Abstract
Introduction.
International TS Clinical Practice Guidelines recommend screening for neurodevelopmental (ND) and mental health (MH) concerns in girls with TS, however it remains unclear whether this is implemented in current practice. The objective of this mixed methods study was to assess screening practices for ND and MH in girls with TS from the perspective of pediatric endocrinologists.
Methods.
Pediatric Endocrine Society members who provide care for girls with TS were invited to complete an electronic survey on screening practices. Descriptive statistics were used to summarize quantitative results concurrently with thematic analysis of free-text survey responses.
Results.
A total of 124 surveys were completed (86% attending pediatric endocrinologists, 81% at academic institutions). Overall, 25% of providers reported their patients with TS received both ND and MH screenings. Only 9 (9%) respondents endorsed screening for ND concerns themselves, while more providers (26%) reported they screen for MH concerns. Multiple barriers to screening for ND and MH concerns within the clinical setting were endorsed. Nearly all providers (>93%) reported they would consider using a short, validated screening tool for ND and MH concerns if such tools were available.
Discussion.
A minority of pediatric endocrinologists currently perform ND or MH screening for patients with TS, however, many would be interested in implementing a brief screening tool into their clinical practice. Given almost all girls with a TS diagnosis receive care from pediatric endocrinologists at least annually, this may be an effective method to increase the proportion of girls with TS who receive recommended screenings.
Keywords: Turner syndrome, neurodevelopment, behavioral health, screening
INTRODUCTION
Turner syndrome (TS) occurs in ~1 in 2,000 females, making it one of the most common pediatric rare disease conditions. The missing or abnormal second sex chromosome affects multiple systems with implications for growth, development, fertility, physical health, and mental health. Girls with TS are at a greater risk for neurodevelopmental delays and/or mental health diagnoses than the general population, with potential adverse effects observed in all health domains. Up to 75% of girls with TS have a learning disability, ~25% have attention-deficit hyperactivity disorder (ADHD), and over half will experience symptoms of anxiety and/or depression [1, 2]. Despite how prevalent these conditions are and their known effect on academic achievement and quality of life, symptom recognition is often delayed or missed altogether in girls with TS. Annual consultation with a clinical psychologist and/or neuropsychologist is not feasible for every girl with TS due to limited resources in many clinical settings. Additionally, while girls with TS are at increased risk for developmental or social-emotional concerns, many of these girls thrive within the educational setting and annual comprehensive psychological and/or neuropsychological evaluations in an outpatient clinical setting is unnecessary. However standardized screening is critical for early symptom recognition to ensure that further evaluation and appropriate intervention can occur. Recently published comprehensive Clinical Practice Guidelines (CPG) for girls and women with TS emphasize the need for “annual developmental and behavioral screenings until adulthood with referrals as indicated”, as well as a suggestion for routine neuropsychological assessments at key timepoints [3]. If and how these recommendations are being implemented in clinical practice has had minimal investigation.
Although the TS CPG recommend multidisciplinary care including neuropsychology and behavioral health clinicians, the few TS multidisciplinary clinics that exist are limited to large tertiary care centers and many do not include any behavioral health clinicians [3]. Given TS is a rare disease, many primary care providers are not familiar with TS-specific care recommendations. Research consistently shows that a minority of children within the general pediatric population receive developmental screening despite universal recommendations in place for many years [4]. Therefore, relying on primary care providers for annual neurodevelopmental and behavioral screenings unique to risks seen in girls with TS is likely to result in wide care disparities. Pediatric endocrinologists, however, are intimately familiar with the manifestations of TS and nearly all girls with TS have routine follow up with a pediatric endocrinologist for treatment of endocrine disorders and short stature at least on an annual basis. As a result, the pediatric endocrinologist often becomes their default TS care director, offering non-endocrine related education, screening, and recommendations related to TS risks. Common examples include obtaining renal imaging, screening for celiac disease and liver dysfunction, monitoring for scoliosis, and ensuring appropriate cardiology follow up. Whether or not screening for neurodevelopmental and behavioral screenings are already being conducted or could possibly be completed in the pediatric endocrinology clinic setting has not been evaluated.
