the COVID-19 pandemic on positive functioning variables (resilience, meaning of life, gratitude, compassion, life satisfaction), emotional distress (depression, anxiety, perceived stress, affect), and posttraumatic growth (PTG). The impact was measured during and after the first month of strict and obligatory confinement in Spain.
Methods: The sample was composed of 438 Spanish residents (78.3% women) between the ages of 18 and 68 (M = 35.68; SD = 13.19) during the first stage (first two weeks) of confinement. The sample was reduced to 197 participants during the second stage (fifth week) of confinement. Several online self-reported questionnaires were administered to assess positive functioning variables, emotional distress, and PTG.
Results: Women, youths, individuals without a partner, with lower monetary incomes, or diagnosed with a mental disorder or chronic illness experienced lower scores in positive functioning variables and greater emotional distress during the first stage of confinement. Linear mixed models showed that scores on positive functioning variables, emotional distress, and PTG worsened in the second stage of confinement. Nevertheless, a structural equations model showed that increases in positive functioning variables in the second stage were associated with increases in life satisfaction (R2 = .450) and related to decreases in emotional distress (R2 = .186), leading in turn to increases in PTG (R2 = .061).
Conclusions: Individuals could experience PTG during strict and mandatory confinement. The increase in PTG during this adverse event was indirectly associated with increases in positive functioning variables (i.e. gratitude, presence of meaning, resilience), through improvements in life satisfaction and emotional distress.
KEYWORDS: COVID-19 pandemic, confinement, positive functioning variables, emotional distress, posttraumatic growth
HIGHLIGHTS
Increases in positive functioning variables (resilience, gratitude, meaning in life) were protective factors associated with the increase in life satisfaction, the decrease in emotional distress, and the increase in posttraumatic growth after strict and forced confinement.
Short abstract
Antecedentes: Las consecuencias adversas de la pandemia de COVID-19 en la salud mental han sido ampliamente estudiadas en los últimos meses. Sin embargo, pocos estudios han examinado los factores psicológicos protectores que pueden explicar cómo los individuos están haciendo frente a la pandemia de COVID-19 y sus confinamientos forzados.
Objetivos: Este estudio analiza el impacto del confinamiento debido a la pandemia COVID-19 sobre las variables de funcionamiento positivo (resiliencia, sentido en la vida, gratitud, compasión, satisfacción con la vida), el malestar emocional (depresión, ansiedad, estrés percibido, afecto) y el crecimiento postraumático (CPT). El impacto se midió durante y después del primer mes de un confinamiento estricto y obligatorio en España.
Métodos: La muestra estuvo compuesta por 438 residentes españoles (78.3% mujeres), con edades comprendidas entre 18 y 68 años (M= 35.68; DT= 13.19) en la primera medición (las dos primeras semanas de confinamiento). La muestra se redujo a 197 participantes en la segunda medición (la quinta semana de confinamiento). Se administraron varios cuestionarios auto-informados online dirigidos a evaluar las variables de funcionamiento positivo, el malestar emocional y el CPT.
Resultados: Los participantes que eran mujeres, más jóvenes, sin pareja, con ingresos económicos más bajos, o diagnosticados con un trastorno mental o enfermedad crónica, experimentaron menores puntuaciones en variables de funcionamiento positivo y mayor malestar emocional en las primeras semanas del confinamiento. Los modelos lineales mixtos mostraron que las puntuaciones en las variables de funcionamiento positivo, el malestar emocional y el CPT empeoraron en la segunda etapa del confinamiento. Sin embargo, un modelo de ecuaciones estructural mostró que los aumentos en la segunda etapa en las variables positivas de funcionamiento se asociaban con aumentos en la satisfacción de la vida (R2 = .450), y se relacionaban con disminuciones en el malestar (R2 = .186), lo que a su vez conducía a aumentos en el CPT (R2 = .061).
Conclusiones: Las personas pueden experimentar CPT durante el confinamiento estricto y obligatorio. El aumento de la CPT durante dicho evento adverso se asoció indirectamente con el aumento de las variables de funcionamiento positivo (i.e. gratitud, sentido en la vida, resiliencia), a través de las mejoras en la satisfacción de la vida y el malestar emocional.
PALABRAS CLAVE: Pandemia COVID-19, confinamiento, variables de funcionamiento positivo, malestar emocional, crecimiento postraumático
Short abstract
背景:最近几个月, COVID-19疫情对心理健康的不良影响被广泛研究。但是, 很少有研究考查可能解释个体如何应对COVID-19疫情及其强制禁闭的保护性心理因素。
目的:本研究分析了因COVID-19疫情而导致的禁闭对正性功能变量 (心理韧性, 生活意义, 感恩, 同情心, 生活满意度), 情绪困扰 (抑郁, 焦虑, 感知压力, 情感) 和创伤后成长 (PTG) 的影响。在西班牙严格和强制禁闭的第一个月期间和之后测量了这些影响。
方法:在禁闭的第一阶段 (前两周), 样本由438名 (女性占78.3%) 年龄在18至68岁之间 (M = 35.68; SD = 13.19) 的西班牙居民组成。在禁闭的第二阶段 (第五周), 样本减少为197名参与者。进行了几次在线自我报告的问卷调查, 以评估正性功能变量, 情绪困扰和PTG。
结果:在禁闭的第一阶段, 女性, 青年, 没有伴侣, 收入较低或被具有精神障碍或慢性疾病诊断的人在正性功能变量方面得分较低, 在情绪困扰上得分较高。线性混合模型显示, 在禁闭的第二阶段, 正性功能变量, 情绪困扰和PTG的得分更差。然而, 结构方程模型显示, 第二阶段正性功能变量的增加与生活满意度的提高 (R2 = .450) 与情绪困扰的减少 (R2 = .186) 有关, 从而导致PTG的提高 (R2 = .061).
结论:个体可能在严格和强制禁闭期间体验到PTG。在此不良事件期间, 通过生活满意度和情绪困扰的改善, PTG的增加与正性功能变量 (即感恩, 意义的存在, 心理韧性) 的提升间接相关。
关键词: COVID-19疫情, 禁闭, 正性功能变量, 情绪困扰, 创伤后成长
1. Introduction
On 11 March 2020, the World Health Organization (WHO) declared a global pandemic due to the coronavirus (COVID-19), caused by the SARS-Cov-2 virus. At that time, America and Europe were the main focal points of the outbreak, and Spain was one of the most affected countries in terms of the number of people infected, the number of related deaths, and the drastic measures taken to manage the outbreak and confinement (e.g. isolation, cessation of non-essential activities, physical distancing, border closures). All these measures had severe impacts on health, social, and economic levels (Nicola et al., 2020). Recent studies have analysed the negative influence of these measures on mental health, finding increases in the rates of stress, anxiety, and other psychological problems (e.g. Brooks et al., 2020; Torales, O’Higgins, Castaldelli-Maia, & Ventriglio, 2020). Although it is essential to investigate the negative impact on mental health, it is also necessary to examine the protective factors that explain how people coped with the pandemic and the confinement. Moreover, analysing whether some ‘positive’ variables could prevent the development of psychological distress and promote growth in this situation seems crucial (Tamiolaki & Kalaitzaki, 2020).
Despite the risk of posttraumatic stress in adverse situations (e.g. pandemic), evidence shows that these situations can also be opportunities for improvement. More specifically, individuals can experience changes in their psychological functioning, such as Post-Traumatic Growth (PTG) (Lau, Yang, Tsui, Pang, & Wing, 2006; Tamiolaki & Kalaitzaki, 2020). PTG has been defined as ‘positive change that occurs as a result of the struggle with highly challenging life crises’ (Tedeschi & Calhoun, 2004, p. 1). This positive transformation involves the emergence of new opportunities in life, positive changes in personal relationships, an enhanced sense of personal strength, a greater appreciation of life, and spiritual changes (Tedeschi, Shakespeare-Finch, Taku, & Calhoun, 2018), without ruling out their possible coexistence with the adverse effects of trauma (Zięba, Wiecheć, Biegańska-Banaś, & Mieleszczenko-Kowszewicz, 2019). Several key factors may enhance or prevent the development of PTG, but there is scarce literature that addresses specifically growth during an epidemic. The present study focuses on the pandemic’s particular impact on psychological growth and the role of several positive aspects (i.e. resilience, gratitude, compassion, meaning in life, life satisfaction) in PTG when facing a world health crisis and confinement measures.
The scientific literature has also shown that a highly stressful situation is likely to promote changes in these positive functioning variables, such as resilience (Bonanno et al., 2007) or gratitude (Vernon, Dillon, & Steiner, 2009). In turn, several protective variables have been shown to affect PTG. ‘Resilience’ is positively correlated with PTG in individuals experiencing traumatic events (Connor & Davidson, 2003; Nishi et al., 2016; Ogińska-Bulik & Kobylarczyk, 2016). This psychological factor is characterized by successful adaptation to an adverse event and the return to adaptive functioning over time (Almedom, 2005), leading to personal growth (Westphal & Bonanno, 2007; Yates, Egeland, & Sroufe, 2003). ‘Gratitude’ experienced during trauma can also promote PTG (Jang & Kim, 2017) because individuals learn to interpret their life as a gift, adopting a more flexible and open-minded perspective, which facilitates their adaptation and growth (Kim & Bae, 2019). For instance, Fishman (2020) proposed a gratitude-based intervention during the COVID-19 crisis to promote well-being, happiness, and flourishing (Emmons, 2007; Fredrikson, 2009; Seligman, 2012). ‘Compassion’ towards strangers has also been shown to contribute to the development of PTG (Malhotra & Chebiyan, 2016). Compassion includes feelings, cognitions, and behaviours focused on the caring, concern, tenderness, and an orientation towards supporting, helping, and understanding others (Sprecher & Fehr, 2005, p. 630). Adopting a compassionate response to others in critical situations can allow growth and recognition of individual strengths through downward social comparison with those still struggling (Malhotra & Chebiyan, 2016). A ‘meaningful life’ allows individuals to re-evaluate traumatic events positively, empower the psychological resources needed to rediscover themselves, restore their fundamental assumptive world, and orient themselves towards future goals (Updegraff, Silver, & Holman, 2008). Previous studies found that a meaningful life was correlated with positive changes and significantly predicted PTG scores when facing different traumatic experiences (Dursun, Saracli, & Konuk, 2014; Linley & Joseph, 2011; Steger, Frazier, & Zacchanini, 2008). Finally, ‘life satisfaction’ is a critical and fluctuating factor in the presence of traumatic situations (Calhoun, Cann, & Tedeschi, 2010). Life satisfaction has been theoretically conceptualized as a holistic or global judgemental process of one’s life, in which the positive functioning variables may have an influence (Pavot & Diener, 2008).
One of the mechanisms that could explain the effect of positive functioning variables on PTG could be the level of positive emotions.1 For instance, Fredrickson, Tugade, Waugh, and Larkin (2003) found that positive emotions may emerge after a stressful situation. They found that the resilience predicted the experience of positive emotions after the terrorist attacks on September 11th, and they in turn, predicted the growth in psychological resources in the long term. According to the Broaden and Build Theory proposed by Fredrickson (2001), certain positive emotions can broaden individuals’ momentary thought-action repertoires, inciting them to experience a broader range of thoughts and actions (e.g. to integrate current life circumstances, to find new and creative solutions to current situations, to find resources to build our wellbeing), and lead to the creation of enduring personal resources (e.g. social, intellectual or psychological resources).
