Abstract
Background
COVID-19 is a significant threat to people's mental health and social well-being. The research examined the effects of social determinants of health on COVID-19 related stress, family's stress and discord, and personal diagnosis of COVID-19.
Methods
In November 2020, the data collection was conducted from 97 counties in North Carolina (N = 1500). Adult residents in North Carolina completed an online COVID-19 impact survey conducted using quota-based sampling on race, income, and county to provide a rapid quasi-representative assessment of COVID impact. The study investigated the variables in a structural model through structural equation modeling. For data analysis, IBM SPSS 26 and AMOS 27 were deployed.
Results
Social determinants of health had direct effects on COVID-19 related stress (β = 0.66, p < 0.001, r2 = 0.43), family's stress and discord (β = 0.73, p < 0.001, r2 = 0.53), and personal diagnosis of COVID-19 (β = 0.52, p < 0.001, r2 = 0.27). These findings indicate that underserved populations experienced higher stress and discord at both individual and family levels and more severe COVID-19 symptoms. Moreover, black participants, whose family income and food access declined significantly more, had worse stress, discord, and COVID-19 symptoms than white participants.
Conclusions
The study suggests that the government and health professionals enhance mental health and family support service accessibility for underprivileged populations through telehealth and community health programs to prevent associated social and health issues such as suicide, violence, and cancer.
Keywords: COVID-19, Social determinants of health, Stress, Discord, Health disparities, Race
1. Introduction
The COVID-19 pandemic impacted the United States of America epidemiologically and socially, with about 29 million coronavirus-positive cases and 522,000 deaths (Centers for Disease Control and Prevention – CDC 2021b). North Carolina had the top-ten highest total number of COVID-19 positive cases in the United States (CDC 2021a). The COVID-19 pandemic is a critical threat to public health and restricts food accessibility, health service access, educational opportunities, health equality, and local business chances (Gao et al., 2020), which can increase people's stress and discord (Cullen et al., 2020; Pfefferbaum and North, 2020). The COVID-19 pandemic has an extensive impact on people socially and mentally, and the investigation of COVID-19 and mental health variables with a social-ecological model (CDC 2020a) is necessary.
Responding to the COVID-19 crisis, the present study investigated COVID-19 symptoms, stress, and discord with a social-ecological model, the social determinants of health approach (CDC 2020a; CDC 2020b). The benefits of researching COVID-19 with social determinants of health were thoroughly discussed regarding health disparities in academia (Singu et al., 2020). Many researchers claimed that scientific studies of health disparities with social determinants of health in COVID-19 (COVID-19) are in demand (Burström and Tao, 2020; Gray et al., 2020). Social determinants of health are conditions that individuals operate their daily lives and affect health outcomes and risks (CDC 2020a; CDC 2020b; Marmot, 2005; Office of Disease Prevention and Health Promotion, 2020; WHO, 2020). Social determinants of health include the areas of healthcare access & quality, social & community context (e.g., social support, civic participation, incarceration), neighborhood & built environment (e.g., food availability), economic stability, and education access & quality. More specifically, the present research investigated the effects of social determinants of health on COVID-19 related stress, family's stress and discord, and personal diagnosis of COVID-19 under the coronavirus pandemic to evaluate the pandemic's mental and social impact. As social determinants of health are defined as social factors affecting health outcomes and risks as mentioned above, the current study set directional paths from social determinants of health to the other health outcome variables, which are COVID-19 related stress, family's stress and discord, and personal diagnosis of COVID-19 (i.e., the severity of COVID-19 symptoms). Moreover, the study compared the results in different races to see how the results varied based on race. To examine the relationships, the study developed three research hypotheses below.
-
1
RH1: Social Determinants of Health have a direct effect on COVID-19 Related Stress.
-
2
RH2: Social Determinants of Health have a direct effect on Family's Stress and Discord.
-
3
RH3: Social Determinants of Health have a direct effect on Personal Diagnosis of COVID-19.
2. Methods
2.1. Sampling & study design
An online survey was conducted using quota-based sampling on race, income, and county in November 2020 to provide a rapid quasi-representative assessment of COVID impact (Ahn, and Norwood, 2020). In November 2020, study participants were recruited through opt-in panels developed by the Qualtrics corporation, which recruits subjects utilizing various methods and third-party validation to confirm individuals’ identity. A cross-sectional study design was selected to investigate correlations among the variables of Personal Diagnosis of COVID-19, COVID-19 Related Stress, Family's Stress and Discord, and Social Determinants of Health.
