Supplemental Digital Content is available in the text.
Keywords: animal models, antibiotics, fluid therapy, sepsis, sex, systematic review
Abstract
OBJECTIVES:
Preclinical studies provide an opportunity to evaluate the relationship between sex and sepsis, and investigate underlying mechanisms in a controlled experimental environment. The objective of our systematic review was to assess the impact of biological sex on treatment response to fluid and antibiotic therapy in animal models of sepsis. Furthermore, we provide a narrative elaboration of sex-dependent differences in preclinical models of sepsis.
DATA SOURCES:
MEDLINE and Embase were searched from inception to March 16, 2020.
STUDY SELECTION:
All studies reporting sex-stratified data comparing antibiotics and/or fluid resuscitation with a placebo or no treatment arm in an in vivo model of sepsis were included.
DATA EXTRACTION:
Outcomes of interest were mortality (primary) and organ dysfunction (secondary). Risk of bias was assessed. Study selection and data extraction were conducted independently and in duplicate.
DATA SYNTHESIS:
The systematic search returned 2,649 unique studies, and two met inclusion criteria. Both studies used cecal ligation and puncture models with imipenem/cilastatin antibiotics. No eligible studies investigated fluids. In one study, antibiotic therapy significantly reduced mortality in male, but not female, animals. The other study reported no sex differences in organ dysfunction. Both studies were deemed to be at a high overall risk of bias.
CONCLUSIONS:
There is a remarkable and concerning paucity of data investigating sex-dependent differences in fluid and antibiotic therapy for the treatment of sepsis in animal models. This may reflect poor awareness of the importance of investigating sex-dependent differences. Our discussion therefore expands on general concepts of sex and gender in biomedical research and sex-dependent differences in key areas of sepsis research such as the cardiovascular system, immunometabolism, the microbiome, and epigenetics. Finally, we discuss current clinical knowledge, the potential for reverse translation, and directions for future studies.
REGISTRATION:
PROSPERO CRD42020192738.
Historically, much of our knowledge and evidence in biomedical research is founded on data from male subjects only, leading to conclusions and clinical guidelines potentially being inappropriately applied to the entire population (1, 2). This issue is even more pervasive in preclinical animal research, where single-sex studies of male animals outnumber those of females six to one in some fields (3). This historical sex bias in animal research is particularly worrisome, given that it has been proposed as a potential factor limiting translational research success (2, 4) and that sex-dependent differences are consistently reported in disease pathogenesis and outcomes (5–7), drug pharmacokinetics and pharmacodynamics (8), and response to treatments (9–12).
Sepsis is the life-threatening organ dysfunction in response to infection, estimated to account for one in five annual deaths worldwide and is recognized by the World Health Organization as a global health priority (13). Despite the incredible effort dedicated to treating sepsis and searching for novel treatments, mortality rates for septic shock have remained at 25–30% (14). Numerous studies investigating the connection between biological sex and sepsis outcomes have been conducted, but two clinical systematic reviews on this topic were inconclusive and recommended further investigation (15, 16).
In order to inform future sepsis studies that account for biological sex and to evaluate novel interventions within representative patient populations, a strong foundational understanding of sex differences is critical. This knowledge must start with the cornerstones of sepsis treatment, namely fluids and antibiotics. Consistent with evidence supporting the efficacy of antibiotic and fluid resuscitation, current clinical guidelines recommend their immediate administration after the development of sepsis (17). However, this treatment does not stratify according to biological sex, and therefore, sex-dependent differences in treatment response are not routinely considered.
Given the limitations of clinical studies of biological sex (i.e., restricted to observational data), animal models offer a unique opportunity to directly evaluate the relationship between biological sex and treatment response in the absence of other confounding variables. There is evidence to suggest that female animals are protected in sepsis, and numerous mechanisms for these potential sex differences have been described (18–20); however, the interaction between biological sex and treatment response has been overlooked. Thus, in this systematic review, we synthesized available evidence to assess the influence of biological sex in animal models of sepsis treated with fluids or antibiotics. The paucity of data found suggested that there may be a lack of awareness or understanding of this issue. Therefore, we were asked by the editors to provide a brief narrative elaboration on the effects of sex and gender in both clinical and preclinical sepsis, highlighting how sex-dependent differences may impact various physiologic and pathologic processes.
MATERIALS AND METHODS
Our protocol was registered on the International Prospective Register of Systematic Reviews (https://www.crd.york.ac.uk/PROSPERO, CRD42020192738). The article was prepared in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist (21) (Appendix 1, Supplemental Digital Content, http://links.lww.com/CCX/A624).
Eligibility Criteria
We included all interventional, in vivo studies (randomized, nonrandomized, or pseudorandomized) that compared antibiotics and/or fluid resuscitation with a placebo or no treatment arm. All included studies must have used a true infectious model of sepsis (e.g., cecal ligation and puncture [CLP] models were included, but models using lipopolysaccharide injection were excluded), reported using animals of both sexes, and reported sex-stratified outcomes. Full-text articles published in English were included. Gray literature, abstracts, commentaries, letters, reviews, and editorials were excluded. Invertebrate animal models were excluded.
Outcomes
Our primary outcome was mortality compared between biological sexes. Organ dysfunction compared between biological sexes was a secondary outcome.
Literature Search Strategy
Our search strategy of MEDLINE and Embase (inception to March 16, 2020) was developed in collaboration with an information specialist with expertise in the design of preclinical systematic searches (Risa Shorr, MLS, Ottawa Hospital Library Services) (Appendix 2, Supplemental Digital Content, http://links.lww.com/CCX/A624). Using the Peer Review of Electronic Search Strategies framework (22), an additional information specialist (not associated with the review) evaluated the strategy.
Study Selection
All studies identified by our search were imported into DistillerSR (Evidence Partners, Ottawa, ON, Canada). Two independent reviewers screened titles, abstracts, and full text for inclusion. All conflicts were resolved through discussion with a senior team member.
Data Extraction
Two independent reviewers extracted relevant information from each study in duplicate, using a pilot-tested and standardized data extraction form created in DistillerSR. Extracted data included study characteristics, intervention characteristics, risk of bias details, and outcomes. Engauge Digitizer Software (http://markummitchell.github.io/engauge-digitizer) was used to extract and quantify data found only in graphical format. Any disagreements were resolved through consensus discussion, and if necessary, a third party was consulted.
Data Analysis
Mortality was analyzed using a Kruskal-Wallis test. For histological measures of organ dysfunction, the mean difference (MD) and pooled sd in histology score between antibiotic treated and placebo-treated animals were calculated for both male and female animal experiments. A random effects inverse variance meta-analyses (with accompanying 95% CIs) was used to analyze the difference between the MDs.
Risk of Bias Assessment
Included studies were assessed for risk of bias using a modified version of the Systematic Review Centre for Laboratory Animal Experimentation risk of bias tool. This is a specifically designed and validated adaptation of the Cochrane Risk of Bias tool for use in preclinical animal studies. Assessments were performed independently and in duplicate by two reviewers.
Deviations From Protocol
A number of outcomes reported in our protocol were not included in the review due to an insufficient number of included articles reporting these outcomes (markers of pulmonary, renal, hepatic, cardiac, and pancreatic dysfunction; bacterial load). In addition, we were not able to perform pooled meta-analysis, conduct our planned subgroup analyses, or assess publication bias due to limited available data. Post hoc, we rescreened articles for neonatal studies but were unable to identify any that met eligibility criteria.
RESULTS
Our literature search returned 2,649 unique citations (Fig. 1). Of the full-text articles screened (n = 176), numerous studies were excluded because either only animals of a single sex were used (n = 31) or even when animals of both sexes were used, no sex-stratified data were provided (n = 40). Two studies met eligibility criteria and were included in this review (23, 24). Both reported sex-dependent effects of antibiotic administration. No studies reported sex-dependent effects of fluid resuscitation. One older study investigating antibiotics briefly stated that no differences were observed between males and females (i.e., line item result); however, no further details were provided (25).
Figure 1.
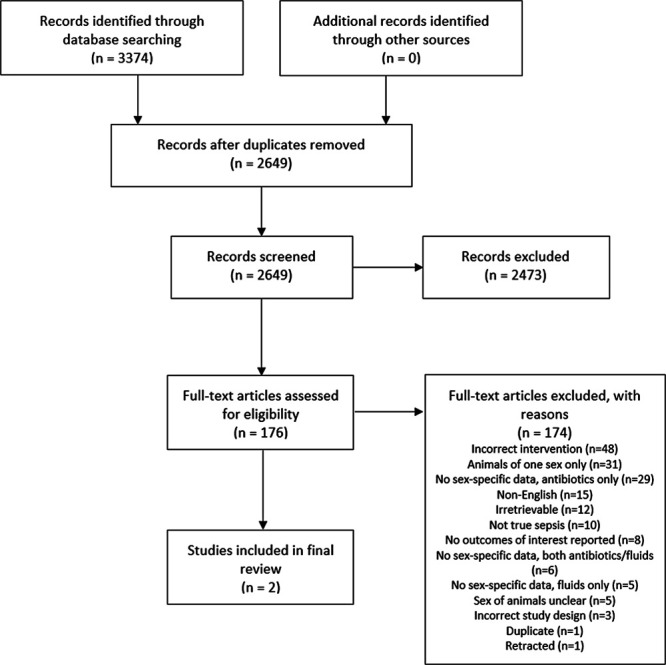
Study selection flow diagram.
Characteristics of Included Studies
Summarized characteristics of included studies are in Table 1. One study was published in 2018 (24), the other in 2019 (23), and both were conducted in the United States. Both used CLP to model sepsis in C57BL/6 mice. The total sample sizes of these two studies were 190 (23) and 200 (24), but data from experiments reporting sex-specific sepsis data used 10–15 (23) or 10 mice (24) per treatment arm.
TABLE 1.
