Abstract
To become a proactive and informed partner in postacute coronavirus disease 2019 (COVID-19) management, patients need to have the knowledge, skills, and confidence to self-manage COVID-19-related health challenges. Due to several restrictions and consequently social isolation, online platforms and forums where people can share information and experiences became more popular and influential. Therefore, this study aimed to identify perceived information needs and care needs of members of 2 Facebook groups for patients with COVID-19 and persistent complaints in the Netherlands and Belgium and patients with COVID-19 who registered at a website of the Lung Foundation Netherlands. Besides demographics and clinical characteristics, the degree of satisfaction with care during and after the infection as well as satisfaction with available information were assessed. Open text fields revealed specific information needs which were summarized. Patients with confirmed or suspected COVID-19 perceive various unmet needs varying from specific information needs (eg, information about permanent lung damage) to general needs (eg, being heard and understood). These data lead to several recommendations to improve care for patients with COVID-19 and justify further development of online platforms specifically addressing these unmet needs.
Keywords: COVID-19, corona, unmet needs, information needs, long-term symptoms, social support
Introduction
By the end of 2019, the World Health Organization was informed of cases of pneumonia of unknown etiology which turned out to be coronavirus disease 2019 (COVID-19) (1). Till now, COVID-19 has been confirmed in millions of people around the world (2). Furthermore, due to limited testing capacity, a clinical status which was considered not severe enough to be tested or to be hospitalized, or symptoms unknown at the time, there were many cases with suspected COVID-19. The majority of these patients was treated at home and symptoms were managed expectantly. Remarkably, part of these patients suffer from persistent symptoms (3) and report an impaired quality of life (4) emphasizing the complexity and severity of post-COVID-19 symptom burden.
A qualitative study revealed that COVID-19 patients are worried about an incomplete recovery of their health (5). This may, at least in part, be due to the fact that patient’s knowledge about COVID-19 and the subsequent recovery process is limited. Indeed, to become a proactive and informed partner in post-COVID-19 management, patients need to have the knowledge, skills, and confidence to self-manage COVID-19-related health challenges (6). Due to several restrictions (eg, no large events and meetings, people were encouraged to work from home, many public places were closed, etc) and consequently social isolation, online platforms and forums where people can share information and experiences became more popular and influential. Especially during public health crises, like the COVID-19 pandemic, risk perception is elevated and patients rely even more on information from social media (7,8). Therefore, this study aimed to identify perceived information needs and care needs of patients with COVID-19 and persistent complaints who are members of online support groups.
Methods
Members from 2 Facebook groups for coronavirus patients with persistent complaints in the Netherlands (∼11 000 members; “Corona ervaringen en langdurige klachten!”) (9) and Flanders (Belgium, ∼1200 members; “Corona patiënten met langdurige klachten [Vlaanderen]”) (10) as well as ∼1200 people who registered at a website of the Lung Foundation Netherlands (www.coronalongplein.nl), a platform for patients with respiratory complaints after COVID-19, were invited to complete an online survey between June 4 and June 11, 2020.
Demographics, marital status, educational level, smoking status, and self-reported pre-existing comorbidities were assessed. Furthermore, the survey contained questions about
℃ hospitalization at the time of the infection,
℃ confirmation of COVID-19 diagnosis for the nonhospitalized patients by physician based on computed tomography scanning/reverse transcription polymerase chain reaction,
℃ confirmation of COVID-19 diagnosis for the nonhospitalized patients by physician based on symptoms, and
℃ no confirmed diagnosis.
Symptoms during the onset of infection as well as during follow-up were assessed. Patients were asked if they were worried about an incomplete recovery following the infection. Experience of support from family members, friends, employer, and colleagues for the current situation was rated by patients as follows: not applicable, rarely or never, occasionally, regularly, or very often.
Data are presented as mean and standard deviation or frequencies and proportions, as appropriate.
Care Needs
Satisfaction with care during and after the infection (aftercare) were rated: I did not need any care, very satisfied, satisfied, dissatisfied, or very dissatisfied. Patients who were very dissatisfied could choose the following reasons: I did not receive any care, I did not feel heard, my concerns have not been taken seriously, I could not consult my general practitioner (GP), or I could not consult a medical specialist.
Information Needs
Respondents were asked to indicate their satisfaction with the information available about COVID-19: no need for information about COVID-19, very satisfied, satisfied, dissatisfied, and very dissatisfied. Patients who were satisfied, dissatisfied, or very dissatisfied had the opportunity to enter further specific information needs in an open-text field. Answers were summarized with 1 or 2 words finally leading to 11 general topics:
future (future prospects, permanent lung damage, aftermath),
clarity (clear, coherent information),
aftercare ([support during] recovery),
“mild” COVID-19 ((course of) “mild” COVID-19 without hospitalization),
support (recognition, understanding, social support, contact with fellow sufferers),
follow-up (feedback/follow-up by GP/medical specialist, medical expertise),
testing (testing, certainty, immunity),
tips (advices, exercises, tips to exercise at home, recovery support),
research (future research, new insights, knowledge development),
unknown (much still remains unclear), and
other.
