Abstract
The coronavirus disease 2019 (COVID-19) pandemic has catalyzed the rapid adoption of telemedicine which encompasses synchronous and asynchronous interactions between patients and providers. In order to facilitate this rapid deployment, there has been numerous regulatory changes to ensure caregivers can effectively communicate with patients during this time. We illustrate a model where people, processes, and technology work together to address the comprehensive needs of multiple sclerosis (MS) patients. We provide a template for how multidisciplinary, academic practices can implement a rapid shift to virtual management during the pandemic using existing infrastructure that can be widely adopted to care for patients with chronic diseases. Telemedicine was incorporated into our entire practice, which encompasses neurology, rehabilitation, advanced practice providers, fellows, social work, and behavioral medicine. Our patient satisfaction results remained stable across almost all domains when compared to survey results from our typical, in-office visits. Our experience demonstrates telemedicine’s transformative potential in successfully managing a multidisciplinary MS clinic during the time of a pandemic and outlines a potential path for other practices to follow.
Keywords: coronavirus disease 2019 (COVID-19), multiple sclerosis, patient experience, psychology, multidisciplinary care, telemedicine
Introduction
On March 11, 2020, the World Health Organization declared the coronavirus disease 2019 (COVID-19) outbreak a pandemic. In the face of a surge in COVID-19 cases, regulatory changes were made to facilitate more widespread use of telemedicine. The Centers for Medicare & Medicaid Services, payers, and institutions issued an array of waivers to allow providers the flexibility to care for patients virtually (1).
This surge in telemedicine is not particularly unique to COVID-19. Telemedicine has been effective in previous outbreaks including SARS-CoV (severe acute respiratory syndrome–associated coronavirus), MERS-CoV (Middle East respiratory syndrome coronavirus), and Zika (2). These initial programs focused primarily on acute care management including remote patient triage and monitoring. Less attention has been directed toward the comprehensive management of chronic conditions such as multiple sclerosis (MS), especially during the previous pandemics.
Multiple sclerosis generally requires lifelong comprehensive, multidisciplinary care to patients to support their physical, mental, and social needs. Unfortunately, MS patients have many barriers limiting their access to healthcare services, some of which are related to their accumulated disability such as impaired mobility, spasticity, cognitive dysfunction, and fatigue (3). Geographic distance and transportation are also significant obstacles for patients, especially those living in rural areas (4). Other factors such as family care responsibilities or work duties may interfere or delay much needed in-person visits. One potential solution to improve accessibility is through virtual or telemedicine programs. This would allow caregivers to provide health care services at a distant site, such as at the patient’s home or nursing facility (5). That being said, most telemedicine programs within neurology focus on stroke and neurocritical care with less resources dedicated to chronic care management (6).
The objective of this article is to describe how our multidisciplinary, academic practice at the Cleveland Clinic Mellen Center for MS Treatment and Research implemented a rapid shift to virtual, MS management during the pandemic using existing infrastructure that can be widely adopted within other practices. Our center includes neurology, physical medicine and rehabilitation (PM&R), social work, and behavioral medicine. This interdisciplinary care model is not unique to MS and the template we outline in this article can help other clinics transition their care during these challenging times. We offer a practical approach aimed to make virtual care more accessible while outlining some of the challenges we faced. We also analyzed patient satisfaction survey results comparing telemedicine encounters during the pandemic with standard in-office satisfaction survey results (gathered from visits prior to the pandemic). We use the term telemedicine to encompass any interactive audio and video interface between a patient and provider. We focused primarily on real-time, audio-video communication tools which is also referred to as virtual synchronous communication. We will also touch on other technologies such as patient messaging portals which are asynchronous forms of telemedicine.
Telemedicine Initiation
Our telemedicine services were originally implemented in 2015 (7). That infrastructure was leveraged to provide outpatient neurology services during the COVID-19 pandemic. Our center primarily utilized the Express Care Online telemedicine platform supported by American Well (Boston, Massachusetts) and paired with our electronic medical record (Epic; Verona, Wisconsin). The American Academy of Neurology has a COVID-19 resource center which has a curated database of materials including references on telemedicine practices (8). Insurance information and reimbursement is in constant flux during this time, but the America’s Health Insurance Plans has a useful website outlying payers’ current telemedicine coverage policy (9). Our organization has also published a COVID response digital playbook which outlines best practices for platforms, billing, and empathic communication (7,10). Other groups within our system have published their transition to telemedicine including epilepsy (11) and the neurological institute (12), which helps demonstrate that virtual services can be an option for outpatient neurological care.
