Abstract
Outpatient clinics are an important part of chronic disease management, including that of celiac disease. During the coronavirus disease 2019 (COVID-19) global pandemic, telephone and online video consultations with health care professionals have substantially increased. This study aimed to explore the experience and opinions of adults, with celiac disease, toward face-to-face clinic appointments and alternatives, such as telehealth. Semistructured qualitative interviews with 37 patients were undertaken (75% White Caucasians, 25% South Asians; 29 patients were not adhering to the gluten-free diet). Interviews were recorded, transcribed, and analyzed by NVivo. Frequently reported issues with face-to-face appointments included travel and car parking costs, needing to take time off work, and frequent changes to appointment time. In addition, South Asian patients highlighted issues with linguistics barriers. Telephone consultations were considered acceptable and practical by the majority of patients based on ease and convenience. Online video consultations were favored by just 9 patients, however it is acknowledged that since the COVID-19 pandemic, there has been a greater exposure to this type of technology. These patient experiences can inform health care service development and are not biased by external health concerns connected with in-person visits during the pandemic.
Keywords: celiac disease, telehealth, telemedicine, outpatient, COVID-19
Introduction
Outpatient clinics (OPCs) are an integral part of patient management in day-to-day clinical practice in the hospital setup, and according to 1 estimate, in England alone, 121.6 million OPC appointments were made with 78% attendance achieved (1). While several pathways exist for referral to OPC (2), 50% of patients are referred by the general practitioner (GP) (3). Additionally, excluding the accident and emergency department, the majority (85%) of secondary care activity happens in the OPC (3,4), where increasing demand has been noted in the past decade (5). From a patients’ perspective, OPC appointments have been described as a source of anxiety (6) especially for older patients (7).
There are several studies which have looked into patient satisfaction with the OPC (8 –14), though none specific to celiac disease (CD). Patient’s satisfaction is a key indicator and undeniably a proxy for clinical care quality. It has been recognized that there are issues faced by patients with the OPC experience, and the Royal College of Physicians 2018 report recommend “alternatives to face-to-face consultations should be made available to patients…” There is an overall paucity of research in exploring patients view, that is, the issues they encounter on a day-to-day basis in relation to OPC, especially so in ethnic minority populations. In view of the current coronavirus disease 2019 (COVID-19) pandemic, alternatives to OPCs have been rapidly developed, with telephone clinics and online video consultations being delivered by health care professionals globally (15,16).
Celiac disease is a chronic autoimmune disorder affecting 1% of the global population (17). It is characterized by permanent intolerance to gluten and in the majority of cases, the condition responds to a gluten-free diet (GFD) which is the only treatment currently available (18). This stated, adherence to a GFD can be very challenging, requiring knowledge and behavior change (19,20). This is one of the key reasons, regular follow-up appointments are considered best practice, with international and national guidelines recommending annual reviews for patients with CD (21,22). In the United Kingdom, there is a diverse offering of annual review provision for adults with CD (23) and concerns with both access and the content of follow-up appointments have been voiced (24).
South Asian patients with CD are poorly represented in the published literature, Muhammad et al (25) highlighted that while South Asian patients were generally satisfied with the information received from their consultant and dietitian (97% and 100%, respectively), more than half reported difficulties following the GFD (76% agreed with the statement “I don’t understand what foods I can eat”). It is important the views of patients with CD with different ethnicities, who are not adhering to the GFD or attending annual reviews, are heard to enable the health care service to reach those in particular need.
The aim of this study was to interview and explore the potential challenges faced by Caucasian and South Asian patients with CD in relation to OPCs and acceptability of alternatives, such as telehealth.
Methods
Short semistructured qualitative telephone interviews were conducted to collect information on patients’ views and experiences of OPCs. Participants were recruited from University Hospital of Leicester, identified through a database of CD patients. The study was undertaken in 2016, prior to the COVID-19 pandemic. Inclusion criteria required patients to be over the age of 18 years, resident in Leicester, and have histologically confirmed CD. A random selection of patients from the data base was approached via postal invitation (n = 255); 135 of the invitations were accepted, giving a return rate of 53%. Thirteen pilot interviews were conducted to gather data to refine the topic guide, none of the data generated in these initial interviews was used for the final analysis. This approach guided the author toward rapport and wording issues and also helped with the timing of the interview. The interviews included questions relating to their experience of OPC appointments and their views on other methods for review appointments. Thirty-seven interviews were conducted, further interviews were cancelled as theme saturation effect was observed.