Coding of 100 answers has been randomly checked by JMD and RM (50 each). Disagreement (<5%) has been discussed until consensus was reached. Informative, appropriate quotes from the open-text fields were manually selected for each group to further illustrate patients’ needs.
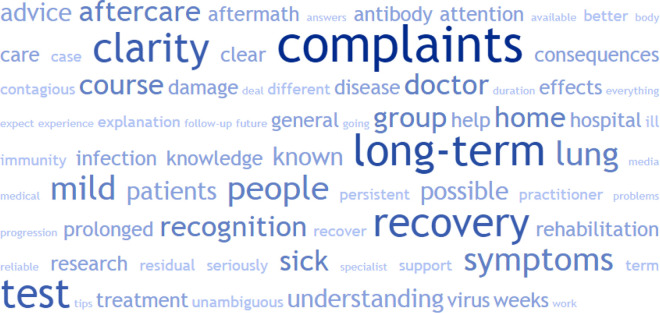
A word cloud has been created by automatically translating Dutch answers into English (via deepl.com) and pasting the translated text into a word cloud generator (tagcrowd.com) to visualize answers and demonstrate the variety of information needs. For creating the word cloud, 75 words have been selected automatically and irrelevant, or obvious words have been deleted manually (eg, “etc,” “lot,” “information,” “info,” “corona”).
Results
Characteristics
In total, 2159 people responded to the online questionnaire (estimated response rate: 16%). Patients who were admitted to the intensive care unit (n = 15) were excluded. Additionally 31 respondents were removed due to missing data (n = 9), an onset of symptoms before January 1, 2020 (n = 8) or reporting that the onset of symptoms was less than 3 weeks ago (n = 14), resulting in 2113 patients (85% women, mean age: 46 ± 11 years, mean body mass index: 26.3 ± 5.2 kg/m2) for the current analysis. More than half of the patients were highly educated, the majority had never smoked and reported a good health status before the infection while two-third had no pre-existing comorbidity. More than one-third of the patients were neither hospitalized nor had a confirmed diagnosis. On average, the survey was completed 79 ± 17 days after the onset of the infection-related symptoms (Table 1).
Table 1.
Patient Characteristics.
| n = 2113 | |
|---|---|
| Women, n (%) | 1803 (85.3) |
| Age, years | 46.2 (11.0) |
| Marital status, n (%) | |
| Alone | 446 (21.1) |
| Married/living together | 1491 (70.6) |
| Divorced | 149 (7.1) |
| Widow(er) | 27 (1.3) |
| Level of education, n (%) | |
| Low | 63 (3.0) |
| Medium | 844 (39.9) |
| High | 1182 (55.9) |
| Not specified | 24 (1.1) |
| Smoking status, n (%) | |
| Currently smokes | 131 (6.2) |
| Smoked before COVID, now quit | 251 (11.9) |
| Never smoked | 1731 (81.9) |
| BMI, kg/m2 | 26.3 (5.2) |
| Self-reported pre-existing comorbidities, n (%) | |
| None | 1239 (61.2) |
| 1 comorbidity | 541 (25.6) |
| ≥2 comorbidities | 279 (13.2) |
| COVID-19 diagnosis, n (%) | |
| Hospitalized | 112 (5.3) |
| Nonhospitalized, confirmed based on CT/RT-PCR | 345 (16.3) |
| Nonhospitalized, confirmed based on symptoms | 882 (41.7) |
| Nonhospitalized, not confirmed by physician | 74 (36.6) |
| Symptoms, n (%) | |
| Time since onset of symptoms (days) | 79.3 (17.2) |
| Symptoms during the infection, n | 14.1 (4.8) |
| Symptoms at this moment, n | 7.0 (3.9) |
| Self-reported health status before the onset of symptoms, n (%) | |
| Good | 1799 (85.1) |
| Moderate | 301 (14.2) |
| Poor | 13 (0.6) |
| Worried about incomplete recovery, n (%) | 1027 (48.6) |
Abbreviations: CT, computed tomography; COVID-19, coronavirus disease 2019; RT-PCR, reverse transcription polymerase chain reaction
The majority of patients perceived social support from family and/or friends regularly to very often. Around 23% and 37% of the patients did not or occasionally experience support from their family members or friends, respectively (Table 2).
Table 2.
