Abstract
The spread of COVID-19 in the United States has led to the use of virtual visits in lieu of in-person care for the high-risk population of patients in rheumatology. We asked patients to score their satisfaction with these visits and if they would have preferred in-person care instead. Of 679 patients seen in May 2020, 512 (75.4%) were virtual (267 [52.1%] by telephone and 245 [47.9%] by video), and 359 (70%) responded to the survey. The majority of patients (74%) were satisfied with their virtual visit, but they were more likely to be satisfied if their visit was over video rather than phone. They preferred an in-person visit if they were meeting a doctor for the first time, and patients who required a language interpreter were significantly less satisfied with virtual care. There was no correlation of age, sex, diagnosis, or testing ordered with satisfaction. The main concern against virtual care was the inability to have a physical exam, while the main reasons in favor of it were avoidance of potential infection and convenience.
Keywords: telemedicine, access to care, patient satisfaction, rheumatology, COVID-19
Introduction
The SARS-CoV-2 virus-related illness (COVID-19) was first reported in the United States in February 2020. Rheumatologists were faced with the challenge of keeping high-risk, immunosuppressed, and frequently elderly patients safe from infection while also continuing to deliver care for their chronic conditions and monitor high risk medications (1).
The use of telemedicine to increase access to care in rheumatology had been a lingering topic for years (2). Even though telemedicine had previously been shown to be both a cost-effective and time-saving mode of care delivery (3 -6), its overall uptake in rheumatology had been sluggish (7). Prepandemic studies had even suggested that rheumatology patients preferred an in-person visit to telemedicine, even when travel was noted to be inconvenient (8).
During the pandemic, telemedicine, both via video and telephone, became necessary almost overnight, to accommodate the needs of our patients while mitigating the risks of infection. This usage of telemedicine was facilitated by changes to HIPAA restrictions by the Centers for Medicare and Medicaid Services in allowing the use of commercial video communication platforms (9,10), and many commercial health insurance plans waiving patient co-pays for telemedicine encounters.
While the rheumatology patient population has been graciously nimble with adapting to these changes, assessing their satisfaction with telemedicine is important; studies on rheumatology patient satisfaction with telemedicine prior to the pandemic were scarce and had small sample sizes (11). Furthermore, the literature has not traditionally delineated satisfaction with telephone versus video encounters. The current study was done at the peak of the first wave of the pandemic in New York state, when most patients automatically had their appointments switched to virtual care (telephone or video). The goal was to get an impression of whether patients were satisfied with these virtual visits and whether they would have chosen to have a virtual or an in-person visit if given the choice.
Methods
We retrospectively collected patient encounter data for the 4-week period from May 1 to May 29, 2020, among 3 rheumatologists at the Rochester Regional Health Rheumatology office. The study was approved by the hospital’s institutional review board. We initially attempted to utilize the electronic medical records portal email system to contact patients, but we did not receive many responses. Therefore, every patient who had a virtual visit during the study period was contacted by phone by the study staff, on average 2 to 6 weeks after the actual encounter. Patients provided verbal informed consent to be in the study.
The appointment type (in-person, telephone, or video) was recorded. Both telephone and video visits were qualified as “telemedicine,” and patient satisfaction was assessed. Video encounters were completed using the following third-party vendors: Epic Warp (EHR), Skype, FaceTime (Apple), and Doximity depending on patient preference. We counted the number of patients who had an in-person visit during the study period, but they were not contacted.
For the telemedicine visits, the following were collected: new patient (NP) versus follow-up (FU) encounter, sex, age, primary rheumatologic diagnosis, presence or absence of fibromyalgia, biologic therapy status, and whether or not laboratory or imaging was ordered during the encounter. Patients who required a language interpreter for communication were called with the assistance of a telephone interpreter on a 3-way phone call. Study patients were asked to respond to the following statements:
I was satisfied with my telemedicine encounter
-
I would have preferred an in-person visit instead of a telemedicine visit
Comment on the reason behind your answer to question number 2
A Likert scale from 1 to 5 (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree) was utilized for statement number 1. A binary yes or no answer was indicated for statement number 2, and then the patient commented freely on their reasoning for their answer.
