Abstract
Purpose
Many public institutions and settings have taken action to limit exposure to and slow the spread of the novel coronavirus (COVID-19). We sought to characterize the impact of stay-at-home orders on our study of cerebral autoregulation and its association with developmental delays in infants with congenital heart disease compared with healthy controls.
Design and methods
We calculated the number of participants recruited (i.e., not enrolled in the study) and assessed (i.e., currently enrolled) before March 2020 (pre-COVID-19) and the number of participants that we could not recruit or assess between March and July 2020 (missed due to COVID-19), separately for congenital heart disease and healthy control infants, in reference to the impacts of COVID-19. We used negative binomial regressions to determine incidence rate ratios which compared participants recruited and assessed pre-COVID-19 and missed due to COVID-19.
Results
Recruitment and assessments significantly decreased following the pandemic, i.e., participants were more likely to be recruited or be assessed pre-COVID-19 compared to during the pandemic. Study participants were 3.3 times as likely to have assessments performed pre-COVID-19 compared to during the COVID-19 pandemic (p < 0.001).
Clinical implications
Clinical research teams may consider making protocol modifications such as virtual visits or video recordings explaining the study, for example, to adjust to the restrictions caused by COVID-19.
Conclusion
The COVID-19 pandemic drastically reduced recruitment and assessments completed in our study. Study teams will need to continue to modify procedures for recruitment and assessments that align with COVID-19 regulations to facilitate research progress during the pandemic.
Keywords: COVID-19, Congenital heart disease, Pediatrics, Clinical research, Stay-at-home order
Introduction
The first laboratory-confirmed case of severe acute respiratory syndrome coronavirus 2
(SARS-CoV-2) or the coronavirus disease (COVID-19) reported to the Centers for Disease Control and Prevention (CDC) was documented in December 2019 (Fan et al., 2020; Stokes et al., 2020). The United States reported its first confirmed case of COVID-19 on January 20th, 2020 (Holshue et al., 2020; Omary & Hassan, 2020). By March 2020, the World Health Organization declared COVID-19 a pandemic (Ghebreyesus, 2020) and the United States declared COVID-19 as a national emergency. Due to the rapid spread of COVID-19, businesses and organizations throughout the world had to close unexpectedly. The reinforcement of physical and social distancing and the implementation of stay-at-home orders put research operations on hold. Research studies were highly affected due to the inability to collect data.
The COVID-19 pandemic has curtailed most clinical research, pausing trials for new enrollment to minimize participants' risk of exposure to COVID-19. From March 1st to April 26th, 2020, 905 clinical trials reported the COVID-19 pandemic as the reason for suspension (Asaad et al., 2020). The suspension of these trials posed significant clinical implications on patients as it slowed potential treatments for non-COVID-19 diseases, e.g., participants with end-stage diseases where drugs offered by clinical trials may be their only potential hope for treatment (Colbert et al., 2020; Asaad et al., 2020). The pandemic was especially devastating for oncology patients in clinical trials because they could not receive the investigational treatments outside of the clinical research unit, nor could clinical researchers provide investigational treatments to their participants outside of their facilities due to research regulations (de Miguel et al., 2020).
Health care facilities quickly implemented new procedures and restrictions that prevented clinical researchers from obtaining their data. Research, including those that required in-person visits, was deemed nonessential and came to a halt (Omary et al., 2020). Researchers could no longer perform experiments, assessments, and recruitment of participants (Weiner et al., 2020), resulting in a pause of data collection, which caused gaps in many research studies. Many medical institutions nationwide encouraged the stay-at-home order, causing most nonessential staff to work remotely at the beginning of March 2020. Although remote research can be performed, many studies cannot function for extended periods without direct contact with participants (Colbert et al., 2020). The purpose of this paper is to evaluate the impact of the COVID-19 pandemic on our research study at Children's Hospital Los Angeles (CHLA).
