Abstract
Objective: To apply continuing care to elderly patients with hip fracture undergoing surgery, and to explore its impact on life quality and long-term functional recovery. Methods: This prospective study was performed in 136 elderly hip fracture patients, who were admitted to the department of orthopedics of our hospital for surgical treatment. According to the random number table, these patients were assigned to the control group and the experimental group (68 patients in each group). Patients in the control group received routine care and guidance for discharge, while those in the experimental group received routine care and continuing care for discharge. The hip joint function (Harris hip score), quality of life (MOS 36-item short form health survey score), compliance to functional exercise, anxiety (self-rating anxiety scale score), depression (self-rating depression scale score), postoperative complications (infection, joint stiffness, and deep vein thrombosis), and satisfaction in care after discharge were compared between the two groups. Results: Compared with the control group, the compliance to functional exercise (rates of compliance to exercise time, exercise action, and exercise site), Harris hip score at 3 months after discharge, MOS 36-item short form health survey scores in physical functioning, general health, social functioning, role-emotional, and mental health, and satisfaction in care outside the hospital in the experimental group were all increased (p<0.05). Meanwhile, self-rating anxiety scale score, self-rating depression scale score, and the incidence of complications like lung infection, joint stiffness, and deep vein thrombosis in the experimental group were lower than those in the control group (p<0.05). Conclusion: The effect of continuous care on life quality and long-term functional recovery of elderly patients with hip fractures is significant. Significant reduction of anxiety, depression, and complications is beneficial to improve satisfaction of care.
Keywords: Continuing nursing, hip fracture, Harris score, anxiety, depression
Introduction
Hip fracture is the fracture of femoral (thigh bone) neck, intertrochanteric, and subtrochanteric. It is mainly related to skeletal factors, including bone mass, femoral neck geometry, bone microstructure, and femoral transformation, falls caused by a variety of factors (such as taking sedatives, cognitive decline, physical disabilities, and gait and balance dysfunction), age factors, and genetic factors [1,2]. With the development of socialization and intensification of population aging, the incidence of hip fracture in the elderly population in China has been raised at a rate of 1% to 3% per year, posing a huge economic burden to the society [3]. Surgical treatment is the essential therapy for elderly patients with hip fracture. Most functional recovery of these patients requires home exercise. However, they are deficient in correct knowledge and skills on rehabilitation care. It means that they can’t receive hospital care when they are at home. Accordingly, prognostic effect is affected [4]. For patients receiving hip fracture surgery, the rehabilitation after discharge has become the focus of clinical attention.
Continuing care refers to the distinct collaborative and continuous care patients received in different health care places (like hospital and home), which is achieved through a series of measurements. In general, it is the shift of continuing care from hospital to home. The focal point is to help patients and their family members improve the self-care ability [5]. There are many reports on the application of continuing care in the postoperative care of elderly patients with hip fracture worldwide [6-9]. Continuing care helps to improve life quality, accelerate long-term functional recovery, and reduce complications. However, there are few reports on the effect of continuing care on anxiety and depression. Here, we applied continuing care to elderly patients with hip fractures and mainly explored its effect. We focused on the effect of continuing care on hip joint function, quality of life, compliance to functional exercise, anxiety, depression, complications, and satisfaction of care, hoping to provide guidance for clinical care.
Materials and methods
General information
This prospective study was conducted in 136 elderly hip fractures patients admitted to the department of orthopedics of The Second Affiliated Hospital of Xi’an Jiaotong University for surgical treatment between March 11, 2017 and July 15, 2019. According to the random number table, these patients were randomly divided into the control group (n=68) and the experimental group (n=68). The general information of patients in the two groups was shown in Table 1. This study was approved by the Ethics Committee of The Second Affiliated Hospital of Xi’an Jiaotong University.
Table 1.