Data were reported as absolute numbers for continuous variables and percentages for categorical variables. Statistical analysis was performed with R Software (R Core Team, 2020). Numerical regression and analysis of variance were performed to test the relationship between the independent variables (age, sex, primary diagnosis, secondary fibromyalgia, whether patient was on biologics, need for an interpreter, and whether diagnostic tests were ordered during a visit) and patient satisfaction scores. The answer to question 1 was looked at as a top 2 box (T2B) score (pooled % scores 4 and 5), versus neutral (% score 3), and versus bottom 2 box (B2B) score (% scores 1 and 2) satisfaction scores. We pooled the data in this fashion to gain an overall positive, neutral, or negative impression of the patient’s experience. Finally, the comments patients made as to the reason they preferred either visit type were divided into recurring themes and codified in order to allow analysis as a nominal variable. This codification into recurring themes was performed by one study staff member for all patients for consistency.
Results
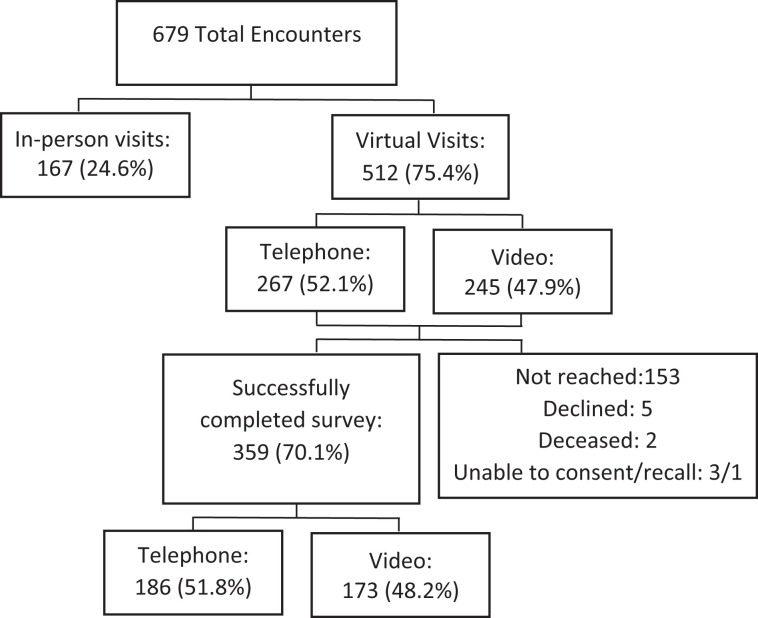
A total of 679 encounters occurred during the study period (see Figure 1). Of these, 167 (24.6%) were seen in person, and 512 (75.4%) were evaluated via telemedicine. The 512 virtual visits included 267 (52.1%) telephone visits and 245 (47.9%) video visits. A total of 359 of the 512 (70.1%) patients responded to the patient satisfaction phone survey. Of the patients not included in the survey response, 2 patients were deceased, 1 patient could not recall the encounter, 3 patients were unable to consent, 5 patients declined to participate, and 153 could not be reached. Of the 359 patients who completed the phone survey, 320 (89.1%) were FU visits, 39 (10.8%) were NP encounters, 186 (51.8%) were by phone, and 173 (48.2%) were conducted over video.
Figure 1.
Patient recruitment.
Table 1 shows patient characteristics. There were 294 (81.9%) female patients, and the median age was 59 years old (range 21-93). The primary diagnoses were representative of those seen in rheumatology clinics and are also detailed in Table 1. Of the patients surveyed, 85 (23.7%) had a concomitant diagnosis of fibromyalgia, 264 (73.5%) were on synthetic disease modifying oral agents alone, and the remaining 95 (26.5%) were on advance therapy (biologic agent or a Janus Kinase inhibitor). There were 24 (6.7%) patients who needed a foreign language interpreter to communicate; the languages interpreted included Spanish, Arabic, Nepali, and Moldovan. Additional testing such as laboratory data, imaging, or nerve conduction studies were ordered in 210 (58.5%) of the encounters.
Table 1.
