Abstract
Background
Telehealth improves access to infectious diseases (ID) and antibiotic stewardship (AS) services in small community hospitals (SCHs), but the optimal model has not been defined. We describe implementation and impact of an integrated ID telehealth (IDt) service for 16 SCHs in the Intermountain Healthcare system.
Methods
The Intermountain IDt service included a 24-hour advice line, eConsults, telemedicine consultations (TCs), daily AS surveillance, long-term AS program (ASP) support by an IDt pharmacist, and a monthly telementoring webinar. We evaluated program measures from November 2016 through April 2018.
Results
A total of 2487 IDt physician interactions with SCHs were recorded: 859 phone calls (35% of interactions), 761 eConsults (30%), and 867 TCs (35%). Of 1628 eConsults and TCs, 1400 (86%) were SCH provider requests, while 228 (14%) were IDt pharmacist generated. Six SCHs accounted for >95% of interactions. Median consultation times for each initial telehealth interaction type were 5 (interquartile range [IQR], 5–10) minutes for phone calls, 20 (IQR, 15–25) minutes for eConsults, and 50 (IQR, 35–60) minutes for TCs. Thirty-two percent of consults led to in-person ID clinic follow-up. Bacteremia was the most common reason for consultation (764/2487 [31%]) and Staphylococcus aureus the most common organism identified. ASPs were established at 16 facilities. Daily AS surveillance led to 2229 SCH pharmacist and 1305 IDt pharmacist recommendations. Eight projects were completed with IDt pharmacist support, leading to significant reductions in meropenem, vancomycin, and fluoroquinolone use.
Conclusions
An integrated IDt model led to collaborative ID/ASP interventions and improvements in antibiotic use at 16 SCHs. These findings provide insight into clinical and logistical considerations for IDt program implementation.
Keywords: antibiotic stewardship, community hospital, critical access hospitals, telehealth, infectious diseases
An integrated infectious diseases (ID) telehealth service increased access to ID and stewardship expertise for 16 community hospitals, leading to improvements in antibiotic use. Additional studies are needed to determine the optimal ID telehealth consultation type and impact on outcomes.
Infectious diseases (ID) consultation and antibiotic stewardship programs (ASPs) improve health care outcomes [1, 2]. However, implementation is challenging in resource-limited settings, and many small community hospitals (SCHs, defined as <200 beds) lack access to these services [3]. The Infectious Diseases Society of America (IDSA) endorses the use of telehealth to increase access to ID care and to ASPs, which are required by national accrediting entities [1, 4–7].
The optimal model for providing ID consultation and ASP support via telehealth has not been defined. Shively and colleagues trained local pharmacists in 2 community hospitals to perform ASP activities under the guidance of remote ID physicians, while on-site ID physicians performed consultations [8]. Monkowski and colleagues provided ID telemedicine consults, while Tande and colleagues provided asynchronous ID eConsult for remote hospitals, but neither described an integrated ASP component [9, 10]. Stevenson and colleagues used a weekly videoconference to support antibiotic stewardship efforts at 2 rural facilities [11]. In a more integrated model, Laible and colleagues established an ASP across a rural health system through a daily call where local pharmacists identified and presented cases [12]. The call was staffed by an ID pharmacist and physician, who also provided telemedicine consults for the remote sites.
To our knowledge, no studies have described a centralized, integrated telehealth program that provides both full-time ID consultation and ASP support for multiple SCHs. The Stewardship in Small Community Hospitals–Optimizing Outcomes and Resources (SCORE) study, a cluster randomized trial in 15 Intermountain Healthcare SCHs, demonstrated the need for both antibiotic stewardship and ID consultation in these facilities, leading to the formation of an integrated system-wide ID telehealth (IDt) program [13, 14]. Herein, we describe the program’s structure, workflow, and impact during the first 18 months of implementation.
METHODS
Practice Setting
Intermountain Healthcare (hereafter Intermountain) is a nonprofit integrated network of 23 hospitals in Utah and Idaho. Between November 2016 and July 2017, an IDt program physically based at Intermountain Medical Center (IMC) near Salt Lake City was implemented in a stepwise manner for Intermountain’s 16 SCHs (15 in Utah and 1 in Idaho), starting with the largest facilities. The supported hospitals comprised 688 staffed inpatient beds (range, 14–146 each). Ten had <30 beds, with 6 rural hospitals having a Critical Access Hospital designation [15]. The closest facility to IMC was 1.7 miles and the farthest was 240 miles, with a total north-south geographic span of 430 miles for all sites.
Service Components and Program Implementation
The IDt program offered both ID consultation and ASP services. IDt consultation included a 24-hour ID hotline staffed by an attending ID physician, who offered 1 of 3 services depending on patient and requesting provider needs: phone advice only, comprehensive chart review and electronic medical record (EMR) documentation (eConsults), or inpatient synchronous telemedicine consultations (TCs) using an encrypted, Health Insurance Portability and Accountability Act (HIPAA)–compliant, 2-way audiovisual connection to interview and examine the patient. ASP services included daily inpatient surveillance and longitudinal project support by an IDt pharmacist and a monthly telementoring webinar provided by the IDt pharmacist and IDt medical director.