To our knowledge, there is limited evidence about how changes in positive functioning variables or psychological resources (e.g. gratitude, resilience) could contribute to higher or lower PTG when facing adversity through buffering emotional distress, especially when the stressor is still present, as in the current study. The general aim of the present study is to analyse the variables associated with the promotion of PTG (i.e. new possibilities, relating to others, personal strength, appreciation of life, and spiritual change) in this negative, collective, uncertain, unexpected, and threatening situation. To do so, in addition to PTG, variables related to positive functioning (i.e. resilience, gratitude, compassion towards strangers, meaning in life, life satisfaction) and emotional distress (i.e. anxiety, depression, perceived stress, negative/positive affect) were assessed during the first two weeks of confinement (i.e. between March 21 and March 29) and during the fifth week of confinement (i.e. on April 19).
The specific objectives were: (1) to explore the differences between sociodemographic variables (i.e. sex, age, mental illness or chronic illness diagnosis, being a healthcare professional, living alone, being in a relationship, and income level) on positive functioning variables, emotional distress, and PTG during the first two weeks of confinement; (2) to analyse the relationships between positive functioning variables, emotional distress, and PTG during the first two weeks of confinement; (3) to investigate the changes in positive functioning variables, emotional distress, and PTG from the first two weeks of confinement to the fifth week; and (4) to analyse whether the improvement in positive functioning variables has an indirect effect on the increase in PTG through the decrease in emotional distress.2 Specifically, we hypothesized that there would be differences on individuals based on their sociodemographic variables in their scores of the study variables (positive functioning variables, emotional distress, and PTG) (Hypothesis 1). In addition, negative correlations would be observed between positive functioning variables and emotional distress, as well as positive correlations between positive functioning variables and PTG at the onset of the confinement (Hypothesis 2). We also hypothesized that there would be changes in positive variables, emotional impact and PTG between the initial moments of confinement and several weeks later (Hypothesis 3).3 Finally, we expect that increases in positive variables would lead to an increase in life satisfaction, related to a decrease in emotional distress, which in turn would predict a greater increase in PTG. (Hypothesis 4).
2. Method
2.1. Participants
This study sample consisted of 438 volunteers (78.3% women) between the ages of 18 and 68 (M = 35.68; SD = 13.19). The inclusion criteria were that they had to be at least 18 years old and living in Spain at the time of confinement. No exclusion criteria were established. During the first two weeks of confinement (i.e. at baseline), the survey was open from March 21 to 29 March 2020.
In the follow-up, in the fifth week of confinement (on April 19), only 197 participants (out of the initial 438) answered the survey again [82.7% women, between the ages of 18 and 68 years old (M = 36.31; SD = 13.42)]. Given the high level of respondent’s attrition, the differences of the sociodemographic measures of respondents and non-respondents in the second assessment were analysed. Chi-squared tests and independent sample t-tests revealed that there were not significant differences between respondents and non-respondents in the second assessment on: age, t(436) = −0.90, p = .367; sex, χ2 (1, N = 438) = 3.27, p = .071; marital status, χ2 (1, N = 438) = 6.38, p = .271; monetary income, χ2 (1, N = 438) = 0.62, p = .969; diagnosis of mental illness, χ2 (1, N = 438) = 0.15, p = .901; diagnosis of chronic illness, χ2 (1, N = 438) = 2.27, p = .132; working as a healthcare professional, χ2 (2, N = 438) = 0.47, p = .789; employment situation, χ2 (5, N = 438) = 7.54, p = .184; being fired during the confinement, χ2 (1, N = 438) = 0.50, p = .480.
2.2. Procedure
Participants were contacted through different social networks (WhatsApp, Facebook, Twitter, and Instagram) and invited to participate in a study to evaluate positive psychological factors during the COVID-19 quarantine in Spain. A raffle for 10 Amazon gift cards worth 40 euros each was offered to encourage participation.
All the participants signed an online informed consent before being included in the study. Next, they completed the online survey through the Qualtrics platform (https://www.qualtrics.com). The average time to complete the survey was 25–30 minutes.
This study began on March 21, seven days after the declaration of the state of alarm in Spain and the imposition of confinement measures. Spain was one of the countries most affected by the pandemic during that period (e.g. on March 25, the death toll in Spain surpassed that of China and was only higher in Italy), and Spanish citizens experienced strict confinement measures (i.e. all citizens were ordered to remain in their residences except to purchase food and medicine, and non-essential shops and businesses were closed). From March 21 to March 29, participants in this study had the opportunity to answer the first questionnaire. March 29 was the day the Spanish government imposed even stricter confinement measures (i.e. suspension of all non-essential activities, except those related to the maintenance of essential social functions or the efficient operating of state and public administrations), in order to limit general circulation as much as possible. The second assessment was carried out on April 19, when confinement measures were relaxed (i.e. the strictest measures ended on April 19, but confinement was still mandatory).
The study was conducted following the principles outlined in the Declaration of Helsinki (World Medical Association, 2013), and it received approval from the ethical committee of the University of Valencia (Spain) (register number: 1593681212393).
2.3. Measures
2.3.1. Socio-demographic characteristics, housing-related variables, and health-related and economic consequences of the coronavirus
The following variables were assessed: sex, age, marital status, diagnosis of mental and chronic illness, monetary income, employment situation, working as a healthcare professional, employment status during the coronavirus situation, size of the home, home with a terrace, number of children <18 years old living at home, living with a disabled person, living with a pet, and the percentage of individuals affected by the coronavirus in terms of health and economy.
2.3.2. Positive functioning measures
2.3.2.1. Meaning in life
The Meaning in Life Questionnaire (MLQ: Steger, Frazier, Oishi, & Kaler, 2006; Steger et al., 2008) is a 10-item self-report questionnaire designed to measure two dimensions of meaning in life: (1) presence of meaning (MLQ-P; e.g. ‘My life has a clear sense of purpose’), and (2) search for meaning (MLQ-S; ‘I am seeking a purpose or mission for my life’). Each dimension is measured by five items on a 7-point Likert-type scale (1 = absolutely true, 7 = absolutely untrue). The total sum scores on each subdimension range from 5 to 35, where higher scores indicate a higher level on the measured MLQ dimensions. In this study, the internal consistencies for the scores for presence of meaning were α = .91 at baseline and α = .91 for the follow-up assessment, whereas for the search for meaning, they were α = .93 and α = .94, respectively.
2.3.2.2. Gratitude
The Gratitude Questionnaire-6 (GQ-6; Magallares, Recio, & Sanjuán, 2018; McCullough, Emmons, & Tsang, 2002) consists of a 6-item self-report questionnaire designed to assess individual differences in the tendency to experience gratitude in daily life. Items are scored on a 7-point Likert-type scale (1 = strongly disagree; 7 = strongly agree). The total sum score ranges from 6 to 42, with higher scores indicating a higher level of gratitude. In this study, the internal consistency for the total score was α = .70 at baseline and α = .67 at the follow-up assessment.
2.3.2.3. Resilience
The Connor-Davidson Resilience Scale (CD-RISC; Campbell‐Sills & Stein, 2007; Notario-Pacheco et al., 2011) is a 10-item self-report questionnaire to measure resilience. Items are scored on a 5-point Likert-type scale (0 = not true at all, 4 = true nearly all the time). The total sum score ranges from 0 to 40, and higher scores indicate greater resilience. The internal consistency for the total score in this study was α = .86 at baseline and α = .84 at the follow-up assessment.
2.3.2.4. Compassion towards strangers
The Compassionate Love Scale for Humanity (CLS-H; Chiesi, Lau, & Saklofske, 2020; Spanish validation by the authors) is a 9-item self-report questionnaire that evaluates the degree to which an individual feels compassion or altruistic love towards strangers, selfless caring, and the motivation to help humanity. Items are scored on a 6-point Likert-type scale (1 = not at all true of me, 6 = very true of me). The total sum score ranges from 9 to 54. The internal consistency for the total score in this study was α = .91 at baseline and α = .91 for the follow-up assessment.
2.3.2.5. Life satisfaction
The Satisfaction with Life Scale (SWLS; Diener, Emmons, Larsen, & Griffin, 1985; Vázquez, Duque, & Hervás, 2013) is a 5-item self-report questionnaire to assess the global cognitive component of subjective well-being. Items are rated on a 7-point Likert-scale (1 = strongly disagree, 7 = strongly agree). The total sum score ranges from 5 to 35, where higher scores indicate greater life satisfaction. The internal consistency for the total score in this study was α = .88 at baseline and at follow-up.
2.3.3. Emotional distress measures
2.3.3.1. Perceived stress (PS)
An ad-hoc visual analogue scale developed by the authors was composed of two items that assessed the degree to which current life situations were appraised as stressful: ‘I’ve felt that I can deal with all the things I should do’; ‘I’ve managed the small daily problems.’ Item responses were rated from 1 (never) to 5 (very often). The total sum score ranged from 2 to 10. The internal consistency for the total score in this study was α = .80 at baseline and α = .79 at the follow-up assessment.
2.3.3.2. Symptoms of depression
The Patient Health Questionnaire-2 (PHQ-2; Kroenke, Spitzer, & Williams, 2003; Rodríguez-Muñoz et al., 2017) is a 2-item self-report questionnaire that is used to screen and detect depressive symptomatology. Item responses are rated on a 4-point Likert-scale (0 = not at all, 3 = nearly every day). The total sum score ranges from 0 to 6. A cut-off score of ≥ 3 is suggested as indicating a possible diagnosis of depressive disorder (Kroenke et al., 2003). The internal consistency for the total score in this study was α = .82 at baseline and α = .80 at the follow-up assessment.
2.3.3.3. Symptoms of anxiety
The Generalized Anxiety Disorder Questionnaire-2 (GAD-2; García-Campayo et al., 2012; Kroenke, Spitzer, Williams, Monahan, & Löwe, 2007) is a 2-item self-report that can be used to screen and detect symptoms of anxiety. Items are scored on a 4-point Likert-type scale (0 = not at all, 3 = nearly every day). The total sum score ranges from 0 to 6. A score of ≥ 3 on the GAD-2 has been identified as an acceptable cut-off score for identifying clinically significant symptoms of anxiety (Kroenke et al., 2007). The internal consistency for the total score in this study was α = .67 at baseline and α = .71 at the follow-up assessment.
2.3.3.4. Positive and negative affect
Positive and Negative Affect Schedule (PANAS; López-Gómez, Hervás, & Vázquez, 2015; Watson, Clark, & Tellegen, 1988). The PANAS consists of 20 items that evaluate two independent dimensions: positive affect (PANAS positive) and negative affect (PANAS negative). The total sum score for each subscale ranges from 5 to 50, using a 5-point Likert-type scale (1 = not at all, 5 = very much). In this study, the internal consistency for the scores on positive affect was α = .92 at baseline and α = .92 at the follow-up assessment, whereas for negative affect, they were α = .87 and α = .89, respectively.