Characteristics of the 359 Patients Who Responded to the Telephone Survey.a
| Characteristic | No. (%) |
|---|---|
| Female | 294 (81.9) |
| Telephone | 186 (51.8) |
| Video | 173 (48.2) |
| Follow-up | 320 (89.1) |
| New patient | 9 (10.8) |
| DMARD | 264 (73.5) |
| Biologic medication | 95 (26.5) |
| Translator needed | 24 (6.7) |
| Testing ordered | 210 (58.5) |
| Primary diagnosis | No. (%) |
| Rheumatoid arthritis | 141 (39.4) |
| Osteoarthritis | 39 (10.9) |
| Systemic lupus | 30 (8.4) |
| Spondyloarthritis | 30 (8.4) |
| Psoriatic arthritis | 21 (5.9) |
| UCTD | 20 (5.6) |
| Fibromyalgia | 17 (4.7) |
| Sjogren’s disease | 16 (4.5) |
| Vasculitis | 14 (3.9) |
| Gout | 10 (2.8) |
| PMR | 7 (2.0%) |
| Pseudogout | 5 (1.4) |
| Scleroderma | 4 (1.1) |
| Myositis | 3 (0.8) |
| Sarcoidosis | 1 (0.3) |
| Bechet’s | 1 (0.3) |
Abbreviations: DMARD, disease modifying anti-rheumatoid drug; UCTD, undifferentiated connective tissue disease; PMR, polymyalgia rheumatica.
a) Median age was 59 years old (range 21-93).
The response to statement 1 is summarized in Table 2. Overall, 266 (74%) of patients chose a T2B score for their experience, indicating a positive overall impression. Of the remaining patients, 52 (14.5%) were neutral about their experience, and 41 (11.4%) indicated a B2B score, implying they were not satisfied with their virtual encounter.
Table 2.
Patient Response to the Statement I was Satisfied With My Telemedicine Encounter on a Likert Scale.a
| Response | No. (%) |
|---|---|
| Agree/strongly agree | 266 (74) |
| Neutral | 42 (14.5) |
| Disagree/strongly disagree | 41 (11.4) |
| Correlation between patient/encounter characteristics and satisfaction score | |
| Characteristics | P value |
| Video vs telephone | .0045b |
| Needed interpreter | .0011b |
| Age | .32 |
| Sex | .62 |
| NP vs FU | .35 |
| Primary diagnosis | .27 |
| Fibromyalgia | .48 |
| Tests were ordered | .53 |
| Biologics use | .84 |
Abbreviations: FU, follow-up encounter; NP, new patient encounter.
a n = 359.
b Statistical significance.
We found that patients were more satisfied with video versus telephone visits (T2B 80.9% vs 68.3%; neutral 11% vs 17.2%; and B2B 8.1% vs 14.5%). The difference between phone and video satisfaction rates was statistically significant (P = .0045). There was also a notable difference between the satisfaction score of patients who needed an interpreter to communicate with their doctor and study staff versus those who did not (T2B 58.3% vs 75.2%; neutral 8.3% vs 14.4%; and B2B 33.4% vs 9.9%). The difference between these 2 groups was also statistically significant (P = .0011). The remainder of the independent variables we looked at (age, sex, NP/FU, primary diagnosis, presence of fibromyalgia, ordering further testing, or whether patient was on advanced therapy) did not show a correlation with patient satisfaction scores.
In their response to statement 2, 54.3% of patients stated yes, they would have preferred an in-person appointment, while 45.6% said no (meaning they would have chosen telemedicine). We tried to find out if there was a relationship between the answer to statement 2 and their satisfaction with their experience (statement 1). Of the patients in the dissatisfied category, 91.4% said that they would have preferred an in-person visit. Interestingly, even in patients who were satisfied with telemedicine, 40.6% stated that they would have preferred an in-person appointment. Furthermore, NPs were more likely to state a preference for in-person visit over a virtual visit, and the difference was statistically significant (P = .01). The remainder of the independent variables did not correlate with the patient’s preference for telemedicine or in-person visits. Of note, the need for an interpreter and NP versus FU also did not meet statistical significance but were closer than the other variables (see Table 3).
Table 3.