Perceived Support From Family, Friends, Employer, and Colleagues by Patients.a
| Family | Friends | Employer | Colleagues | |
|---|---|---|---|---|
| Not applicable | 25 (1.2) | 36 (1.7) | 453 (21.4) | 456 (21.6) |
| Rarely or never | 86 (4.1) | 156 (7.4) | 232 (11.0) | 211 (10.0) |
| Occasionally | 399 (18.9) | 633 (30.0) | 389 (18.4) | 483 (22.9) |
| Regularly | 743 (35.2) | 831 (39.3) | 649 (30.7) | 620 (29.3) |
| Very often | 860 (40.7) | 457 (21.6) | 390 (18.5) | 343 (16.2) |
a Numbers present frequencies and proportions, n (%)
Care and Information Needs
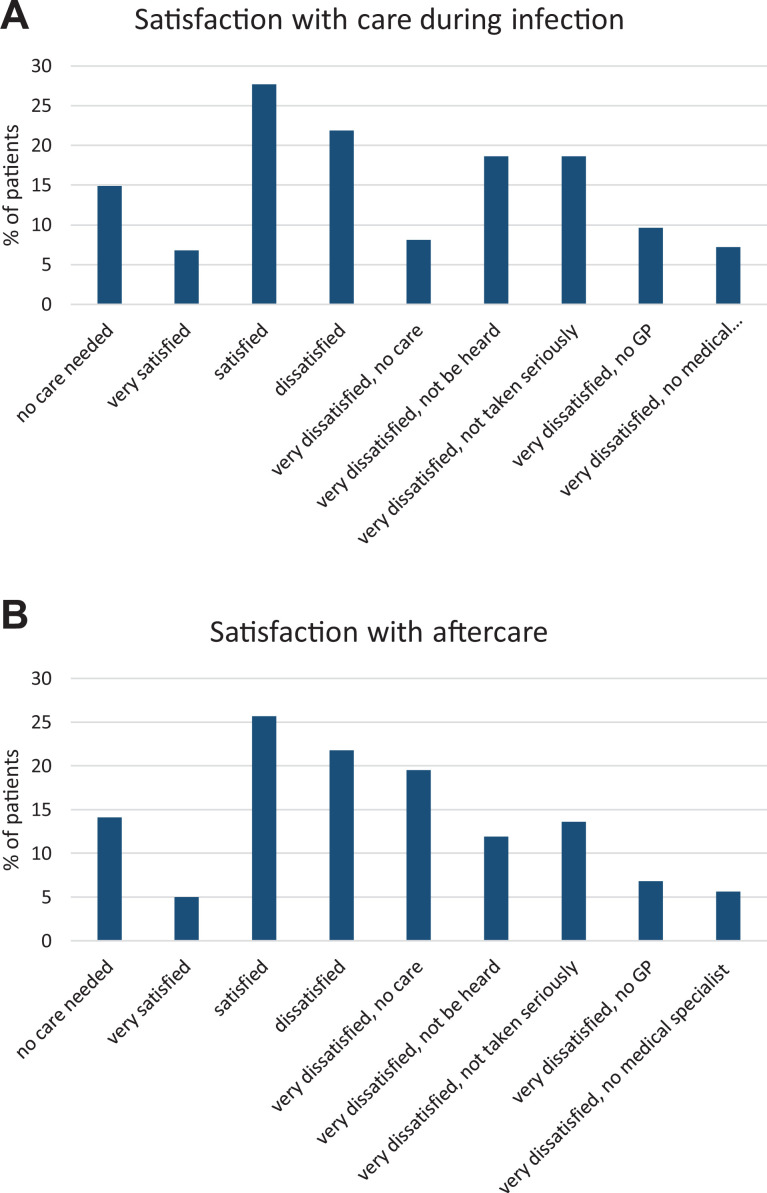
Approximately one-third of the patients were satisfied with care during and/or after the infection (Figure 1A and B). Around 20% of the patients were very dissatisfied because they did not receive any aftercare (Figure 1B) which was supported by the need for more information about aftercare (e-Figure 1, online supplement).
Figure 1.
Satisfaction with (A) care during infection and (B) aftercare. GP indicates general practitioner.