Surveys were received from 1500 respondents in 97 counties out of 100 counties in North Carolina. The sample size was sufficient for the data analysis as literature determined the minimum sample size of 100 for the chosen data analysis method, structural equation modeling (Anderson and Gerbing, 1988; Ding et al., 1995; Lee and Lim, 2013; Moon, 2013; Tabachnick et al., 2001; Tinsley and Tinsley, 1987). Moreover, a power analysis determined the minimum sample sizes of 87 to detect effects and 700 for model structure (Free Statistics Calculator Version. 4.0 - a priori sample size for structural equation modeling). In the power analysis, the selected analysis conditions were anticipated effect size = 0.10, desired statistical power level = 0.80, the number of latent variables = 1, the number of observed variables = 8, and the probability level = 0.50, for the structural model in the present study. The Institutional Review Board (IRB) at the institution, with which the authors were affiliated, approved the data collection protocol.
2.2. Measurements
The study formulated an online survey with the Coronavirus Impact Scale (CIS), extracted from the PhenX Toolkit (Hamilton et al., 2011), officially recognized by the National Institutes of Health. CIS includes 12 questions, and the current research deployed 11 questions without an open-ended question. The first nine questions have a Likert scale of “none”, “mild”, “moderate”, and “severe” (score zero to three) and demonstrate examples for each answer choice. The last two questions have a Likert scale of “ none”, “mild”, “moderate”, “severe”, and “extreme” (score zero to four) and show examples for each answer choice. A higher score meant a more negative change in life under the coronavirus pandemic.
The CIS questions are related to individuals’ negative life changes in 11 life domains. The areas include daily routines, family income, food access, medical care access, mental health treatment access, access to extended family or non-family social support, stress experiences related to COVID-19, stress and discord experiences in the family, personal diagnosis of COVID-19 (i.e., the severity of COVID-19 symptoms), the number of the immediate family diagnosed with COVID-19, and the number of extended family member(s) and/or close friends diagnosed with COVID-19. The CIS item topics were aligned with the current study's interests of personal diagnosis of COVID-19, stress, discord, and social determinants of health domains (i.e., healthcare access & quality, education access & quality, social & community context, economic stability, and neighborhood & built environment).
2.3. Data analysis
2.3.1. Data cleaning & descriptive statistics
The data cleaning included removing survey responses that had missing values of the variables (i.e., Personal Diagnosis of COVID-19, COVID-19 Related Stress, Family's Stress and Discord, Family Income, Medical Health Care Access, Mental Health Treatment Access, Social Support, and Food Access). There was no other data cleaning criterion and retained the dataset as much as possible to maintain the sample's representativeness to North Carolina. In the next step, the study utilized descriptive statistical analysis on variables by producing mean, standard deviations, and standard errors. For the descriptive statistical analysis and data cleaning, IBM Statistical Package for the Social Sciences (SPSS) 26 was used.
2.3.2. Confirmatory factor analysis (CFA) on social determinants of health
As Social Determinants of Health was employed as a latent variable, the study needed to examine its validity through confirmatory factor analysis (CFA) before using it in the hypothesis test. Based on CDC's theoretical approach, Medical Health Care Access, Mental Health Treatment Access, Education Level, Social Support, Family Income, and Food Access were chosen as indicators for Social Determinants of Health (CDC, 2020b). However, Education Level was dismissed because the indicator showed a too low factor loading value (β = 0.07, p < 0.05); the plausible reason is that the present research measured Social Determinants of Health with CIS customized to the COVID-19, and the pandemic was a sudden crisis that had no impact on people's educational level. The analysis software was IBM Analysis of Moment Structures (AMOS) 27.
The CFA model fit was examined with absolute and incremental model fit indices. The absolute fit indices were x2 statistic, goodness of fit index (GFI > 0.90), adjusted goodness of fit index (AGFI > 0.90), root mean square residual (RMSR < 0.10), standardized root mean square residual (SRMR < 0.10), root mean square error of approximation (RMSEA < 0.10), and x2 statistic/degree of freedom (CMIN/DF < 3.0). The relative/incremental model fit indices were normed fit index (NFI > 0.90), comparative fit index (CFI > 0.90), and Tucker-Lewis index (TLI > 0.90). After the model fit test, the study examined the convergent validity coefficient of the latent variables, Social Determinants of Health, by using the formula, . The research also examined the latent variables’ Average Variance Extracted (AVE) by utilizing another formula, . Ideally, the convergent validity coefficient was expected to be 0.70 or greater, and AVE was expected to be 0.50 or greater.