Patient’s Response to the Statement I Would Have Preferred an In-Person Visit Instead, as Either Yes or No and the Reason They Provided for This Choice.
| Response | No. (%) | Reason provided | No. (%) |
|---|---|---|---|
| Yes | 195 (54.3) | Wants physical exam | 72 (36.9) |
| Communicate better in person | 51 (26.8) | ||
| First time meeting this doctor | 25 (12.8) | ||
| Believed better care is delivered in person | 14 (7.2) | ||
| Wants joint injection | 10 (5.1) | ||
| Language difficulty | 8 (4.1) | ||
| Technology issues | 7 (3.6) | ||
| No comment | 7 (3.6) | ||
| No | 164 (45.6) | Avoid COVID-19 | 35 (21.3) |
| Telemedicine is more convenient | 26 (15.9) | ||
| Telemedicine ok for routine follow-ups | 43 (26.2) | ||
| No comment | 60 (36.6) | ||
| Correlation between patient/encounter characteristics and yes/no answer | |||
| Characteristics | P value | ||
| Video vs tele | .08 | ||
| Needed interpreter | .09 | ||
| Age | .23 | ||
| Sex | .95 | ||
| NP vs FU | .01a | ||
| Primary diagnosis | .60 | ||
| Fibromyalgia | .98 | ||
| Tests were ordered | .87 | ||
| Biologics use | .46 | ||
Abbreviations: FU, follow-up encounter; NP, new patient encounter.
a Statistical significance.
The third statement in our survey invited the patients to comment on why they had expressed preference for telemedicine or an in-person visit. Of the patients who preferred telemedicine, 35/164 (21.3%) were concerned about exposure and infection with SARS-COV-2; 26/164 (15.9%) liked the increased convenience in terms of schedule and commute; 43/164 (26.2%) reported telemedicine was appropriate for routine visits, but they would want an in-person visit for an acute issue; and 60/164 (36.6%) left no comment. On the other hand, the 195 patients who preferred an in-person visit, provided the following reasons: 72 (36.9%) wanted to have a physical exam and vitals taken, 51 (26.8%) felt that they were able to communicate better in person, 25 (12.8%) reported that it was their first time meeting this particular physician and they would have preferred an in-person introduction, 14 (7.2%) felt that they would have received superior care in person, 10 (5.1%) wanted to have a joint injection, 8 (4.1%) reported difficulties communicating with their doctor through a telephone language interpreter, 7 (3.6%) struggled with the technology needed for telemedicine, and 7 (3.6%) did not comment.
Discussion
Social distancing measures placed in the spring of 2020 during the COVID-19 pandemic lead to the use of telemedicine by both phone and video in the rheumatology clinic in proportions that had never been done previously. In fact, many of our patients had their appointments automatically switched to a virtual visit during the early days of the pandemic. We studied patient impressions of telemedicine encounters to identify advantages and challenges in utilizing this mode of care delivery. A report from the Hospital for Special Surgery in New York showed that their use of telemedicine during the pandemic peaked in May 2020; this is the same period during which we assessed patient satisfaction (12).
The majority of patients in this study were satisfied with their telemedicine encounter, but those who got to “see” their rheumatologist by video were more likely to express satisfaction than those who had their visit over the phone. This is likely because a video encounter is a closer approximation of a traditional in-person visit and allows for better nonverbal communication. Additionally, patients can demonstrate some physical exam findings to their physician on camera. All of the rheumatologists in our group shared anecdotes, that especially early in the pandemic, many older patients and those who did not readily have access to smartphones and internet could only be contacted by telephone. Some visits, which were initially planned as a video, had to be conducted by telephone when the patient had trouble connecting. Based on our findings, we would not recommend scheduling patients for telephone visits as a first choice, but continuing to offer telephone as an option is important in terms of health equity and access to care for all patients.
Despite the high degree of patient satisfaction, the majority of patients reported that given the choice, they would select to have an in-person visit rather than a virtual one. The biggest concern they expressed in this regard was that they felt it was very important for their doctor to examine them.
A study by Cavagna et al early in the pandemic examined which patients in the rheumatology clinic would be willing to accept telemedicine as an option over an in-person visit (13). Of the 175 patients, they interviewed in March of 2020, 137 (78%) patients were willing to have a telemedicine visit. They found that patients who lived further away and with more advanced education were more likely to accept telemedicine in place of an in-person visit and that a diagnosis of undifferentiated connective tissue disease inversely correlated with acceptance of telemedicine. Another study of 469 patients out of Spain reported that patient satisfaction correlated with their level of education, whereas physician satisfaction with telemedicine correlated with the patient’s ability to successfully navigate connecting through the internet (14). We did not find a diagnosis-specific correlation with satisfaction. Also, our patients were being interviewed after they had actually experienced a virtual visit and only 45.6% indicated that they would have chosen a virtual visit if given the option. Moreover, many of our patients who said they are ok with the virtual care indicated that fear of infection was their main deciding factor. This highlights the fact that while telemedicine is an incredible bridging tool for care now and after the pandemic, patients do not view it on par with their in-person experience. Post-pandemic triage of patients for telemedicine should also take into account our finding that patients who knew their physician well from in-person interactions felt more comfortable having a virtual encounter for routine FUs.