Telemedicine Practices
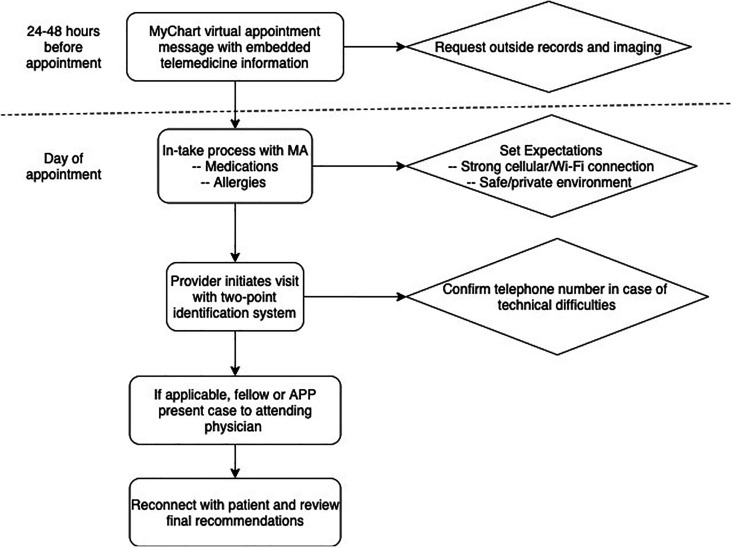
Important to the success of any patient engagement is standard processes to support the ideal experience. With that idea in mind, our workflow and staffing functions were quickly adapted to this new practice. Specifically, we tried to ensure the technology needed to connect providers and patients was ready prior to the appointment. First, our support staff would connect with patients through our messaging portal outlining the necessary steps to connect with their provider (Figure 1). Counseling patients about what to expect was foundational to their confidence. We found it to be helpful to reassure patients that they will have an opportunity to connect with a provider, whether virtual or by phone if any issues occur. We emphasized that patients needed access to a strong internet connection and a safe/private environment (ie, not operating a car or other machinery). Of note, our billing, prior authorizations, and managerial teams maintained their typical workflows but were also able to have successful transition to virtual roles.
Figure 1.
Typical workflow for telemedicine encounters. APP indicates advanced practice practitioner; MA, medical assistants.
Our medical assistants called patients prior to their scheduled visit and review their medications, check the allergies, and collect vital sign information such as weight and blood pressure. If the visit was completed using a video connection, we tried to maximize the available information including completing a comprehensive neurological examination (13). In MS, magnetic resonance imaging is important in understanding the disease status and this was easily enabled virtually simply by turning the camera view to the computer screen. If indicated, changes or modification to disease-modifying therapy were discussed. A major benefit of virtual platforms was the ability to engage family members and loved ones in the visit, with patient permission. For our new consultations, we focused on confirming the diagnosis of MS through a comprehensive review of the available clinical and radiographic information.
Less discussed, but critically important, was how to add multiple providers into one encounter. In our academic practice, we incorporate fellows and advanced practice providers (APP) into visits. Since the fellows, APPs, and attendings were in separate locations, this presented a significant obstacle. The most successful workflow was allowing the fellows or APPs to initiate the visit with the patient. Once the information was gathered from the patient, the encounter was paused and the case presented to the attending physician over the telephone. Once the assessment and plan were finalized, all parties could connect once again to discuss the plan.
Mellen Center Behavioral Medicine Response
Behavioral medicine providers have always been critical in helping our MS patients. During the pandemic, these practitioners were essential in managing the psychological impact of the pandemic as well as to staying connected to patients who may be at a higher risk of mental health disorders. While a range of emotions such as uncertainty, loneliness, fear, and anxiety are normal during this time, we were also seeing rises in anxiety prescriptions, domestic violence, and alcoholism. Therefore, mental health services were incorporated into the telemedicine format to serve the many needs of the patients.
The transition to behavioral medicine virtual care involved several important considerations including ethical, legal, state, and federal guidelines and policy from organization and professional litigating bodies. Clinical judgment balanced with person-centric care was essential in the practice of behavioral medicine telemedicine, and as such, we created a telemedicine protocol with inclusion/exclusion criteria for appropriateness to been seen. Initially, the protocols were much more exclusive; however, we realized the profound need for mental health services and tried to guide as many patients as we could throughout this process. To that end, we offered a range of types of virtual appointments including new evaluations, established visits, and group visits. All individual and group activities were transferred to virtual platforms as well. To see our full protocol, please see the study by Sullivan et al (14). Throughout the process, our ultimate goal was related to compassionate and patient-centered care.