2.3.3. Hypothesis test in a structural model
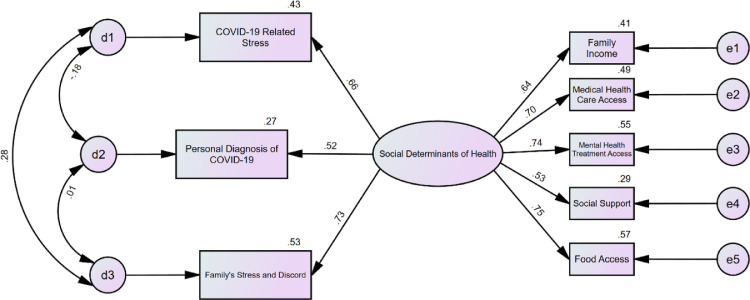
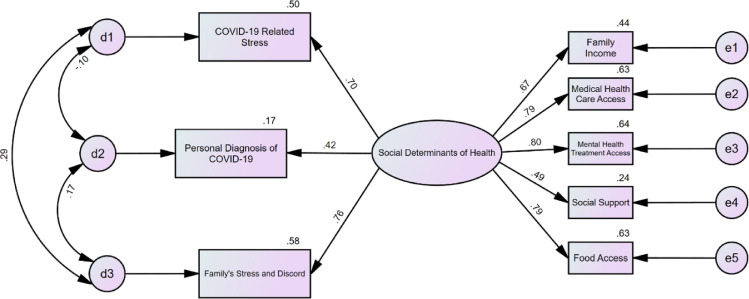
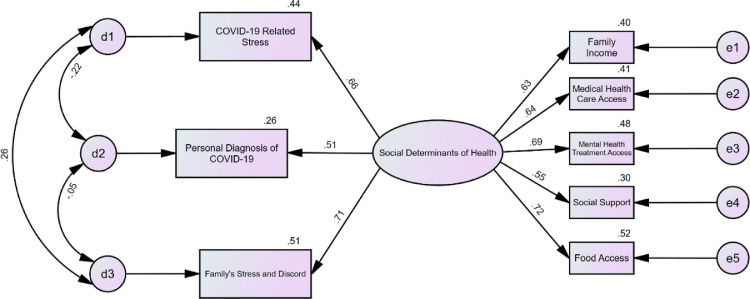
The research investigated Social Determinants of Health's direct effects on COVID-19 Related Stress (RH1), Family's Stress and Discord (RH2), and Personal Diagnosis of COVID-19 Stress (RH3) at α = 0.05 (Fig. 1 ) through structural equation modeling. The structural model's fit was examined with absolute and incremental model fit indices like CFA. In the end, the results were compared in different races (Fig. 2 & 3 ). Additionally, because the numbers of only black (n1 = 287) and white (n2 = 1102) participants met the required minimum sample size for the data analysis (see Section 2.1.), only the white and black subjects’ results were compared. For structural equation modeling, IBM Analysis of Moment Structures (AMOS) 27 was employed.
Fig. 1.
Structural Model for the Hypothesis Test. The oval-shaped variable is a latent variable, and the rectangle-shaped variables are measured variables. e1 to e5 are measurement errors. d1 to d3 are exogenous variables that were not measured but estimated. The two-way arrows are correlations. The one-way arrows are regression relationships. All relationships are significant except for the correlation between Family's Stress and Discord and Personal Diagnosis of COVID-19.
Fig. 2.
Structural Model with Black Participants. Model fit indices: x2 = 62.12 (p < 0.001, degree of freedom = 17), SRMR = 0.04, GFI = 0.95, AGFI = 0.89, NFI = 0.94, TLI = 0.93, CFI = 0.96, and RMSEA = 0.10. The oval-shaped variable is a latent variable, and the rectangle-shaped variables are measured variables. e1 to e5 are measurement errors. d1 to d3 are exogenous variables that were not measured but estimated. The two-way arrows are correlations. The one-way arrows are regression relationships. All factor loading values and correlations are significant except for the correlation between COVID-19 Related Stress and Personal Diagnosis of COVID-19.
Fig. 3.
Structural Model with White Participants. Mode fit indices: x2 = 205.34 (p < 0.001, degree of freedom = 17), SRMR = 0.03, GFI = 0.96, AGFI = 0.91, NFI = 0.93, TLI = 0.91, CFI = 0.90, and RMSEA = 0.10. The oval-shaped variable is a latent variable, and the rectangle-shaped variables are measured variables. e1 to e5 are measurement errors. d1 to d3 are exogenous variables that were not measured but estimated. The two-way arrows are correlations. The one-way arrows are regression relationships. All factor loading values and correlations are significant except for the correlation between Family's Stress and Discord and Personal Diagnosis of COVID-19.