Participants completed a short validated questionnaire by Leffler and colleagues (26) to enable researchers to establish if they were likely to be adhering to the GFD or not. Forty patients had a Coeliac Dietary Adherence Test (CDAT) score >13, this was classified as not adhering to the GFD. Participants were selected to represent a range of dietary adherence, gender, and ethnicities. The interviews were conducted (with ethnic language support where necessary) according to a topic guide which served as a formal structure for conducting the interview. Although it is acknowledged that a topic guide does not provide a rigid structure; such interviews are flexible and open to accepting respondents’ spontaneous descriptions and narratives. The interviews lasted between 20 and 30 minutes. The completed interviews were recorded, transcribed, and then codified using qualitative techniques and the data were subsequently analyzed to reveal key themes using NVivo version 11 (QSR International). Participants were interviewed until the point that the topics were saturated (n = 37) and no further participants were invited for interviews.
Results
Of 37 participants, 28 were White Caucasian (76%) and 9 were South Asian and there was a female predominance (n = 29; 78%). The age of participants ranged from 18 to 85 years (median = 49, interquartile range = 33-60). A large proportion (n = 28) were classified as not adhering to the GFD; of whom 21 were White Caucasian (75%) and 7 South Asian (25%). All patients had seen a dietitian and clinician in an OPC at some stage since their diagnosis.
All patients who were adhering to the GFD (n = 9) reported liking OPCs and they had only positive comments about them. All patients liked the way dietitians explained CD and the patient-related literature they had received. Moreover, the way in which the clinician described the disease to them was well liked by all patients.
“.great clinic with dietitian she explained all the possible issues and she was motivating me as well” “Generally good”, “I am satisfied and it is a good experience” “very empathetic dietitian”.
Themes in Relation to the Content of the OPC Appointment
The OPCs by either clinician or dietitian were regarded as friendly (n = 28), full of information (n = 33), and useful (n = 15), but a few patients found them difficult (n = 4) and useless (n = 3). The general issues were divided into pre- and intra-appointment issues. Among the former group, taking time off for an appointment was a major issue, mainly females (n = 22) found it a source of nonspecific anxiety. Similarly, patients (n = 3) reported issues related to arranging transport for the appointment.
“I have an issue with them, I have to take time off”, “ .have to take time off the work”, “ .time off. so possibly it is difficult for me” and “ . at time difficult to arrange time for appointment you see.”. “logistically speaking it is not a good experience.”.
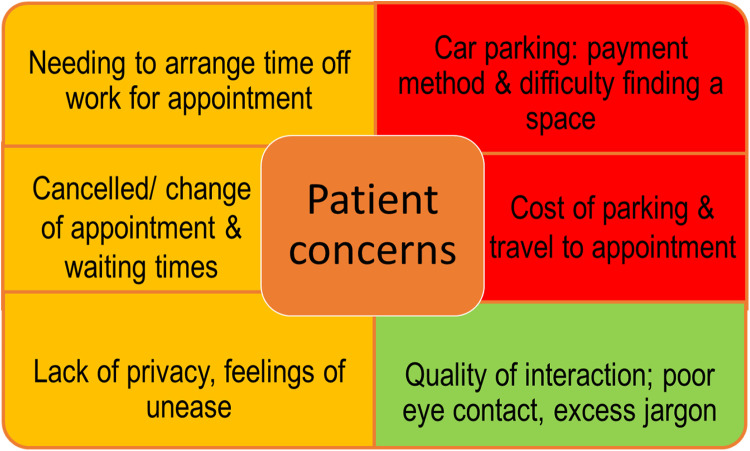
Intra-appointment issues were related to the duration of appointment (n = 7), and the general feeling was that of short (n = 7) and rushed (n = 5) appointment “.everybody seems to be in a hurry”, “.but you cannot discuss all you want to talk about” “.limited time.” Several others (n = 7) thought doctors were explaining things to them in a technical language (n = 3) and there was poor eye contact (n = 4) during clinical interview: “. poor eye contact and the doctor kept on writing in the notes. he even ignored a couple of my questions.” Furthermore, 4 patients commented on the lack of ability of the clinician/dietitian to answer all questions “…did not like the appointment, I was confused about certain things. could not get the answers.” Moreover, 2 patients reported lack of empathy from clinicians and or dietitians but they did not want to feed that back because they did not want to upset people. The main points of patient concerns with OPC are depicted in the diagram below (Figure 1).