Methods
Data collection
We collected data on the number of participants that we recruited (i.e., eligible infants not enrolled in the study) and assessed (i.e., infants currently enrolled in the study) pre-COVID-19, missed due to COVID-19, and post-COVID-19. This equaled 6 time points: (1) participant recruitment before March 2020 (pre-COVID-19); (2) participant assessments pre-COVID-19; (3) participant recruitment missed between March 2020 and July 2020 (missed due to COVID-19); (4) participant assessments missed due to COVID-19; (5) participant recruitment after July 2020 (post-COVID-19) when the county lifted stay-at-home orders; and (6) participant assessments post-COVID-19. Though we collected data on participants post-COVID-19, we did not run any statistical analyses using post-COVID-19 data because we could not successfully recruit or assess participants post-COVID-19 (as of August 2020). We then categorized participants into 2 groups: infants diagnosed with congenital heart disease (CHD) and healthy control (HC) infants.
Statistical analyses
Stratified descriptive analyses (based on group and assessment time points) were conducted and summarized as means with standard deviations for continuous variables and frequencies with proportions for categorical variables. Pearson's chi-square tests evaluated the difference in categorical variables versus CHD status at each assessment time point. We conducted Fisher's Exact test if any value within the category was less than five. Two-sample independent t-tests determined the difference between the means of 2 independent groups of infants at each time point of assessment for continuous variables.
We used negative binomial regressions to estimate incidence rate ratios with 95% confidence intervals. We conducted separate regression analyses to test the association between pre-COVID-19 and missed due to COVID-19 recruitment and assessment for each group. P-values ≤0.05 were considered statistically significant. We conducted all statistical analyses on IBM SPSS Statistics 27.
Results
We recruited a total of 104 (33%) of the 315 infants that were eligible to participate in our study before March 2020 (pre-COVID-19), which included 57 HC and 47 infants diagnosed with CHD. We could not recruit a total of 127 eligible participants, 105 HC and 22 CHD infants, due to COVID-19. We did not recruit any infants between July to August 2020 (post-COVID-19). We performed a total of 160 assessments pre-COVID-19 (68 on HC and 92 on CHD infants). We had 49 infants (35 HC and 14 CHD infants) miss their study assessments due to COVID-19. From July to August 2020, post-COVID-19, we performed 6 HC assessments and 0 CHD assessments. Detailed findings can be found in Table 1 .
Table 1.
Number of participants recruited and assessed pre-COVID-19, missed due to COVID-19, and post-COVID-19.
| Healthy Control Infants | Infants with Congenital Heart Disease | Total | |
|---|---|---|---|
| Participants recruited before March 2020 (pre-COVID-19) | 57 | 47 | 104 |
| Participants we could not recruit due to COVID-19 (missed due to COVID-19) | 105 | 22 | 127 |
| Participants recruited between July and August 2020 (post-COVID-19) | 0 | 0 | 0 |
| Assessments performed pre-COVID-19 | 68 | 92 | 160 |
| Assessments missed due to COVID-19 | 35 | 14 | 49 |
| Assessments performed post-COVID-19 | 6 | 0 | 6 |
Pre-COVID-19, we performed assessments on 48 infants (19 HC, 29 CHD infants) at the neonatal age time point, 44 infants (21 HC, 23 CHD infants) at 3-months of age, 40 infants (16 HC, 24 CHD infants) at 6-months of age, and 30 infants (10 HC, 20 CHD infants) at 9-months of age. Detailed findings can be found in Table 2 . We found a higher proportion of females in the CHD group throughout most age time points (69.2%, 54.2%, 60.0% for neonatal, 6-, 9-months respectively), which was statistically significant (χ2 = 4.7, p = 0.031). We had a high prevalence of Latino participants throughout all age time points (64.6%, 68.2%, 67.5%, 73.3% for neonatal, 3-, 6-, 9-months respectively), especially in the CHD group. The mean gestational age at the time of the neonatal exam was 40.7 weeks (SD ± 0.5). Additionally, we found a statistically significant difference in mean gestational age between the HC and CHD infants at the neonatal time point (t = 5.8, 95%CI: 0.4, 0.9, p < 0.001). Detailed demographic findings can be found in Table 2.
Table 2.