Study Characteristics and Findings of Included Studies
| References; Sample Size | Animal Strain, Species, Age | Sepsis Model | Control Group | Antibiotic Used | Dose, No. of Doses, Route of Administration, Time of Administration | Outcomes | Findings |
|---|---|---|---|---|---|---|---|
| Das et al (23); n = 190 (~40–75 with sex-stratified data reported) | C57BL/6, mice, 10–12 wk | CLP | No treatment | Imipenem/cilastatin | 5 mg/kg, every 12 hr for 7 d, subcutaneous injection, 30 min after sepsis induction | Standardized Histological Injury Scores (heart, lung, liver, spleen, kidney, gut, brain, ovary, testis) | No significant differences between males and females |
| Lewis et al (24); n = 200 (50 total with sex-stratified data reported) | C57BL/6, mice, 8–12 wk | CLP | No treatment/low-dose antibiotics | Imipenem/cilastatin | 25 mg/kg, 1, intraperitoneal injection, 0 and 4 hr after meeting criteria for physiologic deterioration | Mortality | Males had greater treatment response than females |
CLP = cecal ligation and puncture.
The antibiotic used in both studies was imipenem (administered with cilastin, which potentiates the effects of imipenem). One study administered the antibiotic intraperitoneally in a single dose (25 mg/kg) (24), and the other administered it subcutaneously (5 mg/kg) every 12 hours for 7 days (23). One study investigated antibiotic therapy after meeting predetermined criteria defining physiologic deterioration after CLP versus a 4-hour delay (early vs late treatment) (24). The other study administered treatment 30 minutes post CLP (23).
Primary Outcome—Mortality
One study reported sex-specific data (10 mice used per treatment arm (24)); the other reported that sex-dependent differences were not observed (23). Early antibiotic treatment significantly prolonged time to 50% mortality compared with late antibiotic treatment in male mice (3,361 vs 1,546 min), but not in female mice (1,579 vs 1,295 min). Additionally, female mice of both early and late antibiotic treatment groups died significantly sooner than male mice. Even female mice with early antibiotic treatment died significantly sooner than male mice with late antibiotic treatment.
Secondary Outcome—Organ Dysfunction
One study reported histological measures of tissue damage in the heart, lung, liver spleen, kidney, gut, brain, testis, and ovary, stratified by sex (23). No significant differences were observed between response to antibiotic therapy between male and female mice (Appendix 3, Supplemental Digital Content, http://links.lww.com/CCX/A624).
Risk of Bias Assessment
Both studies were deemed to be at high risk of bias due to incomplete outcome reporting (Appendix 4, Supplemental Digital Content, http://links.lww.com/CCX/A624). One study reported randomization of animals, but the method of randomization was not described (24). Neither study reported blinding of either experimenters or during outcome assessment nor whether animal allocation to treatment was concealed.
DISCUSSION
Our preclinical systematic review investigating the effects of sex-dependent differences in treatment response for sepsis identified only two relevant articles. Furthermore, no studies using fluids as treatment were found, and the focus of the two included studies was not on investigating the effects of biological sex. Our results highlight a concerning scarcity of preclinical sepsis studies investigating the effects of biological sex on clinically relevant, foundational therapies for sepsis. Exploring these questions in preclinical animal studies would minimize confounders and could reveal both subtle differences and mechanistic underpinnings that would not be possible in the most rigorous observational clinical studies.
Preclinical sex-dependent differences to sepsis therapy should be understood prior to investigating novel interventions that are typically evaluated in the laboratory setting. Without this knowledge, beneficial effects of novel therapies may be lost when translated to a clinical setting where female and male patients with sepsis will all presumably be treated with fluids and antibiotics. It is also interesting that the two studies that investigated antibiotic therapy demonstrated disparate results, with one finding no difference in mortality, whereas the other observed less mortality in male mice. We cannot rule out that protocol differences may account for these disparate results; more standardized approaches to preclinical experimental design of sepsis studies may address this issue in the future.
Our study has limitations. We were unable to perform meta-analyses due to the lack of included studies. Given that our review focused on treatment response to standard therapies in sepsis, we did not include studies of novel therapies. Similarly, studies exploring mechanisms underlying potential sex-dependent differences using only animals of one sex were also excluded (e.g., using techniques such as testosterone receptor blockade in male animals or ovariectomy in female animals). We would argue, however, that we must first understand sex-dependent responses to standard treatments in order to better predict and evaluate responses to novel therapies. Ultimately, the paucity of studies investigating sex-dependent differences in sepsis with fluid and antibiotic treatment highlights the need for more clinically relevant, methodologically rigorous preclinical studies exploring this issue.
As a result of the paucity of data found, and our subsequent discussion with the editors of Critical Care Explorations, it was felt that a further elaboration was needed on the differential effects of sex in sepsis. Therefore, the following expanded discussion briefly highlights clinical and preclinical research on the effects of biological sex in various physiologic and pathologic processes in sepsis. We begin with a primer on sex and gender considerations in biomedical research. Next, we provide a brief narrative review of potential sex-dependent differences and highlight important knowledge gaps in specific areas of interest in sepsis research: immunometabolism, the epigenome, microbiome, and cardiovascular function during sepsis. Furthermore, we discuss current clinical knowledge and the potential for reverse translation with regard to sex-dependent differences in sepsis and provide suggestions for future studies. The reader should be aware that the following information was not synthesized according to a prespecified protocol and thus should be regarded as a narrative elaboration. Of note, we have also recently published a narrative review discussing sex- and gender-dependent issues in both clinical and preclinical sepsis (20).
Introduction to Sex and Gender in Sepsis Research
Although frequently used interchangeably, “sex” and “gender” encompass two distinct entities. According to the Canadian Institutes of Health Research, sex refers to “a set of biological attributes in humans and animals, including chromosomes, gene expression, hormone levels and function, and reproductive/sexual anatomy” (26). On the other hand, gender refers to the “socially constructed roles, behaviors, expressions, and identities of girls, women, boys, men and gender diverse people” (26). Consistency in the use of this language in biomedical research is imperative to disentangle the effects of sex and gender on human health and disease and to promote the clear dissemination of knowledge. This is of particular importance since sex and gender can have divergent effects on various diseases. For example, female gender is associated with recurrent acute coronary syndrome independent of female sex (27), and feminine gender characteristics have been associated with increased somatic symptoms and chronic diseases, especially in men (28). Guidance on the correct use of the terms sex and gender is available for clinical research (29, 30). Despite this, it has been demonstrated that most clinical practice guidelines use the terms “sex” and “gender” incorrectly, leading to the unique effects of these variables to be relatively underexplored and underappreciated (31, 32). Within the domain of laboratory animal–based sepsis studies, “sex” is almost universally the appropriate term to be used, as the social constructs of gender are not typically studied in this setting.
Sex bias has increasingly been suggested as a potential factor contributing to poor translation, given that animals of predominantly male sex are used in preclinical sepsis studies, whereas females account for approximately half of all sepsis cases in humans (4, 13). Indeed, funding agencies such as the National Institutes of Health in the United States and the Canadian Institutes of Health Research have statements encouraging preclinical scientists to account for sex as a basic biological variable to improve our understanding of health and disease in both males and females (26, 33). Even with the recent advocacy for the incorporation of sex- and gender-based analyses into study design, multiple studies demonstrate that sex bias still persists in both clinical and preclinical research (34, 35). Interestingly, although the use of female animals has significantly increased over the past decade, “sex-based analysis” is conducted and reported in only a minority of studies (35). Results from male and female animals are usually presented in a pooled manner, making it impossible to identify sex-dependent differences. It is critical that laboratory-based studies report sex-stratified data, so that differences (which may not be apparent in a single laboratory study) can be identified by pooling results across multiple studies (e.g., by future preclinical systematic reviews and meta-analysis). Table 2 highlights basic considerations for future preclinical sepsis research.
TABLE 2.
Basic Considerations for Future Preclinical Studies
| 1) Use the terms “sex” and “gender” correctly. Within laboratory animal research, the correct term is almost universally “sex.” |
| 2) Incorporate both male and female animals in preclinical studies. |
| 3) Report data stratified by sex, even if there are no apparent differences. |
In the clinical setting, numerous studies have been conducted investigating the effects of biological sex in sepsis, but few have evaluated the effects of gender. Hence, for this review, we will reference “sex” in clinical studies where participants are classified as either male or female. A recent analysis of global sepsis incidence found that age-adjusted sepsis incidence from 1990 to 2017 was higher among females than males (13). Despite this, females are systematically underrepresented in sepsis clinical trials (36). In this regard, guideline management of sepsis draws from evidence that may not apply equally to males and females. Complicating this discussion is the recognition that disparities in delivery of care between males and females may also impact guideline adherence for sepsis therapy (37), similar to gaps noted in cardiovascular disease (38). Considering mortality in septic patients, numerous individual studies have been conducted, with conflicting evidence. While some studies have shown that males experience higher mortality from sepsis and septic shock (39–41), others demonstrated either higher mortality in females (42–45) or no sex-dependent differences (46, 47). Two systematic reviews have summarized this evidence and demonstrated overall equivocal findings, emphasizing the need for additional, methodologically rigorous studies on this issue (15, 16). Thus, although the following sections largely focus on potential sex-dependent pathophysiology of sepsis as studied in preclinical animal models, it is important to note that large knowledge gaps remain in clinical sepsis research in regards to sex- and gender-dependent differences.
Sex-Dependent Differences in Immunometabolism
Immunometabolism is focused on the dynamic interplay between metabolism and the immune response. Metabolic processes regulate the immune system during normal physiology, but these effects may be amplified during severely pathologic processes such as those which occur during sepsis. Failure to consider the role of metabolic dysfunction during sepsis may contribute to the lack of success in translational sepsis research (48). This section briefly discusses potential sex-dependent differences in the immune response and metabolic processes that may contribute to sex-dependent differences in sepsis.
Sex-dependent differences in the immune response during clinical sepsis have generally been observed on a macroscopic level; however, the data are conflicting. Significantly higher levels of proinflammatory cytokines such as interleukin (IL)–6 and procalcitonin have been observed in male septic patients (49); similarly, endotoxin challenge to healthy volunteers was shown to elicit a greater inflammatory response (tumor necrosis factor [TNF]–α, IL-1β, IL-6, and IL-8) in whole blood from males compared with females (50). In contrast, other studies have found that females exhibited a more proinflammatory response following endotoxin challenge, with higher increases in C-reactive protein, TNF-α, and leukocyte sequestration (51, 52).