IDt staff included 2 IDt physicians (1 IDt medical director, with a total of 1.5 ID physician clinical full-time equivalents [FTEs] dedicated to the IDt program), 1 FTE IDt pharmacist, 0.5 FTE nurse operations manager, and 0.2 FTE data analyst. Baseline data from the SCORE study were used to estimate staffing needs and create a business case [16] that was approved by Intermountain leadership. The IDt physicians and pharmacist obtained Utah and Idaho licenses, and the IDt physicians were credentialed and privileged as telemedicine clinicians at all 16 SCHs.
The IDt medical director and IDt pharmacist conducted site visits to meet SCH leadership and key clinical staff. Telehealth equipment was already installed at all SCHs to support Intermountain’s comprehensive telehealth services (eg, telecritical care, telestroke, telecrisis). All SCHs had a combination of in-room fixed cameras and mobile carts: 13 used primarily in-room cameras for TCs, and 3 used primarily mobile carts that were located on acute care floors. SCH nurses completed an online training module and were then trained in-person regarding their bedside role (eg, assisting with physical examination if needed) and how to prepare patients for TCs. IDt physicians were trained to use the telehealth software and equipment prior to rotating on the IDt service.
IDt Consultation
Local providers at the 16 SCHs used a dedicated phone number to contact the IDt physician, who determined whether the case required phone advice alone, an eConsult, or TC. One IDt physician covered the service on weekdays from 7:30 am to 4:30 pm. A different on-call (non-telehealth) ID physician provided after-hours and weekend coverage (phone advice only) to ensure SCH access 24 hours a day, 7 days a week.
To monitor workload, EMR note templates were created to capture the consultation type (eConsult vs TC), reason for consultation, primary ID diagnosis, time spent reviewing the chart and discussing with primary team, and time spent on-camera. To estimate workload requirements for eConsults vs TCs, we compared duration in minutes for the first telehealth interaction only. A note was not written for telephone-only advice, but the reason for call, requesting site, and time spent on the case were logged in REDCap (Research Electronic Data Capture; copyright 2006–2013 Vanderbilt University) by the answering IDt physician. REDCap entries were used to capture the first interaction between an SCH provider and IDt clinician on cases that did not require an eConsult or TC. Patients were not billed for IDt consultation; rather, each facility paid an annual subscription fee for access to all telehealth services as part of Intermountain’s integrated clinical support system. For outpatient follow-up, SCH patients could be seen in person by an IDt physician at the IMC ID clinic. Alternatively, patients could be followed by their local primary care provider, who could contact the IDt service with additional questions. The SCH with the highest volume of IDt needs was also equipped with capability for outpatient IDt follow-up visits if deemed necessary by the patient’s primary care provider and IDt physician at time of hospital discharge.
Antibiotic Stewardship
Local ASP Structure and Stewardship Interventions
The IDt medical director and pharmacist met with key stakeholders at all 16 SCHs to establish multidisciplinary ASPs led by a local physician and pharmacist champion. The IDt pharmacist and physician attended ASP meetings in person or via teleconference to support the local teams and were designated as formal members of each SCH ASP committee. Daily prospective audit and feedback efforts were driven by local SCH pharmacists, who were trained in person by the IDt pharmacist to review Vigilanz alerts (Vigilanz Corporation, Minneapolis, Minnesota). Alerts prioritized for SCH pharmacists included positive and finalized cultures, intravenous to oral conversion opportunities, and double anaerobic coverage. Vancomycin dosing and antibiotic renal dose adjustment were also part of their daily responsibilities.