Baseline data (x̅ ± sd, n)
| Group | Experimental group (n=68) | Control group (n=68) | χ2/t | P |
|---|---|---|---|---|
| Age (years) | 75.2±7.1 | 73.4±7.9 | 1.397 | 0.165 |
| Gender | 0.474 | 0.491 | ||
| Male | 39 | 35 | ||
| Female | 29 | 33 | ||
| Fracture site | 0.030 | 0.863 | ||
| Intertrochanteric fracture | 38 | 37 | ||
| Femoral neck fracture | 30 | 31 | ||
| Fracture type | 0.031 | 0.860 | ||
| Stable fracture | 41 | 42 | ||
| Unstable fracture | 27 | 26 | ||
| Comorbidities | ||||
| Hypertension | 11 | 13 | 0.201 | 0.652 |
| Diabetes | 9 | 10 | 0.061 | 0.804 |
| Coronary heart disease | 7 | 8 | 0.074 | 0.784 |
| Chronic bronchitis | 4 | 6 | 0.432 | 0.511 |
| Brain atrophy | 4 | 5 | 0.119 | 0.730 |
Inclusion criteria: Patients aged above 65 years; patients needed artificial hip replacement; patients or their family members agreed to take part in this study and signed the informed consent.
Exclusion criteria: Patients had traumatic fracture; patients had the history of mental illness or cognitive impairment; patients had vital organ failure; patients infected before admission; patients participated in other research projects.
Methods
In the control group, patients received routine care, which included perioperative care, postoperative diet, auxiliary rehabilitation exercise, and prevention of complications. One day before leaving the hospital, guidance for discharge was offered by the nurse in charge.
Patients in the experimental group received routine care and continuing care for discharge [6,9,10]. To be specific, continuing care consisted of the following 7 aspects: (1) establishment of the continuing care team. In total, 6 persons (including the department director, head nurse, attending physician, and head of the care team) joined the team; (2) development of a documentation for patients receiving continuing care. The documentation was composed of information such as name, hospitalization number, age, diagnosis, date of surgery, name of surgery, time of admission and discharge, treatment during hospitalization, physical recovery at discharge, telephone number, and home address; (3) formulation of the rehabilitation plan. Patients were instructed to complete step by step rehabilitation training and functional exercise. Also, they were guided to perform on-bed activities, including bridge exercise, isometric contraction exercise of gluteal muscles, hamstrings, quadriceps, and ankle joint flexors and extensors. After surgery, postoperative hip joint abduction training in standing position was carried out. Specifically, it was the practice of standing abduction movements with balanced body, which was maintained by supporting the back of a chair. The exercise could not only restore proprioception and thigh abduction muscle strength, but also help to improve walking gait. One month after surgery, on-bed activities and hip joint abduction training were consciously completed. Also, walking aid training was performed. With single crutches or canes, one-foot weight-bearing training, weight-bearing walking training, and hip joint exercise were performed to rehabilitate the balance function at 2 months after surgery. Three months after surgery, if the balance function was normal, patients could walk without crutches and climb up and down stairs; (4) every two weeks, a face-to-face consultation service, which lasted for 30-40 minutes, was provided after patients were discharged from the hospital; (5) distribution of health handbooks. According to the time after discharge from the hospital, handbooks with different contents were distributed. To be specific, diet and medication knowledge, rehabilitation exercise methods, content and prevention of complications were the main substance; (6) establishment of a dedicated telephone, text message, and WeChat platform. Hotline services were offered by specialist nurse. Health knowledge on postoperative rehabilitation was daily propagated through text messages and WeChat platform; (7) psychological consultation, relaxation therapy, and music therapy were taken to encourage patients to appropriately vent their emotions and relieve their anxiety and depression.
Outcome measures
Three months after discharge, the intervention effect was compared between the two groups.
Main outcome measures
Compliance to functional exercise, which included exercise time, exercise action, and exercise site, were compared between the two groups [11]. Compliance to functional exercise = full adherence to medical advice/the total number of patients * 100%.