Preclinical studies have provided insight into sex-dependent differences in the immune response. Tissue-resident leukocyte populations in the peritoneal and pleural cavities have been shown to be more abundant and yield a greater density of Toll-like receptors (TLRs) in female mice via elevated tissue chemokine expression. This may contribute to higher survival in female animals through enhanced detection and elimination of pathogens (53). In another study, female mice subjected to CLP demonstrated more robust cell-mediated immune responses and a subsequently higher survival rate than male mice (54). Interestingly, male mice subjected to hemorrhage prior to CLP had both increased mortality as well as increased levels of IL-6, TNF-α, and prostaglandin E2 compared with male mice subjected to CLP only (55). In contrast, mortality following CLP did not increase in female mice first subjected to hemorrhage compared with sham, and plasma levels of IL-6 and TNF-α did not increase (55). These differences were credited to the effects of estrogen. This study highlights how sex-dependent differences in immune function may lead to differential outcomes in sepsis depending on various precipitating factors or other superimposed comorbidities. Interestingly, biological sex, but not female reproductive cyclicity, has been shown to influence the peripheral blood immune cell prevalence in mice (56). Specifically, it has been observed that female mice have fewer monocytes, neutrophils, and natural killer cells and that males exhibit greater variability in the peripheral blood immunophenotype (56). The authors also demonstrated that the common practice of using equal numbers of male and female mice is often not appropriate and subsequently provided guidance to facilitate sample size calculations for peripheral immune cells (i.e., that consider the effects of sex) (56). Additionally, a biologically modified beta-glucan (poly-[1, 6]-β-D-glucopyranosyl-[1, 3]-β-D-glucopyranose glucan) was shown to enhance 10-day survival after CLP in female mice but not in male mice and ovariectomized female mice. These results were attributed to the effect of the treatment in decreasing levels of IL-6 and IL-10 and reducing bacterial burden in livers of proestrus female mice (57). Furthermore, 10-day survival in ovariectomized female mice was not improved with a single dose of estrogen administered at the time of fluid resuscitation, highlighting how mechanisms independent of sex hormones likely contribute to fundamental sex-dependent differences.
Hyperinflammation observed in the acute phase of sepsis has been linked to metabolic changes such as energy deprivation, increased metabolic demand, and end-organ failure. The impairment of oxidative phosphorylation and the subsequent metabolic shift toward glycolysis are thought to be due to decreased expression of peroxisomal proliferator-activated receptor (PPAR)-γ (which mediates lipid and glucose metabolism) and impaired mitochondrial function (critical for oxidative phosphorylation and cell metabolism) (48, 58, 59). Interestingly, preclinical studies demonstrated that mitochondria in females have lower levels of oxidative stress (which was suppressed by ovariectomy) and higher levels of antioxidants and antioxidant enzymes (60, 61). This may confer protection during sepsis. Furthermore, sex-dependent differences in expression of various PPAR isoforms (which regulate lipid and glucose metabolism, and immunity) have been observed (62).
Although many of these sex-dependent differences have been attributed, at least in part, to sex hormones, other potential factors such as the dimorphic expression of genes encoded on the X chromosome likely contribute. The X chromosome contains a large number of immune-related genes (63, 64) and also encodes a significant number of mitochondrial genes, which govern the critical role of the mitochondria in immune cell fate and function (65). These contributions from genes encoded on the X chromosome toward immunometabolism are of particular interest given the hemizygosity (referring to individuals with only one member of a chromosome pair) of males for the X chromosome and that 15–25% of genes escape X chromosome inactivation in females (66, 67). For example, escape of the TLR7 gene results in increased expression in males (68).
Currently, immune cell biomarkers such as cytokines are used to represent the pro- or anti-inflammatory state during sepsis, and evidence suggests that sex-dependent differences in the immune response may influence the morbidity and mortality associated with sepsis. Future studies investigating the changes in specific immune cell populations (which may be responsible for differential expression of cytokines) may inform development of therapies targeting specific immune cell populations. Furthermore, a thorough time-course evaluation of immunometabolic shifts which occur during the various stages of sepsis pathogenesis will provide insight into the potential use of time-matched therapeutics. Using integrative omics to decipher the regulation of X chromosome inheritance and its role in immunometabolic regulatory mechanisms could further advance our understanding of observed sex-dependent differences in sepsis. Overall, due to abundant and highly specific potential therapeutic targets, immunometabolism is a promising field of study to explore novel therapeutics for sepsis.
Sex-Dependent Differences in the Microbiome
In addition to the intrinsic biological differences between males and females that are conferred by genetics, the sexes are also distinguished by the microbiome, an important extrinsic biological influence. It is well established that microbiota-host mutualism is critical for immune development and homeostasis, such that alterations of the microbiome can confer susceptibility to infections and sepsis (69–71). Therefore, difference in microbial communities between males and females is a potentially unique driver of sexual dimorphism in sepsis pathogenesis, as the microbiome is both extrinsic to the host and may be modified therapeutically (i.e., via pre-, pro-, and antibiotics). In this section, we discuss key sepsis-related findings regarding the microbiome, and how sex-dependent differences may play a role in divergent sepsis pathogenesis and outcomes.
Clinical observational studies of hospitalized patients have identified an association between intestinal dysbiosis and the risk of acquiring sepsis, in that patients with microbiota dysbiosis (including those with Clostridium difficile infection or those who have received systemic antibiotics) were found to be at significantly higher risk of being readmitted to hospital with sepsis (72, 73). In preclinical studies, pathologic alterations of the microbiome have also been shown to modulate the risk of sepsis, organ dysfunction, and mortality in multiple models of bacterial infection. Notably, prevention of gut dysbiosis in neonatal mice has been shown to prevent late-onset sepsis (74), and mice with higher gut α-diversity have improved survival following CLP compared with genetically identical mice (from different vendors) with lower α-diversity (75). Furthermore, fecal microbiota transplant from mice who survived sepsis into susceptible mice improves survival following CLP (76).
Microbiota differences between males and females exist both anatomically (e.g., the unique urogenital microbiome niche in females), as well as compositionally (77). In a sex-matched study of gut microbiome profiles in 89 different mouse strains, important differences were observed in both microbial composition and biodiversity, with female mice harboring greater bacterial α-diversity as well as greater abundance of key immune-modulating microbial taxa (e.g., Clostridiaceae and Lachnospiraceae families) (78). Given the links between greater gut microbiome biodiversity, colonization with short-chain fatty acid producing taxa (such as Lachnospiraceae), and improved outcomes in sepsis and critical illness, it is possible that sex-dependent composition may contribute to differences in sepsis outcomes as well (71, 79–81).
A key mechanism by which microbiome differences drive sexual dimorphism of disease pathogenesis is through the mutualistic relationship between commensal microbes and the immune system. Landmark studies using combinations of germ-free mice and fecal transplantation between females and males have demonstrated that sex-dependent differences in the microbiome directly confer sexual dimorphism of immune-mediated diseases. For example, in the nonobese diabetic mouse model of type-1 diabetes, there is a significantly higher incidence of diabetes in females compared with males, which is lost when these mice are raised under germ-free conditions (82). Furthermore, transplantation of the intestinal microbiome from male mice into female mice led to a reduced risk of diabetes in females through the induction of hormonal and metabolomic changes that suppressed pancreatic islet inflammation and autoantibody production (83). These and other studies have clearly established that sex-dependent differences in the microbiome can impart significant dimorphism of immune development, function, and pathogenesis in immune-mediated disease.
Further research is also required to clarify how sex-dependent differences in the microbiome contribute to host defense, immunopathogenesis, and outcomes in sepsis. An important first step will be to analyze the microbiome composition and diversity between septic males and females, both in human cohorts and animal models. Causal and mechanistic implications of sex-dependent microbiome differences can then be comprehensively evaluated using germ-free and gnotobiotic approaches to dissect the role of the microbiome, together with genetic tools to delineate the impact of host biological sex (e.g., the Four Core Genotypes model) (84). Understanding the impact of the microbiome in sepsis pathogenesis will not only further our basic understanding of this disease but may yield novel targets for treatments that harness the therapeutic malleability of the microbiome.
Sex-Dependent Differences in Epigenetics
Beginning in embryonic development and continuing throughout the course of life, epigenetic modifications contribute to unique phenotypic expression of every individual. During sepsis, epigenetic changes can profoundly modify the host response during both early and late stages of the disease (reviewed in [85]). Furthermore, pathogens modify host immune responses through epigenetic mechanisms (i.e., production of microRNAs [miRs], enzymes targeting host chromatin, and manipulation of host epigenetic enzymes) (85), highlighting the importance of the epigenome in the host defense. As such, in this section we discuss sex-dependent differences in epigenetics such as X chromosome inactivation and differences in histone modifications and miR expression, which may contribute to sexually dimorphic outcomes in sepsis.
Beginning in utero, X chromosome inactivation occurs in XX females to equalize gene dosage as compared to XY males (86). This process results in a unique mosaic expression of X chromosomes in every female, due to the random inactivation of either the maternal or paternal X chromosome. This X-linked mosaicism may have significant implications in the progression of major disease, including sex-dependent differences in sepsis. For example, skewing of X-inactivation in white blood cells has been shown to correlate with injury severity after trauma (87). In studies using mice subjected to CLP, X-linked polymorphisms and mosaicism in nicotinamide adenine dinucleotide phosphate oxidase 2 and interleukin-1 receptor associated kinase 1 resulted in a unique immune phenotype and were shown to improve survival (88, 89). Although potentially beneficial in sepsis, this process of random X-inactivation can also be detrimental, which is thought to contribute to the higher prevalence of autoimmune diseases in females (90). Interestingly, the number of X chromosomes has been shown to influence production of inflammatory cytokines. Following stimulation of whole blood with various TLR ligands, patients with Klinefelter’s syndrome (who carry two X chromosomes but are phenotypically male) exhibited a similar inflammatory response to females but not males, even after adjustment for levels of sex hormones (91). Likewise, prepubescent patients with Turner’s syndrome (who only have a single X chromosome but are phenotypically female) have been shown to exhibit a similar pattern of cytokine production as prepubescent males (92).