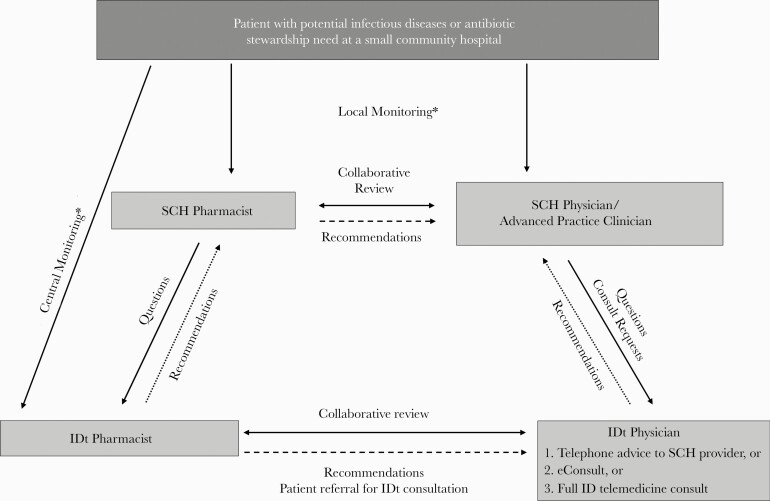
The IDt pharmacist reviewed Vigilanz alerts for positive blood cultures, duration of therapy, broad-spectrum antibiotics, and multidrug-resistant organisms. Interventions were made by contacting the local SCH pharmacist, who communicated with the local provider. SCH pharmacists could also contact the IDt pharmacist with questions. Patients with key ID conditions (eg, Staphylococcus aureus bacteremia) were reviewed with the IDt physician on daily rounds to facilitate IDt consultation or intervention by the IDt pharmacist. The IDt pharmacist also monitored and provided recommendations for IDt service patients. All IDt pharmacist chart reviews (from review of Vigilanz alerts + IDt service patients + phone calls from SCH pharmacists), recommendations, and accepted recommendations (interventions) were tracked in REDCap. A depiction of the IDt program workflow is provided in Figure 1.
Figure 1.
Infectious diseases telehealth (IDt) service components and workflow. *Local and central monitoring consisted of antimicrobial use surveillance, microbiological culture surveillance, and chart review for potential stewardship interventions by the small community hospital (SCH) pharmacist and IDt pharmacist, respectively. The IDt pharmacist occasionally had direct telephonic communication with local SCH providers but more often referred to the IDt physician, who provided recommendations to SCH providers by telephone. The IDt pharmacist used primarily telephone (not video) to communicate with SCHs. Abbreviations: eConsult, electronic consultation (comprehensive chart review, discussion with requesting provider, and documentation in electronic medical record); IDt, infectious diseases telehealth; SCH, small community hospital.
IDt ASP-Provided Resources, Data Tracking, and Education
Annual antibiograms were distributed to all local ASPs by the IMC Microbiology Laboratory. Regional microbiology results were aggregated as necessary due to small sample sizes. Antibiotic use data (days of therapy [DOT] per 1000 days present [DP] submitted through the Centers for Disease Control and Prevention’s National Healthcare Safety Network Antimicrobial Use [NHSN AU] module) [17] were made available to all sites through a dashboard, which was used to compare similar facilities and identify outliers for targeted interventions. The IDt pharmacist facilitated completion of local quality improvement projects by helping with project selection, defining appropriateness criteria (based on guidelines and antibiogram data), developing protocols, collecting and interpreting data, educating providers, and assessing impact.
Education was provided to SCH clinicians during daily patient case interactions. In addition, a monthly 30-minute telementoring webinar provided further education to local pharmacists and clinicians who were new to ASP activities. Key ID and stewardship topics were highlighted with patient cases and literature review. ASP champions were invited to discuss quality improvement projects for collaborative learning and feedback.
Data Sources and Analyses
IDt EMR notes from November 2016 through April 2018 were obtained from Intermountain’s electronic data warehouse, and all documented phone advice calls were obtained from REDCap to measure aggregate IDt workload. A more detailed analysis of the first 6 months was performed, which included manual review of all TCs, eConsults, and phone advice calls to identify ID conditions and causative organisms encountered during consultation. Descriptive statistics were used for all data.
We used an electronic survey with a 5-point Likert scale (ranging from “strongly disagree” to “strongly agree”) to evaluate satisfaction of SCH clinicians who had interacted with the IDt service during the first 3 months following implementation. This included SCH physicians and advanced practice clinicians who requested consults, frontline nurses who assisted with TCs, SCH pharmacists who interacted with the IDt pharmacist, and administrators who assisted with IDt implementation in their facilities. We used a similar survey conducted via telephone to evaluate patient satisfaction using a convenience sample of randomly selected patients for whom a TC was completed in the first 3 months.
To capture daily ASP activities, acknowledged Vigilanz alerts for hospitalized patients were compiled for the both the IDt and SCH pharmacists from November 2016 to April 2018. IDt pharmacist interventions were compiled from REDCap. Quality improvement projects were completed at various timepoints over the first 9 months of the IDt ASP. Therefore, as a conservative estimate, the average antibiotic use rate for targeted antibiotics (obtained from reported NHSN AU data) was compared in the 18 months before and 18 months after IDt service implementation (May 2015 to October 2016 vs November 2016 to April 2018, respectively). Antibiotic use rates were compared using an unpaired 2-tailed t test. P values < .05 were considered statistically significant.
Patient Consent Statement
In accordance with established institutional health care policy and practices, patients consented for their medical care at time of hospital admission, to include the delivery of telehealth care. We analyzed previously collected EMR descriptive data that were deidentified. The Intermountain Healthcare Institutional Review Board reviewed the study proposal and determined that it posed minimal risk and warranted exempt categorization.