3. Results
3.1. Demographics of subjects
In the data cleaning, 35 responses were removed due to missing values, and 1465 subjects were retained out of 1500 total survey responses. All participants were age 18 or older. In annual household income, 18.6% (272 individuals) answered as “less than $30,000″, 25.5% (373 people) responded as “$30,000 - $60,000″, and 56% (820 individuals) answered as “more than $60,000″. In terms of ethnicity (multiple answers available in the survey), 1102 individuals (75.2%) selected White, 287 people (19.6%) chose Black/African American, 56 individuals (3.8%) selected Latino/Hispanic, 14 (1.0%) individuals chose American Indian/Alaska Native, 19 people (1.3%) selected Asian, three individuals (0.2%) chose Native Hawaiian/Pacific Islander, and 15 people (1.0%) selected Other. The race distribution of the subjects was similar to the North Carolina population's race distribution. Regarding the respondent's Education Level, about half of the participants (49.8%) answered as college-level education, and 358 individuals (24.4%) studied beyond college.
3.2. Descriptive statistics results of variables
The results of descriptive statistical analyses of the variables are shown in Table 1 . Family Income average score of 1.01 meant “there was small change; able to meet all needs and pay bills.” The mean of Personal Diagnosis of COVID-19 was 0.20 (zero = none; one = mild symptoms); 1272 participants (86.8%) had no COVID-19 related symptoms, and 193 subjects (13.2%) had COVID-19 symptoms. In Medical Health Care Access (means = 0.89) and Mental Health Treatment Access (mean = 0.59), the average scores were close to one, which represented individuals were most likely to move their medical appointments to telehealth. Regarding Social Support (mean = 1.26), the mean score was close to one, and this demonstrated “Continued visits with social distancing and/or regular phone calls and/or televideo or social media contacts”. In terms of Food Access, the means score was 0.77, which represented the majority of the subjects had sufficient food but experienced difficulties in going to stores and/or finding needed items. In the 801 participants (54.68%) who experienced negative life changes in their food access in the coronavirus crisis, 534 people (36.3%) said they could get enough food but had difficulty getting to stores and/or finding needed items.
Table 1.
Descriptive statistical analysis results.
| Personal Diagnosis of COVID-19 | Family Income | Medical Health Care Access | Mental Health Treatment Access | Social Support | Food Access | Education Level | Family's Stress and Discord | Stress | |
|---|---|---|---|---|---|---|---|---|---|
| Mean | 0.20 | 1.01 | 0.89 | 0.59 | 1.26 | 0.77 | 2.20 | 0.90 | 1.28 |
| Standard Error of Mean | 0.02 | 0.03 | 0.02 | 0.02 | 0.02 | 0.02 | 0.03 | 0.02 | 0.02 |
| Standard Deviation | 0.58 | 0.97 | 0.93 | 0.90 | 0.91 | 0.84 | 1.02 | 0.99 | 0.91 |
Note. See Section 3.2. Descriptive Statistics Results of Variables for details.
3.3. Confirmatory factor analysis: validation of social determinants of health
The model fit indices show the goodness of the CFA model structure of Social Determinants of Health: x 2 = 67.07 (p < 0.001, degree of freedom = 5), SRMR = 0.02, GFI = 0.98, AGFI = 0.94, NFI = 0.97, TLI = 0.94, CFI = 0.97, and RMSEA = 0.09. The convergent validity coefficient was 0.81 , and AVE was 0.46 , which supported that the latent variable of Social Determinants of Health could be estimated with the chosen reflective indicators. Among the indicators for Social Determinants of Health, Food Access (β = 0.75, p < 0.001) and Mental Health Treatment Access (β = 0.74, p < 0.001) were the most significant indicators followed by Medical Health Care Access (β = 0.70, p < 0.001), Family Income (β = 0.64, p < 0.001), and Social Support (β = 0.53, p < 0.001).
3.4. Hypotheses test
The study examined Social Determinants’ direct effects on COVID-19 Related Stress, Family's Stress and Discord, and Personal Diagnosis of COVID-19 in a structural model (Fig. 1). The model fit indices show the goodness of the statistical structure: x 2 = 269.65 (p < 0.001, degree of freedom = 17), SRMR = 0.03, GFI = 0.96, AGFI = 0.91, NFI = 0.94, TLI = 0.91, CFI = 0.94, and RMSEA = 0.10. As shown in Fig. 1, Social Determinants of Health had a direct effect on COVID-19 Related Stress (β = 0.66, p < 0.001) (answer to RH1), and 43% of COVID-19 Related Stress's variances could be explained by Social Determinants of Health (r 2 = 0.43). Also, Social Determinants of Health had a direct effect on Family's Stress and Discord (β = 0.73, p < 0.001) (answer to RH2), and 53% of the variances of Family's Stress and Discord could be explained by Social Determinants of Health (r 2 = 0.53). Moreover, Social Determinants of Health had a direct effect on Personal Diagnosis of COVID-19 (β = 0.52, p < 0.001) (answer to RH3), and 27% of the variances of Personal Diagnosis of COVID-19 could be explained by Social Determinants of Health (r 2 = 0.27). In the results, Social Determinants of Health had the strongest direct effect and explanatory power on Family's Stress and Discord and the weakest direct effect and explanatory power on Personal Diagnosis of COVID-19. Furthermore, COVID-19 Related Stress had a significant correlation with Family's Stress and Discord (r = 0.28, p < 0.001) and with Personal Diagnosis of COVID-19 (r = −0.18, p < 0.001) (Fig. 1). There was no correlation between COVID-19 Related Stress and Personal Diagnosis of COVID-19.