Pre-COVID-19 demographics with descriptive analyses between groups.
| N (%) for both groups | N (%) of CHD infants | N (%) of HC infants | Statistical test | Statistical value | |
|---|---|---|---|---|---|
| Neonatal time point | |||||
| Group Healthy Controls (HC) Congenital Heart Disease (CHD) |
19 (39.6) 29 (60.4) |
||||
| Sex Male Female Missing |
20 (41.7) 25 (52.1) 3 (6.3) |
8 (30.8) 18 (69.2) 0 (0.0) |
12 (63.2) 7 (36.8) 0 (0.0) |
Pearson's χ2 test | χ2 = 4.66⁎ |
| Ethnicity Caucasian Hispanic/Latino Asian/Pacific Islander African American Other Missing |
7 (14.6) 31 (64.6) 2 (4.2) 2 (4.2) 3 (6.3) 3 (6.3) |
3 (11.5) 20 (76.9) 2 (7.7) 1 (3.8) 0 (0.0) 0 (0.0) |
4 (21.1) 11 (57.9) 0 (0.0) 1 (5.3) 3 (15.8) 0 (0.0) |
Fisher's Exact test | χ2 = 6.27 |
| Gestational age at exam (weeks), Mean (±SD)a | 40.7 (±0.5) | 40.5 (±0.3) | 41.1 (±0.4) | T-test | t = 5.76⁎⁎ |
| 3-month time point | |||||
| Group HC CHD |
21 (47.7) 23 (52.3) |
||||
| Sex Male Female |
23 (52.3) 21 (47.7) |
12 (52.2) 11 (47.8) |
11 (52.4) 10 (47.6) |
Pearson's χ2 test | χ2 < 0.01⁎⁎ |
| Ethnicity Caucasian Latino Asian/Pacific Islander Other Missing |
5 (11.4) 30 (68.2) 4 (9.1) 1 (2.3) 4 (9.1) |
1 (4.3) 18 (78.3) 2 (8.7) 1 (4.3) 1 (4.3) |
4 (19.0) 12 (57.1) 2 (9.5) 0 (0.0) 3 (14.3) |
Fisher's Exact test | χ2 = 4.74 |
| 6-month time point | |||||
| Group HC CHD |
16 (40.0) 24 (60.0) |
||||
| Sex Male Female |
17 (42.5) 23 (57.5) |
11 (45.8) 13 (54.2) |
6 (37.5) 10 (62.5) |
Pearson's χ2 test | χ2 = 0.27 |
| Ethnicity Caucasian Latino Asian/Pacific Islander African American Other |
4 (10.0) 27 (67.5) 3 (7.5) 3 (7.5) 3 (7.5) |
2 (8.3) 18 (75.0) 1 (4.2) 2 (8.3) 1 (4.2) |
2 (12.5) 9 (56.3) 2 (12.5) 1 (6.3) 2 (12.5) |
Fisher's Exact test | χ2 = 2.90 |
| 9-month time point | |||||
| Group HC CHD |
10 (33.3) 20 (66.7) |
||||
| Sex Male Female |
11 (36.7) 19 (63.3) |
8 (40.0) 12 (60.0) |
3 (30.0) 7 (70.0) |
Fisher's Exact test | χ2 = 0.29 |
| Ethnicity Caucasian Latino Asian/Pacific Islander African American Other |
3 (10.0) 22 (73.3) 0 (0.0) 3 (10.0) 2 (6.7) |
2 (10.0) 16 (80.0) 0 (0.0) 2 (10.0) 0 (0.0) |
1 (10.0) 6 (60.0) 0 (0.0) 1 (10.0) 2 (20.0) |
Fisher's Exact test | χ2 = 4.02 |
⁎p < 0.05. **p < 0.01.
Gestational age at exam is expressed as mean (±SD), while all other variables are expressed as n (%).