RESULTS
IDt Consultation
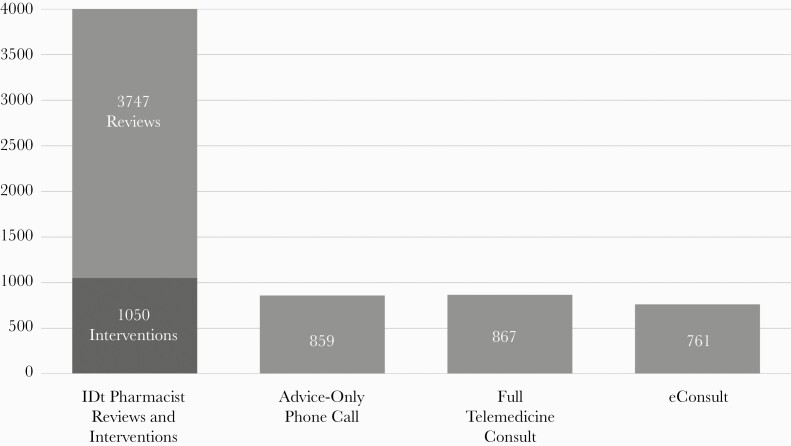
A total of 2487 interactions between an IDt physician and a SCH were identified during the first 18 months of the program. Of these, 859 (35%) were telephone advice only, 761 (30%) were eConsults, and 867 (35%) were TCs (Figure 2). The majority of eConsults and TCs (86%) were requested by an SCH provider, while 14% were initiated through stewardship surveillance by the IDt pharmacist. Each SCH requested at least 1 IDt consultation during the study period, with the 6 largest facilities (ranging in bed size from 30–146) accounting for >95% of interactions. Including all initial telehealth visits, a median time of 5 (interquartile range [IQR], 5–10) minutes was spent on telephone advice-only calls, 20 (IQR, 15–25) minutes on eConsults, and 50 (IQR, 35–60) minutes on TCs. For TCs, a median of 21 (IQR, 17–30) minutes was camera time. Thirty-two percent of all eConsults and TCs resulted in an in-person ID clinic follow-up visit.
Figure 2.
Infectious diseases telehealth (IDt) interventions (18 months). Review: remote chart review completed by the IDt pharmacist for potential stewardship intervention. Intervention: documented change or discontinuation of antimicrobial therapy, or generation of a new IDt physician consultation resulting from IDt pharmacist recommendations.
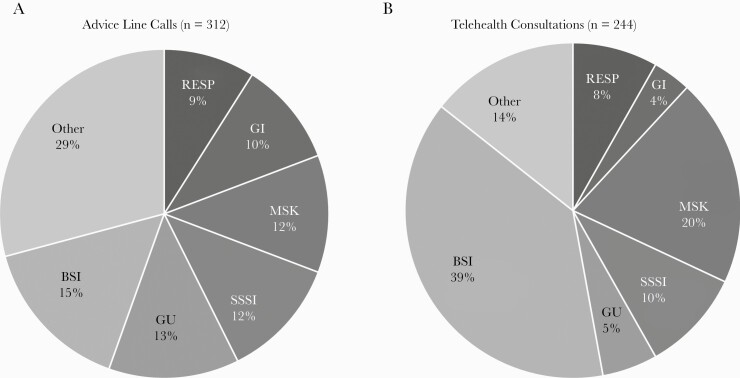
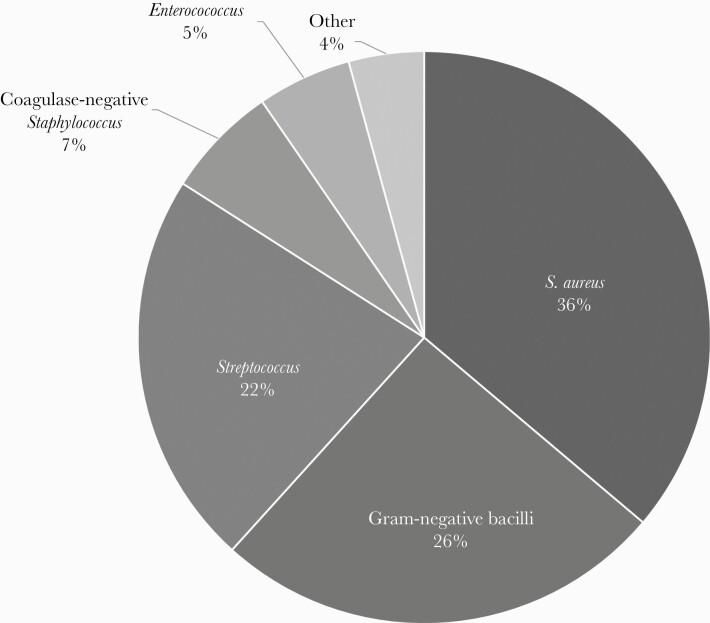
Detailed analysis of the program’s first 6 months included 556 unique patients: 312 for whom advice-only calls were completed and 244 for whom an eConsult or TC was completed. Of the 244 patients, 95 (39%) had eConsults only, 108 (44%) had TCs only, and 41 (17%) had a combination of eConsults and TCs during their hospitalization (eg, patient initially had an eConsult and then had a full TC later in the admission). A total of 431 EMR notes were entered for these 244 patients (155 [36%] eConsults and 276 [64%] TCs). There was a median of 1 telehealth note per patient (IQR, 1–2; range, 1–7). Of the patients who received either eConsults only or TCs only during their hospital course, the time spent on initial eConsult vs initial TC was significantly shorter: median of 16 (IQR, 15–25) minutes vs 55 (IQR, 40–60) minutes (P < .001). Common infection categories stratified by consult type (advice only vs eConsults/TCs) are displayed in Figure 3. Bloodstream infections were the most common reason for contacting the IDt service and Staphylococcus aureus was the most commonly identified organism (Figure 4).