3.5. Results comparison in different races
The results were compared in black and white participants; both structural models show the goodness of model fit (Fig. 2& 3). Black and white subjects showed the same-pattern results to the total subjects. In both races, Social Determinants of Health had direct effects on COVID-19 Related Stress, Family's Stress and Discord (the strongest direct effect and explanatory power), and Personal Diagnosis of COVID-19 (the weakest direct effect and explanatory power). However, there were several differences regarding explanatory power and factor loading values between the two races. In black participants (Fig. 2), 50% of COVID-19 Related Stress could be explained with Social Determinants of Health (r 2 = 0.50, β = 0.70, p < 0.001), whereas it was 44% in the white participants (r 2 = 0.44, β = 0.66, p < 0.001) (Fig. 3). In black participants, 58% of Family's Stress and Discord could be explained with Social Determinants of Health (r 2 = 0.58, β = 0.76, p < 0.001) (Fig. 2), whereas it was 51% in white participants (r 2 = 0.51, β = 0.71, p < 0.001) (Fig. 3). In black subjects, 17% of Personal Diagnosis of COVID-19 could be explained with Social Determinants of Health (r 2 = 0.17, β = 0.42, p < 0.001) (Fig. 2), whereas it was 26% in white subjects (r 2 = 0.26, β = 0.51, p < 0.001) (Fig. 3). Comparing the explanatory power and factor loading values in the different races, Personal Diagnosis of COVID-19 was better explained in white people, while COVID-19 Related Stress and Family's Stress and Discord were better explained in black people.
The correlation patterns were very different from each other. In black participants, Family's Stress and Discord was significantly correlated to COVID-19 Related Stress (r = 0.26, p < 0.001) and to Personal Diagnosis of COVID-19 (r = 0.17, p < 0.05) (Fig. 2), whereas Family's Stress and Discord was not significantly correlated to Personal Diagnosis of COVID-19 in white participants (Fig. 3). Instead, Personal Diagnosis of COVID-19 had a significant correlation with COVID-19 Related Stress (r = −0.22, p < 0.001) in white subjects (Fig. 3). White subjects also showed a significant correlation between Family's Stress and Discord and COVID-19 Related Stress.
4. Discussion
The COVID-19 pandemic's adverse social impact exacerbated individuals’ mental health. Studying the epidemiological phenomenon, the study examined social determinants’ effects on COVID-19 related stress, family's stress and discord, and personal diagnosis of COVID-19. As social determinants of health are social elements influencing health outcomes and risks (CDC, 2020a; CDC, 2020b; Office of Disease Prevention and Health Promotion, 2020), the directional paths from social determinants of health to the other variables were hypothesized. For the investigation, the study developed three research hypotheses (RH), RH1: Social Determinants of Health have a direct effect on COVID-19 Related Stress; RH2: Social Determinants of Health have a direct effect on Family's Stress and Discord; RH3: Social Determinants of Health have a direct effect on Personal Diagnosis of COVID-19. Additionally, the results of the hypothesis tests were compared between black and white participants.
The results supported RH1, finding that the more negatively individuals’ life changed in social determinants of health, the more stress they had about COVID-19 (Fig. 1). In other words, underserved people who should have been more vulnerable to the pandemic's social impact had higher stress. This was also true in the result comparison between black and white participants. Regarding black populations that were more underserved than white people, their stress could be explained more (50%) (Fig. 2) by social determinants of health than white participants’ stress (44%) (Fig. 3). To confirm that black participants were more underserved and socially vulnerable than white participants, the study conducted an independent samples t-test (Table 2 ). In the test results, black participants’ income decreased in the COVID-19 pandemic was significantly worse than white participants (equal variances not assumed, t = 4.17, df = 416.51, p < 0.001, mean difference = 0.28; 0.15 < 95% confidence interval < 0.41). Also, the decline of food access in the coronavirus crisis was worse in black people than white people (equal variances not assumed, t = 1.78, df = 405.74, p < 0.001, mean difference = 0.11; 0.01 < 95% confidence interval < 0.22). The gaps in food access and family income make sense as underserved populations’ food insecurity, including black-headed households, has been a well-known issue in North Carolina, according to USDA (Alisha et al., 2017).