2.3.4. Posttraumatic growth measure
2.3.4.1. PTG
The short form of the PTG Inventory (PTGI-SF; Cann et al., 2010; Cárdenas, Barrientos, Ricci, & Páez, 2015) is a 10-item scale that measures the extent to which individuals report positive life changes in the aftermath of a major life crisis. Items assess each of the five dimensions of PTGI: new possibilities, relating to others, personal strength, appreciation of life, and spiritual change. Items are scored on a 6-point Likert-type scale (1 = I did not experience this change as a result of the event; 6 = I experienced this change to a very great degree as a result of the event). The total sum scores on each subdimensions ranged from 2 to 12. In this study, the internal consistency for the scores on ‘new possibilities’ was α = .73 at baseline and α = .75 at the follow-up assessment; for ‘relating to others’, α = .78 and α = .77; for ‘personal strength’, α = .81 and α = .79; for ‘appreciation of life’, α = .84 and α = .84; and for ‘spiritual change’, α = .48 and α = .47, respectively.
3. Data analyses
First, descriptive statistics were calculated to explore the demographic characteristics, housing-related variables, and percentage of individuals affected by the coronavirus in terms of the health and economy of the sample, both in the first two weeks of confinement and in the fifth week at the follow-up. The sample’s normality was assumed because skewness values were <2 and kurtosis values were <7 in absolute value (Russell, 2002; West, Finch, & Curran, 1995).
Second, independent-samples t-tests and one-way ANOVAs were performed to test whether there were significant differences in positive functioning variables, emotional distress, and PTG according to the sociodemographic variables. Pairwise comparisons of one-way ANOVAs were followed by adjustments using Holm-Bonferroni correction for multiple comparisons (Holm, 1979), using an Excel calculator (Gaetano, 2018). Effect sizes and their 95% Confidence Intervals (CI) were calculated for between-group. The formulas used to calculate effect sizes can be found in Lakens (2013). For calculating unbiased Cohen’s d (or Hedges g) formula number 4 (Lakens, 2013, p. 3) was used and for calculating partial eta squared formula number 13 (Lakens, 2013, p. 6) was used. Partial eta squared of .01, .06, and .14, and Hedges’ g of 0.02, 0.05, and 0.08 were considered, respectively, small, medium, and large effect sizes (Cohen, 1988).
Third, Pearson’s correlations were calculated between the positive functioning variables (GQ-6, MLQ-P, MLQ-S, CD-RISC, CLS-H, SWLS), emotional distress (GAD-2, PHQ-2, PS, PANAS), and PTG (PTGI-SF).
Fourth, linear mixed models were employed for each study variable using the MIXED procedure with one random intercept per subject and without ad hoc imputation. An identity covariance structure was specified to model the covariance structure of the random intercept. For each outcome, time was treated as a within-group factor. Effect size and their 95% CI were calculated for within-group comparisons following the formula number 9 included in Lakens (2013, p. 4), with Hedges’ g correction (Hedges’ g = Cohen’s . Thus, we used raw scores and not linear mixed model estimates. For calculating the 95% confidence intervals of all the effect sizes, we used the effect size calculator based on Uanhoro (2017).
Fifth, Pearson’s correlations were calculated in order to analyse the relationships between the changes in the scores. Finally, two structural equation models were hypothesized, tested, and evaluated. Both of them included a sequence in which the change in four positive functioning variables, including gratitude (GQ-6), presence of meaning in life (MLQ-P), compassion towards strangers (CLS-H), and resilience (CD-RISC), affected participants’ life satisfaction. Life satisfaction affected, in turn, levels of emotional distress, and, finally, distress affected PTG. Life satisfaction, distress, and PTG were modelled as latent factors: life satisfaction, with the measurement model consisting of the five items from the SWLS; distress, with the PHQ-2, GAD-2, PS, and the two dimensions of the PANAS (positive and negative affect) as indicators; and finally, PTG measured with the five dimensions (new possibilities, relation to others, personal strength, spiritual change, and appreciation of life) of the PTGI-SF. However, whereas the first model (partial mediation) included the direct effects of the change in the four positive variables on emotional distress and PTG and the effect of life satisfaction on PTG, the second model (complete mediation) only hypothesized the indirect effects of these variables, but not the direct ones. After comparing the models’ fit, an additional third model was tested. In this model, a correlation between the error terms of the GAD-2 and PANAS negative affect was added to the best fitting model. The goodness of fit was assessed using several fit criteria (Kline, 2015; Tanaka, 1993), including: a) the chi-square statistic, which tests the differences between the observed covariance matrix and the one predicted by the specified model; b) the Comparative Fit Index (CFI), which assumes a non-central chi-square distribution with cut-off criteria of .90 or more (ideally, over .95) indicating adequate fit (Hu & Bentler, 1999); and c) the root mean square error of approximation (RMSEA), with values of .08 considered a reasonable fit (Kline, 2015), and its 90% confidence interval (CI). Finally, the fit of the models was compared. The chi-square difference test has traditionally been used to test for fit differences between nested models (Byrne, 2012). However, there is an increasing tendency to use subjective criteria to make inferences about differences between the CFIs of the models tested. Whereas some authors argue that a difference of .05 or less between two CFIs can be considered negligible (Little, 1997), other authors suggest that this difference value should not exceed .01 (Cheung & Rensvold, 2002). Whenever these differences between competing models with varying parsimony are negligible, the most parsimonious model is chosen because it allows us to test (as explained) for moderation effects. Additionally, the analytical fit of the model was evaluated, including the absence of large modification indices and the strength and interpretability of the estimates. Indirect effects were also calculated, and the CI around the estimate of the effects were also estimated using a bootstrap resampling method. This procedure was recommended as the best method to generate the required sampling distributions for testing indirect effects (MacKinnon, Fairchild, & Fritz, 2007). The model was estimated with Weighted Least Squares Mean and Variance corrected (WLSMV), which is the method of choice given the categorical (ordinal) nature of the variables (Finney & DiStefano, 2006).
All statistical analyses were performed using SPSS v.26 and Mplus v.8 (Muthén & Muthén, 2017).
4. Results
4.1. Descriptive characteristics of the sample
Demographic characteristics, housing-related variables, and percentage of individuals affected by the coronavirus in terms of health and economy are shown in Tables 1–3, both for the sample that participated in the first two weeks of confinement and for those who participated in the fifth week at the follow-up.
Table 1.
Demographic characteristics of the sample
| First two weeks of confinement (March 21 – March 29) N = 438 |
Fifth week of confinement (April 19) N = 197 |
|
|---|---|---|
| Sex (%women) | 78.3% | 82.7% |
| Age (years) M (SD) | 35.68 (13.19) | 36.31 (13.42) |
| 18–24 years old | 25.3% | 21.3% |
| 25–35 years old | 32.4% | 36.0% |
| 36–50 years old | 25.1% | 24.9% |
| >50 years old | 17.1% | 17.8% |
| Diagnosis of Mental illness (% yes) | 5.9% | 6.1% |
| Diagnosis of Chronic disease (% yes) | 18.7% | 21.8% |
| Marital status | ||
| Single | 27.4% | 26.9% |
| In a relationship | 37.2% | 36.5% |
| Married | 26.7% | 24.9% |
| Divorced/Separated | 7.1% | 9.1% |
| Widowed | 0.7% | 1.5% |
| Other | 0.9% | 1.0% |
| Monetary income | ||
| Below the mean | 36.1% | 36.5% |
| At the mean | 50.9% | 50.3% |
| Above the mean | 13.0% | 13.2% |
| Employment situation | ||
| Employee (permanent job) | 39.7% | 37.6% |
| Employee (temporal job) | 16.9% | 18.8% |
| Freelancer | 4.8% | 3.0% |
| Job seeker | 7.8% | 7.1% |
| Student | 23.1% | 22.8% |
| Other | 7.8% | 10.7% |
| Healthcare professional | ||
| Yes (working currently) | 8.7% | 8.1% |
| Yes (but not working currently) | 11.6% | 12.7% |
| Employment situation during coronavirus crisis | ||
| Teleworking | 36.8% | 35.0% |
| Regular workplace (partial time) | 3.4% | 3.6% |
| Regular workplace (full time) | 8.4% | 7.1% |
| Studying | 25.3% | 24.4% |
| Unemployed | 26.2% | 29.9% |
Table 2.
Housing-related characteristics of the sample
| First two weeks of confinement (March 21 – March 29) N = 438 |
Fifth week of confinement (April 19) N = 197 |
|
|---|---|---|
| Size of the house | ||
| Small (small apartment or loft) | 19.2% | 20.8% |
| Medium (medium apartment or house) | 60.0% | 59.9% |
| Large (big apartment or house, detached | 20.5% | 19.3% |
| house, bungalow, duplex) | ||
| Other | 0.2% | 0% |
| House with terrace (% yes) | 69.6% | 69.5% |
| Number of children < 18 years old living with | ||
| None | 78.5% | 79.7% |
| 1 | 10.5% | 9.6% |
| 2 | 9.8% | 8.6% |
| 3 | 0.7% | 1.5% |
| ≥ 4 | 0.5% | 0.5% |
| Number of people living with | ||
| None | 8.9% | 9.6% |
| 1 | 31.7% | 35.5% |
| 2 | 26.0% | 25.4% |
| 3 | 21.5% | 17.3% |
| 4 | 9.4% | 9.1% |
| ≥ 5 | 2.5% | 3.0% |
| Living with a disabled person | ||
| None | 89.3% | 86.8% |
| Older than 70 years old | 4.3% | 3.6% |
| Chronic illness | 3.2% | 3.6% |
| Mental disorder | 1.1% | 2.5% |
| Other | 2.1% | 3.6% |
| Living with a pet | 39.7% | 41.1% |
Table 3.
Percentage of participants affected by the coronavirus in terms of health or economy
| First two weeks of confinement (March 21 – March 29) N = 438 |
Fifth week of confinement (April 19) N = 197 |
|
|---|---|---|
| In contact with coronavirus | ||
| A formal Diagnosis of coronavirus (% yes) | 1.6% | 3.6% |
| Believed to be affected by the coronavirus | ||
| No | 72.8% | 61.4% |
| Yes | 24.7% | 8.1% |
| Not completely sure | 2.5% | 30.5% |
| Relative or friend with a formal diagnosis | 13.2% | 37.1% |
| Fired during coronavirus crisis (% yes) | 10.0% | 10,7% |
| Fear of being fired | ||
| Not at all | 58.0% | 57.9% |
| A little | 22.1% | 22.3% |
| Moderately | 9.1% | 8.1% |
| Some | 6.4% | 8.6% |
| A lot | 4.3% | 3.0% |
4.2. Differences in positive functioning variables, emotional distress, and PTG depending on sociodemographic variables
Descriptive statistics and results of independent-sample t-tests and one-way ANOVAs are shown in Supplementary Information 1. The main results of each sociodemographic variable are summarized in this subsection.
