Abstract
The coronavirus disease 2019 (COVID-19) pandemic has necessitated many rapid changes in the provision and delivery of health care in hospital. This study aimed to explore the patient experience of inpatient care during COVID-19 pandemic. An electronic questionnaire was designed and distributed to inpatients treated at a large University Health Board over a 6-week period. It focused on hospital inpatients’ experience of being cared for by health care professionals wearing personal protective equipment (PPE), explored communication, and patients’ perceptions of the quality of care. A total of 704 patients completed the survey. Results demonstrated that patients believe PPE is important to protect the health of both patients and staff and does not negatively impact on their care. In spite of routine use of PPE, patients were still able to identify and communicate with staff. Although visiting restrictions were enforced to limit disease transmission, patients maintained contact with their relatives by using various electronic forms of communication. Overall, patients rated the quality of care they received at 9/10. This single-center study demonstrates a positive patient experience of care at an unprecedented time.
Keywords: COVID-19, challenges, communication, clinician–patient relationship, patient feedback, patient perspectives/narratives, patient satisfaction, survey data
Introduction
The global coronavirus disease 2019 (COVID-19) pandemic has presented the biggest health care challenge of our generation. It has necessitated an unprecedented number of adaptations in our hospitals to facilitate the safe delivery of health care for patients during the COVID-19 pandemic (1). Adaptations such as the use of personal protective equipment (PPE) and the introduction of visiting restrictions and cohort wards for patients with COVID-19 have become routine in order to limit the spread of severe acute respiratory syndrome coronavirus 2 infection but represent a significant departure from normal hospital practice (2,3). Within our health board, situation-specific PPE guidelines, adapted from the public health England guidance for both aerosol and nonaerosol-generating procedures, were implemented (2). The use of face masks, mandatory for all staff in patient facing roles in clinical areas of the hospital, was the main concern regarding the communication difficulties which were hypothesized to be encountered while using PPE. All visiting was stopped apart from 3 exceptional circumstances including end-of-life care and visiting maternity or pediatric patients. This was a big change from normal visiting rules which allowed relatives to visit hospital inpatients at specified visiting times. These adaptations were implemented to protect the health of both patients and staff, however, we hypothesized that they may influence both the standard of health care delivery but most importantly, the patient experience of inpatient care. We believed that patients may harbor anxiety surrounding the routine use of PPE, may find it difficult to identify staff roles, experience difficulty in communicating with staff, and may feel isolated while alone in the hospital without any visitors.
Throughout the pandemic, there has been a large research effort to collate and disseminate new information regarding COVID-19. Much of literature has focused on epidemiology, treatment options, hospital restructuring, use of PPE, and COVID-19-related mortality (1,4 –8). However, there is a paucity of research relating to the patient experience and patient perceptions of inpatient care at this time. The objective of this study was to understand the patients’ experience of inpatient care during the coronavirus pandemic. The 3 aims of the study were (1) to explore the patient experience of being cared for by health care providers wearing PPE, (2) to understand if communication with staff and relatives was a challenge for patients, and (3) to explore the patients’ perceptions of the quality of inpatient care they received during the coronavirus pandemic. The ongoing COVID-19 pandemic is set to continue to impact the way health care is delivered for the foreseeable future. Understanding the patient perceptions of inpatient care during height of the COVID-19 pandemic will play a significant role in informing decision-making and the restructuring of hospital services going forward to improve care for our patients.
Methods
This single-center patient experience survey was conducted across the Cardiff and Vale University Health Board. A mixed methods questionnaire was designed and refined by a research team composed of clinicians and members of health board’s patient experience team. Questions relating to each of the 3 aims of the study were designed to be answered either with simple yes/no answer or using a validated 5-point Likert scale to provide quantitative data. Several open questions with free text boxes were also included to obtain rich qualitative data regarding patient perceptions of staff wearing PPE and overall comments about their hospital stay. The questionnaire was hosted by the online survey hosting site SurveyMonkey. Both the research proposal and questionnaire were approved, following discussion, by the executive health board committee and research leads from the patient experience team within the health board. Two different data collection techniques were utilized in order to capture the patient experience of both current hospital inpatients and also patients who had already been discharged to continue their recovery at home. Inclusion criteria were any patients who had received inpatient care across the health board over a 6-week period from the beginning of the United Kingdom lockdown (March 23, 2020). This included all medical and surgical specialties across the health boards’ 2 acute hospital sites, the University Hospital of Wales (UHW) and the University Hospital Llandough (UHL). All patients were informed, in the questionnaire introduction, of the aims of the study and that participation was voluntary, answers were confidential, and that consent to take part in the research was implied by completion of the survey. Any patients who had questions or concerns relating to the survey, or their inpatient stay, were encouraged to contact the health boards patient experience team with a contact number provided in the questionnaire.