A negative binomial regression analysis of recruitment and assessments at the different COVID-19 time points among the study participants is shown in Table 3 and Fig. 1 . CHD infants were 2.1 times as likely to be recruited into our study pre-COVID-19 compared to during COVID-19 (missed due to COVID-19) (β = 0.8 exponentiated, 95%CI: 1.9, 3.5, p = 0.003). HC infants were 1.8 times as likely to be recruited into the study pre-COVID-19 compared to during COVID-19 (missed due to COVID-19) (β = 0.6 exponentiated, 95%CI: 1.3, 2.5, p < 0.001). Study participants were 3.3 times as likely to have assessments performed pre-COVID-19 (β = 1.2 exponentiated, 95%CI: 2.4, 4.5, p < 0.001) compared to during the COVID-19 pandemic (missed due to COVID-19). CHD infants were 6.6 times as likely to have an assessment performed pre-COVID-19 compared to during COVID-19 (missed due to COVID-19) (β = 1.9 exponentiated, 95%CI: 3.7, 11.5, p < 0.001). HC infants were 1.9 times as likely to have an assessment performed pre-COVID-19 (β = 0.7 exponentiated, 95%CI: 1.3, 2.9, p = 0.001) than during COVID-19 (missed due to COVID-19).
Table 3.
Incidence rate ratios for the associations of recruiting and assessing infants pre-COVID-19 compared to missed due to COVID-19 between groups.
| Variable | Incidence rate ratio | 95% confidence interval | p-value |
|---|---|---|---|
| Recruitment in both groups | 1.2 | 0.9–1.6 | 0.131 |
| Assessment in both groups | 3.3 | 2.4–4.5 | <0.001** |
| Recruitment in infants with CHD | 2.1 | 1.3–3.5 | 0.003** |
| Recruitment in HC infants | 1.8 | 1.3–2.5 | <0.001** |
| Assessment in CHD infants | 6.6 | 3.7–11.5 | <0.001** |
| Assessment in HC infants | 1.9 | 1.3–2.9 | 0.001** |
Note. This table indicates the likelihood of recruiting eligible infants into our study and the likelihood of currently enrolled infants having study assessments performed before March 2020 (pre-COVID) compared to between March 2020 and July 2020 (missed due to COVID-19). For instance, infants in both groups were 3.3 times more likely to be assessed pre-COVID-19 compared to missed due to COVID-19.
a CHD = Congenital Heart Disease. b HC = Healthy Controls.
⁎p < 0.05. ⁎⁎p < 0.01.
Fig. 1.
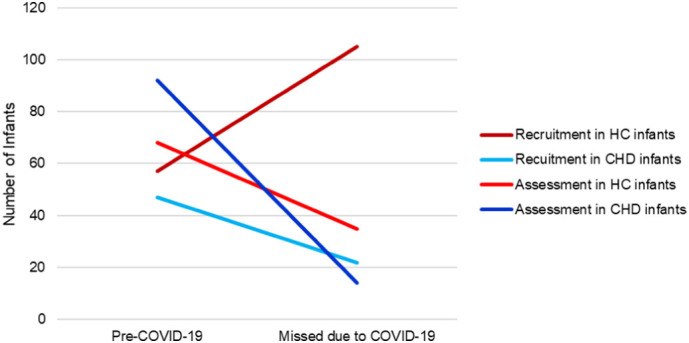
Infant recruitment and assessments at different COVID-19 time points.
Note. This figure depicts the number of infants we recruited and assessed before March 2020 (pre-COVID-19) compared to the number of infants we failed to recruit and assess during March 2020 and July 2020 due to COVID-19 restrictions (missed due to COVID-19).
a CHD = Congenital Heart Disease. b HC = Healthy Controls.
Discussion
We found significantly decreased participant enrollment and follow-up study assessments due to COVID-19. Participants enrolled pre-COVID-19 were less willing to return for their follow-up appointments in fear of unnecessary COVID-19 exposure in the hospital setting. Many of our study participants received care at our institution's specialty clinics and preferred to schedule study assessments on the same day as their clinic visits. Since our institution now provides telehealth visits, many families chose that platform rather than in-person visits. In addition, we could not reschedule many of our missed study assessments as the participants exceeded the age range for that particular assessment time point.
