Abstract
OBJECTIVES:
This article examines work-related and Personality personality factors that could influence health providers in experiencing alarm fatigue. The purpose of this study is to provide a basis to determine factors that may predict the potential of alarm fatigue in critical care staff.
DESIGN:
A questionnaire-based survey and an observational study were conducted to assess factors that could contribute to indicators of alarm fatigue.
INTERVENTIONS:
Factors included patient-to-staff ratio, criticality of the alarm, priority of different tasks, and personality traits.
SETTING:
The study was conducted at an eight-bed ICU in a mid-size hospital in Montana.
SUBJECTS:
Data were collected for six day shifts and six night shifts involving 24 critical care professionals. Within each 12-hour shift, six 15-minute intervals were randomly generated through work sampling for 6 days; a total of 1,080 observations were collected.
MEASUREMENTS:
Alarm fatigue was assessed with the subjective workload assessment technique and Boredom, Apathy, and Distrust Affects, which were measured through validated questionnaires. The Big Five Personality model was used to assess personality traits.
MAIN RESULTS:
Work factors including task prioritization, nurse-to-patient ratio, and length of shifts were associated with indicators of alarm fatigue. Personality traits of openness, conscientiousness, and neuroticism were also associated.
CONCLUSIONS:
We recommend assessing personality traits for critical care staff to be aware of how their individualities can affect their behavior towards alarm fatigue. We also recommend an examination of alternative strategies to reduce alarm fatigue, including examining the use of breaks, work rotation, or shift reduction.
Keywords: affects, alarm fatigue, critical care, personality type, subjective workload assessment technique
With the innovation of new technologies in healthcare systems, the number of clinical alarms has increased drastically (1). However, although these alarms may improve rapid responses to patient needs, they are not without problems. The frequency of nuisance or “nonactionable” alarms can lead to “sensory overload” and “desensitization” in caregivers, potentially making them unwilling to respond to real threats (2–8). Experts have defined this sensory overload and desensitization as alarm fatigue (AF) (6, 9).
Most accounts of AF in the literature describe the feeling of being “overwhelmed” and “desensitized” due to continuously beeping monitors enhanced by the high number of false alarms (9–17). The subjective workload assessment technique (SWAT) is an indicator of the overwhelming sensation caused by increased sound in the work environment (18–23).
Other researchers have incorporated Affect as an indicator of desensitization from tasks that involve alarm monitoring and decision-making (12, 24–26). Affect is defined as experiencing an emotion (27). Negative Affects that may influence the delivery of care related to AF include Boredom, Apathy, and Distrust (BAD) (18). Boredom is the difficulty concentrating or lack of interest in an activity due to low arousal, increased feelings of unpleasantness, and repetitiveness (18). Apathy is a state of the highest level of indifference and, therefore, leads to the suppression of concern or motivation (28). Distrust is the feeling of not being able to rely on or believe in something or someone (29). AF manifests in BAD Affect when nurses perceive the unpleasant alarms as repetitive and unreliable. This, in turn, may lead to a silencing of the alarms without attention to a potential underlying problem, resulting in the potential for errors or adverse patient outcomes.
Deb and Claudio (18) presented a conceptual model (Fig. 1) of the influence of AF on staff performance estimated by the number of ignored alarms and the time that took for nurses to respond to alarms that were not ignored. From Figure 1, it can be seen that they used SWAT to assess the overwhelming sensation nurses feel while BAD Affects indicate desensitization of the alarm. They found that “Staff Performance” was influenced by the presence of AF and the working conditions and personality traits (18).
Figure 1.
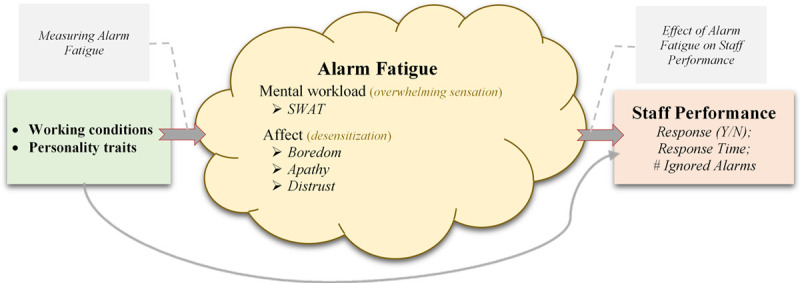
Conceptual model proposed by Deb and Claudio (18). SWAT = subjective workload assessment technique.