Physical Medicine and Rehabilitation Response
The transition to telemedicine services for the PM&R patient population offered a valuable opportunity to overcome potential physical, logistic, or other challenges to on-site care especially for those living in long-term care facilities. For those patients living at home, telemedicine offered a unique glimpse at how a patient is physically functioning in his or her home environment. Physical medicine and rehabilitation offered remote therapeutic treatments tailored to each patient’s unique clinical picture. This included speech, physical and occupational therapies, and spasticity management, gait and transfer interventions, and fall risk reduction. These visits also afforded an opportunity to meet other members of the household who at times offered a different perspective of the patient’s needs and functional status. Some of the visit types such as intrathecal baclofen pump management and Botox injections were safely continued in the office setting following the Centers for Disease Control and Prevention and hospital guidelines to ensure a safe environment.
Patient Experience
Although telemedicine can address barriers to health care, the ultimate sign of success would be patients’ perception of care. In general, patients appreciated flexibility and access during these challenging times. Even if technical difficulties arose and the visit was transitioned to an audio only visit. Our patient satisfaction scores remained stable across almost all domains when compared to the results from traditional in-office evaluations (Table 1). This included questions on how providers conveyed empathy, participated in shared decision-making, and offered appropriate explanations around the planned medical evaluation. Many of these trends were consistent across the entire Neurological Institute. This broader trend is reassuring given the large number of patients surveyed across our institute (n = 1,637). The only question which resulted in a lower score was if patients would recommend our practice to others. For example, the telemedicine Mellen Center score was 82.3%, whereas our in-person results showed 86.2% of patients would recommend our practice to others. A similar response was true across all practices. Future studies are needed to determine patient perspectives on MS care delivery to better determine when to provide virtual versus in-person care and to identify patient concerns.
Table 1.
Patient Satisfaction Survey Results Comparing Office Visits to Telemedicine Encounters.a
| Office Encounter (n = Number of Patients) | CP Explanation | CP Empathy | CP Share Decision-Making | CP Treatment Discussion | Courtesy of CP | Ease of Scheduling | Recommend Practice to Others | Staff Working Together |
|---|---|---|---|---|---|---|---|---|
| Mellen telemedicine (n = 105) | 92.4 | 96.2 | 95.2 | 95.1 | 98.1 | 76.0 | 82.3 | 87.0 |
| Mellen office (n = 471) | 87.3 | 89.1 | 87.9 | 85.7 | 91.0 | 72.3 | 86.2 | 82.1 |
| Behavioral health telemedicine (n = 8) | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 87.5 | 75.0 | 85.7 |
| Behavioral health office (n = 14) | 92.9 | 92.9 | 92.3 | 92.9 | 92.9 | 57.1 | 76.9 | 75.0 |
| PM&R telemedicine (n = 6) | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 80.0 | 100.0 |
| PM&R office (n = 62) | 87.7 | 90.8 | 95.4 | 90.2 | 95.4 | 74.2 | 93.8 | 92.1 |
| Neurological Institute telemedicine (n = 1,637) | 90.6 | 88.2 | 86.4 | 92.7 | 89.8 | 71.8 | 72.0 | 78.3 |
| Neurological Institute office (n = 7534) | 88.0 | 86.2 | 84.9 | 89.3 | 87.8 | 68.2 | 84.8 | 80.3 |
Abbreviations: CP, care provider; PM&R, physical medicine and rehabilitation.
a The values represent the percentage of patients giving the highest possible response to each question.
Conclusion
The COVID crisis is multidimensional in its impact including physically, economically, socially, and psychologically. The utilization of telemedicine has allowed us to continue to provide care while keeping patients and health providers safe during the outbreak. Implementation of telemedicine into chronic disease management will likely prove vital for our healthcare system going forward. In the long term, it has the potential to improve population health and patient care and lower healthcare costs. Yet this rapid deployment has presented many challenges to providers and patients alike. We provide a model for other multispecialty clinics to quickly pivot their care during these challenging times. Providing care virtually adds value to MS patients because it enables continuity of longstanding relationships and helps overcome geographic and physical disability barriers, which are common issues in this population. Although the platform may be different, the caring that encompasses person-centered care is still the same.
Lessons Learned
Communication is key, both interpersonal and operational for telemedicine to succeed.
Flexibility is needed by both the patient and the provider as the pandemic realities were changing day to day.
Group telemedicine visits are a transformative option of care to enhance access, experience, and operations in MS.
Author Biographies
Justin R Abbatemarco is a neuroimmunology fellow at the Cleveland Clinic Mellen Center for Multiple Sclerosis Treatment and Research. He has an interest in a wide spectrum of autoimmune neurological disorders with active research in multiple sclerosis and autoimmune encephalitis.
Jennifer Hartman is a physician assistant at the Cleveland Clinic Mellen Center for Multiple Sclerosis Treatment and Research. She has a particular interest in physical medicine and rehabilitation with a particular focus on spasticity management.