Figure 3.
Conditions seen during first 6 months of infectious diseases telehealth (IDt) service. A, Advice line calls (n = 312). “Other” category (infection control, prophylaxis, travel, human immunodeficiency virus, central nervous system [CNS], laboratory/diagnostic interpretation, ear, nose, and throat [ENT], fever not otherwise specified [NOS], animal bite, sepsis NOS, gynecology [GYN]) (20 calls were specifically for antibiotic selection/dose; reason for call was not specified for 21 cases). B, Telehealth consultations (n = 244). Telehealth consultations includes electronic consultations and telemedicine consultations. “Other” category includes CNS, laboratory/diagnostic interpretation, ENT, sepsis NOS, GYN. Antibiotic selection/dose alone was not a reason for either electronic consultation or full telemedicine consultation visit (as these were typically addressed on IDt pharmacist review/intervention. Abbreviations: BSI, bloodstream infection; GI, gastrointestinal; GU, genitourinary; MSK, musculoskeletal; RESP, respiratory; SSSI, skin and skin structure infection.
Figure 4.
Microorganisms identified on bloodstream infections seen in infectious diseases telehealth consultation during the first 6 months. Ninety-four bloodstream infections where organism was identified: 34 Staphylococcus aureus (28 methicillin susceptible, 6 methicillin resistant); 6 coagulase-negative staphylococci; 24 gram-negative bacilli (12 Escherichia coli, 4 Pseudomonas, 8 other; Klebsiella, Moraxella, Gemella; 21 streptococci (7 group B, 3 group A, 3 viridans group, 2 Streptococcus pneumoniae, 1 group C, 5 not specified); enterococci (5 Enterococcus faecalis); 4 other (2 Leuconostoc, 1 Candida, 1 culture-negative endocarditis).
During the first 3 months following implementation, 22 randomly selected TC patients were contacted via telephone to complete a survey after hospital discharge (mean age, 63; 75% male). All patients felt the service improved care and was necessary (selected “agree” or “strongly agree”), while 20 of 22 (91%) felt it was easy to use (2 mentioned technical difficulties during their initial IDt visits). Ninety-eight SCH clinicians who had used the IDt service were surveyed electronically, and 31 (32%) responded: 97% felt the service improved care, 90% felt it was necessary, 90% felt it was easy to access, and 95% felt it was easy to use. Respondents included physicians and advance practice clinicians (48%), pharmacists (23%), nurses (23%), and hospital administrators (6%). Nursing staff indicated that they enjoyed assisting with physical examinations and appreciated being at the bedside during TC visits to stay informed about their patient’s ID condition because it helped them provide better care for their patients.
Antibiotic Stewardship
During the study period, local SCH pharmacists acknowledged Vigilanz alerts for 14 621 unique patients, of which 2229 (15%) led to an antibiotic stewardship recommendation. Due to variability in documentation, it was not possible to determine how many of these recommendations were accepted by the provider. The IDt pharmacist reviewed 3747 unique patients: 3215 (86%) Vigilanz alerts, 155 (4%) IDt service patients, and 377 (10%) calls from SCH pharmacists. Of the 3747 chart reviews, 1305 (35%) led to a recommendation, and 1050 of these (80%) were accepted (Figure 2). A recommendation for IDt consultation was made for 259 patients, of which 228 (88%) were accepted.
The IDt pharmacist worked with local ASPs at the SCHs to complete 8 separate quality improvement projects. Four medication use evaluations with subsequent targeted interventions led to significant reductions in meropenem, fluoroquinolone, and vancomycin use across 8 facilities, while no significant change in piperacillin-tazobactam use was seen at 1 facility (Table 1). Four process improvement projects were implemented across 8 SCHs, leading to reduced inappropriate surgical prophylaxis and increased pharmacist interventions for emergency department patients that were discharged with pending microbiologic cultures. One SCH implemented a pharmacist-led protocol for real-time intervention on rapid diagnostic testing (RDT) results for positive blood cultures, which significantly reduced time to antibiotic de-escalation compared to RDT alone (Table 1).