Table 2.
Independent samples t-test on family income and food access between black and white participants.
| N | Equal Variances | Mean | Mean Difference | t-value | Degree of Freedom | Significance | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Family Income | 287 (b) | Not assumed | 1.21 (b) | b-w = 0.28 | 4.17 | 416.51 | p < 0.001 | 0.15 | 0.41 |
| 1093 (w) | 0.93 (w) | ||||||||
| Food Access | 287 (b) | Not assumed | 0.84 (b) | b-w = 0.11 | 1.78 | 405.74 | p < 0.001 | −0.01 | 0.22 |
| 1093 (w) | 0.73 (w) | ||||||||
Note. b = black, w = white. See Section 4. Discussion for more details.
The findings from the RH1 test implies that underserved people are more psychologically vulnerable to stressors related to disasters and pandemic (Curtis et al., 2007), including the COVID-19 outbreak, which can result in those people's higher risk of having severe chronic diseases like cancer (Hébert et al., 2015). Thus, the study recommends that the government enhances mental health service accessibility for minority populations marginalized from social and health benefits. One potential intervention can be the increased provision of free online mental-health services for underprivileged and uninsured populations as telemental health services have been demonstrated to be effective (Whaibeh et al., 2020). Another result of the current study also supported this implication. It was found that mental health treatment access was significantly more important for black populations (Fig. 2) than white populations (Fig. 3); Mental Health Treatment Access's factor loading value was β = 0.80 to Social Determinants of Health with the explanatory power of 64% in black people (Fig. 2), whereas those values were significantly smaller as 48% and β = 0.69 in white people (Fig. 3).
Moreover, the data analysis results supported RH2, discovering that the more negatively individuals’ life changed in social determinants of health, the more family stress and discord they had under the COVID-19 pandemic (Fig. 1). This result demonstrates that underprivileged populations experienced more family stress and discord due to the pandemic. The finding is aligned with the result comparison between black and white participants; as described above, black populations were underserved compared to white participants according to the independent samples t-test conducted in the current study. Fifty eight percent of the variances of Family's Stress and Discord in black subjects could be explained with Social Determinants of Health (r 2 = 0.58, β = 0.76, p < 0.001) (Fig. 2), whereas only fifty one percent of the variances of Family's Stress and Discord in white subjects could be explained (r 2 = 0.51, β = 0.71, p < 0.001) (Fig. 3). The findings imply that socially underprivileged people are more exposed to stress and discord within families during the pandemic, which can result in serious social problems and anti-social behavior such as suicide, aggression, and violence (Ferguson et al., 2009; Rubenstein et al., 1998). Therefore, for the prevention, health professionals should rapidly increase community-based health initiatives for underserved populations to better cope with stress and discord within families, especially in a national crisis like COVID-19.
Furthermore, the research results with the total subjects supported RH3, finding that the more negatively individuals’ life changed in social determinants of health, the more severe COVID-19 symptoms they were likely to have (Fig. 1). The finding shows that socially marginalized populations were more frequently diagnosed with COVID-19 and experienced more severe COVID-19 symptoms. It can be empirical evidence for Burström and Tao's (2020) academic argument that inequalities in social determinants of health might result in differential exposure and vulnerability to COVID-19 infection and consequences. However, the finding was not supported by the result comparison between black and white participants in the current research. As explained above, black respondents were more underprivileged than white participants in the independent samples t-test results. Black individuals’ COVID-19 symptom severity was less explained with social determinants of health (explanatory power = 17%) (Fig. 2) than white subjects’ COVID-19 symptom severity (explanatory power = 26%) (Fig. 3). Regarding the unexpected results in the comparison, the present study inferred that there might be another factor significantly affecting COVID-19 symptom severity such as biological features, which can be a research topic for future studies. The results of RH3 with the total subjects show that underserved populations tend to get COVID-19 more often and more severely, which can be empirical evidence for Gray et al. (2020)’s claim that social inequalities could create differential vulnerability to the pandemic. The vulnerability to and severity of COVID-19 symptoms in underprivileged groups are significant problems as they are. At the same time, those can create elevated levels of stress and discord for underprivileged populations, which can result in exacerbated social and health problems such as cancer, suicide, aggression, and violence, as discussed in the previous paragraphs (Ferguson et al., 2009; Hébert et al., 2015; Rubenstein et al., 1998). It is a vicious cycle that is currently happening in marginalized populations under the pandemic in the U.S. To circumvent this negative cycle of social and health problems, the attenuation of socioeconomic inequality and health disparities is necessary. The government and communities should increase health equity and play essential roles in enhancing the social structure for underprivileged populations’ health and safety.