A landmark investigation demonstrated that significant changes in DNA methylation (at hundreds of genomic regions) and histone modifications (specifically H3K27 acetylation and H3K4 methylation) profoundly impact gene expression in response to endotoxin (93). Notably, hypomethylation of the TNF promoter concomitant with displacement of nucleosomes from the binding site for nuclear factor kappa-light-chain-enhancer of activated B cells is known to up-regulate TNF transcription in response to endotoxin stimulation in human monocytes (94, 95). Further, recurrent methylation of this promoter may contribute to “endotoxin tolerance” in the sepsis-associated immune suppression observed in later stages of the disease (96). Male (but not female) offspring of fathers subjected to CLP were shown to have a depressed response 24 hours after a subsequent endotoxin challenge, with lower plasma concentrations of IL-6, TNF-α, and IL-10 (97). Interestingly, these findings were attributed to alterations in sperm DNA methylation, providing evidence for intergenerational sex-dependent differences mediated via epigenetics. In a separate study, median autosomal DNA methylation in males was decreased, whereas no differences were found between males and females in mean autosomal DNA methylation (98). Interestingly, epigenetic modifiers such as procainamide and hydralazine (DNA methyltransferase inhibitors) have been shown to improve hypotension, hypoglycemia, and multiple organ dysfunction in endotoxemic mice (99). Significant differences in histone modifications between males and females have also been observed, such as the dimorphic methylation of H3 in the brains of neonatal mice, which was shown to be testosterone independent (100). Although additional studies are needed, it is clear that differences in DNA methylation (101) and histone modifications between males and females likely affect sepsis pathogenesis and outcomes.
Noncoding RNAs (e.g., miRs) are RNA molecules that regulate gene expression and play an important role in the host response to sepsis. For example, certain miRs (miR-221, miR-579, and miR125b) expressed by LPS-tolerant monocytes have been shown to reduce levels of TNF-α in response to endotoxin, which may contribute to sepsis-related immune suppression (102). Significant differences in miR expression between males and females are known to be regulated by both testosterone and estrogen (reviewed in [103]). Given the relatively high number of miRs expressed on the X chromosome (~800 vs 2 on the Y chromosome) (104), both mosaic expression of X chromosome-encoded genes and escape of genes from X-inactivation in females may result in differential expression of miRs that may be relevant in sepsis pathogenesis (105). For instance, miR-548am-5p overexpression decreases susceptibility to mitochondrial apoptosis (106). Future research will need to investigate whether sex-dependent differences in miR expression have clinically relevant effects in sepsis pathogenesis.
Epigenetic modifications have a profound impact on the host response; however, the basic epigenetic changes which occur during sepsis are poorly understood. Specifically, a paucity of clinical studies investigating epigenetic changes in sepsis patients has been conducted, representing an important knowledge gap (85). Likewise, establishing a foundational understanding of sex-dependent epigenetic differences and the underlying mechanisms in healthy subjects will be critical to subsequently identify the role of these differences in sepsis pathogenesis and outcomes.
Cardiovascular Sex-Dependent Differences
Cardiovascular dysfunction is common in sepsis and is characterized by compromised ventricular function, systemic vasodilation and vascular dysfunction, as well as the development of cardiac arrhythmias. Sex-dependent differences in cardiovascular function during sepsis have been observed in both clinical and preclinical studies and may contribute to differential outcomes in sepsis. This section will briefly discuss the evidence surrounding sex-dependent differences in myocardial performance, vascular endothelial function, and response to certain sepsis treatments.
A significant body of evidence suggests that many potential sex-dependent differences in cardiovascular function during sepsis may be attributed to the sex hormones estrogen and testosterone (107). However, given the systemic nature of sepsis, it is difficult to ascertain whether sex-dependent differences stem predominantly from direct or indirect effects of these sex hormones. For example, some sex-dependent differences in sepsis outcomes have been attributed to the modulatory effects of sex hormones on immune function; whereas testosterone has demonstrated immunosuppressive effects (108), estrogen promotes both pro- and anti-inflammatory responses that may improve survival in sepsis (107). However, there may also be nonhormonal explanations for cardiovascular outcomes in sepsis as sex-dependent outcome differences exist in neonatal sepsis where hormonal differences are minimal (75). Nonetheless, delineating the indirect and direct effects of sex hormones on cardiac function, vascular function, and vascular barrier function may improve our understanding of sex-dependent risk profiles (109). As an example, 17-β-estradiol administration to endotoxemic mice was shown to improve myocardial function in isolated hearts (110). In this same experiment, endotoxin also induced increased expression of TNF-α in males (via increases in Rac1 and nicotinamide adenine dinucleotide phosphate oxidase activity, and phosphorylation of extracellular signal-regulated kinase 1/2 and p38 mitogen-activated protein kinase). However, treatment with 17 β-estradiol improved splanchnic circulation but did not improve cardiac output or systemic oxygen consumption in male rats after trauma-hemorrhage and CLP (111).
Although there is a paucity of clinical evidence surrounding sex-dependent differences in septic myocardial performance in humans, there is increasing preclinical evidence of the unique molecular mechanisms underlying sex-dependent differences in septic myocardial impairment in animals. For instance, in a mouse model of endotoxemia, animals of both sexes developed cardiac dysfunction as evidenced by reduced left ventricular ejection fraction and depressed sarcomere shortening in paced cardiomyocytes (112). Interestingly, male mice demonstrated soluble guanylyl cyclase-independent depression of myocardial cellular calcium transients and sarcoplasmic reticulum Ca2+-ATPase inhibition, whereas female mice did not demonstrate these alterations in sarcomere function. Instead, cardiac dysfunction in females may be dependent on soluble guanylyl cyclase-dependent myofilament dysfunction (113). Similar findings have also been demonstrated in mice subjected to CLP (and resuscitated with antibiotics and fluids), where sarcoplasmic reticulum dysfunction was the result of Ca2+-ATPase inhibition in males; however, females were more resistant to these alterations (114).
Vascular endothelial dysfunction (vasomotion and vessel permeability) is also impacted by sepsis in a sex-dependent manner, although clinical evidence is relatively sparse. Vasomotion may be affected by production of nitric oxide with numerous preclinical studies demonstrating estrogen-dependent enhancement of nitric oxide production from endothelial nitric oxide synthase via phosphoinositide 3-kinase/protein kinase B stimulation (115), which is known to be lost in the progression of sepsis (116). Beyond nitric oxide, testosterone has also been shown to have vasodilatory effects (117). However, in contrast to estrogen, testosterone acts directly on vascular smooth muscle cells through calcium or potassium channels (118, 119) and therefore does not require an intact endothelium (120). Whether this mechanism contributes to sex-dependent differences in sepsis will need to be investigated in future clinical studies.
With regard to interventions targeting the cardiovascular system in sepsis, interesting clinical (121, 122) and preclinical (123–125) evidence exists for selective β1-adrenergic blockade. One study demonstrated that β1-adrenergic blockade improved cardiac function in male rats with intraperitoneal sepsis, whereas females responded poorly to β1-adrenergic blockade (125). Interestingly, β1-adrenergic blockade also increased vascular endothelial nitric oxide synthase expression in male CLP mice, but not in female mice (125), suggesting a mechanism for these sex-dependent differences.
Taken together, sex-dependent cardiovascular differences in the molecular and treatment responses are well documented in experimental models of endotoxemia and sepsis, as well as in clinical studies. However, the mechanisms underlying these differences are important knowledge gaps that could inform the use of tailored treatments to improve management, treatment, and long-term recovery in sepsis. Further, whether strategic use of sex hormones as treatment adjuncts to improve clinical management of septic patients may warrant further investigation.
Reverse Translational Sepsis Research
The laboratory is an ideal setting for assessing mechanisms of disease in a controlled environment and allows for “reverse” translation, that is, sophisticated testing of knowledge gaps identified during clinical research and practice. This model for bidirectional knowledge exchange has been championed by various national and international research organizations and ensures that results at the bench and bedside are harmonized to maximize translational impact and improve patient care. In this section, we discuss key sex-dependent differences in sepsis observed in the clinical setting and the potential for reverse translation of this knowledge.
Returning to the focus of our systematic review, we would hypothesize that biological sex would significantly modulate responses to antibiotics and fluids in human sepsis. Sex-dependent differences in pharmacokinetics and drug metabolism are well recognized (8, 126) and contribute to clinically relevant differences in drug responses to digoxin, antidepressants, and chemotherapy (9, 11, 12). When applied to antibiotics, these effects may impact drug levels required for bactericidal activity or the bioavailability of oral antibiotics following first-pass metabolism. Personalized and precision dosing of antibiotics in critical illness is gaining more widespread recognition (127–129), and preclinical investigation that considers biological sex will add to the efficacy of this area of clinical research.
In sepsis, the hemodynamic goal of fluid therapy is to restore effective circulating volume, augment preload and cardiac output, and improve end-organ perfusion. Therefore, before examining sex differences in fluid therapy, consideration must be given to the cardiovascular systems of men and women. For example, females tend to have lower resting blood pressures, normalized blood volumes, and higher total peripheral resistance (130)—notwithstanding the dramatic cardiovascular changes associated with pregnancy. Moreover, response to cardiovascular stress for healthy men and women is also different following intense exercise (131) postural hypotension (132, 133) and hypovolemia (134). The neural-hemodynamic balance between cardiac output and peripheral resistance, mediated by the sympathetic nervous system, appears to have important sex-dependent differences with consequential effects for blood pressure regulation under healthy and diseased conditions (135, 136). From a cardiac performance standpoint, healthy females appear to have higher myocardial perfusion (137), cardiac strain (138), cardiac flow dynamics (139), and more favorable LV twist mechanics following acute reductions in preload (140). These considerations may explain the differing hemodynamic responses encountered by healthy men and women following exposure to endotoxin. One study found reduced blood pressure drop in women despite similar cytokine profiles (141), whereas another study found more dramatic blood pressure drop in females, along with higher proinflammatory mediators and preserved sensitivity to norepinephrine (51). These examples underscore the complex interactions between sex hormones, inflammation, and cardiovascular hemodynamics that require further study in clinical and preclinical research.