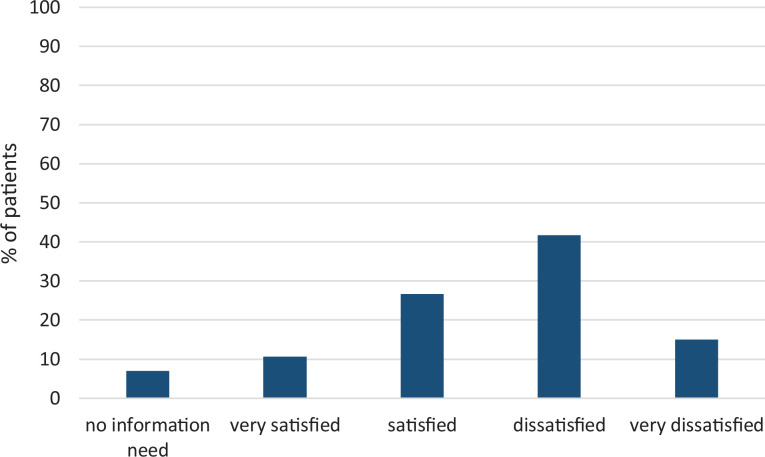
Around 37% of the patients were satisfied or very satisfied with the information available about COVID-19 (Figure 2). Patient needs were very heterogeneous and varied from specific information needs (eg, information about permanent lung damage) to general needs (eg, being heard and understood; Figure 3; e-Figure 1, online supplement).
Figure 2.
Satisfaction with available information.
Figure 3.
Word cloud demonstrating various information needs. The bigger and bolder the word appears, the more often it is mentioned by patients.
Future
Almost half of the patients were worried about incomplete recovery (Table 1). Indeed, patients often wondered “how to proceed” or if and when they could go outside because they still experienced symptoms. Patients would also like more information about long-term complaints and duration of current persistent symptoms.
Clarity
Most patients indicated a need for timely, clear and reliable information: for instance, “according to several websites, patients with “mild” symptoms recover within 2 weeks which was not the case and therefore very frustrating.” According to patients, information on the websites from the national and regional institutes was often contradicting and not up to date: “I would also appreciate better communication from the national institute regarding the recovery period of mild corona and an update of the list of symptoms.” Patients would further appreciate “updates from one reliable source,” even if the answer is “we don’t know.”
Aftercare
Patients indicated information needs about aftercare and possible treatment options. They wonder how they can receive any aftercare without being hospitalized or have been seen by any physician, and if they get any aftercare (eg, rehabilitation), if there is “reimbursement for rehabilitation, also for patients who recovered at home.” Additionally, according to patients, health care providers could be more proactive in giving information about rehabilitation.
“Mild” COVID-19
Patients indicated that they need information about the course and recovery of long-term “mild” symptoms without being hospitalized: “the news is mainly about the severe cases; information about ‘mild’ COVID-19 with persisting symptoms is limited.” Another patient wrote that “it’s labeled as ‘mild’ disease, but it feels very severe”.
Support
Patients do not feel understood and not being taken seriously. “I would like to see more recognition for those of us who were not hospitalized”; “In the end, you already believe that it’s just all in your mind.” Patients indicated that they were looking for peers, “people who also go through this,” to exchange and evaluate their experiences and to verify their symptoms.
Follow-up
Patients perceive that exchanging information and collaboration between professionals with different professions can be improved. They would further appreciate “a GP who monitors how things are going and thinks along with the complaints, thinks along with me about which support I might need and provides advice.”
Testing
Patients indicated that they wanted a test to confirm their diagnosis (in the acute phase) or certainty that they have had COVID-19. “Without a test, it’s all in your mind, it’s a psychological thing.” They were also wondering if they are still contagious since they still have clinical symptoms.
Tips
Patients were looking for some tips or tools to support or accelerate their recovery at home, “a practical guide” about what they could or should do (or leave) to improve their health. They would further appreciate “tips about how to cope with the situation (e.g. fatigue, acceptance).”
Research
Patients also see the need for scientific research since there is still a lot unknown; not only research about COVID-19 affecting the lungs but the whole spectrum of consequences of the disease. They are grateful for the current initiative.
Unknown
Although various unmet information needs exist, patients also realized that COVID-19 is a new disease and therefore a lot is still unknown; “there is simply no information yet.”
Discussion
The current study is the first revealing various patient needs ranging from general care needs to specific information needs in a large sample of patients with confirmed or suspected COVID-19 3 months after the onset of symptoms.
Care Needs
Abrams and colleagues recently stated that “the pandemic has created both challenges and opportunities for delivering care, as system adaptations influence the physician-patient relationship” (8, p. 2474). The current study showed that less than one-third of the patients were satisfied with the care they received during and/or after the onset of symptoms. Two-third of the patients were treated by a GP while 17% were treated by a medical specialist during/after the onset of symptoms (3). Common patient needs were related to aftercare, rehabilitation, tips and advices for exercises, and recovery at home. Indeed, only 20% of the patients were treated by a physiotherapist during/after the onset of symptoms while only 1.5% were treated by an occupational therapist (3). Patients were wondering whether they are eligible for rehabilitation or whether they are reimbursed for rehabilitation since the majority have not been hospitalized or treated by a medical specialist. Following on from this, the Global Rehabilitation Alliance “urges decision makers to ensure that rehabilitation services will be available for all patients with COVID-19 in the acute, post-acute and long-term phase” (11), which is echoed by an European Respiratory Society and American Thoracic Society-coordinated International Task Force (12). Additionally, a considerable proportion of nonhospitalized patients with COVID-19 depend on others for personal care underlining the need for optimal treatment strategies to restore patients’ independency (13).