The perception of alarm utility and the emotional response to alarms may be linked to specific personality traits, as personality has been linked to information-processing, decision-making, stress management, and job performance (30). Therefore, we hypothesize that personality traits are a contributing factor in characterizing the response to AF. Understanding the contributing factors to AF may allow hospital administrators and nurse leaders to target interventions toward predicting and reducing AF in critical care (8, 31–37).
This research expands on previous work by looking at how different factors contribute to the proposed AF indicators. This study aims to examine how work-related factors and personality traits influence SWAT and BAD Affect on critical care staff, thus influencing the experience of AF.
MATERIALS AND METHODS
Approvals from the Montana State University Institutional Review Board (IRB; Federal Wide Assurance 00000165) and the hospital (through the university IRB) were obtained before the study (IRB number SD022614-EX).
Location and Participants
The facility was an eight-bed ICU in a mid-size hospital in Montana. The survey was distributed to all ICU employees, including unit clerks and nurses (n = 37). After assessing the general attitude regarding clinical alarms, an observational study was conducted. Data for 24 nurses (n = 18) and unit clerks (n = 6) who monitored unit alarms were collected during six dayshifts and six nightshifts. Informed consent was obtained from all participants. Participants’ identities were protected by assigning a unique identification number to each person.
Data Collection Methods
The study had two components: a standardized clinical alarm survey and an observational study. The clinical alarm survey was created by the Healthcare Technology Foundation and previously conducted nationwide with physicians (38, 39). The survey consists of two parts: demographic information on job title, years of experience, working unit, and working facility; and alarm-related information, such as how often nuisance alarms occur, how noisy the environment is, and if it is possible to differentiate the alarm sounds and identify the sources from among others. To investigate the variability between the responses, other information was asked of the ICU staff such as age, education, experience working in the ICU, and previous experience participating in this kind of alarm management study.
A paper-based survey was distributed to all ICU employees to assess staff attitude toward the facility’s existing alarm monitoring system. Seventeen out of thirty-seven ICU employees responded (response rate 46%). The responses were kept anonymous and aggregated.
Following the clinical alarm survey, an observational study involving 24 critical care professionals was then conducted to collect information on different factors that could lead to AF, based on a literature review (18). We divided the variables of interest into work-related factors, personality factors, and AF indicators/responses. The factors and responses considered in the study are presented in Table 1.
TABLE 1.
Factors and Responses Considered in This Study
| Type of Variable | Name of Variable |
|---|---|
| Work-related factors | Alarm criticality—high (1), medium (2), low (3) |
| Task priority (current task priority at the moment of alarm)—1 (highest priority) to 5 | |
| Patient-to-staff ratio | |
| Time elapsed (minutes since the start of the shift) | |
| Sound level (decibels) | |
| Personality factors | Extroversion |
| Conscientiousness | |
| Neuroticism | |
| Agreeableness | |
| Openness | |
| Alarm fatigue indicators (responses) | Subjective Workload Assessment Technique (overwhelming sensation) |
| Affect (desensitization): Boredom, Apathy, Distrust |
Within each 12-hour shift, six 15-minute intervals were randomly generated through work sampling (18) for 6 days, and data were collected continuously by two investigators. A total of 1,080 observations were collected. A data collection sheet was created to simplify the data collection process. During the 15-minute intervals, investigators noted new alarms and write down the room number, time alarm went off, and time it took staff to respond to the alarm (if there was a response). They noted the type of alarm, alarm criticality (according to instructions given to us by nurses), whether the alarm was actionable or nonactionable, and what the staff accountable for an alarm was doing at that moment. Following each shift, participants sat down with the observers and told them if the task they were performing at a particular time had higher priority (or could not be interrupted) than the alarm.
Measuring SWAT, BAD Affect, and Personality
The SWAT is a validated, reliable, and widely used multidimensional survey tool to measure perceived mental workload (40). It contains three dimensions: time load, mental effort load, and psychologic stress load. Each dimension is assessed at three discrete levels: low, medium, and high. These levels were later converted into numerical representations, with 1 being low and 3 being high. ICU staff was trained on survey measures at the beginning of the shift. The questions were then administered three times per staff present in the shift, during a pause in their patient care or alarm monitoring activity. The survey was administered orally by asking questions while ensuring no disruption inpatient care.