The objective of this cross-sectional, mixed methods, survey-based study was to assess screening practices of neurodevelopmental and mental health concerns in girls with TS from the perspective of pediatric endocrinologists. This perspective results informs the feasibility of involving of the pediatric endocrinologist in screening for unmet neurodevelopmental and mental health needs of girls with TS.
METHODS
Survey Development.
An electronic survey targeted to those providing endocrine care to youth with TS was developed by an interdisciplinary, multi-center research team including pediatric endocrinologists, clinical psychologists, and a neuropsychologist. The primary focus was to assess clinical practices for neurodevelopmental and mental health screening in girls with TS. Definitions were provided to differentiate “screening” from “evaluation” as well as “neurodevelopmental” from “mental health”. For the purpose of this survey, “screening” was an informal or formal assessment for possible concerns through parent/caregiver interview or use of a screening instrument such as a patient or parent/caregiver-report standardized questionnaires, whereas “evaluation” was a formal direct performance-based assessment using validated measures to diagnose a condition. Neurodevelopmental concerns were described as delayed language or motor milestones, features of autism spectrum disorder, difficulties with learning or academic achievement, attention difficulties, executive functioning or visuospatial difficulties. Examples given for mental health concerns included anxiety, depression, or psychosis. The survey questions were organized into two sections with the first addressing screening practices for neurodevelopmental concerns and the second addressing questions for mental health concerns. Each of the sections solicited the pediatric endocrinology provider’s perspective on the following outcomes: 1) are patients with TS being screened and if so, what does this look like? 2) what are the barriers to screening? 3) could a short, validated screening tool be implemented in the pediatric endocrine clinic setting? Questions had multiple choice answers as well as the option to provide free-text responses when the predetermined answers may not incorporate all possible perspectives. The survey was piloted with pediatric endocrinologists and refined based on feedback, with the Pediatric Endocrine Society Survey Committee approving the final version.
Recruitment.
An email invitation was sent to the listserv for members of the Pediatric Endocrine Society on November 15, 2019 and December 21, 2019 with a subject heading of “Survey: Assessing Treatment Practices for Patients with Turner Syndrome”. The body of the email included a description of the study, eligibility criteria, estimation of 15 minutes for completion, and a link to the anonymous REDCap survey. The link stayed open for three months after which it was disabled and data were exported for analysis. All participants provided informed consent and verified they met eligibility criteria including being a medical provider within a pediatric endocrine setting in the United States or Canada who has cared for a patient with TS within the last two years. No compensation was provided for respondents. The study was approved by the local institutional review board (STUDY00000025).
Quantitative methods.
Surveys were reviewed for incomplete responses and only records from respondents who completed at least one full section were included. Missing data were treated as a separate category of “not reported” for categorical variables and not included for continuous variables or comparative analyses. Primary outcomes included neurodevelopmental screening (i.e., responding “yes” to the question, “Do your patients with TS receive neurodevelopmental screening”), mental health screening, and both neurodevelopmental and mental health screening. Secondary outcomes included whether the respondent ever conducted neurodevelopmental or mental health screening themselves, estimated frequency and indications for screening, barriers to screening, and interest in implementing a screening tool. Descriptive statistics including number and percentages for categorical variables and mean ± standard deviation (or median and interquartile range (IQR)) for continuous variables were used to summarize the survey results. Chi-squared test was used to compare between categorical outcomes with a significance level set at 0.05. Univariate logistic regression was used to assess factors that may be associated with our primary outcomes, and variables that were significant at p<0.01 and determined to be noncolinear were included in a multivariable model. Statistical analyses were conducted in RStudio version 1.3.1093 with R version 4.0.3 (RStudio, PBC, Boston, MA, www.rstudio.com and figures generated in Graphpad Prism version 9.0.0 for Windows, GraphPad Software, La Jolla California USA, www.graphpad.com).
Qualitative methods.
A team-based approach to qualitative thematic analysis was used for a rigorous and trustworthy interpretation of free-text survey responses [5]. The team created a preliminary coding structure based on predetermined response options in the survey. Two team members with qualitative research and clinical expertise (SD, pediatric endocrinologist; TT, psychologist) read through all open-ended survey responses together, collectively applying deductive codes from the codebook and inductively assigning new “open codes” that emerged directly from the data [6]. Next, the team examined patterns in the codes using networks and analytic memo writing to reduce the information into several categories and, finally, to develop broad themes describing barriers and solutions to screening patients with TS [7].