Our results were similar to other studies that described the impact of COVID-19 on research operations and participation. An online survey of 40 oncologists with ongoing clinical trials reported that 35 of the 40 (87.5%) oncologists stopped screening new participants and 25 (62.5%) oncologists stopped recruiting overall (Parikh et al., 2020). Additionally, 11 (27.5%) oncologists reported participant withdrawal from the study due to concerns about COVID-19 (Parikh et al., 2020). We did not experience any participant withdrawals due to COVID-19, but we could not recruit 127 potential participants due to the pandemic. Since we could not recruit 127 potential participants due to COVID-19 and recruited 0 participants within the 4 months of returning to research post-COVID-19, it was clear that the pandemic reduced our enrollment numbers. Furthermore, the number of assessments performed pre-COVID-19 was 27 times higher than the number of assessments performed post-COVID-19.
Other pediatric studies reported similar obstacles to our study due to COVID-19. An online survey asked 91 members of the Pediatric Asthma in Real Life Think Tank and World Allergy Organization Pediatric Asthma Committee around the world to report the challenges they faced in their pediatric asthma clinics due to COVID-19 (Papadopoulos et al., 2020). Seventy-five percent of respondents reported decreased assessments and consultations (half the usual number) during the pandemic (Papadopoulos et al., 2020). A survey asked 34 pediatric oncology centers, in the Middle East, North Africa, and West Asia, about barriers to pediatric oncology management during the pandemic (Saab et al., 2020). Sixty-five percent of respondents indicated that patients canceled their off-therapy visits and 47% of respondents indicated that patients refused to come in for essential visits due to fear of contracting the virus (Saab et al., 2020). Thus, the number of clinical and research visits decreased because parents did not want to expose their vulnerable children to COVID-19.
However, the COVID-19 pandemic did not affect other researchers as they retained enrollment rates similar to the pre-pandemic rates. These investigators modified their protocols for recruitment and data collection to accommodate the new COVID-19 restrictions. Some examples of recruitment methods included online recruiting through social media platforms and digital health media, and obtaining informed consent remotely (Gaba & Bhatt, 2020; Singh & Chaturvedi, 2020). New data collection methods can include in-home visits or virtual monitoring instead of the traditional visits to the research lab (Gaba & Bhatt, 2020; Singh & Chaturvedi, 2020; Weiner et al., 2020). Specifically, researchers conducted visits remotely, incorporated home-based monitoring technologies, and provided delivery or curbside pickup for samples or products (Tuttle, 2020). Aside from minimal virtual recruitment, we have not yet incorporated those types of technologies into our study. Many of these changes to protocol require additional financial resources, which are limited in our project. We are in the process of applying for more research funding to implement some of these measures.
Institutions and researchers enforced strict health precautions and protocols to prevent and reduce exposure to COVID-19, giving participants the option of an in-person or remote visit in July 2020 after re-opening in-person research visits (Tuttle, 2020). Many research studies have had success with participation after the implementation of these new safety protocols. An ongoing study at Geriatric Research Education and Clinical Center reported that 40 of the 51 participants scheduled during the COVID-19 pandemic reported feeling safe coming in for their research appointments (Padala et al., 2020). Furthermore, their participants stated the medical center was safe and prepared because of the implementation of COVID-19 screenings (Padala et al., 2020). Although the participants in this study were also considered a high-risk group, they had the opportunity to consult with their caregivers and family before deciding to come in for their appointments (Padala et al., 2020). In contrast, when we began to contact families to in July 2020, mothers immediately refused to return for our study assessments, due to their concern of exposing their infant to COVID-19, without consultation with the infant's father or other family members. It is unknown if the mother's decisions would have changed after speaking with other family members, but it seemed to help other researchers. Thus, the target population may play a role in the enrollment and participation rates during and after the pandemic.