Marisa McGinley is an assistant professor of Neurology at the Cleveland Clinic Mellen Center for Multiple Sclerosis Treatment and Research. She has a particular focus on patient wellness and distance health platforms.
Robert A Bermel is the director of Cleveland Clinic Mellen Center for Multiple Sclerosis Treatment and Research Center. He has a particular interest in advanced imaging methods to evaluate and improve recovery from inflammatory demyelinating disease.
Adrienne Boissy is the chief experience officer of Cleveland Clinic Health System and also a staff neurologist at the Mellen Center for Multiple Sclerosis Treatment and Research. She has a particular focus on patient wellness.
Desiree T Chizmadia is a physician assistant at the Cleveland Clinic Mellen Center for Multiple Sclerosis Treatment and Research. She has a particular interest in multiple sclerosis management.
Amy B Sullivan is the director of Behavioral Medicine at the Mellen Center for MS Treatment and Research. She has particular research interests on pain, exercise and behavioral medicine.
Mary R Rensel is an assistant professor of Neurology at the Cleveland Clinic Mellen Center for Multiple Sclerosis Treatment and Research while directing the Pediatric MS and the Wellness programming at the Mellen Center. She has a particular focus on patient and physician wellness along with neuromyelitis optica spectrum disorders.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Justin R Abbatemarco, MD  https://orcid.org/0000-0003-1668-4753
https://orcid.org/0000-0003-1668-4753
Amy B Sullivan, PsyD  https://orcid.org/0000-0001-7723-8218
https://orcid.org/0000-0001-7723-8218
References
- 1. Physicians and other clinicians: CMS flexibilities to fight COVID-19. Centers for Medicare & Medicaid Services; 2020. [PubMed] [Google Scholar]
- 2. Ohannessian R. Telemedicine: potential applications in epidemic situations. Eur Res Telemed. 2015;4:95–8. [Google Scholar]
- 3. Chiu C, Bishop M, Pionke JJ, Strauser D, Santens RL. Barriers to the accessibility and continuity of health-care services in people with multiple sclerosis: a literature review. Int J MS Care. 2017;19:313–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Buchanan RJ, Stuifbergen A, Chakravorty BJ, Wang S, Zhu L, Kim M. Urban/rural differences in access and barriers to health care for people with multiple sclerosis. J Health Hum Serv Adm. 2006;29:360–75. [PubMed] [Google Scholar]
- 5. Zissman K, Lejbkowicz I, Miller A. Telemedicine for multiple sclerosis patients: assessment using health value compass. Mult Scler. 2012;18:472–80. [DOI] [PubMed] [Google Scholar]
- 6. George BP, Scoglio NJ, Reminick JI, Rajan B, Beck CA, Seidmann A, et al. Telemedicine in leading US neurology departments. Neurohospitalist. 2012;2:123–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ross L, Bena J, Bermel R, McCarter L, Ahmed Z, Goforth H, et al. Implementation and patient experience of outpatient teleneurology. Telemed J E Health. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. American Academy of Neurology. AAN’s COVID-19 Neurology Resource Center. 2020. Accessed May 22, 2020. https://www.aan.com/tools-and-resources/covid-19-neurology-resource-center/
- 9. AHIP. 2020. Accessed May 22, 2020, https://www.ahip.org/health-insurance-providers-respond-to-coronavirus-covid-19/
- 10. Clinic Clinic. Cleveland Clinic COVID-19 Response Digital Health Playbook. 2020. Accessed May 22, 2020. https://my.clevelandclinic.org/-/scassets/files/org/landing/preparing-for-coronavirus/covid-response-digital-health-playbook.ashx?la=en
- 11. Punia V, Nasr G, Zagorski V, Lawrence G, Fesler J, Nair D, et al. Evidence of a rapid shift in outpatient practice during the COVID-19 pandemic using telemedicine. Telemed J E Health. 2020;26:1301–3. [DOI] [PubMed] [Google Scholar]
- 12. McGinley MP, Ontaneda D, Wang Z, Weber M, Shook S, Stanton M, et al. Teleneurology as a solution for outpatient care during the COVID-19 pandemic. Telemed J E Health. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Evans DA, Benameur K, Busis NA. Telemedicine and COVID-19: American Academy of Neurology. 2020. Accessed May 22, 2020. https://www.aan.com/siteassets/home-page/tools-and-resources/practicing-neurologist--administrators/telemedicine-and-remote-care/20200326-telemedicine-and-covid-19-final.pdf
- 14. Sullivan AB, Kane A, Roth AJ, Davis BE, Drerup ML, Heinberg LJ. The COVID-19 crisis: a mental health perspective and response using telemedicine. J Patient Exp. 2020;7:295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]