Based on available evidence, we would again hypothesize that responses to fluid therapy would differ between females and males. From a practical standpoint, fluids are rarely administered in adults according to weight (despite guideline recommendations), which implies that smaller females are systematically exposed to potentially harmful effects of overresuscitation (142). This sex-dependent disparity may be especially meaningful when considering the use of early vasopressors as a fluid-sparing modality for the management of septic shock (143–145). Furthermore, it is unclear whether the “one-size-fits-all” management for septic shock resuscitation provides equal benefit for men and women; given different baseline hemodynamics and responses to stress, it is possible that resuscitation targets need to be adapted with sex-specific considerations to optimize treatment at the bedside. In addition, it is important to note that other treatments administered to sepsis patients in the clinical setting may affect outcomes in a sex-dependent manner. For example, opioid analgesia is administered to many critically ill patients. Interestingly, buprenorphine has been shown to negatively affect survival in male mice subjected to CLP, but not in female mice (146). In this regard, preclinical studies may offer mechanistic insights that can help development of these novel resuscitation strategies.
Although many arguments are given both in support and in opposition of murine models of sepsis, few would argue against refining and improving the models we currently use. Importantly, key findings from human sepsis studies should be used in the refinement of preclinical models of sepsis (147). A novel model of polytrauma and shock was developed by attempting to reflect the equivalent of an Injury Severity Score greater than 15 (typically used in the clinical setting to identify severely injured patients) (148). Furthermore, the applicability of this model was supported by findings demonstrating a greater magnitude and duration of changes in blood leukocyte gene expression (more closely resembling the human condition) compared with other murine models of trauma (148). Similarly, increasing the severity of a mouse trauma model improved the correlation in transcriptome response compared with humans (149). Another established modification to the CLP model of sepsis involves subjecting mice to hemorrhage prior to CLP, reflecting the high incidence of trauma patients who subsequently develop sepsis (150).
Current clinical knowledge surrounding the use of fluid and antibiotic therapy has informed the development of initiatives such as the Minimum Quality Threshold in Preclinical Sepsis Studies (MQTiPSS) (151). Concerningly, the authors reveal that over 70% of the most highly cited papers using sepsis models published between 2003 and 2012 failed to use or report fluid and/or antibiotic therapy. Considering these findings and the relatively recent emphasis on investigating sex-dependent differences in major disease, our concerning systematic review findings reflect these noted trends. Specific recommendations were subsequently provided by the MQTiPSS to guide the use and reporting of fluid and antibiotic therapy in animal models of sepsis, which will surely serve to improve the applicability and comparability of these studies if implemented by sepsis researchers (151).
Future Directions
Although the investigation of sex- and gender-dependent differences is receiving increasing attention, our systematic review and narrative discussion identify significant knowledge gaps that remain unaddressed in sepsis. Important knowledge gaps and future directions discussed in this article are highlighted in Table 3. As evidenced by this systematic review, clinically relevant, methodologically rigorous preclinical studies investigating sex-dependent differences in sepsis are urgently needed. However, accurately modeling clinical sepsis in animal models remains challenging. In the clinical setting, the development and progression of sepsis is precipitated by a myriad of different pathologic processes and further complicated by the superposition of seemingly endless combinations of comorbidities. Although many preclinical studies attempt to replicate polymicrobial sepsis with models such as CLP, important factors such as technical ability, available resources, and route/dose of administration of different treatments affect the reliability and reproducibility of important findings. Specifically, standardized models of sepsis may improve the applicability and reproducibility of preclinical sepsis studies. Fewer experimental animals may be needed, given that results from one study may more readily be compared with another and that heterogeneity in results may be attributed to the disease process rather than technical factors (152). Two sets of criteria have recently been suggested to further this pursuit, focused on standardizing the technical aspects for various models of sepsis, and describing important parameters and outcomes which should be recorded when studying animal models of sepsis (152). It is also important to recognize that the use of standardized models does not prohibit more complex models of the same disease, as standardized models provide a baseline for comparison (152). These benefits are of particular interest in the investigation of sex-dependent differences, which may only manifest in analyses that include pooled data from many studies. The MQTiPSS has also provided recommendations to improve translational research success in preclinical sepsis studies (153), surrounding study design and humane modeling endpoints (154), preferred types of infections and organ dysfunction endpoints (155), and the aforementioned recommendations surrounding fluid and antibiotic therapy (151). Importantly, the MQTiPSS also highlights sex as an important variable that should be explored (154). Ultimately, increasing recognition of the importance of sex- and gender-dependent differences must be reflected in the frequency by which scientists stratify and analyze data according to sex or gender (i.e., conduct and report sex- and gender-based analyses).
TABLE 3.
Important Knowledge Gaps and Future Directions
| Area of Sepsis Research | Knowledge Gaps and Future Directions |
|---|---|
| Immunometabolism | Characterize sex-dependent immune cell population differences for the development of cell-specific therapeutic targets. |
| Study the sequence of immunometabolic changes in immune cell populations to identify shifts associated with overactive or suppressed immune responses during sepsis, to aid in the development of precise, individualized immunometabolic therapies. | |
| Decipher the regulation of X chromosome inheritance with respect to immunometabolic regulatory mechanisms using an integrative omics approach. | |
| Microbiome | Determine the impact of sex-dependent differences in the microbiome and the influence on sepsis outcomes, in both human cohorts as well as preclinical models. |
| Apply germ-free and gnotobiotic approaches together with genetic tools, to dissect the role of the microbiome in the pathogenesis of sepsis, including the impact of sex-dependent differences. | |
| Determine the impact of biological sex on the therapeutic response to microbiota-targeted therapies in sepsis and critical illness (e.g., antibiotics and digestive decontamination, probiotics, synbiotics). | |
| Epigenetics | Establish a baseline understanding of epigenetic modifications which occur during sepsis (in animal models as well as human cohorts). |
| Investigate the effects of X-linked mosaicism and the role of the X-chromosome in potentially divergent sepsis outcomes in the clinical setting. | |
| Clarify the influence of sex-dependent differences in noncoding RNA expression and histone/gene modifications which may affect the development and progression of sepsis. | |
| Cardiovascular | Stratification of hemodynamic phenotypes in human sepsis according to biological sex. |
| Investigate the direct and indirect effects of sex hormones and/or menopausal status on hemodynamics and cardiovascular function in human sepsis. | |
| Identify sex-dependent resuscitation targets in sepsis. | |
| Investigate the salutary effects of sex hormones as adjunct therapies in sepsis, shock and trauma. | |
| Reverse translation | Apply clinical knowledge to develop novel models and modify existing models of preclinical sepsis to better represent the human condition. |
| Use clinical knowledge of sex-dependent differences in the design of preclinical studies, which may provide mechanistic insight and guide future research. | |
| Apply principles espoused by the minimum quality threshold in preclinical sepsis studies expert consensus statements. |
ACKNOWLEDGMENTS
We thank Risa Shorr, MLS (Librarian, Learning Services, The Ottawa Hospital), for assistance with the systematic search strategy.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Supported, in part, by a Project Grant from the Canadian Institutes of Health Research.