4.2.1. Sex
Women (vs. men) showed significantly lower scores on resilience and positive affect. Moreover, women (vs. men) showed significantly higher scores on compassion and emotional distress (i.e. perceived stress, symptoms of depression and anxiety, and negative affect).
4.2.2. Age-range
Younger individuals (‘18–24’ year-old individuals vs. ‘25–34’ vs. ‘35–50’ vs. ‘50–68’) showed higher scores on emotional distress (i.e. symptoms of depression, perceived stress, and negative affect, and lower scores on positive affect) and lower scores on positive functioning variables (i.e. meaning in life, life satisfaction, resilience, and gratitude; but higher scores on search for meaning in life).
4.2.3. Diagnosis of mental illness
Individuals diagnosed with a mental illness (vs. those not diagnosed) showed lower scores on positive functioning variables (i.e. presence of meaning in life, gratitude, resilience, life satisfaction; but higher scores on search for meaning in life), higher scores on emotional distress (i.e. perceived stress, symptoms of depression and anxiety, and negative affect; but lower scores on positive affect), and lower scores on PTG in relating to others.
4.2.4. Diagnosis of chronic illness
Individuals diagnosed with a chronic illness (vs. those not diagnosed) showed higher scores on the presence of meaning and symptoms of anxiety.
4.2.5. Living alone or not
Individuals living alone did not show significant differences from individuals living with others on any variable.
4.2.6. Being in a relationship or not
Individuals in a relationship or married (vs. single, widowed, or divorced/separated) had higher scores on positive functioning variables (i.e. presence of meaning in life, gratitude, and life satisfaction; but lower scores on search for meaning in life).
4.2.7. Currently working as a healthcare professional or not
Healthcare professionals currently working (vs. healthcare professionals not currently working vs. non-healthcare professionals) showed lower scores on positive functioning variables (i.e. higher scores on the presence of meaning and life satisfaction; but lower scores on search for meaning) and lower emotional distress (i.e. perceived stress and symptoms of depression; but higher scores on positive affect).
4.2.8. Monetary income
Individuals with lower monetary incomes (vs. medium and high monetary incomes) showed lower scores on positive functioning variables (i.e. presence of meaning in life, life satisfaction, gratitude, resilience; but higher scores on search for meaning in life) and higher scores on emotional distress (i.e. perceived stress, symptoms of depression, negative affect; but lower scores on positive affect)
4.3. Relationships between positive functioning variables, emotional distress, and PTG in the first two weeks of confinement
Pearson’s correlations between the study variables are shown in Supplementary Information 2. The main results of the significant correlations are summarized in this subsection.
4.3.1. Positive functioning variables
Significant positive relationships were found among the positive functioning variables – except ‘search for meaning’, which was negatively correlated. In contrast, overall, significant negative relationships were found between positive functioning variables and emotional distress – except for the positive relationship between compassion and symptoms of anxiety. The relationships between the positive functioning variables and positive affect were positive – except for ‘search for meaning’, which was negatively correlated. Finally, overall, significant positive relationships were found between the positive functioning variables and the five PTG dimensions.
4.3.2. Emotional distress variables
Significant positive relationships were found among these variables. Positive affect was negatively correlated with the rest of the emotional distress variables. Moreover, the emotional distress variables (including high positive affect) were positive and significantly associated with the dimensions of PTG.
4.3.3. PTG
Significant positive relationships were found among the dimensions of PTG.
4.4. Changes in positive functioning variables, emotional distress, and PTG from the first two weeks to the fifth week of confinement
Main effects of time were found on several positive functioning variables, emotional distress, and PTG. Table 4 shows the descriptive statistics, the linear mixed model results, and the within-group effect size (Hedges’ g, 95% CI). Results showed that lower scores were achieved in the fifth week (vs. the first two weeks) on the following variables: positive functioning variables (i.e. presence of meaning, search for meaning, gratitude, resilience, compassion), emotional distress (i.e. perceived stress, symptoms of depression), and PTG (i.e. relating to others, appreciation of life, and spiritual changes).
Table 4.
Differences in the study variables between the first two weeks and the fifth week of confinement (N = 197)
| First two weeks of confinement (21st – 29th March) M (SD) |
Fifth week of confinement (April 19) M (SD) |
Linear mixed models | Within-group effect size, g [95% CI] a First two weeks – fifth week |
||
|---|---|---|---|---|---|
| Positive functioning variables | 1. Presence of meaning (MLQ-P) | 25.49 (6.44) | 24.88 (6.67) | F(1,190.925) = 4.31, p = .039 | 0.09 [−0.00, 0.19] |
| 2. Search for meaning (MLQ-S) | 18.83 (8.44) | 16.70 (8.48) | F(1,191.278) = 18.32, p < .001 | 0.25 [0.14, 0.36] | |
| 3. Gratitude (GQ-6) | 36.13 (4.73) | 34.32 (6.31) | F(1,196) = 25.97, p < .001 | 0.31 [0.20, 0.45] | |
| 4. Resilience (CD-RISC) | 30.36 (5.64) | 29.47 (6.16) | F(1,196.000) = 8.86, p = .003 | 0.15 [0.05, 0.25] | |
| 5. Compassion towards strangers (CLS-H) | 39.80 (8.53) | 38.64 (9.28) | F(1,196.000) = 11.59, p < .001 | 0.13 [0.05, 0.21] | |
| 6. Life Satisfaction (SWLS) | 23.57 (6.50) | 23.33 (6.50) | F(1,190.880) = 0.70, p = .405 | 0.04 [−0.05, 0.14] | |
| Emotional distress | 7. Perceived Stress (PS) | 1.62 (1.41) | 1.84 (1.45) | F(1,196) = 4.74, p = .031 | −0.15 [−0.29, −0.01] |
| 8. Symptoms of depression (PHQ-2) | 1.47 (1.53) | 1.93 (1.55) | F(1,193.317) = 18.65, p < .001 | −0.30 [−0.43, −0.16] | |
| 9. Symptoms of anxiety (GAD-2) | 2.15 (1.71) | 2.08 (1.67) | F(1,191.697) = 0.49, p = .484 | 0.04 [−0.11, 0.20] | |
| 10. Positive affect (PANAS positive) | 27.40 (7.81) | 27.20 (8.89) | F(1,196) = 0.13, p = .714 | 0.02 [−0.10, 0.15] | |
| 11. Negative affect (PANAS negative) | 19.99 (6.85) | 19.10 (7.25) | F(1,196) = 3.68, p = .056 | 0.13 [−0.00, 0.26] | |
| PTG dimensions | 12. New possibilities (PTGI-SF) | 4.71 (2.74) | 4.83 (2.65) | F(1,196.000) = 0.52, p = .474 | −0.04 [−0.17, 0.08] |
| 13. Relating to others (PTGI-SF) | 6.31 (2.97) | 5.56 (2.93) | F(1,196.000) = 16.13, p < .001 | 0.25 [0.13, 0.38] | |
| 14. Personal strength (PTGI-SF) | 5.29 (2.99) | 5.61 (2.96) | F(1,196.000) = 2.52, p = .114 | −0.11 [−0.24, 0.03] | |
| 15. Appreciation of life (PTGI-SF) | 6.04 (3.15) | 5.62 (2.96) | F(1,196) = 4.41, p = .037 | 0.14 [0.01, 0.26] | |
| 16. Spiritual change (PTGI-SF) | 3.51 (2.13) | 3.20 (2.02) | F(1,196.000) = 5.15, p = .024 | 0.15 [0.02, 0.28] |
MLQ = The Meaning in Life Questionnaire; GQ-6 = The Gratitude Questionnaire-6; CD-RISC = The Connor-Davidson Resilience Scale; CLS-H = The Compassionate Love Scale for Humanity; SWLS = The Satisfaction with Life Scale; PS = Perceived Stress; PHQ-2 = The Patient Health Questionnaire-2; GAD – 2 = The Generalized Anxiety Disorder Questionnaire-2; PANAS Positive and Negative Affect Schedule; PTGI-SF = short form of the Posttraumatic Growth Inventory. a Hedges’ g correction of Cohen’s d effect size for repeated measures with one group was used (Lakens, 2013, p. 4), using more conservative raw scores and not linear mixed model estimates.
4.5. Relationships between changes in the study variables from the first two weeks to the fifth week of confinement
Pearson’s correlations between the changes in study variables are shown in Table 5. Changes in positive functioning variables, emotional distress, and PTG between the second and fifth weeks of confinement were calculated (i.e. scores in the fifth week minus scores in the second week). The correlations of Table 5 show the associations between the differences from the first phase (the first two weeks) to the second phase (the fifth week) of assessment, regarding whether the variables of interest increase or decrease in the same direction. The main results of the significant correlations are summarized in this subsection.
Table 5.
Relationships between changes in the study variables between the first two weeks and the fifth week of confinement (N = 197)
| Positive functioning variables |
Emotional distress |
PTG dimensions |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | ||
| Positive functioning variables | 1. Presence of meaning (MLQ-P) | 1 | |||||||||||||||
| 2. Search for meaning (MLQ-S) | −.13 | 1 | |||||||||||||||
| 3. Gratitude (GQ-6) | .27*** | −.01 | 1 | ||||||||||||||
| 4. Resilience (CD-RISC) | .35*** | −.07 | .26** | 1 | |||||||||||||
| 5. Compassion towards strangers (CLS-H) | .06 | .02 | .04 | .25*** | 1 | ||||||||||||
| 6. Life Satisfaction (SWLS) | .48*** | −.08 | .34** | .36*** | .01 | 1 | |||||||||||
| Emotional distress | 7. Perceived Stress (PS) | −.01 | .14 | −.11 | −.17* | −.09 | −.14 | 1 | |||||||||
| 8. Symptoms of depression (PHQ-2) | −.04 | .15* | −.12 | −.13 | −.02 | −.13 | .37*** | 1 | |||||||||
| 9. Symptoms of anxiety (GAD-2) | −.10 | −.00 | .01 | −.19** | .02 | −.21** | .16* | .27*** | 1 | ||||||||
| 10. Positive affect (PANAS positive) | .14* | −.10 | .24*** | .30*** | .12 | .27*** | −.44*** | −.43*** | −.13 | 1 | |||||||
| 11. Negative affect (PANAS negative) | −.21** | −.05 | −.22** | −.23*** | .00 | −.23*** | .15* | .28*** | .61*** | −.30*** | 1 | ||||||
| PTG dimensions | 12. New possibilities (PTGI-SF) | −.03 | .16* | .03 | −.06 | .08 | .06 | −.13 | −.19** | −.04 | .16* | −.11 | 1 | ||||
| 13. Relating to others (PTGI-SF) | −.01 | .08 | .00 | .02 | .05 | .19** | −.20** | −.10 | −.03 | .11 | −.00 | .51*** | 1 | ||||
| 14. Personal strength (PTGI-SF) | .01 | .14 | .07 | .06 | .07 | .09 | −.15* | −.22** | −.07 | .28*** | −.12 | .70*** | .57*** | 1 | |||
| 15. Appreciation of life (PTGI-SF) | −.14 | .16* | .04 | .00 | .06 | .03 | −.14* | −.05 | −.03 | .03 | .01 | .57*** | .49*** | .45*** | 1 | ||
| 16. Spiritual change (PTGI-SF) | .04 | .01 | −.02 | −.03 | .17* | .06 | −.07 | −.03 | .01 | .04 | −.03 | .50*** | .46*** | .43*** | .34*** | 1 | |
| M (SD) | −0.70 (4.52) | −2.02 (6.62) | −1.80 (4.96) | −0.89 (4.19) | −1.16 (4.79) | −0.24 (4.03) | 0.22 (1.44) | 0.44 (1.45) | −0.90 (1.63) | −0.19 (7.38) | −0.89 (6.54) | 0.13 (2.48) | −0.75 (2.63) | 0.32 (2.83) | −0.41 (2.75) | −0.30 (1.88) | |
*** p < .001; ** p < .01; * p < .05. MLQ = The Meaning in Life Questionnaire; GQ-6 = The Gratitude Questionnaire-6; CD-RISC = The Connor-Davidson Resilience Scale; CLS-H = The Compassionate Love Scale for Humanity; SWLS = The Satisfaction with Life Scale; PS = Perceived Stress; PHQ-2 = The Patient Health Questionnaire-2; GAD – 2 = The Generalized Anxiety Disorder Questionnaire-2; PANAS Positive and Negative Affect Schedule; PTGI-SF = short form of the Posttraumatic Growth Invent.