For the inpatient survey, a team of 4 clinical researchers underwent specific training and were provided with secure, health board tablet devices. They attended inpatient wards across the 2 main inpatient sites at UHW and UHL. As patients with confirmed or suspected COVID-19 were cared for on specific COVID-19 cohort wards, our clinical researchers visited both COVID-19 cohort and noncohort wards wearing appropriate PPE. Patients were invited to complete the survey using the tablet devices provided if they gave verbal consent to participate. Any patients who were unable to use the devices were assisted to complete the survey by the clinical researchers. For the discharged patient survey, a list was extracted of all inpatients discharged from the health board over a 6-week period. A link to the survey was sent out to these patients via text message or email to invite them to complete the survey online. Discharged patients were given a 7-day period to respond. Anonymized data were exported from the SurveyMonkey hosting site and analyzed using Microsoft Excel. Quantitative data were analyzed in relation to each of the 3 study aims, and thematic analysis was utilized for qualitative data analysis. Results were presented at the executive health boards’ operational meeting and distributed to staff members of the health board via the hospital communications team.
Results
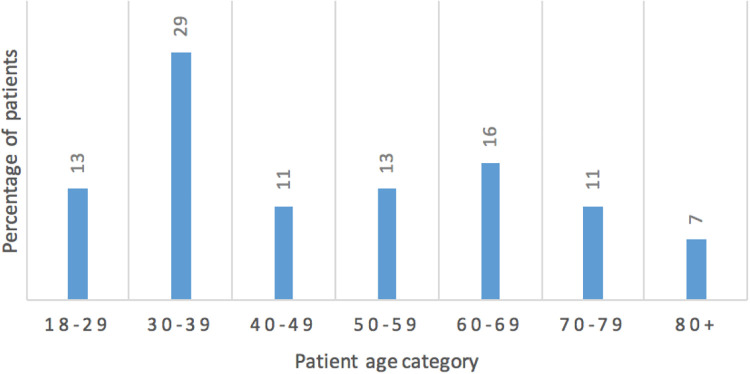
A total of 704 patients completed the survey. One hundred and two inpatients took part in the study, recruited by the clinical research teams based on the wards, and 602 discharged patients responded to the electronic link to take part in the study; 74% of inpatients had been treated in the UHW with the remaining 26% treated at the UHL. The age range of patients is demonstrated in Figure 1. A total of 2742 patients who had been discharged from the 2 hospital sites during the 6-week period commencing the 23rd of March (United Kingdom lockdown) and had provided mobile or email contact details were invited to complete the questionnaire using an electronic link. These included emergency admissions, elective admissions, and maternity admissions. The 602 patient responses resulted in an overall questionnaire response rate of 22%. The total number of emergency admissions across the 2 hospital sites over the 6-week period was 3092 patients. Compared to the corresponding 6-week period from the previous year where there were 5583 emergency admissions, this represented a decrease of 45% in the total number of emergency admissions.
Figure 1.
The age range of patients who completed the survey.
The first section of the questionnaire contained questions relating to the first aim: the patient experience of being cared for by staff wearing PPE. Results of these questions are displayed in Table 1.
Table 1.
Results for questions relating to the first aim of the study.
| Questions | Always | Often | Sometimes | Rarely | Never |
|---|---|---|---|---|---|
| Were you worried about catching COVID-19 while in hospital? | 23% | 11% | 29% | 18% | 19% |
| How often did staff wear PPE while caring for you? | 68% | 25% | 7% | 0% | N/A |
| Did staff wearing PPE make you feel anxious? | 2% | 5% | 10% | 14% | 69% |
| Questions | Yes | No | |||
| Do you believe it is important for staff to wear PPE to protect the health of their patients? | 98% | 2% | |||
| Do you believe it is important for staff to wear PPE to protect their own health? | 99% | 1% | |||
| At this time would you feel anxious being cared for by staff who were not wearing PPE? | 68% | 32% | |||
Abbreviations: COVID-19, coronavirus disease 2019; PPE, personal protective equipment; N/A, not available.
The second section contained questions relating to the second aim of the study: exploring communication between both patients and health care workers and patients and their relatives during their inpatient stay. The results are displayed in Table 2.