Figure 1.
Patient focused issues related to outpatient clinics by adults with celiac disease. Red are the most important themes followed by amber and green.
Themes Related to the Process of the OPC Appointment
Car parking
Car parking was the most frequently mentioned negative issue with regard to hospital appointments (n = 25). Parking was considered unpredictable (n = 23), difficult to find a parking space (n = 20), and expensive (n = 17). Additionally, it was difficult to get into the car park and to exit the main barrier (n = 7). Patients also highlighted other negative aspects such as the inability to pay through debit or credit card (n = 10) and that the parking payment machines would only accept coins and would not give change (n = 11). Also, the parking payment machines were designed so that one had to pay for a predetermined amount of time, which meant that there was potential for overpayment or risk fines, as asserted by the patients:
“…think the hospital car park is a serious main issue . costly and always eager to charge more. that is the real issue…with clinical appointments. .charges are on the mount and people pay a fine because they are late to collect their cars “…many issues such as parking which is not cheap these days. used to be reasonable a few years ago. but now it is all about money you see., and “.Parking is another issue, very strange issue not sure how to describe it.”
In relation to car parking, the punitive intentions of the private parking company for minor parking violation led to anxiety. The majority of patients (n = 28) suggested abolition of car park charges for patients, for example, such as in Welsh hospitals or just a nominal parking fee.
Repeat cancellation and waiting time
Other issues with OPCs were repeated cancellations and changes in time of attendance (n = 10) and prolonged waiting times (n = 11); these were further aggravated by the over parking issues and related anxiety. Repeat cancellation caused rearranging time off with employers (n = 7), distress (n = 3), rearranging transport (n = 6), and feelings of diagnostic delay (n = 3).
“well they keep on changing, I had it changed 2 times on average as far as I know”, “.lots of alteration, you do wait for them and then someone goes on leave or clinic is cancelled. eleventh hour cancellation” and “Well they keep on changing and you have to wait again, there are days when you are happy to talk about your health and there are days where are you not. you see.”
Privacy in the OPC
Privacy in clinic was another issue raised by the participants (n = 23):
“…you are seen by many people in the same clinical area where other people are sitting. They might know you. privacy is non-existent in the NHS. people shouting your name. Mr this and that. Mrs this and that. honestly .[sounding frustrated]” Serious issues with the privacy. no way I am going to discuss my personal problems there”, I have heard people talking aloud and even in the clinical room you can hear what the other person is saying, no privacy at all. How can you bring up emotional subjects when people are listening to you outside?
Cost to patients and environment
Cost was an issue for a majority of patients (n = 33) in particular travel (n = 17) and parking (n = 12) related costs. A few patients (n = 3) also suggested that travel to hospital on transport came at cost to the environment and a different mode, that is, telephone clinic was suggested as an alternative.
Alternatives to face-to-face outpatient appointment
Telephone interaction was considered acceptable (n = 25) and practical (n = 24) by the patients based on ease (n = 33), flexibility (n = 29), and convenience (n = 19) by the patients. Theme analysis showed that patients approved of it as a practical intervention based on their experience of using the telephone in both personal and professional lives. It was considered important for privacy (n = 27) and ease of communication (n = 18). In addition, the telephone clinic gave control to the patients to stop the conversation when they wanted to (n = 20). There were, however, concerns such as lack of face-to-face contact for the participants (n = 4), which may lead to an uncomfortable situation, as body language cannot be seen and read by either the health care professional or the patient.
“I prefer the telephone, one to one”, “Telephonic teaching is OK”, “telephone fing [thing] is the best”, “certainly telephonic interview with a leaflet or skype etc.”, I think telephonic interview/CD link etc. “telephonic interview or talking as you mentioned.” “Telephone I think is better choice.”
However, it is noteworthy that when telephone group discussion/clinic was presented as an option of interaction, the majority (n = 25) opposed the idea.
“not really . difficult and not a very good idea” “many people and talking together. not sure I will be heard. so sorry, “Not an attractive idea. I am sorry”
Online one-to-one appointment video links were favored by 9 patients. An online film link was favored (n = 20), but only in relation to web-based teaching, not to replace OPC. Compact discs, DVDs, or books were only favored by 2 of the participants. Mixed feelings were noted about email and text messages.
