Abstract
Millions of Americans live with dementia. Caregivers of this population provide countless hours of multifaceted, complex care that frequently cause unrelenting stress which can result in immense burden. However, it is not fully understood what efforts can be made to reduce the stress among caregivers of persons with dementia (PWD). Therefore, the aim of this pretest–posttest designed study was to evaluate changes in caregiver burden after providing an educational intervention to those caring for PWD in Arkansas. Forty-one participants completed the Zarit Caregiver Burden Scale before and after attending a 4-hour dementia-focused caregiving workshop. The analysis of the means, standard deviations, and paired t tests showed that there was an increase in the confidence and competence in caring for PWD 30 to 45 days after attending the workshop. Health care providers need to understand both the vital role caregivers provide in managing a PWD and the importance of the caregiver receiving education about their role as a caregiver. Utilizing caregiver educational programs is a first step.
Keywords: caregiving, caregiver burden, dementia, caregiver tools
Introduction
Dementia is the sixth leading cause of death in the United States and in Arkansas (1). Arkansas had over 58 000 citizens living with dementia in 2020 and approximately 80% of those were living at home. The Alzheimer’s Association (2020) reported that about 452 000 family caregivers in Arkansas provide unpaid care each year for a loved one and most provide this care without adequate education. In addition, the support services for these individuals in Arkansas are very minimal. Although short-term respite stays in senior living facilities, nursing homes, and in-home are available, they are very limited and most are private pay and not affordable for many families. Free Dementia Caregiver Workshops, offered by the research team and partnering organizations, seek to fill a knowledge gap by providing caregivers with tips that focus on how to maintain the respect, dignity, and quality of life for the person living with dementia (PWD), while helping to reduce the stress and burden of the caregiver.
So what is caregiver burden? To understand caregiver burden, it is important to understand the role of a family (or informal) caregiver. Informal caregivers are the unpaid family and friends who supervise, coordinate, assist with, or provide direct care and services on a regular basis. This includes tasks such as meal preparations, driving, bill paying, household and yard chores, care management, phone contacts, personal hygiene, listening, and general companionship. In many scenarios, caregivers are providing these care duties in addition to working full- or part-time and having responsibilities for their own family.
Caregiver burden is an all-encompassing term used to describe the physical, emotional, and financial toll of providing care (2). It is the subjective stress perceived by the caregiver in his or her situation and no caregiver is immune to the possibility of experiencing some form of burden. When evaluating husbands and wives as caregivers, Zarit and his colleagues defined it as “The extent to which caregivers perceive that caregiving has had an adverse effect on their emotional, social, financial, physical and spiritual function” (p. 261) (3). Gillick emphasized the multidimensional toll caregiving can place on the care providers and stressed that caregiving is a highly individualized experience (4). Caregivers, just like all individuals, have different thresholds for what constitutes an adverse stressor or burden.
Literature Review
As the population of Americans living with dementia increases, the burden of caring for that population also increases. According to the 2020 Alzheimer’s and Dementia Report, the current 5.8 million Americans living with dementia (1) is expected to increase to over 15 million by 2050 (5). Approximately 20% are living in nursing or assisted-living homes (6) and almost 80% live in the community with care provided by family or friends. Therefore caregivers of PWD are frequently forced to assume roles that have considerable responsibility (6,7) often leading to heavy burdens (5). The burnout impact can be psychological, physical, spiritual and/or financial and therefore, caregiver burden is considered to be very complex and multidimensional (8). The burden of caring for a PWD can carry significant consequences for informal caregivers which thus also impacts the individual with dementia and even society as a whole (5,9). Furthermore, a PWD having behavioral issues such as irritability, agitation, and wandering (5) can cause an increased rate of morbidity and mortality for both the PWD and the caregiver (7).
Community-dwelling PWDs are usually cared for by informal caregivers. According to the National Academies of Sciences, Engineering, and Medicine (10), at least 17.7 million individuals in the United States are caregivers of an older adult, and according to the National Center on Caregiving (11), women provide nearly 75% of caregiving support in the United States, most of whom are unpaid informal caregivers. These are caregivers such as family members or friends and they provide most of the assistance and supervision of care that are necessary to fulfil the basic needs of the PWD (5) including bathing, dressing, and meal preparation (9). However, most caregivers lack caregiving knowledge and have limited exposure to care-related training (1,5) which can lead to more burden for the caregiver.