Table 2.
Results for questions relating to the second aim of the study.
| Questions | Always | Often | Sometimes | Rarely | Never |
|---|---|---|---|---|---|
| Did staff involved in your care introduce themselves? | 71% | 19% | 8% | 2% | 0% |
| When staff wore PPE, were you able to identify their roles? | 50% | 27% | 16% | 5% | 2% |
| Did you find it difficult to communicate with staff while they wore PPE? | 3% | 7% | 27% | 26% | 37% |
| Did you feel lonely during your inpatient stay? | 16% | 16% | 29% | 16% | 23% |
| Questions | Yes | No | |||
| Were you able to communicate with your friends and family during your hospital stay? | 94% | 6% | |||
Abbreviation: PPE, personal protective equipment.
Enquiry into the method of communication used by inpatients to communicate with their relatives identified that 84% utilized phone calls, 69% text messages, 44% video calls, 27% social media, and 7% used emails.
Patients were invited to enter any free text comments they would like to make about staff wearing PPE. Thematic analysis was carried out using these free text comments. Common positive themes were that patients described that they understood PPE was necessary and made them feel safe and reassured. Negative themes included communication difficulties with staff due to facial expressions being hidden or voices muffled by the use of face masks. In addition, patients described variability in the PPE worn by staff in the hospital.
The third section contained questions relating to the third study aim: exploring patient perceptions of the quality of care they received as an inpatient. The results are displayed in Table 3.
Table 3.
Results for questions relating to the third aim of the study.
| Question | Always | Often | Sometimes | Rarely | Never |
|---|---|---|---|---|---|
| During your stay, do you believe that there were adequate hospital staff to care for you? | 66% | 21% | 9% | 3% | 1% |
| Question | Yes | No | |||
| Do you think the extra precautions staff took by wearing PPE had a negative impact on your care? | 5% | 95% | |||
When asked to rate the quality of care inpatients had received during their recent hospital stay on a scale of 1 to 10, with 10 being the highest score, the mean score was 9.
Patients were invited to enter any comments they would like to make about their hospital stay. Thematic analysis was carried out to analyze this information. The overwhelmingly positive themes were patients describing the excellent care they had received and messages of thanks to hospital staff for their kindness, care, compassion, and professionalism.
Discussion
Patient Experience of Being Cared for by Health Care Providers Wearing PPE
Personal protective equipment has been in the spotlight since the beginning of the COVID-19 pandemic (9). The provision of adequate PPE in the clinical setting was both an initial procurement and logistical challenge as the prevalence of viral illness spread and increased across the world (10). Public Health England was quick to define and publish situation-specific guidance for PPE in the clinical setting to protect health care workers and limit disease transmission (2). Personal protective equipment does, however, represent a physical barrier to human interaction, both in terms of concealing facial expression and also acting as a partial sound barrier. In addition, for patients in hospital, while used for their protection, we hypothesized that patients may harbor anxiety when cared for by staff wearing PPE and may not fully understand the rationale for its routine use. At a time when the United Kingdom government set out the “Stay home, Protect the NHS, Save lives” message and instigated lockdown rules, we believed that patients may have had significant anxiety regarding contracting the virus when coming into hospital to receive medical treatment (11). Survey results showed that around 1/3 of patients described concern about contracting COVID-19 while in hospital (34% positive response, 23% always, 11% often), around 1/3 a neutral response (29% neutral response of sometimes), and 1/3 were not concerned (37% negative response, 18% rarely, and 19% never). The majority of patients (93%) were cared for regularly by staff wearing PPE in the clinical setting (68% always and 23% often) and indicated that they believed PPE use was of importance to protect the health of both health care workers (99%) and patients (98%). The survey demonstrated low levels of anxiety with 14% of patients describing that staff wearing PPE rarely made them feel anxious and 69% never felt anxious. Contrary to our belief of patients feeling anxious when cared by the staff wearing PPE, we demonstrated that patients felt reassured when being cared for by staff wearing PPE. In fact, 68% described that they would in fact feel anxious if staff were not wearing PPE to care for them.