BAD Affects were estimated using validated questionnaires (18). The Boredom Proneness Scale (BPS) assesses Boredom in relation to individuals’ connectedness with the environment and willingness to access adaptive resources and recognize urgencies (18). It contains 10 questions with five potential answers for each question (Strongly Disagree, Disagree, Neutral, Agree, or Strongly Agree). BPS was administered at the end of the shift.
The Apathy Evaluation Scale (18) was applied to assess Apathy among staff. A validated short version with 10 items was used for this research to measure staff apathy by means of a retrospective survey after each observational shift. Each question had four potential answers for each question (Strongly Disagree, Neutral, Agree, or Strongly Agree). Like the BPS, it was administered at the end of the shift.
Our review of the literature did not give any established and valid tool to measure Distrust for the hospital staff during their alarm monitoring tasks. Therefore, we created a survey tool to measure staff Distrust toward alarms that contained three questions. The first two questions were created based on an Intercultural Scale to measure trust in automation (18). A third question was added on expert opinion. The three questions were assessed at three levels (Yes, I don’t know, or No). The questions were validated by two registered nurses, two unit clerks, and the ICU manager. Responses to the Distrust scale were collected with the SWAT questions as participants carried out their tasks during the shift.
The Big Five Personality Questionnaire was used to assess personality traits of nurses and unit clerks (18). This validated test divides personalities along five dichotomies: Extraversion versus Introversion, Openness versus Closedness to Experience, Agreeableness versus Hostility, Conscientiousness versus Lack of Conscientiousness, and Emotional Stability versus Neuroticism.
Participants were emailed a link to the survey, which uses a series of questions to determine personality type. Each participant sent a link of his/her personality test result back to the researchers. The personality-type dimensions were documented for each participant using a unique identification number.
Statistical Analysis
Linear regression and analysis of variance analyses (40) were conducted. Multivariate Adaptive Regression Splines identified significant factors and their importance by assigning importance scores to each variable. Importance scores were calculated on a 100% scale such that the most important variable always gets a 100% score. This score represents the increase in the model-generalized cross-validation when including a variable either by itself or as part of an interacting group (40).
RESULTS
Results from the clinical alarm survey are presented in Table 2. Most respondents (greater than 84%; statement 3) agreed or strongly agreed with the statements divulging the purpose of clinical alarms and the necessity for prioritized and easily differentiated audible and visual alarms. Likewise, a large percentage of respondents confirmed the occurrence of frequent nuisance alarms (84.6%; statement 5), which disrupt patient care (84.6%; statement 6) and reduce trust in alarms causing caregivers to disable alarms (53.8%, neutral: 46.2%; statement 7).
TABLE 2.
Responses in Percentages to Clinical Alarm Survey
| Statements | Agree or Strongly Agree | Neutral | Disagree or Strongly Disagree |
|---|---|---|---|
| 1) The purpose of clinical alarms is to alert staff of hazardous patient condition | 100.0% | — | — |
| 2) Alarm sounds and/or visual displays should differentiate alarm priority | 100.0% | — | — |
| 3) Alarm sounds and/or visual displays should be distinct based on source | 84.6% | 15.4% | — |
| 4) Alarms should affect multiple senses (audible, visual, proprioceptive, etc.) | 92.3% | 7.7% | — |
| 5) Nuisance alarms occur frequently | 84.6% | 7.7% | 7.7% |
| 6) Nuisance alarms disrupt patient care | 84.6% | 15.4% | — |
| 7) Nuisance alarms reduce trust in alarms and cause caregivers to turn them off | 53.8% | 46.2% | — |
| 8) The alarms used on my floor/area are adequate to alert staff | 69.2% | 15.4% | 15.4% |
| 9) There have been frequent instances where alarms could not be heard | 53.8% | 7.7% | 38.5% |
| 10) The staff is sensitive to alarms and responds quickly | 30.8% | 23% | 46.2% |
| 11) It can be confusing to determine which device is in alarm | 46.2% | 15.3% | 38.5% |
| 12) A central alarm management staff is helpful | 46.2% | 7.7% | 23.1% |
| 13) Alarm integration and communication systems via wireless devices (e.g., pager and cell phone) are useful in improving alarm management and response | 23.1% | 53.8% | 23.1% |
| 14) Smart alarms would be effective in reducing false alarms and improving response | 84.6% | 15.4% | — |
| 15) Policies and procedures exist within the facility to regulate alarms, and they are followed | 23.1% | 30.7% | 46.2% |
| 16) There is a requirement in your institution to document that the alarms are set and are appropriate for each patient | 30.8% | 23% | 46.2% |
Many of the staff agreed that smart alarms could help minimize some of these nuisance alarms (84.6%; statement 14) and that a central alarm management system could be useful (69.2%; statement 12). Responses were divergent on the statements about the complexity of hearing, recognizing alarms, and responding to alarms. Differing opinions were also observed on the questions concerning integrating alarm information with communications systems (e.g., pagers and cell phones), improving policies and procedures to regulate alarms properly, and developing patient-specific alarm settings. This divergence may indicate that the technology surrounding alarm monitoring systems requires training and experience to master.