4.5.1. Positive functioning variables
Overall, the following significant relationships were found: (1) significant positive relationships among the changes in the positive functioning variables ─except for ‘change in search for meaning’, which did not correlate with any other change in positive functioning variable─; (2) significant negative relationships between the positive functioning variables and emotional distress, and significant positive relationships with positive affect; and (3) non-significant relationships between the positive functioning variables and PTG ─except for specific significant relationships between change in the search for meaning, compassion, and life satisfaction and some of the dimensions of PTG─.
4.5.2. Emotional distress
Overall, the following significant relationships were found: (1) significant positive relationships among the changes in emotional distress ─except for the significant negative relationships found between the ‘change in positive affect’ and the rest of the changes in emotional distress─; and (2) significant negative relationships between changes in variables of emotional distress and PTG, as well as significant positive relationships between positive affect and some dimensions of PTG.
4.5.3. PTG
Significant positive relationships were found among the changes in the dimensions of PTG.
4.6. Results of the predictive model: do the changes in positive functioning variables predict the change in PTG through life satisfaction and emotional distress?
After exploring the Pearson’s correlations shown in Table 5, two structural equation models were hypothesized, tested, and evaluated (partial and complete mediation models). Both models included a sequence that tested whether changes in positive functioning variables (i.e. presence of meaning, gratitude, compassion, resilience)4 predicted the change in PTG through the change in life satisfaction and emotional distress, as proposed in our fourth hypothesis. Table 6 shows the fit indexes for these models. Because the most parsimonious model was also the best fitting one, it was retained as the best representation of the data. However, the overall fit was not completely satisfactory, and a posteriori modification was included (as recommended by the modification indices): the correlation between the error terms of GAD-2 and PANAS negative affect. This latest model showed an adequate fit (see Table 6).
Table 6.
Fit indexes for the structural equation models tested
| χ2 | df | p | CFI | RMSEA | RMSEA CI | |
|---|---|---|---|---|---|---|
| Partial mediation model | 235.429 | 135 | <.001 | .887 | .062 | [.048, .075] |
| Complete mediation model | 235.073 | 144 | <.001 | .898 | .057 | [.043, .070] |
| Complete mediation model with a posterior modification | 211.772 | 143 | <.001 | .923 | .050 | [.035, .063] |
CFI = Comparative Fit Index; RMSEA = Root mean Squared Error of Approximation; RMSEA CI = RMESEA 90% Confidence Interval.
The standardized estimation parameters are shown in Figure 1. All the a priori structural effects were statistically significant – except for the effect of the increase in compassion on the increase in life satisfaction – providing support for the theoretical model. The model showed medium effects for the hypothesized effects. The changes in positive functioning variables throughout the pandemic explained 45% (R2 = .450) of the variance in life satisfaction during this same period of time. Among these changes, change in gratitude showed the highest predictive power and was the most important variable in changing life satisfaction. The explained variance of the change in distress was 18.6% (R2 = .186), with a negative relationship with change in life satisfaction: increases in levels of life satisfaction during the pandemic were related to decreases in distress. Finally, change in emotional distress explained 6.1% of the change in post-traumatic growth (R2 = .061), pointing to a negative relationship between these two variables: decreases in emotional distress were related to increases in post-traumatic growth.
Figure 1.
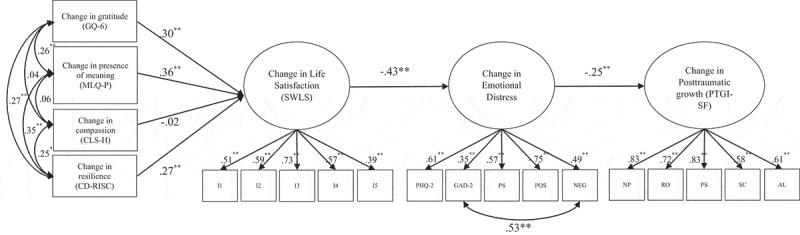
The predictive model of changes in life satisfaction, emotional distress, and PTG, through the positive functioning variables, from the first two weeks to the fifth week of confinement
Notes. *p < .010; **p < .001; I1 = item 1; I2 = item 2; I3 = item 3; I4 = item 4; I5 = item 5; PHQ = Patient Health Questionnaire; GAD = Generalized Anxiety Disorder; PSS = Perceived Stress Scale; POS = Positive Affect – PANAS; NEG = Negative Affect – PANAS; NP = New possibilities; RO = Relation to others; PS = Personal strength; SC = Spiritual change; AL = Appreciation of life. Indirect effects are marked with dashes. For the sake of clarity, standard errors are not shown.
The model proposed indirect effects from gratitude, presence/search for meaning, compassion, and resilience to post-traumatic growth. Again, except for compassion (β = .007, 95% CI [−.020, .016]), the indirect effects were statistically significant. The indirect effect of the increase in gratitude on the increase in post-traumatic growth was β = .032, 95% CI [.007, .079]; the effect of the increase in presence of meaning was β = .038, 95% CI [.008, .093]; the effect of the increase in resilience was β = .029, 95% CI [.003, .089]; and the effect of the increase in life satisfaction was β = .107, 95% CI [.016, .226].
5. Discussion
This study analysed the psychological impact of strict and mandatory confinement on positive functioning variables (resilience, gratitude, compassion, meaning in life, life satisfaction), emotional distress (symptoms of depression and anxiety, perceived stress, affect), and PTG (new possibilities, relating to others, personal strength, appreciation of life, and spiritual change) in one of the countries most affected by COVID-19 at the beginning of the pandemic. First, we will discuss the results related to the impact of the first two weeks of confinement, and then the changes that occurred after the most difficult weeks (in the fifth week).
5.1. The initial psychological impact of the COVID-19 during the first two weeks of confinement
The analyses of potential differences in the impact of confinement on individuals based on sociodemographic variables showed differences in positive functioning variables and emotional distress in all the groups in the first two weeks, supporting the first study hypothesis. Women, youths (i.e. 18–24 years old), people diagnosed with a mental disorder or chronic illness, individuals without a partner, or those with lower monetary incomes experienced lower scores on positive functioning variables and greater emotional distress during the first stage of confinement. However, no statistically significant differences in PTG were found for any group —except for the lower scores on the ‘relating to others’ subscale in individuals diagnosed with a mental disorder — as the null hypotheses were not rejected in all the comparisons, and confidence intervals of effect sizes included the zero value.
Regarding sex and age, findings are consistent with previous studies that found that being a woman and being younger are the strongest predictors of greater psychological impact due to the COVID-19 pandemic (Özdin & Bayrak Özdin, 2020; Rodríguez-Rey, Garrido-Hernansaiz, & Collado, 2020; Varshney, Parel, Raizada, & Sarin, 2020; Wang et al., 2020a). Moreover, women showed higher scores on compassion ‒a variable correlated with anxiety in this study‒. Regarding mental and health status, as expected, individuals diagnosed with a mental illness achieved lower scores on positive functioning variables, a greater impact in terms of emotional distress, and a lower capacity for PTG in terms of relating to others. In contrast, individuals diagnosed with a chronic disease – who were considered as a particularly vulnerable population in terms of health during the COVID-19 pandemic – showed higher scores on the presence of meaning in life, but also higher levels of anxiety. This higher anxiety in this group could be considered adaptive in this context, given the necessity of taking special care of their health during the pandemic. This is in line with other studies in different countries (e.g. China, India, or Turkey) that suggest that the pandemic has a greater psychological impact on vulnerable groups (Guan et al., 2020; Holmes et al., 2020; Özdin & Bayrak Özdin, 2020; Rodríguez-Rey et al., 2020; Varshney et al., 2020).
With regard to having a partner, individuals being in a relationship (vs. those not being in a relationship) did not statistically significantly differ in emotional distress (i.e. null hypotheses were not rejected, and confidence intervals of effect sizes include the zero value). However, they showed a greater ‘psychological armour’, given the significantly greater levels of gratitude and life satisfaction found. Similarly, Rodríguez-Rey et al. (2020) found that being married and living with the partner was a protective factor against mental suffering. However, a lower income level resulted in a greater negative psychological impact of the COVID-19 pandemic, as shown in other studies with Spanish (Rodríguez-Rey et al., 2020) and Chinese samples (Wang et al., 2020a). However, the higher level of positive emotions that coexisted with the negative emotions in the lower income population should be noted.
In this regard, the coexistence of positive and negative emotions has also been found in other stressful situations, such as in terrorist attacks (Fredrickson et al., 2003; Linley, Joseph, Cooper, Harris, & Meyer, 2003; Smith, Rasinski, & Toce, 2001; Vázquez & Hervás, 2010). For instance, the study by Vázquez and Hervás (2010) revealed the presence of both positive (i.e. strength, excitement, pride, and joy) and negative emotions (i.e. distress, hate, and shame) in a sample of individuals who experienced the 11 March 2004 Madrid terrorist attacks. Other studies have also shown that mixed emotions are commonly reported in response to negative events and when stressors are still present (vs. absent) (Hui, Fok, & Bond, 2009; Scott, Sliwinski, Mogle, & Almeida, 2014). Future studies could analyse whether the coexistence of positive and negative emotions helps to buffer emotional distress and promote PTG in the long-term in relation to the pandemic crisis.