Rating and understanding patients’ satisfaction and interpreting their feedback (cocreation) provide important insights and outcomes to ultimately improve health care services (14). A considerable proportion of patients who were very dissatisfied with their care during the infection reported that they did not feel heard or taken seriously while dissatisfaction about aftercare was mostly explained by receiving no care. Indeed, patients also indicated that providers can play a more proactive role and be more concerned or involved in the patient journey. Patients are challenged as active and essential members of the treatment team (15), but health care professionals are also encouraged to be involved, listen, and understand (16). Patient experience has been associated with perceptions of care embracing the aphorism that “patients don’t care how much you know until they know how much you care” further underlining the importance of relational aspects of care and communication skills (17,18). However, the absence of face-to-face conversations, fear of infection, and/or personal protective equipment may hinder communication and challenges (virtual) shared decision-making (8). Therefore, health care professionals are encouraged to engage patients in their own home, create opportunities for patients to access multiple platforms, and/or provide access to care team members through telehealth (8,19).
Information Needs
Meeting information needs has been shown to be associated with patients’ satisfaction with care and quality of life (20). In the current study, besides patients who were dissatisfied or very dissatisfied, also patients who were satisfied with the available information indicated relevant unmet information needs. Patients specified the need for “clear information” or “clarity” since they often perceived contradicting information and did not find information about their specific situation: persistent, “mild” symptoms without being hospitalized. Till now, patients with severe COVID-19 who have been admitted to the hospital received most attention from researchers and society. A social media listening study revealed important unfiltered and uninfluenced insights on the impact of disease on patients’ life: patients actively share experiences on forums and seek information on social media (21) further underlining the need to interconnect with patients where they are: online. Indeed, social media influence during COVID-19 has resulted in an “infodemic” highlighting the importance of patient engagement (8). Overall, patients tend to prefer the Internet for the ease of access to information, while they trust their physicians more for their clinical expertise and experience (22). Thus, timely and reliable information by physicians or other trusted parties (eg, patients’ associations, like Lung Foundation Netherlands, for instance via www.coronalongplein.nl) may play an important role. Furthermore, providing information is essential for the shared decision-making process (23) and to empower patients to become active stakeholders by utilizing their knowledge, capabilities, and responsibility (15,24). In addition, in this context, considering the educational level of the target population is essential since it is associated with knowledge processing (25). Remarkably, the majority of the current study population was highly educated. In addition, patient’s context and social facilitation influence self-management (26) emphasizing the need for holistic models considering patient’s family and social context (27). Providing information and knowledge to the patient’s social environment might contribute to the patient’s degree of self-management. In the current study, 23% of the patients did not or occasionally experience support from their family members which might have stimulated their search for recognition online.
Although the number of research articles is rapidly increasing, there are still lots of unanswered questions with regard to COVID-19. Patients indicated the need for certainty and reported to be worried about incomplete recovery. Patients wanted clear information but also acknowledged that a lot is still unknown. On the one hand, timely testing might prevent a specific degree of worriedness and contribute to more certainty and understanding of the situation. However, scaling up testing capacity needs some time. On the other hand, in uncertain situations where evidence-based facts and knowledge are lacking, goal setting and dispositional hope might be included as components of any physician–patient shared decision-making approach (8).
Recommendations for Health Care Providers
Coronavirus disease 2019 has created many difficulties but has also forced us to re-examine how to provide more patient-centred and high-quality care (8). The current findings revealed some important insights leading to several recommendations to improve care for patients with (mild) COVID-19:
Listen to the patient and try to understand what matters to them but also fulfill a proactive role and be involved in health care.
Know patients’ needs, adapt information, be prepared for future scenarios.
Provide timely, clear and reliable information, preferably using a central online information point.
Involve patients’ context and environment, consider social support.
If possible, timely facilitate testing for COVID-19 and follow-up of persistent complaints.
Facilitate any aftercare, ranging from tips or advices about exercises at home to an (inpatient) rehabilitation program, if indicated: provide the right treatment to the right patient at the right time.
Connect with patients where they are: online and preferably live.