The regression analyses revealed effective models for the AF indicators, as presented in Figure 2. The adjusted coefficients of determination values confirm significant associations between work-related and personality factors and the SWAT and BAD affect indicators. The models suggest that nearly the same common work-related and personality factors explain most of the variance in SWAT and BAD Affect.
Figure 2.
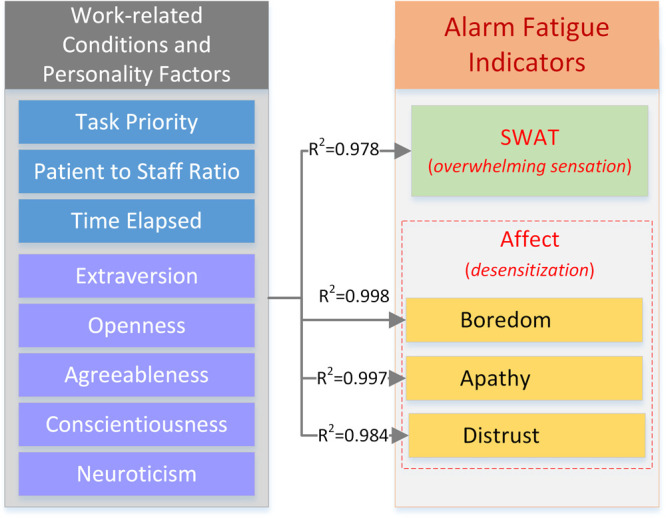
Association of significant work-related and personality factors with subjective workload assessment technique and Boredom, Apathy, and Distrust (BAD) Affect.
Table 3 lists only the significant factors, with importance scoring higher than 10.00%, for SWAT and BAD Affect. A factor with 100% represents the most important factor for a specific response. The other percentages represent importance relative to the most important factor. For example, a 50% importance means a factor’s importance is only half of the importance compared with the most important.
TABLE 3.
Summary of Influencing Factors With Importance Scoring Higher Than 10.00% According to Multivariate Adaptive Regression Splines
| Factor | Subjective Workload Assessment Technique | Boredom | Apathy | Distrust |
|---|---|---|---|---|
| Neuroticism | 100 | 45.41 | 29.10 | — |
| Agreeableness | 47.56 | 100 | 65.42 | 39.74 |
| Conscientiousness | — | — | 100 | 40.90 |
| Patient-to-staff ratio | 60.84 | 98.64 | 75.43 | 100 |
| Task priority | 11.66 | — | — | — |
| Time elapsed | 34.19 | 30.00 | 31.57 | 61.16 |
| Extroversion | 23.92 | 45.42 | 50.20 | — |
| Openness | — | 14.82 | — | 66.70 |
Statistically significant factors influencing SWAT include work-related factors: patient-to-staff ratio, time elapsed since the beginning of the shift, and task priority; personality factors include neuroticism, agreeableness, and extroversion.
Boredom also includes patient-to-staff ratio, time elapsed, and four personality factors (neuroticism, agreeableness, extroversion, and openness). Similarly, Apathy is associated with two work-related factors (patient-to-staff ratio and time elapsed) and four personality factors (neuroticism, agreeableness, conscientiousness, and extroversion). Finally, Distrust is associated with the common two work-related factors and three personality factors (agreeableness, conscientiousness, and openness).
Table 4 displays the positive or negative influence of the significant factors on each AF indicator. The results show some factors have a directly proportional influence on SWAT and the BAD indicators, whereas others may have an inversely proportional influence.
TABLE 4.
Effect of Factors on the Alarm Fatigue Indicators
| Work-Related and Personality Factors | Alarm Fatigue Indicators | |||
|---|---|---|---|---|
| Subjective Workload Assessment Technique | Boredom | Apathy | Distrust | |
| Task priority | – | |||
| Time elapsed | + | – | – | – |
| Patient-to-staff ratio | – | – | + | + |
| Extroversion | – | + | – | |
| Conscientiousness | – | – | ||
| Neuroticism | + | – | + | |
| Agreeableness | + | + | + | + |
| Openness | – | – | ||
+ indicates directly proportional influence.