Caregiver burden can lead to exhaustion, loss of control, stress, chronic disease, loss of self-identity, withdrawal from family and friends, and substance abuse (11). Those caring for someone with dementia have shown stress and burnout with high prevalence of clinical depression and anxiety (7). Furthermore, depressed caregivers are more likely to have coexisting anxiety disorders, alcohol use disorder, and/or chronic diseases such as diabetes, heart disease, and ulcers (1,9,12). Studies also show caregivers who experience chronic stress and frustration may be at greater risk for cognitive decline themselves including short-term memory loss and low verbal IQ (7,6). For example, a woman providing at least 9 hours of care to her spouse with dementia has a 2-fold risk of heart disease (11), and those women who are aged 66 to 69 years who experience chronic caregiving stress have a 63% higher mortality rate than noncaregivers of the same age (9,11,13).
Studies show evidence supporting that caregiver training can reduce overall caregiver burden, yet according to the Center for Disease Control (12) only 1 in 5 caregivers report receiving training. Baharudin et al (7) found specific coping strategies should be included in caregiver training including self-distraction, active coping, planning, and acceptance, all of which were demonstrated to have a mediation effect on the relationship between the behavioral and psychological symptoms of a PWD and caregiver burden. Baharudin et al (7) also noted that caregiver burnout was reduced when problem-focused and action-oriented coping skills were emphasized within caregiver training sessions. Furthermore, research and caregiver training priorities have been determined to include psychoeducation, training in psychological strategies and skills, professional support with an online forum, and discussions via support groups with others (14,15). Access to educational resources related to caregiving of PWD is vital to a more efficient, healthy routine for the caregiver and the PWD (5).
Caregiver Dementia Workshop
The Arkansas Geriatric Education Collaborative (AGEC) recognizes this immense pressure and burden on caregivers and the need for high-quality programs to improve their interventions, skills, and coping strategies. One of the goals of AGEC, a federally funded Health Resources and Services Administration Geriatric Workforce Enhancement Program, is to educate family caregivers about dementia and the best practices involved in the care of their loved ones. The program reaches this goal by teaching a free community program that provides education and resources to family caregivers.
The caregiver dementia workshop is a half-day workshop offered throughout rural Arkansas and covers many facets of dementia and caregiving. It begins with a review of dementia and Alzheimer’s disease. It is critical that caregivers understand dementia and the expected progression through stages. They also need to understand how multifaceted caregiving is and why it can be a hidden burden. Basic rules of caregiving are reviewed and time is spent in assisting the participants to understand the changes in physical functions and behaviors that occur with a PWD. They are taught various techniques about how to respond or adjust to the altered behaviors and needs of the PWD with patience, care, and safety. Time is spent role playing various verbal and physical communication approaches.
They are also given information about expectations regarding how they may feel as a caregiver, details about caregiver stress, and the importance of self-care. Caregivers must understand that they are not only a care provider, but a care or case manager, a source for medical and financial information, an advocate, an emotional supporter, the housekeeper, the cook, the deliverer of medication, and a behavioral analyst. They are provided with tips about how to manage each of their roles, and how to care for themselves. Ample time is also allowed to discuss alternative options for caregiving such as respite, paid caregivers, residential dementia specialty units, and nursing homes. They are provided with printed and virtual resources to refer to later. Finally, the participants are encouraged to have important health, personal, and financial papers available regarding the PWD as well as their legal documents prepared such as general and medical powers of attorney, a living will, and any necessary estate plans.