Hip joint function, which was evaluated by Harris hip score, was compared between the two groups [12]. Pain, function, deformity, and joint mobility were the 4 aspects of the scale. The total score was 100 points. The higher the score was, the better the hip joint function.
Quality of life, which was accessed with MOS 36-item short form health survey (SF-36), was compared between the two groups. The Cronbach’s alpha coefficient was 0.75, while the structural coefficient was 0.825. The total score was 100 points. The higher the score was, the better the life quality [13].
Secondary outcome measures
The anxiety status was compared between the two groups with self-rating anxiety scale (SAS) [14]. There were anxiety symptoms when SAS score was over 50 points. The higher the SAS score was, the severer the anxiety.
The depression status was compared between the two groups using self-rating depression scale (SDS) [15]. Mild depression: 53-62 points; moderate depression: 63-72 points; severe depression: above 72 points. The higher the SDS score was, the severer the depression.
The incidence of complications, which was composed of lung infection, joint stiffness, and deep vein thrombosis of the lower extremities, was compared between the two groups [16]. Multiple complications observed in the same patient were counted based on the number of each complication. The incidence of complications = the number of complications/the total number of patients * 100%.
In order to assess the satisfaction in care, patients were required to fill in the self-made satisfaction survey scale (Supplementary Table 1). The validity of the scale was 0.87, while the Cronbach’s α coefficient was 0.89. Satisfied: 90-100 points; basically satisfied: 60-89 points; dissatisfied: <60 points. Satisfaction in nursing = (satisfied + basically satisfied)/the total number of patients * 100%.
Statistical methods
All data were analyzed using SPSS statistical software version 20.0. The enumeration data were calculated as number/percentage (n/%); comparison was conducted with chi-square test. The measurement data, which was normally distributed and had homogeneous variance, were calculated as mean ± standard deviation (x̅ ± sd); independent sample t test was used for inter-group comparison. The rank data was analyzed using rank sum test. The difference was statistically significant when P value was less than 0.05.
Results
Baseline data
There were no significant differences on general information such as age, gender, fracture site, fracture type, and comorbidities between the two groups (all P>0.05, Table 1).
Compliance to functional exercise
Compared with the control group, rates of compliance to exercise time, exercise action, and exercise site in the experimental group were improved (all P<0.05, Table 2).
Table 2.
Compliance to functional exercise (n, %)
| Group | Compliance to exercise time | Compliance to exercise action | Compliance to exercise site |
|---|---|---|---|
| Experimental group (n=68) | 57 (83.82) | 55 (80.88) | 52 (76.47) |
| Control group (n=68) | 32 (47.06) | 34 (50.00) | 40 (58.82) |
| χ2 | 18.752 | 14.338 | 4.838 |
| P | 0.000 | 0.000 | 0.028 |
Harris hip score
Harris hip score at 3 months after discharge in the experimental group was significantly increased when compared with the control group (P<0.05, Table 3).
Table 3.
Harris hip score (x̅ ± sd, score)
| Group | At discharge | 3 months after discharge |
|---|---|---|
| Experimental group (n=68) | 26.85±7.19 | 60.75±5.16*** |
| Control group (n=68) | 26.57±7.42 | 53.85±6.19*** |
| t | 18.421 | 7.061 |
| P | 0.065 | 0.000 |
Note: Compared with at discharge;
P<0.001.
SF-36 score
SF-36 scores in physical functioning, general health, social functioning, role-emotional, and mental health in the experimental group were higher than those in the control group (all P<0.05, Table 4).
Table 4.