RESULTS
Sample demographics.
A total of 166 surveys were initiated, 124 eligible providers completed the first section on neurodevelopmental screening, and 120 completed both the neurodevelopmental and mental health screening sections. Demographics of the respondents are shown in Table 1. The region of practice, number of years in practice, total clinical volume, and TS patient volume were diverse. The majority practiced at academic institutions. However, less than a third of these institutions had a TS multidisciplinary clinic. Of the institutions with a TS multidisciplinary clinic, 70% had at least one behavioral health specialist on the team, defined as a psychologist, psychiatrist, developmental pediatrician, or social worker. Approximately half of all respondents knew about the most recent TS CPG [3].
Table 1.
| Demographics of Respondents | N (%) | |
|---|---|---|
| Gender | ||
| Female | 85 (68.5%) | |
| Male | 30 (24.2%) | |
| Not reported | 9 (7.3%) | |
| Race | ||
| White | 95 (76.6%) | |
| Asian | 13 (10.5%) | |
| More than one race | 2 (1.6%) | |
| Not reported | 14 (11.3%) | |
| Ethnicity | ||
| Hispanic/Latino | 8 (6.5%) | |
| Not Hispanic/Latino | 103 (83.1%) | |
| Not reported | 13 (10.5%) | |
| Clinical Role |
||
| Pediatric Endocrinologist | 101 (81.5%) | |
| Adult Endocrinologist | 1 (0.8%) | |
| Fellow | 12 (9.7%) | |
| Advanced Practice Provider | 2 (1.6%) | |
| Not reported | 8 (6.5%) | |
| Years in Practice | ||
| 0–5 | 15 (12.1%) | |
| 6–10 | 29 (23.4%) | |
| 11–15 | 25 (20.2%) | |
| 16–20 | 8 (6.5%) | |
| >20 | 39 (31.5%) | |
| Not reported | 8 (6.5%) | |
| Practice Setting | ||
| Academic Medical Center | 95 (80.5%) | |
| Community Hospital | 9 (7.6%) | |
| Private Practice | 7 (5.9%) | |
| Not reported | 7 (5.9%) | |
| Region | ||
| U.S. Pacific | 13 (11%) | |
| U.S. Mountain | 15 (12%) | |
| U.S. West South Central | 10 (8%) | |
| U.S. East South Central | 3 (2%) | |
| U.S. South Atlantic | 22 (18%) | |
| U.S. West North Central | 9 (7%) | |
| U.S. East North Central | 18 (15%) | |
| U.S. Mid-Atlantic | 1 (1%) | |
| U.S. New England | 12 (10%) | |
| Canada Prairies | 1 (1%) | |
| Canada Ontario | 1 (1%) | |
| Canada Quebec | 1 (1%) | |
| Not reported | 7 (6%) | |
| # of Patients/Month With
TS | ||
| 0–1 | 50 (40.3%) | |
| 2–5 | 52 (41.9%) | |
| >5 | 15 (12.1%) | |
| Not reported | 7 (5.6%) | |
| # of Clinical Patients/Week | ||
| <10 | 15 (12.1%) | |
| 11–25 | 35 (28.2%) | |
| 26–50 | 53 (42.7%) | |
| >50 | 14 (11.3%) | |
| Not reported | 7 (5.6%) | |
| Multidisciplinary Team | ||
| TS MDC at Institution | 36 (29.0%) | |
| No TS MDC at Institution | 82 (66.1%) | |
| Not reported | 6 (4.8%) | |
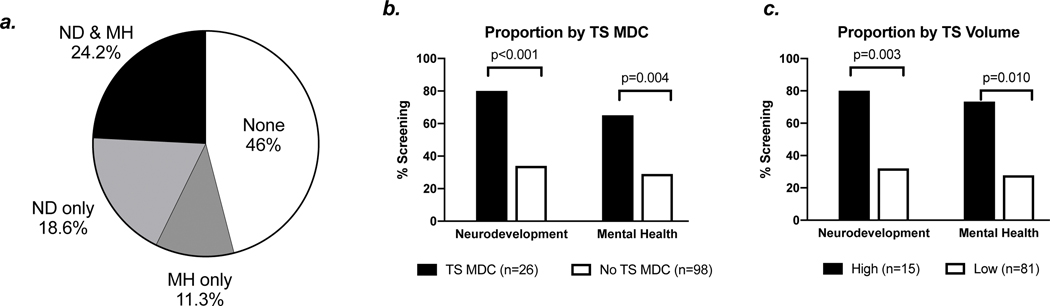
Are patients receiving screening?