Methods
This was an institutional review board approved (#228441) pretest–posttest designed study completed by the AGEC at the University of Arkansas for Medical Sciences. We wanted to know if the tools and skills that were taught in the workshops were effective in reducing the burden for the caregiver. Convenience sampling was used as participants were recruited from regularly scheduled caregiver workshops throughout the state of Arkansas. Individuals who registered for the workshops were informed about this study prior to attending the workshop via verbal and written documents. The criteria for inclusion were that participants age be ≥18 years, he or she had to be a caregiver of an individual with dementia, had a phone for follow-up contact, and had the ability to read and write. Exclusion criteria included the inability to understand/complete the informed consent form or did not attend the entire workshop. Participants were excluded at the time of the workshop if they did not meet the criteria after a review of the criteria with them by the trained instructor. The participants were recruited from clinical and community partners. Flyers were posted in community centers, senior centers, and clinic waiting rooms, emails announcing the workshops were sent out from community partners to their listserv, and the workshops and study opportunity were posted on the research group’s website and Facebook page. Interested individuals called the research group or their partner to register.
Participants were provided a verbal explanation of the study and consent process along with a letter of explanation and the informed consent form. After obtaining informed consent, they were asked to complete the pretest which was a 12-item questionnaire, the Zarit Burden Interview (ZBI). The completed questionnaires were then coded for anonymity and data were entered into SPSS by a trained research assistant.
The data collection tool, the short ZBI (ZBI-12) consists of 12 questions in 2 main domains, personal strain and role strain and 4 subscales of sacrifice/strain, inadequacy, embarrassment/anger, and loss of control. Scoring of the item responses are based on a 5-point Likert-type scale ranging from 0 = never, 1 = rarely, 2 = sometimes, 3 = quite frequently, and 4 = nearly always. A cumulative score of 48 is possible and the higher scores represent higher feelings of burden. The ZBI-12 classifies cumulative scores 0 to 10 as “no to mild burden,” 10 to 20 as “mild to moderate burden,” and scores above 20 as “high burden.” The ZBI-12 has been validated in its use with caregivers of those with cognitive impairment and the relations between the short and the full version showed that the measure had good internal consistency reliability with a Cronbach’s α coefficient of 0.92 to 0.97, and a 2-way analysis of variance found that the short version produced almost exact results of the full version (16). Therefore, the ZBI-12 was chosen for this study since it produces comparable results to those of the full version and leads to easier administration and completion of the questionnaire.
After the participants completed the pretest, they attended the workshop as described in the “Caregiver Dementia Workshop” section above. The initial participant questionnaires were assigned coded numbers when they were transferred from paper copies to the database. The follow-up posttest, the exact same ZBI-12, was administered over the phone by a trained research assistant 30 to 45 days after the workshop and then entered into the database using the same codes. The pretest and posttest responses were matched by their assigned codes by the data analyst. The goal was to evaluate changes in caregiver burden after the educational intervention. The survey was anonymous but contact information and basic demographic data on age, gender, race, and ethnicity were collected.
Results
The matched pre- and posttest survey (ZBI) data from 41 respondents were used for the descriptive analysis. Eighty-three percent were women, and the ages ranged from 30 to 79 years. Twenty-seven percent (n = 11) were 50 to 59 years old and a few (12%, n = 5) were younger than 50 years. More than a third of the respondents (68%, n = 28) identified as white/Caucasian, 20% (n = 8) as African-American/black, and 12% (n = 5) were of various ethnicities (Asian, American Indian, Alaska Native, and more than one race).
Knowledge and confidence level: After attending the workshop, the participants increased both their levels of knowledge and confidence in caregiving. Comparisons of the pretest versus posttest (mean ± standard deviation) for the knowledge level rose from 2.78 ± 0.79 to 3.98 ± 0.65 and for the confidence level from 3.02 ± 0.91 to 4.02 ± 0.72.
Likewise, the paired samples t test showed a significant increase in the posttest means for both the caregiver’s knowledge level, t(40) = −7.61, P = .001, α = 0.95, and confidence level, t(40) = −5.845, P = 0.001, α = 0.95. The Cohen’s d values indicated a large effect size in the 2 variables: knowledge (d = 1.656) and confidence (d = 1.218) suggesting that participation in the workshop was beneficial to the improvement of these 2 caregiving attributes.