Our sample also included healthcare professionals who were currently working, which was a particularly relevant group because they were facing a very stressful situation (e.g. overcrowded hospitals, lack of advanced medical equipment to protect themselves from COVID-19, and an inability to take proper care of patients). Surprisingly, results showed higher scores on positive functioning variables, which were associated with lower emotional distress levels. These findings contradict previous research that found that Chinese healthcare professionals exposed to COVID-19 – especially women, nurses in Wuhan, and individuals on the frontline – reported higher emotional distress (Lai et al., 2020). Nevertheless, the more positive emotional state found in our study is consistent with the study by Varshney et al. (2020), who also found similar results in an Indian sample. Along the same lines, Sun et al. (2020) carried out a qualitative study on the psychological experience of nurses caring for COVID-19 patients during the outbreak of the epidemic, revealing that positive emotions occurred simultaneously or progressively with negative emotions (e.g. after the first week, positive emotions prevailed in 70% of the nurses). However, our findings should be interpreted with caution because the sample of healthcare professionals was small (8.7% of the total sample), and we have limited information about their situation (e.g. level of expertise or whether they specifically take care of COVID-19 patients).
Regarding the correlations between positive functioning variables and emotional distress, the second hypothesis was supported. Overall, positive functioning variables were positively related to positive affect and negatively associated with the emotional distress variables – except for ‘search for meaning in life’, which was positively correlated with emotional distress and negatively with the other positive variables. In this regard, Park, Park, and Peterson (2010) pointed out that searching for meaning in life was only linked to well-being when individuals already had a substantial presence of meaning in life; and Steger, Oishi, and Kesebir (2011) also found a complex interplay between the search and presence of meaning, suggesting that the role of the presence of meaning in life satisfaction was moderated by the search for meaning. Nevertheless, our findings point out that the search for meaning in life during the initial stages of the pandemic outbreak ‒ without controlling the possible moderator effect of the presence of meaning in life – may be a risk factor for experiencing emotional distress.
Another unexpected finding was the correlation between compassion and higher anxiety levels, which could be related to the intrinsic nature of compassion when one is exposed to others’ pain and suffering, and this can lead to emotional distress (Radey & Figley, 2007). This is particularly relevant in the context of the present study, where people were exposed to a situation that was out of their control. On the one hand, this situation provided them with the opportunity to help others, thus giving them a sense of satisfaction or fulfilment (although these opportunities were limited because of confinement). On the other hand, exposure to others’ suffering increased (e.g. infected people dying in the hospital without being able to see their relatives, elderly people alone in retirement homes and isolated in their rooms, and healthcare professionals overwhelmed by the healthcare crisis). Hence, this result points out that the effects of compassion may depend on the specific characteristics of the situation. Therefore, it is necessary to understand which of the positive functioning variables promote a positive upward spiral process in an early stage and which ones do not.
Regarding correlations with PTG, significant positive relationships were found between its five dimensions and most of the positive functioning variables. Search for meaning in life was also positively related to PTG, suggesting that it is a complex variable related to higher emotional distress, but also to higher PTG. This result is congruent with a previous study that found that both presence and search for meaning in life are pathways to experiencing PTG (Dursun et al., 2014). Moreover, PTG was also associated with higher emotional distress, suggesting that the presence of emotional distress does not exclude experiencing PTG during the initial outbreak of a chronic stressor. This result coincides with Dursun et al. (2014), who found that the severity of posttraumatic stress was the main positive predictor of PTG. In this regard, it is important to keep in mind that the experience of a stressful situation is embedded in the definition of PTG itself, and the challenge provoked by the traumatic situation shatters fundamental schemas of life (Tedeschi & Calhoun, 2004). Later, this experience leads to a process of growing or flourishing in the case of PTG.
Furthermore, it is important to note that our results also showed correlations between positive affect and PTG. Indeed, positive emotions are closely related to PTG in resilient individuals, constituting an active ingredient that helps them to thrive despite the aftermath of a crisis (Fredrickson et al., 2003), which would be aligned with the Broaden and Build Theory proposed by Fredrickson (2001). Given the complex relationships between PTG, emotional distress, and positive affect, it would be informative to find out whether there are different PTG patterns of responses. For example, some individuals may only experience negative affect, whereas others only experience positive affect; another possibility is that both positive and negative affect coexist in some individuals. Future studies could use cluster analyses to verify this point and analyse the potential profiles of PTG responses.
5.2. Psychological impact during the first month of confinement
After the first month of confinement, positive functioning variables, emotional distress, and PTG deteriorated, except for some specific variables that remained stable. Hence, our third hypothesis was supported. Greater decreases were observed in the variables of gratitude and the presence of meaning in life, and greater increases were noted in symptoms of depression. These results contradict those obtained in a study carried out in China a month after the pandemic began (Wang et al., 2020b). The authors found that stress, anxiety, and depression remained stable – and even had a (not significant) tendency to decline. One tentative explanation for this discrepancy is related to the cultural and contextual differences between the samples. For example, the pandemic had not yet been declared by the WHO at the time the assessment was carried out in China, and confinement was not mandatory in all the cities in China. On 8 February 2020, there was a decline in the number of new cases and an increase of the number of recovered patients in China.
Another surprising result was that PTG, in terms of ‘deeper relationships with others’, was also highly affected. This result somewhat contradicts the social phenomenon that spontaneously occurred during the first weeks of confinement in Spain, where people collectively honoured healthcare professionals by standing on their balconies or at their windows at 8 pm every day to applaud them, a practice that had a strong following in our sample. However, the results could also be influenced by the prohibition on having physical contact with relatives or friends – a behaviour that is salient and ingrained in the Mediterranean culture.
5.3. Variables that predict changes in PTG after one month of confinement
In order to explain the reasons for experiencing PTG, we performed correlation analyses of the change in the scores from the first two weeks to the fifth week of the pandemic. Surprisingly, results showed that, overall, the increases (or decreases) in positive functioning were not statistically significantly correlated with the increases (or decreases) in PTG, as most of the confidence intervals included the zero value. However, the changes in emotional distress correlated with the changes in the positive functioning variables and the PTG dimensions. Given these results, and in order to test our fourth hypothesis, we confirmed the fit of the following structural equations model: the increases in the presence of meaning in life, gratitude, and resilience ‒but not compassion‒ led to an increase in life satisfaction, explaining 50.6% of the variance, and the increase in gratitude was the best predictor of changes in life satisfaction. Moreover, the increase in life satisfaction led to a decrease in emotional distress (explaining 19.6% of the variance), which in turn led to an increase in PTG (explaining 5.3% of the variance). In this line, during the SARS pandemic in Hong Kong in 2003, Lau et al. (2006) reported some positive psychological impacts (e.g. increased social and family support, increased mental health awareness, lifestyle changes) in a large percentage (between 30–60%) of individuals experiencing the pandemic.
Thus, increasing positive functioning factors, such as resilience or gratitude, could minimize emotional distress and build enduring resources (Fredrickson et al., 2003). This model highlights that: (1) the increase in positive functioning variables and life satisfaction reduced the impact of emotional distress; (2) the increase in gratitude, presence of meaning in life, and resilience generated a ‘cascade’ of psychological changes that promoted both a reduction in emotional distress and more PTG in this particular situation; (3) lower emotional distress would be necessary to experience PTG, which agrees with a recent systematic review revealing that PTG does not necessarily require the presence of emotional suffering (Mangelsdorf, Eid, & Luhmann, 2019).
5.4. Limitations
This longitudinal study has some limitations. First, the lack of baseline measurements (before confinement) keeps us from verifying the extent to which individuals experienced pre-post confinement changes in each study variable. Second, the analyses are performed at only two points in time, limiting the variability and dynamism of changes in each variable within- and between-days in this first month of confinement due to the pandemic. Third, the sample was small, and the representativeness of the sample was limited because it was collected on social media, two-thirds of the sample were women, and there was no participation of individuals older than 68 years old. Fourth, the interpretation of results linked to the gratitude questionnaire should be viewed cautiously, given that the internal consistency was limited (Cronbach’s alpha ranged from .67 to .70). Finally, the high attrition rate must be highlighted because only 45% of the individuals who initially participated answered the second assessment.
5.5. Clinical implications and future directions
Several clinical implications can be outlined. First, there are specific socio-demographic groups (i.e. women, younger individuals, individuals without a partner, individuals with lower economic incomes, and individuals diagnosed with a mental disorder), who are more psychologically vulnerable due to their poorer positive functioning and their greater emotional distress during the first weeks of confinement. However, none of these groups seemed to be disadvantaged in their capacity to experience PTG at the beginning of confinement. Second, the mechanisms underlying this increase in PTG could be partially associated with the increase in gratitude, presence of meaning in life, and resilience because these increases were associated with greater life satisfaction and buffered emotional distress. Nevertheless, these conclusions are tentative and should be replicated, given the study limitations mentioned above.
Future studies could map the emotions through the entire confinement in order to find out how positive functioning and emotional distress change over time, and how these factors interact with the increase in PTG. Moreover, the long-term effects could also be analysed in order to confirm the maintenance of the findings and analyse the changes once confinement had ended and there was less probability of being infected. If the results are confirmed in future studies, we could tentatively propose prevention programmes focused on increasing gratitude, meaning in life, and resilience to prevent emotional distress and enhance individuals’ positive long-term changes. At the moment, we are analysing the daily, weekly, and monthly measurements of the participants from March 21 to June 21 (the data until the state of alarm ended in Spain). However, this is the first step in developing appropriate psychological interventions to buffer the psychological impact of the COVID-19 consequences, which are urgently requested by several authors (Duan & Zhu, 2020; Holmes et al., 2020; Xiang et al., 2020).
5.6. Conclusion
In conclusion, this study reveals that there are specific socio-demographic groups (i.e. women, younger individuals, individuals without a partner, individuals with lower economic resources, or individuals diagnosed with a mental disorder or a chronic disease) with a higher risk of experiencing lower scores on positive functioning variables and greater emotional distress during the first two weeks of confinement. Moreover, the findings point out that, in general, positive functioning, emotional distress, and PTG worsen after five weeks of confinement. However, this study also highlights that some individuals can experience PTG during the first month of strict and obligatory confinement. According to our tested model, this increase is indirectly associated with increases in gratitude (the greatest predictor), presence of meaning in life, and resilience, facilitated by improvements in life satisfaction and emotional distress. In contrast, the increase in compassion towards strangers did not have a protective role in buffering emotional distress and, in turn, promoting PTG. Nevertheless, given the sample’s limitations (small sample, high attrition rate, convenience social media sampling), these findings are tentative. To our knowledge, this is the first study to highlight individuals’ capacity to augment personal resources during a pandemic in order to flourish during a chronic, unknown, collective, and threatening stressor.
Supplementary Material
Acknowledgments
We would like to thank CIBERObn, an initiative of ISCIII (ISC III CB06 03/0052).
Funding Statement
This work was supported by Excellence Research Program PROMETEO [PROMETEO/2018/110], (Conselleria d’Educació, Investigació, Cultura I Esport, Generalitat Valenciana).
Notes
In the present study, positive emotions’ scores were also included in the calculation of emotional distress of the tested model, with negative affect, anxiety, depression, and perceived stress.
Life satisfaction was introduced in a second level – as an ‘outcome’ of the positive functioning variables. Previous studies have shown the influence of gratitude (Toepfer, Cichy, & Peters, 2012), presence of meaning (Steger & Kashdan, 2007), resilience (Smith, Saklofske, Keefer, & Tremblay, 2016) on life satisfaction.