More respondents reported their patients with TS receive some form of neurodevelopmental screening (42%) compared to mental health screening (37%, p<0.001), while only 26% reported their patients with TS receive both neurodevelopmental and mental health screenings as recommended in the TS CPG. Very few providers (9%) endorsed ever conducting neurodevelopmental screening themselves, compared to 26% who reported having conducted mental health screenings themselves (p<0.001). Other providers who endorsed their patients receive screening either work directly with a specialist who conducts screening and/or refer to specialists in other clinical or community settings.
In univariate regression analyses, factors that were independently associated with both neurodevelopmental and mental health screening included TS patient volume more than five patients per month (OR 8.2, 95%CI 2.6–28.9), knowledge of the TS CPG (OR 3.6, 95%CI 1.4–9.9), and practicing at an institution with a TS multidisciplinary clinic with an integrated behavioral health specialist (OR 5.5, 95%CI 2.2–14.3). Practice type (academic vs other), region of practice, role (fellow, attending, midlevel), clinical load (patients per week), and number of years in practice were not associated with either neurodevelopmental or mental health screening. In a multivariable model, both TS patient volume of more than five per month (p=0.025) and presence of a TS multidisciplinary clinic with an integrated behavioral health specialist (p=0.027) remained significant with the outcome of reporting both neurodevelopmental and mental health screening.
Among the respondents that report their patients receive neurodevelopmental screening, 32% estimated fewer than half of their patients receive screening and 20% stated they only recommend screening for patients if a concern is present during the visit. Among the 66 providers who reported at least some of their patients receive mental health screening, 41% estimated less than half of their patients with TS receive this screening with 19% reporting they only recommend screening for patients if a concern presented during the visit.
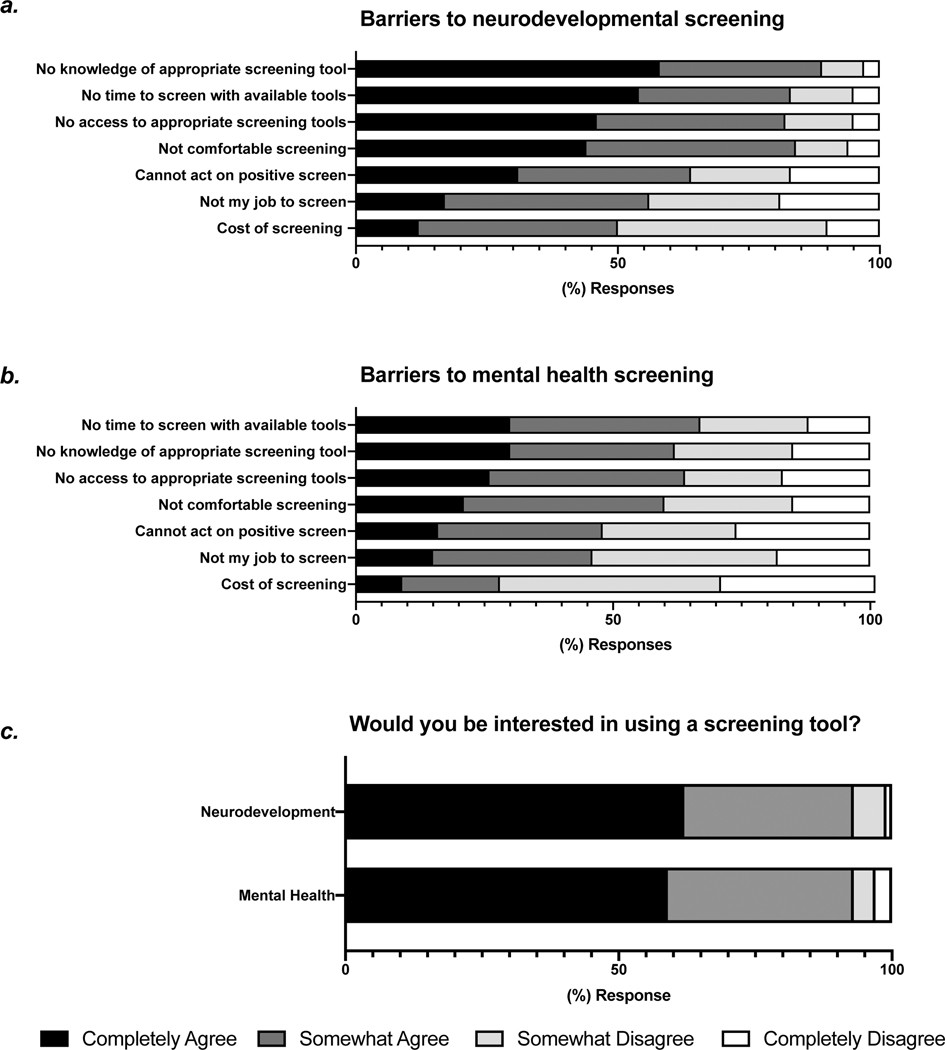
Barriers to screening.