Additionally, comparing the results of black and white subjects, there were different patterns of correlations. In both races, COVID-19 related stress and family stress and discord were positively correlated, which means the higher level of stress regarding the pandemic an individual had, the worse stress and discord the person experienced in his or her family. However, black participants’ family discord and stress were positively correlated to personal diagnosis of COVID-19 (Fig. 2), whereas those two variables were not significantly correlated in white participants (Fig. 3). Also, white subjects' COVID-19 related stress and personal diagnosis of COVID-19 were negatively correlated (Fig. 3), while those two variables were not significantly correlated in black subjects (Fig. 2). In other words, underserved populations’ COVID-19 symptom severity interacted more with their stress and discord at family levels than at individual levels. These differences can be another research topic for future studies in terms of why those different correlation patterns of stress and discord at family and individual levels were observed in the pandemic.
Conclusions
The study made empirical evidence that underserved populations are more mentally vulnerable to COVID-19 related stressors, which can cause a higher risk of having severe chronic illnesses. Thus, it is recommended that the government increases mental health accessibility for underprivileged people through telemental health services. Moreover, the research found the significance of family stress and discord in underserved populations under the pandemic. Thus, health professionals need to facilitate more community-based health programs to help underprivileged people better cope with family stress and conflict. Furthermore, the study discovered that socially marginalized populations were more often diagnosed with COVID-19 and had severe coronavirus symptoms. The research suggests that government and communities must increase health equity by strengthening the social structure for underserved populations’ health and safety.
Limitations
The study selected a cross-sectional design without investigating causal relationships. Future studies can address causality among variables in longitudinal study designs with multiple waves of data collection. Second, the research utilized self-reported survey results depending upon respondents’ recalls. Lastly, there was a lack of empirical studies about stress and discord in the COVID-19 pandemic. The majority of the previous studies were commentary, conceptual, or theoretical without abundant data collections.
Author statement/contributors
-
•
Dohyun Lee1, Ph.D., Department of Kinesiology & Recreation Administration, North Carolina Central University, Durham, NC 27707. Phone: 919–530–6162. E-mail: dohyun.lee@nccu.edu
-
•
Christopher Paul2, Ph.D., Department of Public Administration, North Carolina Central University, Durham, NC 27707. E-mail: cpaul5@nccu.edu
-
•
William Pilkington3, D.P.A, Julius L. Chambers Biomedical Biotechnology Research Institute, North Carolina Central University, Durham, NC 27707. E-mail: wpilkington@nccu.edu
-
•
Timothy Mulrooney4, Ph.D., Department of Environmental, Earth and Geospatial Sciences, North Carolina Central University, Durham, NC 27707. E-mail: tmulroon@nccu.edu
-
•
Nicole Diggs5, Ph.D., Department of Public Administration, North Carolina Central University, Durham, NC 27707. E-mail: sdiggs1@nccu.edu
-
•
Deepak Kumar6, Ph.D., Julius L. Chambers Biomedical Biotechnology Research Institute, North Carolina Central University, Durham, NC 27707. E-mail: dkumar@nccu.edu
Role of the funding source
This work is supported by the North Carolina Policy Collaboratory at the University of North Carolina at Chapel Hill with funding from the North Carolina Coronavirus Relief Fund established and appropriated by the North Carolina General Assembly.
Declaration of Competing Interest
There was no conflict of interest in the present study.
Acknowledgment
None.
References
- Alisha C.J., Rabbitt M.P., Gregory C.A., Singh A. United States Department of Agriculture, Economic Research Service; 2017. Household Food Security in the United States in 2016 (No. 291968) [Google Scholar]
- Ahn S., Norwood F.B. Measuring Food Insecurity during the Covid-19 Pandemic of Spring 2020. Appl Econ Perspect Policy. 2020 doi: 10.1002/aepp.13069. [DOI] [Google Scholar]
- Anderson J.C., Gerbing D.W. Structural equation modeling in practice: a review and recommended two-step approach. Psychol. Bull. 1988;103(3):411. [Google Scholar]
- Burström B., Tao W. Social determinants of health and inequalities in COVID-19. Eur. J. Public Health. 2020;30(4):617–618. doi: 10.1093/eurpub/ckaa095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2020a). Social-Ecological Model: A Framework for Prevention. Retrieved January 13, 2021, from https://www.cdc.gov/violenceprevention/publichealthissue/social-ecologicalmodel.html.