SF-36 score (x̅ ± sd, score)
| Group | Experimental group (n=68) | Control group (n=68) | t | P |
|---|---|---|---|---|
| Physical functioning | 78.21±11.31 | 65.78±9.29 | 7.003 | 0.000 |
| General health | 91.61±10.20 | 85.50±12.26 | 3.159 | 0.002 |
| Social functioning | 72.32±11.27 | 65.48±10.30 | 3.694 | 0.000 |
| Role-emotional | 63.85±9.22 | 55.95±7.23 | 5.560 | 0.000 |
| Mental health | 68.55±10.21 | 57.45±7.40 | 7.259 | 0.000 |
Note: SF-36: MOS 36-item short form health survey.
SAS and SDS score
Compared with the control group, SAS and SDS score in experimental group was declined (both P<0.001, Figure 1).
Figure 1.
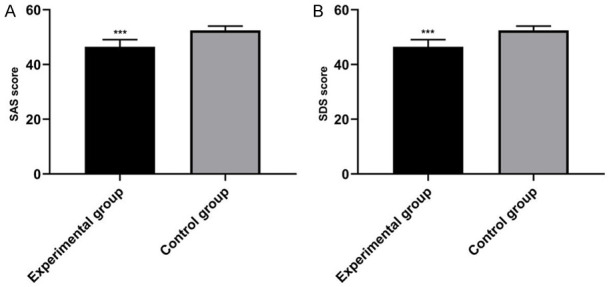
Comparison of SAS and SDS score between the two groups. A: SAS score; B: SDS score. Compared with control group, ***P<0.001. SAS: self-rating anxiety scale; SDS: self-rating depression scale.
Complications
The incidence of complications such as lung infection, joint stiffness, and deep vein thrombosis in the experimental group was significantly lower than that in the control group (P<0.05, Table 5).
Table 5.
Complications (n, %)
| Group | Lung infection | Joint stiffness | Deep vein thrombosis | The incidence of complications |
|---|---|---|---|---|
| Experimental group (n=68) | 2 (2.94) | 3 (4.41) | 0 (0.00) | 5 (7.35) |
| Control group (n=68) | 8 (11.76) | 4 (5.88) | 6 (8.82) | 18 (26.47) |
| χ2 | 3.519 | 8.843 | ||
| P | 0.172 | 0.003 | ||
Satisfaction in care
Satisfaction in care outside the hospital in the experimental group, which was composed of 35 cases of satisfied, 28 cases of basically satisfied, and 5 cases of dissatisfied, was significantly increased when compared with the control group (92.65% vs 79.41%, P<0.05, Table 6), which consisted of 27 cases of satisfied, 27 cases of basically satisfied, and 14 cases of dissatisfied.
Table 6.
Satisfaction in care (n, %)
| Group | Satisfied | Basically satisfied | Dissatisfied | Satisfaction in care |
|---|---|---|---|---|
| Experimental group (n=68) | 35 (51.47) | 28 (41.18) | 5 (7.35) | 63 (92.65) |
| Control group (n=68) | 27 (39.70) | 27 (39.70) | 14 (20.59) | 54 (79.41) |
| U/χ2 | 1.761 | 4.956 | ||
| P | 0.078 | 0.026 | ||
Discussion
In continuing care, rehabilitation exercise continuously performed during the shift from hospital to home. Compared with routine care, continuing care is more authoritative, and has higher degree of acceptance. For patients receiving no continuing care, they are short of strict supervision of home exercise. Some of them refuse to exercise independently, resulting in inferior long-term functional recovery [17]. In our study, we found that compliance to functional exercise (the rates of compliance to exercise time, exercise work, and exercise site were 83.82%, 80.88%, and 76.47%, respectively) and Harris hip score (3 months after discharge) in the experimental group were higher than those in control group. These were basically consistent with previous report, which also indicate that continuing care can effectively promote patients’ postoperative recovery of hip joint function [18].