Dr. Lalu is supported by The Ottawa Hospital Anesthesia Alternate Funds Association and holds a University of Ottawa Junior Research Chair in Innovative Translational Research. Dr. Macala is supported by the Royal Alexandra Hospital Foundation. Dr. Fox-Robichaud is the Scientific Director of Sepsis Canada and is funded by grants from the Canadian Institutes of Health Research and National Science and Engineering Research Council of Canada. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Harris DJ, Douglas PS. Enrollment of women in cardiovascular clinical trials funded by the National Heart, Lung, and Blood Institute. N Engl J Med. 2000; 343:475–480 [DOI] [PubMed] [Google Scholar]
- 2.Zucker I, Beery AK. Males still dominate animal studies. Nature. 2010; 465:690. [DOI] [PubMed] [Google Scholar]
- 3.Beery AK, Zucker I. Sex bias in neuroscience and biomedical research. Neurosci Biobehav Rev. 2011; 35:565–572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dyson A, Singer M. Animal models of sepsis: Why does preclinical efficacy fail to translate to the clinical setting? Crit Care Med. 2009; 37:S30–S37 [DOI] [PubMed] [Google Scholar]
- 5.Wada H, Miyauchi K, Daida H. Gender differences in the clinical features and outcomes of patients with coronary artery disease. Expert Rev Cardiovasc Ther. 2019; 17:127–133 [DOI] [PubMed] [Google Scholar]
- 6.Cenko E, van der Schaar M, Yoon J, et al. Sex-related differences in heart failure after ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2019; 74:2379–2389 [DOI] [PubMed] [Google Scholar]
- 7.Silbiger S, Neugarten J. Gender and human chronic renal disease. Gend Med. 2008; 5(Suppl A):S3–S10 [DOI] [PubMed] [Google Scholar]
- 8.Soldin OP, Mattison DR. Sex differences in pharmacokinetics and pharmacodynamics. Clin Pharmacokinet. 2009; 48:143–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rathore SS, Wang Y, Krumholz HM. Sex-based differences in the effect of digoxin for the treatment of heart failure. N Engl J Med. 2002; 347:1403–1411 [DOI] [PubMed] [Google Scholar]
- 10.Cenko E, van der Schaar M, Yoon J, et al. Sex-specific treatment effects after primary percutaneous intervention: A study on coronary blood flow and delay to hospital presentation. J Am Heart Assoc. 2019; 8:e011190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.LeGates TA, Kvarta MD, Thompson SM. Sex differences in antidepressant efficacy. Neuropsychopharmacology. 2019; 44:140–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Özdemir BC, Csajka C, Dotto GP, et al. Sex differences in efficacy and toxicity of systemic treatments: An undervalued issue in the era of precision oncology. J Clin Oncol. 2018; 36:2680–2683 [DOI] [PubMed] [Google Scholar]
- 13.Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: Analysis for the global burden of disease study. Lancet. 2020; 395:200–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reinhart K, Daniels R, Kissoon N, et al. Recognizing sepsis as a global health priority - a WHO resolution. N Engl J Med. 2017; 377:414–417 [DOI] [PubMed] [Google Scholar]
- 15.Failla KR, Connelly CD. Systematic review of gender differences in sepsis management and outcomes. J Nurs Scholarsh. 2017; 49:312–324 [DOI] [PubMed] [Google Scholar]
- 16.Papathanassoglou E, Middleton N, Benbenishty J, et al. Systematic review of gender- dependent outcomes in sepsis. Nurs Crit Care. 2017; 22:284–292 [DOI] [PubMed] [Google Scholar]
- 17.Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Crit Care Med. 2018; 46:997–1000 [DOI] [PubMed] [Google Scholar]
- 18.Knöferl MW, Angele MK, Diodato MD, et al. Female sex hormones regulate macrophage function after trauma-hemorrhage and prevent increased death rate from subsequent sepsis. Ann Surg. 2002; 235:105–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barter J, Kumar A, Stortz JA, et al. Age and sex influence the hippocampal response and recovery following sepsis. Mol Neurobiol. 2019; 56:8557–8572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang M, Macala KF, Fox-Robichaud A, et al. Sex- and gender-dependent differences in clinical and preclinical sepsis. Shock 2021. [online ahead of print] [DOI] [PubMed]
- 21.Moher D, Liberati A, Tetzlaff J, et al. ; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009; 6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McGowan J, Sampson M, Salzwedel DM, et al. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016; 75:40–46 [DOI] [PubMed] [Google Scholar]
- 23.Das P, Panda SK, Agarwal B, et al. Novel chitohexaose analog protects young and aged mice from CLP induced polymicrobial sepsis. Sci Rep. 2019; 9:2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewis AJ, Griepentrog JE, Zhang X, et al. Prompt administration of antibiotics and fluids in the treatment of sepsis: A murine trial. Crit Care Med. 2018; 46:e426–e434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baker CC, Chaudry IH, Gaines HO, et al. Evaluation of factors affecting mortality rate after sepsis in a murine cecal ligation and puncture model. Surgery. 1983; 94:331–335 [PubMed] [Google Scholar]
- 26.Canadian Institutes of Health Research. How to Integrate Sex and Gender Into Research. Available at: https://cihr-irsc.gc.ca/e/50836.html. Accessed September 27, 2020
- 27.Pelletier R, Khan NA, Cox J, et al. ; GENESIS-PRAXY Investigators. Sex versus gender-related characteristics: Which predicts outcome after acute coronary syndrome in the young? J Am Coll Cardiol. 2016; 67:127–135 [DOI] [PubMed] [Google Scholar]
- 28.Ballering AV, Bonvanie IJ, Olde Hartman TC, et al. Gender and sex independently associate with common somatic symptoms and lifetime prevalence of chronic disease. Soc Sci Med. 2020; 253:112968. [DOI] [PubMed] [Google Scholar]
- 29.Clayton JA, Tannenbaum C. Reporting sex, gender, or both in clinical research? JAMA. 2016; 316:1863–1864 [DOI] [PubMed] [Google Scholar]
- 30.Clayton JA. Studying both sexes: A guiding principle for biomedicine. FASEB J. 2016; 30:519–524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schiebinger L, Stefanick ML. Gender matters in biological research and medical practice. J Am Coll Cardiol. 2016; 67:136–138 [DOI] [PubMed] [Google Scholar]
- 32.Tannenbaum C, Clow B, Haworth-Brockman M, et al. Sex and gender considerations in Canadian clinical practice guidelines: A systematic review. CMAJ Open. 2017; 5:E66–E73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.National Institutes of Health. Consideration of Sex as a Biological Variable in NIH-funded Research. Available at: https://grants.nih.gov/grants/guide/notice-files/not-od-15-102.html. Accessed September 27, 2020
- 34.Feldman S, Ammar W, Lo K, et al. Quantifying sex bias in clinical studies at scale with automated data extraction. JAMA Netw Open. 2019; 2:e196700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Woitowich NC, Beery A, Woodruff T. A 10-year follow-up study of sex inclusion in the biological sciences. Elife. 2020; 9:e56344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Antequera A, Madrid-Pascual O, Solà I, et al. Female under-representation in sepsis studies: A bibliometric analysis of systematic reviews and guidelines. J Clin Epidemiol. 2020; 126:26–36 [DOI] [PubMed] [Google Scholar]
- 37.Sunden-Cullberg J, Nilsson A, Inghammar M. Sex-based differences in ED management of critically ill patients with sepsis: A nationwide cohort study. Intensive Care Med. 2020; 46:727–736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Regitz-Zagrosek V. Therapeutic implications of the gender-specific aspects of cardiovascular disease. Nat Rev Drug Discov. 2006; 5:425–438 [DOI] [PubMed] [Google Scholar]
- 39.Adrie C, Azoulay E, Francais A, et al. ; OutcomeRea Study Group. Influence of gender on the outcome of severe sepsis: A reappraisal. Chest. 2007; 132:1786–1793 [DOI] [PubMed] [Google Scholar]
- 40.Couto DdO, Peixoto Júnior AA, Farias JLMd, et al. Associação entre sexo e mortalidade em pacientes com sepse: Os hormônios sexuais influenciam o desfecho? Revista Brasileira de Terapia Intensiva. 2011; 23:297–303 [PubMed] [Google Scholar]
- 41.Schröder J, Kahlke V, Staubach KH, et al. Gender differences in human sepsis. Arch Surg. 1998; 133:1200–1205 [DOI] [PubMed] [Google Scholar]
- 42.Eachempati SR, Hydo L, Barie PS. Gender-based differences in outcome in patients with sepsis. Arch Surg. 1999; 134:1342–1347 [DOI] [PubMed] [Google Scholar]
- 43.Nachtigall I, Tafelski S, Rothbart A, et al. Gender-related outcome difference is related to course of sepsis on mixed ICUs: A prospective, observational clinical study. Crit Care. 2011; 15:R151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pietropaoli AP, Glance LG, Oakes D, et al. Gender differences in mortality in patients with severe sepsis or septic shock. Gend Med. 2010; 7:422–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sakr Y, Elia C, Mascia L, et al. The influence of gender on the epidemiology of and outcome from severe sepsis. Crit Care. 2013; 17:R50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wichmann MW, Inthorn D, Andress HJ, et al. Incidence and mortality of severe sepsis in surgical intensive care patients: The influence of patient gender on disease process and outcome. Intensive Care Med. 2000; 26:167–172 [DOI] [PubMed] [Google Scholar]
- 47.Mahmood K, Eldeirawi K, Wahidi MM. Association of gender with outcomes in critically ill patients. Crit Care. 2012; 16:R92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Koutroulis I, Batabyal R, McNamara B, et al. Sepsis immunometabolism: From defining sepsis to understanding how energy production affects immune response. Crit Care Explor. 2019; 1:e0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oberholzer A, Keel M, Zellweger R, et al. Incidence of septic complications and multiple organ failure in severely injured patients is sex specific. J Trauma. 2000; 48:932–937 [DOI] [PubMed] [Google Scholar]
- 50.Aulock SV, Deininger S, Draing C, et al. Gender difference in cytokine secretion on immune stimulation with LPS and LTA. J Interferon Cytokine Res. 2006; 26:887–892 [DOI] [PubMed] [Google Scholar]
- 51.van Eijk LT, Dorresteijn MJ, Smits P, et al. Gender differences in the innate immune response and vascular reactivity following the administration of endotoxin to human volunteers. Crit Care Med. 2007; 35:1464–1469 [DOI] [PubMed] [Google Scholar]
- 52.Wegner A, Benson S, Rebernik L, et al. Sex differences in the pro-inflammatory cytokine response to endotoxin unfold in vivo but not ex vivo in healthy humans. Innate Immun. 2017; 23:432–439 [DOI] [PubMed] [Google Scholar]