– indicates inversely proportional influence.
Empty cells represent no association.
Task priority had a negative influence on SWAT and no influence on BAD Affect. Positive influences of work-related factors were noted for time elapsed on SWAT and staffing ratios on Apathy. Positive influences of personality factors were noted for Extroversion and Boredom, Neuroticism and SWAT and Apathy, and Agreeableness on all indicators. Openness did not have a positive influence on any indicator.
DISCUSSION
Perceptions of Alarms
Staff responses to alarms elucidate the role of the alarms in the work shift. Alarms that are perceived as nuisances are likely to be turned off, thus rendering them useless as alerts to patient situations. Perhaps this explains why so many in our sample disagreed with the statement that the staff is sensitive to alarms. AF can result in nurses silencing alarms perceived as nuisances and may explain some of the apparent negative responses in the survey. This may also explain the high level of agreement with the statement that nuisance alarms disrupt patient care.
Although alarms are designed to interrupt a nurse’s activity, the overwhelming presence of nuisance alarms may render them completely irrelevant in getting the nurse’s attention. The finding that nearly 70% agreed with the statement that a central alarm management system could be useful suggests that nursing managers who invest in a central monitoring system may reduce AF in floor nurses and improve the efficacy of alarms in general.
Work-Related Factors Influencing AF
Our analysis revealed three work-related factors that contribute to indicators of AF. Task Priority suggests that an interruption during a high-priority task creates higher levels of AF as measured by the SWAT tool. Ideally, an alarm alerts the nurse to a need to reprioritize tasks and address the most critical situations first. During a high-priority situation, the nurse experiences increased mental workload when another alarm sounds. A nuisance alarm that does not directly influence the task at hand—or worse indicates a low-priority concern—creates a distraction and may negatively impact the nurse’s ability to prioritize and is likely to increase AF.
AF was also affected by the time of the alarm in relation to the start of the shift—nurses who were later in their shifts experienced increased indicators of AF with sounding alarms. Awareness of the timing of AF in a shift is important to decrease adverse effects and may be useful in decisions related to shift length or could suggest a need for rotation alarm monitoring duties. Critical care staff who have responded to alarms for a longer period of time would be expected to experience higher levels of AF.
Surprisingly, we found a decrease in the measurement of BAD Affect as the shift continued. We expected BAD to increase as AF set in. However, nurses may adapt to the alarm settings and be able to identify which ones require priority, thus decreasing the potential for BAD Affect. Interestingly, this did not seem to affect indicators of AF.
A final work-related factor associated with indicators of AF is the patient-to-staff ratio, representing the nurse’s workload. To our surprise, critical care professionals saw a decrease in their perception of workload with an increased patient-to-staff ratio, which would suggest a decrease in AF. In other words, with more patients, nurses felt less overwhelmed by the alarms. This is opposite to what was reported by Weinger and Smith (41). However, this may speak to the ability of the critical care nurse to more acutely focus attention on high-priority tasks and ignore nuisance alarms. Increased patient care inevitably results in an increase in the number of alarms, including nuisance alarms. It is conceivable that as the alarms increased, nurses narrowed their focus on current tasks and tuned out nuisance alarms.
Personality Factors Influencing AF
Three personality traits emerged as influencing AF. Neuroticism describes a person’s moodiness and emotional stability. A higher level of neuroticism represents higher susceptibility to anxiety, irritability, and sadness (42). Critical alarms are designed to increase anxiety; it is not surprising that those with a higher neuroticism score experienced increased indicators of AF. The allostatic load induced by an alarm may increase the nurse’s priority level to each alarm and may induce increased fatigue at the need to process each new alert.
A second personality trait is conscientiousness, representing the tendency to be organized and dependable (42). Individuals with a high level of consciousness tend to have good impulse control and goal-directed behaviors. Conscientiousness had a negative association with Apathy and Distrust; participants with a higher consciousness score reported lower levels of Apathy and Distrust. Those who are able to plan and organize may effectively create a goal-oriented routine that reduces the desensitization feeling. This, in turn, results in decreased AF, because the nurse feels organized in prioritizing care needs. Additionally, a dependable personality may be well-practiced in responding to emerging and changing patient needs, which are signaled by alarms. A conscientious nurse, then, may not view the alarms as quite the intrusion as a less conscientious nurse.