Clinical implications
Research studies must modify their protocols and procedures to accommodate COVID-19 precautions and a changing research environment. In order to accommodate physical distancing recommendations, essential research staff are required to work restricted hours with either split schedules or staggered shifts (Omary et al., 2020). We have adjusted the total number of persons allowed in our shared lab at one time and are limited to one study assessment per day. Recruitment activities have been altered to virtual meetings or telephone calls. Other researchers have created recruitment videos or instructional videos for data/specimen collection (Brezing et al., n.d; Izmailova et al., n.d). In order to continue to have successful recruitment and retention, researchers must be flexible and adjust their protocols to accommodate the new COVID-19 era.
Our institution introduced re-entry and recovery plans for researchers in early July 2020. In our study specifically, the suspension of study assessments interrupted our ability to perform neurodevelopmental exams and refer participants to the Regional Centers for possible early intervention services, if applicable. Therefore, those infants affected by CHD may not have received the necessary screening and referrals for interventions to improve their development and future quality of life. Pre-COVID-19, families preferred to schedule a research appointment on the same day that they had a clinical visit. However, since most clinics offered telehealth visits, parents were less likely to come in-person for a research appointment or non-essential hospital visit. To help ease their concerns, we emphasized the safety of the research visits with: (1) wearing personal protective equipment; (2) routine hand hygiene; (3) assessment performed in a private room in a building across the street from the hospital; (4) and following hospital regulations, including COVID-19 screenings and using standard precautions. These actions have facilitated our follow-up study assessments.
Limitations
Our study had a few limitations. We could not determine how our recruitment and assessments were affected post-COVID-19 compared to during COVID-19 (missed due to COVID-19) and pre-COVID-19 as we were unsuccessful in recruiting and assessing eligible infants from July to August 2020 when stay-at-home restrictions were loosened. Another limitation is the assumption that our sample size was large enough to use negative binomial regression. We believe we had a sufficient sample size, since we detected significant differences between timeframes. In addition, the precision of our results might be compromised as the use of negative binomial regressions indicated that we had overdispersion in our data; variances were much larger than the means. Nevertheless, our results shed light on how the COVID-19 pandemic has impacted pediatric clinical research.
Conclusion
The COVID-19 pandemic greatly impacted our study with a drastic decrease in participant recruitment and assessment. Alternative or contingency plans, e.g., virtual or telephone recruitment and visits, may be beneficial for researchers (who have the financial and personnel means) to implement these types of changes immediately. The restrictions on study progress can negatively impact investigators by limiting their ability to collect data in their projected timeframe or may be harmful to the participant who may need the life-saving investigative treatment. Investigators must be flexible and be able to quickly adapt to the constraints caused by the COVID-19 pandemic. For the foreseeable future, modifying protocols to the changing environment of the COVID-19 pandemic will facilitate the progress of research and patient outcomes.
Declarations of Competing Interest
None.
Author statement
N.T. conceived of the idea for the manuscript. M.T. performed and wrote the methods, statistical analyses, and results. J.L. wrote the introduction and discussion. J.W. wrote the abstract and highlights. J.N. revised and edited the manuscript. M.B. verified the analytical methods and supervised the findings and revisions of this work. N.T. performed the final revisions and edits. All authors discussed the results and contributed to the final manuscript.