For the pretest, the ZBI total scores (refer to Table 1) ranged from 7 to 47, while the posttest scores ranged from 4 to 31. The higher ZBI total scores in the pretest suggested the participants’ higher family caregiver burden perception. In contrast, the lower posttest scores after the workshop indicated an improvement and a positive effect on the participant’s family caregiver burden perception. Similarly, the paired samples t test scores showed a statistically significant change between the pretest and posttest values, t(38) = 6.97, P = .0001, α = 0.95, of the ZBI total perception score means. This change was also evident in the large effect size of the Cohen’s d = 0.78.
Table 1.
Zarit Burden Interview survey results.a,b
| Mean ± SD | P ≤ .05 | Cohen’s d | ||
|---|---|---|---|---|
| Question | Pre | Post | ||
| Sacrifice/strain | ||||
| Do you feel that because of the time you spend with your relative that you don’t have enough time for yourself? | 1.79 ± 1.00 | 2.05 ± 1.02 | .040c | 0.257 |
| Do you feel stressed between caring for your relative and trying to meet other responsibilities for your family or work? | 2.21 ± 0.83 | 2.15 ± 1.14 | .744 | 0.060 |
| Do you feel strained when you are around your relative? | 1.58 ± 0.98 | 1.18 ± 1.04 | .005c | 0.397 |
| Do you feel that your health has suffered because of your involvement with your relative? | 1.13 ± 1.17 | 1.33 ± 1.20 | .198 | 0.168 |
| Do you feel that you don’t have as much privacy as you would like because of your relative? | 1.24 ± 1.24 | 1.11 ± 1.27 | .360 | 0.104 |
| Do you feel that your social life has suffered because you are caring for your relative? | 1.51 ± 1.23 | 1.56 ± 1.29 | .762 | 0.039 |
| Inadequacy | ||||
| Do you feel you should be doing more for your relative? | 2.31 ± 0.89 | 2.03 ± 1.18 | .054c | 0.267 |
| Do you feel you could do a better job in caring for your relative? | 2.38 ± 0.91 | 2.00 ± 1.00 | .017c | 0.398 |
| Embarrassment/anger | ||||
| Do you feel angry when you are around the relative? | 1.29 ± 0.96 | 0.89 ± 0.92 | .020c | 0.425 |
| Do you feel that your relative currently affects your relationships with other family members or friends in a negative way? | 1.23 ± 1.01 | 1.31 ± 1.00 | .696 | 0.079 |
| Loss of control | ||||
| Do you feel that you have lost control of your life since your relative’s illness? | 1.44 ± 1.29 | 1.51 ± 1.32 | .653 | 0.053 |
| Do you feel uncertain about what to do about your relative? | 2.23 ± 1.01 | 1.77 ± 1.09 | .009c | 0.438 |
Abbreviation: SD, standard deviation.
a Pre- and posttest means ± SD, and P ≤ .05 of the Zarit Burden Interview questions (n = 39).
b Scale: 0 = never, 1 = rarely, 2 = sometimes, 3 = quite frequently, and 4 = nearly always.
cStatistically significant at the 95% significance level.
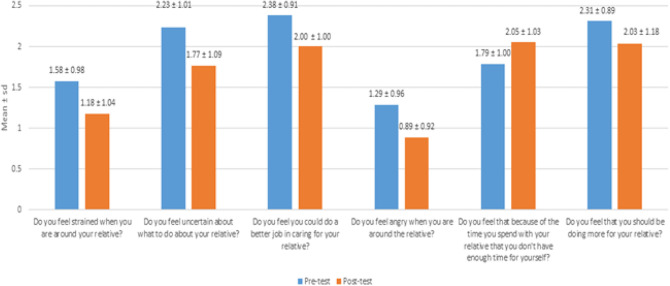
In 6 of the 12 statements asked in the ZBI-12 survey, participants indicated statistically significant improvements on the following subscales: 2 each for the sacrifice/strain and inadequacy subscale and 1 each for the embarrassment/anger and loss of control subscale. Figure 1 indicates the improvements in 6 of the 12 ZBI measures, pretest versus posttest. In order of significance relative to the paired t test results at the 95% significance level, Figure 1 displays the statements that showed the best improvements for the participants. The Cohen’s d values ranged from 0.257 to 0.438, indicating a small to medium effect size for these 6 questions.