Table 1.
Small Community Hospital Stewardship Projects Facilitated by the Infectious Diseases Telehealth (IDt) Pharmacist and IDt Physician During First 18 Months
| Projects | Hospitals, No.a | Hospital Size, No. of Beds | Baseline Data (May 2015–October 2016) | Intervention Data (November 2016–April 2018) | Key Interventions by IDt and Local ASP Pharmacistsb |
|---|---|---|---|---|---|
| Medication use evaluations | |||||
| Meropenem | 5 | 18–90 | 13 DOT/1000 DP | 9 DOT/1000 DP (P = .03)c | • Education on local resistance using local antibiograms, ASP committee meetings, and guideline review |
| Vancomycin | 2 | 28–56 | 75 DOT/1000 DP | 53 DOT/1000 DP (P < .01) | • Education on SSTI, UTI, CAP guidelines |
| • Implementation of MRSA nasal swabs for CAP | |||||
| Piperacillin-tazobactam | 1 | 25 | 59 DOT/1000 DP | 85 DOT/1000 DP (P = .09)d | • Education on appendicitis guideline |
| • Initiation of 48-h timeout | |||||
| Fluoroquinolone | 1 | 14 | 147 DOT/1000 DP | 82 DOT/1000 DP (P < .01) | • Education on management of ASB, and appropriate treatment of UTI and CAP |
| Process improvement projects | |||||
| Allergy assessment and surgical prophylaxis | 2 | 26–30 | 30%–50% inappropriate clindamycin use | <5% inappropriate use | • Nurse/physician education on allergies |
| • Prospective pharmacist order review | |||||
| Pharmacist-led RDT protocol for bacteremia | 1 | 148 | Median 33 h to antibiotic de-escalatione with RDT alone | Median 14 h to antibiotic de-escalatione when real-time pharmacist intervention added to RDT (P = .01) | • Developed RDT protocol and trained local pharmacists |
| • 24/7 real-time intervention by local pharmacists on RDT results/bacteremia | |||||
| Pharmacist review of finalized ED cultures | 4 | 26–90 | ED cultures not being reviewed in timely/standardized manner postdischarge | 121 recommendations made to optimize antibiotics | • Trained local pharmacists and developed guideline for common ED conditions |
| 19 documented as good catch/avoided safety event | • IDt pharmacist available for questions | ||||
| Surgical prophylaxis audit | 1 | 25 | 14% suboptimal antibiotic timing/ documentation | Reduced to 7% | • Physician education |
| • Active pharmacist surveillance |
Abbreviations: ASB, asymptomatic bacteriuria; ASP, antibiotic stewardship program; ED, emergency department; CAP, community-acquired pneumonia; DOT/1000 DP, days of therapy per 1000 days present; IDt, infectious diseases telehealth; MRSA, methicillin-resistant Staphylococcus aureus; RDT, rapid diagnostic test; SSTI, skin and soft tissue infection; UTI, urinary tract infection.
aMultiple hospitals could participate in each project. Hospitals that completed multiple projects appear more than once.
bPatient charts were reviewed for all quality improvement projects to assess appropriateness, and physicians were given feedback on their prescribing.
cMean antibiotic usage (DOT/1000 DP) over 18-month intervention period compared to mean usage over 18-month baseline period.
dAn increase in patients admitted with infectious diseases conditions requiring piperacillin-tazobactam may have led to increased usage.
eTime to de-escalation compared using Kaplan-Meier survival analysis with log-rank test.
Six telementoring webinars were completed during the last 6 months of the study period. Between 10 and 25 participants called into each session, comprised primarily of pharmacists. Sample topics included asymptomatic bacteriuria, Clostridioides difficile management, system antibiotic stewardship updates, and the role of nursing in stewardship.
DISCUSSION
A multicomponent IDt service supporting 16 SCHs was well-utilized and well-received by staff and patients. We identified bloodstream infections as the most common reason for IDt consultation and S. aureus as the most common pathogen. Furthermore, we found that IDt consultations were evenly distributed between telephone calls, eConsults, and TCs, with a significant difference in amount of time spent on each consult type. These findings provide important insight into clinical and logistical considerations for implementing an IDt service.
Published data are limited on reasons for requesting IDt consultation in SCHs, but 1 recent study also found bacteremia to be common in a 150-bed hospital [9]. While facility size alone may be a driver of IDt consultation volumes, bacteremia incidence may be a reasonable gauge for estimating IDt needs. Indeed, we observed that the 6 largest facilities accounting for >95% of IDt consultations also had the highest incidence of positive blood cultures during the 18-month study period. Staphylococcus aureus bacteremia was common in our facilities and is a condition for which ID consultation is known to improve outcomes [18]. Focusing clinical, operational, and educational efforts on this important ID condition may provide an opportunity to demonstrate the value of an IDt service.