- 53.Scotland RS, Stables MJ, Madalli S, et al. Sex differences in resident immune cell phenotype underlie more efficient acute inflammatory responses in female mice. Blood. 2011; 118:5918–5927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zellweger R, Wichmann MW, Ayala A, et al. Females in proestrus state maintain splenic immune functions and tolerate sepsis better than males. Crit Care Med. 1997; 25:106–110 [DOI] [PubMed] [Google Scholar]
- 55.Diodato MD, Knöferl MW, Schwacha MG, et al. Gender differences in the inflammatory response and survival following haemorrhage and subsequent sepsis. Cytokine. 2001; 14:162–169 [DOI] [PubMed] [Google Scholar]
- 56.Breznik JA, Schulz C, Ma J, et al. Biological sex, not reproductive cycle, influences peripheral blood immune cell prevalence in mice. J Physiol. 2021; 599:2169–2195 [DOI] [PubMed] [Google Scholar]
- 57.Newsome CT, Flores E, Ayala A, et al. Improved antimicrobial host defense in mice following poly-(1,6)-β-D-glucopyranosyl-(1,3)-β-D-glucopyranose glucan treatment by a gender-dependent immune mechanism. Clin Vaccine Immunol. 2011; 18:2043–2049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Drosatos K, Khan RS, Trent CM, et al. Peroxisome proliferator-activated receptor-γ activation prevents sepsis-related cardiac dysfunction and mortality in mice. Circ Heart Fail. 2013; 6:550–562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kelly B, O’Neill LA. Metabolic reprogramming in macrophages and dendritic cells in innate immunity. Cell Res. 2015; 25:771–784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Borrás C, Sastre J, García-Sala D, et al. Mitochondria from females exhibit higher antioxidant gene expression and lower oxidative damage than males. Free Radic Biol Med. 2003; 34:546–552 [DOI] [PubMed] [Google Scholar]
- 61.Gaignard P, Savouroux S, Liere P, et al. Effect of sex differences on brain mitochondrial function and its suppression by ovariectomy and in aged mice. Endocrinology. 2015; 156:2893–2904 [DOI] [PubMed] [Google Scholar]
- 62.Park HJ, Choi JM. Sex-specific regulation of immune responses by PPARs. Exp Mol Med. 2017; 49:e364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Markle JG, Fish EN. SeXX matters in immunity. Trends Immunol. 2014; 35:97–104 [DOI] [PubMed] [Google Scholar]
- 64.Fischer J, Jung N, Robinson N, et al. Sex differences in immune responses to infectious diseases. Infection. 2015; 43:399–403 [DOI] [PubMed] [Google Scholar]
- 65.Weinberg SE, Sena LA, Chandel NS. Mitochondria in the regulation of innate and adaptive immunity. Immunity. 2015; 42:406–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Carrel L, Willard HF. X-inactivation profile reveals extensive variability in X-linked gene expression in females. Nature. 2005; 434:400–404 [DOI] [PubMed] [Google Scholar]
- 67.Wainer Katsir K, Linial M. Human genes escaping X-inactivation revealed by single cell expression data. BMC Genomics. 2019; 20:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pisitkun P, Deane JA, Difilippantonio MJ, et al. Autoreactive B cell responses to RNA-related antigens due to TLR7 gene duplication. Science. 2006; 312:1669–1672 [DOI] [PubMed] [Google Scholar]
- 69.McDonald B, Zucoloto AZ, Yu IL, et al. Programing of an intravascular immune firewall by the gut microbiota protects against pathogen dissemination during infection. Cell Host Microbe. 2020; 28:660–668.e4 [DOI] [PubMed] [Google Scholar]
- 70.Jacobs MC, Haak BW, Hugenholtz F, et al. Gut microbiota and host defense in critical illness. Curr Opin Crit Care. 2017; 23:257–263 [DOI] [PubMed] [Google Scholar]
- 71.Levy M, Kolodziejczyk AA, Thaiss CA, et al. Dysbiosis and the immune system. Nat Rev Immunol. 2017; 17:219–232 [DOI] [PubMed] [Google Scholar]
- 72.Prescott HC, Dickson RP, Rogers MA, et al. Hospitalization type and subsequent severe sepsis. Am J Respir Crit Care Med. 2015; 192:581–588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Baggs J, Jernigan JA, Halpin AL, et al. Risk of subsequent sepsis within 90 days after a hospital stay by type of antibiotic exposure. Clin Infect Dis. 2018; 66:1004–1012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Singer JR, Blosser EG, Zindl CL, et al. Preventing dysbiosis of the neonatal mouse intestinal microbiome protects against late-onset sepsis. Nat Med. 2019; 25:1772–1782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fay KT, Klingensmith NJ, Chen CW, et al. The gut microbiome alters immunophenotype and survival from sepsis. FASEB J. 2019; 33:11258–11269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gong S, Yan Z, Liu Z, et al. Intestinal microbiota mediates the susceptibility to polymicrobial sepsis-induced liver injury by granisetron generation in mice. Hepatology. 2019; 69:1751–1767 [DOI] [PubMed] [Google Scholar]
- 77.Valeri F, Endres K. How biological sex of the host shapes its gut microbiota. Front Neuroendocrinol. 2021; 61:100912. [DOI] [PubMed] [Google Scholar]
- 78.Org E, Mehrabian M, Parks BW, et al. Sex differences and hormonal effects on gut microbiota composition in mice. Gut Microbes. 2016; 7:313–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Xu R, Tan C, Zhu J, et al. Dysbiosis of the intestinal microbiota in neurocritically ill patients and the risk for death. Crit Care. 2019; 23:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kim SM, DeFazio JR, Hyoju SK, et al. Fecal microbiota transplant rescues mice from human pathogen mediated sepsis by restoring systemic immunity. Nat Commun. 2020; 11:2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lamarche D, Johnstone J, Zytaruk N, et al. ; PROSPECT Investigators; Canadian Critical Care Trials Group; Canadian Critical Care Translational Biology Group. Microbial dysbiosis and mortality during mechanical ventilation: A prospective observational study. Respir Res. 2018; 19:245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yurkovetskiy L, Burrows M, Khan AA, et al. Gender bias in autoimmunity is influenced by microbiota. Immunity. 2013; 39:400–412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Markle JG, Frank DN, Mortin-Toth S, et al. Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science. 2013; 339:1084–1088 [DOI] [PubMed] [Google Scholar]
- 84.Golden LC, Itoh Y, Itoh N, Iyengar S, et al. Parent-of-origin differences in DNA methylation of X chromosome genes in T lymphocytes. Proc Natl Acad Sci U S A. 2019; 116:26779–26787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Binnie A, Tsang JLY, Hu P, et al. Epigenetics of sepsis. Crit Care Med. 2020; 48:745–756 [DOI] [PubMed] [Google Scholar]
- 86.Wutz A, Gribnau J. X inactivation Xplained. Curr Opin Genet Dev. 2007; 17:387–393 [DOI] [PubMed] [Google Scholar]
- 87.Pena G, Michalski C, Donnelly RJ, et al. Trauma-induced acute X chromosome skewing in white blood cells represents an immuno-modulatory mechanism unique to females and a likely contributor to sex-based outcome differences. Shock. 2017; 47:402–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chandra R, Federici S, Németh ZH, et al. Cellular mosaicism for X-linked polymorphisms and IRAK1 expression presents a distinct phenotype and improves survival following sepsis. J Leukoc Biol. 2014; 95:497–507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chandra R, Federici S, Németh ZH, et al. Female X-chromosome mosaicism for NOX2 deficiency presents unique inflammatory phenotype and improves outcome in polymicrobial sepsis. J Immunol. 2011; 186:6465–6473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Selmi C, Brunetta E, Raimondo MG, et al. The X chromosome and the sex ratio of autoimmunity. Autoimmun Rev. 2012; 11:A531–A537 [DOI] [PubMed] [Google Scholar]
- 91.Lefèvre N, Corazza F, Valsamis J, et al. The number of X chromosomes influences inflammatory cytokine production following toll-like receptor stimulation. Front Immunol. 2019; 10:1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Casimir GJ, Heldenbergh F, Hanssens L, et al. Gender differences and inflammation: An in vitro model of blood cells stimulation in prepubescent children. J Inflamm (Lond). 2010; 7:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Novakovic B, Habibi E, Wang SY, et al. β-Glucan reverses the epigenetic state of LPS-induced immunological tolerance. Cell. 2016; 167:1354–1368.e14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sullivan KE, Reddy AB, Dietzmann K, et al. Epigenetic regulation of tumor necrosis factor alpha. Mol Cell Biol. 2007; 27:5147–5160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.El Gazzar M, Liu T, Yoza BK, et al. Dynamic and selective nucleosome repositioning during endotoxin tolerance. J Biol Chem. 2010; 285:1259–1271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.El Gazzar M, Yoza BK, Chen X, et al. G9a and HP1 couple histone and DNA methylation to TNFalpha transcription silencing during endotoxin tolerance. J Biol Chem. 2008; 283:32198–32208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bomans K, Schenz J, Tamulyte S, et al. Paternal sepsis induces alterations of the sperm methylome and dampens offspring immune responses-an animal study. Clin Epigenetics. 2018; 10:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Johansson A, Enroth S, Gyllensten U. Continuous aging of the human DNA methylome throughout the human lifespan. PLoS One. 2013; 8:e67378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Shih CC, Liao MH, Hsiao TS, et al. Procainamide inhibits DNA methylation and alleviates multiple organ dysfunction in rats with endotoxic shock. PLoS One. 2016; 11:e0163690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tsai HW, Grant PA, Rissman EF. Sex differences in histone modifications in the neonatal mouse brain. Epigenetics. 2009; 4:47–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Singmann P, Shem-Tov D, Wahl S, et al. Characterization of whole-genome autosomal differences of DNA methylation between men and women. Epigenetics Chromatin. 2015; 8:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.El Gazzar M, McCall CE. MicroRNAs distinguish translational from transcriptional silencing during endotoxin tolerance. J Biol Chem. 2010; 285:20940–20951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sharma S, Eghbali M. Influence of sex differences on microRNA gene regulation in disease. Biol Sex Differ. 2014; 5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ghorai A, Ghosh U. miRNA gene counts in chromosomes vary widely in a species and biogenesis of miRNA largely depends on transcription or post-transcriptional processing of coding genes. Front Genet. 2014; 5:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Song R, Ro S, Michaels JD, et al. Many X-linked microRNAs escape meiotic sex chromosome inactivation. Nat Genet. 2009; 41:488–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Matarrese P, Tieri P, Anticoli S, et al. X-chromosome-linked miR548am-5p is a key regulator of sex disparity in the susceptibility to mitochondria-mediated apoptosis. Cell Death Dis. 2019; 10:673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Albertsmeier M, Pratschke S, Chaudry I, et al. Gender-specific effects on immune response and cardiac function after trauma hemorrhage and sepsis. Viszeralmedizin. 2014; 30:91–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Erikoğlu M, Sahin M, Ozer S, et al. Effects of gender on the severity of sepsis. Surg Today. 2005; 35:467–472 [DOI] [PubMed] [Google Scholar]