Figure 1.
Improved ZBI measures, pretest versus posttest mean ± SD. SD indicates standard deviation; ZBI, Zarit Burden Interview.
Discussion
Caregiver burden is described in many ways, but in summary it is the mental, emotional, and physical state of exhaustion when caring for someone else. A caregiver can begin the day or week being positive and upbeat but after a while, they can become depressed and even apathetic not just about their own personal health but the health of their loved one as well. The work is hard and seemingly never ending. The stress of spending their time, energy, and money providing care takes a monumental toll on the most dedicated caregiver. They need help. As has been previously demonstrated in studies of those individuals caring for a PWD, interventions including educating the caregivers have been shown to increase caregiver knowledge, decrease depression and improve their moods, reduce stress, and even delaying nursing home placement for the PWD (8,17,18).
The results from this study support the idea that providing appropriate information in a manner that is easily understood and translated to their everyday tasks of caregiving can make a big difference. Most caregivers do not understand the basics of dementia such as memory loss that disrupts daily life and causes problems and confusion such as when a PWD tries to brush his teeth without first applying toothpaste to the toothbrush. Caregivers also do not know how to deal with some of the nuances that come with an individual with dementia. Providing them with information and simple, yet effective tools and tips, was shown to not only improve their knowledge about caregiving, but also improve their confidence in caring for their loved one. Knowing why their loved one may seem to be acting out, have a significant change in personality, or suddenly start using curse words or not caring how they look or smell means that the caregiver is usually more tolerant and looks for ways to adapt rather than becoming stressed or angry. Just the simple skill of knowing to agree with their loved one versus trying to correct them or to orient them can be huge. It can mean the difference between a pleasant or a belligerent evening. Seeking to understand the reality and feelings of their loved one, keeping a normal-toned, respectful voice and avoiding embarrassing their loved one are all skills that can help to avoid unpleasant situations and allow reduced overall caregiver stress.
Becoming overwhelmed while caregiving happens quickly and often the family ends up in a crisis mode. Skills learned in these workshops have been shown to help the caregiver know what to do and when to do it. Knowing how to respond in certain situations can mean the difference between the PWD being able to remain at home or having to live in a residential facility or between having a pleasant bath time or a battle during a bath thus creating more opportunities for stress, anger, or even a devastating fall. This is consistent with the findings of a meta-analysis completed by Brodaty et al almost 20 years ago when they found a significant effect of interventions, including education, on caregiver burden, knowledge/abilities, psychological, and subjective well-being of the health of caregivers of those with dementia (17).
Instilling in caregivers the importance of taking a respite break, the importance of maintaining their own personal health and educating caregivers about how their good health equates to providing the best possible care for the PWD is essential. Note that the participants in the study were not tested on their baseline dementia knowledge or knowledge gained after the educational intervention. However, the significant improvement in caregiver stress burden after attending the workshop clearly indicates that the practical caregiving skills and key educational information provided about dementia were very beneficial for the caregivers.
Besides the mental, emotional, and physical toll caregiving has on the caregiver, caregiving can also impact the health of the caregiver, and they need to know when to ask for help. Knowing the warning signs like feeling betrayed, anxious, or even physical body aches from frequent exhaustion allows the caregiver to recognize when additional help is needed. In the caregiver workshop, the value of taking a respite from caregiving is emphasized and they are provided information about various respite grants that might be available to them. Knowing that they are not alone in this journey of caregiving and that there are numerous resources available might also have provided greater reassurance and security.
Although not part of the formal study, participants’ verbal comments made after the workshop and during the follow-up phone calls were very positive. Many stated how they enjoyed the class, learned new information, and how they incorporated the new information into daily caregiving. They also shared about how they were using their new skills to have positive conversations and interactions with other caregivers, thus further increasing their knowledge and confidence of caring for their loved one.
Limitations
A limitation to this study was the use of a single group pretest–posttest design which resulted in a small sample size of matched participants. Not all participants who initially consented to be in the study were available or willing for a follow-up posttest within the 15-day period (30-45 days after the workshop) as outlined in the study protocol. Therefore, there were only 41 participants. The use of self-report questionnaires was also a limitation. It is never known how honest participants are in reporting or understanding of the questions asked.
