INTRODUCTION
The goals of gender-affirming masculinizing mastectomy are to remove the breast and create a natural, symmetric chest contour that matches the patient’s body habitus.1 Periareolar incisions minimize scarring but are limited to thin patients with small breasts and associated with high revision rates.2–7 In contrast, inframammary incisions allow the surgeon to more accurately tailor the chest contour, remove excess skin, and resize and reposition the nipple.8–11 Scar placement along the inferior border of the pectoralis major muscle (PMM) helps camouflage the scars, but creating symmetric, inconspicuous scars can be the most challenging aspect of gender-affirming masculinizing mastectomy.10
Variations in breast characteristics include size, baseline asymmetry, ptosis, nipple-areolar complex and inframammary fold (IMF) positions, and amount of lateral breast tissue.8–11 Thus, the amount of breast and skin excised can vary by side, but the goal is to achieve symmetrical scars. One method for achieving symmetrical chest contour and scars is intraoperative tailor tacking.12 This may require repeated trials to achieve the desired result and is often difficult to teach, as is a surgeon’s artistic skill and judgment. An analytical and methodical approach would facilitate teaching and achieve desired aesthetic outcomes in an area of anatomic variability.
We present our novel marking technique of inframammary mastectomy with free nipple grafting (IMFNG), which achieves a symmetric masculine-appearing chest with minimal intraoperative tailoring and revision.
TECHNIQUE
This study was approved by the UCSF Institutional Review Board, and informed consent was obtained for all patients depicted.
Preoperative Marking
In the preoperative area, the IMFs are marked, and PMM identified and marked by palpating along and above the IMF while lifting the breast and asking the patient to flex. (See Video 1 [online], which displays the surgeon marking ptotic breasts in the preoperative area. It is important to mark the native IMF and the inferior border of the PMM, where the final scar will be.) (See Video 2 [online], which displays the surgeon marking asymmetric breasts in the preoperative area. For both sides, it is important to mark the native IMF and the inferior border of the PMM, where the final scar will be.)
Video 1. Marking ptotic breasts. Video 1 from “A Technique for Optimizing Symmetry in Gender-Affirming Mastectomy“.
Video 2. Marking asymmetric breasts. Video 2 from “A Technique for Optimizing Symmetry in Gender-Affirming Mastectomy”.
The goal is to place the final scar along the inferior border of the PMM. This new IMF, which is often 1–2 cm above the native IMF, is marked and then transposed to the anterior surface of the breast. The markings are replicated on the contralateral side to achieve symmetry.
In the operating room, the patient is positioned supine on a hinged table. To create a gentle curve to the final scar along PMM insertion, the senior author had been using tailor tacking but found this method tedious and difficult to teach. To develop a reproducible marking method, she measured these tailor tackings from the midline and found the curvatures and dimensions were similar in most patients. Using these measurements, she developed the current technique that relies on the new IMF and the sternum as landmarks for symmetrical, reliable scar positions.
Intraoperative Marking
The new IMF that is marked preoperatively is confirmed and extended to the midline as a long horizontal line (LHL). Three horizontal lines are drawn 1 cm apart superiorly from the LHL. Moving superiorly to inferiorly, the length of each line is 3 cm, 5 cm, and 7 cm centered at the sternal midline. (See Video 3 [online], which displays the detailed intraoperative markings that are made by the surgeon. The markings over the midline are designed to minimize intraoperative tailor tacking.)
Video 3. Intraoperative markings. Video 3 from “A Technique for Optimizing Symmetry in Gender-Affirming Mastectomy”.
The ends of these lines are then connected in a trapezoidal shape to intersect with the LHL. The superior line that was marked preoperatively by transposing the new IMF onto the anterior surface of the breast is connected to the top-most corner of the trapezoid (Fig. 1A). This intersection point can be adjusted anywhere along the trapezoidal “curve,” depending on breast size and amount of skin requiring resection (Fig. 1B). The senior author extends the lateral incision aiming toward the posterior axillary line in a gentle curve to remove lateral skin and soft tissue. To achieve symmetric lateral curvature, the senior author draws a triangle composed of the LHL (base), height, and the extended native IMF line (hypotenuse). She measures these limbs and transposes them to the contralateral side.
Fig. 1.