Acknowledgments
This study was supported by Children's Hospital Los Angeles Clinical Services Research Grant and SC CTSI (NCATS) through Grant UL1TR0001855. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
References
- Asaad M., Habibullah N.K., Butler C.E. The impact of COVID-19 on clinical trials. Annals of Surgery. 2020;272(3):e222–e223. doi: 10.1097/SLA.0000000000004113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brezing, C. A., Luo Sx Fau, Mariani, J. J., Mariani Jj Fau, Levin, F. R., & Levin, F. R. Digital clinical trials for substance use disorders in the age of Covid-19. (1935–3227 (Electronic)). [DOI] [PMC free article] [PubMed]
- Colbert L.E., Kouzy R., Abi Jaoude J., Ludmir E.B., Taniguchi C.M. Cancer research after COVID-19: Where do we go from Here? Cancer Cell. 2020;37(5):637–638. doi: 10.1016/j.ccell.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan J., Liu X., Pan W., Douglas M., Bao S. Epidemiology of coronavirus disease in Gansu Province, China, 2020. Emerging Infectious Disease Journal. 2020;26(6):1257. doi: 10.3201/eid2606.200251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaba P., Bhatt D.L. The COVID-19 pandemic: A catalyst to improve clinical trials. Nature Reviews. Cardiology. 2020;17(11):673–675. doi: 10.1038/s41569-020-00439-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghebreyesus T. 2020. WHO director-General’s opening remarks at the media briefing on COVID-19 - 11 march 2020. [Google Scholar]
- Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H.…Pillai S.K. First case of 2019 novel coronavirus in the United States. The New England Journal of Medicine. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izmailova, E. S., Ellis, R., & Benko, C. Remote monitoring in clinical trials during the COVID-19 pandemic. (1752–8062 (Electronic)). [DOI] [PMC free article] [PubMed]
- de Miguel M., Doger B., Boni V., Hernández-Guerrero T., Moreno I., Morillo D., Moreno V., Calvo E. Increased vulnerability of clinical research units during the COVID-19 crisis and their protection. Cancer. 2020;126(17):3907–3911. doi: 10.1002/cncr.32980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omary M.B., Eswaraka J., Kimball S.D., Moghe P.V., Panettieri R.A., Jr., Scotto K.W. The COVID-19 pandemic and research shutdown: Staying safe and productive. The Journal of Clinical Investigation. 2020;130(6):2745–2748. doi: 10.1172/JCI138646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omary M.B., Hassan M. Opinion: Here’s how we restore productivity and vigor to the biomedical research workforce in the midst of COVID-19. Proceedings of the National Academy of Sciences. 2020;117(33):19612. doi: 10.1073/pnas.2014730117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padala P.R., Jendro A.M., Padala K.P. Conducting clinical research during the COVID-19 pandemic: Investigator and participant perspectives [viewpoint] JMIR Public Health and Surveillance. 2020;6(2) doi: 10.2196/18887. e18887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papadopoulos N.G., Custovic A., Deschildre A., Mathioudakis A.G., Phipatanakul W., Wong G.…Zar H.J. Impact of COVID-19 on pediatric asthma: practice adjustments and disease burden. The Journal of Allergy and Clinical Immunology. In Practice. 2020;8(8):2592–2599. doi: 10.1016/j.jaip.2020.06.001. e2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parikh P., Mehta P., Krishna Kumar M.V.T., Govind Babu K. Clinical trials facing “serious adverse events” during the ongoing COVID-19 pandemic [original article] Indian Journal Medical and Paediatric Oncology. 2020;41(3):295–298. doi: 10.4103/ijmpo.ijmpo_173_20. [DOI] [Google Scholar]
- Saab R., Obeid A., Gachi F., Boudiaf H., Sargsyan L., Al-Saad K.…Jeha S. Impact of the coronavirus disease 2019 (COVID-19) pandemic on pediatric oncology care in the Middle East, North Africa, and West Asia region: A report from the Pediatric Oncology East and Mediterranean (POEM) group. Cancer. 2020;126(18):4235–4245. doi: 10.1002/cncr.33075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A.G., Chaturvedi P. Clinical trials during COVID-19. Head & Neck. 2020;42(7):1516–1518. doi: 10.1002/hed.26223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes E., Zambrano L., Anderson K., Marder E., Raz K., Felix S.…Fullerton K. Vol. 69. 2020. Coronavirus disease 2019 case surveillance — United States, January 22–may 30, 2020; pp. 759–765. external icon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuttle K.R. Impact of the COVID-19 pandemic on clinical research. Nature Reviews. Nephrology. 2020;16(10):562–564. doi: 10.1038/s41581-020-00336-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner D.L., Balasubramaniam V., Shah S.I., Javier J.R., on behalf of the Pediatric Policy, C COVID-19 impact on research, lessons learned from COVID-19 research, implications for pediatric research. Pediatric Research. 2020;88(2):148–150. doi: 10.1038/s41390-020-1006-3. [DOI] [PubMed] [Google Scholar]