Patient Communication With Health Care Staff and Relatives
Communication with patients is at the heart of health care in the modern era focusing on patient autonomy (12). Staff introductions are key to establishing an initial rapport at the beginning of any patient interaction. When donned with PPE, this is particularly crucial as many of the usual identifying features such as scrub color and name badges may be concealed. The survey demonstrated that staff were excellent at introducing themselves to patients (71% always and 19% often). In spite of staff wearing PPE, the majority of patients answered that they were still able to identify staff roles with only a small number finding this a challenge (5% rarely and 2% never). Even with PPE face masks concealing facial expression and muffling voices, only a small minority of patients described finding difficulty in communication with staff wearing PPE (3% always, 7% often). Strict visiting restrictions have been key to a strategy of reducing COVID-19 hospital-community transmission by limiting exposure of those in the community to the hospital setting. While important to limit exposure, patient communication with their loved ones and relatives visiting contributes significantly to patient well-being. Approximately 2/3 of patients did describe loneliness during their inpatient stay as a result of the visiting restrictions (16% always, 16% often, 29% sometimes). However, 94% of patients stated that they were still able to communicate with their family. The most common methods of communication were phone calls, text messages, and video calls, respectively.
Patient Perceptions of the Quality of Inpatient Care
The most important aspect of the study was to ascertain the patient-perceived quality of the inpatient care they received during the coronavirus pandemic. Hospital staffing was a significant concern at the start of the COVID-19 pandemic where staff sickness had the potential to cause problems with workforce provision (13). Restructuring of the hospital workforce also resulted in both departmental changes and redeployment of staff to different specialties and clinical areas of the hospital (14,15). Despite these workforce challenges, the majority of patients surveyed reported that they believed there were adequate staff in the hospital to care for them (66% always, 21% often). In addition to the previous patient experience of PPE described, 95% of patients did not think that the extra precautions staff took be wearing PPE had a negative impact on their care. The most important finding of the survey was the overall patient-perceived quality of care they received as an inpatient during the COVID-19 pandemic. Even with all the measures and adaptations put in place to manage patients with COVID-19, patients reported that overall, they rated the care they received at a mean of 9/10.
Limitations
There are several limitations of this study. As this is a single-center study, the positive patient experience of inpatient care from our health board is a direct reflection of the health care provided by staff in our institution. However, although the patient-perceived quality of care may be unique to our health board, the patient reported experience relating to PPE which is standardized by the public health England guidance is likely to broadly reflect the patient experience across similar health care organizations in the United Kingdom. Patient age ranges displayed in Figure 1 do not reflect that of the typical inpatient age range in a large teaching hospital and are skewed toward a younger age-group. A limitation of this data collection technique of sending an electronic link is likely to have introduced a selection bias as patients in the older age-group may have encountered difficulty in accessing or using electronic devices to complete the electronic questionnaire. Also, the electronic questionnaire link could only be sent to patients who had provided mobile or email details to the hospital. The main limitation is that the questionnaire utilized mainly yes/no and Likert scale questions with only 2 open questions inviting free text comments. While this technique allowed interpretation of a large data set in relation to the 3 study aims, in-depth rich qualitative data regarding the inpatient experience during COVID-19 could be collected using a smaller sample size and qualitative data collection techniques such as semistructured patient interviews. This technique could be particularly beneficial in exploring how communication with patients could be improved while staff wear PPE.
Conclusion
This study provides an insight into the patient experience of hospital inpatient care during the COVID19 pandemic. From the study, we conclude that the 4 most important messages of the study are:
Patients believe that PPE is important to protect the health of both patients and staff and does not impact negatively on their care of make them feel anxious.
Clinical staff are identifiable even when wearing PPE and patients are able to communicate easily with staff in spite of using PPE.
Visiting restrictions have resulted in patients feeling lonely, however patients have access to multiple methods of communication and thus are still able to maintain contact with their loved ones during their inpatient stay.
Overall, patients believed there are adequate staff in the hospital and rate the quality of care they received at 9 out of 10.
The current challenge in hospital care is adapting the health care service to restart the delivery of elective services in a climate where COVID-19 is likely to have ongoing presence both in hospitals and in the community (15,16). Understanding the patient experience, particularly with regard to being cared for by staff, wearing PPE is an integral part of informing the adaptation of these services. Although the findings of this study reflect a very positive patient experience, identification of staff, communication while wearing PPE, and patient communication with their relatives still represent the biggest challenges.
Recommendations
In our health board, we have implemented 3 measures to address these challenges.
To enable staff to be identified by patients with ease, large and reusable name badges have been suggested.
Patient leaflets will aim to provide patients with information regarding the measures taken by the health board to reduce the risk of COVID-19 transmission in the hospital including information about the role and benefits of PPE.