“I get so many email and . Well I might not get through them you see.” “Emails have their own issues. I mean spam etc. “Emails, hmm. good. will give it a try, not sure it will affect me a lot”
South Asian patients and clinical appointments
All South Asian patients (n = 9) were born outside the United Kingdom and had spent more than 10 years living in the United Kingdom. One of the general comments was difficulty understanding doctors because of linguistic barriers (n = 3) and about the availability of interpreters in clinic (n = 4).
“.by telling us in our language…personal interpreters.”, “Drs should speak to us in easy language.”, “. we understand English but we are not language masters…”, “we need interpreters. explaining things to us in our language.”, “.in a language we understand.”, “. not in my language. and very patchy.”, “good explanation in our local languages might be useful. after all there are many Asian doctors they can explain things to us in our languages.”
Two patients were concerned about the religious implications of GFD but other than that, the majority of the issues were the same, that is, car parking (n = 7), delays in appointment (n = 5), and cost associated with travel to OPC.
Discussion
This study is first to ask adults with CD about their experience of attending OPCs and their preferences for future provision. The Royal College of Physicians report highlighted similar issues around OPC for a broad range of disciplines, and valuable suggestions were put forwarded to improve the system with the needs of the patients clearly present within discussions (3). A strength of the current study was the diverse group of adults with histology confirmed CD diagnosis, inclusive of adults of different ethnic groups and those not adhering to the GFD.
The issues of waiting time has previously been identified and suggestions forwarded with strategies coined to tackle the issue (27 –31). Our study has brought to surface the effect of waiting time on patients, their work, and daily lives including transport arrangements and feelings of delay either in treatment of diagnostic workup. Research has shown that this indeed is one of the major factors for patients’ dissatisfaction regarding clinics and correcting this factor may improve satisfaction (from 50%-74%) among patients (32). Our study highlights that delay and cancellation of appointments is a source of anxiety for patients but it is also accepted that the issue is multifactorial and apart from hospital cancellations and lack of staff there are also patients who arrive late affecting the flow and waiting time of the clinic as well as those who do not attend (DNA) (33).
Car parking emerged as a major issue for the majority of the patients in terms of cost, fear of civil notices, and difficulty to find places to park. These issues are not unique to patients with CD and have been highlighted previously (34,35), a factor that even determined choice of hospital for treatment (36) and an element of satisfaction with service (37). Our study reiterates the importance of the issue in a unified fashion and issues were raised about car parking ticket machines and the punitive nature of the Trust for overparking.
The participants reported a relative lack of privacy in the OPC environment. This concern has been raised in other disciplines (38 –40), and needs due consideration as privacy is one of the fundamental ethical and legal rights of the patients (41). It is not surprising that issues of privacy are directly related to patient satisfaction (42,43). This area too needs further detailed interview-based research, as there is a difference of perception in relation to the concept of privacy as it is multifactorial and differs between cultures (42,44,45). It may be suggested that the structure of the OPC should be changed in a way that consultation rooms are away from the waiting area and doors should be soundproof.
Our study indicates the acceptability of telephone clinics as an alternative to hospital-based OPC appointments, this is in agreement with a recent finding from of a larger cohort of Italian adults with CD (16). In view of the COVID-19 pandemic, there has been a rapid move toward telephone clinics and online video consultations globally (15,16), given the fact that by their inherent nature, telephone clinics are contactless, cost effective, acceptable, and practical. A reduction in patients who DNA was observed when telephone consultations were offered compared with face-to-face consultations (46). An observational study reported patients with CD who had a telephone clinic with a nurse were more likely to receive an annual review, have their symptoms assessed, and their diet reviewed compared with those who had GP follow-up provision (47). A controlled, prospective study demonstrated improved GFD adherence after a telephone clinic that was sustained for 6 months. The authors proposed a flexible approach to allow patients to choose whether they would prefer a telephone clinic rather than attend an outpatient appointment at a hospital (48), recognizing it may not be suitable for patients with hearing difficulties, linguistic barriers, or those who have issues with telephone or internet access. The importance of personalized advice by a health care professional with expertise in CD was reiterated in the study. While “Telehealth” has been used sporadically in other areas with varying success (49), very little research has been undertaken in patients with CD.