The directionality in the change of Hypothesis 3 was not established given that confinement was a chronic and uncertain stressor, experienced worldwide, in which there was scarce evidence regarding its psychological effects (especially, evidence related to positive functioning variables and PTG).
Change in search for meaning was not introduced in the model, as this variable showed no significant differences with the rest of the positive functioning variables, and showed a positive significant relationship with symptoms of depression, as in previous studies (e.g. Steger et al., 2006; Steger, Oishi, & Kashdan, 2009).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are openly available in OSF at https://osf.io/7uswb/.
Ethics statement
The study received approval from the ethical committee of the University of Valencia (Spain) (register number: 1593681212393). Following the General Data Protection Regulation (EU) 2016/679, and the principles outlined in the Declaration of Helsinki (World Medical Association, 2013), all participants were informed about the study and their rights. All participants gave their consent before the start of the study
Supplemental Material
Supplemental data for this article can be accessed here.
References
- Almedom, A. M. (2005). Resilience, hardiness, sense of coherence, and posttraumatic growth: All paths leading to “light at the end of the tunnel”? Journal of Loss and Trauma, 10(3), 253–18. DOI: 10.1080/15325020590928216 [DOI] [Google Scholar]
- Bonanno, G. A., Galea, S., Bucciarelli, A., & Vlahov, D. (2007). What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology, 75(5), 671–682. DOI: 10.1037/0022-006X.75.5.671 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. DOI: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne, B. M. (2012). Structural equation modeling with Mplus: Basic concepts, applications and programming. New York: Routledge Academic. [Google Scholar]
- Calhoun, L. G., Cann, A., & Tedeschi, R. G. (2010). The posttraumatic growth model: Socio-cultural considerations. In Weiss T. & Berger R. (Eds.), Posttraumatic growth and culturally competent practice: Lessons learned from around the globe (pp. 1–14). Hoboken, NJ: Wiley. [Google Scholar]
- Campbell‐Sills, L., & Stein, M. B. (2007). Psychometric analysis and refinement of the connor–davidson resilience scale (CD‐RISC): Validation of a 10‐item measure of resilience. Journal of Traumatic Stress, 20(6), 1019–1028. DOI: 10.1002/jts.20271 [DOI] [PubMed] [Google Scholar]
- Cann, A., Calhoun, L. G., Tedeschi, R. G., Taku, K., Vishnevsky, T., Triplett, K. N., & Danhauer, S. C. (2010). A short form of the posttraumatic growth inventory. Anxiety, Stress, & Coping, 23(2), 127–137. DOI: 10.1080/10615800903094273 [DOI] [PubMed] [Google Scholar]
- Cárdenas, M., Barrientos, J., Ricci, E., & Páez, D. (2015). Spanish adaptation and validation of the posttraumatic growth inventory–short form. Violence and Victims, 30(5), 756–769. DOI: 10.1891/0886-6708.VV-D-13-00165 [DOI] [PubMed] [Google Scholar]
- Cheung, G. W., & Rensvold, R. B. (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 9(2), 233–255. DOI: 10.1207/S15328007SEM0902_5 [DOI] [Google Scholar]
- Chiesi, F., Lau, C., & Saklofske, D. H. (2020). A revised short version of the compassionate love scale for humanity (CLS-H-SF): Evidence from item response theory analyses and validity testing. BMC Psychology, 8(1), 1–9. DOI: 10.1186/s40359-020-0386-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates, Publishers. [Google Scholar]
- Connor, K. M., & Davidson, J. R. (2003). Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety, 18(2), 76–82. DOI: 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Diener, E., Emmons, R. A., Larsen, R. J., & Griffin, S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49(1), 71–75. DOI: 10.1207/s15327752jpa4901_13 [DOI] [PubMed] [Google Scholar]
- Duan, L., & Zhu, G. (2020). Psychological interventions for people affected by the COVID-19 epidemic. The Lancet Psychiatry, 7(4), 300–302. DOI: 10.1016/S2215-0366(20)30073-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dursun, P., Saracli, S., & Konuk, O. (2014). The roles of meaningful life and posttraumatic stress in posttraumatic growth in a sample of Turkish university students. Procedia-Social and Behavioral Sciences, 159, 702–706. DOI: 10.1016/j.sbspro.2014.12.454 [DOI] [Google Scholar]
- Emmons, R. A. (2007). Gratitude, subjective well-being, and the brain. In Larsen R. J. & Eid M. (Eds.), The science of subjective well-being. New York, NY: The Guilford Press. [Google Scholar]
- Finney, S. J., & DiStefano, C. (2006). Non-normal and categorical data in structural equation modeling. In Hancock G. R. & Muller R. O. (Eds.), Structural equation modeling: A second course (pp. 269–314). Greenwich, CT: Information Age Publishing. [Google Scholar]
- Fishman, M. D. (2020). The silver linings journal: Gratitude during a pandemic. Journal of Radiology Nursing, 39(3), 149–150. DOI: 10.1016/j.jradnu.2020.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson, B. L. (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56(3), 218–226. DOI: 10.1037/0003-066X.56.3.218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson, B. L., Tugade, M. M., Waugh, C. E., & Larkin, G. R. (2003). What good are positive emotions in crisis? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11, 2001. Journal of Personality and Social Psychology, 84(2), 365–376. DOI: 10.1037/0022-3514.84.2.365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrikson, B. L. (2009). Positivity: Groundbreaking research reveals how to embrace the hidden strength of positive emotions, overcome negativity, and thrive. New York, NY: Crown Publishing group. [Google Scholar]
- Gaetano, J. (2018). Holm-Bonferroni sequential correction: An Excel calculator (1.3) [Microsoft Excel workbook]. Retrieved from https://www.researchgate.net/publication/322568540_Holm-Bonferroni_sequential_correction_An_Excel_calculator_13
- García-Campayo, J., Zamorano, E., Ruiz, M. A., Pérez-Páramo, M., López-Gómez, V., & Rejas, J. (2012). The assessment of generalized anxiety disorder: Psychometric validation of the Spanish version of the self-administered GAD-2 scale in daily medical practice. Health and Quality of Life Outcomes, 10(1), 114. DOI: 10.1186/1477-7525-10-114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan, W. J., Liang, W. H., Zhao, Y., Liang, H. R., Chen, Z. S., Li, Y. M., … He, J. X. (2020). Comorbidity and its impact on 1590 patients with Covid-19 in China: A nationwide analysis. European Respiratory Journal, 55(5), 2000547. DOI: 10.1183/13993003.00547-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holm, S. (1979). A simple sequential rejective method procedure. Scandinavian Journal of Statistics, 6, 65–70. [Google Scholar]
- Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., … Bullmoret, E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. DOI: 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. DOI: 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hui, C. M., Fok, H. K., & Bond, M. H. (2009). Who feels more ambivalence? Linking dialectical thinking to mixed emotions. Personality and Individual Differences, 46(4), 493–498. DOI: 10.1016/j.paid.2008.11.022 [DOI] [Google Scholar]
- Jang, H., & Kim, J. (2017). A meta-analysis on relationship between post-traumatic growth and related variables. Korean Journal of Counseling and Psychotherapy, 18, 85–105. DOI: 10.15703/kjc.18.5.201710.85 [DOI] [Google Scholar]
- Kim, E. S., & Bae, S. M. (2019). Gratitude moderates the mediating effect of deliberate rumination on the relationship between intrusive rumination and posttraumatic growth. Frontiers in Psychology, 10, 2665. DOI: 10.3389/fpsyg.2019.02665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline, R. B. (2015). Principles and practice of structural equation modeling. New York, NY: Guilford publications. [Google Scholar]
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2003). The patient health Questionnaire-2: Validity of a two-item depression screener. Medical Care, 41(11), 1284–1292. DOI: 10.1097/01.MLR.0000093487.78664.3C [DOI] [PubMed] [Google Scholar]
- Kroenke, K., Spitzer, R. L., Williams, J. B., Monahan, P. O., & Löwe, B. (2007). Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine, 146(5), 317–325. DOI: 10.7326/0003-4819-146-5-200703060-00004 [DOI] [PubMed] [Google Scholar]
- Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., … Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), e203976–e203976. DOI: 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakens, D. (2013). Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Frontiers in Psychology, 4, 863. DOI: 10.3389/fpsyg.2013.00863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau, J. T., Yang, X., Tsui, H. Y., Pang, E., & Wing, Y. K. (2006). Positive mental health-related impacts of the SARS epidemic on the general public in Hong Kong and their associations with other negative impacts. Journal of Infection, 53(2), 114–124. DOI: 10.1016/j.jinf.2005.10.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linley, P. A., & Joseph, S. (2011). Meaning in life and posttraumatic growth. Journal of Loss and Trauma, 16(2), 150–159. DOI: 10.1080/15325024.2010.519287 [DOI] [Google Scholar]
- Linley, P. A., Joseph, S., Cooper, R., Harris, S., & Meyer, C. (2003). Positive and negative changes following vicarious exposure to the September 11 terrorist attacks. Journal of Traumatic Stress, 16(5), 481–485. DOI: 10.1023/A:1025710528209 [DOI] [PubMed] [Google Scholar]
- Little, T. D. (1997). Mean and covariance structures (MACS) analyses of cross-cultural data: Practical and theoretical issues. Multivariate Behavioural Research, 32(1), 53–76. DOI: 10.1207/s15327906mbr3201_3 [DOI] [PubMed] [Google Scholar]
- López-Gómez, I., Hervás, G., & Vázquez, C. (2015). An adaptation of the Positive and Negative Affect Schedules (PANAS) in a Spanish general sample. Behavioral Psychology, 23(3), 529–548. [Google Scholar]
- MacKinnon, D. P., Fairchild, A. J., & Fritz, M. S. (2007). Mediation analysis. Annual Review of Psychology, 58(1), 593–614. DOI: 10.1146/annurev.psych.58.110405.085542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magallares, A., Recio, P., & Sanjuán, P. (2018). Factor structure of the gratitude questionnaire in a Spanish sample. The Spanish Journal of Psychology, 21, 1–7. DOI: 10.1017/sjp.2018.55 [DOI] [PubMed] [Google Scholar]
- Malhotra, M., & Chebiyan, S. (2016). Posttraumatic growth: Positive changes following adversity - an overview. International Journal of Psychology and Behavioral Sciences, 6(3), 109–118. DOI: 10.5923/j.ijpbs.20160603.03 [DOI] [Google Scholar]
- Mangelsdorf, J., Eid, M., & Luhmann, M. (2019). Does growth require suffering? A systematic review and meta-analysis on genuine posttraumatic and postecstatic growth. Psychological Bulletin, 145(3), 302–338. DOI: 10.1037/bul0000173 [DOI] [PubMed] [Google Scholar]