Limitations
The external validity of the current findings is limited, as mostly women responded, who are more likely to present themselves with symptoms than men (28). Moreover, only COVID-19 patients from 2 Facebook groups with self-reported persistent symptoms and patients who registered on www.coronalongplein.nl were included in the study. The current study should mostly be used to create a broader awareness among health care professionals, employers, insurers, and society about the unmet information and care needs of patients with “mild” COVID-19 and persistent symptoms. The size of this persistent symptomatic group of “mild” COVID-19 remains to be determined, as well as their symptom trajectory over time. Taken the abovementioned limitations into consideration, the current study population might not present a reliable sample but it highlights the existence and relevant information and care needs of a large unheard group.
Conclusions
Patients with confirmed or suspected COVID-19 perceive various unmet information and care needs. These data justify further development of online platforms specifically addressing these unmet needs. Moreover, effort should be put into involving and educating family, friends, colleagues, employers, and other community members of these patients with persistent complaints.
Supplemental Material
Supplemental Material, sj-docx-1-jpx-10.1177_2374373521997222 for Understanding and Being Understood: Information and Care Needs of 2113 Patients With Confirmed or Suspected COVID-19 by Sarah Houben-Wilke, Jeannet M Delbressine, Anouk W Vaes, Yvonne MJ Goërtz, Roy Meys, Felipe VC Machado, Maarten Van Herck, Chris Burtin, Rein Posthuma, Frits ME Franssen, Nicole HP van Loon, Bita Hajian, Herman Vijlbrief, Yvonne Spies, Alex van ’t Hul, Daisy JA Janssen and Martijn A Spruit in Journal of Patient Experience
Acknowledgments
The research team acknowledges the valuable input from the patient representatives to develop the survey, and the technical support by ASolutions’ Martijn Briejers and Oscar Wagemakers. The scientific work of YMJG is financially supported by Lung Foundation Netherlands grant 4.1.16.085, RM is financially supported by Lung Foundation Netherlands grant 5.1.18.232, and FVCM is financially supported by EU-grant ZonMw ERACoSysMed 90030355.
Author Biographies
Sarah Houben-Wilke is knowledge coordinator in Ciro, Horn, The Netherlands. She graduated in health sciences and her research is mainly focussed on personalized health care and patient-reported outcomes in COPD.
Jeannet M Delbressine is a biomedical engineer and movement scientist. She has participated in several research projects predominantly focused on patients with pulmonary conditions.
Anouk W Vaes is working as a senior researcher in Ciro, Horn, The Netherlands. She has a background in physiotherapy and movement science. Her research is mainly focused on physical activity in COPD.
Yvonne M J Goërtz is a PhD student at Ciro and Maastricht University, The Netherlands, investigating the underlying factors of fatigue in patients with COPD.
Roy Meys is a scientific researcher at Ciro, Horn, The Netherlands. He is currently working as a PhD student on the topic of exercise testing and pulmonary rehabilitation in patients with asthma.
Felipe V C Machado is graduated in physiotherapy with a master's degree in rehabilitation sciences by the State University of Londrina, Brazil. He is currently working as a PhD student on the topic of body composition abnormalities in patients with chronic respiratory diseases.
Maarten van Herck is a PhD student at Ciro, Maastricht University, and Hasselt University, investigating fatigue in patients with chronic lung diseases.
Chris Burtin is a physiotherapist who works as an assistant professor at Hasselt University, Belgium. His field of expertise is exercise and physical activity in chronic lung disease and lung cancer.
Rein Posthuma is a chest physician at Maastricht University Medical Center and Ciro, The Netherlands. He is specialized in COPD, pulmonary intervention and rehabilitation.
Frits M E Franssen is a pulmonologist with a clinical, scientific and educational focus on personalized management of COPD. He is the medical director and a member of the Executive Board of Ciro, Horn, The Netherlands, and a staff member at the department of Respiratory Medicine in Maastricht University Medical Center, The Netherlands.
Nicole H P van Loon is a specialist in Internal Medicine, both working in Ciro, Horn, The Netherlands, as a general internist with focus on chronic diseases and comorbidities and in Maastricht University Medical Center, The Netherlands with focus on acute medicine.
Bita Hajian is respiratory physician and scientist in Ciro, Horn, The Netherlands. Her field of expertise concerns chronic obstructive pulmonary disease (COPD), severe asthma and pulmonary rehabilitation.
Herman Vijlbrief is working as a spokesman at The Lung Foundation Netherlands. He has a background in sociology and has been working as a TV reporter. His main focus is storytelling and impact realization.
Yvonne Spies is working as a programme director at The Lung Foundation Netherlands. She has a background in work and organizational psychology. Her main focus is impact realization.
Alex van ’t Hul is dedicated to research about the development, implementation and evaluation of the effectiveness of integrated care in patients with chronic airway diseases. Non-pharmacological interventions such as physiotherapy and pulmonary rehabilitation form key elements.