There are certain limitations in this study; only patients with CD were interviewed and thus the views cannot easily be generalized to other patient groups. Although we did include the views of South Asians as well as Caucasians, given the numbers the study’s findings cannot be generalizable to all cultures and backgrounds and thus further research is required to encompass a broader range of patients whereby our study can inform the research design. One final word, this study was conducted 4 years prior to the severe acute respiratory syndrome coronavirus 2 pandemic and there is a possibility that patients may have changed their opinion. It has been reported that studies exploring patient satisfaction with telehealth during the pandemic may be artificially inflated during COVID-19 due to external health concerns connected with in-person visits (50).
In summary, face-to-face appointments with health care professionals do have fundamental problems which can be partially overcome by telephone and online consultations. We recommend further exploration and evaluation of their use in clinical practice for potential continued service provision after the COVID-19 pandemic.
Footnotes
Authors’ Note: HM, SR, YJ, and SI contributed to conceptualization of study; HM, SR, and YJ contributed to methodology; HM, SR, YJ, and SI contributed to formal analysis; HM, SR, and YJ contributed in writing—original draft preparation; HM, SR, YJ, and SI contributed in writing—review and editing. All authors have read and agreed to the published version of the manuscript. All patients gave their informed consent for inclusion before they participated in the study. HM and YJ have previously received a DSI nutrition project award. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the procedures of the University of Roehampton (LCS 15/130) and NHS Research and Ethics Committee (REC) (Ref: 15/YH/0289).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Humayun Muhammad  https://orcid.org/0000-0001-9670-9556
https://orcid.org/0000-0001-9670-9556
References
- 1. NHS England. Provisional monthly hospital episode statistics for admitted patient care, outpatient and accident and emergency data - April 2018 - December 2018. 2019. Accessed May, 2021. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-episode-statistics-for-admitted-patient-care-outpatient-and-accident-and-emergency-data/april-2018---december-2018/content
- 2. NHS UK. Source of referral to outpatients. 2019. Accessed May, 2021. https://www.datadictionary.nhs.uk/data_dictionary/attributes/s/smo/source_of_referral_for_out-patients_de.asp?shownav=0
- 3. RCP. Outpatients: the future - royal college of physicians. 2018. Accessed May, 2020. https://www.rcplondon.ac.uk/projects/outputs/outpatients-future-adding-value-through-sustainability
- 4. Buchan J, Charlesworth A, Gershilick B, Seccombe I. Rising Pressure: The NHS Workforce Challenge. Workforce profile and trends of the NHS in England; 2017. [Google Scholar]
- 5. King’s Fund. Hospital activity. 2017. Accessed May, 2021. https://www.kingsfund.org.uk/projects/nhs-in-a-nutshell/hospital-activity, 2020
- 6. de Iongh A. Appointment day-the tip of an iceberg. BMJ. 2018;360. doi:https://doi.org/10.1136/bmj.k430 [DOI] [PubMed] [Google Scholar]
- 7. Age UK. Painful Journeys: why getting to hospital appointment is a major issue for older patients. In depth policy report. 2017. Accessed May, 2021. https://www.ageuk.org.uk/contentassets/7354623c9df1491a84cc34ef46105647/painful_journeys_campaignreport.pdf
- 8. Oluwole EO, Osibogun O, Adegoke O, Adejimi AA, Adewole AM, Osibogun A. Medication adherence and patient satisfaction among hypertensive patients attending outpatient clinic in Lagos University Teaching Hospital, Nigeria. Niger Postgrad Med J 2019;26:129–37. [DOI] [PubMed] [Google Scholar]
- 9. Wang X, Chen J, Burstrom B, Burstrom K. Exploring pathways to outpatients’ satisfaction with health care in Chinese public hospitals in urban and rural areas using patient-reported experiences. Int J Equity Health. 2019;18:29–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zakare-Fagbamila RT, Seyferth E, Cheng TZ, Clement M, Stroup B, Gottfried ON. Chief complaints and feedback from clinic satisfaction tool: thematic analysis of a new outpatient communication tool. Int J Clin Pract. 2019;73(4): e13318. [DOI] [PubMed] [Google Scholar]