Finally, nurses categorized with agreeableness had higher scores on indications of AF. Agreeableness refers to trust and empathy for other people. High levels of agreeableness represent more cooperation with people and systems, whereas low levels represent more competitiveness (42). Nurses who have more empathy for patients might want to make sure they respond to most alarms or check (even if from a distance) that a patient is safe. This constant responsiveness requires remembering and prioritizing multiple pieces of information simultaneously and may increase the psychologic stress of responding to alarms.
Those who were identified as extroverted on the Big Five survey had lower levels of AF and Apathy but experienced higher levels of Boredom. Extroversion is associated with qualities that may potentially influence AF. For example, extroverts may pay more attention to their external environment than introverts. Because alarms are a part of the external environment, extroverts may display a baseline comfort level with alarms that may not be present in introverts. People with a high percentile for extroversion tend to be more proactive (43). Extroversion includes traits such as assertiveness and an increased level of activity (42, 44). These traits may help mitigate AF, because the extrovert is quick to assert control over an alarm and quickly estimates the Task Priority.
People with a high percentile of openness prefer variety are intellectually curious and exhibit independence of judgment (42). Openness did not influence SWAT or Apathy for critical care staff but negatively affected Boredom and Distrust: higher levels of openness resulted in lower levels of Boredom and Distrust. Those with high levels of openness may be curious about the source of an alarm may prefer the variety offered by the interruptions of audible alarms.
CONCLUSIONS
This in-depth analysis of the association between different factors and AF indicators reveals the influence of work-related and personality factors.
The concept of how to mitigate AF beyond the conventional wisdom of minimizing nuisance alarms and alarm individualization to a particular patient is an important one and one that deserves more attention. Our main hypothesis was that work-related stressors and personality traits were contributing factors to developing AF. We identified ways nurse managers might use these factors as they plan nursing care and nursing shifts. Based on definitions of the Big Five personality traits, the ideal personality to work in critical care settings with numerous audible alarms would be an individual with lower susceptibility to anxiety, higher levels of competitiveness, assertiveness, and proactiveness, with good impulse control, goal-directed behaviors, and high intellectual curiosity with high independence of judgment.
Attention to the length of work shifts, task priority, and nurse-to-patient ratios may help reduce AF in critical care nurses. Kubiszyn et al (45) suggested the benefit of cognitive and personality tests in predicting behaviors in critical workplace settings. Likewise, we recommend using personality assessments on critical care nurses as a tool for implementing strategies to reduce AF.
A limitation of this study is the low sample size. Although we used 24 critical care staff and collected 1,080 observations, the results are limited to these 24 professionals. Future research should focus on conducting a balanced experiment in a controlled setting. This would require recruiting the exact number of participants with different combinations of personality traits and manipulating the work environment (audible alarms, tasks, and time elapsed) to measure SWAT and BAD Affect. It will be crucial to also investigate ways to reduce critical care professionals’ anxiety and irritability in this environment.
Footnotes
Supported, in part, by Bozeman Deaconess Hospital (they prefer to remain anonymous).
The authors have disclosed that they do not have any potential conflicts of interest.
This work was performed at Bozeman Deaconess Hospital and Montana State University.