The choices for barriers to neurodevelopmental and mental health screening for girls with TS that were selected by respondents are shown in Figure 3. In the qualitative analysis, respondents described challenges that differed between implementing neurodevelopmental versus mental health screening that emerged, although time was a key factor within both domains.
Neurodevelopment is not endocrinology. Some respondents described neurodevelopmental screenings as outside the role of an endocrinologist: “There are many things that fall under an endocrinologist’s purview when caring for these kids, and I don’t think this is one.” Another commonly reported barrier was the lack of time to conduct screenings unrelated to endocrine issues: “There is not enough time in a clinic visit for this even if it is only 3 minutes. It then takes time for the provider to score it, evaluate the score, and then counsel the patient, make appropriate referrals etc. I think it is a good idea in concept, but I don’t think there is enough time in a busy clinic day.”
Systemic problems in mental health care. Respondents described general problems with mental health follow up care in their communities such as long waitlists, insurance issues, and a lack of TS trained providers: “No mental health providers in the area have experience with girls with TS and most exclude patients based on insurance or take 6+ months to get an appointment.” Providers lamented their lack of options to follow up with a positive mental health screening: “If you have a positive screen, then what do you do? For example, the wait time for psych at my institution is 8 months.”
Potential solutions and theoretical implementation of a TS screening tool.
Respondents also provided suggestions for potential solutions related to screening instruments and effective clinical practice.
TS specific instruments. Respondents described the potential utility of screeners and guidelines specific to the unique needs of girls with TS: “If a short (about 3 minute), validated screening tool for neurodevelopmental concerns in Turner Syndrome was available I would be interested in using it in my clinic - definitely, IF I was given resources for who to refer them to if they screen positive.” Further, such screeners could be used to address barriers related to lack of available providers with TS experience: “TS-specific instruments/guidelines will be helpful for us to share with the regular neuropsychologists as well who may not be familiar with TS.” Nearly all providers reported they would consider using a short, validated screening tool for neurodevelopmental (93%) or mental health (93%) concerns in TS if such tools were available.
Multidisciplinary collaborations. Respondents noted that, although they did not always have the time or training to conducting such screenings, they supported partnering with developmental pediatricians, trainees, primary care providers, social workers, and medical assistants to accomplish this: “We have a social worker who carries out preliminary screening and helps organize referrals for detailed screening, so I do not perform it myself. I do believe it is in my purview to see that it has been done, but I do not have the expertise or time to perform it personally.” Multidisciplinary clinics allowed respondents to practice within their scope while simultaneously meeting the complex needs of girls with TS: “I believe that care of children with Turner syndrome is best done in a multispecialty system. I take care of the growth and endocrine issues, a cardiologist should take care of the cardiovascular issues, a nephrologist the renal issues, and a developmental specialist the neurodevelopmental screening and issues.” Indeed, respondents who reported behavioral health specialist(s) are part of the multidisciplinary clinic for TS at their institution were 3.2 more likely to report their TS patients receive both neurodevelopmental and mental health screening (95% CI 1.7– 6.0).