- 11. Bedeir YH, Grawe BM. Patient factors influencing outpatient satisfaction in patients presenting with shoulder pain. J Shoulder Elbow Surg. 2018;27:e367–71. [DOI] [PubMed] [Google Scholar]
- 12. Patel S, Sutton AV, Thorpe J, Tsai KY, Crew AB. Patient satisfaction and quality of care: a prospective study at outpatient dermatology clinics. Cutis. 2018;102:33–35. [PubMed] [Google Scholar]
- 13. Hirukawa M, Ohira Y, Uehara T, Noda K, Suzuki S, Shikino K, et al. Satisfaction of patients and physicians with outpatient consultations at a university hospital. Intern Med. 2015;54:1499–1504. [DOI] [PubMed] [Google Scholar]
- 14. Puri N, Gupta A, Aggarwal AK, Kaushal V. Outpatient satisfaction and quality of health care in North Indian medical institute. Int J Health Care Qual Assur. 2012;25:682–97. [DOI] [PubMed] [Google Scholar]
- 15. Luciani LG, Mattevi D, Cai T, Giusti G, Proietti S, Malossini G. Teleurology in the time of COVID-19 pandemic: here to stay?. Urology. 2020;140:4–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Siniscalchi M, Zingone F, Savarino EV, D’Odorico A, Ciacci C. COVID-19 pandemic perception in adults with celiac disease: an impulse to implement the use of telemedicine: COVID-19 and CeD . Dig Liver Dis. 2020;52:1071–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Singh P, Arora A, Strand TA, Leffler DA, Catassi C, Green PH, et al. Global prevalence of celiac disease: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2018;16:823–36. [DOI] [PubMed] [Google Scholar]
- 18. Lebwohl B, Sanders DS, Green PH. Coeliac disease. Lancet. 2018;391:70–81. [DOI] [PubMed] [Google Scholar]
- 19. Zarkadas M, Dubois S, MacIsaac K, Cantin I, Rashid M, Roberts KC, et al. Living with coeliac disease and a gluten-free diet: a Canadian perspective. J Hum Nutr Diet. 2013;26:10–23. [DOI] [PubMed] [Google Scholar]
- 20. Muhammad H, Reeves S, Jeanes YM. Identifying and improving adherence to the gluten-free diet in people with coeliac disease. Proc Nutr Soc. 2019;78:1–8. [DOI] [PubMed] [Google Scholar]
- 21. NICE. Coeliac disease: recognition, assessment Coeliac disease: recognition, assessment and management and management. 2015. Accessed May, 2021. https://www.nice.org.uk/guidance/ng20/resources/coeliac-disease-recognition-assessment-and-management-pdf-1837325178565
- 22. Husby S, Murray JA, Katzka DA. AGA clinical practice update on diagnosis and monitoring of celiac disease—changing utility of serology and histologic measures: expert review. Gastroenterology. 2019;156:885–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kallos S, Jeanes Y. Cross-sectional survey of the dietetic provision for adults with coeliac disease in the UK. J Hum Nutr Diet. 2020;33:6–15. [Google Scholar]
- 24. Crocker H, Jenkinson C, Peters M. Healthcare experiences and quality of life of adults with coeliac disease: a cross-sectional study. J Hum Nutr Diet. 2020;33:741–51. [DOI] [PubMed] [Google Scholar]
- 25. Muhammad H, Reeves S, Ishaq S, Mayberry J, Jeanes YM. Adherence to a gluten free diet is associated with receiving gluten free foods on prescription and understanding food labelling. Nutrients. 2017;9:705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Leffler DA, Dennis M, Edwards George JB, Jamma S, Magge S, Cook EF, et al. A simple validated gluten-free diet adherence survey for adults with celiac disease. Clin Gastroenterol Hepatol. 2009;7:530–32. [DOI] [PubMed] [Google Scholar]
- 27. Sun J, Lin Q, Zhao P, Zhang Q, Xu K, Chen H, et al. Reducing waiting time and raising outpatient satisfaction in a Chinese public tertiary general hospital-an interrupted time series study. BMC Public Health. 2017;17:668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lewis AK, Harding KE, Snowdon DA, Taylor NF. Reducing wait time from referral to first visit for community outpatient services may contribute to better health outcomes: a systematic review. BMC Health Serv Res. 2018;18:869–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mohebbifar R, Hasanpoor E, Mohseni M, Sokhanvar M, Khosravizadeh O, Mousavi Isfahani H. Outpatient waiting time in health services and teaching hospitals: a case study in Iran. Glob J Health Sci. 2013;6:172–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Prentice JC, Fincke BG, Miller DR, Pizer SD. Outpatient wait time and diabetes care quality improvement. Am J Manag Care. 2011;17:43. [PubMed] [Google Scholar]