REFERENCES
- 1.Borowski M, Görges M, Fried R, et al. : Medical device alarms. Biomed Tech (Berl). 2011; 56:73–83 [DOI] [PubMed] [Google Scholar]
- 2.Simpson KR, Lyndon A: False alarms and overmonitoring: Major factors in alarm fatigue among labor nurses. J Nurs Care Qual. 2019; 34:66–72 [DOI] [PubMed] [Google Scholar]
- 3.Sowan AK, Vera AG, Fonseca EI, et al. : Nurse competence on physiologic monitors use: Toward eliminating alarm fatigue in intensive care units. Open Med Inform J. 2017; 11:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li SYW, Tse MK, Brecknell B, et al. : Spearcon sequences for monitoring multiple patients: Laboratory investigation comparing two auditory display designs. Hum Factors. 2019; 61:288–304 [DOI] [PubMed] [Google Scholar]
- 5.Alsaad AA, Alman CR, Thompson KM, et al. : A multidisciplinary approach to reducing alarm fatigue and cost through appropriate use of cardiac telemetry. Postgrad Med J. 2017; 93:430–435 [DOI] [PubMed] [Google Scholar]
- 6.Mitka M: Joint commission warns of alarm fatigue: Multitude of alarms from monitoring devices problematic. JAMA. 2013; 309:2315–2316 [DOI] [PubMed] [Google Scholar]
- 7.Paine CW, Goel VV, Ely E, et al. : Systematic review of physiologic monitor alarm characteristics and pragmatic interventions to reduce alarm frequency. J Hosp Med. 2016; 11:136–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hravnak M, Pellathy T, Chen L, et al. : A call to alarms: Current state and future directions in the battle against alarm fatigue. J Electrocardiol. 2018; 51:S44–S48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sendelbach S, Funk M: Alarm fatigue: A patient safety concern. AACN Adv Crit Care. 2013; 24:378–386 [DOI] [PubMed] [Google Scholar]
- 10.Cvach M: Monitor alarm fatigue: An integrative review. Biomed Instrum Technol. 2012; 46:268–277 [DOI] [PubMed] [Google Scholar]
- 11.Torabizadeh C, Yousefinya A, Zand F, et al. : A nurses’ alarm fatigue questionnaire: Development and psychometric properties. J Clin Monit Comput. 2017; 31:1305–1312 [DOI] [PubMed] [Google Scholar]
- 12.Turmell JW, Coke L, Catinella R, et al. : Alarm fatigue: Use of an evidence-based alarm management strategy. J Nurs Care Qual. 2017; 32:47–54 [DOI] [PubMed] [Google Scholar]
- 13.Oliveira AEC, Machado AB, Santos EDD, et al. : Alarm fatigue and the implications for patient safety. Rev Bras Enferm. 2018; 71:3035–3040 [DOI] [PubMed] [Google Scholar]
- 14.Ketko AK, Martin CM, Nemshak MA, et al. : Balancing the tension between hyperoxia prevention and alarm fatigue in the NICU. Pediatrics. 2015; 136:e496–e504 [DOI] [PubMed] [Google Scholar]
- 15.Pishori T: A Stochastic Simulation Model of Alarm Response Strategies on a Telemetry Floor. 2012. Available at: http://digitalcommons.uconn.edu/gs_theses/256/. Accessed May 1, 2019
- 16.Baillargeon E: Alarm Fatigue: A Risk Assessment. 2013. Available at: https://digitalcommons.ric.edu/etd/216/. Accessed May 1, 2019
- 17.Hussain M, Dewey J, Weibel N: Reducing alarm fatigue: Exploring decision structures, risks, and design. EAI Endorsed Trans Pervasive Health Technol. 2017; 3:1–14 [Google Scholar]
- 18.Deb S, Claudio D: Alarm fatigue and its influence on staff performance. IIE Trans Healthcare Syst Eng. 2015; 5:183–196 [Google Scholar]
- 19.McNeer RR, Bennett CL, Dudaryk R: Intraoperative noise increases perceived task load and fatigue in anesthesiology residents: A simulation-based study. Anesth Analg. 2016; 122:512–525 [DOI] [PubMed] [Google Scholar]
- 20.Shah SJ: Effects of Visibility and Alarm Modality on Workload, Trust in Automation, Situation Awareness, and Driver Performance. 2016. Available at: https://digitalcommons.odu.edu/cgi/viewcontent.cgi?article=1035&context=psychology_etds. Accessed May 1, 2019
- 21.Sato H, Miyashita T, Kawakami H, et al. : Influence of mental workload on the performance of anesthesiologists during induction of general anesthesia: A patient simulator study. BioMed Res Int. 2016; 2016:1058750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Edworthy J, Reid S, Peel K, et al. : The impact of workload on the ability to localize audible alarms. Appl Ergon. 2018; 72:88–93 [DOI] [PubMed] [Google Scholar]
- 23.Dehais F, Roy RN, Scannella S: Inattentional deafness to auditory alarms: Inter-individual differences, electrophysiological signature and single trial classification. Behav Brain Res. 2019; 360:51–59 [DOI] [PubMed] [Google Scholar]