- Centers for Disease Control and Prevention (CDC). (2020b). Social determinants of health. Retrieved January 13, 2021, from https://www.cdc.gov/socialdeterminants/about.html.
- Centers for Disease Control and Prevention (CDC). (2021a). CDC COVID Data Tracker. Retrieved January 13, 2021, from https://covid.cdc.gov/covid-data-tracker/#cases_casesinlast7days.
- Centers for Disease Control and Prevention (CDC). (2021b). CDC COVID Data Tracker. Retrieved March 6, 2021, from https://covid.cdc.gov/covid-data-tracker/#datatracker-home.
- Cullen W., Gulati G., Kelly B.D. Mental health in the Covid-19 pandemic. QJM: Int. J. Med. 2020;113(5):311–312. doi: 10.1093/qjmed/hcaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis A., Mills J.W., Leitner M. Katrina and vulnerability: the geography of stress. J. Health Care Poor Underserved. 2007;18(2):315–330. doi: 10.1353/hpu.2007.0029. [DOI] [PubMed] [Google Scholar]
- Ding L., Velicer W.F., Harlow L.L. Effects of estimation methods, number of indicators per factor, and improper solutions on structural equation modeling fit indices. Struct. Eq. Model.: Multidiscipl. J. 1995;2(2):119–143. http://dx.doi.org/10.1080/10705519509540000. [Google Scholar]
- Free Statistics Calculator Version 4.0. A Priori Sample Size for Structural Equation Models. Retrieved from https://www.danielsoper.com/statcalc/calculator.aspx?id=89., 2021.
- Ferguson C.J., San Miguel C., Hartley R.D. A multivariate analysis of youth violence and aggression: the influence of family, peers, depression, and media violence. J. Pediatr. 2009;155(6):904–908. doi: 10.1016/j.jpeds.2009.06.021. [DOI] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. 2020;15(4) doi: 10.1371/journal.pone.0231924. ... [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray D.M., Anyane-Yeboa A., Balzora S., Issaka R.B., May F.P. COVID-19 and the other pandemic: populations made vulnerable by systemic inequity. Nat. Rev. Gastroenterol. Hepatol. 2020;17(9):520–522. doi: 10.1038/s41575-020-0330-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton The PhenX toolkit: get the most from your measures. Am. J. Epidemiol. 2011;174(3):253–260. doi: 10.1093/aje/kwr193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hébert J.R., Braun K.L., Kaholokula J.K.A., Armstead C.A., Burch J.B., Thompson B. Considering the role of stress in populations of high-risk, underserved community networks program centers. Prog. Community Health Partnerships: Res. Educ. Action. 2015;9:71. doi: 10.1353/cpr.2015.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H.S., Lim J.H. JypHyunJae Publishing Co; Seoul: 2013. Kujobangjeongshik Mohyungboonsekwa AMOS 20.0 [Structural Equation Modeling with AMOS 20.0] [Google Scholar]
- Marmot M. Social determinants of health inequalities. Lancet North Am. Ed. 2005;365(9464):1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- Moon S. Hakjisa; Seoul: 2013. Kujobangjeongshikmodelingeui Yehaewa Jeokyong [Basic Concepts and Applications of Structural Equation Modeling] [Google Scholar]
- Office of Disease Prevention and Health Promotion, Department of Health and Human Services. (2020). Healthy People 2030, U.S.Retrieved January 13, 2021, from https://health.gov/healthypeople/objectives-and-data/social-determinants-health.
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Rubenstein J.L., Halton A., Kasten L., Rubin C., Stechler G. Suicidal behavior in adolescents: stress and protection in different family contexts. Am. J. Orthopsychiatry. 1998;68(2):274–284. doi: 10.1037/h0080336. [DOI] [PubMed] [Google Scholar]
- Singu S., Acharya A., Challagundla K., Byrareddy S.N. Impact of social determinants of health on the emerging COVID-19 pandemic in the United States. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.00406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick B.G., Fidell L.S., Osterlind S.J. 5th ed. Pearson; New York, NY: 2001. Using Multivariate Statistics. [Google Scholar]
- Tinsley H.E., Tinsley D.J. Uses of factor analysis in counseling psychology research. J. Couns. Psychol. 1987;34(4):414. http://dx.doi.org/10.1037/0022-0167.34.4.414. [Google Scholar]
- Whaibeh E., Mahmoud H., Naal H. Telemental health in the context of a pandemic: the COVID-19 experience. Curr. Treat. Options Psychiatry. 2020;7(2):198–202. doi: 10.1007/s40501-020-00210-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Social Determinants of Health. Retrieved January 13, 2021, from https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1.