- McCullough, M. E., Emmons, R. A., & Tsang, J. A. (2002). The grateful disposition: A conceptual and empirical topography. Journal of Personality and Social Psychology, 82(1), 112–127. DOI: 10.1037/0022-3514.82.1.112 [DOI] [PubMed] [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (2017). Mplus: Statistical analysis with latent variables: User’s guide (Version 8). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nicola, M., Alsafi, Z., Sohrabi, C., Kerwan, A., Al-Jabir, A., Iosifidis, C., … Agha, R. (2020). The socio-economic implications of the coronavirus pandemic (COVID-19): A review. International Journal of Surgery, 78, 185–193. DOI: 10.1016/j.ijsu.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishi, D., Kawashima, Y., Noguchi, H., Usuki, M., Yamashita, A., Koido, Y., & Matsuoka, Y. J. (2016). Resilience, post-traumatic growth, and work engagement among health care professionals after the Great East Japan Earthquake: A 4-year prospective follow-up study. Journal of Occupational Health, 58(4), 347–353. DOI: 10.1539/joh.16-0002-OA [DOI] [PMC free article] [PubMed] [Google Scholar]
- Notario-Pacheco, B., Solera-Martínez, M., Serrano-Parra, M. D., Bartolomé-Gutiérrez, R., García-Campayo, J., & Martínez-Vizcaíno, V. (2011). Reliability and validity of the Spanish version of the 10-item Connor-Davidson Resilience Scale (10-item CD-RISC) in young adults. Health and Quality of Life Outcomes, 9(1), 63–68. DOI: 10.1186/1477-7525-9-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogińska-Bulik, N., & Kobylarczyk, M. (2016). Association between resiliency and posttraumatic growth in firefighters: The role of stress appraisal. International Journal of Occupational Safety and Ergonomics, 22(1), 40–48. DOI: 10.1080/10803548.2015.1109372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özdin, S., & Bayrak Özdin, Ş. (2020). Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. International Journal of Social Psychiatry, 1–8. DOI: 10.1177/0020764020927051 [DOI] [PMC free article] [PubMed]
- Park, N., Park, M., & Peterson, C. (2010). When is the search for meaning related to life satisfaction? Applied Psychology: Health and Well‐Being, 2(1), 1–13. DOI: 10.1111/j.1758-0854.2009.01024.x [DOI] [Google Scholar]
- Pavot, W., & Diener, E. (2008). The satisfaction with life scale and the emerging construct of life satisfaction. The Journal of Positive Psychology, 3(2), 137–152. DOI: 10.1080/17439760701756946 [DOI] [Google Scholar]
- Radey, M., & Figley, C. R. (2007). The social psychology of compassion. Clinical Social Work Journal, 35(3), 207–214. DOI: 10.1007/s10615-007-0087-3 [DOI] [Google Scholar]
- Rodríguez-Muñoz, M. D. L. F., Castelao, P. L., Olivares, M. C., Soto, C. B., Izquierdo, N. M., Ferrer, F. B., & Huynh-Nhu, L. (2017). PHQ-2 as first screening instrument of prenatal depression in primary health care, Spain. Revista Española de Salud Publica, 91, e201701010. [PubMed] [Google Scholar]
- Rodríguez-Rey, R., Garrido-Hernansaiz, H., & Collado, S. (2020). Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Frontiers in Psychology, 11, 1540. DOI: 10.3389/fpsyg.2020.01540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell, D. W. (2002). In search of underlying dimensions: The use (and abuse) of factor analysis in personality and social psychology bulletin. Personality and Social Psychology Bulletin, 28(12), 1629–1646. DOI: 10.1177/014616702237645 [DOI] [Google Scholar]
- Scott, S. B., Sliwinski, M. J., Mogle, J. A., & Almeida, D. M. (2014). Age, stress, and emotional complexity: Results from two studies of daily experiences. Psychology and Aging, 29(3), 577–587. DOI: 10.1037/a0037282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman, M. E. (2012). Flourish: A visionary new understanding of happiness and well-being. New York, NY: Simon and Schuster. [Google Scholar]
- Smith, M. M., Saklofske, D. H., Keefer, K. V., & Tremblay, P. F. (2016). Coping strategies and psychological outcomes: The moderating effects of personal resiliency. The Journal of Psychology, 150(3), 318–332. DOI: 10.1080/00223980.2015.1036828 [DOI] [PubMed] [Google Scholar]
- Smith, T. W., Rasinski, K. A., & Toce, M. (2001). America rebounds: A national study of public response to the September 11th terrorist attacks. Preliminary findings. Chicago: NORC, University of Chicago. [Google Scholar]
- Sprecher, S., & Fehr, B. (2005). Compassionate love for close others and humanity. Journal of Social and Personal Relationships, 22(5), 629–651. DOI: 10.1177/0265407505056439 [DOI] [Google Scholar]
- Steger, M. F., Frazier, P., Oishi, S., & Kaler, M. (2006). The meaning in life questionnaire: Assessing the presence of and search for meaning in life. Journal of Counseling Psychology, 53(1), 80–93. DOI: 10.1037/0022-0167.53.1.80 [DOI] [Google Scholar]
- Steger, M. F., Frazier, P. A., & Zacchanini, J. L. (2008). Terrorism in two cultures: Stress and growth following September 11 and the Madrid train bombings. Journal of Loss and Trauma, 13(6), 511–527. DOI: 10.1080/15325020802173660 [DOI] [Google Scholar]
- Steger, M. F., & Kashdan, T. B. (2007). Stability and specificity of meaning in life and life satisfaction over one year. Journal of Happiness Studies, 8(2), 161–179. DOI: 10.1007/s10902-006-9011-8 [DOI] [Google Scholar]
- Steger, M. F., Oishi, S., & Kashdan, T. B. (2009). Meaning in life across the life span: Levels and correlates of meaning in life from emerging adulthood to older adulthood. The Journal of Positive Psychology, 4(1), 43–52. DOI: 10.1080/17439760802303127 [DOI] [Google Scholar]
- Steger, M. F., Oishi, S., & Kesebir, S. (2011). Is a life without meaning satisfying? The moderating role of the search for meaning in satisfaction with life judgments. The Journal of Positive Psychology, 6(3), 173–180. DOI: 10.1080/17439760.2011.569171 [DOI] [Google Scholar]
- Sun, N., Shi, S., Jiao, D., Song, R., Ma, L., … Wang, H. (2020). A qualitative study on the psychological experience of caregivers of COVID-19 patients. American Journal of Infection Control, 48(6), 592–598. DOI: 10.1016/j.ajic.2020.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamiolaki, A., & Kalaitzaki, A. E. (2020). “That which does not kill us, makes us stronger”: COVID-19 and posttraumatic growth. Psychiatry Research, 289, 113044. DOI: 10.1016/j.psychres.2020.113044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka, J. S. (1993). Multifaceted conceptions of fit in structural equation models. In Bollen K. A. & Long J. S. (Eds.), Testing structural equation models (pp. 10–40). Newbury Park, CA: Sage. [Google Scholar]
- Tedeschi, R. G., & Calhoun, L. G. (2004). Target article: “Posttraumatic growth: Conceptual foundations and empirical evidence”. Psychological Inquiry, 15(1), 1–18. DOI: 10.1207/s15327965pli1501_01 [DOI] [Google Scholar]
- Tedeschi, R. G., Shakespeare-Finch, J., Taku, K., & Calhoun, L. G. (2018). Posttraumatic growth: Theory, research, and applications. London: Routledge. [Google Scholar]
- Toepfer, S. M., Cichy, K., & Peters, P. (2012). Letters of gratitude: Further evidence for author benefits. Journal of Happiness Studies, 13(1), 187–201. DOI: 10.1007/s10902-011-9257-7 [DOI] [Google Scholar]
- Torales, J., O’Higgins, M., Castaldelli-Maia, J. M., & Ventriglio, A. (2020). The outbreak of COVID-19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry, 66(4), 317–320. DOI: 10.1177/0020764020915212 [DOI] [PubMed] [Google Scholar]
- Uanhoro, J. O. (2017). Effect size calculators. Retrieved from https://effect-size-calculator.herokuapp.com/
- Updegraff, J. A., Silver, R. C., & Holman, E. A. (2008). Searching for and finding meaning in collective trauma: Results from a national longitudinal study of the 9/11 terrorist attacks. Journal of Personality and Social Psychology, 95(3), 709–722. DOI: 10.1037/0022-3514.95.3.709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varshney, M., Parel, J. T., Raizada, N., & Sarin, S. K. (2020). Initial psychological impact of COVID-19 and its correlates in Indian Community: An online (FEEL-COVID) survey. PLoS ONE, 15(5), e0233874. DOI: 10.1371/journal.pone.0233874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vázquez, C., Duque, A., & Hervás, G. (2013). Satisfaction with Life Scale in a representative sample of Spanish adults: Validation and normative data. The Spanish Journal of Psychology, 16, 1–15. DOI: 10.1017/sjp.2013.82 [DOI] [PubMed] [Google Scholar]
- Vazquez, C., & Hervas, G. (2010). Perceived benefits after terrorist attacks: The role of positive and negative emotions. The Journal of Positive Psychology, 5(2), 154–163. DOI: 10.1080/17439761003630060 [DOI] [Google Scholar]
- Vernon, L. L., Dillon, J. M., & Steiner, A. R. (2009). Proactive coping, gratitude, and posttraumatic stress disorder in college women. Anxiety, Stress, & Coping, 22(1), 117–127. DOI: 10.1080/10615800802203751 [DOI] [PubMed] [Google Scholar]
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., & Ho, R. C. (2020a). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. DOI: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., McIntyre, R. S., … Ho, C. (2020b). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity, 87, 40–48. DOI: 10.1016/j.bbi.2020.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson, D., Clark, L. A., & Tellegen, A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 47(6), 1063–1070. DOI: 10.1007/978-94-007-0753-5_2212 [DOI] [PubMed] [Google Scholar]
- West, S. G., Finch, J. F., & Curran, P. J. (1995). Structural equation models with non normal variables: Problems and remedies. In Hoyle R. H. (Ed.), Structural equation modeling: Concepts, issues, and applications (pp. 56–75). Thousand Oaks, CA: Sage publications. [Google Scholar]
- Westphal, M., & Bonanno, G. A. (2007). Posttraumatic growth and resilience to trauma: Different sides of the same coin or different coins? Applied Psychology, 56(3), 417–427. DOI: 10.1111/j.1464-0597.2007.00298.x [DOI] [Google Scholar]
- World Medical Association . (2013). World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA, 310(20), 2191–2194. DOI: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- Xiang, Y. T., Yang, Y., Li, W., Zhang, L., Zhang, Q., Cheung, T., & Ng, C. H. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry, 7(3), 228–229. DOI: 10.1016/S2215-0366(20)30046-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yates, T. M., Egeland, B., & Sroufe, L. A. (2003). Rethinking resilience: A development process perspective. In Luther S. S. (Ed.), Resilience and vulnerability: Adaptation in the context of childhood adversities (pp. 234–256). Cambridge: Cambridge University Press. [Google Scholar]
- Zięba, M., Wiecheć, K., Biegańska-Banaś, J., & Mieleszczenko-Kowszewicz, W. (2019). Coexistence of post-traumatic growth and post-traumatic depreciation in the aftermath of trauma: Qualitative and quantitative narrative analysis. Frontiers in Psychology, 10, 687. DOI: 10.3389/fpsyg.2019.00687 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are openly available in OSF at https://osf.io/7uswb/.