In a study from March 2020 performed in Poland, 244 rheumatology patients were surveyed regarding their attitude toward telemedicine (15). The lack of ability to perform additional testing and to be physically examined by the rheumatologists were the most frequently reported concerns regarding virtual consultation for their patients. Similarly, our study identified physical exam as the primary reason patients prefer an in-person visit, but we did not find that the physician’s decision to order further test during the visit actually impacted the patient’s perceived satisfaction. An unstructured telephone interview with 12 patients at the University of Alabama Rheumatology clinic on the subject of telemedicine highlighted similar themes to our study, including fear of infection being the main driver toward accepting telemedicine during the pandemic and the desire for having a physical exam performed (16). Of note, they only interviewed patients whose primary language was English.
Many of the studies on patient satisfaction in rheumatology exclude individuals who need an interpreter. A previously underreported finding of ours was that patients requiring interpreters were less satisfied with a virtual visit. We suspect this is also due in part to decreased nonverbal cues during virtual visits. Decreased sound clarity or temporary technological glitches can also further complicate an existing language barrier. The challenge of caring for patients who need interpreters is an important consideration for the wider application of telemedicine during and postpandemic.
One of the strengths of our study is that we were able to look at a large number of telemedicine encounters in a brief period of time and had a high response rate to our survey, making this one of the most extensive studies of telemedicine in rheumatology to date. The majority of our patients were female, which is representative of patients with autoimmune disease. We were also able to include a representative sample of rheumatologic diseases.
We acknowledge some limitations to our analysis, the first of which is its retrospective nature. Furthermore, the majority of our patients were scheduled for FU visit with only 10% of the telemedicine visits marked as an NP encounter. The explanation for this is that patients were preferentially offered in-person NP visits, and these were not included in this study. Additionally, patients with preexisting negative opinions of telemedicine may have insisted on in-person visits and therefore not been included in this study. The use of a 3-question method allowed us to collect targeted information to facilitate decision-making in regard to scheduling a patient for in-person versus virtual care and assess a larger number of patients. Some of the patients seen in a FU appointment were meeting a new physician due to physician retirement, and these patients may have been less satisfied with telemedicine due to transitioning to a new physician. The number of patients who required an interpreter was also small and may have impacted statistical analysis. Lastly, we did not compare telemedicine visits to in-person encounters and acknowledge that this information may have offered further insight into patient impressions of telemedicine. We also expect that patient impressions of telemedicine may differ during the COVID-19 pandemic versus before and after.
Telemedicine will be an increasing rheumatology access option in both ambulatory and inpatient settings going forward. This analysis provides insight into patient impressions of telemedicine. New rheumatology patients and those requiring an interpreter may be best served by an in-person visit, whereas routine rheumatologic FU visits may be convenient for a virtual encounter. Our work adds to the growing body of telemedicine literature that will help optimize rheumatology care and visit type.
Author Biographies
Mahta Mortezavi is a physician in the department of allergy, immunology and rheumatology at the Rochester general hospital, Rochester, NY, USA.
Sravani Lokineni is a resident in the department of internal medicine at the Rochester general hospital, Rochester, NY, USA with a keen interest in allergy, immunology and rheumatology.
Megha Garg is a physician in the department of allergy, immunology and rheumatology at the Rochester general hospital, Rochester, NY, USA.
Ya Li Chen is a physician in the department of allergy, immunology and rheumatology at the Rochester general hospital, Rochester, NY, USA.
Allison Ramsey is a physician in the department of Allergy and immunology at the Rochester general hospital, Rochester, NY, USA.