Three months after surgery is critical for the recovery of elderly patients with hip fracture. Postoperative recovery is inevitably accompanied by a series of problems, such as depression and anxiety. In continuing care, relevant knowledge on home rehabilitation after hip fracture surgery, development of the disease, and psychological counseling were explained to patients. Accordingly, patients’ anxiety and depression are effectively reduced. They maintain a good psychological state, and have more confidence in functional recovery. A virtuous circle is then formed. In our study, we found that SAS and SDS score in the experimental group were decreased when compared with the control group, suggesting that continuing care can alleviate patients’ anxiety and depression after discharge.
After hip fracture surgery, complications are inevitable. What’s worse, these complications pose a great negative impact on the prognosis of the disease. The reduction of postoperative complications is of great importance for the treatment of the disease. Scientific rehabilitation exercise after discharge plays a significant role in the reduction of complications [19-21]. With improved compliance to functional exercise, patients’ physical fitness is improved through continuous scientific rehabilitation training. In our study, the incidence of complications in the experimental group (7.35%) was lower than that in the control group (26.47%), denoting that continuing care can not only improve patients’ compliance to functional exercise and hip joint function, but also reduce adverse reactions like postoperative infection, joint stiffness, and deep vein thrombosis. It is of positive significance for patients’ long-term rehabilitation. The incidence of complications was slightly higher than that reported by Wu et al. [6]. This might be related to the population enrolled. In our study, the elderly, who was prone to complications due to their unique population characteristics, was enrolled.
Continuing care helps to improve the quality of life. In continuing care, satisfied functional recovery is achieved after exercising in accordance with medical advice. In addition, more social and family support is offered. However, in routine care, the rate of compliance to functional exercise is low. Moreover, due to the poor psychological quality, patients are prone to severe postoperative anxiety and depression. As a result, postoperative prognosis is severely influenced, and the quality of life is reduced. In our study, SF-36 scores in physical functioning (78.21±11.31), general health (91.61±10.20), social functioning (72.32±11.27), role-emotional (63.85±9.22), and mental health (68.55±10.21) in the experimental group were significantly increased when compared with the control group, suggesting that patients receiving continuing care have improved life quality. These were basically consistent with the results reported by Wu et al. [6].
Finally, satisfaction of care after discharge was compared between the two groups. In continuing care, the compliance to rehabilitation exercise after discharge is increased. Meanwhile, anxiety and depression are reduced. Thereby, the incidence of complications is reduced, and clinical prognosis is improved. In other words, patients have a pleasant subjective experience of medical treatment. In our study, satisfaction of care in the experimental group was significantly higher than that in the control group.
However, we do not assess the anxiety, depression, and life quality of the main caregivers after discharge. A long-term care effect research will be conducted in an amplified sample to confirm the feasibility and importance of the continuing care in main caregivers and elderly patients undergoing surgery.
In summary, the effect of continuing care on life quality and long-term functional recovery of elderly patients with hip fractures is significant. Significant reduction of anxiety, depression, and complications is beneficial to, improve satisfaction of care.
Disclosure of conflict of interest
None.