DISCUSSION
This cross-sectional survey of US and Canadian pediatric endocrinologists revealed that less than a quarter report knowledge of their patients with TS receiving neurodevelopmental and mental health screening per the TS CPG. A minority of endocrine providers are currently performing neurodevelopmental or mental health screening for patients with TS, however many would be interested in implementing a brief screening tool into their clinical practice. Many respondents were uncomfortable with providing neurodevelopmental screening with current training and tools. There was a greater sense of comfort with conducting mental health screenings, but challenges with being able to find adequate follow up care for positive screens were expressed by the majority of respondents. These preliminary survey data suggest that incorporating neurodevelopmental and/or mental health screenings for girls with TS into pediatric endocrinology care may be feasible if several barriers are addressed.
While neurodevelopmental deficits and psychosocial concerns are well-recognized as part of the TS phenotype, many girls are not identified early or appropriately supported leading to greater problems in adulthood. The TS CPG advocate for annual screening of these risks but our results support the anecdotal impression that there is large variability in care practices across the country. These results support that behavioral health clinicians integrated into a multidisciplinary care setting for girls with TS is ideal, therefore advocating for these clinic models whenever feasible. Indeed, multidisciplinary TS clinics have proven beneficial for several non-endocrine outcomes; however, many clinical practices do not have trained behavioral health clinicians available to be integrated into routine care[8]. Therefore, novel approaches are needed to ensure all girls with TS receive routine screening that will identify neurodevelopmental and mental health concerns early.
One proposal is to incorporate a screening process into routine endocrine care. Nearly all girls with TS regularly see endocrinology, so endocrinologists already assume responsibility for screening for other non-endocrine risks in TS, and mental health screening has been successfully implemented in endocrine practices for other patient populations such as type 1 diabetes [9]. Furthermore, neurodevelopmental and mental health screening has been implemented in other unrelated subspecialties that care for chronic pediatric diseases, including pediatric hematology/oncology, pulmonology, gastroenterology, and cardiology [10–14]. In order to accomplish this, a TS-specific screening tool would need to be developed and validated as while there are many generic screening instruments, nothing has been validated within the TS population and the sensitivity for identifying the unique deficits in girls with TS is unknown. Disease-specific screening tools have been developed and validated in other populations, including: congenital heart disease, craniofacial conditions, and disorders of sex development [15–17]. For such a screening tool to be implemented by pediatric endocrinologists for patients with TS, our results support the importance of such a tool being short (< 3 minutes) and straightforward for non-behavioral health clinicians to interpret. Parent-reported surveys integrated into the electronic medical record, automatic scoring, and system-generated recommendations could minimize time and involvement of the endocrinologist and ideally another member of the medical team could be trained to facilitate the implementation of such a tool [18, 19]. Finally, local resources for acting on a positive screen need to be established prior to implementation of a screening program, particularly for mental health concerns in areas with limited resources [20]. In one study evaluating mental health screening in a pediatric allergy clinic, free mental health consultations were only attended by 1% of families with no difference between those who had or had not received screening in the clinic, emphasizing the necessity of a systems approach to this problem [21].
Exploring clinician’s perspectives on neurodevelopmental and mental health screening within an endocrine practice assesses the feasibility of one proposal to address the lack of screening per best practice recommendations. Additional approaches such as implementing screening in a primary care, educational, or home setting should also be explored although similar barriers will likely present. Importantly, development and validation of a brief TS-specific screening tool could be implemented in other settings as well. It is important to note that by utilizing endocrinology care as an infrastructure to conduct screenings, we are not suggesting replacement of behavioral health clinicians with endocrinologists, or that endocrinologists should begin conducting behavioral health assessments or interventions. By screening for neurodevelopmental and mental health concerns however, the endocrinologist conveys the importance of these factors in their overall health and can encourage further evaluation and intervention from local systems including early intervention and school district services, primary care resources, private therapies, and telehealth in addition to traditional mental health services [22].
The primary limitation to this survey-based study is the low response rate (~11%) when compared to the total number of emails dispersed, which is lower than several other published Pediatric Endocrine Society surveys (18–21%) [23, 24]. However, given the specific inclusion criteria of active clinicians who treat girls with TS, it is likely that many of the Pediatric Endocrine Society members would not have been eligible. As it is reasonable to assume that respondents had an interest in the topic, our estimation of the proportion of endocrinologists currently screening or willing to implement a new screening tool may be inflated. Furthermore, these results do not necessarily reflect the proportion of girls with TS receiving screening, just the knowledge of the pediatric endocrinologist of whether screening is being conducted. Despite these limitations, this study employed mixed methods to assess the viewpoints of pediatric endocrinologists and provides valuable information for developing and integrating neurodevelopmental and/or mental health screening for youth with TS.