To facilitate communication between patients and their relatives, health board owned tablet devices have been loaned to wards, where clinical staff are encouraged to assist patients in communicating with their relatives. This has been most beneficial for patients who are unable to use tablet devices without assistance or do not have their own devices for electronic communication. These measures are likely to be beneficial to all hospitals caring for patients at this challenging time.
The positive patient experience of care during the COVID-19 pandemic identified in this study is a testament to the motivation, dedication, and strong work ethic of the hospital workforce across our health board who have worked tirelessly to ensure that a high standard of patient care has been maintained during an unprecedented time for the health service.
Acknowledgments
We would like to thank Mr Tunia Patel for his assistance with data collection.
Author Biographies
Thomas Key is a specialist registrar in Trauma & Orthopaedic Surgery.
Avadhut Kulkarni is a junior clinical fellow in Trauma and Orthopaedic Surgery.
Vikram Kandhari is a senior clinical fellow in Trauma & Orthopaedic Surgery.
Zayd Jawad is a core surgical trainee (CT2).
Angela Hughes is the assistant director of Patient Experience.
Khitish Mohanty is a consultant in Trauma & Orthopaedic Surgery, specialising in Major Trauma and Pelvic Surgery.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Thomas Key  https://orcid.org/0000-0002-0885-7928
https://orcid.org/0000-0002-0885-7928
References
- 1. Low TY, Hartman M, Chee CYJ, Mohankumar B, Ang SBL, San MT. et al. Restructuring the surgical service during the COVID-19 pandemic: experience from a tertiary institution in Singapore. Am J Surg. 2020;107:e252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. COVID-19 Personal Protective Equipment (PPE) [Internet]. GOV.UK; Published April 2020. Accessed July 11, 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe [Google Scholar]
- 3. Cardiff and Vale University Health Board & VUHB. Cardiff & vale university health board - CVUHB - COVID-19 [Internet]. Published March 2020. Accessed July 11, 2020. http://www.cardiffandvaleuhb.wales.nhs.uk/covid-19
- 4. Johnson RM, Vinetz JM. Dexamethasone in the management of Covid-19. BMJ. 2020;370:m2648. [DOI] [PubMed] [Google Scholar]
- 5. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55:105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liu M, Cheng SZ, Xu KW, Yang Y, Zhu QT, Zhang H. et al. Use of personal protective equipment against coronavirus disease 2019 by healthcare professionals in Wuhan, China: cross sectional study. BMJ. 2020;369:m2195. doi:10.1136/bmj.m2195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nepogodiev D, Bhangu A, Glasbey JC, Li E, Omar OM, Simoes JF. et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396:27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Diaz A, Sarac BA, Schoenbrunner AR, Janis JE, Pawlik TM. Elective surgery in the time of COVID-19. Am J Surg. 2020;219:900–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. RCS Survey Findings: PPE and Testing During the COVID-19 Pandemic [Internet]. Royal College of Surgeons; Published April 2020. Accessed July 11, 2020]. https://www.rcseng.ac.uk/coronavirus/survey-findings-ppe/ [Google Scholar]
- 10. Neville S, Foster P. How poor planning left the UK without enough PPE | free to read [Internet]. Published 2020. Accessed July 11, 2020. https://www.ft.com/content/9680c20f-7b71-4f65-9bec-0e9554a8e0a7
- 11. Coronavirus: Stay at Home, Protect the NHS, Save Lives - Web Version [Internet]. GOV.UK; Published March 2020. Accessed July 11, 2020. https://www.gov.uk/government/publications/coronavirus-covid-19-information-leaflet/coronavirus-stay-at-home-protect-the-nhs-save-lives-web-version [Google Scholar]
- 12. Ridd M, Shaw A, Lewis G, Salisbury C. The patient–doctor relationship: a synthesis of the qualitative literature on patients’ perspectives. Br J Gen Pract. 2009;59:e116–e133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Black JRM, Bailey C, Przewrocka J, Dijkstra KK, Swanton C. COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet. 2020;395:1418–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hourston GJM. The impact of despecialisation and redeployment on surgical training in the midst of the COVID-19 pandemic. Int J Surg. 2020;78:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mathai NJ, Venkatesan AS, Key T, Wilson C, Mohanty K. COVID-19 and orthopaedic surgery: evolving strategies and early experience. Bone Joint Open. 2020;1:160–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jain A, Jain P, Aggarwal S. SARS-CoV-2 impact on elective orthopaedic surgery: implications for post-pandemic recovery. J Bone Joint Surg Am. 2020;102:e68. [DOI] [PMC free article] [PubMed] [Google Scholar]