The optimal type of IDt consultation is unknown. Improvements in length of stay and mortality have been observed following implementation of TCs [9] and eConsults [10], but IDt consultation types have not been compared. The optimal modality may depend on the specific ID condition. For example, phone-only compared to in-person consultation has been associated with higher mortality for S. aureus bacteremia [19, 20]. Our program is unique in that our telephysicians had options to provide phone-only advice, eConsults, or TCs. The teleconsultation type was left to the provider’s discretion, which raises logistical and clinical considerations. While eConsults are more time efficient and might be adequate for certain ID conditions (eg, uncomplicated gram-negative bacteremia with clear and controlled source), TCs may be preferable for certain conditions such as central nervous system infections, complicated S. aureus bacteremia, critically ill patients; in patients where a detailed history is needed (eg, fever of unknown origin and returning travelers); or if IDt clinicians are uncomfortable with the data presented by the referring provider. Additional studies are needed to determine the impact of IDt consultation type on outcomes for specific ID conditions.
Regarding the telestewardship service, we established and supported ASPs at 16 Intermountain SCHs, and IDt expertise was highly utilized. Empowering local ASPs with full-time centralized surveillance, project support, and education was an effective AS model leading to significant improvements in targeted antibiotic use and processes. Success with centralized telestewardship has been reported by other health care systems [12]; thus, it may be a feasible model for extending access and resources to SCHs within a health care system.
The stewardship and consult components of the IDt service were highly complementary, which is consistent with findings in previous studies [8, 21, 22]. IDt pharmacist recommendations were associated with a high acceptance rate, and nearly a quarter of recommendations led to IDt physician consultations. Active surveillance facilitated timely consultation for key conditions (eg, S. aureus bacteremia), which was important because IDt consultation was not mandated by the health system, and some SCH clinicians lacked awareness of the benefits or utility of a new IDt service. Surveillance led to real-time education for SCH clinicians during staffing of individual cases and formal on-site grand rounds to maximize clinician engagement. Similarly, IDt physician and pharmacist participation in local ASPs promoted good stewardship practices among the same clinicians. This integrated multidisciplinary approach facilitated consistent communication, empowerment, and building of relationships with SCH clinicians, which was critical to our program’s success.
There are several noteworthy limitations of our study. First, we did not assess impact of IDt consultation or telestewardship on clinical outcomes, overall antibiotic use, avoided transfers, or cost savings, which we plan to evaluate in future studies. Second, all SCHs were part of the same health care system, with a shared EMR, access to centralized data, and preexisting telehealth resources (including a facility subscription model and on-site equipment), which was a clear advantage for both the IDt consult and ASP components. Our program design and success may not be generalizable to health care systems lacking similar resources or to those providing services to external facilities. Third, our pre/post stewardship analysis showed improvement at SCHs targeting specific antibiotics with projects, but an interrupted time series analysis was not used and complimentary antibiotic use was not assessed. Last, due to the comprehensive nature of our service, it was not possible to determine the impact of individual components (IDt consultations vs ASP) or specific interventions (eg, monthly telementoring webinar) on outcomes. While we believe our model reflects best practice, other health systems will have to adapt based on available personnel and resources when implementing similar programs.
CONCLUSIONS
We implemented a large-scale, multicomponent IDt program that increased access to ID care and stewardship expertise for 16 SCHs. An integrated IDt and tele-ASP model was essential for success, leading to collaborative interventions and significant improvements in targeted antibiotic use and processes.
Next steps for our IDt program are to evaluate its impact on clinical outcomes, antibiotic use, transfers, and cost savings, and to investigate the optimal IDt consultation type for specific conditions. We intend to evaluate opportunities for direct billing of patient insurance (eg, for inpatient consultation or scheduled outpatient video visits) with the changing regulatory landscape surrounding telehealth billing [23]. We also plan to expand the program by providing IDt/ASP support for additional Intermountain and non-Intermountain facilities, and by adding IDt physician and IDt pharmacist FTEs to support program operations.
Notes
Acknowledgments. We thank our small community hospital patients and health care team members throughout the Intermountain health care system for their assistance with developing, implementing, and evaluating our program. Countless small community hospital clinicians and antibiotic stewardship program champions across the system were essential to the success of the infectious diseases telehealth service. We also thank Intermountain leaders in Telehealth and Pharmacy Services for their support.