In conclusion, ~10% of endocrine care providers currently screen their patients with TS for neurodevelopmental concerns and ~25% screen for mental health concerns. Notably, many acknowledge they have no knowledge of their patients receiving routine screening for these well-known risks. Although there are several barriers to screening for neurodevelopmental and mental health concerns within the pediatric endocrinology clinic setting, most providers would be interested in utilizing a short, validated TS-specific screening tool. Additional research is needed to develop such a tool with the considerations described in this report, as well as addressing the issue of access to quality behavioral health services more globally.
Fig. 1.
a. Slightly over half of all respondents reported their patients with Turner syndrome (TS) receive screening for neurodevelopmental (ND) concerns, mental health (MH) concerns, or both neurodevelopmental and mental health concerns (ND & MH). Respondents who practiced at an institution with a TS multidisciplinary clinic (MDC) with an integrated behavioral health specialist (b) and those who see at least five patients with TS per month (c) were more likely to report their patients with TS receive ND and MH screenings.
Fig. 2.
Responses endorsed by pediatric endocrine respondents for barriers to neurodevelopmental (a) and mental health (b) screening, and whether they would be interested in implementing a screening tool in the pediatric endocrinology clinic setting.
Acknowledgement
The authors would like to thank the Pediatric Endocrine Society and their members for distributing and completing this survey.
Funding Sources
This work was supported by Abigail Wexner Research Institute at Nationwide Children’s Hospital (CC); NIH/NCATS UL1TR002733; NIH/NICHD K23HD092588 (SD); and NIH/NCI K08CA237338 (LN). Contents are the authors’ sole responsibility and do not necessarily represent official NIH views.
Conflict of Interest Statement
SD has received grant funding from the NICHD, Pediatric Endocrine Society, Endocrine Fellows Foundation, Turner Syndrome Global Alliance, and Association for X&Y Chromosome Variations (AXYS). CC and AT have received grant funding from the NIMHD and NICHD. LN has received grant funding from the NCI. SD, LN, JK are members of the Pediatric Endocrine Society.
Footnotes
Statement of Ethics
This study was approved by the Institutional Review Board at Nationwide Children’s Hospital (STUDY00000025). All respondents provided electronic informed consent for their anonymous survey responses to be used for research.
REFERENCES
- 1.Hutaff-Lee C, Bennett E, Howell S, Tartaglia N. Clinical developmental, neuropsychological, and social-emotional features of Turner syndrome. Am J Med Genet C Semin Med Genet. 2019;181(1):126–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morris LA, Tishelman AC, Kremen J, Ross RA. Depression in Turner Syndrome: A Systematic Review. Arch Sex Behav. 2020;49(2):769–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gravholt CH, Andersen NH, Conway GS, Dekkers OM, Geffner ME, Klein KO, et al. Clinical practice guidelines for the care of girls and women with Turner syndrome: proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. Eur J Endocrinol. 2017;177(3):G1–g70. [DOI] [PubMed] [Google Scholar]
- 4.Hirai AH, Kogan MD, Kandasamy V, Reuland C, Bethell C. Prevalence and Variation of Developmental Screening and Surveillance in Early Childhood. JAMA Pediatr. 2018;172(9):857–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cascio MA, Lee E, Vaudrin N, Freedman DA. A Team-based Approach to Open Coding: Considerations for Creating Intercoder Consensus. Field Methods. 2019;31(2):116–30. [Google Scholar]
- 6.Johnny S The Coding Manual for Qualitative Researchers Hardcover. SAGE Publications Ltd2015. [Google Scholar]
- 7.Creswell JW. Qualitative inquiry and research design (international student edition). Choosing among five approaches. 14 142017. [Google Scholar]