Footnotes
Authors’ Note: Ethical approval for this study was obtained from Rochester Regional Health Institutional Review Board (Approval Number: IRB2002A Mortezavi). Ethical approval to report this study was obtained from Rochester Regional Health Institutional Review Board (Approval Number: IRB2002A Mortezavi). All procedures in this study were conducted in accordance with the Rochester Regional Health Institutional Review Board (Approval Number: IRB2002A Mortezavi). All procedures in this study were conducted in accordance with the Rochester Regional Health Institutional Review Board (Approval Number: IRB2002A Mortezavi). Verbal informed consent was obtained from the patients for their anonymized information to be published in this article.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Dr Mortezavi was only in clinical practice at the time the study was conducted and adjudicated and now also serves as a Medical Director for Pfizer Inflammation and Immunology. Dr Ramsey is on Speaker’s bureau for Sanofi/Regeneron, where she lectures on asthma and atopic dermatitis.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Mahta Mortezavi, MD  https://orcid.org/0000-0003-4666-071X
https://orcid.org/0000-0003-4666-071X
References
- 1. Nune A, Iyengar K, Ahmed A, Sapkota H. Challenges in delivering rheumatology care during COVID-19 pandemic. Clin Rheumatol. 2020;39:2817–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Battafarano DF, Ditmyer M, Bolster MB, Fitzgerald JD, Deal C, Bass AR, Molina R, Erickson AR, Hausmann JS, Klein-Gitelman M, Imundo LF, Smith BJ, Jones K, Greene K, Monrad SU. 2015. American College of Rheumatology Workforce Study: Supply and Demand Projections of Adult Rheumatology Workforce, 2015-2030. Arthritis Care Res (Hoboken). 2018;70(4):617–626. [DOI] [PubMed] [Google Scholar]
- 3. Kessler EA, Sherman AK, Becker ML. Decreasing patient cost and travel time through pediatric rheumatology telemedicine visits. Pediatr Rheumatol Online J. 2016;14:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wood PR, Caplan L. Outcomes, satisfaction, and costs of a rheumatology telemedicine program: a longitudinal evaluation. J Clin Rheumatol. 2019;25:41–44. [DOI] [PubMed] [Google Scholar]
- 5. Davis P, Howard R, Brockway P. Telehealth consultations in rheumatology: cost-effectiveness and user satisfaction. J Telemed Telecare. 2001;7:10–11. [DOI] [PubMed] [Google Scholar]
- 6. Poulsen KA, Millen CM, Lakshman UI, Buttner PG, Roberts LJ. Satisfaction with rural rheumatology telemedicine service. Int J Rheum Dis. 2015;18:304–14. [DOI] [PubMed] [Google Scholar]
- 7. Lewtas J. Telemedicine in rheumatology. J Rheumatol. 2001;28:1745–6. [PubMed] [Google Scholar]
- 8. Bullock DR, Vehe RK, Zhang L, Correll CK. Telemedicine and other care models in pediatric rheumatology: an exploratory study of parents’ perceptions of barriers to care and care preferences. Pediatr Rheumatol Online J. 2017;15:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. American Health Insurance Plans (AHIP). Health Insurance Providers Respond to COVID-19. 2020. Accessed April 5, 2021. https://www.ahip.org/health-insurance-providers-respond-to-coronavirus-covid-19/ [Google Scholar]
- 10. US Department of Health and Human Services. Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency 2020. Accessed April 5, 2021. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html [Google Scholar]
- 11. Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. BMJ. 2000;320:1517–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gkrouzman E, Wu DD, Jethwa H, Abraham S. Telemedicine in rheumatology at the advent of the COVID-19 pandemic. HSS J. 2020;16:108–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cavagna L, Zanframundo G, Codullo V, Pisu MG, Caporali R, Montecucco C. Telemedicine in rheumatology: a reliable approach beyond the pandemic. Rheumatology (Oxford). 2021;60(1):366–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tornero-Molina J, Sanchez-Alonso F, Fernandez-Prada M, Bris-Ochaita ML, Sifuentes-Giraldo A, Vidal-Fuentes J. Tele-rheumatology during the COVID-19 pandemic. Reumatol Clin. 2020: S1699–258X(20)30240-0. English, Spanish. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Opinc A, Lukasik Z, Makowska J. The attitude of Polish rheumatology patients towards telemedicine in the age of the COVID-19 pandemic. Reumatologia. 2020;58:134–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hall AG, Kim DH, Rainey C, Singh JA. Telemedicine including video-based visits in rheumatology in COVID-19 pandemic: not yet ideal. J Clin Rheumatol. Epub ahead of print 1 December 2020. doi: 10.1097/RHU.0000000000001690. [DOI] [PMC free article] [PubMed] [Google Scholar]