- 109.Kher A, Wang M, Tsai BM, et al. Sex differences in the myocardial inflammatory response to acute injury. Shock. 2005; 23:1–10 [DOI] [PubMed] [Google Scholar]
- 110.Zhu H, Shan L, Peng T. Rac1 mediates sex difference in cardiac tumor necrosis factor-alpha expression via NADPH oxidase-ERK1/2/p38 MAPK pathway in endotoxemia. J Mol Cell Cardiol. 2009; 47:264–274 [DOI] [PubMed] [Google Scholar]
- 111.Kuebler JF, Jarrar D, Toth B, et al. Estradiol administration improves splanchnic perfusion following trauma-hemorrhage and sepsis. Arch Surg. 2002; 137:74–79 [DOI] [PubMed] [Google Scholar]
- 112.Turdi S, Han X, Huff AF, et al. Cardiac-specific overexpression of catalase attenuates lipopolysaccharide-induced myocardial contractile dysfunction: Role of autophagy. Free Radic Biol Med. 2012; 53:1327–1338 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 113.Hobai IA, Aziz K, Buys ES, et al. Distinct myocardial mechanisms underlie cardiac dysfunction in endotoxemic male and female mice. Shock. 2016; 46:713–722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chen J, Chiazza F, Collino M, et al. Gender dimorphism of the cardiac dysfunction in murine sepsis: Signalling mechanisms and age-dependency. PLoS One. 2014; 9:e100631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ma XL, Gao F, Chen J, et al. Endothelial protective and antishock effects of a selective estrogen receptor modulator in rats. Am J Physiol Heart Circ Physiol. 2001; 280:H876–H884 [DOI] [PubMed] [Google Scholar]
- 116.Kimmoun A, Ducrocq N, Levy B. Mechanisms of vascular hyporesponsiveness in septic shock. Curr Vasc Pharmacol. 2013; 11:139–149 [PubMed] [Google Scholar]
- 117.Channer KS, Jones TH. Cardiovascular effects of testosterone: implications of the “male menopause”? Heart. 2003; 89:121–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.English KM, Jones RD, Jones TH, et al. Testosterone acts as a coronary vasodilator by a calcium antagonistic action. J Endocrinol Invest. 2002; 25:455–458 [DOI] [PubMed] [Google Scholar]
- 119.Deenadayalu VP, White RE, Stallone JN, et al. Testosterone relaxes coronary arteries by opening the large-conductance, calcium-activated potassium channel. Am J Physiol Heart Circ Physiol. 2001; 281:H1720–H1727 [DOI] [PubMed] [Google Scholar]
- 120.English KM, Jones RD, Jones TH, et al. Gender differences in the vasomotor effects of different steroid hormones in rat pulmonary and coronary arteries. Horm Metab Res. 2001; 33:645–652 [DOI] [PubMed] [Google Scholar]
- 121.Morelli A, Ertmer C, Westphal M, et al. Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: A randomized clinical trial. JAMA. 2013; 310:1683–1691 [DOI] [PubMed] [Google Scholar]
- 122.Gore DC, Wolfe RR. Hemodynamic and metabolic effects of selective beta1 adrenergic blockade during sepsis. Surgery. 2006; 139:686–694 [DOI] [PubMed] [Google Scholar]
- 123.Ackland GL, Yao ST, Rudiger A, et al. Cardioprotection, attenuated systemic inflammation, and survival benefit of beta1-adrenoceptor blockade in severe sepsis in rats. Crit Care Med. 2010; 38:388–394 [DOI] [PubMed] [Google Scholar]
- 124.Kimmoun A, Louis H, Al Kattani N, et al. β1-Adrenergic inhibition improves cardiac and vascular function in experimental septic shock. Crit Care Med. 2015; 43:e332–e340 [DOI] [PubMed] [Google Scholar]
- 125.Mathieu C, Desrois M, Kober F, et al. Sex-mediated response to the beta-blocker landiolol in sepsis: An experimental, randomized study. Crit Care Med. 2018; 46:e684–e691 [DOI] [PubMed] [Google Scholar]
- 126.Meibohm B, Beierle I, Derendorf H. How important are gender differences in pharmacokinetics? Clin Pharmacokinet. 2002; 41:329–342 [DOI] [PubMed] [Google Scholar]
- 127.Roberts JA, Abdul-Aziz MH, Lipman J, et al. ; International Society of Anti-Infective Pharmacology and the Pharmacokinetics and Pharmacodynamics Study Group of the European Society of Clinical Microbiology and Infectious Diseases. Individualised antibiotic dosing for patients who are critically ill: Challenges and potential solutions. Lancet Infect Dis. 2014; 14:498–509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Roberts JA, Roger C, De Waele JJ. Personalized antibiotic dosing for the critically ill. Intensive Care Med. 2019; 45:715–718 [DOI] [PubMed] [Google Scholar]
- 129.Rello J, van Engelen TSR, Alp E, et al. Towards precision medicine in sepsis: A position paper from the European Society of Clinical Microbiology and Infectious Diseases. Clin Microbiol Infect. 2018; 24:1264–1272 [DOI] [PubMed] [Google Scholar]
- 130.Best SA, Okada Y, Galbreath MM, et al. Age and sex differences in muscle sympathetic nerve activity in relation to haemodynamics, blood volume and left ventricular size. Exp Physiol. 2014; 99:839–848 [DOI] [PubMed] [Google Scholar]
- 131.Eijsvogels TM, Scholten RR, van Duijnhoven NT, et al. Sex difference in fluid balance responses during prolonged exercise. Scand J Med Sci Sports. 2013; 23:198–206 [DOI] [PubMed] [Google Scholar]
- 132.Shoemaker JK, Hogeman CS, Khan M, et al. Gender affects sympathetic and hemodynamic response to postural stress. Am J Physiol Heart Circ Physiol. 2001; 281:H2028–H2035 [DOI] [PubMed] [Google Scholar]
- 133.Fu Q, Arbab-Zadeh A, Perhonen MA, et al. Hemodynamics of orthostatic intolerance: Implications for gender differences. Am J Physiol Heart Circ Physiol. 2004; 286:H449–H457 [DOI] [PubMed] [Google Scholar]
- 134.Fu Q, Witkowski S, Okazaki K, et al. Effects of gender and hypovolemia on sympathetic neural responses to orthostatic stress. Am J Physiol Regul Integr Comp Physiol. 2005; 289:R109–R116 [DOI] [PubMed] [Google Scholar]
- 135.Hart EC, Charkoudian N, Wallin BG, et al. Sex differences in sympathetic neural-hemodynamic balance: Implications for human blood pressure regulation. Hypertension. 2009; 53:571–576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hogarth AJ, Mackintosh AF, Mary DA. Gender-related differences in the sympathetic vasoconstrictor drive of normal subjects. Clin Sci (Lond). 2007; 112:353–361 [DOI] [PubMed] [Google Scholar]
- 137.Nickander J, Themudo R, Sigfridsson A, et al. Females have higher myocardial perfusion, blood volume and extracellular volume compared to males - an adenosine stress cardiovascular magnetic resonance study. Sci Rep. 2020; 10:10380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Lawton JS, Cupps BP, Knutsen AK, et al. Magnetic resonance imaging detects significant sex differences in human myocardial strain. Biomed Eng Online. 2011; 10:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Rutkowski DR, Barton GP, François CJ, et al. Sex differences in cardiac flow dynamics of healthy volunteers. Radiol Cardiothorac Imaging. 2020; 2:e190058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Williams AM, Shave RE, Stembridge M, et al. Females have greater left ventricular twist mechanics than males during acute reductions to preload. Am J Physiol Heart Circ Physiol. 2016; 311:H76–H84 [DOI] [PubMed] [Google Scholar]
- 141.Coyle SM, Calvano SE, Lowry SF. Gender influences in vivo human responses to endotoxin. Shock. 2006; 26:538–543 [DOI] [PubMed] [Google Scholar]
- 142.Malbrain MLNG, Van Regenmortel N, Saugel B, et al. Principles of fluid management and stewardship in septic shock: It is time to consider the four D’s and the four phases of fluid therapy. Ann Intensive Care. 2018; 8:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Li Y, Li H, Zhang D. Timing of norepinephrine initiation in patients with septic shock: A systematic review and meta-analysis. Crit Care. 2020; 24:488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Macdonald SPJ, Keijzers G, Taylor DM, et al. ; REFRESH trial investigators. Restricted fluid resuscitation in suspected sepsis associated hypotension (REFRESH): A pilot randomised controlled trial. Intensive Care Med. 2018; 44:2070–2078 [DOI] [PubMed] [Google Scholar]
- 145.Hjortrup PB, Haase N, Bundgaard H, et al. ; CLASSIC Trial Group; Scandinavian Critical Care Trials Group. Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the CLASSIC randomised, parallel-group, multicentre feasibility trial. Intensive Care Med. 2016; 42:1695–1705 [DOI] [PubMed] [Google Scholar]
- 146.Cotroneo TM, Hugunin KM, Shuster KA, et al. Effects of buprenorphine on a cecal ligation and puncture model in C57BL/6 mice. J Am Assoc Lab Anim Sci. 2012; 51:357–365 [PMC free article] [PubMed] [Google Scholar]
- 147.Efron PA, Mohr AM, Moore FA, et al. The future of murine sepsis and trauma research models. J Leukoc Biol. 2015; 98:945–952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Gentile LF, Nacionales DC, Cuenca AG, et al. Identification and description of a novel murine model for polytrauma and shock. Crit Care Med. 2013; 41:1075–1085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Gentile LF, Nacionales DC, Lopez MC, et al. A better understanding of why murine models of trauma do not recapitulate the human syndrome. Crit Care Med. 2014; 42:1406–1413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Stephan RN, Kupper TS, Geha AS, et al. Hemorrhage without tissue trauma produces immunosuppression and enhances susceptibility to sepsis. Arch Surg. 1987; 122:62–68 [DOI] [PubMed] [Google Scholar]
- 151.Hellman J, Bahrami S, Boros M, et al. Part III: Minimum Quality Threshold in Preclinical Sepsis Studies (MQTiPSS) for fluid resuscitation and antimicrobial therapy endpoints. Shock. 2019; 51:33–43 [DOI] [PubMed] [Google Scholar]
- 152.Remick DG, Ayala A, Chaudry IH, et al. Premise for standardized sepsis models. Shock. 2019; 51:4–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Osuchowski MF, Ayala A, Bahrami S, et al. Minimum quality threshold in pre-clinical sepsis studies (MQTiPSS): An international expert consensus initiative for improvement of animal modeling in sepsis. Shock. 2018; 50:377–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Zingarelli B, Coopersmith CM, Drechsler S, et al. Part I: Minimum quality threshold in preclinical sepsis studies (MQTiPSS) for study design and humane modeling endpoints. Shock. 2019; 51:10–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Libert C, Ayala A, Bauer M, et al. Part II: Mnimum quality threshold in preclinical sepsis studies (MQTiPSS) for types of infections and organ dysfunction endpoints. Shock. 2019; 51:23–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