- 31. Birk HO, Gut R, Henriksen LO. Patients’ experience of choosing an outpatient clinic in one county in Denmark: results of a patient survey. BMC Health Serv Res 2011;11:262–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Eilers GM. Improving patient satisfaction with waiting time. J Am Coll Health. 2004;53:41–48. [DOI] [PubMed] [Google Scholar]
- 33. Medway AM, de Riese WT, de Riese CS, Cordero J. Why patients should arrive late: the impact of arrival time on patient satisfaction in an academic clinic. Healthc (Amst). 2016;4:188–91. [DOI] [PubMed] [Google Scholar]
- 34. Twiddy M, Czoski Murray CJ, Mason SJ, Meads D, Wright JM, Mitchell ED, et al. A qualitative study of patients’ feedback about outpatient parenteral antimicrobial therapy (OPAT) services in Northern England: implications for service improvement. BMJ open 8.1 (2018): e019099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fradgley EA, Paul CL, Bryant J, Oldmeadow C. Getting right to the point: identifying Australian outpatients’ priorities and preferences for patient-centred quality improvement in chronic disease care. Int J Qual Health Care. 2016;28:470–477. [DOI] [PubMed] [Google Scholar]
- 36. Smith H, Currie C, Chaiwuttisak P, Kyprianou A. Patient choice modelling: how do patients choose their hospitals?. Health Care Manag Sci. 2018;21:259–268. [DOI] [PubMed] [Google Scholar]
- 37. Coleman S, Havas K, Ersham S, Stone C, Taylor B, Graham A, et al. Patient satisfaction with nurse-led chronic kidney disease clinics: a multicentre evaluation. J Ren Care. 2017;43:11–20. [DOI] [PubMed] [Google Scholar]
- 38. Wang Z, Pukszta M. . Private rooms, semi-open areas, or open areas for chemotherapy care: perspectives of cancer patients, families, and nursing staff. HERD. 2018;11:94–108. [DOI] [PubMed] [Google Scholar]
- 39. Johnson GM, Little R, Staufenberg A, McDonald A, Taylor KGM. How do they feel? Patients’ perspectives on draping and dignity in a physiotherapy outpatient setting: a pilot study. Man Ther. 2016;26:192–200. [DOI] [PubMed] [Google Scholar]
- 40. Perkins VH. The importance of patients and their privacy. Health Aff (Millwood). 2011;30:181; author reply 182. [DOI] [PubMed] [Google Scholar]
- 41. Frenkell DA, Wood DM. Patients’ right to privacy and public interest. Med Law. 2015;34:285–96. [PubMed] [Google Scholar]
- 42. Lin YK, Lin CJ. Factors predicting patients’ perception of privacy and satisfaction for emergency care. Emerg Med J. 2011;28:604–8. [DOI] [PubMed] [Google Scholar]
- 43. Nayeri ND, Aghajani M. Patients’ privacy and satisfaction in the emergency department: a descriptive analytical study. Nurs Ethics. 2010;17:167–77. [DOI] [PubMed] [Google Scholar]
- 44. Lamas E, Coquedano C, Bousquet C, Ferrer M, Chekroun M, Zorrilla S, et al. Patients’ perception of privacy of personal data, shared in online communities: are we in the presence of a paradox? Stud Health Technol Inform. 2018;251:237–40. [PubMed] [Google Scholar]
- 45. Hartigan L, Cussen L, Meaney S, O’Donoghue K. Patients’ perception of privacy and confidentiality in the emergency department of a busy obstetric unit. BMC Health Serv Res. 2018;18:978–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wignall D, Lee L, Gkentzis A.. A review of telephone urological follow-up in a district general hospital during the COVID-19 pandemic. SN Compr Clin Med. 2020:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Pritchard L, Waters C, Murray IA, Bebb J, Lewis S. Comparing alternative follow-up strategies for patients with stable coeliac disease. Frontline Gastroenterol. 2020;11:93–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Muhammad H, Revees S, Ishaq S, Jeanes Y. Telephone clinic improves gluten free dietary adherence in adults with coeliac disease; sustained at 6 months . Frontline Gastroenterol. 2020. (In Press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Cottrell MA, Hill AJ, O’Leary SP, Raymer ME, Russell TG. Clinicians’ perspectives of a novel home-based multidisciplinary telehealth service for patients with chronic spinal pain. Int J Telerehabil. 2018;10:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Agha Z, Schapira R, Laud PW, McNutt G, Roter DL. Patient satisfaction with physician-patient communication during telemedicine. Telemed J E Health. 2009;15:830–39. [DOI] [PubMed] [Google Scholar]