Conclusions
The half-day workshops in this study were successful and demonstrated that caregivers of patients with dementia can be empowered through education which can reduce their caregiver burden. The ZBI-12 questionnaire results suggested the positive contribution of the workshop in helping ease the caregivers’ burden in 6 of the 12 variables in the survey. The burden of stress associated with caregiving is often underappreciated by health care providers. If caregivers are equipped with core dementia knowledge and are skilled in nonpharmacological management, it could go a long way toward improving the care of the PWD at home and could potentially reduce unnecessary trips to the clinic, emergency room, and premature admission to a long-term care facility. It is also noted that more research in this area could better inform health care providers and educators about how to further reduce the burden of caregivers of PWD. Clinical programs and communities should therefore give serious consideration to investing in more research and caregiver education to promote a healthier caregiver workforce and to ensure a better quality of life for both the PWD and their caregivers.
Acknowledgments
We thank our community partners, including the UAMS Centers on Aging, for their assistance in gathering preliminary data. This work was supported by the Health Resources and Services Administration’s Geriatric Workforce Enhancement Program under grant #U1QHP28723.
Author Biographies
Robin E. McAtee, PhD, RN is an assistant professor in the department of Geriatrics at the Reynolds Institute on Aging, College of Medicine, at the University of Arkansas for Medical Sciences. She has extensive experience in nursing, management, research, teaching, evaluation, and leadership. She is currently the Director of the Arkansas Geriatric Education Collaborative, a Geriatric Workforce Enhancement Program grant from HRSA and the evaluator on a Administration for Community Living grant through the Arkansas Department of Human Services.
Laura Spradley, MS is Outreach Coordinator for the Arkansas Geriatric Education Collaborative (AGEC) at the University of Arkansas for Medical Sciences (UAMS). She has a background in dietetics and has over 30 years of healthcare management experiences in education and training.
Leah Tobey, PT, DPT, MBA is a graduate of Ouachita Baptist University, The University of Central Arkansas with a doctorate in physical therapy, and lastly, The University of Arkansas at Little Rock with an M.B.A. She joined the University of Arkansas for Medical Sciences (UAMS) in 2013 and has 11 years of clinical PT experience treating in the areas of orthopedics, geriatrics, and pelvic floor rehab. She continues PT in the UAMS Interventional Pain Dept. and is the clinical coordinator for the Arkansas Geriatric Education Collaborative (AGEC) at UAMS.
Whitney Thomasson, MAP is the research assistant for the Arkansas Geriatric Education Collaborative (AGEC) at the University of Arkansas for Medical Sciences. She is a graduate of The University of Arkansas at Little Rock with a Masters of Applied Psychology, with an emphasis in Industrial/Organizational Psychology.Gohar Azhar, MD is a clinician-scientist and a Professor of Geriatrics at the Reynolds Institute on Aging, College of Medicine, at UAMS with expertise in both basic and clinical research. Currently, she is the Director of the Pat Walker Memory Center, Director of Clinical Research and Co-Director of the Cardiovascular Aging Program. Her clinical research involves the study of heart failure in the elderly, memory disorders, frailty, centenarians and caregiver stress.
Cynthia C. Mercado, EMBA, MA is a Research Assistant in the Office of Medical Education, University of Arkansas for Medical Sciences. She has an MBA and a Masters in Gerontology. She conducts surveys, assessments, and qualitative evaluations in medical education and collaborates with the Arkansas Geriatric Education Collaborative (AGEC) in their various project studies.