Daisy J A Janssen is physician in old age medicine and palliative care in Ciro, Horn, The Netherlands, and associate professor at the Maastricht University, The Netherlands. Her field of expertise concerns palliative care and psychosocial needs of patients with advanced chronic diseases.
Martijn A Spruit is executive board member at Ciro, a specialized pulmonary rehabilitation centre in Horn, The Netherlands, and full professor in Rehabilitation Sciences at Maastricht University, The Netherlands.
Authors’ Note: SH-W, JMD, AWV, YMJG, RM, FVCM, and MvH were responsible for the data collection. MAS is the principal investigator of this trial. SH-W, JMD, and MAS drafted the manuscript. All authors critically reviewed and revised the manuscript. This study was approved by the medical ethics committee of Hasselt University (MEC2020/041).The medical ethics committee of Maastricht University stated that the Medical Research Involving Human Subjects Act (WMO) does not apply for this study and that an official approval of this study by the committee was not required (METC2020-1978). All procedures in this study were conducted in accordance with the medical ethics committee of Hasselt University (MEC2020/041) and medical ethics committee of Maastricht University (METC2020-1978) approved protocols. All respondents gave digital informed consent.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: FMEF reports grants and personal fees from AstraZeneca, personal fees from Boehringer Ingelheim, personal fees from Chiesi, personal fees from GlaxoSmithKline, grants and personal fees from Novartis, personal fees from TEVA, outside the submitted work; DJAJ reports personal fees from AstraZeneca, personal fees from Boehringer Ingelheim, personal fees from Novartis, outside the submitted work; MAS reports grants from Lung Foundation Netherlands, grants from Stichting Astma Bestrijding, grants and personal fees from Boeheringer Ingelheim, and grants and personal fees from AstraZeneca, outside the submitted work. SH-W, JMD, AWV, YMJG, RM, FVCM, MvH, CB, RP, NHPvL, HV, YS, and AvH have nothing to declare.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Sarah Houben-Wilke  https://orcid.org/0000-0001-6214-0365
https://orcid.org/0000-0001-6214-0365
Daisy J. A. Janssen  https://orcid.org/0000-0002-1827-9869
https://orcid.org/0000-0002-1827-9869
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Pneumonia of unknown cause – China; 2020. Accessed June 17, 2020. https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/
- 2.Coronavirus Resource Center; 2020. Accessed June 07, 2020. https://coronavirus.jhu.edu/map.html
- 3.Goërtz YMJ, Van Herck M, Delbressine JM, Vaes AW, Meys R, Machado FVC, et al. Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? ERJ Open Res. 2020;6:00542–2020. doi:10.1183/23120541.00542-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meys R, Delbressine JM, Goertz YMJ, Vaes AW, Machado FVC, Van Herck M, et al. Generic and respiratory-specific quality of life in non-hospitalized patients with COVID-19. J Clin Med. 2020;9:3993. doi:10.3390/jcm9123993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ladds E, Rushforth A, Wieringa S, Taylor S, Rayner C, Husain L, et al. Persistent symptoms after Covid-19: qualitative study of 114 “long Covid” patients and draft quality principles for services. BMC Health Serv Res. 2020;20:1144. doi:10.1186/s12913-020-06001-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the patient activation measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39:1005–26. doi:10.1111/j.1475-6773.2004.00269.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abrams EM, Greenhawt M. Risk communication during COVID-19. J Allergy Clin Immunol Pract. 2020;8:1791–94. doi:10.1016/j.jaip.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abrams EM, Shaker M, Oppenheimer J, Davis RS, Bukstein DA, Greenhawt M. The challenges and opportunities for shared decision making highlighted by COVID-19. J Allergy Clin Immunol Pract. 2020;8:2474–80. e1. doi:10.1016/j.jaip.2020.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Public Facebook Group: Corona ervaringen en langdurige klachten! 2020.
- 10.Public Facebook Group: Corona patiënten met langdurige klachten (Vlaanderen). 2020.