Potential conflicts of interest. All authors: No reported conflicts of interest.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Schmitt S, McQuillen DP, Nahass R, et al. Infectious diseases specialty intervention is associated with decreased mortality and lower healthcare costs. Clin Infect Dis 2014; 58:22–8. [DOI] [PubMed] [Google Scholar]
- 2. Barlam TF, Cosgrove SE, Abbo LM, et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis 2016; 62:e51–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stenehjem E, Hyun DY, Septimus E, et al. Antibiotic stewardship in small hospitals: barriers and potential solutions. Clin Infect Dis 2017; 65:691–6. [DOI] [PubMed] [Google Scholar]
- 4. Young JD, Abdel-Massih R, Herchline T, et al. Infectious Diseases Society of America position statement on telehealth and telemedicine as applied to the practice of infectious diseases. Clin Infect Dis 2019; 68:1437–43. [DOI] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. Core elements of hospital antibiotic stewardship programs. Available at: https://www.cdc.gov/antibiotic-use/core-elements/hospital.html. Accessed 20 April 2020. [DOI] [PMC free article] [PubMed]
- 6. The Joint Commission. New antimicrobial stewardship standard. Available at: https://www.jointcommission.org/assets/1/6/New_Antimicrobial_Stewardship_Standard.pdf. Accessed 20 April 2020.
- 7. Centers for Medicare and Medicaid Services. Conditions of participation for hospitals and critical access hospitals (CAHs). Available at: https://www.federalregister.gov/documents/2019/09/30/2019–20736/medicare-and-medicaid. Accessed 20 July 2020.
- 8. Shively NR, Moffa MA, Paul KT, et al. Impact of a telehealth-based antimicrobial stewardship program in a community hospital health system. Clin Infect Dis 2020; 71:539–45. [DOI] [PubMed] [Google Scholar]
- 9. Monkowski D, Rodes LV, Templer S, et al. A retrospective cohort study to assess the impact of an inpatient infectious disease telemedicine consultation service on hospital and patient outcomes. Clin Infect Dis 2020; 70:763–70. [DOI] [PubMed] [Google Scholar]
- 10. Tande AJ, Berbari EF, Ramar P, et al. Association of a remotely offered infectious diseases econsult service with improved clinical outcomes. Open Forum Infect Dis 2020; 7:ofaa003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stevenson LD, Banks RE, Stryczek KC, et al. A pilot study using telehealth to implement antimicrobial stewardship at two rural Veterans Affairs medical centers. Infect Control Hosp Epidemiol 2018; 39:1163–9. [DOI] [PubMed] [Google Scholar]
- 12. Laible BR, Grosdidier J, Nazir J. Developing an antimicrobial stewardship program across a rural health system: the Avera Health experience. Am J Health Syst Pharm 2019; 76:108–13. [DOI] [PubMed] [Google Scholar]
- 13. Stenehjem E, Hersh AL, Sheng X, et al. Antibiotic use in small community hospitals. Clin Infect Dis 2016; 63:1273–80. [DOI] [PubMed] [Google Scholar]
- 14. Stenehjem E, Hersh AL, Buckel WR, et al. Impact of implementing antibiotic stewardship programs in 15 small hospitals: a cluster-randomized intervention. Clin Infect Dis 2018; 67:525–32. [DOI] [PubMed] [Google Scholar]
- 15. Critical Access Hospitals. Rural health information hub. Available at: https://www.ruralhealthinfo.org/topics/critical-access-hospitals. Accessed 25 September 2020.
- 16. Spellberg B, Bartlett JG, Gilbert DN. How to pitch an antibiotic stewardship program to the hospital C-suite. Open Forum Infect Dis 2016; 3:ofw210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention. Antimicrobial use and resistance (AUR) module. Available at: www.cdc.gov/nhsn/pdfs/pscmanual/11pscaurcurrent.pdf. Accessed 30 August 2020.
- 18. Bai AD, Showler A, Burry L, et al. Impact of infectious disease consultation on quality of care, mortality, and length of stay in Staphylococcus aureus bacteremia: results from a large multicenter cohort study. Clin Infect Dis 2015; 60:1451–61. [DOI] [PubMed] [Google Scholar]
- 19. Forsblom E, Ruotsalainen E, Ollgren J, Järvinen A. Telephone consultation cannot replace bedside infectious disease consultation in the management of Staphylococcus aureus bacteremia. Clin Infect Dis 2013; 56:527–35. [DOI] [PubMed] [Google Scholar]
- 20. Saunderson RB, Gouliouris T, Nickerson EK, et al. Impact of routine bedside infectious disease consultation on clinical management and outcome of Staphylococcus aureus bacteraemia in adults. Clin Microbiol Infect 2015; 21:779–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Messacar K, Campbell K, Pearce K, et al. A handshake from antimicrobial stewardship opens doors for infectious disease consultations. Clin Infect Dis 2017; 64:1449–52. [DOI] [PubMed] [Google Scholar]
- 22. Morrill HJ, Gaitanis MM, LaPlante KL. Antimicrobial stewardship program prompts increased and earlier infectious diseases consultation. Antimicrob Resist Infect Control 2014; 3:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Department of Health and Human Services. Billing for telehealth during COVID-19. Available at: https://telehealth.hhs.gov/providers/billing-and-reimbursement/. Accessed 14 February 2021.