Authors’ Note: This study was approved by the University of Arkansas for Medical Sciences (UAMS) Institutional Review Board (#228441). All procedures in this study were conducted in accordance with the UAMS Institutional Review Board approved protocols. Written informed consent was obtained from the participants for their anonymized information to be published in this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Whitney Thomasson, MAP  https://orcid.org/0000-0002-0043-4154
https://orcid.org/0000-0002-0043-4154
References
- 1. Alzheimer’s Association, Alzheimer’s & Dementia. 2020 Alzheimer’s disease facts and figures. Alzheimers Dement. 2020. doi:10.1002/alz.12068. Accessed March 29, 2021. [Google Scholar]
- 2. George LK, Gwyther LP. Caregiver well-being: a multidimensional examination of family caregivers of demented adults. Gerontologist. 1986;26:253–59. [DOI] [PubMed] [Google Scholar]
- 3. Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: a longitudinal study. Gerontologist. 1986;26:260–66. [DOI] [PubMed] [Google Scholar]
- 4. Gillick MR. The critical role of caregivers in achieving patient-centered care. JAMA. 2013;310:575–76. [DOI] [PubMed] [Google Scholar]
- 5. Chiao CY, Wu HS, Hsiao CY. Caregiver burden for informal caregivers of patients with dementia: a systematic review. Int Nurs Rev. 2015;62:340–50. doi:10.1111/inr.12194 [DOI] [PubMed] [Google Scholar]
- 6. Lepore M, Ferrell A, Wiener J. Living arrangements of people with Alzheimer’s disease and related dementias: implications for services and supports. Report, Research Summit on Dementia Care: Building Evidence for Services and Supports, October 2017.
- 7. Baharudin A, Che Din N, Subramaniam S. The associations between behavioral-psychological symptoms of dementia (BPSD) and coping strategy, burden of care and personality style among low-income caregivers of patients with dementia. BMC Public Health. 2019;19:447. doi:10.1186/s12889-019-6868-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Selwood A, Johnston K, Katona C, Lyketsos C, Livingston G. A systematic review of the effect of psychological interventions on family caregivers of people with dementia. J Affect Disord. 2007;101:75–89. [DOI] [PubMed] [Google Scholar]
- 9. Schulz R, Eden J. Family caregiving roles and impacts. Family Caring for an Aging America. National Academies Press; November 2016. Accessed May 7, 2021. Report. https://www.ncbi.nlm.nih.gov/books/NBK396398// [PubMed] [Google Scholar]
- 10. Fordyce M. National Center on Caregiving. Caregiver Health. 2009 National Policy Statement. Report, Family Caregiver Alliance; 2009. [Google Scholar]
- 11. Roth DL, Fredman L, Haley WE. Informal caregiving and its impact on health: a reappraisal from population-based studies. Gerontologist. 2015;55:309–19. doi:10.1093/geront/gnu177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Center for Disease Control and National Association of Chronic Disease Directors. Caregiving for family and friends: a public health issue. 2018. Accessed May 7, 2021. https://www.cdc.gov/aging/agingdata/docs/caregiver-brief-508.pdf/
- 13. Brodaty H. Family caregivers of people with dementia. Dialogues Clin Neurosci. 2009;11:217–28. Accessed May 7, 2021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181916/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Etxeberria I, Salaberria K, Gorostiaga A. Online support for family caregivers of people with dementia: a systematic review and meta-analysis of RCTs and quasi-experimental studies. Aging Ment Health. 2020;2:1–16. doi:10.1080/13607863.2020.1758900 [DOI] [PubMed] [Google Scholar]
- 15. Harvath TA, Mongoven JM, Bidwell JT, Cothran FA, Sexson KE, Mason D, et al. Research priorities in family caregiving: process and outcomes of a conference on family-centered care across the trajectory of serious illness. Gerontologist. 2020;60:S5–S13. doi:10.1093/geront/gnz138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, O’Donnell M. The Zarit Burden Interview: a new short version and screening version. Gerontologist. 2001;41:652–57. doi:10.1093/geront/41.5.652 [DOI] [PubMed] [Google Scholar]
- 17. Brodaty H, Green A, Koschera A. Meta-analysis of psychosocial interventions for caregivers of people with dementia. J Am Geriatri Soc. 2003;51:657–64. [DOI] [PubMed] [Google Scholar]
- 18. Pinquart M, Sorensen S. Helping caregivers of persons with dementia: which interventions work and how large are their effects? Int Psychogeriatr. 2006;18:577–95. doi:10.1017/S1041610206003462 [DOI] [PubMed] [Google Scholar]