- 11.Gutenbrunner C, Stokes EK, Dreinhofer K, Monsbakken J, Clarke S, Côté P, et al. Why rehabilitation must have priority during and after the COVID-19-pandemic: a position statement of the global rehabilitation alliance. J Rehabil Med. 2020;52:jrm00081. doi:10.2340/16501977-2713 [DOI] [PubMed] [Google Scholar]
- 12.Spruit MA, Holland AE, Singh SJ, Tonia T, Wilson KC, Troosters T. COVID-19: interim guidance on rehabilitation in the hospital and post-hospital phase from a European respiratory society and American thoracic society-coordinated international task force. Eur Respir J. 2020;56:2002197. doi:10.1183/13993003.02197-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vaes AW, Machado FVC, Meys R, Delbressine JM, Goertz YMJ, Van Herck M, et al. Care dependency in non-hospitalized patients with COVID-19. J Clin Med. 2020;9:2946. doi:10.3390/jcm9092946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang L, Tong H, Demirel HO, Duffy VG, Yih Y, Bidassie B. A practical model of value co-creation in healthcare service. Procedia Manufact. 2015;3:200–207. doi:10.1016/j.promfg.2015.07.129 [Google Scholar]
- 15.Houben-Wilke S, Augustin IM, Wouters BB, Stevens RA, Janssen DJA, Spruit MA, et al. The patient with a complex chronic respiratory disease: a specialist of his own life? Expert Rev Respir Med. 2017;11:919–24. doi:10.1080/17476348.2017.1392242 [DOI] [PubMed] [Google Scholar]
- 16.Cappuccio A, Sanduzzi Zamparelli A, Verga M, Nardini S, Policreti A, Porpiglia PA, et al. Narrative medicine educational project to improve the care of patients with chronic obstructive pulmonary disease. ERJ Open Res. 2018;4:00155–2017. doi:10.1183/23120541.00155-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Graham B, Endacott R, Smith JE, Latour JM. ‘They do not care how much you know until they know how much you care’: a qualitative meta-synthesis of patient experience in the emergency department. Emerg Med J. 2019;36:355–63. doi:10.1136/emermed-2018-208156 [DOI] [PubMed] [Google Scholar]
- 18.Tongue JR, Epps HR, Forese LL. Communication skills. Instr Course Lect. 2005;54:3–9. [PubMed] [Google Scholar]
- 19.Meyer MA. COVID-19 pandemic accelerates need to improve online patient engagement practices to enhance patient experience. J Patient Exp. 2020;7:657–64. doi:10.1177/2374373520959486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Larson CO, Nelson EC, Gustafson D, Batalden PB. The relationship between meeting patients’ information needs and their satisfaction with hospital care and general health status outcomes. Int J Qual Health Care. 1996;8:447–56. doi:10.1093/intqhc/8.5.447 [DOI] [PubMed] [Google Scholar]
- 21.Cook NS, Kostikas K, Gruenberger JB, Shah B, Pathak P, Kaur VP, et al. Patients’ perspectives on COPD: findings from a social media listening study. ERJ Open Res. 2019;5:00128–2018. doi:10.1183/23120541.00128-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clarke MA, Moore JL, Steege LM, Koopman RJ, Belden JL, Canfield SM, et al. Health information needs, sources, and barriers of primary care patients to achieve patient-centered care: a literature review. Health Informatics J. 2016;22:992–1016. doi:10.1177/1460458215602939 [DOI] [PubMed] [Google Scholar]
- 23.Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–67. doi:10.1007/s11606-012-2077-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Russo R, Tartaglione AM, Cavacece Y. Empowering patients to co-create a sustainable healthcare value. Sustainability. 2019;11:1–20. doi:10.3390/su11051315 [Google Scholar]
- 25.Chin J, Morrow D, Stine-Morrow E, Conner-Garcia T, Graumlich JF, Murray MD. The process-knowledge model of health literacy: evidence from a componential analysis of two commonly used measures. J Health Commun. 2011;16:222–41. doi:10.1080/10810730.2011.604702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ryan P, Sawin KJ. The individual and family self-management theory: background and perspectives on context, process, and outcomes. Nurs Outlook. 2009;57:217–25. e216. doi:10.1016/j.outlook.2008.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenhalgh T. Patient and public involvement in chronic illness: beyond the expert patient. BMJ. 2009;338:b49. doi:10.1136/bmj.b49 [DOI] [PubMed] [Google Scholar]
- 28.Bardel A, Wallander MA, Wallman T, Rosengren A, Johansson S, Eriksson H, et al. Age and sex related self-reported symptoms in a general population across 30 years: Patterns of reporting and secular trend. PloS One. 2019;14:e0211532. doi:10.1371/journal.pone.0211532 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-jpx-10.1177_2374373521997222 for Understanding and Being Understood: Information and Care Needs of 2113 Patients With Confirmed or Suspected COVID-19 by Sarah Houben-Wilke, Jeannet M Delbressine, Anouk W Vaes, Yvonne MJ Goërtz, Roy Meys, Felipe VC Machado, Maarten Van Herck, Chris Burtin, Rein Posthuma, Frits ME Franssen, Nicole HP van Loon, Bita Hajian, Herman Vijlbrief, Yvonne Spies, Alex van ’t Hul, Daisy JA Janssen and Martijn A Spruit in Journal of Patient Experience