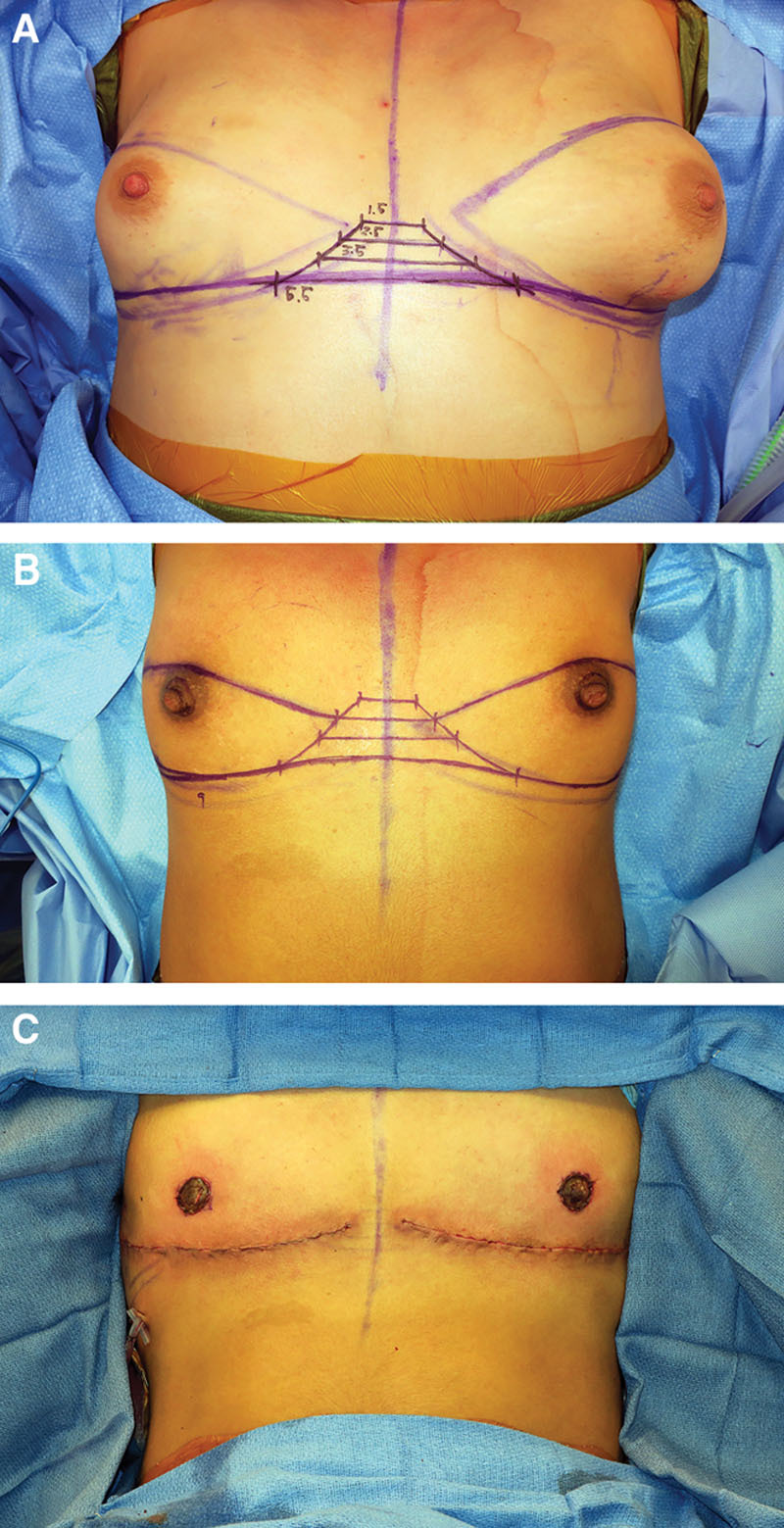
Photographs of intraoperative markings on patients with different breast and chest sizes. A, Markings showing the superior incision connecting to the top-most corner, at the 1.5 cm mark. B, Markings showing the superior incision connecting along the trapezoidal curve. C, Final reconstruction after nipple resizing and repositioning and closure.
Surgical Procedure
Next, the mastectomy and reconstruction are performed. (See Video 4 [online], which displays the mastectomy, reconstruction, and nipple graft inset after the markings are finalized.)
Video 4. Full surgery. Video 4 from “A Technique for Optimizing Symmetry in Gender-Affirming Mastectomy”.