- 8.Morgan TL, Kapa HM, Crerand CE, Kremen J, Tishelman A, Davis S, et al. Fertility counseling and preservation discussions for females with Turner syndrome in pediatric centers: practice patterns and predictors. Fertil Steril. 2019;112(4):740–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marker AM, Patton SR, McDonough RJ, Feingold H, Simon L, Clements MA. Implementing clinic-wide depression screening for pediatric diabetes: An initiative to improve healthcare processes. Pediatr Diabetes. 2019;20(7):964–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iturralde E, Adams RN, Barley RC, Bensen R, Christofferson M, Hanes SJ, et al. Implementation of Depression Screening and Global Health Assessment in Pediatric Subspecialty Clinics. J Adolesc Health. 2017;61(5):591–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Annett RD, Patel SK, Phipps S. Monitoring and Assessment of Neuropsychological Outcomes as a Standard of Care in Pediatric Oncology. Pediatr Blood Cancer. 2015;62 Suppl 5:S460–513. [DOI] [PubMed] [Google Scholar]
- 12.Schatz J, Schlenz AM, Smith KE, Roberts CW. Predictive validity of developmental screening in young children with sickle cell disease: a longitudinal follow-up study. Dev Med Child Neurol. 2018;60(5):520–6. [DOI] [PubMed] [Google Scholar]
- 13.Daly B, Kral MC, Tarazi RA. The role of neuropsychological evaluation in pediatric sickle cell disease. Clin Neuropsychol. 2011;25(6):903–25. [DOI] [PubMed] [Google Scholar]
- 14.Knutson S, Kelleman MS, Kochilas L. Implementation of Developmental Screening Guidelines for Children with Congenital Heart Disease. J Pediatr. 2016;176:135–41.e2. [DOI] [PubMed] [Google Scholar]
- 15.Marino BS, Lipkin PH, Newburger JW, Peacock G, Gerdes M, Gaynor JW, et al. Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: a scientific statement from the American Heart Association. Circulation. 2012;126(9):1143–72. [DOI] [PubMed] [Google Scholar]
- 16.Crerand CE, Kapa HM, Litteral J, Pearson GD, Eastman K, Kirschner RE. Identifying Psychosocial Risk Factors Among Families of Children With Craniofacial Conditions: Validation of the Psychosocial Assessment Tool-Craniofacial Version. Cleft Palate Craniofac J. 2018;55(4):536–45. [DOI] [PubMed] [Google Scholar]
- 17.Ernst MM, Gardner M, Mara CA, Délot EC, Fechner PY, Fox M, et al. Psychosocial Screening in Disorders/Differences of Sex Development: Psychometric Evaluation of the Psychosocial Assessment Tool. Horm Res Paediatr. 2018;90(6):368–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.White P, Kenton K. Use of electronic medical record-based tools to improve compliance with cervical cancer screening guidelines: effect of an educational intervention on physicians’ practice patterns. J Low Genit Tract Dis. 2013;17(2):175–81. [DOI] [PubMed] [Google Scholar]
- 19.Jetelina KK, Woodson TT, Gunn R, Muller B, Clark KD, DeVoe JE, et al. Evaluation of an Electronic Health Record (EHR) Tool for Integrated Behavioral Health in Primary Care. J Am Board Fam Med. 2018;31(5):712–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Geist R Improving access to mental health services for youth and parents. Paediatr Child Health. 2004;9(8):533–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shemesh E, Lewis BJ, Rubes M, Ambrose MA, Cahill MK, Knight C, et al. Mental Health Screening Outcomes in a Pediatric Specialty Care Setting. J Pediatr. 2016;168:193–7.e3. [DOI] [PubMed] [Google Scholar]
- 22.Findling RL, Stepanova E. The Workforce Shortage of Child and Adolescent Psychiatrists: Is It Time for a Different Approach? J Am Acad Child Adolesc Psychiatry. 2018;57(5):300–1. [DOI] [PubMed] [Google Scholar]
- 23.Marks BE, Wolfsdorf JI, Waldman G, Stafford DE, Garvey KC. Pediatric Endocrinology Trainees’ Education and Knowledge About Insulin Pumps and Continuous Glucose Monitors. Diabetes Technol Ther. 2019;21(3):105–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guttmann-Bauman I, Thornton P, Adhikari S, Reifschneider K, Wood MA, Hamby T, et al. Pediatric endocrine society survey of diabetes practices in the United States: What is the current state? Pediatr Diabetes. 2018;19(5):859–65. [DOI] [PubMed] [Google Scholar]