Supporting Information
References
- 1.Berggren M, Karlsson A, Lindelöf N, Englund U, Olofsson B, Nordström P, Gustafson Y, Stenvall M. Effects of geriatric interdisciplinary home rehabilitation on complications and readmissions after hip fracture: a randomized controlled trial. Clin Rehabil. 2018;33:64–73. doi: 10.1177/0269215518791003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tomioka S, Fujino Y, Nakaya T, Ohtani M, Kubo T, Matsuda S. Equality of treatment for hip fracture irrespective of regional differences in socioeconomic status: analysis of nationwide hospital claims data in Japan. Tohoku J Exp Med. 2019;247:161–171. doi: 10.1620/tjem.247.161. [DOI] [PubMed] [Google Scholar]
- 3.Lynn R, Corrinda B, Nick F, Gordon S, Hollick R, Nguyen H, Prescott G, Marks A. Hip fracture incidence and mortality in chronic kidney disease: the GLOMMS-II record linkage cohort study. BMJ Open. 2018;8:e020312. doi: 10.1136/bmjopen-2017-020312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou W, Liu GH, Yang SH, Shao ZW, Mi BB. Systematic literature review on surgical treatment of elderly hip fractures. Chin J Orthop. 2017;37:1093–1099. [Google Scholar]
- 5.Mahon MM. Continuing care. Am J Nurs. 2019;119:10. doi: 10.1097/01.NAJ.0000580176.66064.d3. [DOI] [PubMed] [Google Scholar]
- 6.Wu YY, Xi RR, Zhou Y. Effect of continuous nursing on long-term functional recovery of elderly patients with hip fracture. J Clin Pathol. 2016;36:1717–1723. [Google Scholar]
- 7.Sun JL, Li QZ. Application value analysis of continuous nursing intervention in 90 patients with hip fracture. Genom Appl Biol. 2018;37:989–995. [Google Scholar]
- 8.He D, Qian HJ, Zhou L, Hu SL. A qualitative study on the continuous nursing needs of elderly patients with hip fracture after hip replacement. Chin J Mod Nurs. 2020;26:1188–1191. [Google Scholar]
- 9.Lv H, Wu Q. Effect of continuous nursing on postoperative functional recovery of elderly patients with hip fracture. Chongqing Med J. 2018;11:395–397. [Google Scholar]
- 10.Jia M, Zhang R, sun YY, Zhang CM. Effect of family rehabilitation nursing guidance on postoperative rehabilitation of elderly patients with hip fracture. Chin J Mod Nurs. 2018;24:1653–1656. [Google Scholar]
- 11.Si Q, Zhao Y, Li S, Sun WD. Analysis of functional exercise compliance after hip replacement. Med Clin Res. 2017;34:352–354. [Google Scholar]
- 12.Mahomed NN, Arndt DC, Mcgrory BJ, Harris WH. The Harris hip score: comparison of patient self-report with surgeon assessment. J Arthroplasty. 2001;16:575–580. doi: 10.1054/arth.2001.23716. [DOI] [PubMed] [Google Scholar]
- 13.de Melo DF, Martins FLM, Souza ADC, Galdino D, do Prado GF. Utilizao do SF-36 em ensaios clínicos envolvendo pacientes fibromiálgicos: determinao de critérios mínimos de melhora clínica. Rev Neurociências. 2019;12:147–151. [Google Scholar]
- 14.Dunstan DA, Scott N, Todd AK. Screening for anxiety and depression: reassessing the utility of the Zung scales. BMC Psychiatry. 2017;17:329. doi: 10.1186/s12888-017-1489-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sepehry AA. In: Zung self-rating depression scale. Sepehry AA, editor. New York: Springer; 2011. [Google Scholar]
- 16.Wei JX, Wang HH, Zhu WN, Ding QF. Analysis of clinical characteristics and influencing factors of complications in elderly patients with hip fracture. Sichuan Med J. 2017;038:39–42. [Google Scholar]
- 17.Shi LY, Chen Y, Yang Y. Evaluation of rehabilitation effect of continuous nursing after total hip replacement. J Xinjiang Med Univ. 2017;40:1362–1364. [Google Scholar]
- 18.Ding RX, Dai LF. Effect of “hospital community family” continuity nursing on discharged patients with limb dysfunction stroke. J Bengbu Med Coll. 2017;42:1003–1005. [Google Scholar]
- 19.Zhang L, Zhao JN. Prevention of complications after total hip arthroplasty. Chin J Orthop. 2018;31:6–10. doi: 10.3969/j.issn.1003-0034.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 20.Yan XJ, Yang YF, Wang S. Study on the intervention effect of continuous nursing in elderly patients after hip replacement. J Armed Police Logist Coll Med Edit. 2019;28:68–69. [Google Scholar]
- 21.Zhong XH, Song JM. Effect of continuous nursing on quality of life and treatment compliance of discharged patients with lung cancer. Chongqing Med J. 2020;49:746–749. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