The nipple-areolar complex is harvested as a full-thickness skin graft with a 2-cm diameter, the inferior incision is made, and the breast is dissected in the prepectoral plane. For smaller breasts, this dissection is carried to the clavicle to ensure the least amount of tension on the closure. The breast is then amputated and contoured to resemble a male chest and match the patient’s body. To ensure better medial chest definition, the medial flap is thinned, and the native IMF is obliterated by excision of the residual breast parenchyma at the level of the IMF. Excising this residual tissue removes the shadow under the final scar, achieving superior chest aesthetics. All excised breast tissue is sent to pathology.
With the patient seated, the incision is temporarily closed with staples to check for symmetry, and nipple positions are marked over the inferior, lateral portion of the chest. The incisions are closed in layers over a drain to prevent seroma formation and nipple grafts are inset (Fig. 1C). A nipple bolster is used to avoid scarring of the normal chest skin around the nipple (See Video 4 [online], which displays the mastectomy, reconstruction, and nipple graft inset after the markings are finalized): the nipple is covered with Xeroform, gauze, and a Tegaderm, and air is vacuumed out with a needle to create negative pressure. The chest is wrapped in ACE bandages for additional compression. All patients receive a preoperative dose of antibiotics, and no postoperative antibiotics are prescribed.
Postoperative Care
The patient is seen in clinic at 1, 2, and 6 week intervals. The drains are removed, and the nipple bolster dressings are changed at the first postoperative visit. The ACE bandages are also replaced for an additional week. At the 2-week visit, the patient is instructed to place a petroleum-based ointment on their nipple grafts covered by a non-adherent dressing for 3-4 weeks until healed. No additional chest compression is required, and scar care with silicone tape is recommended.
RESULTS
Of the 105 patients who underwent IMFNG using this technique, 72% identified as trans-men and 25% as gender queer, nonbinary, or agender. All patients met the World Professional Association for Transgender Health criteria for surgery. The median age was 24 years, mean BMI was 27.6 (95% CI 27–29), 80% were on hormone therapy at the time of surgery, and 97% reported binding their chests to hide the appearance of their breasts. Most patients (90%) had medium-to-large breasts and Grade II or Grade III ptosis (61%) (Table 1).
Table 1.
Preoperative Characteristics of 105 Patients Who Underwent Inframammary Mastectomy with Free Nipple Grafting
| Age, y, median (IQR) | 24 (20–30) |
| BMI (kg/m2), mean (95% CI) | 27.6 (27–29) |
| Breast size, N (%) | |
| Small | 11 (10%) |
| Medium | 62 (59%) |
| Large | 30 (29%) |
| Missing | 2 (2%) |
| Breast ptosis, N (%) | |
| None | 33 (31%) |
| Grade I | 5 (5%) |
| Grade II | 27 (26%) |
| Grade III | 32 (30%) |
| Pseudoptosis | 1 (1%) |
| Missing | 7 (7%) |
| Skin Elasticity, N (%) | |
| Poor | 11 (10%) |
| Moderate | 38 (36%) |
| Good | 52 (50%) |
| Missing | 4 (4%) |
IQR, interquartile range; BMI, body mass index; CI, confidence interval.
Every procedure was performed with one assisting trainee (PGY 2–PGY 6). Average operative time was 175 minutes (95% CI 165–185 minutes). Mean follow-up time was 13 weeks. The most common complications were hypertrophic scarring (17%) and nipple hypopigmentation (20%). Four patients (4%) required an unplanned reoperation to evacuate a hematoma (Table 2).
Table 2.
Surgical Characteristics and Postoperative Complications after IMFNG in 105 Patients
| Surgical Characteristic | Mean (95% CI) |
|---|---|
| Length of surgery | 175 (165–185) min |
| Breast tissue removed | 552 (462–642) g |
| Estimated blood loss | 59 (53–64) mL |
| Length of follow-up | 13 (11–16) weeks |
| Complication | N (%) |
| Hematoma | 7 (7%) |
| Infection | 6 (6%) |
| Seroma | 10 (10%) |
| Hypertrophic scarring | 17 (17%) |
| Nipple loss (partial or complete) | 0 (0%) |
| Nipple hypopigmentation | 20 (20%) |
| Minor contour deformity/asymmetry | 12 (12%) |
| Triamcinolone injection | 4 (4%) |
| Nipple tattoo | 0 (0%) |
| Revision surgery | 1 (1%) |
DISCUSSION
A reproducible, objective technique for obtaining symmetric chest scars is one of the challenges with IMFNG. To obtain symmetric scars, our calculated marking technique relies less on artistic assessments, making it easier to teach to trainees. Most hypertrophic scarring was asymptomatic and mild, which did not require intervention. Nipple hypopigmentation noted early in follow-up is expected to resolve and can be corrected with nipple tattoos.