- 24.Thomas LC, Gast C, Grube R, et al. : Fatigue detection in commercial flight operations: Results using physiological measures. Proc Manuf. 2015; 3:2357–2364 [Google Scholar]
- 25.Löffler A: Worth the Effort? Measuring Component Processes of Effort-Based Decision Making in Lesion Patients. 2015. 2015. Available at: https://escholarship.mcgill.ca/concern/theses/jd473027p. Accessed April 1, 2018
- 26.Hunter A, Eastwood JD: Does state boredom cause failures of attention? Examining the relations between trait boredom, state boredom, and sustained attention. Exp Brain Res. 2018; 236:2483–2492 [DOI] [PubMed] [Google Scholar]
- 27.Hogg MA, Abrams D, Martin GN: Social condition and attitudes. : Psychology. Fifth Edition. Martin GN, Carlson NR, Buskist W. (Eds). Harlow, United Kingdom, Pearson Education Limited, 2013, pp 684–721 [Google Scholar]
- 28.Godefroy O: The Behavioral and Cognitive Neurology of Stroke. Second Edition. New York, Cambridge UniversityPress, 2013 [Google Scholar]
- 29.Harrison DM, Chervany NL: Trust and distrust definitions: One bite at a time. : Trust in Cyber-Societies. Falcone R, Singh M, Tan Y-H. (Eds). Berlin, Germany, Springer, 2001, pp 27–54 [Google Scholar]
- 30.Franklin C, Johnson LV, White L, et al. : The relationship between personality type and acceptable noise levels: A pilot study. ISRN Otolaryngol. 2013; 2013:902532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Casey S, Avalos G, Dowling M: Critical care nurses’ knowledge of alarm fatigue and practices towards alarms: A multicentre study. Intensive Crit Care Nurs. 2018; 48:36–41 [DOI] [PubMed] [Google Scholar]
- 32.Sowan AK, Gomez TM, Tarriela AF, et al. : Changes in default alarm settings and standard in-service are insufficient to improve alarm fatigue in an intensive care unit: A pilot project. JMIR Hum Factors. 2016; 3:1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Solet JM, Barach PR: Managing alarm fatigue in cardiac care. Prog Pediatr Cardiol. 2012; 33:85–90 [Google Scholar]
- 34.Purbaugh T: Alarm fatigue a roadmap for mitigating the cacophony of beeps. Clin Dimension. 2014; 33:4–7 [DOI] [PubMed] [Google Scholar]
- 35.Venella J: Drawing up a new game plan to reduce alarm fatigue. Biomed Instrum Technol. 2017; 51:71–72 [DOI] [PubMed] [Google Scholar]
- 36.Kane-Gill SL, O’Connor MF, Rothschild JM, et al. : Technologic distractions (part 1): Summary of approaches to manage alert quantity with intent to reduce alert fatigue and suggestions for alert fatigue metrics. Crit Care Med. 2017; 45:1481–1488 [DOI] [PubMed] [Google Scholar]
- 37.Winters BD, Cvach MM, Bonafide CP, et al. ; Society for Critical Care Medicine Alarm and Alert Fatigue Task Force: Technological distractions (part 2): A summary of approaches to manage clinical alarms with intent to reduce alarm fatigue. Crit Care Med. 2018; 46:130–137 [DOI] [PubMed] [Google Scholar]
- 38.Clark T, David Y, Baretich M, et al. : Impact of Clinical Alarms on Patient Safety. HTF 2006. Available at: http://www.thehtf.org/documents/White%20Paper.pdf. Accessed March 18, 2014
- 39.Clinical Alarm Task Force: Impact of clinical alarms on patient safety: A report from the American College of Clinical Engineering Healthcare Technology Foundation. J Clin Eng. 2007; 32:22–33 [Google Scholar]
- 40.Huggins A, Claudio D: A performance comparison between the subjective workload analysis technique and the NASA-TLX in a healthcare setting. IISE Trans Healthcare Syst Eng. 2018; 8:59–71 [Google Scholar]
- 41.Weinger MB, Smith NT: Vigilance, alarms and integrated monitoring systems. : Anesthesia Equipment: Principles and Applications. Malvern, PA, Mosby, 1993, pp 350–384 [Google Scholar]
- 42.Power RA, Pluess M: Heritability estimates of the Big Five personality traits based on common genetic variants. Transl Psychiatry. 2015; 5:e604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang Y, Ang C, Jiang Z, et al. The role of trait extraversion in shaping proactive behavior: A multilevel examination of the impact of high-activated positive affect. Personal Indiv Diff. 2019; 136:107–112 [Google Scholar]
- 44.Harari MB, Thompson AH, Viswesvaran C: Extraversion and job satisfaction: The role of trait bandwidth and the moderating effect of status goal attainment. Personal Indiv Diff. 2018; 136:107–112 [Google Scholar]
- 45.Kubiszyn TW, Meyer GJ, Finn SE, et al. : Empirical support for psychological assessment in clinical health care settings. Prof Psychol Res Pract. 2000; 31:119 [Google Scholar]