Gender-affirming surgery is a burgeoning field, and trainees are becoming more exposed at academic centers around the world.12,13 For top surgery, artistic skill can be difficult to teach, and it takes time and experience to acquire. Our marking technique was created to teach trainees how to understand the aesthetic outcomes of this surgery and provide a reproducible method. The marking technique does not override clinical judgment in the operating room but does provide a guide. For a training program to be teaching these surgeries with favorable aesthetic outcomes and almost no tailor tacking is an important educational milestone.
Footnotes
Published online 15 June 2021.
Disclosure: All the authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Canner JK, Harfouch O, Kodadek LM, et al. Temporal trends in gender-affirming surgery among transgender patients in the United States. JAMA Surg. 2018; 153:609–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berry MG, Curtis R, Davies D. Female-to-male transgender chest reconstruction: A large consecutive, single-surgeon experience. J Plast Reconstr Aesthet Surg. 2012; 65:711–719. [DOI] [PubMed] [Google Scholar]
- 3.Bjerrome Ahlin H, Kölby L, Elander A, et al. Improved results after implementation of the Ghent algorithm for subcutaneous mastectomy in female-to-male transsexuals. J Plast Surg Hand Surg. 2014; 48:362–367. [DOI] [PubMed] [Google Scholar]
- 4.Hage JJ, Bloem JJ. Chest wall contouring for female-to-male transsexuals: Amsterdam experience. Ann Plast Surg. 1995; 34:59–66. [DOI] [PubMed] [Google Scholar]
- 5.Lindsay WR. Creation of a male chest in female transsexuals. Ann Plast Surg. 1979; 3:39–46. [PubMed] [Google Scholar]
- 6.Monstrey S, Selvaggi G, Ceulemans P, et al. Chest-wall contouring surgery in female-to-male transsexuals: A new algorithm. Plast Reconstr Surg. 2008; 121:849–859. [DOI] [PubMed] [Google Scholar]
- 7.Namba Y, Watanabe T, Kimata Y. Mastectomy in female-to-male transsexuals. Acta Med Okayama. 2009; 63:243–247. [DOI] [PubMed] [Google Scholar]
- 8.Ammari T, Sluiter EC, Gast K, et al. Female-to-male gender-affirming chest reconstruction surgery. Aesthet Surg J. 2018; 30:807–814. [DOI] [PubMed] [Google Scholar]
- 9.Frey JD, Yu JZ, Poudrier G, et al. Modified nipple flap with free areolar graft for component nipple-areola complex construction: Outcomes with a novel technique for chest wall reconstruction in transgender men. Plast Reconstr Surg. 2018; 142:331–336. [DOI] [PubMed] [Google Scholar]
- 10.Knox ADC, Ho AL, Leung L, et al. A review of 101 consecutive subcutaneous mastectomies and male chest contouring using the concentric circular and free nipple graft techniques in female-to-male transgender patients. Plast Reconstr Surg. 2017; 139:1260e–1272e. [DOI] [PubMed] [Google Scholar]
- 11.Kääriäinen M, Salonen K, Helminen M, et al. Chest-wall contouring surgery in female-to-male transgender patients: A one-center retrospective analysis of applied surgical techniques and results. Scand J Surg. 2017; 106:74–79. [DOI] [PubMed] [Google Scholar]
- 12.Gonzalez E, Frey JD, Bluebond-Langner R. Technical refinements in gender-affirming top surgery. Plast Reconstr Surg. 2020; 146:38–40. [DOI] [PubMed] [Google Scholar]
- 13.Morrison SD, Chong HJ, Dy GW, et al. ; Transgender Educational Study Group. Educational exposure to transgender patient care in plastic surgery training. Plast Reconstr Surg. 2016; 138:944–953. [DOI] [PubMed] [Google Scholar]


